Abstract
Background/purpose
Stepwise removal (SWR) and selective removal (SCR) are proposed techniques to treat deep carious lesions, but it is currently uncertain which technique is better. This meta-analysis aimed to compare the therapeutic effects of SCR and SWR for deep carious lesions in both primary and permanent teeth.
Materials and methods
PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang, and VIP databases were searched until June 9, 2021. Success was the primary outcome. Secondary outcomes included pulp exposure, tooth extraction, pulp necrosis, pulpitis, and endodontic treatment. The effect size of each outcome was tested for heterogeneity. The source of heterogeneity was explored by meta regression analysis. Subgroup analysis and sensitivity analysis were conducted for the outcomes.
Results
Nine studies of 1550 patients with 1929 deep carious teeth were included. SCR had a significantly higher success rate than SWR (pooled relative risk [RR] = 1.123, 95% confidence interval [CI] = 1.056–1.194, I2 = 52.3%, P < 0.001). The incidence of pulp exposure was significantly lower in the SCR group than that in the SWR group (pooled RR = 0.266, 95%CI = 0.096–0.740, I2 = 0.0%, P = 0.011). The incidence of pulp necrosis in the SCR group was approximately 14.2% of that in the SWR group (pooled RR = 0.142, 95%CI = 0.026–0.789, I2 = 0.0%, P = 0.026). Compared with SWR, SCR reduced the incidence of pulpitis by about 76.3% (pooled RR = 0.237, 95%CI = 0.090–0.623, I2 = 0.0%, P = 0.003).
Conclusion
SCR may be a better treatment for deep caries to achieve better outcomes than SWR. Future research on comparing SCR and SWR for different outcomes in deep carious lesions is warranted to confirm our findings.
Keywords: Selective removal, Stepwise removal, Deep carious lesions, Meta-analysis
Introduction
Dental caries is a common oral disease caused by an ecologic shift within the dental biofilm, from a balanced microbial population to an acidogenic, aciduric and cariogenic microbial population developed and maintained through frequent consumption of fermentable dietary carbohydrates,1 with a high prevalence and causes a lot of health expenditure globally,2,3 affecting both children and adults.4 These affected populations usually develop deep caries when they do not obtain early and sufficient dental care and optimum systemic fluoride, and lack enough oral hygiene.5,6 In 2016, the International Caries Consensus Collaboration (ICCC) has radiographically defined deep caries as a condition where the teeth are damaged to 1/3 or 1/4 of the dentin near the dental pulp, or suffer from a risk of dental pulp exposure.1 Deep caries can cause severe inflammatory pulpal responses, and may lead to pulp necrosis, lowering quality of life.7,8 Therefore, it is of great necessity to take effective therapeutic measures.
Traditional treatment via the complete removal of deep carious lesions, removing all carious dentin to hard dentin, has been regarded as overtreatment, causing pulp exposure and pulp complications which usually need endodontic therapy.1,9, 10, 11 As alternatives, stepwise removal (SWR) and selective removal (SCR) of deep carious lesions are proposed. SWR is a two-step technique to remove carious lesions, with the first step of caries removal to soft dentin and placing a temporary restoration for sealing, and the second step of temporary restoration removal (re-entry), caries removal to firm dentin and placing a permanent restoration.12 Although it can decrease the risk of pulp exposure and maintain pulp vitality, the need for re-entry is in question because sealed lesions seem to be arrested clinically and radiographically.7,13,14 In SCR, partial removal of carious dentin and restoration are conducted in a single stage.12,15 SCR also reduces the incidence of pulp exposure and the loss of pulp vitality.16 Thus, SWR and SCR are recommended over the complete removal, as indicated by a Cochrane systematic review.17 Hoefler et al. showed that SCR related to fewer pulpal complications than SW in permanent teeth with deep dentin caries.18 SCR was found by Elhennawy et al. to present comparable success (absence of restorative/endodontic complications or pulp exposure) and restoration integrity to SWR 2 years later in primary molars with deep carious lesions.19 In anothor study, SE and SW also demonstrated similar success (absence of restorative/endodontic complications, indicating pulp vitality and restoration integrity) rate after 1-year for deep carious lesions in permanent teeth.20 A previous review reported that SCR to soft dentin had a higher success rate (pulp vitality survival rate), while SCR to firm dentin exhibited a lower success rate compared with SWR for permanent teeth with deep carious lesions.21 SWR and SCR can bring great success in pulp vitality and restorative outcomes for 3 years, and SCR can be more efficacious to maintain pulp vitality after deep caries treatment for permanent teeth, as proposed by doctor Brignardello-Peterse.22 As shown above for endodontic complications and pulp vitality, it is uncertain which of SWR and SCR is better in treating deep carious lesions.
This study aimed to comprehensively evaluate the efficacy of SCR versus SWR in the therapy of deep carious lesions by making a meta-analysis of randomized controlled trials (RCTs).
Materials and methods
Search strategy
Two authors searched PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang, and VIP databases until June 9, 2021. English search terms included “Caries” OR “Dental Caries” OR “Dental Decay” OR “Carious Lesion” OR “Carious Dentin” OR “Dental White Spot” AND “Incomplete Removal” OR “Incomplete Remove” OR “Incomplete Excavation” OR “Partial Removal” OR “Partial Excavation” OR “Stepwise Removal” OR “Stepwise Excavation” OR “Stepwise Excavate” OR “Ultraconservative Removal” OR “Ultraconservative Excavation” OR “Minimal Invasive Removal” OR “Minimal Invasive Remove” OR “Minimal Invasive Excavation” OR “Pulp Capping”. Disagreement was resolved via discussion with another author.
Inclusion and exclusion criteria
Studies with the following characteristics would be included: (1) patients with deep caries; (2) patients receiving SCR as the intervention (SCR group) and SWR as the control (SWR group); (3) comprising at least one of the following outcome measures; (4) RCTs; (5) studies in English and Chinese.
Studies would be excluded from our analysis according to the following criteria: (1) involving animal experiments; (2) having incomplete data or unable to provide valid data; (3) reviews, meta-analyses, case reports, conference reports, editorial materials, and protocols; (4) unable to get full texts.
Outcome measures
Success was the primary outcome. Secondary outcomes included pulp exposure, tooth extraction, pulp necrosis, pulpitis, and endodontic treatment.
Success outcome was defined as positive response to cold and/or heat testing, no sensitivity to percussion and palpation, no spontaneous pain, no fistula, no periodontal tissue swelling, no abnormal tooth movement, no periapical lesion, no inter-radicular or periapical radiolucency, no thickening of periodontal spaces, no pathological internal and external tooth resorption, and continuity of root and apex development in young permanent teeth with immature roots as to pulp vitality; no Charlie or Delta scores for all features of the modified USPHS criteria as to restorations.23
Data extraction and quality assessment
The extracted data included author, year of publication, author's country, study design, sample size, age (years), lesion extension, number of teeth, tooth type, SCR/SWR, cavity reopen interval (months), surface, arch, time of follow-up, and quality assessment. The modified Jadad scale was employed to evaluate study quality, with 1–3 as low quality and 4–7 as high quality.24 The above data extraction and quality assessment were carried out by two authors independently.
Statistical analysis
The relative risk (RR) value was used as the effect size, represented by a 95% confidence interval (CI). The effect size of each outcome was tested for heterogeneity. If the heterogeneity statistic I2 ≥ 50%, the random effect model was adopted for analysis; on the contrary, the fixed effect model was utilized. When I2 ≥ 50%, meta regression analysis was performed to explore the source of heterogeneity. Subgroup analysis was carried out based on tooth type and follow-up time. All the outcomes were subjected to sensitivity analysis. Statistical analysis was conducted using Stata 15.1 (Stata Corporation, College Station, TX, USA). P<0.05 indicated significant difference.
Results
Study selection
Up to June 9, 2021, 1733 publications were identified in PubMed, Embase, Web of Science, and Cochrane Library; 1360 articles were retrieved from CNKI, WanFang and VIP. After removing duplicates, 1914 studies were left. Then in consideration of titles and abstracts, 38 studies remained for full-text screening. At last, 9 English articles6,19,20,25, 26, 27, 28, 29, 30 were included in the current meta-analysis. Fig. 1 shows the flow chart of screening qualified studies.
Figure 1.
Flow chart for screening qualified studies.
Characteristics of included studies
The 9 included studies comprised 1550 patients with a total of 1929 deep carious teeth, of which 952 teeth belonged to the SCR group and 922 belonged to the SWR group. These studies were conducted between 2010 and 2021. Five studies25, 26, 27,29,30 had caries≥1/2 dentin, one6 had caries≥3/4 dentin, and three19,20,28 had caries>2/3 dentin. Besides, seven studies6,20,25, 26, 27,29,30 covered permanent teeth, and three studies6,19,28 covered deciduous teeth, of which one study6 covered both. Follow-up time ranged from 1 year to 5 years. As regards the quality of the eligible studies, 4 articles were of low quality and 5 of high quality. The baseline characteristics of the included studies are illustrated in Table 1.
Table 1.
Baseline characteristics of the included studies.
| Author | Year | Country | Study design | N | Age (years) | Lesion extension | Number of teeth | Tooth type | SCR/SWR | Cavity reopen interval (months) | Surfaces | Arch | Follow-up (months) | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maltz et al.25 | 2010 | Brazil | Multicenter randomized controlled clinical trial | 232 | 6–53 | Caries≥1/2 dentin | 299 | Permanent molars 299 | 153/146 | 2 | – | – | 24 | 3 |
| Orhan et al.6 | 2010 | Turkey | Randomized controlled clinical trial | 123 | 4–15 | Caries≥3/4 dentin | 154 | Primary mandibular second molars 94, permanent mandibular first molars 60 | 50/49 | 3 | – | – | 12 | 5 |
| Maltz et al.26 | 2012 | Brazil | Multicenter randomized controlled clinical trial | 233 | 17.17 ± 10.91 | Caries≥1/2 dentin | 299 | Permanent molars 299 | 152/147 | 4 ± 4 | One 184, two or more 29 | – | 36 | 4 |
| Maltz et al.27 | 2013 | Brazil | Multicenter randomized controlled clinical trial | 233 | 17.17 ± 10.91 | Caries≥1/2 dentin | 299 | Permanent molars 299 | 153/146 | 4 ± 4 | – | – | 18 | 3 |
| Elhennawy et al.28 | 2018 | Germany | Prospective, two-arm, parallel-group, single-blinded, randomized controlled superiority pilot trial | 74 | 6.3 ± 1.5 | Caries>2/3 dentin | 74 | Primary molars 74 | 37/37 | 6 | One 37, two 37 | Upper 32, lower 42 | 12 | 6 |
| Maltz et al.29 | 2018 | Brazil | Multicenter randomized controlled clinical trial | 233 | 17.17 ± 10.91 | Caries≥1/2 dentin | 299 | Permanent molars 299 | 152/147 | 4 ± 4 | One 200, two or more 29 | – | 60 | 3 |
| Labib et al.20 | 2019 | Egypt | Randomized controlled, clustered two-arm superiority trial | 115 | 29 ± 6 | Caries>2/3 dentine | 132 | Permanent premolars 58, permanent molars 74 | 66/66 | 3–4 | One 47, two or more 85 | Upper 55, lower 77 | 12 | 5 |
| Jardim et al.30 | 2020 | Brazil | Multicenter randomized controlled clinical trial | 233 | 17.2 ± 10.9 | Caries≥1/2 dentin | 299 | Permanent molars 299 | 152/147 | 4 ± 4 | One 150, two or more 22 | Upper 77, lower 95 | 60 | 3 |
| Elhennawy et al.19 | 2021 | Germany | Prospective, two-arm, parallel-group, single-blinded, randomized controlled superiority pilot trial | 74 | 6.3 ± 1.5 | Caries>2/3 dentin | 74 | Primary molars 74 | 37/37 | 6 | One 37, two 37 | Upper 32, lower 42 | 24 | 6 |
SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Primary outcome
Success
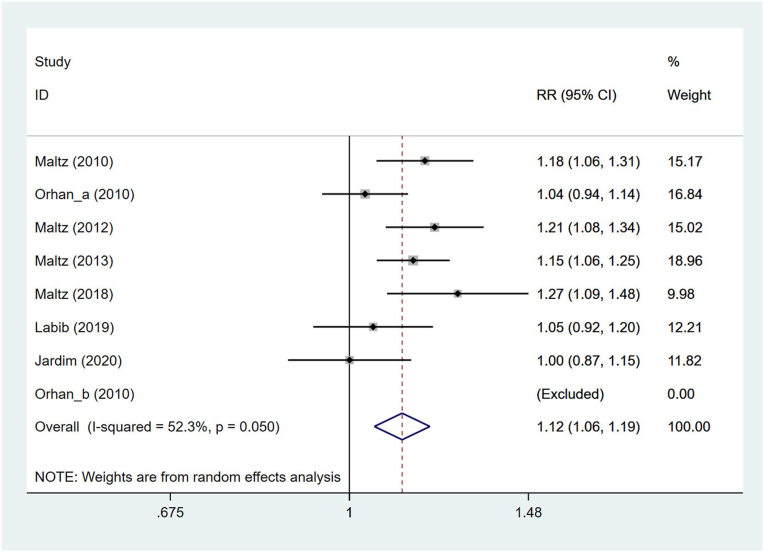
A total of 8 sets of data from 7 studies6,20,25, 26, 27,29,30 were used to assess success. The random effect model was applied after the heterogeneity test (I2 = 52.3%). According to the combined analysis, SCR had a significantly higher success rate than SWR (pooled RR = 1.123, 95%CI = 1.056–1.194, P < 0.001) (Fig. 2). Then subgroup analysis was conducted based on tooth type and follow-up time. No statistical difference was observed in the success rate between SCR and SWR when the teeth were primary teeth (RR = 1.035, 95%CI = 0.942–1.138, P = 0.474). For permanent teeth, SCR was significantly more successful than SWR (RR = 1.142, 95%CI = 1.075–1.214, I2 = 39.8%, P < 0.001). While follow-up time was less than 24 months (RR = 1.087, 95%CI = 1.010–1.169, I2 = 38.1%, P = 0.025) and 24–36 months (RR = 1.193, 95%CI = 1.106–1.287, I2 = 0.0%, P < 0.001), the success rate of SCR was significantly greater than that of SWR. SCR did not significantly differ from SWR concerning treatment success if follow-up period>36 months (RR = 1.123, 95%CI = 0.885–1.426, I2 = 81.4%, P = 0.34) (Table 2). Meta regression analysis used to detect the source of heterogeneity demonstrated that tooth type and follow-up time had nothing to do with the heterogeneity between studies (P > 0.05).
Figure 2.
Forest plot for success in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Table 2.
Comprehensive and subgroup analyses for different outcomes in the selective removal (SCR) group versus stepwise removal (SWR) group.
| Outcomes | RR (95%CI) | P | I2 |
|---|---|---|---|
| Success | |||
| Overall | 1.123 (1.056, 1.194) | <0.001 | 52.3 |
| Tooth type | |||
| Primary | 1.035 (0.942, 1.138) | 0.474 | NA |
| Permanent | 1.142 (1.075, 1.214) | <0.001 | 39.8 |
| Follow-up (months) | |||
| <24 | 1.087 (1.010, 1.169) | 0.025 | 38.1 |
| 24–36 | 1.193 (1.106, 1.287) | <0.001 | 0.0 |
| >36 | 1.123 (0.885, 1.426) | 0.34 | 81.4 |
| Pulp exposure | |||
| Overall | 0.266 (0.096, 0.740) | 0.011 | 0.0 |
| Tooth type | |||
| Primary | 0.464 (0.109, 1.979) | 0.300 | 0.0 |
| Permanent | 0.170 (0.038, 0.765) | 0.021 | 0.0 |
| Tooth extraction | |||
| Overall | 1.628 (0.400, 6.630) | 0.496 | 0.0 |
| Tooth type | |||
| Primary | 3.047 (0.325, 28.572) | 0.329 | 0.0 |
| Permanent | 0.951 (0.139, 6.522) | 0.959 | 0.1 |
| Follow-up (months) | |||
| <24 | 3.000 (0.318, 28.330) | 0.338 | 0.0 |
| 24–36 | 0.965 (0.143, 6.534) | 0.971 | 3.3 |
| Pulp necrosis | |||
| Overall | 0.142 (0.026, 0.789) | 0.026 | 0.0 |
| Pulpitis | |||
| Overall | 0.237 (0.090, 0.623) | 0.003 | 0.0 |
| Endodontic treatment | |||
| Overall | 0.681 (0.270, 1.721) | 0.416 | 0.0 |
| Follow-up (months) | |||
| <24 | 0.855 (0.313, 2.334) | 0.759 | 0.0 |
| 24–36 | 0.181 (0.009, 3.716) | 0.267 | NA |
SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval; NA, not available.
Secondary outcomes
Pulp exposure
Four studies6,20,27,28 including 5 sets of data evaluated pulp exposure. Owing to good homogeneity (I2=0.0%), the fixed effect model was adopted. It was revealed that the incidence of pulp exposure was significantly lower in the SCR group than that in the SWR group (pooled RR = 0.266, 95%CI = 0.096–0.740, P = 0.011) (Fig. 3). Subgroup analysis based on tooth type showed that for primary teeth, no statistical difference existed in the incidence of pulp exposure between the SCR and SWR groups (RR = 0.464, 95%CI = 0.109–1.979, I2 = 0.0%, P=0.300); with respect to permanent teeth, SWR led to a higher occurrence rate of pulp exposure than SCR (RR = 0.170, 95%CI = 0.038–0.765, I2 = 0.0%, P=0.021) (Table 2).
Figure 3.
Forest plot for pulp exposure in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
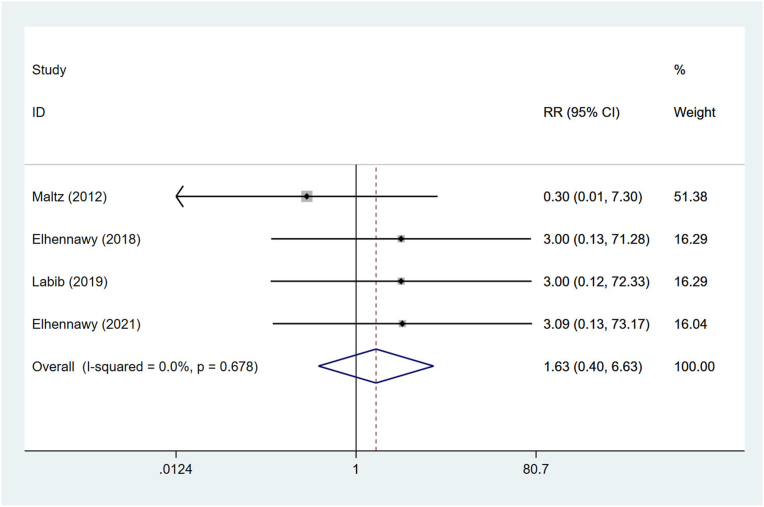
Tooth extraction
Tooth extraction was investigated in 4 trials.19,20,26,28 It turned out that SCR exerted a similar influence on tooth extraction to SWR (pooled RR = 1.628, 95%CI = 0.400–6.630, I2 = 0.0%, P = 0.496) (Fig. 4). After grouping based on tooth type and follow-up time, the results illustrated that no significant difference was observed between the SCR and SWR groups for both primary teeth (RR = 3.047, 95%CI = 0.325–28.572, I2=0.0%, P = 0.329) and permanent teeth (RR = 0.951, 95%CI = 0.139–6.522, I2=0.1%, P = 0.959); when follow-up time was <24 months (RR = 3.000, 95%CI = 0.318–28.330, I2=0.0%, P = 0.338) and 24–36 months (RR = 0.965, 95%CI = 0.143–6.534, I2=3.3%, P = 0.971), the incidences of tooth extraction in the two groups were comparable (Table 2).
Figure 4.
Forest plot for tooth extraction in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Pulp necrosis
Two studies26,27 were qualified to analyze the impacts of SCR and SWR on pulp necrosis. As a result, the incidence of pulp necrosis in the SCR group was approximately 14.2% of that in the SWR group (pooled RR = 0.142, 95%CI = 0.026–0.789, I2 = 0.0%, P = 0.026) (Fig. 5, Table 2).
Figure 5.
Forest plot for pulp necrosis in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Pulpitis
In regard to pulpitis, the comprehensive analysis of 2 studies26,27 exhibited that compared with the SWR group, the SCR group reduced the incidence of pulpitis by about 76.3% (pooled RR = 0.237, 95%CI = 0.090–0.623, I2 = 0.0%, P = 0.003) (Fig. 6, Table 2).
Figure 6.
Forest plot for pulpitis in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Endodontic treatment
Three reports20,26,27 probed into endodontic treatment. As illustrated in Table 2, SCR and SWR had similar impacts on endodontic treatment (pooled RR = 0.681, 95%CI = 0.270–1.721, I2 = 0.0%, P = 0.416). The SCR group did not significantly differ from the SWR group concerning endodontic treatment when follow-up time was shorter than 24 months (RR = 0.855, 95%CI = 0.313–2.334, I2 = 0.0%, P = 0.759) and within 24–36 months (RR = 0.181, 95%CI = 0.009–3.716, P = 0.267) (Fig. 7, Table 2).
Figure 7.
Forest plot for endodontic treatment in the SCR group versus SWR group. SCR, selective removal; SWR, stepwise removal; RR, relative risk; CI, confidence interval.
Sensitivity analysis
Sensitivity analysis was conducted by deleting one study and synthetically analyzing the remaining studies. Its result showed that one-study deletion did not significantly affect the overall outcomes, indicating that the findings of this meta-analysis were stable and robust, as shown in Table 2.
Discussion
The present meta-analysis made a comparison of SCR and SWR in terms of their therapeutic effects on deep carious lesions via comprehensively analyzing 9 RCTs with 1550 patients. It was indicated that SCR brought a higher success rate as well as lower incidences of pulp exposure, pulp necrosis and pulpitis than SWR for the population suffering from deep caries. These findings may serve as references for the treatment of deep carious lesions, and promote clinical decision-making, which may help patients obtain early treatment and favorable outcomes.
Aïem et al. found that pulp exposure and pulpo-periodontal complications did not differentiate between SWR and SCR for deep carious lesions in deciduous teeth via a meta-analysis of 2 RCTs.31 Another systematic review and meta-analysis demonstrated that SCR was associated with a reduced risk of pulp exposure but had similar success of maintaining pulpal health as compared with SWR in treating dental caries of permanent teeth.10 In this evaluation, we focused on the comparison of SCR and SWR for deep carious lesions in both primary and permanent teeth; tooth extraction, pulp necrosis, pulpitis, and endodontic treatment also acted as outcome measures apart from success and pulp exposure. Then SCR was shown to be more effective than SWR in regard to success, which was supported by a previous review to some extent that success rates were higher after SCR to soft dentin versus SWR in deep carious lesions.21 Besides, doctor Brignardello-Petersen22 pointed out that SCR and SWR had great success rates, but SCR can be more efficient in tooth vitality conservation which was a measure of success in the current study. In a systematic review, both SCR and SWR exhibited comparable success rates of >88% for permanent teeth with deep caries.18 These two techniques were successful in preserving pulp vitality for the treatment of deep carious lesions in primary and young permanent teeth as confirmed by Alsadat et al.,32 but which technique is optimal needs more investigations. Our preference for SCR was based on a relatively large sample size. To be specific, the success rate of SCR may be 1.123 times that of SWR in treating deep carious lesions. The lower success rate of SWR may be attributed to the patients’ low compliance with the second visit which may be caused by loss of temporary restorations. Hence, enduring materials could be placed to achieve sufficient cavity sealing to improve therapeutic effects.
This analysis also preferred SCR to SWR with respect to the incidence of pulp exposure, pulp necrosis and pulpitis for deep caries management. Specifically, the incidence of pulp exposure, pulp necrosis and pulpitis after SCR may be 73.4%, 85.8% and 76.3% lower than that after SWR, respectively. Consistently, Schwendicke et al. illustrated that SWR resulted in more pulp exposure, primarily in its second step, compared with SCR;33 and SWR raised the probability of pulp exposure in contrast to SCR, as concluded by Hoefler et al.18 According to a review, if deep caries could not be controlled and treated in a timely and effective manner, it would lead to pulpitis and eventually pulpal necrosis.34 Thus, the higher incidence of pulp exposure after SWR may relate to the greater occurrence rate of pulpitis and pulp necrosis in deep carious lesions. SCR and subsequent sealing were validated to hinder the progression of deep carious lesions since the bacteria in the cavity tissue were harmless after separation from the external environment,35 so the re-entry step could be unnecessary which may do harm to the pulp and worsen the lesion progress by mechanical means. Few studies are carried out to compare SCR with SWR in terms of pulp exposure, pulp necrosis and pulpitis except for the studies included in our meta-analysis, indicating that future investigations should pay more attention to these aspects. Furthermore, subgroup analysis was performed in the present assessment to enhance a deeper understanding of the impacts of two techniques on some outcomes from the perspective of tooth type and follow-up time. For permanent teeth, the success rate of SCR may be 14.2% greater than that of SWR, and SCR may reduce the incidence of pulp exposure by 83% versus SWR. When follow-up time was less than 24 months and 24–36 months, the success rate of SCR may be 8.7% and 19.3% higher than that of SWR, respectively. Although SCR and SWR exerted similar influences on primary teeth, considering the service life of deciduous teeth, the cost of treatment, and the discomfort of children increased by the second removal,1 it is not recommended to adopt SWR for deep caries in primary teeth.
Some strengths were displayed in our study. First, more data were provided on the comparison of SCR and SWR for deep carious lesions in both primary and permanent teeth. Second, pulpitis, pulp necrosis, endodontic treatment and tooth extraction were also measured. Limitations were as follows: first, the definition of the success outcome was inconsistent; second, the inclusion of low-quality articles may weaken the power of the results; third, literature in other languages was not included.
SCR brought a higher success rate as well as lower incidences of pulp exposure, pulp necrosis and pulpitis than SWR for patients with deep carious lesions. More investigations are necessary to reinforce our points.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This study was supported by the Sanming Project of Medicine in Shenzhen (SZSM202111012) and Shenzhen Fund for Guangdong Provincial High-level Clinical Key Specialties (No. SZGSP008).
References
- 1.Schwendicke F., Frencken J.E., Bjørndal L., et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res. 2016;28:58–67. doi: 10.1177/0022034516639271. [DOI] [PubMed] [Google Scholar]
- 2.Bernabé E., Sheiham A., Age, period and cohort trends in caries of permanent teeth in four developed countries Am J Public Health. 2014;104:e115–e121. doi: 10.2105/AJPH.2014.301869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Listl S., Galloway J., Mossey P.A., Marcenes W. Global economic impact of dental diseases. J Dent Res. 2015;94:1355–1361. doi: 10.1177/0022034515602879. [DOI] [PubMed] [Google Scholar]
- 4.Kassebaum N.J., Bernabé E., Dahiya M., Bhandari B., Murray C.J., Marcenes W. Global burden of untreated caries: a systematic review and mearegression. J Dent Res. 2015;94:650–658. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 5.Dean J.A. 10th ed. Elsevier; Amsterdam: 2016. Treatment of deep caries, vital pulp exposure, and pulpless teeth; pp. 221–242. [Google Scholar]
- 6.Orhan A.I., Oz F.T., Orhan K. Pulp exposure occurrence and outcomes after 1- or 2-visit indirect pulp therapy vs complete caries removal in primary and permanent molars. Pediatr Dent. 2010;32:347–355. [PubMed] [Google Scholar]
- 7.Bjørndal L., Reit C., Bruun G., et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci. 2010;118:290–297. doi: 10.1111/j.1600-0722.2010.00731.x. [DOI] [PubMed] [Google Scholar]
- 8.Clarkson J.E., Ramsay C.R., Ricketts D., et al. Selective caries removal in permanent teeth (SCRiPT) for the treatment of deep carious lesions: a randomised controlled clinical trial in primary care. BMC Oral Health. 2021;21:336. doi: 10.1186/s12903-021-01637-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwendicke F., Stolpe M., Innes N. Conventional treatment, hall technique or immediate pulpotomy for carious primary molars: a cost-effectiveness analysis. Int Endod J. 2016;49:817–826. doi: 10.1111/iej.12537. [DOI] [PubMed] [Google Scholar]
- 10.Barros M., De Queiroz Rodrigues M.I., Muniz F., Rodrigues L.K.A. Selective, stepwise, or nonselective removal of carious tissue: which technique offers lower risk for the treatment of dental caries in permanent teeth? A systematic review and meta-analysis. Clin Oral Invest. 2020;24:521–532. doi: 10.1007/s00784-019-03114-5. [DOI] [PubMed] [Google Scholar]
- 11.Barthel C.R., Rosenkranz B., Leuenberg A., Roulet J.F. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endod. 2000;26:525–528. doi: 10.1097/00004770-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Duncan H.F., Galler K.M., Tomson P.L., et al. European society of endodontology position statement: management of deep caries and the exposed pulp. Int Endod J. 2019;52:923–934. doi: 10.1111/iej.13080. [DOI] [PubMed] [Google Scholar]
- 13.Bjørndal L., Thylstrup A. A practice-based study on stepwise excavation of deep carious lesions in permanent teeth: a 1-year follow-up study. Community Dent Oral Epidemiol. 1998;26:122–128. doi: 10.1111/j.1600-0528.1998.tb01938.x. [DOI] [PubMed] [Google Scholar]
- 14.Kidd E.A. How 'clean' must a cavity be before restoration? Caries Res. 2004;38:305–313. doi: 10.1159/000077770. [DOI] [PubMed] [Google Scholar]
- 15.Schwendicke F., Dörfer C.E., Paris S. Incomplete caries removal: a systematic review and meta-analysis. J Dent Res. 2013;92:306–314. doi: 10.1177/0022034513477425. [DOI] [PubMed] [Google Scholar]
- 16.Edwards D., Bailey O., Stone S., Duncan H. The management of deep caries in UK primary care: a nationwide questionnaire-based study. Int Endod J. 2021;54:1804–1818. doi: 10.1111/iej.13585. [DOI] [PubMed] [Google Scholar]
- 17.Ricketts D., Lamont T., Innes N.P., Kidd E., Clarkson J.E. Operative caries management in adults and children. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD003808.pub3. Cd003808. [DOI] [PubMed] [Google Scholar]
- 18.Hoefler V., Nagaoka H., Miller C.S. Long-term survival and vitality outcomes of permanent teeth following deep caries treatment with step-wise and partial-caries-removal: a systematic review. J Dent. 2016;54:25–32. doi: 10.1016/j.jdent.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Elhennawy K., Finke C., Paris S., Reda S., Jost-Brinkmann P.G., Schwendicke F. Selective vs stepwise removal of deep carious lesions in primary molars: 24 months follow-up from a randomized controlled trial. Clin Oral Invest. 2021;25:645–652. doi: 10.1007/s00784-020-03536-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Labib M.E., Hassanein O.E., Moussa M., Yassen A., Schwendicke F. Selective versus stepwise removal of deep carious lesions in permanent teeth: a randomised controlled trial from Egypt-an interim analysis. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-030957. e030957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carvalho J.C., Dige I., Machiulskiene V., et al. Occlusal caries: biological approach for its diagnosis and management. Caries Res. 2016;50:527–542. doi: 10.1159/000448662. [DOI] [PubMed] [Google Scholar]
- 22.Brignardello-Petersen R. Stepwise and partial caries removal probably have high success rates up to 3 years after treatment of deep carious lesions, but partial caries removal is more likely to preserve tooth vitality. J Am Dent Assoc. 2017;148 doi: 10.1016/j.adaj.2017.02.012. e38. [DOI] [PubMed] [Google Scholar]
- 23.Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Invest 2005;9:215–232. [DOI] [PubMed]
- 24.Jadad A.R., Moore R.A., Carroll D., et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Maltz M., Moura M., Jardim J.J., Marques C., Paula L., Mestrinho H.D. Partial caries removal in deep lesions: 19-30 months follow-up study. 2010;51:20–23. [Google Scholar]
- 26.Maltz M., Garcia R., Jardim J.J., et al. Randomized trial of partial vs. stepwise caries removal: 3-year follow-up. J Dent Res. 2012;91:1026–1031. doi: 10.1177/0022034512460403. [DOI] [PubMed] [Google Scholar]
- 27.Maltz M., Jardim J.J., Mestrinho H.D., et al. Partial removal of carious dentine: a multicenter randomized controlled trial and 18-month follow-up results. Caries Res. 2013;47:103–109. doi: 10.1159/000344013. [DOI] [PubMed] [Google Scholar]
- 28.Elhennawy K., Finke C., Paris S., Reda S., Jost-Brinkmann P.G., Schwendicke F. Selective vs stepwise removal of deep carious lesions in primary molars: 12-months results of a randomized controlled pilot trial. J Dent. 2018;77:72–77. doi: 10.1016/j.jdent.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 29.Maltz M., Koppe B., Jardim J.J., et al. Partial caries removal in deep caries lesions: a 5-year multicenter randomized controlled trial. Clin Oral Invest. 2018;22:1337–1343. doi: 10.1007/s00784-017-2221-0. [DOI] [PubMed] [Google Scholar]
- 30.Jardim J.J., Mestrinho H.D., Koppe B., et al. Restorations after selective caries removal: 5-year randomized trial. J Dent. 2020;99:103416. doi: 10.1016/j.jdent.2020.103416. [DOI] [PubMed] [Google Scholar]
- 31.Aïem E., Joseph C., Garcia A., Smaïl-Faugeron V., Muller-Bolla M. Caries removal strategies for deep carious lesions in primary teeth: systematic review. Int J Paediatr Dent. 2020;30:392–404. doi: 10.1111/ipd.12616. [DOI] [PubMed] [Google Scholar]
- 32.Alsadat F.A., El-Housseiny A.A., Alamoudi N.M., Alnowaiser A.M. Conservative treatment for deep carious lesions in primary and young permanent teeth. Niger J Clin Pract. 2018;21:1549–1556. doi: 10.4103/njcp.njcp_202_18. [DOI] [PubMed] [Google Scholar]
- 33.Schwendicke F., Meyer-Lueckel H., Dörfer C., Paris S. Failure of incompletely excavated teeth–a systematic review. J Dent. 2013;41:569–580. doi: 10.1016/j.jdent.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 34.Bjørndal L., Simon S., Tomson P.L., Duncan H.F. Management of deep caries and the exposed pulp. Int Endod J. 2019;52:949–973. doi: 10.1111/iej.13128. [DOI] [PubMed] [Google Scholar]
- 35.Oliveira E.F., Carminatti G., Fontanella V., Maltz M. The monitoring of deep caries lesions after incomplete dentine caries removal: results after 14-18 months. Clin Oral Invest. 2006;10:134–139. doi: 10.1007/s00784-006-0033-8. [DOI] [PubMed] [Google Scholar]