Autogenous tooth transplantation (ATT) refers to the relocation of an autogenous tooth to another tooth extraction site or a surgically formed recipient site.1 Although ATT has been performed for centuries, its popularity has varied over the years due to its unpredictable results. The key factor that affects the success rate of ATT is the vitality of the periodontal ligament (PDL) of the donor tooth. Mechanical injuries and prolonged extraoral time during operation can damage the PDL.2 Over the past ten years, three-dimensional (3D) printing technology has become more attainable for clinicians and has enabled them to administer more accurate, cost-effective, and time-efficient treatments to patient.3 This paper describes a case of ATT wherein we transplanted the lower third molar to the second molar position using a 3D replica and presurgical cone-beam computed tomography (CBCT) in an anatomically challenging site to increase the success rate of ATT.
A 24-year-old male patient presented to our outpatient department on January 20, 2021, with a complaint of gingival swelling and bleeding in the lower left posterior tooth for 3 months. Intraoral examination revealed large caries with polyps and gingival swelling over the distal side of tooth 37. Radiography revealed severe carious destruction of tooth 37 with questionable prognosis (Fig. 1A and B). During the examinations, we found that tooth 38 was nonfunctional and malpositioned (Fig. 1C). Therefore, we planned to replace tooth 37 with tooth 38. Presurgical CBCT was performed to analyze the geometry of the surgical site and the donor tooth. The results indicated a severe lingual depression of the submandibular fossa under tooth 37; however, preparing the recipient site was considered more critical (Fig. 1D and E). Thus, a 3D replica of the donor tooth was used to prepare and fit the extraction socket of tooth 37 before actual transplantation of tooth 38. Postsurgical root canal therapy and restoration were then administered, and the results were satisfactory (Fig. 1F and J).
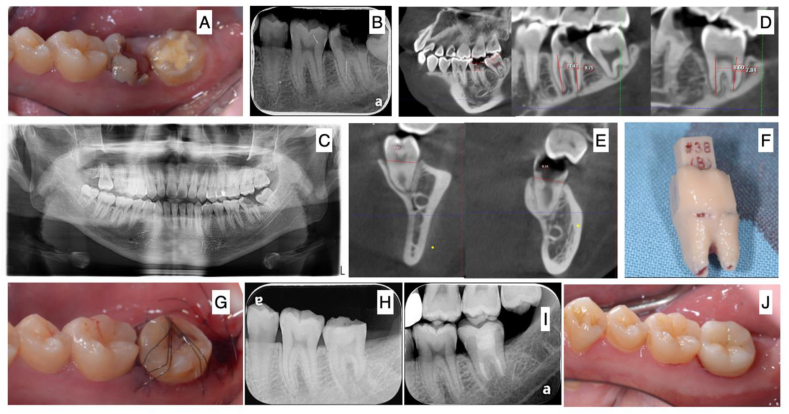
Figure 1.
Clinical photographs and radiographs of the case. (A) Large polyps and caries with gingival swelling on the distal side of tooth 37. (B) Severe carious destruction in the distal area of tooth 37. The distance between margin of caries and furcation was less than 4 mm. (C) Teeth 28, 38, and 48 can be regarded as candidate donor teeth for autogenous tooth transplantation. (D) Demonstrations of presurgical CBCT analysis of the geometry of surgical site and donor tooth. Tooth 38 was considered the most suitable donor tooth. (E) Severe lingual depression of submandibular fossa noted under tooth 37. (F) 3D-printed tooth replica. (G) Clinical photograph showing that tooth 38 was transplanted to the socket of tooth 37 perfectly and was splinted with sutures. (H) Endodontic treatment administered within 2 weeks after tooth transplantation. (I) Overlay restoration administered to restore the occlusal function on July 5, 2022. (J) Postsurgical intraoral photo of tooth 38 5 months after the surgery. No discomfort or any symptoms or signs were noted.
The key factor determining the success of ATT is the PDL vitality of the donor tooth.4 Presurgical CBCT is used to analyze both the donor tooth and the recipient site because it serves the following purposes: it 1) generates a precise 3D-printed analog donor tooth, 2) measures the geometry of the donor tooth and recipient site for clinical adjustment during surgery, and 3) helps plan the optimal biologic position of the transplanted tooth. The use of the 3D-printed tooth replica reduces the number of fitting attempts to achieve a good fit of the donor tooth in the modified socket during surgery. Therefore, the chances of iatrogenic damage to the PDL are avoided.5 Another benefit of the 3D replica is reduced extraoral time, which enhances the vitality of the attached PDL. Thus, with the aid of CBCT and a 3D-printed tooth replica, the success rate of ATT has increased. With proper case selection and appropriate surgical techniques, ATT may be a feasible treatment option in addition to implants and fixed partial dentures.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
All the authors declare no potential financial and nonfinancial conflicts of interest.
Acknowledgments
None.
Contributor Information
Yen-Wen Huang, Email: marr529@yahoo.com.tw.
Chih-Yuan Fang, Email: 100044@w.tmu.edu.tw.
References
- 1.Andreasen J.O., Paulsen H.U., Yu Z., et al. A long-term study of 370 autotransplanted premolars. Part I. Surgical procedures and standardized techniques for monitoring healing. Eur J Orthod. 1990;12:3–13. doi: 10.1093/ejo/12.1.3. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen J.O. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg. 1981;10:54–61. doi: 10.1016/s0300-9785(81)80008-7. [DOI] [PubMed] [Google Scholar]
- 3.Turkyilmaz I., Wilkins G.N. 3D printing in dentistry- exploring the new horizons. J Dent Sci. 2021;16:1037–1038. doi: 10.1016/j.jds.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsukiboshi M. Autotransplantation of teeth: requirements for predictable success. Dent Traumatol. 2002;18:157–180. doi: 10.1034/j.1600-9657.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- 5.Moin D.A., Verweij J.P., Waars H., Merkesteyn R.V., Wismeijer D. Accuracy of computer- assisted template-guided autotransplantation of teeth with custom three-dimensional designed/printed surgical tooling: a cadaveric study. J Oral Maxillofac Surg. 2017;75:925.e1–925.e7. doi: 10.1016/j.joms.2016.12.049. [DOI] [PubMed] [Google Scholar]