Abstract
Crohn's disease (CD) is a chronic inflammatory disease mainly affecting the gastrointestinal tract. With the increased availability of modalities in the last two decades, the treatment of CD has advanced remarkably. Although medical treatment is the mainstay of therapy, most patients require surgery during the course of their illness, especially those who experience complications. Nutritional optimization and ERAS implementation are crucial for patients with CD who require surgical intervention to reduce postoperative complications. The increased surgical risk was found to be associated with the use of corticosteroids, but the association of surgical risk with immunomodulators, biologic therapy, such as anti‐TNF mediations, anti‐integrin medications, and anti‐IL 12/23 was low in certainty. Decisions about preoperative medication must be made on an individual case‐dependent basis. Preoperative imaging studies can assist in the planning of appropriate surgical strategies and approaches. However, patients must be informed of any alterations to their treatment. In summary, the management of perioperative medications and surgery‐related decision‐making should be individualized and patient‐centered based on a multidisciplinary approach.
Keywords: Crohn's disease, enhanced recovery after surgery, nutritional support, perioperative care
Most Crohn's disease patients require surgery during the course of their illness, especially those who experience complications. The management of perioperative medications and surgery‐related decision‐making should be individualized and patient‐centered based on a multidisciplinary approach.

1. INTRODUCTION
Crohn's disease (CD) is a chronic relapsing inflammatory disease mainly affecting the gastrointestinal tract. Often characterized by abdominal pain, fever, or diarrhea with blood or mucus passage, 1 CD is primarily treated medically; however, most patients require more than one surgery during the course of their illness and must therefore be evaluated through a multidisciplinary approach. 2 , 3 The common indications for surgery in patients with CD include abscesses, complex internal fistulas, fibrostenotic strictures, free perforation with peritonitis, and massive hemorrhage unresponsive to other therapies. 4 , 5 In addition, Crohn's colitis‐associated dysplasia and cancer are also indications for surgery in CD patients. 6 , 7 Surgery for CD carries a high risk of complications. With the increased availability of biologics in the last two decades, the treatment of CD has advanced considerably. However, questions about the surgical trend, rate, and perioperative management of biologics remain. In this review, we compiled up‐to‐date information about the temporal trend of surgery, nutrition, and medication consideration; enhanced recovery after surgery (ERAS); the perioperative care of CD; image and surgical dilemmas in CD surgery; and finally, recurrence and complications in CD surgery.
2. TEMPORAL TREND OF CD SURGICAL RATE, INDICATIONS, AND METHODS
The lifetime risk of bowel resection in patients with CD has historically been high, and many patients require several surgeries. 8 , 9 Approximately 40% to 50% of patients with CD undergo intestinal surgery within 10 years of diagnosis, and the risk of postoperative recurrence was approximately 50% within 10 years. 10 These percentages have improved over time, with patients who received diagnoses in the 1990s having an approximate 14%, 28%, and 39% risk of surgery at 1, 5, and 10 years, respectively, from the initial diagnosis. 11
The management of CD has changed considerably over the last 20 years. Immunomodulators and biological therapies now play key roles in treating patients with CD. Current reports have indicated that surgery rates at 1 and 5 years in the postbiologic era are lower than those recorded in the prebiologic era (14.8% and 31.2% vs. 12.6% and 24.2%, respectively). 11 , 12 Although no direct comparison has been made between Eastern and Western countries, the surgical rate is either compatible 13 , 14 or less in Eastern countries than that in Western countries. 15 , 16
During the past decade, several population‐based studies have assessed the temporal trends of CD surgery, but results have been conflicting. 12 , 17 In a Swedish population‐based database study, the cumulative incidence of the first abdominal surgical procedure following a CD diagnosis decreased by two‐thirds over the past 25 years, whereas the rate of repeat surgery has remained stable despite the introduction of biological therapy. 18 In a Canadian population‐based study from 1996 to 2013, surgery rates in a large population of adult patients with CD decreased by 8.4% each year. 19 In addition, a paradigm shift has occurred whereby elective operations have become more common than emergent surgeries. 20 Although anti‐tumor necrosis factor (TNF) therapy plays a role, this decrease in surgical trends is likely multifactorial, owing to a decline in smoking trends, earlier diagnosis, earlier treatment, improved patient education, and changes in clinical practice. 19 Because biologics such as vedolizumab (VDZ) and ustekinumab (UST) have been available for less than 10 years, estimating the real effect on the CD surgical rate would currently be difficult.
Surgical resection is the treatment of choice for localized CD of the small bowel or colon that is unresponsive to medical treatment. The uptake of minimally invasive surgery in combination with enhanced recovery programs can reduce both complications and hospital stay. 21 An increased use of laparoscopy and decreased intraoperative blood loss may have contributed to offsetting of the impact of increased comorbidity. The rate of penetrating or complicated cases requiring surgical treatment has increased, preoperative biological therapy is more often used, and extensive surgical procedures are more frequently performed. 22 The need for surgery remains, alongside the earlier use of biologicals, an appropriate therapeutic choice for some CD patients with complications.
Stricture is one of the major complications in CD patients, in up to 50% of patients in European countries and in 20.1% to 39.9% patients in Asian countries. 23 Endoscopic balloon dilatation (EBD) can delay or avoid surgery with either initial or recurrent strictures and is a safe and effective procedure for CD‐related stricture. 24 Intestinal strictures longer than 4–5 cm and severely inflamed with ulcers were considered high risk and a potential contraindication to EBD. 23 Surgical treatment, such as strictureplasty, plays an important role in managing the stricture of CD patients, especially when the stricture location is not accessible by endoscopy or the patients were evaluated as high risk/contraindicated for EBD. 25 We also have to be aware of the contraindications for strictureplasty, such as phlegmon or fistula, more than one stricture over a short bowel length, perforation, and any stricture with evidence of dysplasia or malignancy. 26
It is known that there is increased risk of intestinal cancer in CD patients. 6 , 27 A meta‐analysis, which was based on six Western population studies showed an increased risk of intestinal cancer in CD (SIR 1.9; 95% CI, 1.4–2.5). 28 In Asia, only a few population‐based studies have examined the association between IBD and CRC development. 13 A study from Taiwan found that the risk of CRC was not increased significantly in CD (SIR 0.96) compared to the background population. 29 In contrast, a study from Korea found an increased risk of developing CRC in CD patients (SIR: 3.67; 95% CI: 1.58–7.22). 30 Because of the limited number of population‐based studies and relatively short follow‐up duration in Eastern countries, it is difficult to compare the incidence of colitis‐associated intestinal cancer between Western and Asian populations. Intestinal cancer in CD may develop in anorectal regions, especially in CD patients with chronic severe anorectal disease, rectal remnant, and strictures. 31 , 32 , 33 , 34 In addition, the incidence of anorectal cancer in CD may be higher in Asia than in Western countries. 35 Therefore, patients with longstanding disease who have chronic non‐healing fistula, increase in bloody discharge, or increasing perianal pain should undergo examination under anesthesia with biopsy and curettage of the fistula track as well as close endoscopic and radiographic surveillance. 36
3. IMAGING IN A PERIOPERATIVE SETTING
Cross‐sectional imaging is recommended for preoperative evaluation in patients with CD 5 , 37 to assist in defining the disease extent, assessing disease activity, and detecting complications such as strictures, fistulas, and abscesses.
The three main imaging modalities available are magnetic resonance imaging (MRI), computed tomography (CT), and intestinal ultrasound (IUS). The enterography technique is also used for small bowel distension in MRI and CT. MRI and CT have high and comparable accuracy for the diagnosis and detection of complications in patients with CD. 38 , 39 IUS is also a reliable diagnostic tool, although its accuracy is lower than that of the other tools for disease proximal to the terminal ileum. 38 Because of the absence of radiation exposure, MRI is preferred over CT in elective settings, especially for young patients. However, in emergency settings, CT is recommended because of its wide availability and short scanning time compared with MRI. 37 In addition, CT is sufficiently sensitive to detect intraperitoneal free gas and should be performed when intestinal perforation is suspected. 40
Most guidelines recommend biological therapy, in particular anti‐TNF, in addition to the antibiotics and/or drainage for patients with complex perianal CD. 41 , 42 For evaluation of perianal fistulizing CD, pelvic MRI is the preferred first‐line test. 40 MRI is superior to CT in terms of its soft tissue contrast for the delineation of fistula morphology and the relationship with the anal sphincter complex (Figure 1). The most commonly used classification is the Parks classification, which includes four types of fistulas: intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric. 43 It can help to determine the complexity of the treatment procedure. Transrectal ultrasonography is an alternative to MRI, though the combined use of these two tools with examination under anesthesia can further improve diagnostic accuracy. 44 Understanding the anatomy of perianal fistula and evaluation of the presence of proctitis are imperative for the selection of appropriate options for surgical repair, 42 , 45 including loose seton, 46 , 47 fistulotomy, 41 disconnection procedures (advancement flaps, 48 the ligation of the intersphincteric fistula tract [LIFT] procedure 49 ), infill procedures (glues, 50 , 51 plugs 52 ), and ablative procedures (video‐assisted anal fistula treatment [VAAFT], 53 fistula tract using laser [FiLaC] 54 ). Recently, there is still a promising treatment using mesenchymal stem cells to treat CD‐related fistula. 55
FIGURE 1.
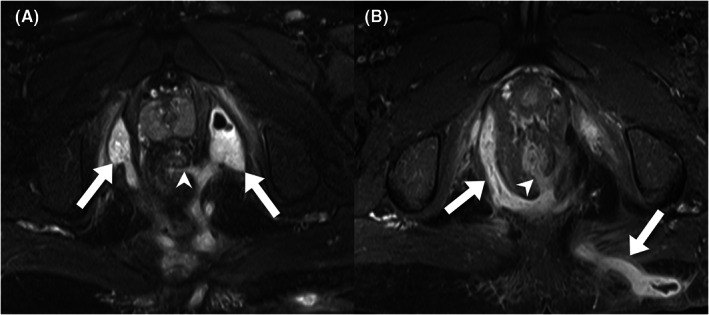
Pelvic MRI of a 20‐year‐old man with CD for preoperative evaluation of the perianal fistula. (A) An axial T2‐weighted image with fat saturation presents a suprasphincteric fistula tract at the 3 o'clock position (arrowhead), with branching and abscess formation at bilateral ischioanal fossae (arrows). (B) a postcontrast axial T1‐weighted image of another fistula tract (arrowhead), with branching fistulae extending to the right ischioanal fossa and left gluteal region (arrows)
Percutaneous image‐guided drainage is recommended as the primary treatment for well‐defined accessible intraabdominal abscesses in CD (Figure 2). 4 The successful drainage rate is 74% to 100%, 56 which can negate the need for subsequent surgery in 29.3% of patients. 57 Percutaneous drainage can serve as a bridge to elective surgery, during which time medical and nutritional optimization can be implemented.
FIGURE 2.
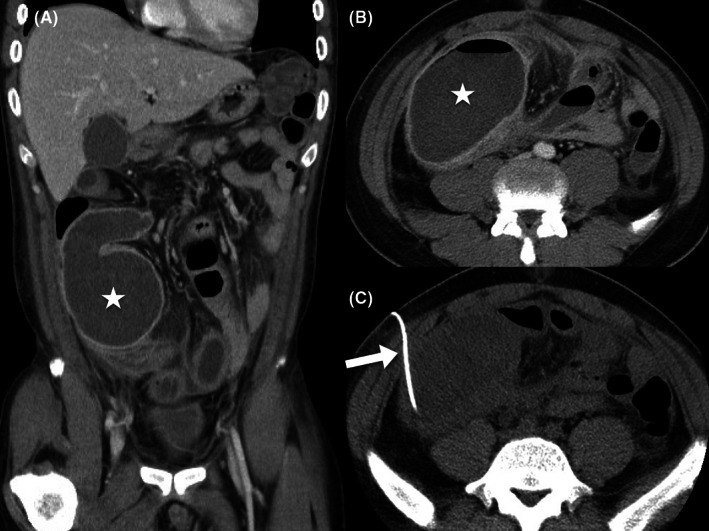
Contrast‐enhanced CT of a 29‐year‐old man with CD who presented with right lower quadrant pain that lasted for 3 months. (A and B) coronal and axial images of inflammatory changes of the ileal loops, with a large abscess formation (star) on the lower right abdomen. (C) CT‐guided percutaneous drainage of the abscess was performed, and a pigtail catheter (arrow) was inserted into the abscess. The abscess was successfully treated
Detection of small bowel and colorectal cancer in patients with IBD is challenging. The presenting symptoms may overlap with active IBD, and the endoscopic biopsy sometimes could be false‐negative and the definite diagnosis is made only after surgery. On imaging, the tumor may present as a soft tissue mass, which is helpful for the diagnosis; but in a substantial number of cases, it may present as stenosis with circumferential wall‐thickening, which is difficult to differentiate from inflammation or fibrotic stricture. 58 , 59 Symptomatic strictures in patients with long‐standing IBD after a prolonged remission, or strictures refractory to medical therapy, should be evaluated carefully and may refer for surgical consultation. 60
Imaging studies assist in the planning of appropriate surgical strategies and approaches. However, studies have reported that unexpected intraoperative findings lead to modification of the planned surgical procedure in 9% and 26% of patients. 61 , 62 Therefore, surgeons should always search for possible additional lesions intraoperatively, and patients should be informed of the possibility of procedure modification.
4. PERIOPERATIVE NUTRITIONAL MANAGEMENT OF CD
Nutritional optimization is essential for surgical patients to obtain favorable surgical outcomes. Presurgical malnutrition could increase the incidence of complication, such as infection, abscesses, anastomotic leakage, and ineffective wound healing. 63 , 64 The European Society for Clinical Nutrition and Metabolism guidelines on inflammatory bowel disease (IBD) recommend integration of nutritional support into the overall medical management of patients with IBD requiring surgery. The ERAS guidelines should be applied in perioperative management. 65
Presurgical nutrition screening should be executed to identify patients with a high risk of malnutrition, such as in patients with enterocutaneous fistula. 66 , 67 Severe malnutrition is indicated when at least one of the following criteria are met: (1) more than 10% to 15% of unintentional weight loss within 6 months; (2) a body mass index of less than 18.5 kg/m2; and (3) a serum albumin level of less than 30 g/L (without hepatic or renal dysfunction). Because they are influenced by active disease, serum albumin levels should be carefully interpreted. 68 , 69 For elective surgical patients with malnutrition, surgery should be postponed in favor of administering an oral nutrition supplement (ONS), enteral nutrition (EN), peripheral parenteral nutrition (PN), or total parenteral nutrition supplementary to EN support for 7 to 14 days. Longer support periods might be necessary for severely malnourished patients. 68 , 69
EN is preferred over PN if gastrointestinal function is not contraindicated. Because nutrition requirements cannot be fulfilled through natural food intake, natural food intake with ONS is advised. The nasogastric or nasojejunal feeding routes are alternatives when oral intake is impossible. Because EN support cannot fulfill more than 60% of nutrition requirements, PN support can be considered. 65 , 68 Protein intake must be increased to 1.2–1.5 g/kg in patients with active IBD. 68 Micronutrient deficiencies, such as in iron, vitamin B12, vitamin D, and zinc should be monitored and corrected in timely manner. 68 Patients should begin natural food intake (gradually progressing form clear liquids, low residue semisolids, and low residue solids to a normal diet) or EN support as early as possible if the gastrointestinal function is not compromised. 68 , 69 , 70 , 71 If EN is impossible, PN can be used for nutritional support. 68 , 69 , 70 The perioperative nutritional management is summarized in Figure 3.
FIGURE 3.
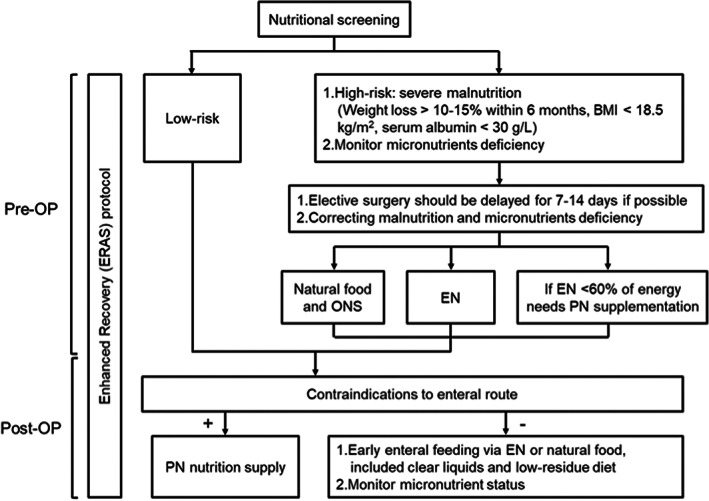
Perioperative nutritional management of CD
5. PERIOPERATIVE PHARMACOTHERAPY
5.1. Immunomodulation
Immunomodulators suppress inflammation through T‐cell‐mediated mechanisms. The suppression of the inflammatory process by T cells may cause impaired collagen synthesis and reduce strength, which may increase the risk of anastomotic dehiscence. 72
A retrospective international multicenter study 73 enrolled 231 patients undergoing ileocolonic resections for active CD to examine the relationship between preoperative immunosuppressive and biologic agents and postoperative complications. The study revealed that immunosuppressive or biologic therapies prior to surgery did not significantly influence the incidence of overall complications, intraabdominal sepsis, or anastomotic leakage. According to the multivariate analysis, blood transfusions, perforating disease, and previous resections were significant risk factors for overall complications, including intraabdominal sepsis and anastomotic leakage.
A meta‐analysis by Huang et al 74 that included six studies with a total of 2146 patients indicated that immunomodulation was not a risk factor for the complication of intraabdominal sepsis, with a pooled odds ratio (OR) of 1.07 (95% CI: 0.66–1.73). A similar result was obtained in another meta‐analysis. 75 Although no robust evidence is yet available, immunomodulation is likely safe to continue perioperatively in patients with CD. 5
5.2. Corticosteroids
Systemic corticosteroids (CSs) are recommended for the induction of clinical response and remission, but not maintenance, in patients with CD. 76 In a study pooling data from 71 controlled clinical trials, Stuck et al 77 suggested that the risk of infection was not increased in patients given a daily dose of less than 10 mg or a cumulative dose of less than 700 mg of prednisone. However, for a dosage of 10 mg daily, the overall rate of infection‐related complications was 12.7% in 2111 CS‐treated patients versus 8% in the 2087 controls (RR: 1.6; 95% CI: 1.3–1.9; P < 0.001).
The subgroup analysis of the meta‐analysis evaluated whether preoperative CS was a risk factor, 74 revealing that CS administration was associated with a high risk of intraabdominal sepsis complications (OR 1.99; 95% CI: 1.54–2.57). A similar meta‐analysis evaluated preoperative CS treatment and the risk of postoperative complications in patients with IBD undergoing abdominal surgery. 78 The results indicated that CS treatment was associated with all postoperative complications (OR 1.41, 95% CI: 1.07–1.87) and an increased risk of postoperative infection complications (OR 1.68, 95% CI: 1.24–2.28). The researchers further concluded that patients who received high doses of perioperative oral steroids (more than 40 mg) had a higher risk of overall complications (OR 2.04, 95% CI: 1.28–3.26).
The European Crohn's and Colitis Organization (ECCO) guidelines 2 stated that a prednisolone dosage of 20 mg daily or equivalent for more than 6 weeks is a risk factor for surgical complications. Therefore, patients must be weaned from CSs when possible. In patients whose high‐dose steroids cannot be tapered, a staged surgery with a temporary stoma may be considered. 4
5.3. Biologics
Biologic agents, such as anti‐TNF, VDZ, and UST, are effective medications for inducing remission in patients with moderate‐to‐severe CD who have not responded to conventional therapy. 76 However, a significant proportion of patients do not achieve mucosal healing and eventually require surgical intervention after step‐up therapy. 79 , 80 Moreover, surgical intervention is required for 50% of patients with CD within 10 years of diagnosis. 81 The following paragraph details preoperative biologic therapy and the risk of postoperative complications.
5.4. Anti‐TNF agents
The impact of preoperative medical therapy on postoperative surgical complications has been widely studied. Among these therapies, anti‐TNF drugs are the most studied biologics with respect to the perioperative management of IBD. Because of the limited heterogeneous data from small retrospective studies, the effects of anti‐TNF agents and the risk of perioperative infection in patients with CD remain controversial. No clear consensus has been met as to whether exposure to anti‐TNF therapy is associated with an increased risk of postoperative complications.
As reported in the Table 1, several meta‐analysis studies have addressed this topic. However, all were based on case–control or cohort studies. For overall complications, several studies 75 , 82 , 83 , 84 , 85 , 86 revealed no increase in risk, whereas others 87 , 88 , 89 , 90 , 91 concluded that anti‐TNF is associated with a mildly increased risk of overall postoperative complications in patients with CD. All meta‐analyses on patients with CD who received preoperative anti‐TNF but two 74 , 84 have reported an increased risk of infection or sepsis complications. 75 , 82 , 83 , 85 , 87 , 89 , 90 , 92
TABLE 1.
Meta‐analysis studies of postoperative outcomes in patients with CD treated with anti‐TNF agents
| Authors | Type of complication | No. studies included | Study population | Experiment | Anti‐TNF group complication rate (%) | Non‐anti‐TNF group complication rate (%) | OR (CI) |
|---|---|---|---|---|---|---|---|
| Kopylov et al 82 |
Overall Infectious Noninfectious |
6 6 4 |
1316 1159 834 |
Anti‐TNF‐α agents |
142/336 (42) 78/287 (27) 39/200 (20) |
284/980 (30) 165/872 (19) 60/634 (9) |
1.72 (0.93–3.19) 1.50 (1.08–2.08) 1.26 (0.65–2.42) |
| Billioud, et al 83 |
Overall Infectious |
6 7 |
1316 1699 |
Anti‐TNF‐α agents |
85/336 (25) 99/484 (21) |
196/980 (20) 169/1215 (14) |
1.31 (0.96–1.77) 1.45 (1.03–2.05) |
| Narula et al 87 |
Infectious Non‐infectious Total |
15 11 13 |
3244 2496 3840 |
Anti‐TNF‐α agents |
214/987 (22) 227/813 (28) 464/1059 (44) |
328/2257 (15) 316/1683 (9) 801/2781 (29) |
1.56 (1.09–2.24) 1.57 (1.14–2.17) 1.73 (1.23–2.43) |
| Rosenfeld et al 86 |
Major Minor Repeat operation |
6 3 3 |
1129 564 710 |
Infliximab |
99/257 (39) 25/148 (17) 18/173 (10) |
223/872 (26) 17/416 (4) 29/537 (5) |
1.59 (0.89–2.86) 1.80 (0.87–3.71) 1.33*0.55–3.30 |
| El‐Hussuna et al 88 | All anastomotic |
13 11 |
2046 2340 |
Anti‐TNF‐α agents |
238/419 (57) 45/593 (8) |
589/1627 (36) 143/1747 (8) |
1.25 (1.10–1.43) 0.91 (0.56–1.47) |
| Yang et al 89 |
Total Infectious |
13 10 |
2538 2116 |
Infliximab |
235/663 (35) 168/626 (27) |
479/1875 (26) 280/1490 (19) |
1.45 (1.04–2.02) 1.47 (1.08–1.99) |
| Ali et al 75 |
Total Infectious |
7 12 |
1454 3057 |
Anti‐TNF‐α agents |
235/431 (55) 152/823 (18) |
192/1023 (19) 317/2234 (14) |
1.16 (0.97–1.40) 1.29 (1.07–1.55) |
| Huang et al 74 | Septic | 6 | 1833 | Anti‐TNF‐α agents | Not reported | Not reported |
1.29 (0.79–2.11) |
| Waterland et al 92 |
Total infectious Abdominal sepsis |
8 9 |
1782 3988 |
Infliximab |
165/548 (30) 60/697 (9) |
252/1234 (20) 148/3291 (4) |
1.52 (1.14–2.03) 1.22 (0.87–1.72) |
| Lin et al 90 |
Total Infectious |
20 15 |
7159 7063 |
Anti‐TNF agents |
476/1673 (28) 272/1625 (17) |
1086/5486 (20) 461/5438 (8) |
1.53 (1.11–2.09) 2.09 (1.19–3.65) |
| Xu et al 84 |
Overall Infectious |
16 14 |
5498 5179 |
infliximab |
619/1309 (47) 301/1244 (24) |
1064/4189 (25) 485/3935 (12) |
1.17 (0.82–1.66) 1.23 (0.87–1.74) |
| Law et al 91 | Total | 27 | Not reported | Anti‐TNF Agents | Not reported | Not reported | 1.43 (1.09–1.87] |
| Hanzel et al 85 |
Total Infectious |
6 6 |
1224 1721 |
Anti‐TNF Agents |
179/447 (40) 112/694 (16) |
207/777 (27) 93/1027 (9) |
1.03 (0.71–1.51) 2.05 (1.40–3.01) |
In other studies, the critical risk factors for serious infections are high disease activity and ineffective disease control, CS treatment, and concomitant immunomodulation. In the REMIND study group, 93 a total of 209 patients with CD who underwent ileocecal resection were analyzed. CS treatment 4 weeks before surgery was significantly associated with an elevated postoperative complication rate (OR 2.69; 95% CI: 1.15–6.29; P = 0.022). Neither preoperative exposure to anti‐TNF agents (n = 93, 44%) nor trough serum anti‐TNF levels were significant risk factors for postoperative complications. Yamamoto et al 94 published a case–control study that revealed that malnutrition increases the risk of infection complications after surgery. The detrimental effects of malnutrition on postoperative infection may be enhanced in patients who have received biologic therapy preoperatively.
In 2018, the ECCO‐ESCP consensus on surgery for CD indicated that anti‐TNF therapy is associated with a high risk of postoperative sepsis complications after abdominal surgery for CD. The safest period for omission of anti‐TNF therapy is unknown. 5 In 2020, the ECCO revised this statement, concluding that the current evidence does not support such an association and that cessation of therapy is not mandatory. 4
5.5. VDZ
Vedolizumab, a biologic agent that selectively inhibits the migration of leukocytes into the intestinal tract, is an effective medical therapy for IBD. 95 In the clinical trial, 96 complications related to colectomy and bowel surgery and resection were infrequent, with minimal differences observed between VDZ and placebos. Furthermore, the frequency of postoperative complications in a postmarketing setting is low. 97
Lightner et al 98 performed a retrospective multicenter cohort study to compare preoperative VDZ to anti‐TNF therapy in relation to the incidence of postoperative complications. A total of 146 patients received VDZ, and 289 patients received anti‐TNF prior to abdominal surgery. In the multivariate analysis, exposure to VDZ was an independent significant predictor of postoperative surgical site infection (OR: 5.78, 95% CI: 2.99–11.76, P < 0.01). Another retrospective cohort study by Yamada et al 99 revealed that an age of over 65 years (OR 3.56, 95% CI: 1.30–9.76) and low albumin levels (OR 2.26, 95% CI: 1.28–4) were associated with an increased risk of 30‐day postoperative complications, whereas VDZ treatment was not (OR 0.56, 95% CI: 0.28–1.07, P = 0.08)
A meta‐analysis by Guo et al 100 indicated that, compared with a control group, the incidence of infection complications was reduced after preoperative treatment with VDZ (OR = 0.40, P = 0.04). However, VDZ increased the risk of ileus (OR = 2.43, P = 0.01), all surgical site infections (SSIs) (OR = 2.97, P < 0.001), readmission (OR = 2.74, P < 0.001), and return to the operating room (OR = 2.11, P = 0.04). However, two other meta‐analysis studies have reported no significant difference between VDZ treatment groups and control groups. 91 , 101 The aforementioned results are summarized in Table 2. In general, VDZ is safe in a surgical setting, although larger randomized studies with perioperative drug monitoring are necessary to draw a solid conclusion. 4
TABLE 2.
Meta‐analysis studies of postoperative outcomes in patients with CD treated with vedolizumab (VDZ)
| Authors | Type of complication | No. studies included | Study population | Control | Vedo group complication rate (%) | Control group complication rate (%) | OR (CI) |
|---|---|---|---|---|---|---|---|
| Guo et al 100 |
Any complication Infectious All SSI |
2 2 2 |
143 360 569 |
Non‐vedolizumab | Not reported | Not reported |
2.09 (0.36–12.02) 0.40 (0.14–0.94) 2.97 (1.75–5.02) |
| Guo et al 100 |
All SSI ileus |
2 3 |
343 343 |
Anti‐TNF‐α agents |
Not reported | Not reported |
3.69 (1.69–8.08) 2.46 (1.16–5.22) |
| Guo et al 100 |
All SSI Ileus |
2 2 |
366 366 |
Non‐biological agents | Not reported | Not reported |
2.47 (1.21–5.04) 2.40 (1.14–5.07) |
| Yung et al 101 |
All complication Infectious SSIs Major |
2 2 2 2 |
343 343 343 343 |
Anti‐TNF‐α agents |
40/140 (29) 33/140 (24) 27/140 (19) 13/140 (9) |
41/203 (20) 24/203 (12) 18/203 (9) 12/203 (6) |
1.45 (0.31–6.86) 1.00 (0.07–13.86) 1.16 (0.08–17.38) 1.16 (0.10–13.90) |
| Yung et al 101 |
All complications Infectious SSIs Major |
2 2 2 2 |
366 366 366 366 |
Non‐biological agents |
40/140 (29) 33/140 (24) 27/140 (19) 13/140 (9) |
55/226 (24) 30/226 (13) 25/226 (11) 19/226 (8) |
1.24 (0.21–7.52) 0.84 (0.04–15.88) 0.91 (0.07–11.58) 0.84 (0.18–3.91) |
| Law et al 91 | Infectious | 4 | Not reported | Not reported | Not reported | Not reported | 1.32 (0.51–3.42) |
5.6. UST
Ustekinumab, a monoclonal antibody against interleukin‐12/23 p40, was approved by the Food and Drug Administration (FDA) in September 2016. Thus, a relatively small number of patients have been exposed to UST compared with anti‐TNF therapy, which has been approved since 1998. 95
A multicenter cohort study of UST‐treated patients with CD who underwent abdominal surgery between 2009 and 2016 was performed. 102 Compared with anti‐TNF‐treated patients, no significant difference in postoperative wound infection or anastomotic leaking was observed. The study concluded that patients with CD treated with preoperative UST did not experience an increase in postoperative complications. A similar result was obtained in another retrospective study. 103 However, a retrospective study based on a single‐center series produced contradictory results. 104 Compared with 277 patients with CD who were not treated with biologic therapy in the 12 weeks prior to major abdominal surgery, the 57 patients with CD who received UST had a significantly higher risk of intraabdominal sepsis on multivariable logistic regression.
A systematic review and meta‐analysis by Garg et al 105 analyzed the risk of postoperative complications in patients with CD exposed to UST preoperatively. No difference in the rates of intraabdominal sepsis was noted between the UST and the anti‐TNF groups (7.2%, 95% CI: 3–16.4 vs 11.9%, 95% CI: 5.9–22.5; P = 0.4). A further analysis of three studies directly comparing UST and anti‐TNF treatment revealed that the OR of intraabdominal sepsis was 0.41 (95% CI: 0.12–1.23, P = 0.11; Table 3). The researchers concluded that the postoperative complication rate in patients with preoperative UST exposure may be similar to that for patients treated with anti‐TNF medication. However, studies with a more robust design and larger sample sizes are required to verify these results.
TABLE 3.
Meta‐analysis studies of postoperative outcomes in patients with CD treated with ustekinumab (UST)
| Authors | Type of complication | No. studies included | Study population | Control | UST group complication rate (%) | Control group complication rate (%) | OR (CI) |
|---|---|---|---|---|---|---|---|
| Garg et al 105 | Intra‐abdominal sepsis | 3 | 583 | Anti‐TNF agent | 4/102 | 47/481 | 0.41 (0.14–1.23) |
The evidence regarding immunomodulation and biologic therapy, such as anti‐TNF and anti‐integrin medications and anti‐interleukin‐12/23, remains weak. 91 An inherent indication bias in the studies revealed a relationship between biologics and postoperative complications. These postoperative complications may be related to the severity of the IBD that served as an indicator for biologic therapy rather than the biologic itself. 106 Thus, whether these medications affect postoperative infectious complications is uncertain, and no firm conclusions can be drawn regarding their safety in the perioperative period.
Each patient's individual case must be taken into consideration when decisions are made about preoperative IBD medications. Complications after surgery can usually be minimized with optimal preparation. CSs and, possibly, anti‐TNF agents may increase the risk of infection and septic shock. Therefore, a preoperative drug‐free interval, when feasible, could be implemented to reduce this risk.
6. ADVANCES IN OPERATIVE PROCEDURES
6.1. Anastomotic techniques
To reduce reoperation rates, various surgical techniques were analyzed. Radical resection of the mesentery can reduce surgical recurrence, as verified through a cohort study. 107 Another frequently discussed surgical technique is anastomosis. The safety and efficacy of types of anastomoses, such as hand‐sewn, stapled, end‐to‐end, end‐to‐side, or side‐to‐side anastomoses, were evaluated. However, researchers have failed to determine the optimal anastomotic method for recurrence prevention. 108 , 109 , 110
In 2003, Kono proposed a novel anastomotic technique, named Kono‐S anastomosis, 111 for reducing the recurrence of CD after surgery. The key steps are as follows: First, the bowels are transected using a linear staple cutter such that the mesentery is in the middle of the staple line at a 90° angle. Second, the staple lines are sutured together transversely to create a supporting column for the eventual dimension of the anastomosis. Then, 7‐cm long longitudinal enterotomies are created at the antimesenteric aspect, beginning 1 cm from the supporting column; the anastomoses of the bowels are then constructed transversely in a hand‐sewn fashion. 111 Several cohort studies and one randomized controlled trial have supported the use of this technique for reducing the postoperative recurrence rate. 112 , 113 , 114
6.2. Laparoscopic surgery in CD
Initially, laparoscopic surgery was not used for CD because of the intraoperative characteristics, such as extensive inflammation, enteric fistulae, thickened mesentery, and skipped lesions throughout the bowels. However, the use of laparoscopy in most gastrointestinal procedures has become standard and increasingly accepted for treating patients with CD. 115 , 116
For primary uncomplicated ileocolic resection, the benefits of laparoscopic surgery including a quicker return of bowel function, shorter length of hospital stay, fewer short‐term postoperative complications, lower incidence of incisional hernia and postoperative small bowel obstruction, and improved cosmesis have been well‐documented. 117 , 118 , 119 Even in recurrent complicated cases, several studies have reported that laparoscopic ileocolic resection can be performed in carefully selected patients and has comparable outcomes to primary laparoscopic resection. 120 , 121 , 122 For small bowel resection, a retrospective review revealed that laparoscopic surgery is associated with an equivalent or improved morbidity over open surgery in select patients with small bowel CD. 123
In summary, retrospective studies and randomized studies have indicated that laparoscopic approaches for patients with CD are both safe and feasible. The choice of laparoscopic or open approaches depends on patient factors, surgeon preference, and equipment availability.
6.3. Role of the mesentery
Studies of mesenteric anatomy have demonstrated that the mesentery is continuous. 124 Increasing evidence indicates that inflammation in mesenteric adipose tissue, adipocyte hyperplasia, and fibroblast differentiation collectively produces an “outside‐in” phenomenon that contributes to bowel inflammation and fibrosis. 125 Based on these related studies, mesenteric resection may also interrupt local recruitment of fibroblast precursors (i.e., fibrocytes 126 ), which can differentiate into either adipocytes or fibroblasts. 127
As mentioned, before surgery, assessing mesenteric and intestinal disease activity for CD through imaging studies is crucial. However, accurately identifying the edge of the lesion during surgery remains a challenge. Studies have reported that the severity of mesenteric inflammation is closely related to the subsequent recurrence probability and can be used as a predicator of disease prognosis. 128 , 129 , 130 , 131 The mesenteric thickness tightly and topographically correlates with the area of intestinal inflammation. 132 , 133 , 134 Advanced mesenteric diseases (i.e., fat wrapping) could be regarded as a basis for assessing the need to remove intestinal segments and fat wrapping greater than 50%, which are associated with increased surgical recurrence. 135
To determine whether the bowel segment has been affected by the disease, the “pinch test” (Figure 4) can be applied whereby two fingertips pinch both sides of the mesentery to detect potential mesenteric thickening. The microscopically positive proximal mucosal margins of postoperative specimens could therefore also be used as a reference. However, more research is required to verify the association between inflammation at the edges of the specimen and subsequent recurrence. 136 , 137 Therefore, further prospective randomized studies are necessary to clearly determine the role of resection margins in regards to disease recurrence in patients with CD following ileocecal resection.
FIGURE 4.
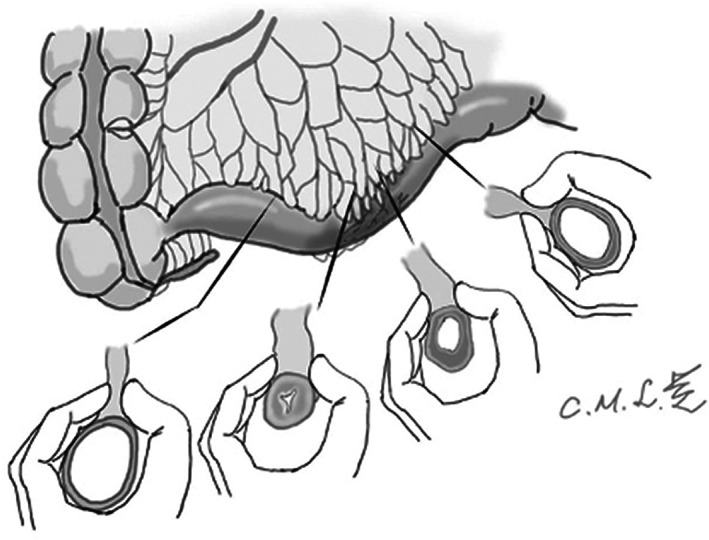
Mesenteric thickening can be detected using the “pinch test,” which can distinguish the contours of a diseased bowel from a healthy bowel. A healthy bowel has a soft, pliable mesentery, whereas a diseased bowel exhibits obvious fat wrapping and swelling, congestion, and a firm mesentery
All these findings support the mesentery's involvement in the pathogenesis of CD and offer a target for future management. 124 , 133 , 138 That is, mesentery‐based strategies could lead to more favorable outcomes after surgery for CD. However, inclusion of the mesentery during surgery may be associated with reduced surgical recurrence rates in CD, but extended resections are currently not recommended because of the heterogeneous evidence. To answer the question of whether mesocolic excision during primary ileocolonic resection reduces postoperative disease recurrence, an international multicenter randomized trial is currently in progress. 139
6.4. Short segment of ileocolonic CD
In one‐third of patients with CD, gross pathologic changes are limited to the terminal part of the ileum. 140 Approximately 40% of patients have ileocolitis, which is inflammation of the distal ileum and proximal colon. 141 An affected bowel of less than 30 cm in length can be defined as localized or a short segment of ileocolonic CD. 142
Early surgical intervention in localized CD has been recommended by the British National Institute for Health and Care Excellence, 143 German clinical practice guideline, 144 and updated ECCO guidelines, 4 with institutions recognizing its advantages in terms of reducing disease recurrence and reoperation rates. Significant improvement in quality of life after surgical resection in the treatment of localized diseases has also been noted in multiple trials. 145 , 146
Surgeons must consider postoperative recurrence prior to initiating surgery for CD. Many surgical methods, such as Kono‐S anastomosis or extensive resection of the mesentery, were discussed and regarded as effective in reducing the rate of recurrence. However, patients with a short segment of ileocolonic CD may have different considerations because of their limited disease entity.
In such situations, a stapled ileocolic end‐to‐side anastomosis is the preferred technique and has been used extensively at Cleveland Clinic in the United States. 147 This technique retains the original physiological angle of 90°, is easier to perform (Figure 5) than stapled side‐to‐side anastomosis, and facilitates endoscopic manipulation during postoperative follow‐up. In addition, more intestinal length may be retained, and the possibility of multiple firing with staple line crossings is reduced.
FIGURE 5.
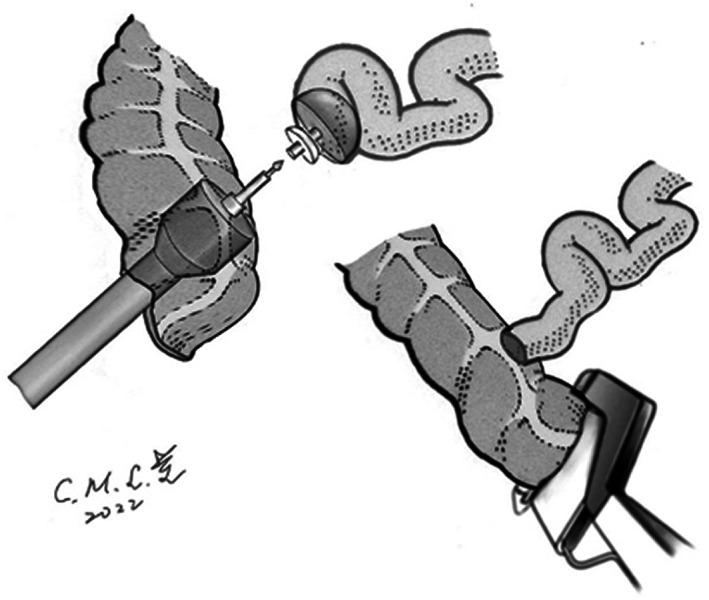
Stapled ileocolic end‐to‐side anastomosis with a circular stapler. The retained stump could be closed using a thoraco‐abdominal or gastrointestinal anastomosis linear stapler at approximately 5 cm distal to an ileocolic anastomosis
Although Kono‐S anastomosis and extended mesenteric excisions have produced some favorable results, 113 , 148 , 149 these surgical procedures are more technically demanding. Taking into account a surgeon's experience and the technical challenges associated with CD‐related complications, 150 for ileocolonic CD, performing high‐risk procedures may be unnecessary.
6.5. ERAS
Enhanced recovery after surgery is an integrated surgical patient care process that allows patients to be assessed in relation to various processes such as outpatient diagnosis, hospitalization waiting periods, preoperative preparation, surgery, postoperative recovery, and discharge tracking. The treatment methods validated through related evidence greatly improve the safety of the surgical anesthesia process and the quality of patients' postoperative recovery, reduce the occurrence of postoperative complications, and significantly enhance the quality of medical care before, during, and after surgery.
The greatest advantage of ERAS is that large investments in hardware are unnecessary; existing professional resources can be used effectively instead. ERAS can be implemented without affecting the operation of existing medical services. ERAS was first used to assist patients who had undergone colorectal cancer surgery. Evidence for its use following surgery for IBD is scarce, with the exception of ileocecal resection in patients with CD, which has been described in several studies. 151 , 152
In addition to the high prevalence of malnutrition, anemia, and sepsis, special consideration should be made for ERAS for patients with IBD, such as in the form of stoma team evaluation before and after surgery and before discharge and review of medications including CSs and biologics. 153
Tailored precision medicine or the establishment of a complete medical model with integrated application continues to be continually developed and refined with increasing evidence.
6.6. Venous thromboembolism prophylaxis
Inflammatory bowel disease is associated with an increased risk of venous thromboembolic events (VTEs), including deep vein thrombosis and pulmonary embolism, which may lead to significantly high risks of complications and mortality.
The incidence of VTEs in Western countries ranges from 0.73 to 1.82 per 1000 people. 154 Patients with IBD have a 1.5‐fold to 4‐fold higher risk of VTEs compared with the general population. The overall incidence of VTEs in patients with IBD was reported to be 2.4 to 2.6 cases per 1000 patients per year. 155 The overall incidence of VTEs in Asian populations is lower, ranging from 0.21 to 0.57 per 1000 people. 156 Regarding East Asian patients with IBD, a multinational collaborative study of 2562 hospitalized patients with IBD from South Korea, Japan, and Taiwan indicated that the average incidence of VTEs was 0.72 to 1.38 per 1000 people per year. 157 Moderate‐to‐severe colitis, IBD flare‐ups requiring hospitalization, CS treatment, previous history or family history of VTEs, and previous major abdominal or pelvic surgery are known risk factors for VTEs in patients with IBD. 158
Current Western guidelines for VTE prophylaxis recommend optimization for all patients with IBD requiring abdominal surgery unless contraindicated. A combination of mechanical and pharmacological prophylaxis should also be considered. 5 The cumulative incidence of VTEs increased from 1.3% at 7 days to 4.3% at 90 days after surgery in patients with IBD. Therefore, extended VTE prophylaxis with 28 days of low molecular weight heparin treatment has been adopted. 159
Routine thromboprophylaxis before the surgery is infrequently used for Asian patients with IBD because of the relatively low incidence of VTEs; however, no consensus has been reached in this regard. However, a risk‐adapted, individualized strategy of VTE prevention is crucial. In patients aged less than 60 years and without other risk factors for VTE, the benefits of routine prophylaxis may not outweigh the risks. 160 VTE prophylaxis is recommended for older patients (aged >60 years) or patients with other associated risk factors. Furthermore, to reduce the risk of VTEs, ambulation should be maintained before and as early as possible after operation, and inflammation must be controlled.
7. POSTOPERATIVE COMPLICATIONS IN PATIENTS WITH CD
The mortality rate of CD‐related surgery is generally low (<1%). 93 The complication rate is approximately 20%, with many complications occurring in the early postoperative period and of a severe nature (Clavien–Dindo classification of >III). The incidence of intraabdominal sepsis complications, including anastomotic leakage and abdominal abscesses, ranges from 9% to 13%. 63 , 161 Extra‐abdominal infection includes pneumonia, bacteremia, urinary infection, and wound infection. Other nonsepsis complications include hemorrhage and VTEs. Patients with colonic disease are more likely to develop postoperative complications than patients with ileal or ileocolonic disease. To improve postoperative outcomes and reduce postoperative complications, determining a patient's individual risk prior to surgery is essential. 162 , 163 Limiting steroid dosage and duration, adjusting biologic administration, and optimizing preoperative nutrition optimization are also crucial. Urgent surgeries must be avoided when possible, because patients with CD have a higher risk of overall postoperative complications and intraabdominal sepsis following urgent surgeries than following elective surgeries. 164
8. POSTOPERATIVE RECURRENCE IN PATIENTS WITH CD
Postoperative recurrences are not uncommon in patients with CD. Rutgeerts et al 165 reported that after 1 year, 73% of patients exhibited recurrence in the neoterminal ileum endoscopically, although only 20% were symptomatic. After 3 years, the endoscopic detection rate had increased to 85%, and the symptomatic rate had increased to 34%. 165 The overall rate of secondary surgery was 28.7%. 166
The strongest predictor of postoperative recurrence is smoking, with smokers having a 2.5‐fold increased risk of surgical recurrence and a 2‐fold increased risk of clinical recurrence compared with nonsmokers. 167 Other risk factors related to a higher rate of postoperative recurrence include prior surgical resection, penetrating or perforating disorders, a young age, colonic lesions, and the presence of perianal disease at surgery. 168
Steroids and probiotics do not assist in the prevention of postoperative recurrence, 169 but azathioprine can delay endoscopic postoperative recurrence. 169 , 170 Biologics presented the most promising data in terms of reducing postoperative recurrence, but this potential must be verified through large randomized control trials. 171 , 172 , 173 , 174 , 175
9. CONCLUSION
Patients with CD often undergo surgery as part of their treatment, especially those who experience complications. Nutritional optimization and ERAS implementation are crucial for patients with CD who require surgical intervention to reduce postoperative complications. No solid evidence has indicated that perioperative medications have an effect on postoperative complications. Decisions about preoperative medication must be made on an individual case‐dependent basis. Preoperative drug‐free intervals may reduce the risk of infection, and preoperative imaging studies can assist in the planning of appropriate surgical strategies and approaches. However, patients must be informed of any alterations to their treatment. In sum, the management of perioperative medications and surgery‐related decision‐making should be individualized and patient‐centered.
DISCLOSURE
Funding: This work was supported by National Taiwan University Hospital (NTUH‐MS 507 to SC Wei).
Conflict of Interest: SC Wei has received consultancy fees from AbbVie, Celltrion, Ferring Pharmaceuticals Inc., Janssen, Pfizer Inc, Takeda, and Tanabe, and speaker fees from AbbVie, Bristol Myers Squibb, Celltrion, Ferring Pharmaceuticals Inc., Pfizer Inc, Janssen, Takeda and Tanabe. CC Lin has received consultant/speaker fees from AbbVie and advisory board member from Janssen.
Author Contribution: All authors have made substantial contributions to the drafting or revising of the intellectual content of the article and have approved the final version for submission.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Mao‐Liang Chiang for providing the hand‐drawn illustrations for Figures 4 and 5.
Lin C‐C, Lin H‐H, Chen H‐C, Chen N‐C, Shih I‐L, Hung J‐S, et al. Perioperative optimization of Crohn's disease. Ann Gastroenterol Surg. 2023;7:10–26. 10.1002/ags3.12621
REFERENCES
- 1. Baumgart DC, Sandborn WJ. Crohn's disease. Lancet. 2012;380(9853):1590–605. 10.1016/s0140-6736(12)60026-9 [DOI] [PubMed] [Google Scholar]
- 2. Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, et al. 3rd European evidence‐based consensus on the diagnosis and Management of Crohn's disease 2016: part 2: surgical management and special situations. J Crohns Colitis. 2017;11(2):135–49. 10.1093/ecco-jcc/jjw169 [DOI] [PubMed] [Google Scholar]
- 3. Kotze PG. The essential role of a multidisciplinary approach in inflammatory bowel diseases. Clin Colon Rectal Surg. 2022;35(1):3–4. 10.1055/s-0041-1740034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Adamina M, Bonovas S, Raine T, Spinelli A, Warusavitarne J, Armuzzi A, et al. ECCO guidelines on therapeutics in Crohn's disease: surgical treatment. J Crohns Colitis. 2020;14(2):155–68. 10.1093/ecco-jcc/jjz187 [DOI] [PubMed] [Google Scholar]
- 5. Bemelman WA, Warusavitarne J, Sampietro GM, Serclova Z, Zmora O, Luglio G, et al. ECCO‐ESCP consensus on surgery for Crohn's disease. J Crohns Colitis. 2018;12(1):1–16. 10.1093/ecco-jcc/jjx061 [DOI] [PubMed] [Google Scholar]
- 6. Shah SC, Itzkowitz SH. Colorectal cancer in inflammatory bowel disease: mechanisms and management. Gastroenterology. 2022;162(3):715–730.e3. 10.1053/j.gastro.2021.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baek S‐J, Lee KY, Song KH, Yu CS. Current status and trends in inflammatory bowel disease surgery in Korea: analysis of data in a Nationwide registry. Ann Coloproctol. 2018;34(6):299–305. 10.3393/ac.July [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wong DJ, Roth EM, Feuerstein JD, Poylin VY. Surgery in the age of biologics. Gastroenterol Rep. 2019;7(2):77–90. 10.1093/gastro/goz004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Slattery E, Keegan D, Hyland J, O'Donoghue D, Mulcahy HE. Surgery, Crohn's disease, and the biological era: has there been an impact? J Clin Gastroenterol. 2011;45(8):691–3. 10.1097/MCG.0b013e318201ff96 [DOI] [PubMed] [Google Scholar]
- 10. Munkholm P, Langholz E, Davidsen M, Binder V. Intestinal cancer risk and mortality in patients with Crohn's disease. Gastroenterology. 1993;105(6):1716–23. 10.1016/0016-5085(93)91068-s [DOI] [PubMed] [Google Scholar]
- 11. Frolkis AD, Dykeman J, Negron ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta‐analysis of population‐based studies. Gastroenterology. 2013;145(5):996–1006. 10.1053/j.gastro.2013.07.041 [DOI] [PubMed] [Google Scholar]
- 12. Annese V, Duricova D, Gower‐Rousseau C, Jess T, Langholz E. Impact of new treatments on hospitalisation, surgery, infection, and mortality in IBD: a focus paper by the epidemiology committee of ECCO. J Crohns Colitis. 2016;10(2):216–25. 10.1093/ecco-jcc/jjv190 [DOI] [PubMed] [Google Scholar]
- 13. Mak WY, Zhao M, Ng SC, Burisch J. The epidemiology of inflammatory bowel disease: east meets west. J Gastroenterol Hepatol. 2020;35(3):380–9. 10.1111/jgh.14872 [DOI] [PubMed] [Google Scholar]
- 14. Sato Y, Matsui T, Yano Y, Tsurumi K, Okado Y, Matsushima Y, et al. Long‐term course of Crohn's disease in Japan: incidence of complications, cumulative rate of initial surgery, and risk factors at diagnosis for initial surgery. J Gastroenterol Hepatol. 2015;30(12):1713–9. 10.1111/jgh.13013 [DOI] [PubMed] [Google Scholar]
- 15. Ye BD, Yang S‐K, Cho YK, et al. Clinical features and long‐term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010;45(10):1178–85. 10.3109/00365521.2010.497936 [DOI] [PubMed] [Google Scholar]
- 16. Riansuwan W, Limsrivilai J. Current status of IBD and surgery of Crohn's disease in Thailand. Ann Gastroenterol Surg. 2021;5(5):597–603. 10.1002/ags3.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rungoe C, Langholz E, Andersson M, Basit S, Nielsen NM, Wohlfahrt J, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979‐2011. Gut. 2014;63(10):1607–16. 10.1136/gutjnl-2013-305607 [DOI] [PubMed] [Google Scholar]
- 18. Kalman TD, Everhov AH, Nordenvall C, Sachs MC, Halfvarson J, Ekbom A, et al. Decrease in primary but not in secondary abdominal surgery for Crohn's disease: nationwide cohort study, 1990‐2014. Br J Surg. 2020;107(11):1529–38. 10.1002/bjs.11659 [DOI] [PubMed] [Google Scholar]
- 19. Dittrich AE, Sutton RT, Haynes K, Wang H, Fedorak RN, Kroeker KI. Incidence rates for surgery in Crohn's disease have decreased: a population‐based time‐trend analysis. Inflamm Bowel Dis. 2020;26(12):1909–16. 10.1093/ibd/izz315 [DOI] [PubMed] [Google Scholar]
- 20. Ma C, Moran GW, Benchimol EI, Targownik LE, Heitman SJ, Hubbard JN, et al. Surgical rates for Crohn's disease are decreasing: a population‐based time trend analysis and validation study. Am J Gastroenterol. 2017;112(12):1840–8. 10.1038/ajg.2017.394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bemelman WA, collaborators SE . Evolving role of IBD surgery. J Crohns Colitis. 2018;12(8):1005–7. 10.1093/ecco-jcc/jjy056 [DOI] [PubMed] [Google Scholar]
- 22. Mege D, Garrett K, Milsom J, Sonoda T, Michelassi F. Changing trends in surgery for abdominal Crohn's disease. Colorectal Dis. 2019;21(2):200–7. 10.1111/codi.14450 [DOI] [PubMed] [Google Scholar]
- 23. Chang CW, Wong JM, Tung CC, Shih IL, Wang HY, Wei SC. Intestinal stricture in Crohn's disease. Intest Res. 2015;13(1):19–26. 10.5217/ir.2015.13.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chang CW, Tu CH, Chou JW, Huang TY, Hsu WH, Wang YP, et al. Endoscopic management of strictures in patients with Crohn's disease ‐ a multi‐center experience in Taiwan. J Formos Med Assoc. 2020;119(10):1500–5. 10.1016/j.jfma.2019.12.005 [DOI] [PubMed] [Google Scholar]
- 25. Lazarev M, Ullman T, Schraut WH, Kip KE, Saul M, Regueiro M. Small bowel resection rates in Crohn's disease and the indication for surgery over time: experience from a large tertiary care center. Inflamm Bowel Dis. 2010;16(5):830–5. 10.1002/ibd.21118 [DOI] [PubMed] [Google Scholar]
- 26. Jobanputra S, Weiss EG. Strictureplasty. Clin Colon Rectal Surg. 2007;20(4):294–302. 10.1055/s-2007-991028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Neri B, Scribano ML, Armuzzi A, et al. Incident colorectal cancer in inflammatory bowel disease. Cancer. 2022;14(3):721. 10.3390/cancers14030721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jess T, Gamborg M, Matzen P, Munkholm P, Sørensen TI. Increased risk of intestinal cancer in Crohn's disease: a meta‐analysis of population‐based cohort studies. Am J Gastroenterol. 2005;100(12):2724–9. 10.1111/j.1572-0241.2005.00287.x [DOI] [PubMed] [Google Scholar]
- 29. Wang LH, Yang YJ, Cheng WC, Wang WM, Lin SH, Shieh CC. Higher risk for hematological malignancies in inflammatory bowel disease: a Nationwide population‐based study in Taiwan. Am J Gastroenterol. 2016;111(9):1313–9. 10.1038/ajg.2016.239 [DOI] [PubMed] [Google Scholar]
- 30. Jung YS, Han M, Park S, Kim WH, Cheon JH. Cancer risk in the early stages of inflammatory bowel disease in Korean patients: a Nationwide population‐based study. J Crohns Colitis. 2017;11(8):954–62. 10.1093/ecco-jcc/jjx040 [DOI] [PubMed] [Google Scholar]
- 31. Sjödahl RI, Myrelid P, Söderholm JD. Anal and rectal cancer in Crohn's disease. Colorectal Dis. 2003;5(5):490–5. 10.1046/j.1463-1318.2003.00510.x [DOI] [PubMed] [Google Scholar]
- 32. Beaugerie L, Carrat F, Nahon S, Zeitoun JD, Sabaté JM, Peyrin‐Biroulet L, et al. High risk of anal and rectal cancer in patients with anal and/or perianal Crohn's disease. Clin Gastroenterol Hepatol. 2018;16(6):892–899.e2. 10.1016/j.cgh.2017.11.041 [DOI] [PubMed] [Google Scholar]
- 33. Ueda T, Inoue T, Nakamoto T, Nishigori N, Kuge H, Sasaki Y, et al. Anorectal cancer in Crohn's disease has a poor prognosis due to its advanced stage and aggressive histological features: a systematic literature review of Japanese patients. J Gastrointest Cancer. 2020;51(1):1–9. 10.1007/s12029-018-0180-6 [DOI] [PubMed] [Google Scholar]
- 34. Kotsafti A, Scarpa M, Angriman I, Castagliuolo I, Caruso A. Fistula‐related cancer in Crohn's disease: a systematic review. Cancer. 2021;13(6):1445. 10.3390/cancers13061445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Uchino M, Ikeuchi H, Hata K, Minagawa T, Horio Y, Kuwahara R, et al. Intestinal cancer in patients with Crohn's disease: a systematic review and meta‐analysis. J Gastroenterol Hepatol. 2021;36(2):329–36. 10.1111/jgh.15229 [DOI] [PubMed] [Google Scholar]
- 36. Wiseman J, Chawla T, Morin F, de Buck van Overstraeten A, Weizman AV. A multi‐disciplinary approach to perianal fistulizing Crohn's disease. Clin Colon Rectal Surg. 2022;35(1):51–7. 10.1055/s-0041-1740038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patel KV, Darakhshan AA, Griffin N, Williams AB, Sanderson JD, Irving PM. Patient optimization for surgery relating to Crohn's disease. Nat Rev Gastroenterol Hepatol. 2016;13(12):707–19. 10.1038/nrgastro.2016.158 [DOI] [PubMed] [Google Scholar]
- 38. Panes J, Bouzas R, Chaparro M, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn's disease. Aliment Pharmacol Ther. 2011;34(2):125–45. 10.1111/j.1365-2036.2011.04710.x [DOI] [PubMed] [Google Scholar]
- 39. Qiu Y, Mao R, Chen BL, Li XH, He Y, Zeng ZR, et al. Systematic review with meta‐analysis: magnetic resonance enterography vs. computed tomography enterography for evaluating disease activity in small bowel Crohn's disease. Aliment Pharmacol Ther. 2014;40(2):134–46. 10.1111/apt.12815 [DOI] [PubMed] [Google Scholar]
- 40. Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, et al. ECCO‐ESGAR guideline for diagnostic assessment in IBD part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13(2):144–64. 10.1093/ecco-jcc/jjy113 [DOI] [PubMed] [Google Scholar]
- 41. Gecse KB, Bemelman W, Kamm MA, Stoker J, Khanna R, Ng SC, et al. A global consensus on the classification, diagnosis and multidisciplinary treatment of perianal fistulising Crohn's disease. Gut. 2014;63(9):1381–92. 10.1136/gutjnl-2013-306709 [DOI] [PubMed] [Google Scholar]
- 42. Adegbola SO, Sahnan K, Twum‐Barima C, Iqbal N, Reza L, Lung P, et al. Current review of the management of fistulising perianal Crohn's disease. Frontline Gastroenterol. 2021;12(6):515–23. 10.1136/flgastro-2020-101489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Parks AG, Gordon PH, Hardcastle JD. A classification of fistula‐in‐ano. Br J Surg. 1976;63(1):1–12. 10.1002/bjs.1800630102 [DOI] [PubMed] [Google Scholar]
- 44. Schwartz DA, Wiersema MJ, Dudiak KM, Fletcher JG, Clain JE, Tremaine WJ, et al. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn's perianal fistulas. Gastroenterology. 2001;121(5):1064–72. 10.1053/gast.2001.28676 [DOI] [PubMed] [Google Scholar]
- 45. Lewis RT, Bleier JI. Surgical treatment of anorectal crohn disease. Clin Colon Rectal Surg. 2013;26(2):90–9. 10.1055/s-0033-1348047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tozer PJ, Lung P, Lobo AJ, Sebastian S, Brown SR, Hart AL, et al. Review article: pathogenesis of Crohn's perianal fistula‐understanding factors impacting on success and failure of treatment strategies. Aliment Pharmacol Ther. 2018;48(3):260–9. 10.1111/apt.14814 [DOI] [PubMed] [Google Scholar]
- 47. Wasmann KA, de Groof EJ, Stellingwerf ME, D'Haens GR, Ponsioen CY, Gecse KB, et al. Treatment of perianal fistulas in Crohn's disease, seton versus anti‐TNF versus surgical closure following anti‐TNF [PISA]: a randomised controlled trial. J Crohns Colitis. 2020;14(8):1049–56. 10.1093/ecco-jcc/jjaa004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rozalén V, Parés D, Sanchez E, Troya J, Vela S, Pacha MÁ, et al. Advancement flap technique for anal fistula in patients with Crohn's disease: a systematic review of the literature. Cir Esp. 2017;95:558–65. 10.1016/j.ciresp.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 49. Kamiński JP, Zaghiyan K, Fleshner P. Increasing experience of ligation of the intersphincteric fistula tract for patients with Crohn's disease: what have we learned? Colorectal Dis. 2017;19(8):750–5. 10.1111/codi.13668 [DOI] [PubMed] [Google Scholar]
- 50. Vidon M, Munoz‐Bongrand N, Lambert J, Maggiori L, Zeitoun JD, Corte H, et al. Long‐term efficacy of fibrin glue injection for perianal fistulas in patients with Crohn's disease. Colorectal Dis. 2021;23(4):894–900. 10.1111/codi.15477 [DOI] [PubMed] [Google Scholar]
- 51. Grimaud JC, Munoz‐Bongrand N, Siproudhis L, et al. Fibrin glue is effective healing perianal fistulas in patients with Crohn's disease. Gastroenterology. 2010;138(7):2275–2281.e1. 10.1053/j.gastro.2010.02.013 [DOI] [PubMed] [Google Scholar]
- 52. Nasseri Y, Cassella L, Berns M, Zaghiyan K, Cohen J. The anal fistula plug in Crohn's disease patients with fistula‐in‐ano: a systematic review. Colorectal Dis. 2016;18(4):351–6. 10.1111/codi.13268 [DOI] [PubMed] [Google Scholar]
- 53. Adegbola SO, Sahnan K, Tozer PJ, Strouhal R, Hart AL, Lung PFC, et al. Symptom amelioration in Crohn's perianal fistulas using video‐assisted anal fistula treatment (VAAFT). J Crohns Colitis. 2018;12(9):1067–72. 10.1093/ecco-jcc/jjy071 [DOI] [PubMed] [Google Scholar]
- 54. Cao D, Li W, Ji Y, Wang X, Cui Z. Efficacy and safety of FiLaC™ for perianal fistulizing Crohn's disease: a systematic review and meta‐analysis. Tech Coloproctol. 2022;26:775–81. 10.1007/s10151-022-02682-1 [DOI] [PubMed] [Google Scholar]
- 55. Carvello M, Lightner A, Yamamoto T, Kotze PG, Spinelli A. Mesenchymal stem cells for perianal Crohn's disease. Cell. 2019;8(7):764. 10.3390/cells8070764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. de Groof EJ, Carbonnel F, Buskens CJ, Bemelman WA. Abdominal abscess in Crohn's disease: multidisciplinary management. Dig Dis. 2014;32(Suppl 1):103–9. 10.1159/000367859 [DOI] [PubMed] [Google Scholar]
- 57. Clancy C, Boland T, Deasy J, McNamara D, Burke JP. A meta‐analysis of percutaneous drainage versus surgery as the initial treatment of Crohn's disease‐related intra‐abdominal abscess. J Crohns Colitis. 2016;10(2):202–8. 10.1093/ecco-jcc/jjv198 [DOI] [PubMed] [Google Scholar]
- 58. Hristova L, Soyer P, Hoeffel C, Marteau P, Oussalah A, Lavergne‐Slove A, et al. Colorectal cancer in inflammatory bowel diseases: CT features with pathological correlation. Abdom Imaging. 2013;38(3):421–35. 10.1007/s00261-012-9947-6 [DOI] [PubMed] [Google Scholar]
- 59. Barral M, Dohan A, Allez M, Boudiaf M, Camus M, Laurent V, et al. Gastrointestinal cancers in inflammatory bowel disease: An update with emphasis on imaging findings. Crit Rev Oncol Hematol. 2016;97:30–46. 10.1016/j.critrevonc.2015.08.005 [DOI] [PubMed] [Google Scholar]
- 60. Annese V, Beaugerie L, Egan L, Biancone L, Bolling C, Brandts C, et al. European evidence‐based consensus: inflammatory bowel disease and malignancies. J Crohns Colitis. 2015;9(11):945–65. 10.1093/ecco-jcc/jjv141 [DOI] [PubMed] [Google Scholar]
- 61. Spinelli A, Fiorino G, Bazzi P, Sacchi M, Bonifacio C, de Bastiani S, et al. Preoperative magnetic resonance enterography in predicting findings and optimizing surgical approach in Crohn's disease. J Gastrointest Surg. 2014;18(1):83–90. 10.1007/s11605-013-2404-1 [DOI] [PubMed] [Google Scholar]
- 62. Seastedt KP, Trencheva K, Michelassi F, Alsaleh D, Milsom JW, Sonoda T, et al. Accuracy of CT enterography and magnetic resonance enterography imaging to detect lesions preoperatively in patients undergoing surgery for Crohn's disease. Dis Colon Rectum. 2014;57(12):1364–70. 10.1097/DCR.0000000000000244 [DOI] [PubMed] [Google Scholar]
- 63. Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P. Risk factors for intra‐abdominal septic complications after a first ileocecal resection for Crohn's disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum. 2007;50(3):331–6. 10.1007/s10350-006-0782-0 [DOI] [PubMed] [Google Scholar]
- 64. Grass F, Pache B, Martin D, Hahnloser D, Demartines N, Hübner M. Preoperative nutritional conditioning of Crohn's patients‐systematic review of current evidence and practice. Nutrients. 2017;9(6):562. 10.3390/nu9060562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017;36(3):623–50. 10.1016/j.clnu.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 66. Makhdoom ZA, Komar MJ, Still CD. Nutrition and enterocutaneous fistulas. J Clin Gastroenterol. 2000;31(3):195–204. 10.1097/00004836-200010000-00003 [DOI] [PubMed] [Google Scholar]
- 67. Papa A, Lopetuso LR, Minordi LM, di Veronica A, Neri M, Rapaccini G, et al. A modern multidisciplinary approach to the treatment of enterocutaneous fistulas in Crohn's disease patients. Expert Rev Gastroenterol Hepatol. 2020;14(9):857–65. 10.1080/17474124.2020.1797484 [DOI] [PubMed] [Google Scholar]
- 68. Bischoff SC, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, et al. ESPEN practical guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2020;39(3):632–53. 10.1016/j.clnu.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 69. Adamina M, Gerasimidis K, Sigall‐Boneh R, Zmora O, de Buck van Overstraeten A, Campmans‐Kuijpers M, et al. Perioperative dietary therapy in inflammatory bowel disease. J Crohns Colitis. 2020;14(4):431–44. 10.1093/ecco-jcc/jjz160 [DOI] [PubMed] [Google Scholar]
- 70. Nickerson TP, Merchea A. Perioperative considerations in Crohn disease and ulcerative colitis. Clin Colon Rectal Surg. 2016;29(2):80–4. 10.1055/s-0036-1580633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Fiorindi C, Cuffaro F, Piemonte G, Cricchio M, Addasi R, Dragoni G, et al. Effect of long‐lasting nutritional prehabilitation on postoperative outcome in elective surgery for IBD. Clin Nutr. 2021;40(3):928–35. 10.1016/j.clnu.2020.06.020 [DOI] [PubMed] [Google Scholar]
- 72. Schroll S, Sarlette A, Ahrens K, Manns MP, Göke M. Effects of azathioprine and its metabolites on repair mechanisms of the intestinal epithelium in vitro. Regul Pept. 2005;131(1–3):1–11. 10.1016/j.regpep.2005.03.001 [DOI] [PubMed] [Google Scholar]
- 73. Yamamoto T, Spinelli A, Suzuki Y, Saad‐Hossne R, Teixeira FV, Albuquerque IC, et al. Risk factors for complications after ileocolonic resection for Crohn's disease with a major focus on the impact of preoperative immunosuppressive and biologic therapy: a retrospective international multicentre study. United European Gastroenterol J. 2016;4(6):784–93. 10.1177/2050640615600116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Huang W, Tang Y, Nong L, Sun Y. Risk factors for postoperative intra‐abdominal septic complications after surgery in Crohn's disease: a meta‐analysis of observational studies. J Crohns Colitis. 2015;9(3):293–301. 10.1093/ecco-jcc/jju028 [DOI] [PubMed] [Google Scholar]
- 75. Ahmed Ali U, Martin ST, Rao AD, Kiran RP. Impact of preoperative immunosuppressive agents on postoperative outcomes in Crohn's disease. Dis Colon Rectum. 2014;57(5):663–74. 10.1097/dcr.0000000000000099 [DOI] [PubMed] [Google Scholar]
- 76. Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, et al. ECCO guidelines on therapeutics in Crohn's disease: medical treatment. J Crohns Colitis. 2019;14(1):4–22. 10.1093/ecco-jcc/jjz180 [DOI] [PubMed] [Google Scholar]
- 77. Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis. 1989;11(6):954–63. 10.1093/clinids/11.6.954 [DOI] [PubMed] [Google Scholar]
- 78. Subramanian V, Saxena S, Kang JY, Pollok RC. Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am J Gastroenterol. 2008;103(9):2373–81. 10.1111/j.1572-0241.2008.01942.x [DOI] [PubMed] [Google Scholar]
- 79. Billioud V, Sandborn WJ, Peyrin‐Biroulet L. Loss of response and need for adalimumab dose intensification in Crohn's disease: a systematic review. Am J Gastroenterol. 2011;106(4):674–84. 10.1038/ajg.2011.60 [DOI] [PubMed] [Google Scholar]
- 80. Peyrin‐Biroulet L, Desreumaux P, Sandborn WJ, Colombel JF. Crohn's disease: beyond antagonists of tumour necrosis factor. Lancet. 2008;372(9632):67–81. 10.1016/s0140-6736(08)60995-2 [DOI] [PubMed] [Google Scholar]
- 81. de Buck van Overstraeten A, Wolthuis A, D'Hoore A. Surgery for Crohn's disease in the era of biologicals: a reduced need or delayed verdict? World J Gastroenterol. 2012;18(29):3828–32. 10.3748/wjg.v18.i29.3828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kopylov U, Ben‐Horin S, Zmora O, Eliakim R, Katz LH. Anti‐tumor necrosis factor and postoperative complications in Crohn's disease: systematic review and meta‐analysis. Inflamm Bowel Dis. 2012;18(12):2404–13. 10.1002/ibd.22954 [DOI] [PubMed] [Google Scholar]
- 83. Billioud V, Ford AC, Tedesco ED, Colombel JF, Roblin X, Peyrin‐Biroulet L. Preoperative use of anti‐TNF therapy and postoperative complications in inflammatory bowel diseases: a meta‐analysis. J Crohns Colitis. 2013;7(11):853–67. 10.1016/j.crohns.2013.01.014 [DOI] [PubMed] [Google Scholar]
- 84. Xu Y, Yang L, An P, Zhou B, Liu G. Meta‐analysis: the influence of preoperative infliximab use on postoperative complications of Crohn's disease. Inflamm Bowel Dis. 2019;25(2):261–9. 10.1093/ibd/izy246 [DOI] [PubMed] [Google Scholar]
- 85. Hanzel J, Almradi A, Istl AC, Yang ML, Fleshner KA, Parker CE, et al. Increased risk of infections with anti‐TNF agents in patients with Crohn's disease after elective surgery: meta‐analysis. Dig Dis Sci. 2022;67(2):646–60. 10.1007/s10620-021-06895-6 [DOI] [PubMed] [Google Scholar]
- 86. Rosenfeld G, Qian H, Bressler B. The risks of post‐operative complications following pre‐operative infliximab therapy for Crohn's disease in patients undergoing abdominal surgery: a systematic review and meta‐analysis. J Crohns Colitis. 2013;7(11):868–77. 10.1016/j.crohns.2013.01.019 [DOI] [PubMed] [Google Scholar]
- 87. Narula N, Charleton D, Marshall JK. Meta‐analysis: peri‐operative anti‐TNFα treatment and post‐operative complications in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37(11):1057–64. 10.1111/apt.12313 [DOI] [PubMed] [Google Scholar]
- 88. El‐Hussuna A, Krag A, Olaison G, Bendtsen F, Gluud LL. The effect of anti‐tumor necrosis factor alpha agents on postoperative anastomotic complications in Crohn's disease: a systematic review. Dis Colon Rectum. 2013;56(12):1423–33. 10.1097/DCR.0b013e3182a48505 [DOI] [PubMed] [Google Scholar]
- 89. Yang ZP, Hong L, Wu Q, Wu KC, Fan DM. Preoperative infliximab use and postoperative complications in Crohn's disease: a systematic review and meta‐analysis. Int J Surg. 2014;12(3):224–30. 10.1016/j.ijsu.2013.12.015 [DOI] [PubMed] [Google Scholar]
- 90. Lin YS, Cheng SW, Wang YH, Chen KH, Fang CJ, Chen C. Systematic review with meta‐analysis: risk of post‐operative complications associated with pre‐operative exposure to anti‐tumour necrosis factor agents for Crohn's disease. Aliment Pharmacol Ther. 2019;49(8):966–77. 10.1111/apt.15184 [DOI] [PubMed] [Google Scholar]
- 91. Law CC, Bell C, Koh D, Bao Y, Jairath V, Narula N. Risk of postoperative infectious complications from medical therapies in inflammatory bowel disease. Cochrane Database Syst Rev. 2020;10(10):CD013256. 10.1002/14651858.CD013256.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Waterland P, Athanasiou T, Patel H. Post‐operative abdominal complications in Crohn's disease in the biological era: systematic review and meta‐analysis. World J Gastrointest Surg. 2016;8(3):274–83. 10.4240/wjgs.v8.i3.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fumery M, Seksik P, Auzolle C, Munoz‐Bongrand N, Gornet JM, Boschetti G, et al. Postoperative complications after ileocecal resection in Crohn's disease: a prospective study from the REMIND group. Am J Gastroenterol. 2017;112(2):337–45. 10.1038/ajg.2016.541 [DOI] [PubMed] [Google Scholar]
- 94. Yamamoto T, Shimoyama T, Umegae S, Kotze PG. Impact of preoperative nutritional status on the incidence rate of surgical complications in patients with inflammatory bowel disease with vs without preoperative biologic therapy: a case‐control study. Clin Transl Gastroenterol. 2019;10(6):e00050. 10.14309/ctg.0000000000000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Baumgart DC, Le Berre C. Newer biologic and small‐molecule therapies for inflammatory bowel disease. N Engl J Med. 2021;385(14):1302–15. 10.1056/NEJMra1907607 [DOI] [PubMed] [Google Scholar]
- 96. Colombel JF, Sands BE, Rutgeerts P, Sandborn W, Danese S, D'Haens G, et al. The safety of vedolizumab for ulcerative colitis and Crohn's disease. Gut. 2017;66(5):839–51. 10.1136/gutjnl-2015-311079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Shen B, Blake A, Lasch K, Smyth M, Bhayat F. Vedolizumab use in patients with inflammatory bowel diseases undergoing surgery: clinical trials and post‐marketing experience. Gastroenterol Rep. 2019;7(5):322–30. 10.1093/gastro/goz034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Lightner AL, Mathis KL, Tse CS, et al. Postoperative outcomes in vedolizumab‐treated patients undergoing major abdominal operations for inflammatory bowel disease: retrospective multicenter cohort study. Inflamm Bowel Dis. 2018;24(4):871–6. 10.1093/ibd/izx076 [DOI] [PubMed] [Google Scholar]
- 99. Yamada A, Komaki Y, Patel N, Komaki F, Aelvoet AS, Tran AL, et al. Risk of postoperative complications among inflammatory bowel disease patients treated preoperatively with vedolizumab. Am J Gastroenterol. 2017;112(9):1423–9. 10.1038/ajg.2017.201 [DOI] [PubMed] [Google Scholar]
- 100. Guo D, Jiang K, Hong J, Zhang M, Shi Y, Zhou B. Association between vedolizumab and postoperative complications in IBD: a systematic review and meta‐analysis. Int J Colorectal Dis. 2021;36(10):2081–92. 10.1007/s00384-021-04017-2 [DOI] [PubMed] [Google Scholar]
- 101. Yung DE, Horesh N, Lightner AL, et al. Systematic review and meta‐analysis: vedolizumab and postoperative complications in inflammatory bowel disease. Inflamm Bowel Dis. 2018;24(11):2327–38. 10.1093/ibd/izy156 [DOI] [PubMed] [Google Scholar]
- 102. Shim HH, Ma C, Kotze PG, Seow CH, al‐Farhan H, al‐Darmaki AK, et al. Preoperative Ustekinumab treatment is not associated with increased postoperative complications in Crohn's disease: a Canadian multi‐Centre observational cohort study. J Can Assoc Gastroenterol. 2018;1(3):115–23. 10.1093/jcag/gwy013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lightner AL, McKenna NP, Tse CS, et al. Postoperative outcomes in Ustekinumab‐treated patients undergoing abdominal operations for Crohn's disease. J Crohns Colitis. 2018;12(4):402–7. 10.1093/ecco-jcc/jjx163 [DOI] [PubMed] [Google Scholar]
- 104. Lightner AL, Grass F, Alsughayer A, Petersen MM, Raffals LE, Loftus EV Jr. Postoperative outcomes in Ustekinumab‐treated patients undergoing abdominal operations for Crohn's disease: single‐center series. J Crohns Colitis. 2019;12(4):402–7. 10.1093/crocol/otz018 [DOI] [PubMed] [Google Scholar]
- 105. Garg R, Mohan BP, Ponnada S, Regueiro M, Lightner AL, Click B. Postoperative outcomes after preoperative ustekinumab exposure in patients with Crohn's disease: a systematic review and meta‐analysis. Ann Gastroenterol. 2021;34(5):691–8. 10.20524/aog.2021.0634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Barnes EL, Lightner AL, Regueiro M. Perioperative and postoperative Management of Patients with Crohn's disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2020;18(6):1356–66. 10.1016/j.cgh.2019.09.040 [DOI] [PubMed] [Google Scholar]
- 107. Coffey CJ, Kiernan MG, Sahebally SM, Jarrar A, Burke JP, Kiely PA, et al. Inclusion of the mesentery in ileocolic resection for Crohn's disease is associated with reduced surgical recurrence. J Crohns Colitis. 2018;12(10):1139–50. 10.1093/ecco-jcc/jjx187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011;(9):CD004320. 10.1002/14651858.CD004320.pub3 [DOI] [PubMed] [Google Scholar]
- 109. McLeod RS, Wolff BG, Ross S, Parkes R, McKenzie M. Recurrence of Crohn's disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis Colon Rectum. 2009;52(5):919–27. 10.1007/DCR.0b013e3181a4fa58 [DOI] [PubMed] [Google Scholar]
- 110. de Barcelos IF, Kotze PG, Spinelli A, Suzuki Y, Teixeira FV, de Albuquerque IC, et al. Factors affecting the incidence of early endoscopic recurrence after ileocolonic resection for Crohn's disease: a multicentre observational study. Colorectal Dis. 2017;19(1):O39–45. 10.1111/codi.13581 [DOI] [PubMed] [Google Scholar]
- 111. Kono T, Ashida T, Ebisawa Y, Chisato N, Okamoto K, Katsuno H, et al. A new antimesenteric functional end‐to‐end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn's disease. Dis Colon Rectum. 2011;54(5):586–92. 10.1007/DCR.0b013e318208b90f [DOI] [PubMed] [Google Scholar]
- 112. Horisberger K, Birrer DL, Rickenbacher A, Turina M. Experiences with the Kono‐S anastomosis in Crohn's disease of the terminal ileum‐a cohort study. Langenbecks Arch Surg. 2021;406(4):1173–80. 10.1007/s00423-020-01998-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Luglio G, Rispo A, Imperatore N, Giglio MC, Amendola A, Tropeano FP, et al. Surgical prevention of anastomotic recurrence by excluding mesentery in Crohn's disease: the SuPREMe‐CD study ‐ a randomized clinical trial. Ann Surg. 2020;272(2):210–7. 10.1097/sla.0000000000003821 [DOI] [PubMed] [Google Scholar]
- 114. Peltrini R, Greco PA, Manfreda A, Luglio G, Bucci L. Kono‐S anastomosis after intestinal resection for Crohn's disease. Updates Surg. 2020;72(2):335–40. 10.1007/s13304-019-00700-w [DOI] [PubMed] [Google Scholar]
- 115. Canin‐Endres J, Salky B, Gattorno F, Edye M. Laparoscopically assisted intestinal resection in 88 patients with Crohn's disease. Surg Endosc. 1999;13(6):595–9. 10.1007/s004649901049 [DOI] [PubMed] [Google Scholar]
- 116. Nguyen SQ, Teitelbaum E, Sabnis AA, Bonaccorso A, Tabrizian P, Salky B. Laparoscopic resection for Crohn's disease: an experience with 335 cases. Surg Endosc. 2009;23(10):2380–4. 10.1007/s00464-009-0362-1 [DOI] [PubMed] [Google Scholar]
- 117. Polle SW, Wind J, Ubbink DT, Hommes DW, Gouma DJ, Bemelman WA. Short‐term outcomes after laparoscopic ileocolic resection for Crohn's disease. A systematic review. Dig Surg. 2006;23(5–6):346–57. 10.1159/000097950 [DOI] [PubMed] [Google Scholar]
- 118. Rosman AS, Melis M, Fichera A. Metaanalysis of trials comparing laparoscopic and open surgery for Crohn's disease. Surg Endosc. 2005;19(12):1549–55. 10.1007/s00464-005-0114-9 [DOI] [PubMed] [Google Scholar]
- 119. Tan JJ, Tjandra JJ. Laparoscopic surgery for Crohn's disease: a meta‐analysis. Dis Colon Rectum. 2007;50(5):576–85. 10.1007/s10350-006-0855-0 [DOI] [PubMed] [Google Scholar]
- 120. Carmichael H, Peyser D, Baratta VM, Bhasin D, Dean A, Khaitov S, et al. The role of laparoscopic surgery in repeat ileocolic resection for Crohn's disease. Colorectal Dis. 2021;23(8):2075–84. 10.1111/codi.15675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Huang R, Valerian BT, Lee EC. Laparoscopic approach in patients with recurrent Crohn's disease. Am Surg. 2012;78(5):595–9. [PubMed] [Google Scholar]
- 122. Pinto RA, Shawki S, Narita K, Weiss EG, Wexner SD. Laparoscopy for recurrent Crohn's disease: how do the results compare with the results for primary Crohn's disease? Colorectal Dis. 2011;13(3):302–7. 10.1111/j.1463-1318.2009.02133.x [DOI] [PubMed] [Google Scholar]
- 123. Horsey ML, Lai D, Herur‐Raman A, et al. Open versus minimally invasive small bowel resection for Crohn's disease: a NSQIP retrospective review and analysis. Surg Endosc. 2021;36:6278–84. 10.1007/s00464-021-08927-8 [DOI] [PubMed] [Google Scholar]
- 124. Coffey JC, O'Leary DP. The mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol. 2016;1(3):238–47. 10.1016/s2468-1253(16)30026-7 [DOI] [PubMed] [Google Scholar]
- 125. Peyrin‐Biroulet L, Gonzalez F, Dubuquoy L, Rousseaux C, Dubuquoy C, Decourcelle C, et al. Mesenteric fat as a source of C reactive protein and as a target for bacterial translocation in Crohn's disease. Gut. 2012;61(1):78–85. 10.1136/gutjnl-2011-300370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med. 1994;1(1):71–81. [PMC free article] [PubMed] [Google Scholar]
- 127. Hong KM, Belperio JA, Keane MP, Burdick MD, Strieter RM. Differentiation of human circulating fibrocytes as mediated by transforming growth factor‐beta and peroxisome proliferator‐activated receptor gamma. J Biol Chem. 2007;282(31):22910–20. 10.1074/jbc.M703597200 [DOI] [PubMed] [Google Scholar]
- 128. Li Y, Zhu W, Gong J, Zhang W, Gu L, Guo Z, et al. Visceral fat area is associated with a high risk for early postoperative recurrence in Crohn's disease. Colorectal Dis. 2015;17(3):225–34. 10.1111/codi.12798 [DOI] [PubMed] [Google Scholar]
- 129. Holt DQ, Moore GT, Strauss BJ, Hamilton AL, De Cruz P, Kamm MA. Visceral adiposity predicts post‐operative Crohn's disease recurrence. Aliment Pharmacol Ther. 2017;45(9):1255–64. 10.1111/apt.14018 [DOI] [PubMed] [Google Scholar]
- 130. Li Y, Ge Y, Gong J, Zhu W, Cao L, Guo Z, et al. Mesenteric lymphatic vessel density is associated with disease behavior and postoperative recurrence in Crohn's disease. J Gastrointest Surg. 2018;22(12):2125–32. 10.1007/s11605-018-3884-9 [DOI] [PubMed] [Google Scholar]
- 131. Li Y, Stocchi L, Liu X, Rui Y, Liu G, Remzi FH, et al. Presence of granulomas in mesenteric lymph nodes is associated with postoperative recurrence in Crohn's disease. Inflamm Bowel Dis. 2015;21(11):2613–8. 10.1097/mib.0000000000000541 [DOI] [PubMed] [Google Scholar]
- 132. Calvin Coffey J, Kiernan M. Adipocyte‐epithelial interactions and Crohn's disease ‐ an emerging drug target. EBioMedicine. 2017;23:193–4. 10.1016/j.ebiom.2017.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Coffey JC, O'Leary DP, Kiernan MG, Faul P. The mesentery in Crohn's disease: friend or foe? Curr Opin Gastroenterol. 2016;32(4):267–73. 10.1097/mog.0000000000000280 [DOI] [PubMed] [Google Scholar]
- 134. Li Y, Zhu W, Zuo L, Shen B. The role of the mesentery in Crohn's disease: the contributions of nerves, vessels, lymphatics, and fat to the pathogenesis and disease course. Inflamm Bowel Dis. 2016;22(6):1483–95. 10.1097/mib.0000000000000791 [DOI] [PubMed] [Google Scholar]
- 135. Ewe K, Herfarth C, Malchow H, Jesdinsky HJ. Postoperative recurrence of Crohn's disease in relation to radicality of operation and sulfasalazine prophylaxis: a multicenter trial. Digestion. 1989;42(4):224–32. 10.1159/000199850 [DOI] [PubMed] [Google Scholar]
- 136. de Groof EJ, van der Meer JHM, Tanis PJ, de Bruyn JR, van Ruler O, D'Haens GRAM, et al. Persistent Mesorectal inflammatory activity is associated with complications after proctectomy in Crohn's disease. J Crohns Colitis. 2019;13(3):285–93. 10.1093/ecco-jcc/jjy131 [DOI] [PubMed] [Google Scholar]
- 137. Fazio VW, Marchetti F, Church M, et al. Effect of resection margins on the recurrence of Crohn's disease in the small bowel. A randomized controlled trial. Ann Surg. 1996;224(4):563–71; discussion 571‐3. 10.1097/00000658-199610000-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Coffey JC, Sehgal R, Walsh D. Mesenteric and peritoneal anatomy. In: Coffey JC, Dockery P, Moran BJ, Heald B, editors. Mesenteric principles of gastrointestinal surgery. 1st ed. Boca Raton, FL: CRC Press; 2017. [Google Scholar]
- 139. Li Y, Mohan H, Lan N, et al. Mesenteric excision surgery or conservative limited resection in Crohn's disease: study protocol for an international, multicenter, randomized controlled trial. Trials. 2020;21(1):210. 10.1186/s13063-020-4105-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Jess T, Riis L, Vind I, Winther KV, Borg S, Binder V, et al. Changes in clinical characteristics, course, and prognosis of inflammatory bowel disease during the last 5 decades: a population‐based study from Copenhagen, Denmark. Inflamm Bowel Dis. 2007;13(4):481–9. 10.1002/ibd.20036 [DOI] [PubMed] [Google Scholar]
- 141. Farmer RG, Hawk WA, Turnbull RB Jr. Clinical patterns in Crohn's disease: a statistical study of 615 cases. Gastroenterology. 1975;68(4 Pt 1):627–35. [PubMed] [Google Scholar]
- 142. Gomollón F, Dignass A, Annese V, Tilg H, van Assche G, Lindsay JO, et al. 3rd European evidence‐based consensus on the diagnosis and Management of Crohn's disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 2017;11(1):3–25. 10.1093/ecco-jcc/jjw168 [DOI] [PubMed] [Google Scholar]
- 143. Martins R, Carmona C, George B, Epstein J. Management of Crohn's disease: summary of updated NICE guidance. BMJ. 2019;367:l5940. 10.1136/bmj.l5940 [DOI] [PubMed] [Google Scholar]
- 144. Preiß JC, Bokemeyer B, Buhr HJ, et al. Updated German clinical practice guideline on “Diagnosis and treatment of Crohn's disease” 2014. Z Gastroenterol. 2014;52(12):1431–84. 10.1055/s-0034-1385199 [DOI] [PubMed] [Google Scholar]
- 145. Gerdin L, Eriksson AS, Olaison G, Sjödahl R, Ström M, Söderholm JD, et al. The Swedish Crohn trial: a prematurely terminated randomized controlled trial of thiopurines or open surgery for primary treatment of Ileocaecal Crohn's disease. J Crohns Colitis. 2016;10(1):50–4. 10.1093/ecco-jcc/jjv184 [DOI] [PubMed] [Google Scholar]
- 146. Wright EK, Kamm MA, De Cruz P, et al. Effect of intestinal resection on quality of life in Crohn's disease. J Crohns Colitis. 2015;9(6):452–62. 10.1093/ecco-jcc/jjv058 [DOI] [PubMed] [Google Scholar]
- 147. Brandstetter S, Monteiro G, de Camargo M, Aiello A, et al. P620 stapled end‐to‐side vs. side‐to‐side anastomosis after ileocecectomy for Crohn's disease: a propensity score‐matched analysis. J Crohns Colitis. 2019;13(Supplement_1):S426–7. 10.1093/ecco-jcc/jjy222.744 [DOI] [Google Scholar]
- 148. Holubar SD, Gunter RL, Click BH, Achkar JP, Lightner AL, Lipman JM, et al. Mesenteric excision and exclusion for ileocolic Crohn's disease: feasibility and safety of an innovative, combined surgical approach with extended mesenteric excision and Kono‐S anastomosis. Dis Colon Rectum. 2022;65(1):e5–e13. 10.1097/dcr.0000000000002287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Zhu Y, Qian W, Huang L, et al. Role of extended mesenteric excision in postoperative recurrence of Crohn's colitis: a single‐center study. Clin Transl Gastroenterol. 2021;12(10):e00407. 10.14309/ctg.0000000000000407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Strong SA. Mesenteric division in Crohn's disease. Oper Tech Gen Surg. 2007;9(1):30–8. 10.1053/j.optechgensurg.2007.04.002 [DOI] [Google Scholar]
- 151. Spinelli A, Bazzi P, Sacchi M, et al. Short‐term outcomes of laparoscopy combined with enhanced recovery pathway after ileocecal resection for Crohn's disease: a case‐matched analysis. J Gastrointest Surg. 2013;17(1):126–32; discussion p.132. 10.1007/s11605-012-2012-5 [DOI] [PubMed] [Google Scholar]
- 152. Zhu Y, Xiang J, Liu W, Cao Q, Zhou W. Laparoscopy combined with enhanced recovery pathway in ileocecal resection for Crohn's disease: a randomized study. Gastroenterol Res Pract. 2018;2018:9648674. 10.1155/2018/9648674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Vigorita V, Cano‐Valderrama O, Celentano V, et al. Inflammatory bowel diseases benefit from enhanced recovery after surgery [ERAS] protocol: a systematic review with practical implications. J Crohns Colitis. 2022;16:845–51. 10.1093/ecco-jcc/jjab209 [DOI] [PubMed] [Google Scholar]
- 154. Huang W, Goldberg RJ, Anderson FA, Kiefe CI, Spencer FA. Secular trends in occurrence of acute venous thromboembolism: the Worcester VTE study (1985‐2009). Am J Med. 2014;127(9):829–39.e5. 10.1016/j.amjmed.2014.03.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010;375(9715):657–63. 10.1016/s0140-6736(09)61963-2 [DOI] [PubMed] [Google Scholar]
- 156. Huang SS, Liu Y, Jing ZC, Wang XJ, Mao YM. Common genetic risk factors of venous thromboembolism in Western and Asian populations. Genet Mol Res. 2016;15(1):15017644. 10.4238/gmr.15017644 [DOI] [PubMed] [Google Scholar]
- 157. Weng MT, Park SH, Matsuoka K, et al. Incidence and risk factor analysis of thromboembolic events in east Asian patients with inflammatory bowel disease, a multinational collaborative study. Inflamm Bowel Dis. 2018;24(8):1791–800. 10.1093/ibd/izy058 [DOI] [PubMed] [Google Scholar]
- 158. Weng MT, Tung CC, Wong JM, Wei SC. Should Asian inflammatory bowel disease patients need routine thromboprophylaxis? Intest Res. 2018;16(2):312–4. 10.5217/ir.2018.16.2.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Brown SR, Fearnhead NS, Faiz OD, Abercrombie JF, Acheson AG, Arnott RG, et al. The Association of Coloproctology of Great Britain and Ireland consensus guidelines in surgery for inflammatory bowel disease. Colorectal Dis. 2018;20(Suppl 8):3–117. 10.1111/codi.14448 [DOI] [PubMed] [Google Scholar]
- 160. Heo CM, Kim TJ, Kim ER, et al. Risk of venous thromboembolism in Asian patients with inflammatory bowel disease: a nationwide cohort study. Sci Rep. 2021;11(1):2025. 10.1038/s41598-021-81657-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Yamamoto T, Allan RN, Keighley MR. Risk factors for intra‐abdominal sepsis after surgery in Crohn's disease. Dis Colon Rectum. 2000;43(8):1141–5. 10.1007/bf02236563 [DOI] [PubMed] [Google Scholar]
- 162. Spinelli A, Allocca M, Jovani M, Danese S. Review article: optimal preparation for surgery in Crohn's disease. Aliment Pharmacol Ther. 2014;40(9):1009–22. 10.1111/apt.12947 [DOI] [PubMed] [Google Scholar]
- 163. Zerbib P, Koriche D, Truant S, Bouras AF, Vernier‐Massouille G, Seguy D, et al. Pre‐operative management is associated with low rate of post‐operative morbidity in penetrating Crohn's disease. Aliment Pharmacol Ther. 2010;32(3):459–65. 10.1111/j.1365-2036.2010.04369.x [DOI] [PubMed] [Google Scholar]
- 164. Udholm LS, Rasmussen SL, Madsbøll TK, Omairi M, El‐Hussuna A. A systemic review and metaanalysis of postoperative outcomes in urgent and elective bowel resection in patients with Crohn's disease. Int J Colorectal Dis. 2021;36(2):253–63. 10.1007/s00384-020-03786-6 [DOI] [PubMed] [Google Scholar]
- 165. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn's disease. Gastroenterology. 1990;99(4):956–63. 10.1016/0016-5085(90)90613-6 [DOI] [PubMed] [Google Scholar]
- 166. Frolkis AD, Lipton DS, Fiest KM, Negrón ME, Dykeman J, deBruyn J, et al. Cumulative incidence of second intestinal resection in Crohn's disease: a systematic review and meta‐analysis of population‐based studies. Am J Gastroenterol. 2014;109(11):1739–48. 10.1038/ajg.2014.297 [DOI] [PubMed] [Google Scholar]
- 167. Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta‐analysis of observational studies. Int J Colorectal Dis. 2008;23(12):1213–21. 10.1007/s00384-008-0542-9 [DOI] [PubMed] [Google Scholar]
- 168. Kim SB, Cheon JH, Park JJ, Kim ES, Jeon SW, Jung SA, et al. Risk factors for postoperative recurrence in Korean patients with Crohn's disease. Gut Liver. 2020;14(3):331–7. 10.5009/gnl19085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Buisson A, Chevaux JB, Bommelaer G, Peyrin‐Biroulet L. Diagnosis, prevention and treatment of postoperative Crohn's disease recurrence. Dig Liver Dis. 2012;44(6):453–60. 10.1016/j.dld.2011.12.018 [DOI] [PubMed] [Google Scholar]
- 170. Markowitz J. Can we change the natural history of Crohn's disease with early immunomodulation? Dig Dis. 2014;32(4):345–50. 10.1159/000358134 [DOI] [PubMed] [Google Scholar]
- 171. Savarino E, Bodini G, Dulbecco P, Assandri L, Bruzzone L, Mazza F, et al. Adalimumab is more effective than azathioprine and mesalamine at preventing postoperative recurrence of Crohn's disease: a randomized controlled trial. Am J Gastroenterol. 2013;108(11):1731–42. 10.1038/ajg.2013.287 [DOI] [PubMed] [Google Scholar]
- 172. Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009;136(2):441–50.e1; quiz 716. 10.1053/j.gastro.2008.10.051 [DOI] [PubMed] [Google Scholar]
- 173. Yoshida K, Fukunaga K, Ikeuchi H, Kamikozuru K, Hida N, Ohda Y, et al. Scheduled infliximab monotherapy to prevent recurrence of Crohn's disease following ileocolic or ileal resection: a 3‐year prospective randomized open trial. Inflamm Bowel Dis. 2012;18(9):1617–23. 10.1002/ibd.21928 [DOI] [PubMed] [Google Scholar]
- 174. Yamada A, Komaki Y, Patel N, Komaki F, Pekow J, Dalal S, et al. The use of vedolizumab in preventing postoperative recurrence of Crohn's disease. Inflamm Bowel Dis. 2018;24(3):502–9. 10.1093/ibd/izx054 [DOI] [PubMed] [Google Scholar]
- 175. Buisson A, Nancey S, Manlay L, Rubin DT, Hebuterne X, Pariente B, et al. Ustekinumab is more effective than azathioprine to prevent endoscopic postoperative recurrence in Crohn's disease. United European Gastroenterol J. 2021;9(5):552–60. 10.1002/ueg2.12068 [DOI] [PMC free article] [PubMed] [Google Scholar]


