Abstract
There is clear evidence that high sodium intake is associated with many health issues including hypertension and cardiovascular diseases (CVDs). Several national and worldwide studies have estimated deaths from CVDs attributable to high sodium. But how to evaluate the impact of high sodium intake on diseases using regional routine monitoring and investigation data is necessary and important. Our study aimed to quantitatively evaluate the high sodium intake attributed to CVDs deaths based on the routine monitoring data from China National Nutrition and Health Survey (CNNHS) in Tianjin, China. The population attributable fractions (PAF) were calculated by comparing the observed systolic blood pressure (SBP) distribution with the theoretical minimum or counterfactual distribution by sex and age groups. The results showed that CVDs deaths due to elevated SBP were 22728 (95% uncertainty intervals: 22679‐23050), accounting for 62.8% of total CVDs deaths. According to sodium intake recommended by World Health Organization (WHO), PAF of CVDs deaths attributable to high sodium diet in our study was 14.6% of total CVDs deaths, accounting for 5228 (95% UI: 5005–5998) cases. The dietary sodium intake of residents is nearly three times than sodium intake recommended by WHO. If sodium intake was reduced to reference level, the potential avoidable CVD deaths attributable to the SBP‐raising effect were more than 5200 among adults 25 aged and over in Tianjin. This evaluation method can be extended to other cities.
Keywords: blood pressure, cardiovascular diseases, population attributable fraction, sodium intake
1. INTRODUCTION
The sodium intake recommended by The World Health Organization (WHO) is below 2000 mg/24 h to prevent chronic disease. 1 There is clear evidence that high sodium intake is associated with many health issues, including cardiovascular diseases (CVDs) and other chronic diseases. 2 The global burden of disease (GBD) research showed that about 70 million disability‐adjusted life‐years and 3 million people died of over‐consumption of sodium in 2017 around the world. 3 Over‐consumption of sodium has been one of the most important factors affecting the GBD. In China, the fraction of all cases of cardiovascular death in this selected population that attributable to sodium intake was 12.6% and a total of 1.18 million deaths in 2013. 4
High sodium intake is associated with elevated blood pressure (BP) and thereby raises the mortality of CVDs, for adults with and without hypertension. 5 , 6 , 7 According to China National Nutrition and Health Survey (CNNHS) 2010–2012, 8 the national average sodium intake is 5013 (95% Confidence Interval, CI: 4858, 5168) mg/24 h, and 92.6% of adults’ sodium intake exceeded the standard in the Chinese proposed intake for preventing non‐infectious chronic diseases (PI‐NCD), with more than twice the WHO recommendations. The intake of salt varies greatly among cities in China. Studies have shown that northern Chinese food sample has a 50% higher sodium content than southern. 9 As a mega city in northern China, about 15 million people are resident in Tianjin and accounting for more than 40% of cardiovascular deaths every year. 10 The latest survey results show that the sodium intake was 5315.8 ± 3196.5 mg/24 h in 2015 and the sodium intake for men was higher than women in Tianjin. 11
Basing the routine monitoring data to establish an evaluation system, and comprehensive estimating the disease burden of controllable risk factors regularly are helpful to formulate specific and effective disease prevention and control strategies. 12 Based on the CNNHS 2015 in Tianjin and Tianjin All Cause of Death Surveillance System covering the whole population, this study estimated the attributable CVDs deaths of residents with high sodium diet by systolic blood pressure (SBP) raising effect in Tianjin.
2. METHODS
2.1. Data sources
This study adopted the 2015 nationally representative cross‐sectional survey of CNNHS in Tianjin program, 13 , 14 which was conducted at seven districts of municipal representativeness. Three sub‐districts or towns were randomly selected from each district by probability proportionate to size sampling (PPS), two neighborhood committees or villages were randomly selected from each selected streets or towns by systematic sampling method, and residents in the selected areas were divided into several groups according to the geographical location of no less than 60 households. One resident group was selected from each selected neighborhood committee or village by PPS. At least 45 households were selected from each resident group to participate in the survey, and no less than 102 people were surveyed by each resident group. Among them, 20 households were investigated as a 3‐day 24‐h dietary survey, and their family condiments were weighed. Survey criteria were defined to include only permanent residents aged 18 and above; participators should live in the local area for more than 6 months within 1 year before the survey; and pregnant women were excluded. During the survey, if there were no suitable respondents or unavailable of selected respondents, they were replaced by rest residents in the same group. The replacement rate should not exceed 35% to ensure representativeness and the actual replacement rate was 24.8%. Totally, 4483 questionnaires and physical examinations, 1955 dietary surveys were completed. The questionnaires included personal information, diseases history (whether suffering from hypertension, etc.), smoking information, physical exercises, dietary habits, and health status.
The blood pressure was gauged by electronic sphygmomanometer (OMRON HBP1300, OMRON Corporation, Kyoto, Japan) with 1 mm Hg accuracy, complying with national metrology certification requirements. Blood pressure was measured and recorded for the first time after 15 min rest, and then every minute. Three times were required totally by taking the average pressure of three diastolic and systolic as results.
Sodium intake was composed of sodium in food and condiments. Hence both individual dietary records and household food consumption were collected over three consecutive days, included two consecutive working days and one rest day. Individual dietary consumption information was collected by trained investigators including all foods consumed at and out of home, type, amounts and place of the meal. Weighting method was used to assess household food consumption, which included all foods and condiments. The Chinese Food Composition was used to calculate the amount of sodium in each food consumed by individuals every day. 8 , 15 , 16 , 17
Totally, 4202 and 1781 cases were included in the analysis of blood pressure and dietary sodium intake aged 25 years and older. This survey was ethically approved by the Ethical Committee of the National Institution and Food Safety, Chinese Center for Disease Control and Prevention (201519‐B). Written informing consent were obtained from all participants.
2.2. Cardiovascular mortality
The death data of CVDs in 2015 were derived from the Tianjin All Cause of Death Surveillance System based on the ICD code of diseased, which covered the registered residence population of the city since 1984. 18 , 19 Previous studies showed that the health outcomes of CVDs related to elevated SBP included ischemic heart disease (ICD‐10:I20‐I25), rheumatic heart disease (I01, I02.0, I05‐I09), aortic aneurysm (I71), endocarditis, myocarditis and myocardial disease (I33, I40, I42), atrial fibrillation and peripheral neuropathy and other circulatory diseases (I48, I73, I70.2, I00, I02.9, I27‐I28, I30‐I32, I34‐I39, I47, I70.8, I72, I77‐I80, I82‐I84, I86‐ I98, G45), ischemic stroke (I63), and hemorrhagic stroke (I61). The relative risk (RR) per 10 mm Hg increase in SBP by age groups (aged 25 and over) and both sex for each health outcome was showed in Table S1. 20
2.3. Relationship of high sodium intake and elevated blood pressure
The data of the association between sodium intake and blood pressure were collected from meta‐analysis of randomized controlled trials and Cochrane studies. 21 The formula was:
where Y is (SBP increase (mm Hg) with each 2300 mg/24 h sodium above the reference level (theoretical minimum distribution); x1 is mid‐value age of study group; x2 is the status of hypertensive: normotensive (x2 = 0) or hypertensive(x2 = 1); x3 is the race: for non‐blacks is 0 and blacks is 1. The theoretical minimum distribution was defined 2000 mg/24 h sodium consistently with the GBD study. Table 1 shows that SBP increase (mm Hg) with each 2300 mg/24 h increase of sodium intake.
TABLE 1.
SBP increase (mm Hg) with each 2300 mg/24 h increase of sodium intake
| SBP increase (mm Hg) | ||
|---|---|---|
| Age group | hypertensive | normotensive |
| 25–29 | 3.2 | 1.3 |
| 30–34 | 3.7 | 1.9 |
| 35–39 | 4.1 | 2.3 |
| 40–44 | 4.8 | 2.9 |
| 45–49 | 5.3 | 3.4 |
| 50–54 | 5.9 | 4.1 |
| 55–59 | 6.5 | 4.6 |
| 60–64 | 6.9 | 5.0 |
| 65–69 | 7.4 | 5.5 |
| 70–74 | 7.9 | 6.1 |
| 75–79 | 8.4 | 6.6 |
| 80+ | 9.0 | 7.1 |
Abbreviation: SBP, systolic blood pressure.
2.4. Statistical analysis
Following the Comparative Risk Assessment framework of GBD, 22 the population attributable fractions (PAF) was calculated by comparing the observed SBP distribution with the theoretical minimum or counterfactual distribution of each disease by sex and age groups. Blood pressure was treated as a continuous variable, and the formula was:
where RR(x) is the relative risk at SBP level x; P(x) is the observed population distribution of SBP; P'(x) is the theoretical minimum SBP distribution (mean of 115 mm Hg with SD of 6 mm Hg) or other counterfactual distributions; and m is the maximum amount of SBP level. CVD mortality attributable to elevated SBP for each disease was calculated by multiplying the PAF with the observed deaths of CVDs by sex and age groups (≥25 years).
Firstly, according to the relationship between the death of CVDs and the elevated SBP, the PAF of the current blood pressure level on CVDs deaths was calculated (step 1); secondly, according to the questionnaires (whether the cases suffering from hypertension) and formula of the effect of dietary sodium intake on elevated SBP, the SBP was measured by excluding the effect of high sodium intake. The PAF of SBP (removed the effect of high sodium intake) on cardiovascular death at present was calculated (step 2). Finally, the PAF of CVDs deaths to the SBP‐raising effect of high sodium intake can be expressed as (step 1–step2). The deaths attributable to high sodium intake was obtained from PAF multiplied by the corresponding number of CVD deaths (Figure 1).
FIGURE 1.
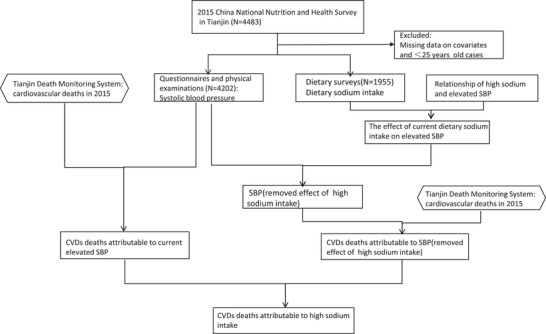
Flowchart of the study design
The measurement data of normal distribution were expressed by means and confidence interval (M, 95%CI). The counting data were expressed by percentage (%). Statistical analysis was carried out with IBM SPSS 19.0 and Office Excel 2013. Uncertainty ranges was estimated by @RISK software (version 6.1 for Excel; Microsoft Corporation, Redmond, WA, USA). 23 Input variables included risk‐factor exposure levels and RR value (RR as a lognormal distribution and others as normal distributions) and output variables included attributable fractions, attributable CVDs deaths. 95% uncertainty intervals were selected for each output variable by using the 1000 iteration values generated between the 2.5th and 97.5th percentile.
3. RESULTS
3.1. Demographic characteristics
There was a total of 4202 (46.0% of males) participants in the final analysis. The mean age was 52.7 ± 14.4. The Prevalence of hypertension was 44.8% (Table 2). The mean of SBP was 141.2 (95%CI: 140.3–142.3) mm Hg for males, and 136.9 (95%CI: 136.0–137.9) mm Hg for females. The SBP for males was higher than females (Table 3). The mean of DBP (Diastolic Blood Pressure) was 84.1 (95%CI: 83.6–84.6) mm Hg for males, and 79.2(95%CI:78.7–79.6) mm Hg for females.
TABLE 2.
Demographic characteristics of participants of the CNNHS in Tianjin
| Variables | Males | Females | Total |
|---|---|---|---|
| Age | 53.4 ± 14.6 | 52.2 ± 14.2 | 52.74 ± 14.4 |
| BMI (kg/m2) a | 25.6(25.5–25.8) | 25.6(25.4–25.8) | 25.6 (5.5–25.7) |
| Systolic Blood Pressure(mm Hg) a | 141.2(140.3–142.3) | 136.9(136.0–137.9) | 138.9(38.2–139.6) |
| Diastolic Blood Pressure(mm Hg) a | 84.1(83.6–84.6) | 79.2(78.7–79.6) | 81.4(81.1–81.8) |
| Hypertension (%) | 50.0 | 40.4 | 44.8 |
| Acute myocardial infarction (%) | 2.2 | 1.2 | 1.7 |
| Atrial fibrillation (%) | 2.6 | 2.4 | 2.5 |
| Heart bypass surgery (%) | .2 | .1 | .1 |
| Percutaneous Coronary Intervention (%) | 1.7 | .7 | 1.1 |
| Angina pectoris | 2.3 | 4.5 | 3.8 |
| Ischemic stroke (%) | 5.7 | 3.4 | 4.5 |
| Hemorrhagic stroke (%) | .8 | .4 | .6 |
Continuous variables have been represented as mean and confidence interval.
TABLE 3.
Distribution of systolic blood pressure among different age groups (mm Hg)
| Males | Females | Total | ||||
|---|---|---|---|---|---|---|
| Age(y) | Mean | 95%CI | Mean | 95%CI | Mean | 95%CI |
| 25–29 | 129.0 | 126.6,131.3 | 118.6 | 116.7,120.4 | 123.4 | 121.8,125.0 |
| 30–34 | 127.5 | 125.2,129.8 | 119.1 | 117.0,121.1 | 122.7 | 121.1,124.2 |
| 35–39 | 133.1 | 130.4,135.9 | 121.6 | 119.1,124.2 | 127.2 | 125.2,129.2 |
| 40–44 | 135.9 | 133.2,138.7 | 126.4 | 124.3,128.5 | 130.3 | 128.5,132.0 |
| 45–49 | 138.3 | 135.5,141.1 | 132.6 | 130.0,135.2 | 135.0 | 133.0,136.9 |
| 50–54 | 139.6 | 137.1,142.0 | 139.2 | 136.6,141.7 | 139.4 | 137.6,141.2 |
| 55–59 | 142.6 | 139.9,145.3 | 141.0 | 138.4,143.5 | 141.7 | 139.8,143.5 |
| 60–64 | 145.4 | 143.2,147.7 | 146.1 | 143.9,148.3 | 145.8 | 144.2,147.3 |
| 65–69 | 149.6 | 146.8,152.5 | 148.0 | 145.1,150.8 | 148.8 | 146.7,150.8 |
| 70–74 | 152.5 | 148.9,156.2 | 157.2 | 153.4,161.0 | 154.8 | 152.2,157.5 |
| 75–80 | 152.7 | 147.6,157.9 | 156.2 | 151.2,161.2 | 154.3 | 150.8,157.9 |
| 80+ | 155.2 | 146.7,163.7 | 149.6 | 141.0,158.1 | 152.8 | 146.8,158.7 |
| Total | 141.2 | 140.3,142.3 | 136.9 | 136.0,137.9 | 138.9 | 138.2,139.6 |
Among the 1781 respondents for dietary survey, 835 were males, accounting for 46.9%; 946 were females, accounting for 53.1%. The mean of dietary sodium intake was 5920.4 (95%CI: 5752.4–6088.5) mg/24 h. The mean of dietary sodium intake ranged from 4924.4 (95%CI: 4202.3–5646.4) to 7422.7 (95%CI: 6674.4–8171.1) mg/24 h for men and 4765.0 (95%CI: 3962.9‐ 5567.1) to 6426.2 (95%CI: 5822.7‐ 7029.6) mg/24 h for women by different age group. Total intake for men residents was higher than women (Table 4).
TABLE 4.
Distribution of dietary sodium intake among different age groups (mg/24h)
| Males | Females | Total | ||||
|---|---|---|---|---|---|---|
| Age(y) | Mean | 95%CI | Mean | 95%CI | Mean | 95%CI |
| 25–29 | 5449.2 | 4560.6,6337.8 | 5596.7 | 4636.7,6556.6 | 5523.7 | 4880.6,6166.8 |
| 30–34 | 6424.2 | 5400.1,7448.3 | 4801.8 | 4049.0,5554.7 | 5481.7 | 4859.9,6103.5 |
| 35–39 | 4924.4 | 4202.3,5646.4 | 5213.6 | 4469.7,5957.6 | 5075.9 | 4564.1,5587.7 |
| 40–44 | 5557.8 | 4487.9,6627.8 | 5192.6 | 4297.5,6087.7 | 5343.2 | 4666.4,6020.0 |
| 45–49 | 6199.4 | 5068.2,7330.6 | 5488.0 | 4769.9,6206.2 | 5805.9 | 5168.8,6442.9 |
| 50–54 | 5663.2 | 5072.7,6253.7 | 5565.3 | 5074.9,6055.7 | 5610.4 | 5233.9,5986.9 |
| 55–59 | 5840.2 | 5162.8,6517.7 | 5541.7 | 5066.8,6016.6 | 5676.7 | 5278.0,6075.5 |
| 60–64 | 7422.7 | 6674.4,8171.1 | 6426.2 | 5822.7,7029.6 | 6896.4 | 6420.2,7372.6 |
| 65–69 | 6545.7 | 5800.0,7291.5 | 6062.8 | 5269.0,6856.6 | 6297.3 | 5755.0,6839.6 |
| 70–74 | 6624.3 | 5486.7,7761.9 | 5557.3 | 4873.1,6241.5 | 6067.9 | 5419.3,6716.6 |
| 75–80 | 5974.2 | 4600.9,7347.4 | 4765.0 | 3962.9,5567.1 | 5420.6 | 4595.9,6245.3 |
| 80+ | 5774.2 | 4730.0,6818.5 | 6464.0 | 4433.4,8494.6 | 6057.2 | 5072.6,7041.9 |
| Total | 6222.0 | 5957.8,6486.1 | 5654.3 | 5441.5,5867.1 | 5920.4 | 5752.4,6088.5 |
3.2. CVDs mortality attributable to elevated SBP
According to Tianjin All Cause of Surveillance System, 36167 CVDs deaths among 25 years old and over in Tianjin in 2015, and the number of CVDs deaths due to elevated SBP was 22728 (95%UI: 22679–23050), accounting for 62.8% CVDs deaths. The top three diseases due to elevated SBP were ischemic heart disease, ischemic and hemorrhagic stroke, respectively, due to12091, 6527, 3829 deaths, and accounting for 64.1%, 58.9%, 68.9% deaths of corresponding diseases. The PAF of CVDs deaths due to elevated SBP for men is higher than women, as shown in Table 5.
TABLE 5.
CVDs deaths attributable to elevated SBP by sex in Tianjin, 2015
| Males | Females | Total | ||||
|---|---|---|---|---|---|---|
| Health outcomes | PAF (95%UI) | Deaths (95%UI) | PAF (95%UI) | Deaths (95%UI) | PAF (95%UI) | Deaths (95%UI) |
| Ischemic heart disease | 65.6% | 6375(5974–6405) | 61.5% | 5621(5558–5959) | 64.1% | 12091(11496–12183) |
| Rheumatic heart disease | 34.2% | 29(28–29) | 33.2% | 36(35–37) | 33.7% | 65(62–66) |
| Aortic aneurysm | 45.8% | 24(23–24) | 43.8% | 15(14–16) | 45.0% | 39(37–40) |
| Endocarditis, myocarditis and myocardial diseases | 48.2% | 16(15–16) | 46.6% | 8(8–9) | 47.2% | 24(23–24) |
| Atrial fibrillation, peripheral vascular disease, and other circulatory diseases | 46.2% | 84(81–84) | 41.3% | 68(63–70) | 44.2% | 152(146–154) |
| Ischemic stroke | 60.6% | 3786(3731–3806) | 56.0% | 2708(2616–2722) | 58.9% | 6527(6397–6622) |
| Hemorrhagic stroke | 70.4% | 2280(2271–2300) | 66.5% | 1540(1532–1627) | 68.9% | 3829(3804–3887) |
| Cardiovascular diseases | 64.4% | 12594(12391–12766) | 60.2% | 9996(9986–10170) | 62.8% | 22728(22679–23050) |
Abbreviation: PAF, population attributable fractions.
3.3. CVDs mortality attributable to the SBP raising effect of dietary sodium intake
Considering sodium intake of 2000 mg/24 h as the theoretical minimum distribution, the PAF of cardiovascular deaths attributable to high sodium diet in Tianjin was 14.6% CVDs deaths, with 5228 (95%UI: 5005–5998) cases. The top three of PAF of high sodium diet for CVDs were ischemic heart disease, hemorrhagic stroke and ischemic stroke. Compared with men, it is slightly higher of the PAF of CVDs deaths due to high sodium diet for women (Table 6).
TABLE 6.
CVDs deaths attributable to high sodium consumption > 2000 mg/24 h by Sex in Tianjin, 2015
| Males | Females | Total | ||||
|---|---|---|---|---|---|---|
| Health outcomes | PAF | Deaths (95%UI) | PAF | Deaths (95%UI) | PAF | Deaths (95%UI) |
| Ischemic heart disease | 14.5% | 1404(1315–1498) | 15.4% | 1410(1317–1503) | 14.8% | 2780(2601–3040) |
| Rheumatic heart disease | 9.8% | 8(7–9) | 9.9% | 11(10–13) | 9.9% | 19(17–25) |
| Aortic aneurysm | 12.1% | 6(5–7) | 11.1% | 4(3–4) | 11.7% | 10(9–11) |
| Endocarditis, myocarditis and myocardial diseases | 12.1% | 4(3–4) | 10.5% | 2(2–3) | 10.9% | 6(5–6) |
| Atrial fibrillation, peripheral vascular disease, and other circulatory diseases | 12.1% | 22(20–25) | 11.9% | 19(17–24) | 12.0% | 41(35–48) |
| Ischemic stroke | 14.1% | 883(835–948) | 14.3% | 691(655–761) | 14.1% | 1565(1422–2007) |
| Hemorrhagic stroke | 14.4% | 466(429–514) | 15.0% | 347(305–398) | 14.5% | 806(744–873) |
| Cardiovascular diseases | 14.3% | 2794(2682–2999) | 15.0% | 2485(2348–2603) | 14.6% | 5228(5005–5998) |
Abbreviation: PAF, population attributable fractions.
4. DISCUSSION
Even though the global burden of CVDs has steadily decreased during the past 10 years, it remains the leading cause of death and disability in developed and several developing countries. 24 As the largest single contributor to global mortality, CVDs accounts for more than 40% of deaths in China 25 and more than 50% of deaths in Tianjin. 10 Population salt reduction is recognized as one of the most cost‐effective, feasible and affordable strategies to prevent CVDs, 26 , 27 especially for developing countries. 28 , 29
This study indicates that the per capita sodium intake was 5920.4 (95%CI: 5752.4–6088.5) mg for people 25 years old and over in Tianjin, which is higher than the average in China (5013 mg/24 h) and nearly three times of the sodium intake recommended by the WHO (2000 mg/24 h). As a key element of human body, sodium mainly acts on regulating extracellular fluid, maintain acid‐base balance and normal blood pressure. Excessive sodium intake will cause hypertension and the occurrence of CVDs. The PAF of CVDs deaths attributed to high salt diet for 25 years old and over in Tianjin was 14.6%, a total of 5228 (95%UI: 5005–5998) attributed deaths. This result is lower than the 2013 GBD China research (PAF: 25.2%), 30 and also lower than the research of Shandong province, China (PAF: 19.9% with reference level of 2000 mg/d). 31 This may be related to the age structure of people in different regions and the proportion of salt sensitivity of people and suggest that our future research should focus on the type of hypertension and degree of aging in different regions. 32 , 33 The top three PAF of high sodium diet for CVDs are ischemic heart disease, hemorrhagic stroke and ischemic stroke, which is in consistent with the national research results. 4 It is indicated that the CVDs caused by high sodium diet has higher ratio for women than men, which should be deserved more attention in the publicity and health education of salt reduction. Moreover, in most families of Tianjin, it is usually woman takes responsible of cooking, so strengthening the publicity of women's salt intake will both benefit health of their own and whole family.
In our study, sodium was mainly from salt and condiments, followed by cereal. It is typical dietary feature of northern China. Relevant studies showed that the dietary sodium in China mainly comes from salt. 8 , 9 It should be noted that the consumption of flour products in northern China is more than twice that in southern China, 34 and the contribution rate of flour products to dietary sodium in northern China ranks third, accounting for 7.1% of the total sodium intake. 8 Therefore, evaluate the impact of high sodium intake on diseases using regional routine monitoring and investigation data is necessary and important for different regions. Our study quantitatively evaluated the relationship between sodium intake and CVDs in Tianjin, China, the design using routinely collected data from CNNHS and All Cause of Death Surveillance System, can be used to rapidly and periodically assess the high sodium risk for CVDs and evaluate the effects of control measures.
The Medium‐ and Long‐Term Plan for the Prevention and Treatment of Chronic Diseases in Tianjin (2017‐2025) puts forward the goal of reducing the per capita salt intake by 15% by 2025. The implementation plan of healthy Tianjin puts forward the advocated salt reduction goal that the per capita daily salt intake is no more than 5 g. Tianjin Centers for Diseases Control and Prevention (CDC) has carried out a series of publicity on the theme of “reducing salt and preventing cardiovascular diseases” since 2015: including special knowledge serialization in mainstream media; Designing of salt reduction toolkits; Cooperation with health supermarkets and health restaurants by playing health promotion videos on salt reduction. Our study can provide baseline data and reference for the evaluation of the above publicity effect and support the government with decision‐making related to salt reduction.
The study design using routinely collected data from death certificates can be a quick, efficient, and reliable method to assess and monitor PAF of high sodium diet for CVDs in other cities or countries that have a routine and reliable surveillance system of CNNHAS and death certification. However, limitations of the study include: firstly, the gold standard for measuring salt intake is to measure sodium in 24‐h urine collection. 35 , 36 Data in study was obtained from dietary survey rather than 24‐h urine, although quality‐control measures had been implemented Strictly. Secondly, the effects of high sodium intake on SBP, the RR values of SBP and CVDs come from Cochrane study and GBD study, where effects come from the global data collection and may not reflect the true effect of Tianjin population. Thirdly, only the single factor of high salt diet with SBP‐raising effect was analyzed, various risk factors were not considered as the combined effect.
5. CONCLUSIONS
Our findings highlight the over‐consumption of sodium has become one of the most important factors affecting the GBD. If sodium intake was reduced to WHO standard, the potential avoidable CVD deaths attributable to the SBP‐raising effect of high sodium intake would be more than 5200 among adults 25 aged and over in Tianjin. Our study also suggests that it can be done more in‐depth research in future, such as screening and individualized treatment of salt sensitive people, which is conducive to improve the blood pressure level of hypertensive patients and reduce the incidence of CVDs.
AUTHOR CONTRIBUTIONS
Xiao‐Dan Xue, Wei Li contributed to the project development, data analysis, manuscript writing and editing. Mei‐Qiu Xie verified the analytical methods and discussed the results. De‐Zheng Wang, Dan‐Dan Li, Peng Xin contributed to data collection. Guo‐Hong Jiang and Wen‐Long Zheng conceived the presented idea and designed the study. All authors discussed the results and commented on the manuscript.
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
This research was supported by the Chinese Nutrition Society, Nutrition science popularization and Communication Research Fund (CNS‐SCP2020‐144) and Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK‐051A). The funder had no role in decision to publish, content of this review paper, or preparation of the review paper. No copyrighted materials or tools were used in this research.
Xue X‐D, Li W, Xie M‐Q, et al. High sodium diet intake and cardiovascular diseases: An attributable death study in Tianjin, China. J Clin Hypertens. 2023;25:30–37. 10.1111/jch.14599
Xiao‐Dan Xue and Wei Li are co‐first authors and contributed equally to this work.
Contributor Information
Wen‐Long Zheng, Email: zhengwenlong2006@126.com.
Guo‐Hong Jiang, Email: jghcdc@126.com.
REFERENCES
- 1. Organization World Health . Guideline: sodium intake for adults and children. Geneva: world Health Organization; 2012. p. 46. [PubMed]
- 2. He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52(5):365‐382. [DOI] [PubMed] [Google Scholar]
- 3. GBD 2017 Causes of Death Collaborators . Global, regional, and national age‐sex‐specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159) :1736‐1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liu S, Cai Y, Zeng X, et al. Deaths and life expectancy losses attributable to diet high in sodium in China. Chin J Epidemiol. 2017;38(8):1022‐1027. [DOI] [PubMed] [Google Scholar]
- 5. Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose‐response meta‐analysis of experimental studies. Circulation. 2021;143(16):1542‐1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta‐analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16(11):761‐770. [DOI] [PubMed] [Google Scholar]
- 7. Sodium Whelton PK. Blood pressure, and cardiovascular disease. Hypertension. 2021; (6):2138‐2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fang K, He Y, Fang Y, Lian Y. Dietary sodium intake and food sources among Chinese adults: data from the CNNHS 2010–2012. Nutrients. 2020;12(2):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Anderson CAM, Appel LJ, Okuda N, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110(5):736‐745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xu ZL, Zhang H, Wang DZ, Song GD, Zhang Y, Shen CF. Analysis on causes of death and life expectancy in residents of Tianjin. J Tianjin Med. 2014;44(12):1510‐1513. [Google Scholar]
- 11. Wang ZB, Pan Y, Xin P, Zhang J, Jiang GH. Dietary intake of sodium and potassium among adult inhabitants and evaluation of survey methods in Tianjin in 2015. J Prev Med. 2019;53(11):1141‐1146. [DOI] [PubMed] [Google Scholar]
- 12. Murray CJL, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448‐457. [DOI] [PubMed] [Google Scholar]
- 13. Xue X, Jiang G, Li W, Wang D, Song G, Zheng W. Status quo on smoking and related change pattern of smoking related behavior in past 20 years in urban residents in Tianjin. Chin J Epidemiol. 2019;40(9):1095‐1098. [DOI] [PubMed] [Google Scholar]
- 14. Pang S, Song P, Sun X, et al. Dietary fructose and risk of metabolic syndrome in Chinese residents aged 45 and above: results from the China National Nutrition and Health Survey. Nutr J. 2021;20(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Du S, Wang H, Zhang B, Popkin BM. Dietary potassium intake remains low and sodium intake remains high, and most sodium is derived from home food preparation for Chinese adults, 1991–2015 trends. J Nutr. 2020;150(5):1230‐1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yang YX, Wang GW, Pan XC. China Food Composition Tables. Peking University Medical Press; 2009. [Google Scholar]
- 17. Huang LN, Wang HJ, Wang ZH, et al. Association of red meat usual intake with serum ferritin and the risk of metabolic syndrome in Chinese adults: a longitudinal study from the china health and nutrition survey. Biomed Environ Sci. 2020;33(1):19‐29. [DOI] [PubMed] [Google Scholar]
- 18. Li W, Xue X, Li D, et al. Smoking cessation‐associated mortality reduction: a case‐control study in Tianjin city. Tob Induc Dis. 2021;19(3):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li W, Wang D, Zhang H, et al. The methodology for assessing smoking‐attributed mortality based on all causes of death surveillance in Tianjin, China. Tob Induc Dis;18(3):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Forouzanfar MH, Afshin A, Alexander LT, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks. Lancet;388(10053):1659‐1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624‐634. [DOI] [PubMed] [Google Scholar]
- 22. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet;380(9859):2224‐2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Corporation P, @RISK software version 6.1 for Excel. http://www.palisade.com/risk/
- 24. Ravera A, Carubelli V, Sciatti E, et al. Nutrition and cardiovascular disease: finding the perfect recipe for cardiovascular health. Nutrients. 2016;8(6):363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhou M, Wang H, Zhu J, et al. Cause‐specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet;387(10015):251‐272. [DOI] [PubMed] [Google Scholar]
- 26. Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world‐a systematic review of progress towards the global target. PLoS ONE. 2015;10(7):e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bibbins‐Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362(7):590‐599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nathan AJ, Scobell A. Global status report on noncommunicable diseases 2010. 2012;91(5):72‐83. [Google Scholar]
- 29. Xi B, Hao Y, Liu F. Salt reduction strategies in China. Lancet. 2014;383(9923):1128. [DOI] [PubMed] [Google Scholar]
- 30. Liu M, Li YC, Liu SW, et al. Burden of disease attributable to high‐ sodium diets in China. J Prev Med. 2013;50(9):759‐763. [DOI] [PubMed] [Google Scholar]
- 31. Zhang J, Guo X, Lu Z, et al. Cardiovascular diseases deaths attributable to high sodium intake in Shandong province, China. J Am Heart Assoc. 2019;8(1): e10737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37(2):429‐432. [DOI] [PubMed] [Google Scholar]
- 33. Weinberger MH. Salt sensitivity is associated with an increased mortality in both normal and hypertensive humans. J Clin Hypertens. 2002;4(4):274‐276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Huang L, Wang H, Wang Z, Zhang J, Zhang B, Ding G. Regional disparities in the association between cereal consumption and metabolic syndrome: results from the China health and nutrition survey. Nutrients. 2019;11(4):764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Holbrook JT, Patterson KY, Bodner JE. Sodium and potassium intake and balance in adults consuming self‐selected diets. Am J Clin Nutr. 1984;40(4):786‐793. [DOI] [PubMed] [Google Scholar]
- 36. Clark AJ, Mossholder S. Sodium and potassium intake measurements: dietary methodology problems. Am J Clin Nutr. 1986;43(3):470‐476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


