Abstract
Background & Aims
The function and structure of social relationships influence mortality in individuals within the general population. We compared aspects of social relationships in individuals with cirrhosis and a matched comparison cohort and studied their association with health-related quality of life (HRQoL) and mortality in cirrhosis.
Methods
Individuals with cirrhosis and comparators were identified among participants of the Danish National Health Surveys 2010–2017. The surveys included questions on functional (social support and loneliness) and structural (living alone/cohabitating and frequency of contacts with relatives and friends) aspects of social relationships and HRQoL (Short Form-12). We estimated associations of aspects of social relationships with HRQoL and all-cause mortality in individuals with cirrhosis through 2020.
Results
Of 541 individuals with cirrhosis and 2,157 comparators, low social support (22% in cirrhosis vs. 13% in comparators), loneliness (35% vs. 20%), and living alone (48% vs. 22%) were more frequent in individuals with cirrhosis than comparators, whereas the frequency of contacts with relatives and friends was similar. Except for living alone, weak functional and structural social relationships were associated with lower mental HRQoL in those with cirrhosis. Physical HRQoL was only marginally associated with social relationships. During 2,795 person-years of follow-up, 269 individuals with cirrhosis died. Functional and not structural aspects of social relationships were associated with risk of mortality in cirrhosis. Specifically, the adjusted hazard ratio was 1.4 (95% CI 1.1–1.9), p = 0.011, for low vs. moderate-to-high social support (functional aspect), and 1.0 (95% CI 0.8–1.3), p = 0.85 for living alone vs. cohabitating (structural aspect).
Conclusions
Individuals with cirrhosis have weaker functional and structural social relationships than matched comparators. Weak functional relationships are associated with lower mental HRQoL and increased risk of mortality in individuals with cirrhosis.
Impact and implications
This study investigated the prevalence of weak social relationships in individuals with cirrhosis and their influence on health-related quality of life and risk of mortality. Individuals with cirrhosis were nearly twice as likely to report low social support, loneliness, and to live alone than a matched comparison cohort. Low social support and loneliness (functional measures of social relationships) were associated with lower mental health-related quality of life and increased risk of mortality risk in cirrhosis, when adjusting for known confounders. We hope that these results will make healthcare providers aware of the functional aspects of the social relationships of individuals with cirrhosis, in addition to the traditional clinical management, and motivate further research of interventions to strengthen the social support of individuals with cirrhosis.
Keywords: Cirrhosis, Social support, Social relationships, Mortality, Alcohol-related liver disease, Cohort study
Abbreviations: CCI, Charlson Comorbidity Index; DNHS, Danish National Health Surveys; HRQoL, Health-Related Quality of Life; HR, Hazard Ratio; ICD-10, International Classification of Diseases, Tenth Revision; ISCED, International Standard Classification of Education; SF-12, Short Form-12
Graphical abstract
Highlights
-
•
Social relationships influence survival in the general population.
-
•
We studied social relationships in cirrhosis in relation to HRQoL and mortality.
-
•
Low social support, loneliness, and living alone occurred more often in cirrhosis.
-
•
Low social support and loneliness were associated with low mental HRQoL and mortality in cirrhosis.
-
•
Living alone vs. cohabitating was not associated with HRQoL or mortality in cirrhosis.
Introduction
Social relationships influence survival through behavioural, psychological, and biological mechanisms.1 In the general population, weak social relationships are associated with an increased mortality risk with an effect size comparable to daily cigarette smoking.2,3 There are functional and structural aspects to social relationships.1 The functional aspect of social relationships includes social support and loneliness. Social support is commonly described as the perceived supportive resources available in one’s social network,1 and loneliness as the subjective state of discrepancy between one’s preferred and actual levels of social contact.4,5 The structural aspect of social relationships is the extent to which an individual participates in social relationships, and it can be described by cohabitation status and frequency of contact with relatives and friends.2 There is only a weak to moderate correlation between the functional and structural aspects of social relationships.6 For instance, far from all individuals who live alone report low social support or loneliness,[7], [8], [9] and as many as 10% of individuals who are cohabitating and therefore have structural social support report low social support or loneliness.7,8
Weak social relationships may be more prevalent in individuals with cirrhosis because of an association with underlying lifestyle factors. For example, heavy drinking, the dominant cause of cirrhosis in Denmark, is associated with an increased likelihood of living alone and with low social support.[10], [11], [12], [13] Further, individuals with weak social relationships have a lower adherence with medical treatments.14,15 Therefore, individuals with cirrhosis who have weak social relationships may be particularly vulnerable and have a poor prognosis.
Knowledge of the impact of social relationships in cirrhosis could motivate studies of interventions to enhance social support in these individuals. There is recent evidence that interventions can enhance social support and decrease hospitalisation rates in selected medical patients,[16], [17], [18] but these studies did not consider cirrhosis.
We therefore conducted a historical cohort study in Denmark of the prevalence of weak social relationships in individuals with cirrhosis and matched comparators. We then investigated whether weak social relationships affected health-related quality of life (HRQoL) and risk of mortality in individuals with cirrhosis.
Patients and methods
In Denmark, citizens have access to universal, tax-financed healthcare and social security benefits. As such, clinical and material support is available to individuals with cirrhosis. We identified individuals with cirrhosis and a matching comparison cohort among the participants of the Danish National Health Surveys (DNHS) 2010, 2013, and 2017. We used the personal identification number given to all residents in Denmark to link information at the individual level from the DNHS, which included questions about social relationships and HRQoL, with national registries on cirrhosis diagnoses and with vital statistics.19 Individuals with cirrhosis were followed for mortality from their participation in the DNHS through 2020.
Danish National Health Surveys
We used data from the 3 DNHS conducted in 2010, 2013, and 2017, described in detail elsewhere.20 In short, DNHS is based on self-administered questionnaires completed digitally or by postal mail by a random sample of Danish residents. Each cross-sectional survey is representative nationally, regionally, and for every municipality. The questionnaires contain approximately 55 key questions.
Around 300,000 individuals (aged >16 years) were invited to participate in each survey year (2010, 2013, and 2017) and the participation rates ranged from 54% to 60%. We extracted data on aspects of social relationships, HRQoL, alcohol, and smoking.
Individuals with cirrhosis
We used the National Patient Registry to identify individuals who had been diagnosed with cirrhosis before participating in the DNHS (International Classification of Diseases, Tenth Revision [ICD-10] K70.3, K70.4, K74.6). The Danish National Patient Registry includes data from inpatient and outpatient hospital contacts since 1995, as well as inpatient data going back to 1977.21 The treating physician specifies up to 20 diagnoses, coded according to ICD-10 since 1994. We restricted the study cohort to those individuals who had their first diagnosis of cirrhosis within 10 years before participating in the DNHS. A history of decompensated cirrhosis at the time of participating in the DNHS was defined according to the Baveno criteria as a history of variceal bleeding or ascites, with or without spontaneous bacterial peritonitis, as indicated by diagnostic and procedure codes registered by the treating physician in the National Patient Registry.22 Table S1 shows the selection of the cohort. All diagnostic and other codes are provided in Table S2.
Comparison cohort
We compared aspects of social relationships between individuals with cirrhosis and comparators among the participants of the DNHS. Weak social relationships are more prevalent in individuals with low socioeconomic status, which was also observed in the DNHS.23 We matched comparators on educational level in addition to sex and age on the day of the cirrhosis diagnosis. For each included patient with cirrhosis, we identified 4 comparators without cirrhosis among the participants in the DNHS. Information on educational level was retrieved from the Population Education Registry.24 We grouped educational level according to the International Standard Classification of Education (ISCED), noting that Denmark has no educational program that corresponds to ISCED level 4, post-secondary non-tertiary education.25 The following 3 educational levels were used in this study: (1) ‘low’: ≤10 years of duration corresponding to lower secondary school or lower; (2) ‘medium-low’: 12 years of duration corresponding to vocational training or lower; (3) ‘medium-high’ or ‘high’: ≥14 years of duration corresponding to a bachelor degree or higher. If educational level was missing (3%), a low level of education was assumed.24
Aspects of social relationships
Information on social relationships was extracted from the DNHS. Information on social support and loneliness described the functional aspects of social relationships, whereas cohabitation status and frequency of contact with relatives and friends described the structural aspects (see Table S3 for measures used to describe social relationships).
Social support can be in the form of emotional or tangible support and further subdivided into received or perceived support.1 We only had information on perceived emotional support, which has the strongest associations with low mental quality of life and survival,6 and was assessed by the question ‘Do you have someone to talk to if you have problems?’. We dichotomised the 4 response options into ‘low’ and ‘moderate-to-high’ social support, in which the responses ‘no, never, or almost never’, and ‘yes, occasionally’ were interpreted as low social support, and ‘yes, most of the time’, and ‘yes, always’ were interpreted as moderate-to-high social support. Loneliness can be interpreted as the subjective state of discrepancy between one’s preferred and actual levels of social contact4,5 and it may also be interpreted as a feeling that could also persist even in social company.26 We only had data available of the first definition of loneliness and this was assessed by the question: ‘Are you ever alone, although you would prefer to be together with other people?’. We dichotomised the 4 response options into ‘loneliness’ and ‘no loneliness’, in which the responses ‘yes, often’ and ‘yes, occasionally’ were interpreted as loneliness and the responses ‘yes, rarely’ and ‘no’ were interpreted as no loneliness. The questions used to measure social support and loneliness have not been formally validated but are included in validated questionnaires to assess social support and loneliness.27,28
Information on cohabitation status was obtained by the question: ‘Do you live together with other people?’ with the subheading ‘I live with a spouse/partner/girlfriend/boyfriend’ with the response categories ‘yes’ and ‘no’. Information on cohabitation status was missing in the DNHS in 5 (1%) of individuals with cirrhosis and in 17 (1%) of comparators, and for these 22 individuals we obtained the cohabitation status from the Family Registry.29 We categorised cohabitation status as living alone or cohabitating. The following questions from the DNHS were used to assess frequency of contacts with relatives and friends: ‘How often are you in contact with family you do not live with?’ and ‘How often are you in contact with friends you do not live with?’ and for both questions it was noted that ‘contact means that you are together, talk on the phone, write to each other, etc.’ For both questions, the response categories were: ‘daily’; ‘several times a week’; ‘several times a month’; ‘less often than once a month’; and ‘never’. We categorised frequency of contacts with family and friends into at least 3 times per week and 2 or fewer times per week, following the categorisation in a prior study of structural aspects of social relationships and mortality risk in the general Danish population, also based on the DNHS.30
Covariates
We included information from the DNHS on HRQoL, alcohol consumption, and smoking. HRQoL was assessed by the Short Form-12 (SF-12). The SF-12 is a brief measure of HRQoL that generates both a physical component score and a mental component score, both ranging from 0 to 100. Higher scores indicate a better health status.31 Alcohol consumption was assessed by obtaining information on the number of standard alcohol drinks consumed each day during a typical week, with a standard drink containing 12 g of alcohol. Smoking was categorised as current smoking or not.31 Comorbidity was defined with the Charlson Comorbidity Index (CCI), based on hospital diagnoses received during the 5 years prior to participation in the DNHS and excluding diagnostic codes for cirrhosis.32
Main analysis: association of social relationships with HRQoL and risk of mortality in cirrhosis
We showed correlations of the included measures of social relationships in the study and prepared cross tabulations of social support, loneliness, cohabitation status, and frequency of contacts with relatives and friends in individuals with cirrhosis and comparators (Table S4).
Next, we prepared tables of clinical characteristics in individuals with cirrhosis according to social support, loneliness, cohabitation status, and frequency of contacts with relatives and friends. We used linear regression to analyse the associations between physical and mental HRQoL and social support, adjusting for age, sex, CCI, smoking, alcohol consumption, and time since cirrhosis diagnosis.
We used the Kaplan-Meier estimator to compute cumulative all-cause mortality according to social support. We used Cox regression to analyse the association between social support and risk of all-cause mortality in individuals with cirrhosis. Individuals with cirrhosis contributed observation time from participation in the DNHS until death, emigration, or end of follow-up on December 31, 2020, whichever occurred first. Time since DNHS was the underlying time-axis and the analyses were adjusted for age, sex, CCI, smoking, alcohol consumption, and time since cirrhosis diagnosis. The proportional hazards assumption was tested for each covariate and globally on the basis of Schoenfeld residuals. No violations were detected. We conducted the same analyses for loneliness, cohabitation status, and frequency of contacts with relatives and friends as for social support.
Risk of mortality in subgroups and analyses of other outcomes
We analysed whether the associations between functional and structural aspects of social relationships and risk of mortality varied between subgroups of individuals with cirrhosis (men/women, alcohol drinkers/alcohol abstainers, compensated/decompensated cirrhosis). Moreover, we analysed the risk of all-cause acute admission, the combined endpoint of risk of decompensation or all-cause death, and liver-related death as other outcomes instead of all-cause mortality risk.
Risk of mortality in comparators
Finally, we used Cox regression to analyse the association of functional and structural aspects of social relationships with risk of all-cause mortality in the comparators. In these comparators-only analyses, we adjusted for age, sex, CCI, smoking, and alcohol consumption.
Results
We identified 541 individuals with cirrhosis and 2,157 comparators matched on gender, age, and educational level among the participants of the DNHS. Their median age at the time of the survey was 62 years and 63% were men (Table 1). Individuals with cirrhosis reported low social support more often than comparators did (22% vs. 13%), and the same pattern was seen for loneliness (35% vs. 20%), and living alone (48% vs. 22%), whereas the percentages with 2 or fewer weekly contacts with relatives and friends were similar (30% vs. 34%).
Table 1.
Comparison of social relationships in individuals with cirrhosis and comparators participating in the Danish National Health Surveys 2010, 2013, or 2017.
| Prevalence (%) | Cirrhosis | Comparators∗ |
|---|---|---|
| Number | 541 | 2,157 |
| Cirrhosis aetiology | ||
| Alcohol | 376 (70) | — |
| Other | 165 (30) | — |
| Men | 347 (64) | 1,359 (63) |
| Age, median (IQR) | 62 (55–68) | 62 (56–69) |
| Low level of education, ≤10 years |
235 (43) |
903 (42) |
| Functional aspects of social relationships | ||
| Social support | ||
| Low social support | 122 (22) | 293 (13) |
| Medium or high social support | 419 (78) | 1,864 (87) |
| Loneliness | ||
| Loneliness | 192 (35) | 431 (20) |
| No loneliness |
349 (65) |
1,726 (80) |
| Structural aspects of social relationships | ||
| Cohabitation status | ||
| Living alone | 262 (48) | 478 (22) |
| Cohabitation | 279 (52) | 1,679 (78) |
| Contact with relatives and friends∗ | ||
| ≤2 times per week | 163 (30) | 722 (34) |
| ≥3 times per week | 346 (64) | 1,325 (61) |
| Missing data | 32 (6) | 110 (5) |
Comparators were matched on age, birth year, sex, and educational level.
Defined as contact by phone, writing, or physical contact with relatives and friends that one is not living with.
Individuals with cirrhosis
Clinical characteristics according to social relationships
Individuals with cirrhosis with weak social relationships were more often current alcohol drinkers and smokers than individuals with stronger social relationships, and they were less likely to have a history of decompensated cirrhosis. This pattern was seen for the functional aspects, social support (Table 2) and loneliness (Table S5), and it was seen for one indicator of the structural aspects, cohabitation status (Table S6). The other structural aspect, frequency of contacts with relatives and friends (Table S7), did not correlate with clinical characteristics.
Table 2.
Characteristics according to social support (a functional aspect of social relationships) in individuals with cirrhosis (n = 541) participating in the Danish National Health Surveys 2010, 2013, or 2017.
| Low social support | Medium or high social support | |
|---|---|---|
| Number |
122 |
419 |
| Other aspects of social relationships | ||
| Loneliness (functional aspect) | 73 (60) | 119 (28) |
| Living alone (structural aspect) | 70 (57) | 192 (46) |
| Contacts with relatives and friends ≤2 per week (structural aspect)∗ |
60 (53) |
103 (26) |
| Demographic and clinical characteristics | ||
| Men | 77 (63) | 270 (64) |
| Age, median (IQR) | 61 (54–68) | 62 (55–68) |
| Low level of education | 58 (48) | 177 (42) |
| History of decompensation | 50 (41) | 207 (49) |
| ≥5 years since cirrhosis diagnosis | 37 (30) | 137 (33) |
| Current alcohol drinkers | 82 (67) | 227 (54) |
| Alcohol amount in drinkers, median drinks per week (IQR) | 15 (6–41) | 12 (5–30) |
| Smoker | 66 (54) | 193 (46) |
| Charlson Comorbidity Index = 0 | 57 (47) | 207 (49) |
| Charlson Comorbidity Index = 1 | 33 (27) | 95 (23) |
| Charlson Comorbidity Index ≥2 | 32 (26) | 117 (28) |
| Physical health-related quality of life SF-12, median (IQR)† | 35 (28–47) | 37 (28–48) |
| Mental health-related quality SF-12, median (IQR)† | 41 (31–52) | 48 (39–57) |
Defined as contact by phone, writing, or physical with relatives and friends. Values on frequency of contacts with relatives and friends were missing in 32 individuals.
Higher scores indicate better health; data for physical and mental SF-12 was missing in 112 individuals. SF-12, Short Form-12.
Health-related quality of life according to social relationships
Adjusted logistic regression showed that individuals with cirrhosis with weak social relationships had a lower mental HRQoL than individuals with stronger social relationships, however, there was no difference for those living alone vs. cohabitating (Table 3 and Fig. 1). For example, individuals with cirrhosis with low social support had a 5.1-point (95% CI 2.6–8.0), p <0.001, lower mental HRQoL score than individuals with cirrhosis with medium or high social support. Loneliness and low frequency of contact with relatives and friends were associated with lower physical HRQoL, but social support and cohabitation status were not.
Table 3.
Associations of HRQoL∗with aspects of social relationships in individuals with cirrhosis (n = 429) who participated in the Danish National Health Surveys 2010, 2013, or 2017.
| Physical HRQoL |
Mental HRQoL |
|||
|---|---|---|---|---|
| Point difference in HRQoL score (95% CI) | p value | Point difference in HRQoL score (95% CI) | p value | |
| Functional aspects of social relationships | ||||
| Social support, low vs. medium or high | -1.6 (-4.4-1.2) | 0.26 | -5.1 (-8.0−2.6) | <0.001 |
| Loneliness, yes vs. no | -3.4 (5.9−0.95) | 0.007 | -9.3 (-11−6.8) | <0.001 |
| Structural aspects of social relationships | ||||
| Living alone vs. cohabitation | -0.62 (-3.0-1.8) | 0.61 | -0.54 (-3.0-1.9) | 0.66 |
| Contact with relatives and friends per week, ≤2 times vs. ≥3 times per week | -2.6 (-0.02−5.1) | 0.05 | -3.9 (-1.3−6.5) | 0.003 |
HRQoL, health-related quality of life. Linear regression was conducted for each aspect of social relationships separately and adjusted for age, sex, history of decompensation, comorbidity, smoking, alcohol consumption, and time since cirrhosis diagnosis.
HRQoL was measured with the Short Form-12, which is rated 1–100 with higher scores indicating better health. For instance, the negative values indicate that HRQoL was lower in those with loneliness than in those without loneliness. Data for physical and mental Short Form-12 was missing in 112 individuals.
Fig. 1.
Box plots of physical and mental health-related quality of life (HRQoL)∗ according to aspects of social relationships in individuals with cirrhosis (n = 429) who participated in the Danish National Health Surveys 2010, 2013, or 2017.
(A) Physical HRQoL; (B) mental HRQoL. ∗HRQoL was measured with the Short Form-12 (SF-12), which is rated 1–100 with higher scores indicate better health; data for physical and mental SF-12 was missing in 112 individuals.
Functional aspects of social relationships and risk of all-cause mortality
Individuals with cirrhosis were followed for 2,795 person-years during which 269 individuals died. Lower social support was associated with higher mortality risk in individuals with cirrhosis with a 5-year mortality risk of 52% (95% CI 44–62) for low and 38% (95% CI 33–43) for moderate-to-high social support (Fig. 2A). The adjusted hazard ratio (HR) for risk of mortality was 1.4 (95% CI 1.1–1.9), p=0.011, for low social support compared with moderate or high social support (Table 4). A similar association was found for loneliness and risk of mortality (Fig. 2B and Table 4).
Fig. 2.
Mortality risk according to aspects of social relationships in individuals with cirrhosis (n = 541) who participated in the Danish National Health Surveys 2010, 2013, or 2017.
(A) Social support; (B) loneliness; (C) cohabitation status; (D) frequency of contacts with relatives and friends.
Table 4.
HRs and 95% CIs of all-cause mortality according to aspects of social relationships in individuals with cirrhosis (n = 541) who participated in the Danish National Health Surveys 2010, 2013, and 2017.
| No. of deaths (person-years) | Mortality rate per 100 person-years | Crude analysis |
Adjusted analysis∗ |
|||
|---|---|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | |||
| Functional aspects of social relationships | ||||||
| Social support | ||||||
| Low social support | 74 (585) | 13 | ||||
| Medium or high social support | 195 (2,210) | 8.8 | ||||
| Social support, low vs. medium or high | 1.5 (1.1–1.9) | 0.005 | 1.4 (1.1–1.9) | 0.011 | ||
| Loneliness | ||||||
| Loneliness | 109 (908) | 12 | ||||
| No loneliness | 160 (1,888) | 8.5 | ||||
| Loneliness, yes vs. no |
1.4 (1.1–1.8) |
0.004 |
1.5 (1.2–1.9) |
0.003 |
||
| Structural aspects of social relationships | ||||||
| Cohabitation status | ||||||
| Living alone | 132 (1,354) | 9.7 | ||||
| Cohabitating | 137 (1,442) | 9.5 | ||||
| Living alone vs. cohabitating | 1.0 (0.81–1.3) | 0.86 | 1.0 (0.82–1.3) | 0.85 | ||
| Contact with relatives and friends | ||||||
| ≤2 times per week | 84 (806) | 10 | ||||
| ≥3 times per week | 161 (1,819) | 8.9 | ||||
| ≤2 times vs. ≥3 times per week |
1.2 (0.91–1.5) |
0.21 |
1.0 (0.8–1.4) |
0.74 |
||
| HR of adjusting variables | ||||||
| Age, per 10-year increase | 1.4 (1.2–1.6) | <0.001 | ||||
| Men vs. women | 1.3 (1.0–1.7) | 0.07 | ||||
| Decompensation history, yes vs. no | 1.3 (1.0–1.7) | 0.01 | ||||
| Years since cirrhosis diagnosis | 0.9 (0.9–1.0) | 0.002 | ||||
| Charlson Comorbidity Index, 1 vs. 0 | 1.4 (1.0–1.9) | 0.04 | ||||
| Charlson Comorbidity Index, ≥2 vs. 0 | 1.5 (1.1–2.0) | 0.009 | ||||
| Alcohol, drinking 1–20 drinks/week vs. abstaining | 1.1 (0.8–1.4) | 0.54 | ||||
| Alcohol, drinking ≥21 drinks/week vs. abstaining | 1.4 (1.0–1.9) | 0.02 | ||||
| Smoking, yes vs. no | 1.1 (0.8–1.4) | 0.65 | ||||
HR, hazard ratio. Analyses were conducted for each aspect of social relationships separately.
Analyses were adjusted for age, sex, history of decompensation, comorbidity, smoking, alcohol consumption and time since cirrhosis diagnosis.
Structural aspects of social relationships and risk of all-cause mortality
Neither cohabitation status nor frequency of contacts with relatives and friends were associated with risk of mortality in cirrhosis (Table 4 and Fig. 2C and D). For example, the 5-year mortality risk according to frequency of contacts with relatives and friends was 46% (95% CI 39–55) for 2 or fewer weekly contacts and 39% (95% CI 34–45) for 3 or more (Fig. 2D) and the 10-year mortality risk according to frequency of contacts with relatives and friends was 67% (95% CI 58–76) for 2 or fewer weekly contacts and 63% (95% CI 56–69) for 3 or more, with an adjusted HR over the entire follow-up period of 1.0 (95% CI 0.8–1.4), p = 0.74 (Table 4).
Risk of mortality in subgroups and analyses of other outcomes
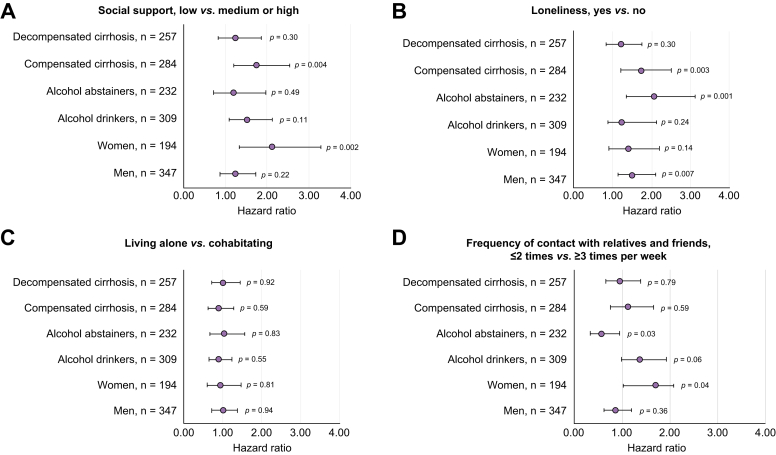
Functional aspects of social relationships were more strongly associated with risk of mortality among individuals with compensated cirrhosis than among individuals with decompensated cirrhosis (Fig. 3 and Table S8). In addition, some aspects (social support and frequency of contact with relatives and friends) were more strongly associated with risk of mortality among women than among men. Finally, cohabitation status did not affect risk of mortality in any subgroup.
Fig. 3.
Mortality risk according to aspects of social relationships in subgroups (men, women, alcohol drinkers, alcohol abstainers, decompensated and compensated cirrhosis) of individuals with cirrhosis (n = 541) who participated in the Danish National Health Surveys 2010, 2013, or 2017.
(A) Social support; (B) loneliness; (C) cohabitation status; (D) frequency of contacts with relatives and friends.
Low social support increased the risk of the combined endpoint of decompensation or mortality (HR 1.5 [95% CI 1.1–1.9], p = 0.007) and tended to increase the risk of a liver-related death (HR 1.4 [95% CI 0.95–2.0], p = 0.09), but not of acute admission (HR 1.2 [95% CI 0.93–1.5], p = 0.14) (Table S9). Loneliness was associated with increased risk of acute admission and with the combined endpoint of decompensation or mortality and tended to be associated with a liver-related death. The structural aspects of social relationships (cohabitation status and frequency of contact with relatives and friends) were not associated with these outcomes.
Comparators
Risk of mortality in comparators
Comparators were followed for 14,978 person-years during which 237 of 2,175 comparators died. For the functional aspects, loneliness and not social support was associated with increased risk of mortality in comparators (Table S10) and this contrasted the findings in individuals with cirrhosis where both social support and loneliness were associated with risk of mortality. For the structural aspects, living alone and not frequency of contact with family and friends were associated with increased risk of mortality in comparators. In contrast, we found a lack of an association of cohabitation status with mortality in individuals with cirrhosis.
Discussion
This study showed that individuals with cirrhosis were more likely to have weak functional social relationships (low social support or loneliness) and to live alone than a matched comparison cohort, whereas the frequency of contacts with relatives and friends was similar. Except for living alone, weak social relationships were associated with lower mental HRQoL in individuals with cirrhosis whereas physical HRQoL was only marginally associated. Individuals with cirrhosis who had low social support had a higher mortality than those who had moderate or high social support. The same pattern was seen for loneliness, whereas cohabitation status and frequency of contacts with relatives and friends did not influence risk of mortality in individuals with cirrhosis.
This is the first study to compare functional and structural aspects of social relationships among individuals with cirrhosis with a matched comparison cohort and prospectively assess their influence on mortality in cirrhosis. Except for frequency of contacts with family and friends, the measures of social relationships that we used have consistently been associated with mental HRQoL and mortality both in the general population2,30,33 and in individuals with heavy drinking or chronic medical illness.5,11,13 The percentage of individuals with cirrhosis in our study with low social support is comparable with findings from a United States study of hepatitis C patients (22% vs. 27%).9
Our results may be affected by selection bias, leading to underestimation of the true proportions of individuals with cirrhosis suffering from low social support, loneliness, and living alone. This bias results from non-participation in health surveys, which is more common in vulnerable individuals including those who live alone or are homeless.20 Their non-participation may lead to an underrepresentation of individuals with cirrhosis with such characteristics20 In fact, we have previously shown that individuals with alcohol-related liver disease who live alone were underrepresented in the DNHS (61% in the registry-based cohort with full coverage vs. 50% in the DNHS cohort).34 Apart from this non-participation bias, participants in the DNHS were representative of all individuals in Denmark with alcohol-related liver disease regarding disease severity and sociodemographic characteristics. Because low social support and loneliness are more frequent in individuals who live alone[7], [8], [9] (Table S4), we find it likely that we underestimated the true prevalence of weak social relationships in individuals with cirrhosis in this study. For example, the true prevalence of loneliness among individuals with cirrhosis could be even higher than the 35% reported here.
The absence of an association between cohabitation status and mortality in individuals with cirrhosis may partly be explained by the underrepresentation of vulnerable individuals who live alone. Moreover, there is evidence that cohabitation status is less important for survival in cirrhosis than in the general population, which we also observed in the present study. For example, in registry-based studies, the influence on mortality of living alone vs. being married was weaker in individuals with cirrhosis (relative risk of 1.2 [95% CI 1.0–1.4]) than in the general Danish population (relative risk of 1.7 [95% CI 1.6–1.8]).35,36 This difference in the influence of marriage on mortality might be explained by the social relationships of individuals with cirrhosis being less supportive or even negative, as reported for individuals with alcohol problems in general11,12 – an interpretation backed up by our finding that individuals with cirrhosis who were cohabitating were more likely than comparators who were cohabitating to report loneliness (25% vs. 13%) (Table S4). A similar explanation of less supportive relationships may account for the absence of an association between frequency of social contacts and mortality in cirrhosis.
The higher prevalence of weak functional relationships in individuals with cirrhosis than comparators found in this study might be ascribed to the influence of poorer physical health in cirrhosis leading to social isolation, that is, reverse causation bias. Lack of detailed clinical and laboratory data is a limitation of this study. Physical HRQoL did correlate with level of loneliness but not with social support, and social support is less affected by physical health than loneliness might be.37 Thus, we think reverse causation bias could not explain the higher prevalence of weak functional relationships in cirrhosis: it is more likely that social isolation precedes a poor physical health.38
It was somewhat surprising that we did not find an association of social support with mortality risk in comparators in contrast to the finding of a higher risk of mortality for low social support in individuals with cirrhosis. However, we believe this is best explained by an underpowered analysis and the fact that 64% of comparators were men: social support may have stronger influence on survival in women, whereas loneliness has a stronger influence on survival in men, similar to our results for women and men with cirrhosis in the subgroup analysis (Fig. 3).39,40
Social relationships are thought to affect survival through behavioural, psychological, and biological mechanisms.1 First, behaviourally, individuals with weak social relationships are more likely to be heavy drinkers, smokers, eating a poor diet, and be non-compliant with medical regimens,1,15,41 and indeed we observed a higher alcohol consumption in individuals with cirrhosis with low social support and loneliness. Heavy drinking may contribute to the association of low social support and loneliness with increased mortality risk in individuals with cirrhosis.11 Although we did adjust the analyses for alcohol consumption at baseline, it is a limitation of our study that we did not have information on alcohol consumption during follow-up. The absence of an association of low social support with decompensation that we found may reflect a lower likelihood of attendance to outpatient clinics with decompensation symptoms, but it may also indicate that low social support increases mortality risk through other pathways than progression in liver disease. Second, psychologically, low social support increases stress and depression, both of which increase mortality in the general population42 and in individuals with cirrhosis.43 In fact, social support is thought to have a greater capacity to reduce mortality in stressful circumstances – such as living with cirrhosis.44 Third, biologically, research points to negative effects of low social support and loneliness on the immune and neuroendocrine systems by affecting the hypothalamic–pituitary–adrenal axis.45 For example, individuals with low social support have fewer immune cells and are more susceptible to infections.44,46 Individuals with cirrhosis may be particularly vulnerable to these effects because of their compromised immune system.47
Implications
We hope that these results will make healthcare providers aware of the functional aspects of the social relationships of their individuals with cirrhosis, in addition to the traditional clinical management of decompensation symptoms, comorbidity, and health-risk behaviours. Randomised trials have shown a positive effect of community-health worker intervention on social support and hospitalisation rates in individuals with chronic disease.16,17 Patient support groups could also be beneficial, particularly if other social relations fail to provide true social support.48 Further research is needed to study how social relations may affect survival in cirrhosis and to understand the relation between low social support and the stigmatisation that many individuals with cirrhosis suffer from.49 At the population-level, interventions are needed to target the negative perception of liver disease. We hope that our findings could inspire randomised trials of interventions to strengthen the social support of individuals with cirrhosis.50
Financial support
GA and PJ were supported by a grant from the Novo Nordisk Foundation (NNF18OC0054612). The funding organisation was not involved in the design and conduct of the study, or in the decision to submit the manuscript for publication.
Authors’ contributions
Contributed to the design of the study: all authors. Analysed the data: GA, MWJ. Wrote the first draft of the manuscript: GA. Contributed to critically revising the paper: all authors.
Data availability statement
Due to its proprietary nature, supporting data of the study cannot be made openly available. Further information about the data and conditions for access are available here (link: https://www.danskernessundhed.dk/Dataudlevering.html).
Conflicts of interest
CJL holds shares in Novo Nordisk. All other authors report no financial support. The authors report no other conflicts of interest in this work.
Please refer to the accompanying ICMJE disclosure forms for further details.
Acknowledgements
The Danish National Health Survey was funded by The Capital Region, Region Zealand, The South Denmark Region, The Central Denmark Region, The North Denmark Region, Ministry of Health and the National Institute of Public Health, University of Southern Denmark.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhepr.2022.100600.
Supplementary data
The following are the supplementary data to this article:
References
- 1.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elovainio M., Hakulinen C., Pulkki-Råback L., Virtanen M., Josefsson K., Jokela M., et al. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Public Health. 2017;2:e260–e266. doi: 10.1016/S2468-2667(17)30075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomaka J., Thompson S., Palacios R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J Aging Health. 2006;18:359–384. doi: 10.1177/0898264305280993. [DOI] [PubMed] [Google Scholar]
- 5.Ong A.D., Uchino B.N., Wethington E. Loneliness and health in older adults: a mini-review and synthesis. Gerontology. 2016;62:443–449. doi: 10.1159/000441651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinhardt J.P., Boerner K., Horowitz A. Good to have but not to use: differential impact of perceived and received support on well-being. J Soc Pers Relat. 2006;23:117–129. [Google Scholar]
- 7.Algren M.H., Ekholm O., Nielsen L., Ersbøll A.K., Bak C.K., Andersen P.T. Social isolation, loneliness, socioeconomic status, and health-risk behaviour in deprived neighbourhoods in Denmark: a cross-sectional study. SSM Popul Health. 2020;10 doi: 10.1016/j.ssmph.2020.100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christensen A.V., Juel K., Ekholm O., Thrysøe L., Thorup C.B., Borregaard B., et al. Significantly increased risk of all-cause mortality among cardiac patients feeling lonely. Heart. 2020;106:140–146. doi: 10.1136/heartjnl-2019-315460. [DOI] [PubMed] [Google Scholar]
- 9.Blasiole J.A., Shinkunas L., LaBrecque D.R., Arnold R.M., Zickmund S.L. Mental and physical symptoms associated with lower social support for patients with hepatitis C. World J Gastroenterol. 2006;12:4665–4672. doi: 10.3748/wjg.v12.i27.4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fialla A.D., de Muckadell O.B.S., Touborg Lassen A. Incidence, etiology and mortality of cirrhosis: a population-based cohort study. Scand J Gastroenterol. 2012;47:702–709. doi: 10.3109/00365521.2012.661759. [DOI] [PubMed] [Google Scholar]
- 11.Åkerlind I., Hörnquist J.O. Loneliness and alcohol abuse: a review of evidences of an interplay. Soc Sci Med. 1992;34:405–414. doi: 10.1016/0277-9536(92)90300-f. [DOI] [PubMed] [Google Scholar]
- 12.Holst C., Tolstrup J.S., Sørensen H.J., Becker U. Family structure and alcohol use disorder: a register-based cohort study among offspring with and without parental alcohol use disorder 2019. Addiction. 2020;115:1440–1449. doi: 10.1111/add.14932. [DOI] [PubMed] [Google Scholar]
- 13.Joutsenniemi K., Martelin T., Kestilä L., Martikainen P., Pirkola S., Koskinen S. Living arrangements, heavy drinking and alcohol dependence. Alcohol Alcohol. 2007;42:480–491. doi: 10.1093/alcalc/agm011. [DOI] [PubMed] [Google Scholar]
- 14.Stafford M., von Wagner C., Perman S., Taylor J., Kuh D., Sheringham J. Social connectedness and engagement in preventive health services: an analysis of data from a prospective cohort study. Lancet Public Health. 2018;3:e438–e446. doi: 10.1016/S2468-2667(18)30141-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiMatteo M.R. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 16.Kangovi S., Mitra N., Norton L., Harte R., Zhao X., Carter T., et al. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: a randomized clinical trial. JAMA Intern Med. 2018;178:1635–1643. doi: 10.1001/jamainternmed.2018.4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X., Wang B., Tan D., Li M., Zhang D., Tang C., et al. Effectiveness of comprehensive social support interventions among elderly patients with tuberculosis in communities in China: a community-based trial. J Epidemiol Community Health. 2018;72:369–375. doi: 10.1136/jech-2017-209458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clayton C., Motley C., Sakakibara B. Enhancing social support among people with cardiovascular disease: a systematic scoping review. Curr Cardiol Rep. 2019;21:1–14. doi: 10.1007/s11886-019-1216-7. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt M., Pedersen L., Sørensen H.T. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 20.Christensen A.I., Lau C.J., Kristensen P.L., Johnsen S.B., Wingstrand A., Friis K., et al. The Danish National Health Survey: study design, response rate and respondent characteristics in 2010, 2013 and 2017. Scand J Public Health. 2022;50:180–188. doi: 10.1177/1403494820966534. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt M., Schmidt S.A.J., Sandegaard J.L., Ehrenstein V., Pedersen L., Sørensen H.T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Franchis R. Expanding consensus in portal hypertension Report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743–752. doi: 10.1016/j.jhep.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Sundhedsstyrelsen. Danskernes Sundhed – Den Nationale Sundhedsprofil 2017. https://www.sst.dk/da/udgivelser/2018/danskernes-sundhed-den-nationale-sundhedsprofil-2017.
- 24.Jensen V.M., Rasmussen A.W. Danish education registers. Scand J Public Health. 2011;39:91–94. doi: 10.1177/1403494810394715. [DOI] [PubMed] [Google Scholar]
- 25.Schneider S.L. The international standard classification of education 2011. Comp Soc Res. 2013 doi: 10.1108/S0195-6310(2013)0000030017. [DOI] [Google Scholar]
- 26.Lasgaard M., Friis K., Shevlin M. “Where are all the lonely people?” A population-based study of high-risk groups across the life span. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1373–1384. doi: 10.1007/s00127-016-1279-3. [DOI] [PubMed] [Google Scholar]
- 27.Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen S., Mermelstein R., Kamarck T., Hoberman H.M. Springer Netherlands; Dordrecht: 1985. Measuring the functional components of social support. Social support: theory, research and applications; pp. 73–94. [Google Scholar]
- 29.Erlangsen A., Fedyszyn I. Danish nationwide registers for public health and health-related research. Scand J Public Health. 2015;43:333–339. doi: 10.1177/1403494815575193. [DOI] [PubMed] [Google Scholar]
- 30.Laugesen K., Baggesen L.M., Schmidt S.A.J., Glymour M.M., Lasgaard M., Milstein A., et al. Social isolation and all-cause mortality: a population-based cohort study in Denmark. Sci Rep. 2018;8:4–11. doi: 10.1038/s41598-018-22963-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gandek B., Ware J.E., Aaronson N.K., Apolone G., Bjorner J.B., Brazier J.E., et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 32.Quan H., Li B., Couris C.M., Fushimi K., Graham P., Hider P., et al. Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 33.Pinquart M., Duberstein P. Associations of social networks with cancer mortality: a meta- analysis. Crit Rev Oncol Hematol. 2010;75:122–137. doi: 10.1016/j.critrevonc.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kann A.E., Jepsen P., Madsen L., Crooks C., Fleming K., Christensen A.I., et al. Motivation to reduce drinking and engagement in alcohol misuse treatment in alcohol-related liver disease: a national health survey. Am J Gastroenterol. 2022;117:918–922. doi: 10.14309/ajg.0000000000001616. [DOI] [PubMed] [Google Scholar]
- 35.Jepsen P., Vilstrup H., Andersen P.K., Sørensen H.T. Socioeconomic status and survival of cirrhosis patients: a Danish nationwide cohort study. BMC Gastroenterol. 2009;9:35. doi: 10.1186/1471-230X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frisch M., Simonsen J. Marriage, cohabitation and mortality in Denmark: national cohort study of 6.5 million persons followed for up to three decades (1982–2011) Int J Epidemiol. 2013;42:559–578. doi: 10.1093/ije/dyt024. [DOI] [PubMed] [Google Scholar]
- 37.Gallant M.P. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;30:170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- 38.Herttua K., Martikainen P., Vahtera J., Kivimäki M. Living alone and alcohol-related mortality: a population-based cohort study from Finland. PLoS Med. 2011;8 doi: 10.1371/journal.pmed.1001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rico-Uribe L.A., Caballero F.F., Martín-María N., Cabello M., Ayuso-Mateos J.L., Miret M. Association of loneliness with all-cause mortality: a meta-analysis. PLoS One. 2018;13 doi: 10.1371/journal.pone.0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lyyra T.-M., Heikkinen R.-L. Perceived social support and mortality in older people. J Gerontol B Psychol Sci Soc Sci. 2006;61:S147–S152. doi: 10.1093/geronb/61.3.s147. [DOI] [PubMed] [Google Scholar]
- 41.Richard A., Rohrmann S., Vandeleur C.L., Schmid M., Barth J., Eichholzer M. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One. 2017;12:1–18. doi: 10.1371/journal.pone.0181442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puterman E., Weiss J., Hives B.A., Gemmill A., Karasek D., Mendes W.B., et al. Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proc Natl Acad Sci U S A. 2020;117:16273–16282. doi: 10.1073/pnas.1918455117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Russ T.C., Kivimäki M., Morling J.R., Starr J.M., Stamatakis E., Batty G.D. Association between psychological distress and liver disease mortality: a meta-analysis of individual study participants. Gastroenterology. 2015;148:958–966.e4. doi: 10.1053/j.gastro.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Uchino B.N. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 45.Vere C.C., Teodor-Streba C., Streba L.M., Ionescu A.G., Sima F. Psychosocial stress and liver disease status. World J Gastroenterol. 2009;15:2980–2986. doi: 10.3748/wjg.15.2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whisman M.A. Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychol. 2010;29:550–554. doi: 10.1037/a0020760. [DOI] [PubMed] [Google Scholar]
- 47.Bonnel A.R., Bunchorntavakul C., Reddy K.R. Immune dysfunction and infections in patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9:727–738. doi: 10.1016/j.cgh.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 48.Ordin Y.S., Karayurt Ö. Effects of a support group intervention on physical, psychological, and social adaptation of liver transplant recipients. Exp Clin Transpl. 2016;14:329–337. doi: 10.6002/ect.2014.0220. [DOI] [PubMed] [Google Scholar]
- 49.Vaughn-Sandler V., Sherman C., Aronsohn A., Volk M.L. Consequences of perceived stigma among patients with cirrhosis. Dig Dis Sci. 2014;59:681–686. doi: 10.1007/s10620-013-2942-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Valery P.C., Powell E., Moses N., Volk M.L., McPhail S.M., Clark P.J., et al. Systematic review: unmet supportive care needs in people diagnosed with chronic liver disease. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-007451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to its proprietary nature, supporting data of the study cannot be made openly available. Further information about the data and conditions for access are available here (link: https://www.danskernessundhed.dk/Dataudlevering.html).