Abstract
Objective
Most young autistic children display emotional and behavioral problems (EBPs). There is evidence that behavioral parenting interventions (BPIs) reduce these. The COVID-19 pandemic and associated lockdowns can be seen as a natural experiment to test the longer-term effect of BPIs under conditions of increased uncertainty.
Method
Opportunistic follow-up (n = 49) of a pilot randomized controlled trial (RCT) cohort (n = 62 autistic children aged 6-11 years; originally randomized to a 12-week group BPI [Predictive Parenting; n = 31] or an attention control [Psychoeducation; n = 31]) was conducted during COVID-19−related lockdowns. Measures of parent-reported child irritability and parenting stress were collected at 3 time points (baseline: mean age = 6.7 years; primary endpoint: mean age = 7.1 years, ∼5 months after randomization; and COVID-19 follow-up: mean age = 8.8 years, ∼2 years after randomization). We tested the magnitude of intervention effects using point estimates of differences in child irritability and parenting stress between arms at primary endpoint and COVID-19 follow-up, covarying for baseline scores. We used area under the curve (AUC) analyses to obtain overall estimates of the average intervention effect across all 3 timepoints. Semi-structured qualitative interviews were conducted with a subsample of parents (n = 18).
Results
A small but significant intervention effect was found from baseline to COVID-19 follow-up in favor of Predictive Parenting on parent-reported child irritability (d = −0.33, 95% CI = −0.65, −0.01) and parenting stress (d = −0.31, 95% CI = −0.59, −0.03). No overall mean intervention effect for these measures as estimated by the AUC analyses (which takes into account the nonsignificant effect at primary endpoint) was found. Interview feedback on the both interventions was positive, and parents reported using strategies from Predictive Parenting during COVID-19−related restrictions.
Conclusion
This opportunistic follow-up study at a time of stress indicates the need for careful consideration of how and when to measure the effects of BPIs in autistic child populations. Future trials should consider both the most appropriate endpoint and in what context effects may be more likely to be seen.
Clinical trial registration information
Autism Spectrum Treatment and Resilience (ASTAR); https://www.isrctn.com; 91411078.
Key words: autism, emotional and behavioral problems, intervention, RCT, follow-up
Autism is a spectrum condition characterized by impairments in social communication and interaction, and the presence of restricted and repetitive behaviors and sensory sensitivities.1 We use the terms “autism” to refer to autism spectrum disorder (ASD; DSM-5) and “autistic children” through this article, as this is preferred terminology by some of the autism community.2 Additional emotional and behavioral problems (EBPs) frequently co-occur at rates much higher than in the general population.3 , 4 These co-occurring EBPs are associated with greater parental stress and poorer well-being.5 Behavioral parenting interventions (BPIs) are well-established approaches for improving behavioral problems in non-autistic children.6 Meta-analysis of randomized controlled trials (RCTs) of BPIs have demonstrated moderate effects on disruptive child behavior in young autistic children and some evidence for reductions in child hyperactivity and parental stress.7 , 8
Although targeting developmental abilities rather than co-occurring problems, RCTs in autistic populations have highlighted the importance of conducting longer-term follow-ups because intervention effects that are nonsignificant at end of trial may be significant later on.9 This could be because intervention effects may take longer for benefits in child presentations to appear. Evidence is mixed as to whether effects of BPIs are reduced, sustained, or amplified in non-autistic child populations over time.10, 11, 12 However, in the Research Units in Behavioral Intervention (RUBI) trial of an individually delivered BPI targeting EBPs in autistic children, divergence from the psychoeducation control arm increased in the 2 months after the core 16-week intervention (although it should be noted that up to 3 booster sessions were offered between 16 and 24 weeks).13
In the current study, we conducted an opportunistic follow-up of an existing cohort during COVID-19−related restrictions and explored whether a pilot RCT of a novel group-based BPI, which did not show significant effects at primary endpoint but had promising feasibility and acceptability data,14 showed any evidence of effect later on. The COVID-19 pandemic and its associated consequences (eg, lockdowns, school closures, changing public health guidance) brought uncertainty about all aspects of daily life and the requirement to adapt routines. This is particularly challenging for autistic populations, as difficulties tolerating uncertainty are common and have been linked to mental health difficulties,15 , 16 and there is strong evidence that restrictions were associated with increased child mental health problems.17 Given our Predictive Parenting BPI aimed to enhance parental skills to predict behavior more effectively, to make life more predictable, and to help children cope with unpredictability,18 we believed that the context of the follow-up may have provided conditions to see whether strategies learned during Predictive Parenting would endure during periods of increased unpredictability. There is also a possibility that the intervention could act as a buffer to the additional environmental stressors.
Method
Sample and Procedure
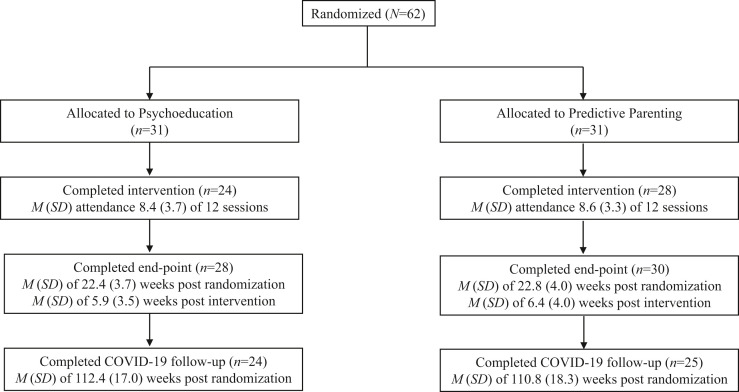
The sample included young autistic children whose parents participated in the Autism Spectrum Treatment and Resilience (ASTAR) pilot RCT as part of the Improving Autism Mental Health program (IAMHealth). ASTAR was a parallel 2-group, 2-site pilot RCT that compared Predictive Parenting to a Psychoeducation attention control (Trial registration: ISRCTN91411078). Parents of 62 children were recruited between November 2017 and October 2018 and randomized to Predictive Parenting (n = 31) or Psychoeducation (n = 31). Because intervention arm composition and content were adapted based on child verbal language (minimally verbal vs verbal), randomization was stratified by verbal ability as well as site (n = 2). Randomization was conducted on blocks of 10 to 18 families on a ratio of 1:1, resulting in groups of 5 to 9 families in each intervention arm for any block. Baseline measures were collected up to 2 months prior to the planned randomization date and primary endpoint measures at approximately 18 to 24 weeks after randomization, once the 12-week intervention finished. Further details on the procedure of the original study can be found in Charman et al. 14 and Palmer et al. 19 Ethical approval for the original pilot RCT was granted from NHS Camden and Kings Cross Research Ethics Committee (16/LO/1769). Parents and, when possible, children gave written informed consent/assent. Figure 1 provides a CONSORT flow diagram. Sample characteristics are given in Table 1 .
Figure 1.
CONSORT Flow Diagram
Table 1.
Sample Characteristics by Intervention Arm
| Psychoeducation (n = 31) | Predictive parenting (n = 31) | |
|---|---|---|
| Baseline characteristics | ||
| Age, y, mean (SD), range | 6.8 (1.1), 4.4-8.3 | 6.5 (1.2), 4.4-8.8 |
| Sex, male, n (%) | 25 (81) | 25 (81) |
| Ethnicity, White, n (%) | 17 (55) | 16 (52) |
| School type,a n (%) | ||
| Mainstream | 20 (65) | 20 (65) |
| Special education | 11 (35) | 11 (35) |
| ADOS–2 CSS, mean (SD), range | 7.71 (1.40), 4-10 | 7.29 (2.35), 1-10 |
| SCQ-L, mean (SD), range | 21.74 (6.63), 9-33 | 25.13 (6.58), 12-37 |
| ABAS–3 GAC, mean (SD), range | 61.45 (12.63), 45-85 | 61.90 (12.98). 46-100 |
| Parental education | ||
| At least 1 parent with A-levels or above, n (%) | 27 (87) | 27 (87) |
| Parental employment prior to pandemic | ||
| At least 1 parent employed, n (%) | 25 (81) | 27 (87) |
| Psychoeducation (n = 24) | Predictive Parenting (n = 25) | |
|---|---|---|
| COVID-19 follow-up characteristics | ||
| Age, y, mean (SD), range | 9.0 (1.30), 6.3-10.8 | 8.6 (1.40), 6.4-11.2 |
| Exposure to COVID-19 | ||
| Positive test in immediate family, n (%) | 1 (4.2) | 1 (4.0) |
| Child suspected, not tested or negative, n (%) | 1 (4.2) | 1 (4.0) |
| Death in the wider family as a result of COVID-19, n (%) | 0 (0.0) | 1 (4.0) |
| Parental employment during pandemic | ||
| At least 1 parent furloughed due to COVID-19, n (%) | 4 (12.9) | 2 (6.5) |
| At least 1 parent dismissed due to COVID-19, n (%) | 1 (3.2) | 3 (9.7) |
| At least 1 parent working more hours than usual, n (%) | 4 (12.9) | 5 (16.1) |
| At least 1 parent working fewer hours than usual, n (%) | 1 (3.2) | 4 (12.9) |
| Level of financial concern,b mean (SD), range | 2.00 (0.93), 1-5 | 2.28 (0.84), 1-5 |
| Child access to education | ||
| Child physical attendance at school at least on some days, n (%) | 15 (62.5) | 10 (40.0) |
| Home environment | ||
| Have access to personal garden/outside space, n (%) | 20 (83.3) | 20 (80.0) |
| Home environment comfort,c mean (SD), range | 1.92 (0.97), 1-4 | 2.00 (1.04), 1-4 |
| COVID-19 impact risk score | 1.25, (1.33), 1-6 | 1.60, (0.96), 1-6 |
Note: ABAS–3 GAC = Adaptive Behaviour Assessment System, third edition General Adaptive Composite; ADOS–2 CSS = Autism Diagnostic Observation Schedule, second edition Calibrated Severity Score; SCQ-L = Social Communication Questionnaire–Lifetime version (all administered at baseline for sample characterization).
Specialist units in a mainstream school are included with mainstream education and specialist-only schools are separate.
Level of financial concern was measured on a 5-point scale from 1 (living comfortably) to 5 (finding it very difficult).
Home environment comfort was measured on a 4-point scale from 1 (very comfortable) to 4 (very problematic).
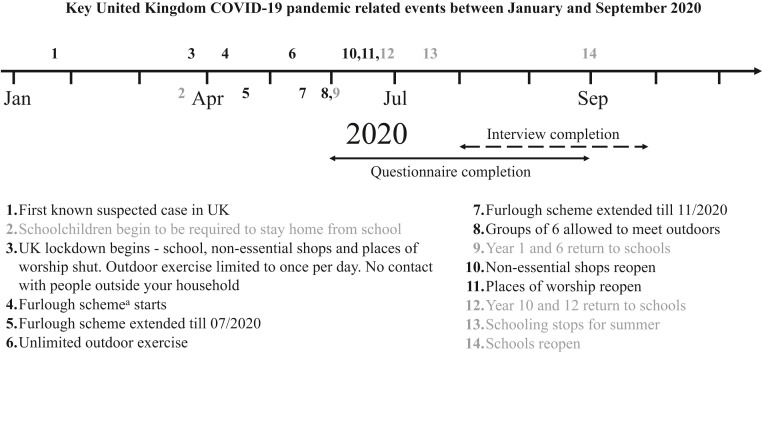
Between June and September 2020, the ASTAR cohort participants were re-contacted and asked to complete the questionnaires described below (Figure 2 provides data collection timeline and COVID-19−related events). At all time points, questionnaires were primarily administered online, although a small proportion of parents at each time point requested either paper copies or via telephone completion.
Figure 2.
Key COVID-19 Pandemic−Related Events in the United Kingdom and Data Collection Periods
Note:Events in black impact all of society. Events in gray relate to schooling.
aNon-essential businesses unable to operate due to restrictions could put staff on temporary leave and have 80% of their regular pay (capped at £2,500) covered by the government.
A subsample (18 of the 25 parents who were invited from the 41 (83.7%) who completed the questionnaires and gave consent for interview) also completed online semi-structured interviews between August and October 2020. We used purposeful sampling to ensure that we sought the views from those who reported a range of experiences during the COVID-19 pandemic on the online questionnaire. Scores on the measures described below (parent-reported child EBPs during the pandemic and parent reports of impacts of the child’s EBPs on their relationships with others) were used to classify families into 3 categories of experience, namely, positive, mixed, and negative. In addition, to increase the diversity of child and home environmental characteristics that might be relevant during pandemic-related restrictions, we sampled across two other variables: whether the child was minimally verbal or verbal, and whether or not they had a garden during lockdown. The interviews were conducted with 17 mothers and 1 father of minimally verbal (n = 9) and verbal (n = 9) children. All interviews were conducted over video-conferencing software at a time convenient for the family and were recorded and transcribed verbatim assisted by the Microsoft Teams auto-capture function. Parents were given the opportunity to review and correct transcripts prior to analysis. The follow-up study was given ethical approval from the Psychiatry, Nursing and Midwifery Research Ethics Subcommittee at King's College London (REMAS ref: 19146, ethical clearance ref: HR-19/20-19146). All parents gave written informed consent.
Interventions
Predictive Parenting consisted of 12 weekly 2-hour groups that extended parents’ understanding of autism and co-occurring EBPs and included techniques to help parents anticipate, prevent, and respond to disruptive behavior and anxiety (see Hallett et al. 18 and Palmer et al. 19 for further information). Psychoeducation also consisted of 12 weekly 2-hour group sessions providing psychoeducation and social support but no specific guidance on managing behavior.
Measures
Parent-reported child irritability was measured using the Irritability subscale of the Aberrant Behavior Checklist (ABC)20 at baseline, primary endpoint, and COVID-19 follow-up. This is a 15-item subscale widely used in populations with developmental disabilities. Items are measured on a 4-point scale, ranging from “not at all a problem” to “the problem is severe in degree,” with higher scores indicating more child irritability. Parenting stress associated with core and co-occurring autism traits was measured at baseline, primary endpoint, and COVID-19 follow-up using the Autism Parenting Stress Index (APSI).21 The APSI consists of 13 items rated on a 5-point scale ranging from “not stressful” to “so stressful we feel we can’t cope,” with higher scores indicating more parenting stress. The APSI has demonstrated good internal validity and test−retest reliability. These two measures were selected because they tapped into key parent-reported child and parent outcomes; additional measures used in the original pilot RCT were not obtained so as to minimize time burden for families (see Charman et al. 14 for further information).
At COVID-19 follow-up, the European Child & Adolescent Psychopharmacology Network (ECNP) Child and Adolescent Mental Health Services (CAMHS) COVID questionnaire was administered. This questionnaire was specifically developed by Simonoff and Coghill to assess the impacts of the COVID-19 pandemic on children and their families. It aimed to tap into a broad range of mental health problems and contextual factors pertinent to periods of restrictions. Questions from the Coronavirus Health and Impact Survey22 were used to inform the questions about mental health, which focussed on problems in the past 2 weeks. Additional questions asked about COVID-19 infection in the child, nuclear family, and wider family, and worries about becoming infected. Contextual factors included information on parental stress, family relationships, employment, and financial stress, adequacy of the home environment and educational provision. In the current study, items from this questionnaire were used to assess differences in COVID-19−related impacts. This included the items that asked about exposure to COVID-19 within the immediate and wider family in the past 2 weeks, changes to their own or partner’s (if applicable) employment situation due to COVID-19 (furloughed [nonessential businesses unable to operate because of restrictions could put staff on temporary leave and have 80% of their regular pay (capped at £2500) covered by the government], dismissed, working more or working fewer hours), concerns about finances (measured on a 5-point scale from “living comfortably” to “finding it very difficult”), child physical attendance at school (yes/no), personal access to garden or outdoor space (yes/no), and comfort of the home environment (measured on a 4-point scale, from very comfortable to very problematic). To look for more systematic differences in the impact of COVID-19 by arm, we calculated a post hoc COVID-19 impact risk score (scored 0-6) based on whether or not the family experienced the following: a parent being furloughed (yes/no), a parent being dismissed (yes/no), concerns about finances (yes/no), no garden/outdoor space (yes/no), a problematic home environment (yes/no), and whether the child did not receive any face-to-face education (yes/no) (total impact risk score ranged from 0-6).
Semi-structured qualitative interviews covered 3 broad areas: (1) views on the usefulness of either Predictive Parenting or Psychoeducation for helping them cope with the pandemic (follow-up prompts included whether specific strategies were used and, if so, how); (2) the family’s experience of the COVID-19 pandemic and impacts on the child and family (follow-up prompts included the impact on the child’s emotions and behaviors, the child’s education, family life, any positive impacts, and changes over the course of the lockdown); and (3) factors that had helped the family cope with the impact of the pandemic (follow-up prompts included asking about the helpfulness of the family’s personal circumstances, formal and informal support networks, and professional help). Qualitative views on the family’s experience of the pandemic and coping strategies are not reported in the current article; only views of the usefulness of the interventions are presented.
Data Analysis
Data analysis of the questionnaires was conducted in Stata 17.23 All variables were assessed for normality. Both χ2 and t tests were used to examine the impact of the COVID-19 restrictions on familial circumstances and the COVID-19 impact risk score by intervention arm. We also conducted an attrition analysis to check that there were no differences in measured baseline characteristics between the group of participants who took part only at baseline vs those who took part at baseline and at the COVID-19 follow-up (Table S1, available online). No significant differences were found in child sex, autism traits, adaptive functioning, child irritability, parenting stress, or parental income or education level.
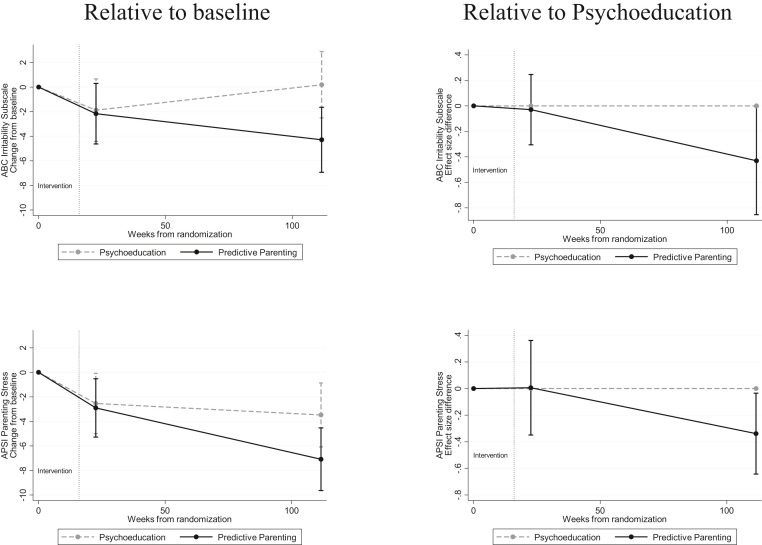
Using gsem we estimated 2 models, one for child irritability and one for parenting stress. Models specified 2 regressions, one predicting primary endpoint outcome and the other predicting COVID-19 follow-up outcome, each covarying for baseline, intervention arm, verbal language grouping, and site (the randomization stratification factors) while allowing for correlation between the primary endpoint and COVID-19 follow-up outcomes. First, we tested intervention arm differences at primary endpoint and at COVID-19 follow-up to look for the effects of Predictive Parenting in comparison to Psychoeducation. Next, using the lincom command, we calculated the area under the curve (AUC) to obtain an overall intervention effect across all 3 time points (sum of the trapezoidal areas between the groups) (Figure 3 ). These AUC effect estimates provide an overall mean effect for unequally spaced measures that summarize intervention effect over the whole period from baseline to follow-up.9 In addition to looking specifically at intervention effects at the COVID-19 follow-up timepoint, we wanted to include a model that accounted for the 3 time points of data and did not wish to be seen as continuing the pilot trial until we found a positive response. The AUC approach provides a principled way of doing this that is sensible and minimizes the analyst’s ability to choose one set of weighting for the time points over another (eg, reducing experimenter degrees of freedom as we allude to above). The AUC was estimated from an analysis methodology equivalent to linear mixed effects models; it combines parameter estimates obtained from a model that recognizes the repeated-measures structure while covarying for baseline. We chose this method over a generalized estimating equation model with robust standard errors and clustering, as these are known to be potentially unreliable in modest-sized samples such as we have. All models were estimated using maximum likelihood, which allows for selective missing data on the assumption that selection depends only on time, intervention arm, covariates, and observed outcomes (ie, missing-at-random).
Figure 3.
Course of Effects by Intervention Arm From Baseline to COVID-19 Follow-up
Note:Group level change relative to baseline (left) and Predictive Parenting relative to Psychoeducation (right). Bars represent time-specific estimates with 95% CIs from repeated-measures models.
Data from the semi-structured interviews were analyzed using an inductive thematic analysis approach based on grounded theory methods24 in NVivo. This involved multiple readings of the transcripts, from which a coding scheme was developed that also drew upon the emerging literature detailing the impacts of the COVID-19 pandemic on young autistic children. The coding scheme identified themes and was applied to the raw data by 1 researcher. Double coding of the data was done on 4 interviews by a second researcher to ensure that the scheme was applied consistently and to check for accuracy. Themes that emerged are reported below.
Results
Table 1 displays the impact of the COVID-19 restrictions on familial circumstances by intervention arm. There were no significant differences by intervention arm on any of the variables or on the COVID-19 impact risk score. Table 2 displays the descriptive statistics by intervention arm for the parent-reported ABC child irritability and the APSI parenting stress scores.
Table 2.
Descriptive Statistics at Each Time Point by Intervention Arm
| Psychoeducation |
Predictive parenting |
|||||
|---|---|---|---|---|---|---|
| Baseline (n = 31) | Primary endpoint (n = 28) | COVID-19 follow-up (n = 24) | Baseline (n = 31) | Primary endpoint (n = 30) | COVID-19 follow-up (n = 25) | |
| ABC-I: mean (SD) | 14.39 (9.90) | 12.71 (8.94) | 15.21 (8.12) | 18.13 (11.02) | 15.30 (9.08) | 13.12 (8.16) |
| APSI: mean (SD) | 21.74 (10.20) | 19.79 (7.75) | 19.29 (9.66) | 24.52 (9.49) | 21.33 (9.96) | 16.56 (8.51) |
Note: Baseline was up to 2 months prior to randomization. Primary endpoint was on average 22.6 weeks after randomization (∼5 months), SD = 3.8 weeks. Follow-up during COVID-19−related restrictions and on average 111.5 weeks after randomization (∼2 years), SD = 17.3 weeks. There were no significant differences in baseline scores on the ABC-I or the APSI for the 2 intervention arms t(60) = −1.41, p = .165, and t(60) = −1.11, p = .272, respectively). ABC-I = Aberrant Behavior Checklist−Irritability subscale; APSI = Autism Parenting Stress Index.
The effect estimates, confidence intervals, and AUC for parent-reported child irritability (ABC) are shown in Figure 3. The point estimate for effect of intervention on child irritability at primary endpoint was not statistically significant (Cohen's d = −0.03 [95% CI = −0.26, 0.21], p = .834), but the point effect at COVID-19 follow-up was statistically significant, with results in favor of Predictive Parenting (Cohen's d = −0.33 [95% CI = −0.65, −0.01], p = .046). However, the AUC analysis, which also takes into account the nonsignificant effect at primary endpoint, did not show a statistically significant difference overall between Predictive Parenting when compared with Psychoeducation (coefficient = −170.79 [95% CI = −400.80, 59.22], p = .146).
The point estimate for effect of intervention on parenting stress (APSI) at primary endpoint was not statistically significant (Cohen's d = −0.01 [95% CI = −0.32, 0.33], p = .973). The point estimate for the intervention effect at COVID-19 follow-up was significant in favor of Predictive Parenting (Cohen's d = −0.31 [95% CI = −0.59, −0.03], p = .029). The combined mean intervention effect comparing Predictive Parenting with Psychoeducation as estimated from the AUC (Figure 3) was not statistically significant (coefficient = −133.89 [95% CI = −371.82, 104.04], p = .270).
Three themes related to the interventions emerged from the interviews: general experience, strategies used, and suggestions for improvement (Table S2, available online, provides more detail). Parents in both Predictive Parenting and Psychoeducation found the groups helpful and reported that they had had positive experiences and that taking part had changed their everyday experience of being a parent. Parents in Predictive Parenting reported that it was helpful to have resources to refer to at a later time. A common suggestion for improvement included having booster sessions to help apply knowledge and implement strategies as children age and the associated parenting challenges change.
Strategies from Predictive Parenting that had been useful during the COVID-19−related restrictions included the following: understanding the function of displayed behavior, use of family rules and routines, praise, ignoring, planning, simplifying language, using visual aids, using sensory items and strategies, and parents taking care of themselves. The quotes below illustrate COVID-19−related strategy implementation.
“Trying to break down why they're doing something has been really helpful. Before I would be stressed out because I don't understand [his behavior]. Now I take a step back and think ‘OK, why is he doing this?’ Then from there I can react a bit better. I have more patience and can figure out, ‘OK, is it attention?’Then I need to spend some time with him. It has helped a lot.”
“There was just a single route that she wanted to take [to school]. One of the specific successes for me was I started introducing slight differences in route and that worked. When we were home during the lockdown and even subsequently, we used to go for walks and it was good to see that she continued saying ‘Let's explore a new route.’ So that has been a very positive thing.”
Discussion
The current study followed up families who had taken part in a pilot RCT testing the feasibility and preliminary efficacy of Predictive Parenting in comparison to Psychoeducation. In the original RCT in which pilot efficacy was measured immediately after intervention, effects on the primary outcome of observed behavior that challenges (we use this terminology because it is a preferred term among the autism community) were not statistically significant, although the direction of effect was in favor of Predictive Parenting.14 However, there was some evidence of benefits on secondary measures (eg, observed child compliance and observed parenting behavior) and high parental satisfaction with the intervention and good intervention fidelity, suggesting that further investigation may be of merit.
This study took advantage of the periods of heightened uncertainty induced by the COVID-19 pandemic to test the longer-term effects of a BPI designed to reduce EBPs in autistic children. Results showed both child irritability and parenting stress were significantly reduced at the COVID-19 follow-up in Predictive Parenting when compared to Psychoeducation, with small effect sizes on both measures of around 0.3. However, we highlight that these findings should be interpreted with the caveat that the overall effect, in terms of comparison of the magnitude of change from baseline to primary endpoint to COVID-19 follow-up in the two groups, as measured by the AUC, was nonsignificant.
Several explanations of the present findings should be considered. As to interpretation of intervention effects at the COVID-19 follow-up assessment, it is possible that the strategies taught in Predictive Parenting provided benefit during periods of unpredictability or stress, as it aimed to help parents promote predictability and to help autistic children with uncertainty. It was also the case that because of restrictions, parents and children were spending more time together, so use of Predictive Parenting strategies may have had greater impact.
However, in addition to the uncertainty induced by the COVID-19 pandemic, the significance of group differences at the COVID-19 follow-up could also be in part due to a longer duration between end of intervention and assessment (and thus significant intervention effects could be interpreted as evidence that COVID-19 and its associated lockdowns did not erode the positive longer-term effects of Predictive Parenting). In the original pilot RCT, effects were measured on average 6.2 weeks after the intervention ended; here, parents completed follow-up measures around 2 years later. The impression from the clinical team when conducting the original study was that families needed more time to implement strategies in the home in order for changes to translate to improvements in child behavior. This was mirrored in the themes that emerged from the semi-structured interviews at COVID-19 follow-up. Thus, we might expect changes in parenting skills and techniques to have a stronger effect with more time between intervention and assessment of child behavior. This is in line with the RUBI trial, in which greater divergence between their BPI and psychoeducation interventions occurred over a longer period of time.13 In addition, baseline ABC-I scores were higher in Bearss et al.'s13 RUBI trial compared to those in our sample (as we did not apply a threshold for eligibility). These relatively low scores reduce the statistical power to find differences between intervention arms and may contribute to why there was no difference at endpoint. Similar longer-term effects are reported elsewhere for parent-mediated interventions targeting autistic symptoms in children9; however, in non-autistic child populations, mixed findings as to whether effects of BPIs are reduced, sustained, or amplified over time are reported.10, 11, 12
Because of the natural experiment-type design of the follow-up study (eg, taking advantage of the increased uncertainty induced by the COVID-19 pandemic), it is not possible to disentangle whether effects are due to the specific circumstances under which outcomes were collected or the longer duration since intervention, or a combination of both. In addition, we did not have information on other interventions provided or stressful life events experienced between the end of the interventions and the COVID-19 follow-up assessment, so we are unable to rule out whether additional unmeasured experiences contributed to differences between the two arms. Either way, results suggest carefully considering the optimal time point to measure the effectiveness of BPIs for autistic children, both in terms of time since intervention and also under what circumstances.
Furthermore, current results cannot distinguish whether effects are because Predictive Parenting provided a buffer against declining child mental health in the context of the COVID-19 pandemic (eg, staves off additional decline in specific circumstances but does not promote outcomes beyond an individual’s typical level) or whether it leads to continued gains as time goes on, such that children in the intervention group end up with outcomes that surpass their baseline measurements (eg, lower levels of irritability and parental stress). We are not able to arbitrate between these alternatives based on the current follow-up data.
Despite not being planned a priori (and thus analyses were not pre-registered), the current study has clear strengths. We highlight the high retention rate in the current cohort (∼80%) and the lack of difference in COVID-19−related impacts between the two arms. We included both verbal and minimally verbal children, meaning that results are more generalizable to autistic children with a range of ability. In terms of limitations, the current outcome measures were all parent-report, and parents were not blinded to intervention arm, although an active attention control comparator was used. Follow-up questionnaires were included in a wider battery of questionnaires that were sent to parents to see how their family had been affected by the pandemic (rather than specifically being about effects of the intervention). Questionnaires were always completed before the semi-structured interviews took place, and interview data collection was completed before analysis of the questionnaire data. Rater effects are therefore unlikely to completely account for the observed results.
To better understand the drivers of longer-term benefits of BPIs, further study of the effects and potential intervention mechanisms (eg, change in parenting behavior and/or parental confidence to mitigate EBPs) is required.25 Our findings from this opportunistic follow-up study highlight the need for careful consideration of measuring the effects of BPIs in autistic child populations (ie, how much time after intervention is needed for parents to adaptively implement novel strategies, and in what contexts effects are most likely to be demonstrated).
Acknowledgments
The authors are grateful to all the families who were involved in the study. They would like to thank other members of the IAMHealth consortium, members of the IAMHealth parents and autistic adults PPI panels and members of the ASTAR Trial Steering Committee for their comments and advice on the original pilot trial design. They would also like to thank Joanne Tarver, PhD, of Aston University and Juan Paris Perez, MSc, of Sant Rafael Hospital and Vall d'Hebron University Hospital, for their help with earlier phases of the study.
Footnotes
Drs. Palmer and Carter Leno served as joint first authors of this work.
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. This study summarises independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research programme (RP-PG-1211-20016). The views expressed in this presentation are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. Additional funding for intervention materials was received from the Maudsley Charity (1157). VCL was supported by the Wellcome Trust through a Sir Henry Wellcome Postdoctoral Fellowship (213608/Z/18/Z). AP and ES received support from the NIHR through a Senior Investigator Award (NF-SI-0617-10120, NF-SI-0514-10073) and from the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust (IS-BRC-1215-20018).
The research was performed with permission from the Psychiatry, Nursing and Midwifery Research Ethics Subcommittee at King's College London.
Consent has been provided for descriptions of specific patient information.
Dr. Pickles served as the statistical expert for this research.
Author Contributions
ES, TC, SS, AP and VS obtained funding. MP, VCL, ES, TC, AP, VS and SS were involved in designing and conducting the study and/or data collection or analysis. VH, JM and LB were involved in developing and delivering the interventions. The manuscript was drafted by MP and VCL and all authors read, made revisions, and approved the final version.
Disclosure: Dr. Pickles has received questionnaire royalties from WPS. Dr. Charman has received consultancy fees from F. Hoffmann-La Roche Ltd. and Servier and royalties from Sage Publications and Guilford Publications. Drs. Palmer, Carter Leno, Hallett, Mueller, Breese, Slonims, Scott, and Simonoff have reported no biomedical financial interests or potential conflicts of interest.
Supplemental Material
References
- 1.American Psychiatric Association . 5th ed. DSM-5. American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 2.Kenny L., Hattersley C., Molins B., Buckley C., Povey C., Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20(4):442–462. doi: 10.1177/1362361315588200. [DOI] [PubMed] [Google Scholar]
- 3.Salazar F., Baird G., Chandler S., et al. Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J Autism Dev Disord. 2015;40(9):1080–1093. doi: 10.1007/s10803-015-2361-5. [DOI] [PubMed] [Google Scholar]
- 4.Simonoff E., Pickles A., Charman T., Chandler S., Loucas T., Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 5.Yorke I., White P., Weston A., Rafla M., Charman T., Simonoff E. The association between emotional and behavioral problems in children with autism spectrum disorder and psychological distress in their parents: a systematic review and meta-analysis. J Autism Dev Disord. 2018;48(10):3393–3415. doi: 10.1007/s10803-018-3605-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute for Health and Clinical Excellence . 2013. Antisocial behaviour and conduct disorders in children and young people: recognition and management (CG158)https://www.nice.org.uk/guidance/cg158 [PubMed] [Google Scholar]
- 7.Postorino V., Sharp W.G., McCracken C.E., et al. A systematic review and meta-analysis of parent training for disruptive behavior in children with autism spectrum disorder. Clin Child Fam Psychol Rev. 2017;20(4):391–402. doi: 10.1007/s10567-017-0237-2. [DOI] [PubMed] [Google Scholar]
- 8.Tarver J.H., Palmer M.L., Webb S., et al. Child and parent outcomes following parent interventions for child emotional and behavioral problems in autism spectrum disorders (ASD): a systematic review and meta-analysis. Autism. 2019;23(7):1630–1644. doi: 10.1177/1362361319830042. [DOI] [PubMed] [Google Scholar]
- 9.Pickles A., Le Couteur A., Leadbitter K., et al. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomised controlled trial. Lancet. 2016;388(10059):2501–2509. doi: 10.1016/S0140-6736(16)31229-6. 2022/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karjalainen P., Santalahti P., Aronen E.T., Kiviruusu O. Parent- and teacher-reported long-term effects of parent training on child conduct problems in families with child protection and other support services: a randomized controlled trial. Child Adolesc Psychiatry Ment Health. 2021;15(7) doi: 10.1186/s13034-021-00358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rimestad M.L., Lambek R., Zacher Christiansen H., Hougaard E. Short- and long-term effects of parent training for preschool children with or at risk of ADHD: a systematic review and meta-analysis. J Atten Disord. 2019;23(5):423–434. doi: 10.1177/1087054716648775. [DOI] [PubMed] [Google Scholar]
- 12.Webster-Stratton C. The long-term effects of a videotape modeling parent-training program: comparison of immediate and 1-year follow-up results. Behav Ther. 1982;13(5):702–714. doi: 10.1016/S0005-7894(82)80026-9. [DOI] [Google Scholar]
- 13.Bearss K., Johnson C., Smith T., et al. Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: a randomized clinical trial. JAMA. 2015;313(15):1524–1533. doi: 10.1001/jama.2015.3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charman T., Palmer M., Stringer D., et al. A novel group parenting intervention for emotional and behavioral difficulties in young autistic children: Autism Spectrum Treatment and Resilience (ASTAR): a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2021;60(11):1404–1418. doi: 10.1016/j.jaac.2021.03.024. doi:S0890-8567(21)00298-7. [DOI] [PubMed] [Google Scholar]
- 15.Boulter C., Freeston M., South M., Rodgers J. Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. J Autism Dev Disord. 2014;44(6):1391–1402. doi: 10.1007/s10803-013-2001-x. [DOI] [PubMed] [Google Scholar]
- 16.Pickard H., Hirsch C., Simonoff E., Happé F. Exploring the cognitive, emotional and sensory correlates of social anxiety in autistic and neurotypical adolescents. J Child Psychol Psychiatry. 2020;61(12):1317–1327. doi: 10.1111/jcpp.13214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.H. Samji, J. Wu, A. Ladak, et al., Review: mental health impacts of the COVID-19 pandemic on children and youth─a systematic review, Child Adolesc Ment Health, 27(2), 2022, 173-189. doi:10.1111/camh.12501. [DOI] [PMC free article] [PubMed]
- 18.Hallett V., Mueller J., Breese L., et al. Introducing ‘Predictive Parenting’: a new group parenting intervention targeting emotional and behavioral difficulties in children with autism spectrum disorder. J Autism Dev Disord. 2021;51(1):323–333. doi: 10.1007/s10803-020-04442-2. [DOI] [PubMed] [Google Scholar]
- 19.Palmer M., Tarver J., Paris Perez J., et al. A novel group parenting intervention to reduce emotional and behavioural difficulties in young autistic children: protocol for the Autism Spectrum Treatment and Resilience (ASTAR) pilot randomised controlled trial. BMJ Open. 2019;(e029959):9. doi: 10.1136/bmjopen-2019-029959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.M.G. Aman and N.N. Singh, Aberrant Behavior Checklist─Community, 1994, Slosson Educational Publications, Inc.,; East Aurora, NY, Supplementary Manual.
- 21.Silva L.M., Schalock M. Autism Parenting Stress Index: initial psychometric evidence. J Autism Dev Disord. 2012;42(4):566–574. doi: 10.1007/s10803-011-1274-1. [DOI] [PubMed] [Google Scholar]
- 22.Nikolaidis A., Paksarian D., Alexander L., et al. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci Rep. 2021;11(1):8139. doi: 10.1038/s41598-021-87270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.StataCorp . College Station, TX: StataCorp LLC; 2021. Stata Statistical Software: release 17. [Google Scholar]
- 24.Palinkas L.A. Qualitative and mixed methods in mental health services and implementation research. J Clin Child Adolesc Psychol. 2014;43(6):851–861. doi: 10.1080/15374416.2014.910791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brookman-Frazee L., Chlebowski C., Villodas M., Roesch S., Martinez K. Training community therapists to deliver an individualized mental health intervention for autism spectrum disorder: changes in caregiver outcomes and mediating role on child outcomes. J Am Acad Child Adolesc Psychiatry. 2021;60(3):355–366. doi: 10.1016/j.jaac.2020.07.896. doi:S0890-8567(20)31338-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.