Abstract
Background
This study was aimed to examine the effectiveness of App-assisted self-care in a Beijing community based on intelligent family physician-optimised collaborative model (IFOCM) program.
Methods
We conducted a survey of 12,050 hypertensive patients between Jan 2014 and Dec 2021. Generalized linear model was used to analyze the covariates that associated with blood pressure (BP) control. Decision tree and random forest algorithm was used to extract the important factors of BP outcome.
Results
The study included 5937 patients, mean age 66.2 ± 10.8, with hypertension in the baseline; 3108(52.4) were female. The community management resulted in mean systolic BP and diastolic BP reductions of 4.6 mmHg and 3.8 mmHg at follow-up. There were 3661 (61.6%) hypertension patients with BP control, increasing from 55.0% in 2014 to 75.0% in 2021. After adjusted for covariates, antihypertensive medication adherence, diabetes, and APP-assisted self-care were common predictors associated with BP control in GLM model and machine learning algorithm.
Conclusion
Community management based on IFOCM program significantly improved BP control in hypertensive patients. APP-assisted self-care would be beneficial for the management of chronic disease.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-023-01965-2.
Keywords: Hypertension, Community and family medicine, Cohort study
Background
Hypertension has become one of the most important causes of disease burden in the world [1]. It is the leading risk factor of cardiovascular disease and stroke, accounting for nearly half of the morbidity and mortality [2–4]. A population-based study involved 1.7 million individuals revealed that hypertension awareness of 36%, treatment of 22.9% and control of only 5.7% in China [5]. Despite the hypertension control rate rising from 6.1% to 16.8% in recent years [6], that current management are insufficient to address the burden of hypertension [7, 8].
Self-management of blood pressure (BP), where patients management their own BP usually in a home environment, is an increasingly strategy of hypertension management [9, 10], which have been demonstrated to improve BP control in many Western countries [11–13]. The evidence for hypertension self-management is limited in China. Several studies [14–16] reported self-management may be a feasible and cost-effectiveness strategy for BP control in Chinese population. However, these studies were small sample size [14–16], cross-sectional [14] or intervention design [15], could not examine the effectiveness of community healthcare in controlling BP in the real world.
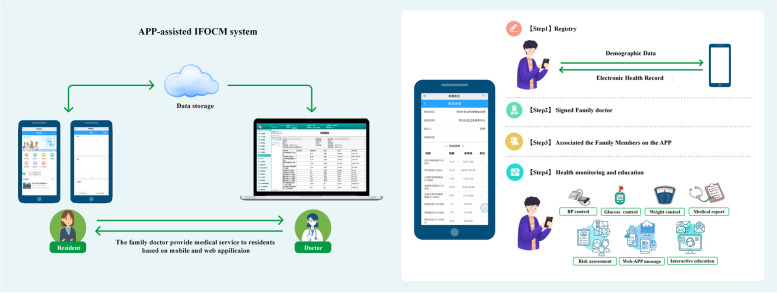
When facing such large number of hypertensive patients, Chinese government launched the Basic Public Health Service Program in 2009 and Family Physician Program in 2016. Beijing was the earliest pilot city implementing the intelligent family physician-optimised coordination model (IFOCM) program in China [17]. With the popular of mobile health, smartphone also provides a promising approach access to self-care management in daily life. Our community health service center is one of the first facilities to apply APP-assisted self-care in the IFOCM program. APP-assisted IFOCM system is designed to help users make consistent monitor and management of physiological indicators, and remind them to take medicine or modify lifestyle. This software system includes an app for users and a web application for contracted family doctors (Fig. 1). In this study, we aimed to examine the effectiveness of BP control in our community and to investigate the role of mobile APP-assisted self-care in the present community-based cohort study.
Fig. 1.
Overview of the APP-assisted IFOCM software system
Methods
Study design
This study was a community-based survey for patients with hypertension, performed by our community healthcare from Jan 2014 to December 2021. All patients having baseline record in the database of Beijing Primary Medical and Public Health Information System were initially considered for inclusion. Patients were included if they: (1) 18 years or older and diagnosed as having hypertension in the baseline; (2) had at least one follow-up record documented in the database; and (3) were not involved in other public health intervention program. Patients were excluded if they had severe neurological or psychiatric disorders; physical disability; and pregnancy hypertension. Informed consent from all subjects and/or their legal guardian was signed in the community health service center, and analysis was performed using deidentified data. The study was approved by the ethics committee of our community health service center.
Data collection
Deidentified data were extracted from the database, which included all patients with chronic diseases managed by community health service center. All individuals participated in baseline survey, physical examination, blood tests. The survey investigated the demographic characteristic, comorbidities such as hypertension, diabetes mellitus, coronary artery disease, and stroke. Physical examination included blood pressure, body weight, body height, waist girth, and hip girth. Blood tests assessed fasting blood-glucose and total cholesterol level. For residents participated IFOCM program, follow-up was conducted by team member in community. Follow-up information, such as systolic blood pressure (SBP), diastolic blood pressure (DBP), blood-glucose, blood lipid level, antihypertensive medication adherence, adverse drug reaction and follow-up date was recorded.
Definition of variable and outcome
Hypertension was diagnosed as a maintained SBP/DBP ≥ 140/90 mmHg, or receiving antihypertensive medications. Baseline and follow-up body mass index (BMI, kg/m2) was calculated as the weight (kg) divided by squared height (m), and obesity was defined as BMI ≥ 27 at follow-up. Waist-hip ratio was calculated as the waist girth divided by hip girth, the ratio ≥ 0.9 was defined as increased level. The follow-up time was calculated as the last recorded visit date subtract baseline date.
We set two primary outcomes: BP control levels (continuous outcome) and BP control rates (categorical outcome). When treated BP as categorical outcome, we assessed the rates of patients with hypertension in control, which was according to the following definitions based on Chinese guideline [6]. For hypertension, BP control during a given visit as a SBP < 140 mmHg and DBP ≤ 90 mmHg, and for diabetes or coronary heart disease, a SBP ≤ 130 mmHg and DBP ≤ 80 mmHg.
Machine learning
We used the random forest (RF) algorithm for the prediction of poor BP control of hypertension patients. RF is a machine learning algorithm that aggregates many predictions to reduce the variance and improve the robustness and precision of outputs [18]. A remarkable characteristic of the RF is that it offers an internal measure to show the importance of each variable on the prediction. Even if the data are missing or unbalanced [19], RF model can work very well for any type of problem regardless of sample size. Generally speaking, RF can quantify which variable contribute most to classification accuracy and suggests an important associated variables evaluated by the model, which can be optimized to obtain the best results from the data they are analyzing. In this study, we compared RF and other machine learning algorithms, including decision tree (DT), support vector machine(SVM), and naïve Bayes(NB) for predicting the outcome of BP control.
Statistical analyses
The statistical analysis was performed by Stata (v.16.0) and R software (v.3.6.3). For normally distributed continuous variables, the values are expressed as mean ± standard deviation (SD) and compared using a 2-sided t-test. The categorical variables are expressed as frequencies, and comparisons are made using the Chi-squared test or Fisher’s exact test when appropriate.
To analyze the outcome of BP control levels, we estimated covariates that affect the values of SBP and DBP, a generalized linear model (GLM) was used to adjust for covariates including demographic characteristic, comorbidity, BMI, waist-hip ratio, baseline blood pressure, blood-glucose and total cholesterol level. Decreases in SBP and DBP in follow-up compared with baseline were considered dependent variables, whereas other covariates were considered independent variables. To analyze the outcome of BP control rates, we estimated covariates that associated with BP control in the GLM, poor BP control was considered dependent variable, and other similar covariates considered as independent variables were adjusted. Predictors of poor BP control manifested a statistical significance of P < 0.05 were subsequently utilized for different machine learning algorithm. Mean Decrease Gini (MDG) involved in RF algorithm with cross-validation was used to rank the important covariates with poor BP control.
Results
Baseline characteristics
A total of 44,039 community residents were recorded in the database at the baseline. The community center has 12,050 hypertensive patients, accounting for 27.3% of the population (Supplement Fig. 1). The difference between hypertensive patients with and without IFOCM management is shown in Supplement Table. Finally, there were 5937 participants thus included in the analysis of BP control, the mean age was 66.2 ± 10.8; 3108(52.4) were female. Baseline characteristics between participants with and without APP-assisted self-care is shown in Table 1. Compared to patients without APP-assisted self-care, APP-assisted group showed significantly greater age (66.5 ± 10.2 vs. 65.5 ± 12.4 years, P = 0.004), BMI (25.9 ± 3.5 vs. 25.6 ± 3.6 kg/m2, P = 0.052), waist (88.8 ± 9.5 vs. 87.6 ± 9.2 cm, P < 0.001) and hip (98.4 ± 9.2 vs. 96.9 ± 9.2 cm, P < 0.001); with significantly lower baseline SBP (128.0 ± 7.3 vs 130.8 ± 6.6 mmHg, P < 0.001) and DBP (76.8 ± 5.6 vs 77.6 ± 5.7 mmHg, P < 0.001). APP-assisted self-care patients were more likely to be female (53.2% vs. 49.7, P = 0.018), unmarried (12.7% vs. 9.0%, P < 0.001), native resident (97.3% vs. 91.0%, P < 0.001), urban citizen (99.8% vs. 99.1%, P < 0.001). Patients with APP-assisted also had more chronic diseases, including diabetes (42.5% vs. 37.4%, P < 0.001), coronary heart disease (34.4% vs. 28.7%, P < 0.001), and stroke (16.7% vs. 14.4%, P = 0.039) than those patients without.
Table 1.
Baseline information of hypertensive patients with and without APP-assisted self-care (N = 5937)
| Total (N = 5937) | With APP-assisted self-care (N = 4454) | Without APP-assisted self-care (N = 1483) | P value | |
|---|---|---|---|---|
| Age, y | 66.2 ± 10.8 | 66.5 ± 10.2 | 65.5 ± 12.4 | 0.004 |
| Gender, n (%) | 0.018 | |||
| Male | 2829(47.6) | 2083(46.8) | 746(50.3) | |
| Female | 3108(52.4) | 2371(53.2) | 737(49.7) | |
| Marriage status, n (%) | < 0.001 | |||
| Married | 5238(88.2) | 3888(87.3) | 1350(91.0) | |
| Single/divorced/widowed | 699(11.8) | 566(12.7) | 133(9.0) | |
| Native resident, n (%) | < 0.001 | |||
| No | 250(4.2) | 117(2.6) | 133(9.0) | |
| Yes | 5687(95.8) | 4337(97.3) | 1350(91.0) | |
| Population composition, n (%) | < 0.001 | |||
| Urban | 5914(99.6) | 4444(99.8) | 1470(99.1) | |
| Rural | 23(0.4) | 10(0.2) | 13(0.9) | |
| Comorbidity, n (%) | ||||
| Diabetes | 2447(41.2) | 1892(42.5) | 555(37.4) | 0.001 |
| Coronary artery disease | 1995(33.6) | 1530(34.4) | 425(28.7) | < 0.001 |
| Stroke | 958(16.1) | 744(16.7) | 214(14.4) | 0.039 |
| Height,cm | 163.6 ± 8.6 | 163.4 ± 8.6 | 164.5 ± 8.6 | < 0.001 |
| Weight, Kg | 69.3 ± 11.7 | 69.3 ± 11.5 | 69.5 ± 12.0 | 0.565 |
| Body Mass Index, kg/m2 | 25.8 ± 3.5 | 25.9 ± 3.5 | 25.6 ± 3.6 | 0.052 |
| Waist, cm | 88.5 ± 9.5 | 88.8 ± 9.5 | 87.6 ± 9.2 | < 0.001 |
| Hip, cm | 98.0 ± 9.2 | 98.4 ± 9.2 | 96.9 ± 9.2 | < 0.001 |
| Waist-hip ratio | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.90 ± 0.1 | 0.300 |
| Fasting blood-glucose | 6.3 ± 1.0 | 6.3 ± 1.1 | 6.3 ± 0.9 | 0.117 |
| Total cholesterol | 4.9 ± 1.0 | 4.8 ± 1.0 | 4.9 ± 0.9 | 0.589 |
| Systolic BP, mmHg | ||||
| Baseline | 128.7 ± 7.2 | 128.0 ± 7.3 | 130.8 ± 6.6 | < 0.001 |
| Follow-up | 124.1 ± 13.8 | 122.6 ± 13.6 | 128.5 ± 13.5 | < 0.001 |
| Difference | -4.6 ± 15.6 | -5.4 ± 15.5 | -2.3 ± 15.9 | < 0.001 |
| Diastolic BP, mmHg | ||||
| Baseline | 77.0 ± 5.7 | 76.8 ± 5.6 | 77.6 ± 5.7 | < 0.001 |
| Follow-up | 73.5 ± 10.6 | 72.6 ± 10.7 | 76.2 ± 9.5 | < 0.001 |
| Difference | -3.5 ± 11.9 | -4.2 ± 12.0 | -1.3 ± 11.1 | < 0.001 |
| Follow-up BP control, n (%) | ||||
| Systolic | 3886(65.4) | 3000(67.4) | 886(59.7) | < 0.001 |
| Diastolic | 4720(79.5) | 3596(80.7) | 1124(75.8) | < 0.001 |
| Overall | 3661(61.6) | 2827(63.4) | 834(56.2) | < 0.001 |
Abbreviation: Data are mean ± standard deviation except where indicated otherwise. APP application. BP blood pressure
Detecting predictors for BP control levels
Compared with baseline, the community management resulted in mean SBP and DBP reductions of 4.6 mmHg and 3.5 mmHg at follow-up, respectively. The effect of hypertension management on decreases in SBP and DBP in follow-up compared with baseline was analyzed and subgroup analyses were conducted based on demographic characteristic, comorbidities, baseline date, APP-assisted self-care, antihypertensive medication adherence and follow-up time (Table 2).
Table 2.
The effect of hypertension management on SBP and DBP level
| Patients | Difference in SBP, mmHg | Difference in DBP, mmHg | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | B | P value | Ba0 | P value* | Mean (95% CI) | B | P value | Ba | P value* | ||
| Age (years), n (%) | -2.30 | < 0.001 | -0.53 | 0.124 | -2.09 | 0.497 | -0.34 | 0.215 | |||
| ≤ 65 | 2902(48.8) | -3.42(-3.97,-2.88) | -3.36(-3.77,-2.95) | ||||||||
| > 65 | 3035(51.2) | -5.73(-6.28,-5.14) | -3.57(-4.01,-3.05) | ||||||||
| Male, n (%) | 0.36 | 0.379 | 0.61 | 0.081 | 0.04 | 0.904 | 0.30 | 0.276 | |||
| No | 3108(52.4) | -4.77(-5.35,-4.28) | -3.49(-3.93,-3.07) | ||||||||
| Yes | 2829(47.6) | -4.41(-4.97,-3.86) | -3.45(-3.90,-3.06) | ||||||||
| Marriage status, n (%) | 0.94 | 0.133 | -0.41 | 0.428 | -0.17 | 0.719 | -0.17 | 0.675 | |||
| Married | 5238(88.2) | -4.49(-4.95,-4.08) | -3.49(-3.82,-3.17) | ||||||||
| Single/divorced/widowed | 699(11.8) | -5.43(-6.56,-4.34) | -3.32(-4.19,-2.42) | ||||||||
| Native resident, n (%) | 1.04 | 0.303 | -0.16 | 0.847 | 0.57 | 0.456 | -0.35 | 0.870 | |||
| No | 5687(95.8) | -4.65(-5.07,-4.24) | -3.50(-3.83,-3.18) | ||||||||
| Yes | 250(4.2) | -3.60(-5.30,-1.97) | -2.92(-4.10,-1.74) | ||||||||
| Population composition, n (%) | -1.93 | 0.555 | -2.01 | 0.453 | 0.65 | 0.794 | -0.72 | 0.291 | |||
| Urban | 5914(99.6) | -4.59(-5.00,-4.19) | -3.47(-3.77,-3.20) | ||||||||
| Rural | 23(0.4) | -6.52(-13.25,1.57) | -2.83(-8.93,2.81) | ||||||||
| Obesity, n (%) | -0.56 | 0.196 | 0.02 | 0.965 | -0.25 | 0.452 | 0.01 | 0.993 | |||
| No | 4028(67.8) | -4.42(-4.93,-3.92) | -3.39(-3.77,-3.02) | ||||||||
| Yes | 1909(32.2) | -4.98(-5.68,-4.31) | -3.64(-4.15,-3.09) | ||||||||
| Increased Waist-hip ratio, n (%) | -0.83 | 0.046 | -0.37 | 0.289 | -0.74 | 0.018 | -0.40 | 0.146 | |||
| No | 3578(60.2) | -4.27(-4.77,-3.78) | -3.18(-3.55,-2.81) | ||||||||
| Yes | 2359(39.8) | -5.10(-5.71,-4.48) | -3.92(-4.39,-3.42) | ||||||||
| Diabetes, n (%) | -1.29 | 0.002 | -1.52 | < 0.001 | -0.91 | 0.004 | -1.06 | < 0.001 | |||
| No | 3490(58.8) | -4.07(-4.59,-3.56) | -3.10(-3.47,-2.69) | ||||||||
| Yes | 2447(41.2) | -5.36(-6.02,-4.77) | -4.01(-4.54,-3.54) | ||||||||
| Coronary artery disease, n (%) | -0.05 | 0.909 | 0.34 | 0.342 | 0.35 | 0.285 | 0.39 | 0.176 | |||
| No | 3982(67.0) | -4.59(-5.07,-4.08) | -3.59(-3.97,-3.23) | ||||||||
| Yes | 1955(33.0) | -4.63(-5.35,-3.93) | -3.24(-3.81,-2.69) | ||||||||
| Stroke, n (%) | -1.16 | 0.035 | -0.12 | 0.784 | -0.01 | 0.993 | 0.12 | 0.741 | |||
| No | 4979(83.8) | -4.41(-4.89,-4.01) | -3.47(-3.79,-3.16) | ||||||||
| Yes | 958(16.2) | -5.57(-6.49,-4.74) | -3.47(-4.22,-2.73) | ||||||||
| Baseline date, n (%) | -3.39 | < 0.001 | -2.91 | < 0.001 | -2.44 | < 0.001 | -2.39 | < 0.001 | |||
| 2014–2017 | 3822(64.4) | -4.05(-4.52,-3.68) | -3.05(-3.38,-2.72) | ||||||||
| 2018–2021 | 2115(35.6) | -5.50(-5.98,-5.03) | -3.75(-4.21,-3.29) | ||||||||
| APP-assisted self-care, n (%) | -3.11 | < 0.001 | -4.59 | < 0.001 | -2.88 | < 0.001 | -2.91 | < 0.001 | |||
| No | 1483(25.0) | -2.27(-3.12,-1.49) | -1.31(-1.89,-0.72) | ||||||||
| Yes | 4454(75.0) | -5.38(-5.86,-4.94) | -4.19(-4.59,-3.84) | ||||||||
| Antihypertensive medication adherence, n (%) | -13.47 | < 0.001 | -13.04 | < 0.001 | -6.95 | < 0.001 | -6.86 | < 0.001 | |||
| No | 846(14.2) | 6.95(5.82,8.14) | 2.49(1.68,3.26) | ||||||||
| Yes | 5091(85.8) | -6.52(-6.96,-6.12) | -4.46(-4.78,-4.15) | ||||||||
| Follow-up time, n (%) | -2.04 | < 0.001 | 0.55 | 0.219 | -1.15 | 0.001 | 0.68 | 0.057 | |||
| ≤ 1 year | 1443(24.4) | -3.05(-3.74,-2.27) | -2.60(-3.13,-2.05) | ||||||||
| > 1 year | 4494(75.6) | -5.10(-5.57,-4.64) | -3.75(-4.10,-3.36) | ||||||||
Abbreviation: SBP Systolic blood pressure, DBP Diastolic blood pressure, B Beta coefficient
Ba, adjusted beta coefficient
* Adjusted P values
Univariate GLM analysis using the difference in SBP or DBP level between baseline and follow-up as the dependent variable reveled that age (B = -2.30, P < 0.001), increased waist-hip ratio (B = -0.83, P = 0.046), diabetes (B = -1.29, P = 0.002), stroke (B = -1.16, P = 0.035), baseline date (B = -3.39, P < 0.001), APP-assisted self-care (B = -3.11, P < 0.001), antihypertensive medication adherence (B = -13.47, P < 0.001) and follow-up time (B = -2.04, P < 0.001) was associated with decreases in SBP level; increased waist-hip ratio (B = -0.74,P = 0.018), diabetes (B = -0.91, P = 0.004), baseline date (B = -2.44, P < 0.001), APP-assisted self-care (B = -2.88, P < 0.001), antihypertensive medication adherence (B = -6.95, P < 0.001) and follow-up time (B = -1.15, P = 0.001) was associated with decreases in DBP level.
After adjusted covariates in the multivariable GLM analysis, the results revealed that patients with diabetic exhibited a significant SBP reduction (B = -1.52, p < 0.001; -5.36 mmHg, 95% CI [-6.02, -4.77] vs. -4.07 mmHg, 95%CI [-4.59, -3.56]) and DBP reduction (B = -1.06, p < 0.001; -4.016 mmHg, 95% CI [-4.54, -3.54] vs. -3.10 mmHg, 95%CI [-3.47, -2.69]) compared to those without diabetic. Later baseline date was associated with significant lower SBP reduction (B = -2.91, p < 0.001; -5,50 mmHg, 95% CI [-5.98, -5.03] vs. -4.05 mmHg, 95%CI [-4.52, -3.68]) and DBP reduction (B = -2.39, p < 0.001; -3,75 mmHg, 95% CI [-4.21, -3.29] vs. -3.05 mmHg, 95%CI [-3.38, -2.72]). In those patients with APP-assisted self-care, the results suggested a significant reduction both in SBP level (B = -4.59, p < 0.001; -5.38 mmHg, 95% CI [-5.86, -4.94] vs. -2.27 mmHg, 95%CI [-3.12, -1.49]) and in DBP level (B = -2.91, p < 0.001; -4.19 mmHg, 95% CI [-4.59, -3.84] vs. -1.31 mmHg, 95%CI [-1.89, -0.72]). Similarly, for patients with antihypertensive medication adherence, significant reduction was also found in SBP level (B = -13.04, p < 0.001; -6.52 mmHg, 95% CI [-6.96, -6.12] vs. 6.95 mmHg, 95%CI [5.82,8.14]) and in DBP level (B = -6.86, p < 0.001; -4.46 mmHg, 95% CI [-4.78, -4.15] vs. 2.49 mmHg, 95%CI [1.68,3.26]).
Detecting predictors for BP control rates
There were 3661(61.6%) hypertension patients with BP control, which increased from 55.0% in 2014 to 75.0% in 2021 (Supplement Fig. 2). The effect of hypertension management on overall BP control in follow-up was analyzed and subgroup analyses were conducted (Table 3). Univariate GLM analysis using poor BP control as the dependent variable reveled that native resident (P < 0.001), diabetes (P < 0.001), coronary artery disease (P < 0.001), stroke (P = 0.001), baseline date (P < 0.001), APP-assisted self-care (P < 0.001), antihypertensive medication adherence (P < 0.001), and follow-up time (P < 0.001) are important factors associated with poor BP control. After adjusted covariates in the multivariable GLM analysis, the results revealed that native resident (OR = 0.50, 95%CI [0.34,0.74], P < 0.001), diabetes (OR = 1.50, 95%CI [1.33,1.70], P < 0.001), coronary artery disease (OR = 1.35, 95%CI [1.19,1.53], P < 0.001), stroke (OR = 1.20, 95%CI [1.02,1.41], P = 0.026), baseline date (OR = 0.72, 95%CI [0.62,0.83], P < 0.001), APP-assisted self-care (OR = 0.51,95%CI [0.44,0.59], P < 0.001), antihypertensive medication adherence (OR = 0.14,95%CI [0.11,0.16], P < 0.001) and follow-up time (OR = 2.02,95% CI [1.70,2.40], P < 0.001) are predictors for BP control.
Table 3.
Overall BP control in hypertension patients with different characteristics
| Total (N = 5937) | Good control (N = 3661) | Poor control (N = 2276) | Univariate analysis | Multivariable analysis | |||
|---|---|---|---|---|---|---|---|
| OR(95%CI) | P value | OR(95%CI) | P value | ||||
| Age (years), n (%) | 1.06(0.96,1.18) | 0.251 | 0.89(0.78, 1.02) | 0.091 | |||
| ≤ 65 | 2902(48.8) | 1811(49.5) | 1091(47.9) | ||||
| > 65 | 3035(51.2) | 1850(50.5) | 1185(52.1) | ||||
| Male, n(%) | 1.03(0.93,1.14) | 0.612 | 0.99(0.87, 1.13) | 0.893 | |||
| No | 3108(52.4) | 1926(52.6) | 1182(51.9) | ||||
| Yes | 2829(47.6) | 1735(47.4) | 1094(48.1) | ||||
| Marriage status, n (%) | 0.92(0.78,1.08) | 0.281 | 1.00(0.83, 1.21) | 0.986 | |||
| Married | 5238(88.2) | 3243(88.6) | 1995(87.7) | ||||
| Single/divorced/widowed | 699(11.8) | 418(11.4) | 281(12.3) | ||||
| Native resident, n (%) | 0.44(0.32, 0.60) | < 0.001 | 0.50(0.34, 0.74) | < 0.001 | |||
| No | 250(4.2) | 195(5.3) | 55(2.4) | ||||
| Yes | 5687(95.8) | 3466(94.7) | 2221(97.6) | ||||
| Population composition, n (%) | 1.03(0.45,2.39) | 0.937 | 1.76(0.62, 4.97) | 0.285 | |||
| Urban | 5914(99.6) | 3647(99.6) | 2267(99.6) | ||||
| Rural | 23(0.4) | 14(0.4) | 9(0.4) | ||||
| Obesity, n (%) | 1.09(0.98, 1.22) | 0.121 | 0.98(0.86, 1.11) | 0.724 | |||
| No | 4028(67.8) | 2511(68.6) | 1517(66.6) | ||||
| Yes | 1909(32.2) | 1150(31.4) | 759(33.4) | ||||
| Increased Waist-hip ratio, n (%) | 1.09(0.98,1.20) | 0.131 | 1.07(0.94, 1.22) | 0.279 | |||
| No | 3578(60.2) | 2234(61.0) | 1344(59.1) | ||||
| Yes | 2359(39.8) | 1427(39.0) | 932(40.9) | ||||
| Diabetes, n (%) | 1.91(1.71,2.12) | < 0.001 | 1.50(1.33, 1.70) | < 0.001 | |||
| No | 3490(58.8) | 2372(64.8) | 1118(49.1) | ||||
| Yes | 2447(41.2) | 1289(35.2) | 1158(50.9) | ||||
| Coronary artery disease, n (%) | 1.54(1.38, 1.71) | < 0.001 | 1.35(1.19, 1.53) | < 0.001 | |||
| No | 3982(67.0) | 2590(70.7) | 1392(61.2) | ||||
| Yes | 1955(33.0) | 1071(29.3) | 884(38.8) | ||||
| Stroke, n (%) | 1.27(1.11, 1.46) | 0.001 | 1.20(1.02, 1.41) | 0.026 | |||
| No | 4979(83.8) | 3117(85.1) | 1862(81.8) | ||||
| Yes | 958(16.2) | 544(14.9) | 414(18.2) | ||||
| Baseline date, n(%) | 0.63(0.56–0.70) | < 0.001 | 0.72(0.62, 0.83) | < 0.001 | |||
| 2014–2017 | 3822(64.4) | 2210(60.4) | 1612(70.8) | ||||
| 2018–2021 | 2115(35.6) | 1451(39.6) | 664 (29.2) | ||||
| APP-assisted self-care, n (%) | 0.74(0.66–0.83) | < 0.001 | 0.51(0.44, 0.59) | < 0.001 | |||
| No | 1483(25.0) | 834(22.8) | 649(28.5) | ||||
| Yes | 4454(75.0) | 2827(77.2) | 1627(71.5) | ||||
| Antihypertensive medication adherence, n (%) | 0.16(0.14–0.20) | < 0.001 | 0.14(0.11, 0.16) | < 0.001 | |||
| No | 846(14.2) | 218(6.0) | 628(27.6) | ||||
| Yes | 5091(85.8) | 3443(94.0) | 1648 (72.4) | ||||
| Follow-up time, n (%) | 1.96(1.72–2.24) | < 0.001 | 2.02(1.70, 2.40) | < 0.001 | |||
| ≤ 1 year | 1443(24.4) | 1055(28.8) | 388(17.0) | ||||
| > 1 year | 4494(75.6) | 2606(71.2) | 1888(83.0) | ||||
Testing prediction accuracy of predictors in machine learning algorithm
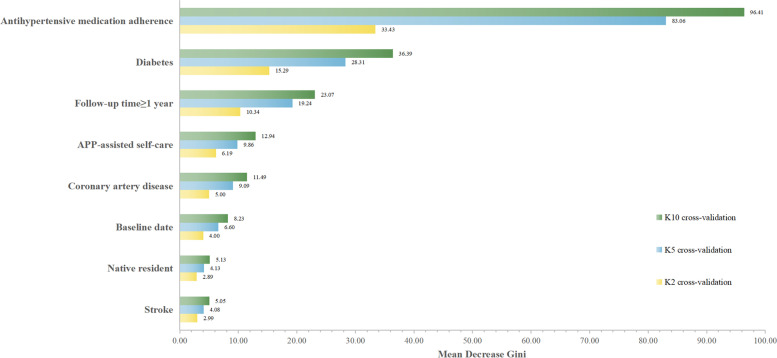
Multivariate GLM analysis implicated eight independent variables that were significantly associated with poor BP control: native resident, diabetes, coronary artery disease, stroke, baseline date, APP-assisted self-care, antihypertensive medication adherence, and follow-up time. All independent variables were then incorporated into the machine learning system, generating a predictive model of poor BP control. Te compare the performance of four algorithms were shown in Table 4 for twofold, fivefold and tenfold cross-validations. It is observed that RF-based algorithm performs better for all cross-validations compared to DT, SVB, and NB, giving the highest classification accuracy and area under the curve (AUC). Moreover, other performance parameters such as sensitivity (SE), specificity(SPE), positive predictive value(PPV), negative predictive value(NPV) for three cross-validations were also shown in Table 4. The DT was drawn to identify important factors associated with BP control (Supplement Fig. 3). Mean Decrease Gini (MDG) was calculated to rank the important predictors with poor BP control in the RF algorithm. A twofold, fivefold and tenfold cross-validation was then performed within the train set. The mean values of MDG from cross-validated results were shown in Fig. 2.
Table 4.
Performance evaluation of RF and other machine learning algorithm
| Cross-validation | Algorithm | Performance evaluation parameters | |||||
|---|---|---|---|---|---|---|---|
| ACC(%) | SE(%) | SPE(%) | PPV (%) | NPV (%) | AUC | ||
| K2 | DT | 70.12 | 42.10 | 87.52 | 67.66 | 70.86 | 0.6712 |
| SVM | 70.95 | 44.36 | 87.46 | 68.75 | 71.66 | 0.6642 | |
| NB | 66.33 | 45.00 | 79.60 | 57.83 | 69.95 | 0.6874 | |
| RF | 71.03 | 34.88 | 91.01 | 70.88 | 69.20 | 0.7291 | |
| K5 | DT | 70.14 | 42.09 | 87.50 | 67.57 | 70.89 | 0.6788 |
| SVM | 70.96 | 44.46 | 87.46 | 68.77 | 71.71 | 0.6601 | |
| NB | 66.32 | 44.99 | 79.56 | 57.79 | 69.93 | 0.6885 | |
| RF | 71.96 | 35.35 | 91.03 | 71.45 | 69.31 | 0.7316 | |
| K10 | DT | 70.11 | 42.11 | 87.56 | 67.76 | 70.90 | 0.6686 |
| SVM | 70.94 | 44.45 | 87.43 | 68.78 | 71.68 | 0.6619 | |
| NB | 70.92 | 44.40 | 87.46 | 68.83 | 71.64 | 0.6774 | |
| RF | 71.37 | 33.53 | 91.63 | 71.34 | 68.91 | 0.7286 | |
Abbreviation: DT Decision tree, SVM Support Vector Machine, NB Naïve Bayes, RF Random forest, ACC Accuracy, SE Sensitivity, SPE Specificity, PPV Positive predictive value, NPV Negative predictive value, AUC Area under the curve, K2 Twofold cross-validation, K5 Fivefold cross-validation, K10 Tenfold cross-validation
Fig. 2.
The importance of predictors for poor BP control in random forest algorithm
Discussion
This community-based cohort study was to examine the effectiveness of community healthcare in controlling BP and to investigate the role of mobile APP-assisted self-care. Compared with baseline, the community management resulted in mean SBP and DBP reductions of 4.6 mmHg and 3.5 mmHg. There were 61.6% hypertensive patients with good BP control, increasing from 55.0% in 2014 to 75.0% in 2021. After adjusting for covariates, common predictors in GLM models and machine learning algorithm revealed that antihypertensive medication adherence, diabetes, and APP-assisted self-care were associated with BP control. Overall, the APP-assisted self-care would be helpful for the management of hypertensive patients in a Beijing community.
The results of this study were similar to other cohort studies, confirmed the importance of compliance management in the antihypertensive treatment [19, 20], and the unsatisfied hypertension control in treated patients with chronic disease history such as diabetes [20, 21], coronary artery disease [20, 21], and stroke [21]. Moreover, our results further confirmed the effect of APP-assisted self-care model with the guidance of general practitioners when compared to previous studies reporting self-management on hypertensive patients in other counties [9–13]. One strength of our study is the large population-based sample in a Chinese community. To date, only a few studies [14–16] concerning self-management for BP control have been reported in China, but most of them were small sample size, investigator initiated cross-sectional survey [14] or intervention study [15], which are insufficient to address the huge burden of hypertension.
In recent years, community-based family-doctor-contracted services have been put into practice in many cities in China, such as Shanghai [22] and Beijing [17]. Research in Shanghai [22] revealed the self-management might help to achieve greater control of noncommunicable diseases. The advantage of IFOCM program in Beijing is that it initiated by a government for long-term continuous and comprehensive management of hypertensive patients [17]. This patient-centered healthcare model similar to home-based primary care practices reported in the United States [23–25]. In the IFOCM, hypertensive patient needs to be provided periodic follow-up and continuity of BP management, which is essential to improve hypertension awareness, treatment and control. The emergence of mobile health makes it more convenient for community health service to provide healthcare and disease management. The advantage of APP in IFOCM program is that patients can easily access to APP from the community WeChat official account, without download from any other APP stores and regular update. On the online platform, patients can check own health record,medical report,physiological data such as BP level, glucose level and body weight, and interactive with contracted family doctor (Fig. 1). In the present cohort study, we provided a mobile APP-assisted self-care model for community hypertension patients in Beijing, China, which lowered patients’ BP level and improve the BP control rate at follow-up. This model could serve as a good example for managing hypertensive patients registered in other community health services, especially in those with limited family doctors or general practitioners. Future work should apply applications of mobile Health for the control of other chronic diseases in community settings.
This study had several limitations. First, there were 50.7% of baseline hypertensive patients not participated in IFOCM program and failed to attend the follow-up survey in the present study. Therefore, a selection bias may exist. Second, although we adjusted all measured covariates when performing analysis, there were still unmeasured covariates, such as the number of antihypertensive drugs, what kind of drug prescribed to BP control, the primary IFOCM system could not access to outpatient records for the present, thus confounding bias cannot be avoided in the statistic analysis. Third, this was a single center study in community health service, multicenter study with long-term follow-up is needed to further examine the effect of App-assisted self-care in community hypertension management.
Conclusion
In summary, this study found that antihypertensive medication adherence, diabetes, and APP-assisted self-care were associated with follow-up BP level and BP control rate. The APP-assisted self-care succeeded in the management of hypertensive patients in a Beijing community.
Supplementary Information
Additional file 1: SFigure 1 Study flow chart.
Additional file 2: SFigure 2 Overall BP control rate of new diagnosed cases in community.
Additional file 3: SFigure 3 Predictive decision tree model of poor BP control in hypertensive patients
Additional file 4: Stable. Baseline information of hypertensive patients participated or not participated in the IFOCM program (N=12050).
Acknowledgements
We would like to thank the colleagues who supported our study in community, and all participants for taking part in the present study.
Abbreviations
- IFOCM
Intelligent family physician-optimised collaborative model
- BP
Blood pressure
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- BMI
Body mass index
- RF
Random forest
- DT
Decision tree
- SVM
Support vector machine
- NB
Naïve Bayes
- SD
Standard deviation
- OR
Odds ratio
- GLM
Generalized linear model
- MDG
Mean Decrease Gini
- AUC
Area under the curve
- SE
Sensitivity
- SPE
Specificity
- PPV
Positive predictive value
- NPV
Negative predictive value
Authors’ contributions
Conceptualization, Yousheng Qi and Weimin Li; Data collection, Fang Xing, Nan Xia, Suolei Zhang, Jinfeng Yin, Liyi Qin, Chendi Zhu, Qing Gao, Junnan Jia and Yuesong Zhao; Formal analysis, Yijia Guo; Funding acquisition, Weimin Li; Methodology, Yijia Guo and Weimin Li; Project administration, Fang Xing and Yousheng Qi; Data Supervision, Yousheng Qi; Writing-original draft, Fang Xing and Yijia Guo; Writing-review & editing, Fang Xing, Yijia Guo, Nan Xia, Suolei Zhang,Jinfeng Yin, Liyi Qin, Chendi Zhu, Qing Gao, Junnan Jia, Yuesong Zhao, Yousheng Qi and Weimin Li. The author(s) read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (U1903118). The funding organization had no role in the design, conduct, analysis and interpretation or preparation of this study.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to local policy but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Informed consent was obtained from all subjects and/or their legal guardian, and analysis was performed using deidentified data. All methods were carried out in accordance with relevant guidelines and regulations.The study protocol was approved by the ethics committee of Heyi community health service center, Beijing,China.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fang Xing and Yijia Guo contributed equally to this work and should be considered as joint first authors.
Contributor Information
Yousheng Qi, Email: tyyysqb@126.com.
Weimin Li, Email: 1711362459@qq.com.
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, Diaz R, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 3.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Executive summary: heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 4.He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, Wang J, Chen CS, Chen J, Wildman RP, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 5.Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study. Lancet. 2017;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 6.Writing Group of 2018 Chinese Guidelines for the Management of Hypertension 2018 Chinese guidelines for the management of hypertension [in Chinese] Chin J Cardiol. 2019;24(01):24–56. [Google Scholar]
- 7.Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, Shao L, Tian Y, Dong Y, Zheng C, et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 8.Hesketh T, Zhou X. Hypertension in China: the gap between policy and practice. Lancet. 2017;390(10112):2529–2530. doi: 10.1016/S0140-6736(17)32743-5. [DOI] [PubMed] [Google Scholar]
- 9.McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, Jones MI, Jowett S, Little P, Penaloza C, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799–808. doi: 10.1001/jama.2014.10057. [DOI] [PubMed] [Google Scholar]
- 10.Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, Earle K, George J, Godwin M, Green BB, et al. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. doi: 10.1371/journal.pmed.1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310(1):46–56. doi: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J, Bradburn P, Farmer A, Grant S, Greenfield SM, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391(10124):949–959. doi: 10.1016/S0140-6736(18)30309-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson AJ, Singh K, Myint UK, Grant RW, Jethwani K, Murachver E, Harris K, Lee TH, Kvedar JC. Evaluating a web-based self-management program for employees with hypertension and prehypertension: a randomized clinical trial. Am Heart J. 2012;164(4):625–631. doi: 10.1016/10.1016/j.ahj.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Qu Z, Parry M, Liu F, Wen X, Li J, Zhang Y, Wang D, Li X. Self-management and blood pressure control in China: a community-based multicentre cross-sectional study. BMJ Open. 2019;9(3):e025819. doi: 10.1136/bmjopen-2018-025819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Li T, Chen J, Xie Y, An X, Lv Y, Lin A. A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China. A Cluster-Randomized Controlled Trial. Int J Environ Res Public Health. 2019;16(21):4058. doi: 10.3390/ijerph16214058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang X, Liao H, Shi D, Li X, Chen X, He S. Cost-effectiveness analysis of different hypertension management strategies in a community setting. Intern Emerg Med. 2020;15(2):241–250. doi: 10.1007/s11739-019-02146-9. [DOI] [PubMed] [Google Scholar]
- 17.Li D, Wei X, Wu H, Liu X, Ge C, Gao W. Effect of an intelligent family physician-optimised coordination model program on hypertension management in a Beijing community. Aust J Prim Health. 2020;26(5):402–409. doi: 10.1071/PY19218. [DOI] [PubMed] [Google Scholar]
- 18.Fernandez-Lozano C, Hervella P, Mato-Abad V, Rodríguez-Yáñez M, Suárez-Garaboa S, López-Dequidt I, Estany-Gestal A, Sobrino T, Campos F, Castillo J, et al. Random forest-based prediction of stroke outcome. Sci Rep. 2021;11(1):10071. doi: 10.1038/s41598-021-89434-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu W, Goldberg SI, Shubina M, Turchin A. Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study. BMJ. 2015;350:h158. doi: 10.1136/bmj.h158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang X, Zhong H, Xiao L. The effect of community hypertension management on blood pressure control and its determinants in southwest China. Int Health. 2020;12(3):203–212. doi: 10.1136/10.1093/inthealth/ihaa002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gu J, Zhang XJ, Wang TH, Zhang Y, Chen Q. Hypertension knowledge, awareness, and self-management behaviors affect hypertension control: a community-based study in Xuhui District, Shanghai. China Cardiology. 2014;127(2):96–104. doi: 10.1159/000355576. [DOI] [PubMed] [Google Scholar]
- 22.Leff B, Weston CM, Garrigues S, Patel K, Ritchie C. Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc. 2015;63(5):963–969. doi: 10.1111/jgs.13382. [DOI] [PubMed] [Google Scholar]
- 23.Tayloe DT., Jr Patient-Centered Medical Homes in 2016. N C Med J. 2016;77(4):279–282. doi: 10.18043/ncm.77.4.279. [DOI] [PubMed] [Google Scholar]
- 24.Shi L, Lee DC, Chung M, Liang H, Lock D, Sripipatana A. Patient-Centered Medical Home Recognition and Clinical Performance in U.S. Community Health Centers. Health Serv Res. 2017;52(3):984–1004. doi: 10.1111/1475-6773.12523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang J, Zhang T, Wang L, Guo D, Liu S, Lu W, Liang H, Zhang Y, Liu C. The effect of family doctor-contracted services on noncommunicable disease self-management in Shanghai. China Int J Health Plann Manage. 2019;34(3):935–946. doi: 10.1002/hpm.2865. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: SFigure 1 Study flow chart.
Additional file 2: SFigure 2 Overall BP control rate of new diagnosed cases in community.
Additional file 3: SFigure 3 Predictive decision tree model of poor BP control in hypertensive patients
Additional file 4: Stable. Baseline information of hypertensive patients participated or not participated in the IFOCM program (N=12050).
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to local policy but are available from the corresponding author on reasonable request.