SUMMARY
A 59-year-old woman with follicular thyroid carcinoma underwent total thyroidectomy followed by radioiodine treatment. Following treatment, the whole-body scan did not show any abnormal radioiodine uptake. However, during the follow-up, the serum thyroglobulin (Tg) value increased without detectable thyroglobulin-antibodies. We performed a Ga-68 DOTA-TATE PET/CT showing a sternal lesion and several lung nodules with high somatostatin receptor density. Also, on the next day, FDG PET/CT was performed, which confirmed the findings. Considering the high levels of somatostatin receptor expression in such metastases, we planned lu177 DOTA-TATE therapy. After two cycles of lu177 DOTA-TATE injection, serum thyroglobulin significantly dropped, and she claimed that her sternal pain and dyspnea were much better. This was the case of a patient suffering from iodine-refractory follicular thyroid carcinoma, with somatostatin-receptor expression, treated with 177Lu-DOTA-TATE, showing a significant response.
INTRODUCTION
The term differentiated thyroid carcinoma (DTC) encompasses papillary, follicular, and hurtle cell carcinomas of the thyroid ( 1 ). Medullary thyroid carcinoma is not included in this term. DTCs generally show favorable outcomes when treated promptly. Surgery ± radioactive iodine ablation (RIA) is the gold standard of curative treatment ( 1 ). However, some patients may lack the ability to take up radioactive iodine or even lose this ability (previous RIA-responsive cells were destroyed, but some less differentiated cells remained and progressed) as the disease progresses ( 2 ). This diminished uptake of radioactive iodine also restricts RIA-refractory patients’ survival ( 1 ). The family of somatostatin receptors was shown to regulate thyroid cells proliferation (both normal and neoplastic tissue) ( 1 ). Additionally, multiple studies detected these receptors on thyroid tumor cells. Such features suggest potential therapeutic effects for agents like 111-In-octreotide, 90Y-DOTA-TOC, and lu177 DOTA-TATE ( 1 ). Herein, we report our experience of managing an RIA-refractory FTC with lu177 DOTA-TATE therapy, which alleviated the patient’s symptoms and decreased Tg level.
CASE REPORT
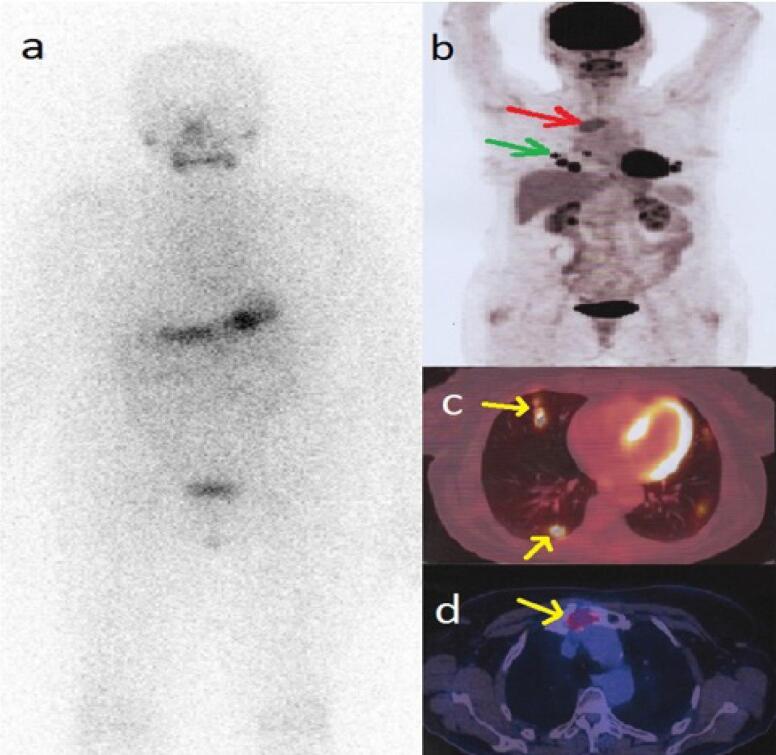
A 59-year-old woman was referred to our tertiary clinic with increased thyroglobulin (Tg) levels detected during follow-up of follicular thyroid carcinoma (FTC). She was diagnosed with FTC nine years ago (pT2N0) and treated with total thyroidectomy plus 30 millicuries (mCi) of I-131 at that point. Post-ablation whole-body iodine scan did not reveal any pathologic finding and just post surgical thyroid remnant was evident. His first serum Tg level was 0.01 ng/mL in the TSH stimulated state (serum TSH = 33); the anti-Tg antibody was absent. The neck ultrasonography was unremarkable back then. The patient had poorly adhered to her follow-up visits during that time. an empirical dose (200 mCi) of I-131 was administered, and the post-treatment scan was negative ( a ) ( Figure 1A ). On the follow-up(After 14 months), Tg level was more than 500 ng/mL with suppressed TSH. Neck ultrasonography and diagnostic I-131 scan were negative. According to the guidelines of that time and because we had just a diagnostic scan showing no iodine avidity. Rising (After 6 months) serum Tg levels (>30,000 ng/mL) were documented in the absence of anti-Tg antibody, indicating a metastatic disease. Also, the patient reported severe sternal region pain. Thus, FDG PET/CT was performed, which showed pulmonary nodules and a lytic lesion of sternal manubrium with FDG uptake ( Figures 1A-D ).
Figure 1. whole-body iodine scan ( a ) after administration of 200 mCi I-131 was negative. FDG PET/CT maximum intensity projection (MIP) ( b ) shows sternal and pulmonary metastases, which are more precisely localized on transaxial slices ( c , d ).
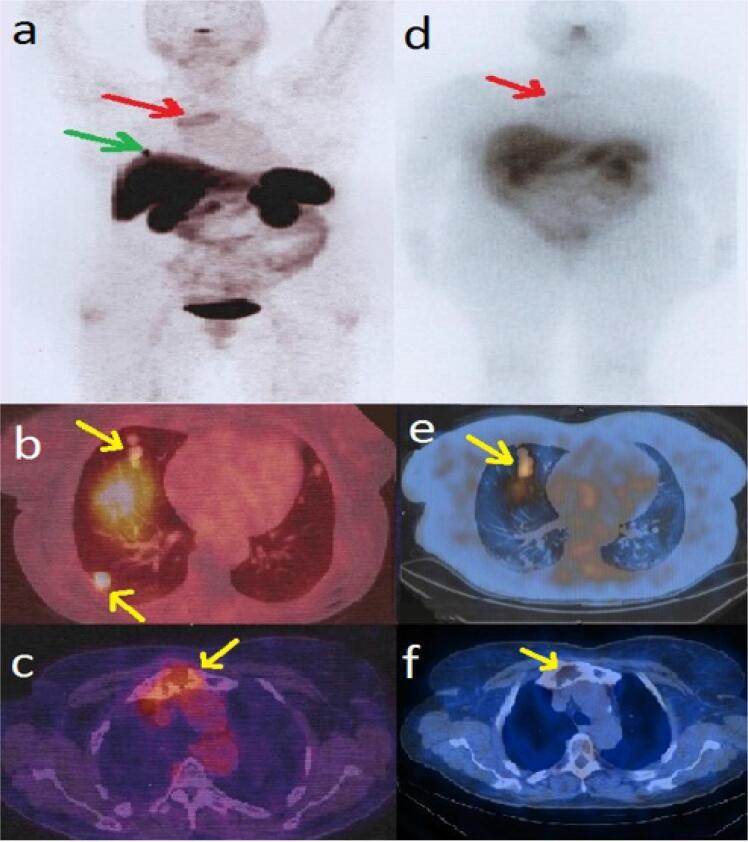
By performing Ga-68 DOTA-TATE PET/CT to evaluate somatostatin receptor avidity, we tried to give our patient a chance to be treated with somatostatin-receptor radiopharmaceuticals. It confirmed the findings of FDG PET/CT ( Figures 2A-C ). Therefore, the patient received 200 mci of lu177 DOTA-TATE, and a post-treatment whole-body scan was performed. The SPECT/CT images showed increased uptake in pulmonary nodules and tracer uptake in the margin of lytic lesion of the sternum ( Figures 2D-F ). Three months after the first cycle of lu177 DOTA-TATE therapy, blood analysis showed declined Tg level to 1,760 ng/mL and subsequently to 982 ng/mL two months after completing the second cycle. Additionally, the patient declared significant improvement of clinical symptoms.
Figure 2. Ga-68-DOTATE MIP ( a ) and PET/CT ( b, c ) confirmed the lesions detected by FDG PET/CT. Therefore, the patient received 200 mci of lu177 DOTA-TATE and performed post-treatment WBS ( d ). lu177 DOTA-TATE SPECT/CT showed increased uptake in pulmonary nodules ( e ) and uptake in the margin of lytic lesion of the sternum (f ).
DISCUSSION
We reported a case of RIA-refractory FTC that was successfully managed via lu177 DOTA-TATE. About 25%-50% of patients with locally advanced or metastatic differentiated non-medullary thyroid carcinoma (DTC) become non-responsive to RAI ( 2 , 3 ). Treatment options are limited, one of which is recently proposed as PRRT, and there are few cases in the literature performing this treatment option ( 1 , 4 - 6 ). It has been reported that this treatment produces stabilization and even partial disease remission in these patients ( 7 ). Çinkir and Elboğa conducted a clinical study on ten thyroid cancer patients to assess the efficacy of lu177 DOTA-TATE treatment after detecting the presence of somatostatin receptors via Ga-68 labeled DOTATATE PET scan. Although she included MTC patients in her study, the overall results were promising ( 8 ). They had only one FTC stage-IV patient with no metastasis or lymph node involvement who remained stable during the follow-up. Versari and cols. performed a similar study on 11 patients, but they used 90Y-DOTATOC for PRRT; they treated three patients of FTC, two of whom remained stable, and one of them experienced disease progression ( 9 ).
In contrast to these promising outcomes, Budiawan and cols. reported 16 RIA-refractory thyroid carcinoma cases, four of which were FTC. They were treated with PRRT using 90-Yttrium, or 177-Lutetium, which showed poor long-term outcomes ( 1 ). These findings are explained mainly by these studies’ variable inclusion criteria. Çinkir and Elboğa did not include metastatic patients; however, metastasis was an inclusion feature for the Budiawan study. Although lu177 DOTA-TATE significantly reduced Tg levels and improved our patient’s sternal region pain and dyspnea, further long-term studies are needed before PRRT can be established as an option in treating RAI-refractory metastatic FTC ( 8 ).
In conclusion, lu177 DOTA-TATE therapy could be an effective alternative treatment modality in patients with elevated thyroglobulin and negative iodine scan. A sufficient somatostatin receptor expression must be confirmed in diagnostic imaging modalities like Ga-68 DOTA-TATE PET/CT scan. According to our knowledge, our case is the first RIA-resistant metastatic FTC with such a dramatic response to lu177 DOTA-TATE therapy.
Footnotes
Informed consent: written informed consent was obtained from the patient to publish the mentioned results and images anonymously.
REFERENCES
- 1.Budiawan H, Salavati A, Kulkarni HR, Baum RP. Peptide receptor radionuclide therapy of treatment-refractory metastatic thyroid cancer using (90)Yttrium and (177)Lutetium labeled somatostatin analogs: toxicity, response and survival analysis. Am J Nucl Med Mol Imaging. 2014;4(1):39–52. [PMC free article] [PubMed] [Google Scholar]
- 2.Schlumberger M, Brose M, Elisei R, Leboulleux S, Luster M, Pitoia F, et al. Definition and management of radioactive iodine-refractory differentiated thyroid cancer. Lancet Diabetes Endocrinol. 2014;2(5):356–358. doi: 10.1016/S2213-8587(13)70215-8. [DOI] [PubMed] [Google Scholar]
- 3.Asioli S, Erickson LA, Righi A, Jin L, Volante M, Jenkins S, et al. Poorly differentiated carcinoma of the thyroid: validation of the Turin proposal and analysis of IMP3 expression. Mod Pathol. 2010;23(9):1269–1278. doi: 10.1038/modpathol.2010.117. [DOI] [PubMed] [Google Scholar]
- 4.Elboğa U, Özkaya M, Sayiner ZA, Çelen YZ. Lu-177 labelled peptide treatment for radioiodine refractory differentiated thyroid carcinoma. BMJ Case Rep. 2016;2016:bcr2015213627–bcr2015213627. doi: 10.1136/bcr-2015-213627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliván-Sasot P, Falgás-Lacueva M, García-Sánchez J, Vera-Pinto V, Olivas-Arroyo C, Bello-Arques P. Use of (177)Lu-dotatate in the treatment of iodine refractory thyroid carcinomas. Rev Esp Med Nucl Imagen Mol. 2017;36(2):116–119. doi: 10.1016/j.remn.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Roll W, Riemann B, Schäfers M, Stegger L, Vrachimis A. 177Lu-DOTATATE therapy in radioiodine-refractory differentiated thyroid cancer: a single center experience. Clin Nucl Med. 2018;43(10):e346–e351. doi: 10.1097/RLU.0000000000002219. [DOI] [PubMed] [Google Scholar]
- 7.Czepczyński R, Matysiak-Grześ M, Gryczyńska M, Bączyk M, Wyszomirska A, Stajgis M, et al. Peptide receptor radionuclide therapy of differentiated thyroid cancer: efficacy and toxicity. Arch Immunol Ther Exp (Warsz) 2015;63(2):147–154. doi: 10.1007/s00005-014-0318-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Çinkir HY, Elboğa U. An alternative therapy option in metastatic thyroid Cancer: peptide receptor radionuclide therapy. İstanbul Tıp Fakültesi Dergisi. 2020:111–120. [Google Scholar]
- 9.Versari A, Sollini M, Frasoldati A, Fraternali A, Filice A, Froio A, et al. Differentiated thyroid cancer: a new perspective with radiolabeled somatostatin analogues for imaging and treatment of patients. Thyroid. 2014;24(4):715–726. doi: 10.1089/thy.2013.0225. [DOI] [PubMed] [Google Scholar]