Abstract
Objectives:
The sustained subluxation or dislocation of the femoral head over time does not permit normal development of acetabulum and results in predictable pattern of acetabular growth disturbance that is termed hip dysplasia. The primary aim of this study is to analyze and quantify the volume mismatch between acetabulum and femoral head of affected side as compared to normal hip.
Methods:
A prospective observational study was conducted by including isolated untreated unilateral idiopathic developmental dysplasia of hip (DDH). After routine clinical and radiographic examination, computed tomography (CT) of both hips was done with pre-determined radiation dosage within safe limits for the pediatric age group in 18 patients of median age 2 years (range 1–5 years).
Results:
A significant difference was noted between acetabular index (p<0.001), acetabular volume (p<0.001), femoral head volume (p<0.001), and acetabular anterior sectoral angle (p=0.002) of the affected and the normal hips. As compared to the normal side, the acetabulum is 2.6 times smaller than the normal side and femoral epiphysis volume by 3.8 times. A significant negative correlation (r=−0.66, p=0.04) was noted between posterior acetabular sectoral angle and acetabular volume of affected hip.
Conclusion:
CT is an important investigation in evaluation of late-presenting DDH. The absence of femoral head in its orthotopic location affects the volume of acetabulum as well as that of femoral head. The abnormality of the volume of acetabulum which is seen as related to the dysplasia should be studied and assessed in detail in a child of late-presenting DDH. This would guide us toward the coverage defect and type of osteotomy to be performed.
Keywords: Acetabulum, developmental dysplasia of hip, upper femoral epiphysis, volume
Normal development of the hip joint requires the formation of a balanced and harmonious relationship between the growth of the acetabular and triradiate cartilages and the femoral head. Developmental dysplasia of hip (DDH) is a specific condition, in which the harmonious relationship is shattered. The sustained subluxation or dislocation of the femoral head over time does not permit normal development of the acetabulum and results in a predictable pattern of acetabular growth disturbance that is termed hip dysplasia.[1] The most important concept in the management of DDH is the reduction of the femoral head into the true acetabulum by closed or open reduction to restore this relationship.[2] Major treatment options focus on decreasing the pressure on the joint by putting femoral head in acetabular cavity.
In these patients, the degree of acetabular malformation at birth ranges from mild to severe. A ridge in the ischial and iliac portion of the acetabular cartilage, which divides the surface of the socket into two sections, is a common abnormal anatomical component that causes the Ortolani sign.[3] Without treatment, the ridge may become more prominent, and the femoral head stays dislocated in the secondary acetabulum a few weeks or months after birth. The acetabular growth plate adjoining the ilium is more oblique, and the newly developing bone at the superoposterior margin of the acetabulum appears underdeveloped.[4] These abnormalities can be corrected by subsequent growth when the femoral head has been reduced concentrically in the primary acetabulum during infancy.[5] On the other hand, when dislocation is not reduced during this period, the obliquity of the acetabular roof and distortion of the hip joint will increase, making the reduction more difficult and traumatic. It can be easily estimated that recovery of the dysplastic acetabulum is more uncertain if the dislocation has not been reduced after the child starts to walk.[6] It also has been noted in infants that reduction is difficult due to hypertrophied acetabular cartilage which reduces the volume of acetabulum.[7] These point toward the fact that the shape, size, and volume of acetabulum are dependent on the orthotopic location of the femoral proximal epiphysis inside it. The primary aim of this study is to analyze and quantify the volume mismatch between acetabulum and femoral head of the affected side as compared to the normal hip.
Methods
This study was a prospective observational cross-sectional study conducted at a tertiary level medical teaching hospital from June 2018 to May 2020. Ethical clearance was obtained from the Institutional Ethics Committee (AIIMS/IEC/19/715). The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the parents of the children enrolled in the study. All cases of isolated untreated unilateral idiopathic DDH were included in the study. Bilateral cases, previously surgically intervened, teratologic and syndromic dislocations were excluded from the study. After routine clinical and radiographic examination, computed tomography (CT) of both hips was done with pre-determined radiation dosage which are within acceptable standard limits for the pediatric age group.[8] The pelvis was placed squared with both the lower limbs parallel during the CT scan. The knees were also included for the purpose of calculation of femur anteversion. The images chosen were different for each femoral head and acetabulum depending on the best fit. For the femoral head, the cut with maximal volume was selected, and for the acetabulum, the cut with maximum depth of acetabulum was selected.
The parameters calculated from the CT were
Femoral head volume (Fig. 1a and b) - Multiplanar reconstruction the epiphysis at its widest area noted on coronal section was done.[9] After shading of the femoral epiphysis by pre-loaded clipping and segmentation software, 3D volume rendering was done.
Acetabular volume (Fig. 1c) - The volume of acetabulum was calculated considering acetabulum to be a partial hemisphere.[10] The formula used was V=13πh (3r2−h2), where h = depth of acetabulum and r = radius of the acetabulum at its maximum width on coronal plane.[11]
Acetabular index (Fig. 2) - It was calculated on the coronal section of hip where the acetabular opening is the widest. It is the angle between the line drawn between triradiate cartilage and lateral lip of acetabulum and the Hilgenreiner line.
Anterior acetabular sector angle (Fig. 3a) - It was measured on the axial section where the acetabulum is widest. The calculation was done between a tangential line from the triradiate cartilage to the most prominent point of the anterior acetabulum and the Hilgenreiner line.
Posterior acetabular sector angle (Fig. 3b) - It was measured on the axial section where the acetabulum is widest. The calculation was done between a tangential line from the triradiate cartilage to the most prominent point of the posterior acetabulum and the Hilgenreiner line.
Femur anteversion (Fig. 3c) - For the femoral neck axis, the slice displaying the middle of the femoral neck (on which the anterior and posterior cortices were parallel to each other) was selected. For the axis of the femoral condyles, a slice through the most prominent point of the condyles was selected. The femur anteversion was measured as the angle subtended by the femoral neck axis and the posterior bicondylar axis.
Acetabular anteversion (Fig. 3d) - It was done on the axial section where the acetabulum was widest. The angle measured between a vertical line and the line joining the anterior and posterior lips of acetabulum is the acetabular anteversion.
Figure 1.
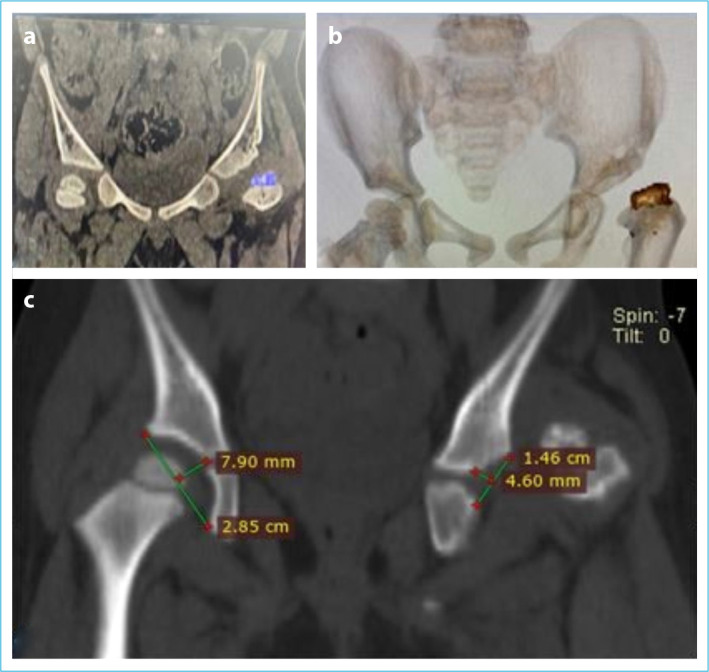
(a, b) Depiction of the head of femoral epiphysis on the affected side. (c) Measurements required for calculation of acetabular volume considering it as a partial hemisphere.
Figure 2.
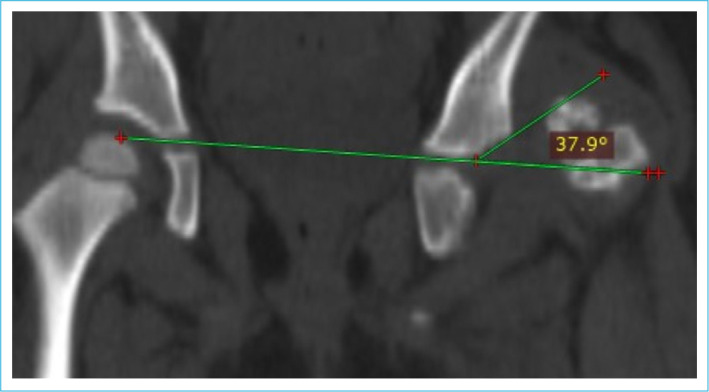
Calculation of acetabular index.
Figure 3.
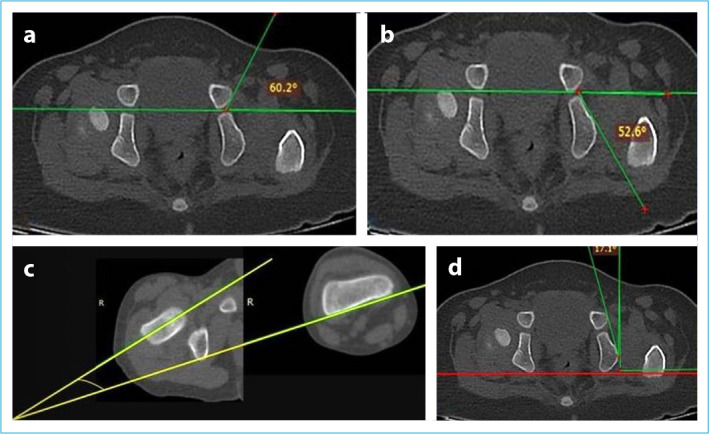
(a) Depiction of anterior acetabular sectoral angle. (b) Depiction of posterior acetabular sectoral angle. (c) Depiction of femoral anteversion. (d) Depiction of acetabular anteversion.
Statistical Analysis
The data were entered into MS Excel 2010 version for Windows. Data were analyzed using SPSS 23.0 version for Windows (IBM, New York, USA). All of the parameters were assessed for normality of distribution with the help of Shapiro–Wilk test. Non-parametric data were expressed in terms of median and interquartile range (IQR), while parametric data were expressed by mean and standard deviation. Correlation between parameters was assessed with Kendall’s tau correlation for non-parametric data. Association between parameters of affected and normal hips was established with Mann–Whitney U-test. A linear regression was established to assess the effect of all the radiological parameters on acetabular volume. Significance level was set at p<0.05.
Results
A total of 18 patients with median age of 2 years (IQR: 3, range 1–5 years) were found eligible for the study. Among these, 14 patients were female. There were 11 patients with the left-sided DDH and seven patients with the right-sided DDH. A significant difference was noted between acetabular index (p<0.001), acetabular volume (p<0.001), and femoral head volume (p<0.001) of the affected and the normal hips (Table 1). As compared to the normal side, the acetabulum is 2.6 times smaller than the normal side and femoral epiphysis volume by 3.8 times (Fig. 4). The acetabular anterior sectoral angle was found to be significantly different between affected and normal hip (p=0.002). However, there was no difference between posterior sectoral angle of affected and normal hip (p=0.28). Although the acetabular anteversion in affected hips did not change significantly (p=0.53) from the normal hips, the femoral anteversion showed a statistically significant difference (increased anteversion in affected hips, p=0.04) between the two.
Table 1.
The descriptive statistics of all acetabular parameters and femoral parameters
| Median | IQR | 95% CI | Range | Variance | p | |
|---|---|---|---|---|---|---|
| Age in years | 2 | 3 | 1.47–3.52 | 1–5 | 2.05 | |
| Affected acetabular volume (cm3) | 1.9 | 2.1 | 1.4–3.2 | 0.9–4.8 | 1.59 | <0.05 |
| Normal acetabular volume (cm3) | 5.15 | 2.1 | 4.07–6.7 | 2.6–9.1 | 3.43 | |
| Affected side AI | 33.5 | 7 | 29.8–36.6 | 26–41 | 22.6 | <0.05 |
| Normal side AI | 22.5 | 3 | 21.3–23.5 | 20–24 | 2.2 | |
| Affected acetabular anterior sectoral angle | 79 | 7.4 | 72.7–88.04 | 65–108 | 124.7 | <0.05 |
| Normal acetabular anterior sectoral angle | 72 | 5.8 | 66.8–74.1 | 60–76 | 25.88 | |
| Affected acetabular posterior sectoral angle | 59 | 11.4 | 51.01–61.08 | 42.6–64.1 | 49.5 | >0.05 |
| Normal acetabular posterior sectoral angle | 61.05 | 12 | 49.6–67.6 | 27–70 | 158.1 | |
| Affected acetabular anteversion | 20.2 | 8.1 | 14.53–22.44 | 7–26 | 30.49 | >0.05 |
| Normal acetabular anteversion | 18.6 | 10.6 | 12.45–21.1 | 7–25 | 36.5 | |
| Affected femoral head volume (cm3) | 5.1 | 5.74 | 2.75–7.5 | 0–9.9 | 11.02 | <0.05 |
| Normal femoral head volume (cm3) | 12.95 | 6.1 | 10.46–16.19 | 8.2–20.7 | 16.08 | |
| Affected femoral anteversion | 62.5 | 36.7 | 43.9–68.7 | 30–75 | 300.11 | <0.05 |
| Normal femoral anteversion | 36 | 25 | 26.17–50.63 | 19–25 | 292.4 |
IQR: Interquartile range, CI: Confidence interval, AI: Acetabular index.
Figure 4.
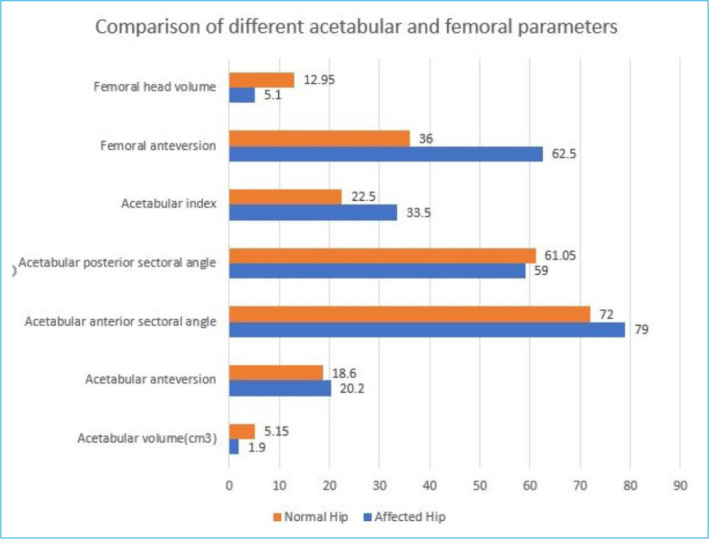
Comparison of different acetabular and femoral parameters between affected and normal hips.
A significant negative correlation (r=−0.66, p=0.04) was noted between posterior acetabular sectoral angle and acetabular volume of affected hip (Fig. 5). However, there was no significant correlation between acetabular volume and any other acetabular or femoral parameters (Table 2). Similarly, femoral head volume was found not to be correlating with any of the femoral head or acetabular parameters. A linear regression was performed to establish which of these parameters influenced the acetabular volume of the affected hip. Affected acetabular volume was found to be significantly influenced by acetabular posterior sectoral angle (R2 = 0.45, p=0.04). Acetabular volume of affected hip was not found to be influenced by affected femoral head volume (R2 = 0.31, p=0.09), affected acetabular index (R2 = 0.09, p=0.38), affected acetabular anterior sectoral angle (R2 = 0.13, p=0.3), affected acetabular anteversion (R2 = 0.15, p=0.25), or affected femoral anteversion (R2 = 0.002, p=0.89).
Figure 5.
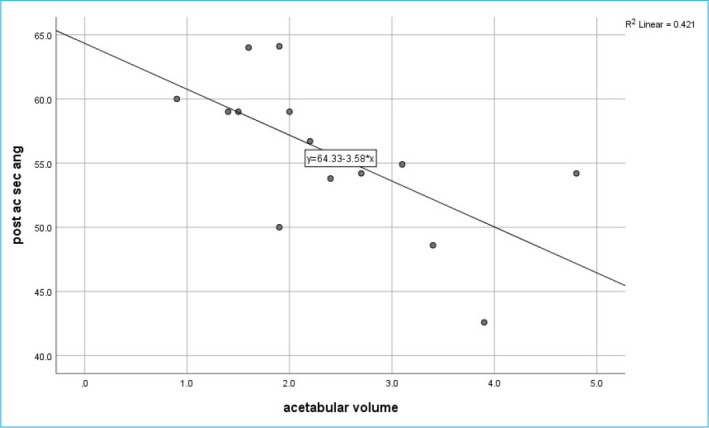
Scatter plot showing negative correlation between acetabular volume and acetabular posterior sectoral angle of affected hip.
Table 2.
Correlation between acetabular and femoral parameters of affected hip
| Affected hip AI | Affected hip ASA | Affected hip PSA | Affected AAV | Affected FAV | Affected FHV | Affected AV | |
|---|---|---|---|---|---|---|---|
| Affected femoral head volume | |||||||
| r | 0.175 | −0.181 | −0.434 | −0.108 | −0.046 | 1 | 0.559 |
| p | 0.63 | 0.62 | 0.21 | 0.76 | 0.89 | 0.09 | |
| Affected acetabular volume | |||||||
| r | 0.306 | −0.359 | −0.66 | −0.549 | −0.423 | 0.559 | 1 |
| p | 0.39 | 0.3 | 0.04 | 0.1 | 0.22 | 0.09 |
r: Correlation coefficient, AI: Acetabular index, ASA: Anterior sectoral angle, PSA: Posterior sectoral angle, AAV: Acetabular anteversion, FAV: Femoral anteversion, FHV: Femoral head volume, AV: Acetabular volume.
Discussion
The growth of acetabular height and width depends on the interstitial growth of the triradiate cartilage.[10] Growth in depth and the construction of the final acetabular shape, however, heavily depend on the interaction with a spherical femoral head which should be orthotopic its location. Even a frank dislocation, left untreated, does not prevent a child from walking, is a known fact. The typical lurch in an untreated DDH child is a tell-tale evidence of this fact. The altered biomechanics in such a hip where the femoral head is subjected to weight-bearing stresses but the empty acetabulum does not get the requisite stresses for growth adds to the poorer development of the acetabulum. The femoral head is also smaller as compared to the normal hip, since the counter stresses generated by a congruent acetabulum on its surfaces are absent. It wobbles freely in the soft tissues on the gluteal region, at times reaching the dorsum ilii to form a false acetabulum. All in all, both the head and the developing acetabulum are at a disadvantage for having the normal stresses for growth; yet the acetabulum is far more at a disadvantage since it does not have independent provision of having the weight-bearing forces directed to it in the absence of an orthotopic femoral head.[12]
When the femoral heads in growing rats were excised or dislocated, Harrison found that the acetabular socket failed to develop in depth and there were atrophy and degeneration of the articular cartilage, while the triradiate cartilage remained histologically normal.[13] The acetabulum requires the spherical femoral head as a template about which it forms. In fact, the condition of proximal focal femoral deficiency punctuates the interplay between the developing femoral head and the developing acetabulum. Presence in part of the proximal femur allows development of an acetabulum. Complete absence of the proximal femur yields an absent acetabulum.[14]
The normal development of the acetabulum is dependent on the orthotopic location of the femoral epiphysis within it and the stresses of weight bearing that pass through it. Patients with frank dislocation have been noted to have frank progressive dysplasia. Dysplasia does not resolve completely in patients if untreated even after 6 months of life.[15] This persistent dysplasia and alteration of acetabular volume is present simultaneously. Since this study only assessed the preoperative parameters, it is difficult to ascertain which the cause is and which the effect is or whether they mean the same. This is one of the first studies where the authors have tried to quantify the acetabular and femoral epiphysis volume and how it is altered from the normal side.
Treatment of late-presenting DDH is an enigma with many unpredictable prognoses. These patients have a poorer outcome as compared to early presenting DDH before 6 months of age due to increased redislocation rates as well as failure to correct the acetabular dysplasia completely. As per the current literature, open reduction with pelvic and/or femoral osteotomies is currently the treatment of choice.[16] There is currently no uniformity regarding its treatment all over the world and doubts over what kind of pelvic osteotomy should be done for best outcome are still being debated. The rates of reoperation following index open surgeries can be as high as 74%.[17] This is usually due to associated morphological bony abnormalities of the acetabulum and femoral epiphysis.[18] The high rates of failure in late-presenting children have focused more on the technical and surgical aspects of the procedure. However, the consistent poor results of these groups of patients from all over the world may be a pointer to a cause which has been hitherto not studied. The authors of this study believe that acetabular and femoral epiphysis volume are important surrogate markers which can help surgeons to treat as well as prognosticate these patients in a much more scientific way. Hence, this study was outlined so as to study the above factors in late-presenting DDH.
This study showed a significant difference between the absolute volumes of the acetabulum and femoral epiphysis of the affected and normal side. The results, although, did not show any significant difference between the femur epiphysis volume to acetabular volume ratio. They remain proportionate to each other, whether it is the affected side or normal side. This means, the volume, which, in turn, affects the stability of the reduction and residual dysplasia, is dependent on both acetabulum and femoral head. These values tend to be normal only when femoral epiphysis is in the orthotopic location inside the acetabulum. Whether these values move toward normalcy after reduction needs to be seen in the future studies evaluating these parameters post-reduction. It was also seen in this study that posterior acetabular sectoral angle is the single most important factor among other parameters affecting the acetabular volume. This important finding should lead to us treat DDH as a global undercoverage entity rather than an anterior undercoverage as has been historically propagated. Hence, advanced imaging techniques like CT should become the norm in evaluation of patients of DDH who present in walking age and osteotomies carried out accordingly to treat the dysplasia. This clinical implication of the present study cannot be understated. The incidence of failed index surgery, leading to posterior dislocation of hip can be minimized by studying the acetabular volume as well as sectoral angles, the posterior one more specifically. Femur anteversion was significantly increased in the affected side in the patients. Numerous studies have favored as well as have been ambivalent regarding the need for femoral derotation surgery at index surgery.[18]
This study is not without its share of limitations and strengths. It is limited by its small sample size which may be inadequate for postulating a definite recommendation considering the prevalence rate of DDH. The CT evaluation only assessed the bony evaluation but the presence of articular cartilage may also influence the results which has not been assessed here. This thesis was initially meant to be prospective longitudinal study to compare the studied parameters pre- and post-reduction which could not be done due to the unfortunate advent of the pandemic. The correlation obtained between the posterior acetabular sector angle and the acetabular volume should also be tested in a study with larger sample size and including participants of older age. Nevertheless, this is one of the first few studies assessing the acetabular and femoral epiphysis volume and the factors affecting it. This study helps us to understand the coverage defects in DDH in a much better way. This understanding may also help the surgeons in reducing the complications other than redislocation like avascular necrosis.
Conclusion
CT is one of the re-emerging and important investigations in evaluation of DDH. The absence of femoral head in its orthotopic location affects the volume of acetabulum as well as that of femoral head. The abnormality of the volume of acetabulum which is seen as related to the dysplasia should be studied and assessed in detail in a child of late form DDH. This would guide us toward the coverage defect and type of osteotomy to be performed.
Disclosures
Ethics Committee Approval:
Ethical clearance was obtained from the Institutional Ethics Committee (AIIMS/IEC/19/715). The study was conducted in accordance with the Declaration of Helsinki.
Peer-review:
Externally peer-reviewed.
Conflict of Interest:
None declared.
Authorship Contributions
Concept – S.S.A., V.S.; Design – S.B., V.S., S.S.A.; Supervision – V.S., S.S.A., U.C.; Materials – S.B., K.G., S.C.; Data collection &/or processing – S.B., K.G., S.C.; Analysis and/or interpretation – S.P., S.B.; Literature search – S.B., S.P., S.C.; Writing – S.B., V.S., S.S.A.; Critical Review – V.S., S.S.A.; Critical review – V.S., S.S.A.
References
- 1.Keller MS, Nijs ELF, Applegate KE. Developmental dysplasia of the hip. In: Medina LS, Applegate KE, Blackmore CC, editors. Evidence-Based Imaging in Pediatrics. New York, NY: Springer; 2010. pp. 295–309. [Google Scholar]
- 2.Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop. 1994;14:3–8. doi: 10.1097/01241398-199401000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Guarniero R. Dysplasia of hip development: update. Rev Bras Ortop. 2015;45:116–21. doi: 10.1016/S2255-4971(15)30279-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HT, Wenger DR. The morphology of residual acetabular deficiency in childhood hip dysplasia: three-dimensional computed tomographic analysis. J Pediatr Orthop. 1997;17:637–47. doi: 10.1097/00004694-199709000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Vaquero-Picado A, González-Morán G, Garay EG, Moraleda L. Developmental dysplasia of the hip: update of management. EFORT Open Rev. 2019;4:548–56. doi: 10.1302/2058-5241.4.180019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moseley CF. Developmental hip dysplasia and dislocation: management of the older child. Instr Course Lect. 2001;50:547–53. [PubMed] [Google Scholar]
- 7.Tréguier C, Baud C, Ferry M, Ferran JL, Darnault P, Chapuis M, et al. Irreducible developmental dysplasia of the hip due to acetabular roof cartilage hypertrophy. Diagnostic sonography in 15 hips. Orthop Traumatol Surg Res. 2011;97:629–33. doi: 10.1016/j.otsr.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Starr V, Ha BY. Imaging update on developmental dysplasia of the hip with the role of MRI. AJR Am J Roentgenol. 2014;203:1324–35. doi: 10.2214/AJR.13.12449. [DOI] [PubMed] [Google Scholar]
- 9.Magu NK, Magu S, Rohilla RK, Batra A, Jaipuria A, Singh A. Computed tomographic evaluation of the proximal femur: A predictive classification in displaced femoral neck fracture management. Indian J Orthop. 2014;48:476–83. doi: 10.4103/0019-5413.139857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vandenbussche E, Saffarini M, Taillieu F, Mutschler C. The asymmetric profile of the acetabulum. Clin Orthop Relat Res. 2008;466:417–23. doi: 10.1007/s11999-007-0062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volume of a partial hemisphere Calculator High accuracy calculation for life or science. Available at https://keisan.casio.com/exec/system/1223391859 Accessed Oct 19, 2020.
- 12.Ferrer-Torrelles M, Ceballos T, Ferrer-Loewinsohn A. Development of the hip joint in relation to congenital dislocation. Acta Orthop Belg. 1990;56:13–22. [PubMed] [Google Scholar]
- 13.Harrison TJ. The influence of the femoral head on pelvic growth and acetabular form in the rat. J Anat. 1961;95:12–24. [PMC free article] [PubMed] [Google Scholar]
- 14.Strayer LM., Jr Embryology of he human hip joint. Clin Orthop Relat Res. 1971;74:221–40. [PubMed] [Google Scholar]
- 15.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg. 2001;9:401–11. doi: 10.5435/00124635-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Ye W, Xu L, Li L, Zhu W, Zheng Z. Sequential one-stage combined procedure for treating bilateral developmental hip dysplasia after walking age. J Int Med Res. 2019;47:2901–9. doi: 10.1177/0300060519848943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swarup I, Ge Y, Scher D, Sink E, Widmann R, Dodwell E. Open and closed reduction for developmental dysplasia of the hip in New York State: incidence of hip reduction and rates of subsequent surgery. JB JS Open Access. 2020;5:e0028. doi: 10.2106/JBJS.OA.19.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuhanioğlu Ü, Cicek H, Ogur HU, Seyfettinoglu F, Kapukaya A. Evaluation of late redislocation in patients who underwent open reduction and pelvic osteotomy as treament for developmental dysplasia of the hip. Hip Int. 2018;28:309–14. doi: 10.5301/hipint.5000571. [DOI] [PubMed] [Google Scholar]


