Abstract
Background:
In recent years, many studies have explored the associations among impulsivity, history of abuse, the emergence of eating disorders with episodes of binge eating (EDBE) and their severity. Nevertheless, factors associated with successful clinical outcomes of EDBE are still unknown. Our study aimed to test the hypothesis that a history of abuse is associated with unsuccessful clinical outcomes of EDBE through an effect mediated by impulsivity.
Methods:
We assessed patients older than 15 years, 3 months with EDBE at inclusion and at 1 year. Recovery was defined as the absence of eating disorders at 1 year. A mediation analysis was performed by means of structural equation modelling.
Results:
We included 186 patients in our analyses (54% bulimia nervosa, 29% anorexia nervosa binge eating/purging type and 17% binge-eating disorder); 179 (96%) were female. One-third (n = 63) of patients reported a history of abuse, and recovery was observed for 20% of the sample (n = 38). Contrary to our assumption, a history of abuse was not associated with the absence of recovery of EDBE at 1 year. Factors unfavourable for achieving recovery were anxiety disorders (odds ratio [OR] 0.41), vomiting (OR 0.39), physical hyperactivity (OR 0.29), negative urgency and a lack of perseverance (OR 0.85 for both). Only positive urgency was positively associated with recovery (OR 1.25).
Limitations:
We excluded 219 patients lost to the 1-year follow-up.
Conclusion:
Our findings may help to deconstruct the empirical belief that traumatic events may interfere with the successful course of treatment for eating disorders. A high level of positive urgency may be associated with more receptivity to care.
Introduction
Eating disorders with episodes of binge eating (EDBE) include anorexia nervosa binge eating/purging type (AN-BP), bulimia nervosa, and binge-eating disorder. All are characterized by recurrent episodes of binge eating, defined as the consumption of large amounts of food in a discrete period of time with a sense of a lack of control.1
In recent years, many studies have explored the association between impulsivity and eating disorders, especially when episodes of binge eating are present.2–5 Impulsivity is defined as a predisposition to react quickly and unexpectedly in response to internal or external stimuli without regard for negative consequences for oneself or others.6 Thus, clinically, impulsivity may lead patients to make rash and imprudent decisions toward food (binge-eating episodes)7 or toward other types of impulsive behaviours, such as purging (vomiting and laxative use8), substance use disorders,9 nonsuicidal self-injury10 and suicide attempts.8
Neuropsychology research on EDBE has shown possible impairment in executive functions, especially inhibition. Patients may encounter difficulty in intentionally regulating their thinking and actions to reach primary goals.11 Inhibition corresponds to the ability to suppress inappropriate, dangerous or unrequested behaviour.11 It requires continuous monitoring and updating of actions in response to environmental changes. Lack of inhibitory control could be involved in the inability to resist binge cravings, disinhibited behaviour and loss of control during a binge-eating episode.12 A link between a response inhibition deficit and the intensity of binge-eating episodes has been established; nevertheless, poor agreement between the measure of inhibitory control and impulsivity has been reported.13 This may be explained in particular by the way impulsivity is measured; that is, by providing a global score rather than a profile of scores measuring several domains.14 However, in 2010, Dick and colleagues identified an overlap between response inhibition, measured with behavioural tasks, and the “urgency” domain of impulsivity,15 as explored with the Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency (UPPS-P) model.16 Impulsivity is conceptualized as having multiple facets, and the widely used UPPS-P model encompasses 5 different domains: emotion-based dispositions to act rashly when experiencing negative (negative urgency) or positive (positive urgency) mood; a deficit in conscientiousness, including a lack of premeditation and a lack of perseverance; and sensation seeking, described as the tendency to seek out novel experiences.17
Among the 5 domains of impulsivity, it seems that negative urgency has major importance in the initiation and maintenance of EDBE. Negative-mood-like distress is an antecedent to binge-eating episodes and increases vulnerability to binge eating and purging.18,19 Thus, the link between impulsivity (specifically urgency) and EDBE should be examined more closely.
In addition, many studies have reported an association between history of abuse and EDBE. On one hand, a history of trauma, such as emotional, physical or sexual abuse and emotional or physical neglect, is often found in patients with EDBE.20 On the other hand, a more acute symptomatology of eating disorders could be found in case of trauma. For example, Backholm and colleagues showed that traumatic exposure was associated with greater self-reported severity of eating disorder symptoms in a sample of 4524 patients with anorexia nervosa, bulimia nervosa, binge-eating disorder and eating disorders not otherwise specified as well as with greater psychosocial impairment, more psychiatric comorbidity, and more negative self-image.21 Focusing on early trauma, Guillaume and colleagues suggested that emotional abuse was linked to increased severity of all clinical features of eating disorders, while sexual and physical abuse were associated with more severe restraint, eating and shape concerns.20 If most studies found an association between history of trauma and the severity of eating disorders, only a few were interested in the effect of history of trauma on the evolution of eating disorders.
Impulsivity could mediate the effect of trauma on EDBE symptoms and course, and several conceptual models integrating childhood trauma, impulsivity and psychopathology are in line with this assumption. Muehlenkamp and colleagues found a significant pathway not only from childhood abuse through low self-esteem to body dissatisfaction, but also from childhood abuse to impulsive behaviours (nonsuicidal self-injury in their study) via psychopathology and dissociation;22 they explored impulsivity through neuroticism or nonsuicidal self-injury, but not on its own. Other authors have gone further, suggesting that a traumatic background caused, for example, by a history of sexual abuse may be at the origin of the multi-impulsivity profile found in patients with eating disorders.23 This could explain the varied symptomatology (e.g., drug use, suicide attempts, repeated nonsuicidal self-injury) of some patients with EDBE, who require adapted and multidisciplinary medical care. Some authors have even supported the assumption that multi-impulsive bulimia may represent a subtype of bulimia nervosa characterized by a history of more trauma and specific psychopathology (e.g., higher levels of anxiety and nonsuicidal self-injury).24 This triad of trauma, impulsivity and eating disorders represents an important psychological aspect to consider in the prevention and medical care of eating disorders and, more broadly, the promotion of healthy eating behaviours.7
Thus, we assumed that the traumatic context of physical or sexual abuse could generate increased impulsivity, which may worsen the clinical evolution of EDBE. The objectives of our study were twofold. The main objective was to formally test our primary working hypothesis by fitting a supposed theoretical mediation model on empirical data. The proposed model assumed that a history of abuse was a direct factor associated with EDBE recovery 1 year after the start of specialized care and an indirect factor associated with EDBE recovery at 1 year through an effect mediated by impulsivity. The secondary objective was exploratory and aimed to identify if other baseline characteristics (e.g., suicidal risk, psychiatric comorbidities, or eating disorder characteristics) could be associated with recovery at 1 year in order to generate data-driven hypotheses for future study.
Methods
Participants and procedure
The EVALuation of behavioural ADDictions (EVALADD) cohort (NCT01248767) was set up in 2008 in the Addictology and Psychiatry Department of the University Hospital of Nantes, France. The aim of EVALADD is to investigate the risk factors involved in the initiation and maintenance of behavioural addictions. Participation in the cohort is offered to all patients aged 15 years, 3 months (the legal age in France for obtaining care in the “adult” department) and older who start specialized care for their behavioural addiction. Patients with severe cognitive impairments or a poor understanding of the French language, making it difficult to complete the assessment, are not included. Patients in the EVALADD cohort participate in a face-to-face semi-structured interview conducted by qualified and experienced staff members and complete self-report questionnaires at inclusion (the start of care), 6 months, 12 months and yearly thereafter.
The first disorders explored were gambling disorder and gaming disorder. Since 2012, patients with eating disorders have also been eligible for inclusion in the EVALADD cohort. The EVALADD eating disorders cohort was specifically built to analyze the evolution of patients with eating disorders and the assessment of sociodemographic, clinical and eating disorder characteristics to take into account several factors potentially involved in the course of eating disorders. The selection of each variable has been discussed among clinicians and researchers to comply with the scientific literature while remaining acceptable for the patients.
For the present study, we collected data from the EVALADD eating disorders cohort, and we used only data collected at inclusion and 12 months. We applied supplementary inclusion criteria as follows: current diagnosis of EDBE (AN-BP, bulimia nervosa or binge-eating disorder) according to the DSM-IV/DSM-5 criteria, and having available data on the variables of interest for the mediation analysis (i.e., history of abuse at inclusion, UPPS-P questionnaire at inclusion and recovery at the 1-year follow-up).
Treatment
Our eating disorders unit is considered a National Reference Center in France, as we provide multiprofessional care based on a biopsychosocial approach to eating disorders, according to published guidelines.25–27 Several objectives are pursued: to screen for and to treat comorbidities; to restore patients to a healthy weight; to alleviate symptoms related to eating disorders, such as binge symptoms, purge strategies, dietary restriction, and distortion of body image; and to guide patients and families to functional recovery. Treatment is adapted to each patient’s situation, taking into account clinical features and the patient’s and their family’s wishes. We favour outpatient treatment, but inpatient treatment is usually delivered in cases of severe malnutrition, suicidal risk, environmental difficulties, or failure of outpatient treatment.
Measures
Sociodemographic characteristics
Sociodemographic characteristics collected at inclusion and at the 12-month follow-up assessment were age, sex, marital status and professional status.
Eating disorder characteristics
The diagnosis of eating disorders was made using the Mini International Neuropsychiatric Interview (MINI), which is a structured diagnostic interview that allows rapid and systematic investigations of the main psychiatric disorders.28 To follow nosographic evolutions, we used the fifth version of the MINI (according to DSM-IV criteria29) before 2017, then the version adapted to comply with DSM-5, which introduced new diagnostic criteria for anorexia nervosa and bulimia nervosa and added binge-eating disorder as a new type of eating disorder. Recovery at 1 year was defined as the absence of any eating disorder according to the MINI at the 12-month follow-up assessment. This follow-up period was chosen to balance between having a sufficient duration to appreciate the clinical evolution of eating disorders and the increased risk of drop-outs possible with a longer follow-up.
Eating disorder characteristics were identified using a semi-structured interview designed to fit the EVALADD cohort in a systematic and standardized way (for example, see Fauconnier and colleagues30). These characteristics, assessed by trained research staff with experience with eating disorders, were age at the beginning of eating problems (onset of problem from the point of view of the patient), eating disorder duration, current body mass index, and harmful behaviours associated with the current eating disorder. We assessed for the presence of vomiting, the use of laxative or enema, the use of appetite suppressants and nonsuicidal self-injury in the 3 months preceding study entry and, according to the DSM-5, were considered to be present if they occurred at least once a month. Potomania corresponded to water intake greater than 3 L/day. Hyperactivity was defined as performing a physical activity at least 1 hour/day at least 6 days/week for at least 4 weeks.31
Psychiatric comorbidities
Using the MINI, we assessed the presence of current or lifetime psychiatric comorbidities: mood disorders (major depressive episode [MDE], dysthymia, and [hypo]manic episodes), anxiety disorders (panic disorders, agoraphobia, social phobia, obsessive–compulsive disorder [OCD], posttraumatic stress disorder [PTSD], and generalized anxiety disorder), substance use disorderss (alcohol and other psychoactive substances, excluding nicotine) and psychotic syndrome. Mood disorders, anxiety disorders and substance use disorders were considered to be present if at least 1 of these types of disorder was diagnosed. The risk of suicide was also explored using the MINI. We used only the presence or absence of the risk, regardless of the level of risk. We opted to use only DSM-IV categorization to ensure consistency in classification. Thus, OCD and PTSD were categorized as anxiety disorders.
Impulsivity
The UPPS Impulsivity Behaviour Scale was initially developed to explore 4 dimensions of impulsivity16: urgency, lack of premeditation, lack of perseverance and sensation seeking. The UPPS-P17 is an adaptation of the original UPPS that includes 5 dimensions of impulsivity: positive urgency, negative urgency, lack of premeditation, lack of perseverance and sensation seeking. We used the UPPS-P French short version.32 Urgency refers to the tendency to feel a strong progressive impulse under a positive (positive urgency) or negative (negative urgency) effect. A lack of premeditation refers to difficulty considering the consequences of an act before committing it. A lack of perseverance refers to an individual’s inability to stay focused on a task that may be boring or difficult. Finally, sensation seeking integrates 2 aspects: a tendency to enjoy and pursue exciting activities and an eagerness for new experiences (dangerous or not). The higher the score, the more severe the impulsivity. During data collection, we switched from the UPPS to the short version of the UPPS-P. As the positive urgency score was not available in the earlier UPPS version, we excluded patients who were assessed using the UPPS from the analyses. Psychometric properties of the UPPS-P were empirically estimated both for the original English version33 and the French version.32 The short version of the UPPS-P showed adequate psychometric properties on various aspects of validity (e.g., structural validity, concurrent validity) and reliability (e.g., good internal consistency for the various subscales, strong test-retest stability). The estimated Cronbach α for our data were all above 0.70 (0.78 for negative urgency, 0.77 for positive urgency, 0.84 for lack of premeditation, 0.85 for lack of perseverance, 0.83 for sensation seeking).
History of abuse
To assess history of traumatic events, we used a revised version of the French life events questionnaire (EVE),34 which was previously used in another study involving the EVALADD cohort.35 The revised EVE questionnaire explores 6 areas: family; professional life; social life; marital and emotional life; health; and other traumatic events, which include physical and sexual abuse. For each event, the patient had to say whether it had occurred in their lifetime; whether the event was traumatic or not; and, if yes, the intensity of the trauma (scored from 0 to 10). In the present study, we used only the items referring to the occurrence of physical and/or sexual abuse to qualify the presence of a history of abuse. We considered that patients experienced a history of abuse if they reported being exposed to physical and/or sexual abuse, regardless of the subjective intensity of the related traumatic experience.
Statistical analysis
We describe baseline and outcome characteristics of the whole cohort using appropriate position and dispersion statistics.
As the main objective of this study was to formally test our primary working hypothesis — that a history of abuse could explain recovery at 1 year both directly and indirectly by impulsivity scores (mediation effects) — we could have tested its plausibility by fitting a mediation analysis model on the empirical data using structural equation modelling (SEM; “path analysis” model). However, in our data set, the occurrence of a statistical association between history of abuse and recovery at 1 year could be explored first by means of a bivariate comparison using a χ2 test. Based on our data, the null hypothesis of no association between history of abuse and recovery at 1 year against an α level at 5 % was not rejected. Therefore, the results of fitting a mediation analysis model on our data are not shown, as results would be consistent with the bivariate comparison and would not show a direct (or indirect through impulsivity) association between history of abuse and recovery at 1 year.
As our main hypothesis was not confirmed based on our data, we performed secondary exploratory analyses to determine characteristics other than a history of abuse that could be associated with EDBE recovery at 1 year. All sociodemographic, psychopathological and eating disorder characteristics were included in the bivariate comparison, as they all could potentially contribute to recovery. Bivariate comparisons of baseline factors against the presence or absence of recovery were performed using 2-sample t tests for quantitative variables and χ2 or Fisher exact tests (when appropriate) for qualitative variables. Baseline factors with a p value of the bivariate comparison < 0.05 were included in a multivariate logistic regression model as potential independent factors associated with recovery at 1 year. The selection of the final model was performed by means of a stepwise backward and forward procedure: the model with the lowest Akaike information criterion was selected as the final model. Adjusted odds ratios (ORs) were estimated using the parameters of the final model.
All statistical tests were performed against an α level of 5 %. As these secondary analyses were exploratory and only for generating data-driven hypotheses for future study, we did not adjust the family-wise error rate for multiple testing, as usually advocated for exploratory analyses in epidemiology performed on a reasonable number of characteristics, in order to avoid an excessive loss of power.36 Analyses were performed using R 4.1.0.37
Ethics
The EVALADD was conducted in accordance with the Guideline for Good Clinical Practice and the Declaration of Helsinki and with approval from our ethics committee, obtained in 2008.
Results
Patient selection
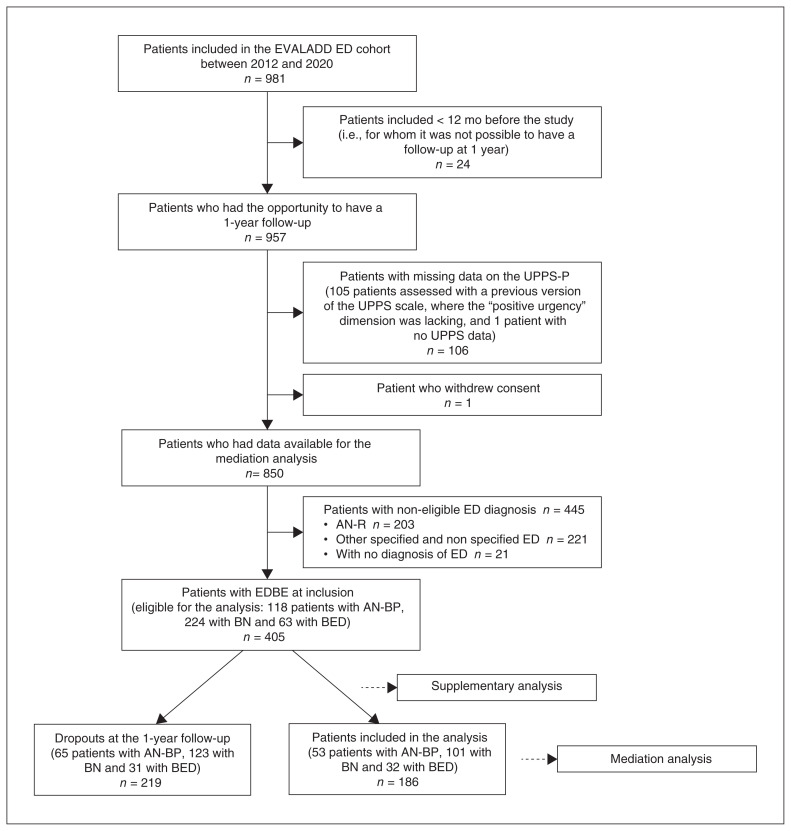
From the 981 patients included in the EVALADD eating disorders cohort between 2012 and 2020, 405 were eligible for the present study. Among them, 219 dropped out (did not attend the 1-year visit). Several features of patients who dropped out differed from those of included patients. Patients lost to follow-up were most likely to have comorbid substance use disorders and to present potomania. They also had a greater lack of perseverance on the short version of the UPPS-P scale at baseline, and a history of abuse was more frequent (46% v. 34 %) (Appendix 1, available at www.jpn.ca/lookup/doi/10.1503/jpn.210218/tab-related-content). Finally, 186 patients were included in the mediation analysis (Figure 1).
Figure 1.
Inclusion of patients in the study. AN-BP = anorexia nervosa binge-eating/purging type; AN-R = anorexia nervosa restrictive type; BED = binge-eating disorder; BN = bulimia nervosa; ED = eating disorders; EDBE = eating disorder with binge-eating episodes; EVALADD = EVALuation of behavioural ADDictions cohort; UPPS = Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking; UPPS-P = Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency (UPPS-P) Impulsive Behavior Scale.
Characteristics of the study population
The characteristics of the patients included are detailed in Table 1. Our sample had a mean age of 26.5 ± 9.9 years and was composed mostly of women (96%). Eating disorder diagnoses among the sample were bulimia nervosa (54%), AN-BP (29%) and binge-eating disorder (17%). At inclusion, mood disorders were the most common psychiatric comorbidity (86%), followed by anxiety disorders (73%). One-third of patients reported a history of abuse. Recovery from EDBE was observed at 1 year in 20% of the sample (n = 38).
Table 1.
Participant characteristics at baseline (n = 186)
| Characteristic | Mean ± SD or n (%) |
|---|---|
| Structured interview | |
| Female sex | 179 (96) |
| Age, yr | 26.5 ± 9.9 |
| Marital status: living as a couple | 44 (24) |
| Work status: in job | 65 (35) |
| Work status: student | 84 (45) |
| Past or current comorbidities (MINI) | |
| Mood disorders* | 159 (86) |
| Risk of suicide | 114 (61) |
| Anxiety disorders | 136 (73) |
| Alcohol or substance use disorders | 42 (23) |
| UPPS-P Impulsivity Behaviour Scale | |
| Negative urgency | 10.7 ± 3.0 |
| Positive urgency | 10.8 ± 2.8 |
| Lack of premeditation | 8.0 ± 2.8 |
| Lack of perseverance | 8.0 ± 2.8 |
| Sensation seeking | 10.0 ± 3.1 |
| History of abuse (EVE) | 63 (34) |
| Type of eating disorder (MINI) | |
| Bulimia nervosa | 101 (54) |
| Anorexia nervosa binge-eating/purging type | 53 (29) |
| Binge-eating disorder | 32 (17) |
| Recovery at 1 year | 38 (20) |
| Structured interview | |
| Age at onset of problem eating | 16.3 ± 6.1 |
| Eating disorder duration | 10.1 ± 9.5 |
| Current BMI† | 21.5 ± 6.0 |
| Associated behaviours | |
| Vomiting | 112 (60) |
| Physical hyperactivity | 55 (30) |
| Use of laxatives or enema | 23 (12) |
| Nonsuicidal self-injury | 20 (11) |
| Use of appetite suppressants | 17 (9) |
| Potomania | 14 (8) |
BMI = body mass index; EVE = French life event questionnaire; MINI = MINI International Neuropsychiatric Interview; SD = standard deviation; UPPS-P = Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency Impulsive Behavior Scale.
Data missing for 1 participant.
Data missing for 6 participants.
Association between history of abuse and recovery from EDBE at 1 year
In our sample, a history of abuse was observed in 32% (n = 48) of the patients who had not recovered from EDBE at 1 year compared with 39% (n = 15) of the patients who had recovered at 1 year, showing no association between history of abuse and EDBE recovery at 1 year p = 0.41; Table 2).
Table 2.
Bivariate comparisons between recovery at 1 year and sociodemographic, psychopathological and eating disorder characteristics
| Characteristic | Mean ± SD or n (%) | p value | |
|---|---|---|---|
|
| |||
| No recovery at 1 year | Recovery at 1 year | ||
| Structured interview | |||
| Female sex | 142 (96) | 37 (97) | > 0.99 |
| Age, yr | 26.8 ± 9.9 | 25.3 ± 10.0 | 0.41 |
| Marital status: living as a couple | 36 (24) | 8 (2) | 0.67 |
| Work status: in job | 56 (38) | 9 (24) | 0.24 |
| Work status: student | 63 (43) | 21 (55) | 0.24 |
| Past or current comorbidities (MINI) | |||
| Mood disorders* | 129 (87) | 30 (81) | 0.34 |
| Risk of suicide | 96 (65) | 18 (47) | 0.048 |
| Anxiety disorders | 113 (76) | 23 (60) | 0.0497 |
| Alcohol or substance use disorders | 33 (22) | 9 (24) | 0.85 |
| UPPS-P Impulsivity Behaviour Scale | |||
| Negative urgency | 10.9 ± 2.9 | 9.9 ± 3.3 | 0.01 |
| Positive urgency | 10.7 ± 2.8 | 11.3 ± 2.8 | 0.19 |
| Lack of premeditation | 8.2 ± 2.7 | 7.6 ± 3.0 | 0.28 |
| Lack of perseverance | 8.2 ± 2.8 | 7.2 ± 2.5 | 0.04 |
| Sensation seeking | 10.0 ± 3.0 | 10.1 ± 3.6 | 0.94 |
| History of abuse (EVE) | 48 (32) | 15 (39) | 0.41 |
| Type of eating disorder (MINI) | |||
| Bulimia nervosa | 82 (55) | 19 (50) | 0.02 |
| Anorexia nervosa binge-eating/purging type | 46 (31) | 7 (18) | 0.02 |
| Binge-eating disorder | 20 (14) | 12 (32) | 0.02 |
| Structured interview | |||
| Age at onset of problem eating | 16.4 ± 5.9 | 16.1 ± 7.0 | 0.80 |
| Eating disorder duration | 10.4 ± 9.4 | 9.2 ± 9.6 | 0.49 |
| Current BMI† | 21.0 ± 6.0 | 23.5 ± 5.7 | 0.02 |
| Associated behaviours | |||
| Vomiting | 96 (65) | 16 (43) | 0.01 |
| Physical hyperactivity | 50 (34) | 5 (13) | 0.01 |
| Use of laxatives or enema | 21 (14) | 2 (5) | 0.17 |
| Nonsuicidal self-injury | 17 (11) | 3 (8) | 0.77 |
| Use of appetite suppressants | 15 (10) | 2 (5) | 0.53 |
| Potomania | 11 (7) | 3 (8) | > 0.99 |
BMI = body mass index; EVE = French life event questionnaire; MINI = MINI International Neuropsychiatric Interview; SD = standard deviation; UPPS-P = Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency Impulsive Behavior Scale.
Data missing for 1 participant.
Data missing for 6 participants.
Exploration of factors associated with recovery
The secondary objective was to identify the sociodemographic, psychopathological or clinical factors (at inclusion) that were associated with EDBE recovery at 1 year. Table 2 shows the results of the bivariate comparisons, after which 8 factors were retained as potentially associated with EDBE recovery at 1 year: risk of suicide, anxiety disorder, negative urgency, lack of perseverance, type of eating disorder, current body mass index, vomiting and physical hyperactivity. As our main objective was related to the link between impulsivity and the clinical evolution of EDBE, other dimensions of impulsivity (positive urgency, a lack of premeditation and sensation seeking) were forced in the multivariate model despite being nonsignificant in bivariate analyses. Table 3 shows the results of the final model. Several factors were unfavourable to recovery from eating disorders: anxiety disorders (OR 0.41, 95% CI 0.18–0.97); purging behaviours such as vomiting (OR 0.39, 95% CI 0.17–0.85); physical hyperactivity (OR 0.29, 95% CI 0.09–0.79); and 2 dimensions of impulsivity, namely, negative urgency (OR 0.85, 95% CI 0.73–0.99) and a lack of perseverance (OR 0.85, 95% CI 0.72–0.99). Only positive urgency was positively associated with recovery (OR 1.25, 95% CI 1.06–1.49).
Table 3.
Multivariate logistic regression model of predictive factors of recovery
| Factor | OR (95% CI) | β coefficient | SE | p value |
|---|---|---|---|---|
| Intercept | — | −0.52 | 1.01 | — |
| Anxiety disorders (yes v. no) | 0.41 (0.18–0.97) | −0.89 | 0.43 | 0.04 |
| Current vomiting (yes v. no) | 0.39 (0.17–0.85) | −0.94 | 0.40 | 0.02 |
| Current hyperactivity (yes v. no) | 0.29 (0.09–0.79) | 1.25 | 0.55 | 0.02 |
| Negative urgency | 0.85 (0.73–0.99) | −0.16 | 0.08 | 0.04 |
| Positive urgency | 1.25 (1.06–1.49) | 0.22 | 0.08 | 0.01 |
| Lack of perseverance | 0.85 (0.72–0.99) | −0.17 | 0.08 | 0.04 |
CI = confidence interval; OR = odds ratio; SE = standard error.
Discussion
Our study aimed to test the hypothesis that a history of abuse is a direct factor associated with EDBE recovery 1 year after the start of specialized care and an indirect factor associated with EDBE recovery at 1 year through an effect mediated by impulsivity. To the best of our knowledge, this study is the first to look for a link between a history of abuse and EDBE recovery beyond the severity of eating disorders at a given time.20,21 In our sample, 34% of patients had a history of abuse. This rate fluctuates in the literature, especially according to the population studied, the definition of trauma/abuse, the time of data collection and the scales used for measurement (e.g., 19% traumatic lifelong events among patients with a DSM-IV eating disorde reported by Backholm and colleagues,21 and 78% and 79% of childhood trauma among patients with AN-BP and bulimia nervosa, respectively, reported by Corstorphine and coleagues23). Surprisingly, a history of abuse was not associated with EDBE recovery in our sample. This is a clinically important finding because if traumatic exposure is linked to the onset and severity of eating disorders, our results suggest that trauma does not constitute an impediment to recovery.
A patient’s life history is commonly examined during treatment for eating disorders. Thus, traumatic experiences, among others (e.g., family history of eating disorders, early menarche, childhood obesity, low self-esteem), can be a focus of therapy and considered vulnerability factors for eating disorders. In a recent study, Castellini and colleagues found a lower rate of full recovery in adult patients with anorexia nervosa and bulimia nervosa who had experienced childhood maltreatment (physical abuse, sexual abuse or parental antipathy or neglect) than among those who had not experienced childhood maltreatment (12.1% v. 31%).38 They hypothesized that patients who had experienced abuse suffered more frequently from persistent depression at 3 years. In our sample, 155 patients had an MDE at inclusion. At 1 year, more than two-thirds of these patients met the criteria for MDE, which corresponds to persistent depression, whether they had experienced abuse or not (70.7% v. 67.3%), with no significant difference between the groups (results not shown). Thus, our results do not support the assumption that depressive symptomatology could be a confounding factor for the outcomec of eating disorders in patients who have experienced abuse.
We also explored potential factors associated with EDBE recovery at 1 year. Patients with a past or current anxiety disorder (including PTSD and OCD) at inclusion were significantly less likely to achieve recovery at 1 year. Purging behaviours (vomiting and hyperactivity) were also unfavourable to recovery. Purging behaviours have not been identified as negative prognostic indicators in previous studies on the topic, and contradictory data exist about anxiety disorders;39–42 unexplored by Franko and colleagues43), specifically in EDBE. If only few studies have suggested that anxiety disorders could be associated with the course of eating disorders,42 particularly via disinhibition behaviours,41 it is well established that trait anxiety and other traits associated with both eating disorders and anxiety-like obsessionality play a role in the evolution of eating disorders.44–46 The poorer outcomes associated with comorbid anxiety disorders may be because they are more challenging to treat than other disorders. For example, compared with mood disorders (more frequent than anxiety disorders in our sample at inclusion), anxiety disorders can be harder to resolve. Clinicians make use of fewer therapeutic class options, and tolerance to pharmacotherapy can be reduced among patients with anxiety disorders compared with depressive disorders.47 Binge-eating episodes in patients with comorbid anxiety disorder can be viewed as a coping strategy.48 Thus, in the absence of more efficient coping strategies, anxiety disorders can be a worsening factor for eating disorders and an obstacle to their resolution. In addition, purging behaviours are hallmarks of more severe eating disorders and, therefore, could be associated with a slighter chance of recovery at 1 year. Finally, in the present study, we specifically focused on EDBE — not on all types of eating disorders, and not solely on bulimia — and we assessed recovery at 1 year rather than a longer-term evolution. One can assume that a history of anxiety disorders and purging behaviours could be associated with a slower EDBE recovery rather than an impediment to long-term recovery.
Although studies have highlighted the link between impulsivity and eating disorders,4,18 there is a lack of data about the link between patterns of impulsivity and the evolution of eating disorders. In our study, 3 dimensions of impulsivity were directly linked to EDBE recovery. Negative urgency, which refers to impulsive actions in negative mood contexts, and a lack of perseverance, which is defined as difficulty staying focused on a task that can be hard or boring,16 were both unfavourable for the EDBE recovery at 1 year. These results are consistent with previous research. Negative urgency has already been reported to be associated with bulimic symptoms in cross-sectional49 and prospective longitudinal50 studies and with recovery,51 especially in women who reported that eating alleviated negative affect.52 Peterson and Fischer also found that a lack of perseverance at baseline contributed significantly to binge-eating frequency at 8 months of follow-up in individuals with bulimia nervosa.50
Positive urgency, which refers to the tendency to act impulsively when experiencing intense positive affect, is a facet of impulsivity that was more recently brought to light.53 In our study, positive urgency was the only positive factor associated with recovery. While positive urgency is commonly associated with substance use disorders, in particular alcohol use disorder,53,54 some studies previously showed an increased positive urgency in eating concerns55 and in binge-eating and purging disorders,56,57 while others did not.53 To date, no data are available on the positive urgency and evolutionary pattern of eating disorders. Two main hypotheses can be proposed. First, a high level of positive urgency could reflect better reactivity to positive affect, the extent to which individuals feel enthusiastic, active, and alert.58 One can assume that these feelings are associated with personality traits such as enhanced extraversion and openness as well as lower neuroticism59 and that these traits allow more receptivity to care, contrary to consciousness and neuroticism, which are often associated with binge eating.60,61 Second, considering that impulsivity was assessed at inclusion, the association between high positive urgency and eating disorder recovery could be explained by the fact that specific care particularly targets this facet of impulsivity. In this case, patients would benefit from a wider margin of evolution than patients with high impulsivity in other domains. These patients may experience substantial healing of their global impulsiveness, which is widely associated with bulimic symptoms, thereby leading to a better chance of recovery. However, positive urgency is a quite recent construct that has not yet been sufficiently explored, and these links are only assumptions.
Limitations
Although the present study contributes to our knowledge regarding the association between a history of abuse and recovery from EDBE, it has limitations. If the main result of our study is the lack of a statistically significant association between a history of abuse and recovery at 1 year, it must be noted that statistical independence between 2 variables cannot be strictly demonstrated, as the risk of a type-II error cannot be dismissed. We had to exclude a large proportion of patients because they had no 1-year follow-up data available (either because they were lost to follow-up or to their study enrolment being too recent), which could lead to an attrition bias. Loss to follow-up could be explained either by a positive or negative evolution of a patient’s eating disorder (in the case of an improvement, patients may have not seen any benefit to a novel interview, and in the case of worsening, they may have stopped their care). In some cases, loss to follow-up could correspond to a change in residence or unavailability at the time of the scheduled visit. Supplementary analysis on patients lost to follow-up (Appendix 1) suggests that they could have had a more severe EDBE (e.g., more comorbid substance use disorders, more frequent potomania). Patients lost to follow-up were more likely to have a history of abuse than included patients (46% v. 34%), which could have biased the link between history of abuse and EDBE recovery at 1 year in our study because data were not missing at random. The only characteristic associated with the outcome that differed between patients included in our study and those who were lost to follow-up was the lack of perseverance score on the short version of the UPPS-P scale, which was higher in the loss to follow-up sample (mean 8.9 v. 8.0). This characteristic, which was slightly associated with a negative outcome in our study (OR 0.85), could indicate that patients who were lost to follow-up may have had a slightly worse prognosis. Thus, we cannot exclude the possibility of a bias of underestimation. Concerning the history of abuse, our data did not allow us to investigate the impact of the type of abuse or the age at which the abuse occurred, which may have been relevant in relation to recovery. Finally, the average duration of eating disorders (> 10 yr) and the rate of psychiatric comorbidities (86% for mood disorders and 73% for anxiety disorders) indicate that our results may be applicable only to a population of that severity. As anxiety disorders have been found to be a prognostic indicator of the outcome, the specificity of our sample might have affected results.
Nevertheless, these limitations are counterbalanced by several strengths. Our results are based on a large and representative sample of 186 patients. Sociodemographic data (96% female, mean age 26.5 yr) and clinical data (mean age of problematic eating disorders 13 yr, 29% AN-BP, 54% bulimia nervosa, 17% binge-eating disorder) are typical characteristics of patients treated for EDBE. Our study offers a longitudinal view of the evolution of eating disorders at 1 year. Moreover, we considered 3 types of eating disorders characterized by bulimic symptoms and not only AN-BP or bulimia nervosa, as in many studies. We used validated diagnostic and clinical tools and structured interviews led by trained staff, which limit the measurement bias.62
Conclusion
In our study, history of abuse was not found to be associated with EBDE recovery, either directly or indirectly by mediation of impulsivity. Our findings must be confirmed by further studies, but they could help to deconstruct the empirical belief that traumatic events could interfere with the successful course of treatment for eating disorders. Our results encourage clinicians to continue exploring life history and to link some adverse experiences to affective and cognitive conditions in eating disorders.
Whereas the distinction between negative and positive urgency has been questioned in recent work,63 the potential association between positive urgency and recovery at 1 year found in our study merits closer examination and further study. The evolution of impulsive personality traits could be a marker of the effectiveness of care in eating disorders, and prospective studies could enhance our understanding of psychological patterns of recovery. Impulsivity-targeted care could then evolve.
Supplementary Material
Footnotes
Competing interests: None declared.
Contributors: C. Cabelguen, A. Vanier, M. Laslandes, M. Grall-Bronnec and G. Challet-Bouju designed the study. C. Cabelguen, A. Saillard, J. Leboucher, M. Rousselet, E. Thiabaud and M. Grall-Bronnec acquired the data, which C. Cabelguen, A. Vanier, M. Grall-Bronnec and G. Challet-Bouju analyzed. C. Cabelguen, A. Saillard, M. Laslandes and G. Challet-Bouju wrote the article, which all authors reviewed. All authors approved the final version to be published, agree to be accountable for all aspects of the work and can certify that no other individuals not listed as authors have made substantial contributions to the paper.
References
- 1.American Psychiatric Association. DSM-5 : Diagnostic and statistical manual of mental health disorders. Fifth edition. Washington DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Claes L, Vandereycken W, Vertommen H. Impulsivity-related traits in eating disorder patients. Pers Individ Dif 2005;39:739–49. [Google Scholar]
- 3.Evans BC, Felton JW, Lagacey MA, et al. Impulsivity and affect reactivity prospectively predict disordered eating attitudes in adolescents: a 6-year longitudinal study. Eur Child Adolesc Psychiatry 2019;28:1193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fischer S, Smith GT, Anderson KG. Clarifying the role of impulsivity in bulimia nervosa. Int J Eat Disord 2003;33:406–11. [DOI] [PubMed] [Google Scholar]
- 5.Schag K, Teufel M, Junne F, et al. Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS ONE 2013;8:e76542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moeller FG, Barratt ES, Dougherty DM, et al. Psychiatric aspects of impulsivity. Am J Psychiatry 2001;158:1783–93. [DOI] [PubMed] [Google Scholar]
- 7.Bénard M, Bellisle F, Kesse-Guyot E, et al. Impulsivity is associated with food intake, snacking, and eating disorders in a general population. Am J Clin Nutr 2019;109:117–26. [DOI] [PubMed] [Google Scholar]
- 8.Favaro A, Santonastaso P. Purging behavior, suicide attempts, and psychiatric symptoms in 398 eating disordered subjects. Int J Eat Disord 1996;20:99–103. [DOI] [PubMed] [Google Scholar]
- 9.Baker JH, Mazzeo SE, Kendler KS. Association between broadly defined bulimia nervosa and drug use disorders: common genetic and environmental influences. Int J Eat Disord 2007;40:673–8. [DOI] [PubMed] [Google Scholar]
- 10.Varela-Besteiro O, Serrano-Troncoso E, Rodriguez-Vicente V, et al. Suicidal ideation and self-injurious behavior in adolescents with eating disorders. Actas Esp Psiquiatr 2017;45:157–66. [PubMed] [Google Scholar]
- 11.Sweerts SJ, Romo L. Impulsivité alimentaire et troubles du comportement alimentaire : de la neuropsychologie à la psychologie clinique. Ann Méd-Psychol Rev Psychiatr 2020;178:314–7. [Google Scholar]
- 12.Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev 2004; 28:343–51. [DOI] [PubMed] [Google Scholar]
- 13.Roberts W, Fillmore MT, Milich R. Linking impulsivity and inhibitory control using manual and oculomotor response inhibition tasks. Acta Psychol (Amst) 2011;138:419–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nigg JT. On inhibition/disinhibition in developmental psychopathology: views from cognitive and personality psychology and a working inhibition taxonomy. Psychol Bull 2000;126:220–46. [DOI] [PubMed] [Google Scholar]
- 15.Dick DM, Smith G, Olausson P, et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict Biol 2010;15:217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull 2008;134:807–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynam D, Smith G, Whiteside S, et al. The UPPS-P: assessing five personality pathways to impulsive behavior. Technical report. West Lafayette. Purdue University; 2006. [Google Scholar]
- 18.Fischer S, Smith G, Cyders M. Another look at impulsivity: a meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clin Psychol Rev 2008;28: 1413–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smyth JM, Wonderlich SA, Heron KE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol 2007;75:629–38. [DOI] [PubMed] [Google Scholar]
- 20.Guillaume S, Jaussent I, Maimoun L, et al. Associations between adverse childhood experiences and clinical characteristics of eating disorders. Sci Rep 2016;6:35761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Backholm K, Isomaa R, Birgegård A. The prevalence and impact of trauma history in eating disorder patients. Eur J Psychotraumatology 2013;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muehlenkamp JJ, Claes L, Smits D, et al. Non-suicidal self-injury in eating disordered patients: a test of a conceptual model. Psychiatry Res 2011;188:102–8. [DOI] [PubMed] [Google Scholar]
- 23.Corstorphine E, Waller G, Lawson R, et al. Trauma and multi-impulsivity in the eating disorders. Eat Behav 2007;8:23–30. [DOI] [PubMed] [Google Scholar]
- 24.Myers TC, Wonderlich SA, Crosby R, et al. Is multi-impulsive bulimia a distinct type of bulimia nervosa: psychopathology and EMA findings. Int J Eat Disord 2006;39:655–61. [DOI] [PubMed] [Google Scholar]
- 25.Haute Autorité de Santé. Anorexie mentale : Prise en charge — recommandation de bonne pratique. Available: https://www.has-sante.fr/jcms/c_985715/fr/anorexie-mentale-prise-en-charge (accessed 2010 Sept. 30).
- 26.Haute Autorité de Santé. Boulimie et hyperphagie boulimique : Repérage et éléments généraux de prise en charge — recommandation de bonne pratique. Available: https://www.has-sante.fr/upload/docs/application/pdf/2019-09/boulimie_et_hyperphagie_boulimique_-_recommandations.pdf (accessed 2019 Sept. 12).
- 27.National Collaborating Centre for Mental Health (UK). Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Leicester (UK): British Psychological Society (UK); 2004. Available: http://www.ncbi.nlm.nih.gov/books/NBK49304/ (accessed 2022 Aug. 30). [PubMed] [Google Scholar]
- 28.Lecrubier Y, Sheehan DV, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry 1997;12:224–31. [Google Scholar]
- 29.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22–33, quiz 34–57. [PubMed] [Google Scholar]
- 30.Fauconnier M, Rousselet M, Brunault P, et al. Food addiction among female patients seeking treatment for an eating disorder: prevalence and associated factors. Nutrients 2020;12:1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rizk M, Lalanne C, Berthoz S, et al. Problematic exercise in anorexia nervosa: testing potential risk factors against different definitions. PLoS One 2015;10:e0143352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Billieux J, Rochat L, Ceschi G, et al. Validation of a short French version of the UPPS-P Impulsive Behavior Scale. Compr Psychiatry 2012;53:609–15. [DOI] [PubMed] [Google Scholar]
- 33.Cyders MA, Littlefield AK, Coffey S, et al. Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addict Behav 2014;39:1372–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferreri M, Vacher J, Tawils S, et al. Life events and depression. A new methodological approach. Psychol Med 1987;19:2441–8. [Google Scholar]
- 35.Guillou-Landreat M, Guilleux A, Sauvaget A, et al. Factors associated with suicidal risk among a French cohort of problem gamblers seeking treatment. Psychiatry Res 2016;240:11–8. [DOI] [PubMed] [Google Scholar]
- 36.Bender R, Lange S. Adjusting for multiple testing–when and how? J Clin Epidemiol 2001;54:343–9. [DOI] [PubMed] [Google Scholar]
- 37.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria; 2020. [Google Scholar]
- 38.Castellini G, Lelli L, Cassioli E, et al. Different outcomes, psychopathological features, and comorbidities in patients with eating disorders reporting childhood abuse: a 3-year follow-up study. Eur Eat Disord Rev 2018;26:217–29. [DOI] [PubMed] [Google Scholar]
- 39.Bell L. Does concurrent psychopathology at presentation influence response to treatment for bulimia nervosa? Eat Weight Disord 2002;7: 168–81. [DOI] [PubMed] [Google Scholar]
- 40.Steinhausen HC, Weber S. The outcome of bulimia nervosa: findings from one-quarter century of research. Am J Psychiatry 2009;166: 1331–41. [DOI] [PubMed] [Google Scholar]
- 41.Hussenoeder FS, Conrad I, Engel C, et al. Analyzing the link between anxiety and eating behavior as a potential pathway to eating-related health outcomes. Sci Rep 2021;11:14717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord 2007;40:293–309. [DOI] [PubMed] [Google Scholar]
- 43.Franko DL, Tabri N, Keshaviah A, et al. Predictors of long-term recovery in anorexia nervosa and bulimia nervosa: Data from a 22-year longitudinal study. J Psychiatr Res 2018;96:183–8. [DOI] [PubMed] [Google Scholar]
- 44.Lilenfeld LRR, Wonderlich S, Riso LP, et al. Eating disorders and personality: a methodological and empirical review. Clin Psychol Rev 2006;26:299–320. [DOI] [PubMed] [Google Scholar]
- 45.Meier M, Kossakowski JJ, Jones PJ, et al. Obsessive-compulsive symptoms in eating disorders: a network investigation. Int J Eat Disord 2020;53:362–71. [DOI] [PubMed] [Google Scholar]
- 46.Le Grange D, Lock J, Agras WS, et al. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther 2012;50:85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strawn JR, Geracioti L, Rajdev N, et al. Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based treatment review. Expert Opin Pharmacother 2018;19:1057–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas M, Lovell A. Anxiety and compulsion patterns in the maintenance of bingeing/purging behaviours by individuals with bulimia nervosa. J Psychiatr Ment Health Nurs 2015;22:20–9. [DOI] [PubMed] [Google Scholar]
- 49.Anestis MD, Selby EA, Joiner TE. The role of urgency in maladaptive behaviors. Behav Res Ther 2007;45:3018–29. [DOI] [PubMed] [Google Scholar]
- 50.Peterson CM, Fischer S. A prospective study of the influence of the UPPS model of impulsivity on the co-occurrence of bulimic symptoms and non-suicidal self-injury. Eat Behav 2012;13:335–41. [DOI] [PubMed] [Google Scholar]
- 51.Bardone-Cone AM, Butler RM, Balk MR, et al. Dimensions of impulsivity in relation to eating disorder recovery. Int J Eat Disord 2016;49: 1027–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fischer S, Wonderlich J, Breithaupt L, et al. Negative urgency and expectancies increase vulnerability to binge eating in bulimia nervosa. Eat Disord 2018;26:39–51. [DOI] [PubMed] [Google Scholar]
- 53.Cyders MA, Smith GT, Spillane NS, et al. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess 2007;19: 107–18. [DOI] [PubMed] [Google Scholar]
- 54.Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res 2013;37:1441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stojek MM, Fischer S, Murphy CM, et al. The role of impulsivity traits and delayed reward discounting in dysregulated eating and drinking among heavy drinkers. Appetite 2014;80:81–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Claes L, Islam MA, Fagundo AB, et al. The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS One 2015;10:e0126083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Michael ML, Juarascio A. Elevated cognitive dietary restraint mediates the relationship between greater impulsivity and more frequent binge eating in individuals with binge-spectrum eating disorders. Eat Weight Disord 2021;26:2795–800. [DOI] [PubMed] [Google Scholar]
- 58.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54:1063–70. [DOI] [PubMed] [Google Scholar]
- 59.McCrae RR, Costa PT, Ostendorf F, et al. Nature over nurture: temperament, personality, and life span development. J Pers Soc Psychol 2000;78:173–86. [DOI] [PubMed] [Google Scholar]
- 60.Cassin SE, von Ranson KM. Personality and eating disorders: a decade in review. Clin Psychol Rev 2005;25:895–916. [DOI] [PubMed] [Google Scholar]
- 61.Dorard G, Khorramian-Pour M. Binge eating disorder: links with personality and emotionality. Encephale 2017;43:114–9. [DOI] [PubMed] [Google Scholar]
- 62.Keel PK, Mitchell JE, Davis TL, et al. Impact of definitions on the description and prediction of bulimia nervosa outcome. Int J Eat Disord 2000;28:377–86. [DOI] [PubMed] [Google Scholar]
- 63.Billieux J, Heeren A, Rochat L, et al. Positive and negative urgency as a single coherent construct: evidence from a large-scale network analysis in clinical and non-clinical samples. J Pers 2021;11:1252–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.