Abstract
Background:
Racial/ethnic minorities have experienced disproportionate opioid-related overdose death rates in recent years. In this context, we examined inequities in community-based naloxone access across racial/ethnic groups in Massachusetts.
Methods:
We used data from: the Massachusetts Department of Public Health on community-based overdose education and naloxone distribution (OEND) programs; the Massachusetts Office of the Chief Medical Examiner on opioid-related overdose deaths, and; the United States Census American Community Survey for regional demographic/socioeconomic details to estimate community populations by race/ethnicity and racial segregation between African American/Black and white residents. Race/ethnicity groups included in the analysis were African American/Black (non-Hispanic), Hispanic, white (non-Hispanic), and “other” (non-Hispanic). We evaluated racial/ethnic differences in naloxone distribution across regions in Massachusetts and neighborhoods in Boston descriptively and spatially, plotting the race/ethnicity-specific number of kits per opioid-related overdose death per jurisdiction. Lastly, we constructed generalized estimating equations models with a negative binomial distribution to compare the race/ethnicity-specific naloxone distribution rate by OEND programs.
Results:
From 2016–2019, the median annual rate of naloxone kits received from OEND programs in Massachusetts per racial/ethnicity group ranged between 160–447 per 100,000. In a multivariable analysis, we found that the naloxone distribution rates for racial/ethnic minorities were lower than the rate for white residents. We also found naloxone was more likely to be distributed in racially segregated communities than non-segregated communities.
Conclusion:
We identified racial/ethnic inequities in naloxone receipt by individuals in Massachusetts. Additional resources focused on designing and implementing OEND programs for racial/ethnic minorities are warranted to ensure equitable access to naloxone.
Keywords: naloxone distribution, racial inequity, OEND, opioids, overdose
INTRODUCTION
In 2021, overdose mortality in the United States (US) increased to unprecedented levels, with most deaths attributable to fentanyl and related analogs (Ahmad et al., 2021; Hedegaard and Warner, 2021; Mattson et al., 2021). Opioid-related overdose mortality rates have differed among racial/ethnic groups (Friedman et al., 2021; Kariisa et al., 2021; Khatri et al., 2021; Kiang et al., 2021; Ray et al., 2020; Schuler et al., 2021). Across the United States, non-Hispanic African American/Black people who use drugs (PWUD) have been experiencing surging numbers of overdose deaths due to opioids or the co-involvement of opioids and cocaine (Kariisa et al., 2021). When evaluating race/ethnicity and gender-specific rates in the US, overdose deaths rose the fastest among African American/Black men, among whom overdose mortality tripled between 2015 and 2020 and in 2021 was higher than any other racial/ethnic group (Gramlich, 2022). Gramlich also reported that Hispanic men had the second-highest increase in overdose deaths. The same pattern has been found in Massachusetts, with the greatest growth in opioid-related overdose death rates occurring among non-Hispanic African American/Black residents (22.1 to 36.0 per 100,000) from 2019 to 2020, followed by Hispanic/Latino persons (32.2 to 36.3 per 100,000) (Massachusetts Department of Public Health, 2021).
Up until the early 2010s, white/non-Hispanic people had the highest opioid-related overdose death rate (Hoopsick et al., 2021), and treatment and opioid-related overdose prevention efforts were often directed towards white PWUD (Hansen, 2017; Hart and Hart, 2019; Lassiter, 2015; Mendoza et al., 2019). There was also a drastic shift away from previous responses to drug crises in the US, where policymakers had historically taken a “tough on crime” approach (Donnelly et al., 2019; Hart and Hart, 2019; Messner and Rosenfeld, 2012, 2012; Shachar et al., 2020, 2020).
In contrast, as a result of the implementation of racialized and punitive policies in earlier decades, such as the Harrison Narcotics Tax Act of 1914, the Marijuana Tax Act of 1937, and the Anti-Drug Abuse Acts of 1986 and 1988, African American/Black and Hispanic people have been disproportionately criminalized and discriminated against for drug use that was depicted at the time to take place largely within their communities (Hart and Hart, 2019; Musto, 1999). Although some of these policies are no longer enforced or have been reformed, African American/Black and Hispanic populations continue to be incarcerated for drug-related charges at disproportionately higher rates than their white counterparts (Bishop et al., 2020; Nellis, 2021). The differences in the approach to the drug crises based on race and ethnicity illustrates how structural racism has shaped drug policy in the US, and its potential to affect the implementation of naloxone distribution in communities of color today (Bailey et al., 2020; Hart and Hart, 2019).
Naloxone (a medication that effectively reverses opioid overdoses) has been distributed by overdose education and naloxone distribution (OEND) programs for more than two decades (Abouk et al., 2019; Davis and Carr, 2015; Strang et al., 1999). There is evidence that racial/ethnic minorities have less access to naloxone distributed through pharmacies (Chatterjee et al., 2022; Guadamuz et al., 2019). Two of the plausible causes include the presence of “pharmacy deserts” in low-income and predominantly racial/ethnic minority neighborhoods, and the increased likelihood of failing to stock naloxone among the pharmacies that are present in these neighborhoods (Guadamuz et al., 2019; Qato et al., 2014). In contrast, ecological studies have not shown racial/ethnic disparities in access to naloxone distributed by community-based OEND programs and have suggested potential benefits to people residing in predominantly minority communities (Nolen et al., 2021; Rowe et al., 2016). In a previous study evaluating community-based naloxone coverage equity in Rhode Island and Massachusetts (Nolen et al., 2021), we found higher volumes of naloxone were being distributed by community-based OEND programs to municipalities with higher percentages of African American/Black residents and residents in poverty. Although we were able to identify the demographic composition of communities that were receiving naloxone from these programs, we did not account for the racial/ethnic makeup of those who were actually receiving naloxone within those communities, and whether these persons had a similar racial/ethnic makeup as those experiencing overdoses in the communities. Thus, the objective of this study was to build upon our previous research and, by using individual-level OEND program data, to examine inequities in naloxone access at the individual level across racial/ethnic groups. We chose to study Massachusetts because, unlike many other states, OEND programs in Massachusetts collect race/ethnicity data for individual naloxone recipients. Using statistical and spatial methods, we determined whether there was naloxone coverage equity across racial/ethnic groups in 46 distinct geographic areas that make up Massachusetts.
Methods
Data and Measures
We used data collected by the Massachusetts Department of Public Health (MDPH)-supported OEND programs. The study period was from October 1, 2016, to December 31, 2019. During the study period, there were 27 community-based OEND program sites funded by MDPH to distribute naloxone kits and provide overdose prevention education to individuals at high risk for witnessing or experiencing an opioid overdose (Lim et al., 2019; Walley et al., 2013). MDPH funds community-based harm reduction programs, which typically provide syringe services and OEND to reach high risk populations and has been doing so since 2007. All the programs are required to report the race/ethnicity of everyone who received state purchased naloxone.
We aggregated the OEND naloxone data by race/ethnicity of the recipient for 46 contiguous population areas (CPAs). The CPAs were adapted from 21 catchment areas developed by the Massachusetts Behavioral Health Partnership (“Emergency Services Program Mobile Crisis Intervention,” 2016). We chose the catchment areas as the foundational geographic unit for creating our CPAs because they are spatial designations that were designed by, and relevant to, stakeholders in Massachusetts who can benefit from the results of our analysis. To distinguish between urban and non-urban geospatial areas, we identified municipalities with a population of 50,000 or more within each catchment area as distinct CPAs. This resulted in 21 remaining catchment areas and 25 large municipalities representing a total of 46 CPAs included in the analysis (Supplementary Figure 1).
Due to the population size of Boston, the large number of overdoses across multiple neighborhoods, and the racial and ethnic diversity at the neighborhood level, (Record et al., 2016; US Census Bureau and American Community Survey, 2020), we created race/ethnicity stratified maps for Boston on a neighborhood level. We operationalized neighborhoods as defined by the Boston Planning and Development Agency, a local government agency that oversees the zoning of neighborhoods in Boston (Neighborhood Profiles, 2017); however, the relatively small neighborhoods (Chinatown, Leather District, North End, and West End) in the inner city were collapsed into a ‚“Downtown” neighborhood.
We obtained race/ethnicity-stratified opioid-related overdose death data from the Massachusetts Office of the Chief Medical Examiner. Race/ethnicity information of the decedent was obtained from next of kin at the time of death. The medical examiner identifies overdose deaths using toxicological analyses, death scene investigation, and autopsy report. Both intentional and unintentional opioid-related overdoses were included in the analysis. Massachusetts uses a single, centralized statewide medical examiner system, which results in deaths being investigated in a consistent and reliable manner (Walley et al., 2019).
The United States Census American Community Survey (ACS) was used to obtain population estimates for each CPA by race/ethnicity. Specifically, the 2019 race/ethnicity-stratified, five-year population estimates were extracted from the ACS on a municipality-level and collapsed into the defined CPAs. The mutually exclusive racial/ethnic groups used in the analysis were: African American/Black (non-Hispanic), white (non-Hispanic), Hispanic (any race), and other races (non-Hispanic). The other category includes those who self-identified as American Indian and Alaska Native, Asian, Native Hawaiian or other Pacific Islander, two or more races, and unknown.
Previous studies have found that poverty and the percentage of African American/Black (non-Hispanic) residents are positively associated with naloxone distribution at a community level (Nolen et al., 2021; Rowe et al., 2016). We further investigated these associations by including poverty level and racial residential segregation between African American/Black (non-Hispanic) and white (non-Hispanic) residents, in the model. We chose racial segregation instead of the percentage of African American/Black (non-Hispanic) residents, because our outcome already relies on the number of residents in each CPA stratified by race/ethnicity. We used the dissimilarity index (Massey and Denton, 1988) to calculate racial segregation. This index is defined as the percentage of African American/Black (non-Hispanic) residents that would need to change residence for CPAs to have an equal distribution of African American/Black (non-Hispanic) and white (non-Hispanic) residents across the state. An index score of zero indicates perfect integration, whereas 1 indicates complete segregation and higher proportion of African American/Black (non-Hispanic) residents. Lastly, we aggregated municipality-level counts of residents in poverty from the ACS and calculated each CPA’s percentage of residents in poverty.
Spatial and Statistical Analysis
We used geospatial methods to analyze the median number of naloxone kits distributed by OEND programs per opioid-related overdose death for each racial/ethnic group in each CPA in Massachusetts and neighborhood in Boston over the four-year study period. We chose to use the number of racial/ethnic-specific opioid-related overdose deaths as our denominator due to its standardized classification in the International Classification of Diseases (Jalal et al., 2018). Consistent with previous studies, we chose to use the number of naloxone kits distributed per opioid-related overdose death as a measure for naloxone availability and access (Bird et al., 2015; Chen et al., 2006; Zang et al., 2021). The median number of naloxone kits distributed by OEND programs per opioid-related overdose death per racial/ethnic group was then mapped using ArcGIS version 10. We also created boxplots for the annual number of naloxone kits distributed by OEND programs per opioid-related overdose death per racial/ethnic group in each CPA. Due to small population sizes, some CPAs had an annual number of zero opioid-related overdose deaths in a given racial/ethnic group, which cannot be included to calculate the ratio of the number of naloxone kits distributed per opioid-related overdose death. To address this issue, we created two boxplots. The first boxplot included a reassignment of the annual number of opioid-related overdose deaths to one if it was equal to zero. The second, we excluded any CPA with an annual opioid-related overdose death count of zero.
Finally, we evaluated naloxone access equity using a multivariable generalized estimating equation (GEE) model with a negative binomial distribution (Equation 1). We chose a negative binomial distribution due to overdispersion in the naloxone count data. Our outcome was the number of naloxone kits distributed to each racial/ethnic group in each CPA. The independent variable is the race/ethnicity of the recipients of naloxone in each CPA. We also included in the model the opioid-related overdose death rate, percentage of residents in poverty, and dissimilarity index. We used R version 3.5.2, SAS version 9.4, and ArcGIS version 10 in this analysis. This study was approved and considered exempt by the Brown University School of Public Health and the Boston University Medical Campus Institutional Review Boards. Data for this study were obtained through an approved request to the MDPH. MDPH is not responsible for the authors’ analysis, opinions and conclusions contained in this document.
RESULTS
The 46 CPAs had a median population of 94,916 residents (interquartile range: 61,528–184,122). The median percentage of African American/Black (non-Hispanic) residents among the CPAs was 4.8% (IQR: 2.8%–7.2%); of Hispanic residents (any race) 7.9% (IQR: 4.5%–15.8%); of residents in the other race category 7.4% (IQR: 4.1%–12.3%); and of white (non-Hispanic) residents 76.9% (IQR:62.0%–84.0%, see Supplementary Table 1).
Compared to the other racial/ethnic groups, white (non-Hispanic) residents had the highest median rate of opioid-related overdose deaths (range across years: 24.8–28.3 per 100,000) and the highest median rate of naloxone kits received (range across years: 303.5–446.5 per 100,000) across all years of the study period (Table 1).
Table 1.
Crude rate of OEND naloxone distribution and opioid-related overdose death among 46 contiguous population areas, stratified by race/ethnicity, 2016–2019, Massachusetts.
| Overall (2016–2019) Median (IQR) |
2016 Median (IQR) |
2017 Median (IQR) |
2018 Median (IQR) |
2019 Median (IQR) |
|
|---|---|---|---|---|---|
| Rateb of Naloxone Kits Received (per 100,000) by Race/Ethnicity of Recipient | |||||
| African American/Black (non-Hispanic) | 271.2 (239.1, 302.1) | 247.0 (151.3, 412.1) | 295.3 (170.4, 559.6) | 215.2 (134.1, 448.2) | 322.5 (171.3, 588.2) |
| Hispanic | 277.4 (245.1, 331.0) | 309.6 (191.2, 489.0) | 244.5 (135, 562.7) | 245.3 (130.2, 630.9) | 395.5 (202.2, 745.4) |
| Othera (non-Hispanic) | 186.2 (174.6, 193.9) | 159.8 (74.4, 315.3) | 179.5 (64.8, 363.4) | 196.9 (71.8, 417.2) | 193.0 (108.1, 543.4) |
| White (non-Hispanic) | 351.8 (335.1, 380.1) | 345.6 (249.7, 617.5) | 358.0 (223.9, 824.6) | 303.5 (194.2, 818.3) | 446.5 (207.9, 997.4) |
| Opioid-related Overdose Death Rateb (per 100,000) by Race/Ethnicity of Decedent | |||||
| African American/Black (non-Hispanic) | 11.2 (6.2, 14.7) | 0.0 (0.0, 18.0) | 14.3 (0.0, 36.1) | 8.2 (0.0, 24.8) | 16.2 (0.0, 25.7) |
| Hispanic | 17.7 (17.6, 17.7) | 17.7 (1.4, 35.9) | 17.6 (0.0, 33.5) | 17.5 (0.0, 31.2) | 17.8 (35.3) |
| Othera (non-Hispanic) | 0. 0 (0.0, 0.7) | 0.0 (0.0, 10.7) | 0.0 (0.0, 11.0) | 2.9 (0.0, 17.9) | 0.0 (0.0, 11.3) |
| White (non-Hispanic) | 26.0 (24.8, 27.4) | 27.2 (19.4, 58.5) | 24.8 (17.3, 52.5) | 28.3 (15.5, 44.9) | 24.6 (15.5, 44.9) |
Other includes American Indian, Asian, Hawaiian/Pacific Islander, Multi-racial and those who refused to answer
OEND: opioid overdose education and naloxone distribution
denominator of each rate is the race/ethnicity specific population estimate in each of the contiguous population areas
In some years, the median opioid-related overdose death rate across the CPAs was 0 for African American/Black and ‚“other” races due to some CPAs’ having a small percentage of African American/Black (non-Hispanic) residents and ‚“other”races. This leads to no annual reporting of opioid-related overdose deaths occurring in these CPAs.
Boxplots describe the annual number of naloxone kits received per opioid-related overdose death across the racial/ethnic groups in each of the CPAs (Figure 1A). The annual median numbers of kits per opioid-related overdose death for the white (non-Hispanic) and Hispanic residents were similar, between 11.9 and 14.8. Residents in the ‚“other” race category received fewer naloxone kits for each overdose death than white (non-Hispanic) and Hispanic residents in 2016 and 2019. The median for this group increased from 10.0 in 2016 to 12.5 in 2017 and remained the same in 2018 and 2019. Similar to residents in the ‚“other” race, across all years in the study period, African American/Black (non-Hispanic) residents had a lower median number of naloxone kits for each opioid-related overdose death compared to white (non-Hispanic) residents. However, the number of naloxone kits per opioid-related overdose death among this group increased from 9.7 in 2016 to 13.0 in 2019, driven primarily by the increase in naloxone distribution. Although the median number of kits per death remained lower than white (non-Hispanic) residents, the gap between the two racial groups narrowed over the course of the study period. When we excluded CPAs with no reported opioid-related overdose deaths, the median number of naloxone kits per opioid-related overdose death was similar across all racial/ethnic groups in 2016 and 2017. However, for the years 2018 and 2019, residents in the ‚“other” race had the highest median number kits per death at 17 and 18, respectively.
Figure 1.
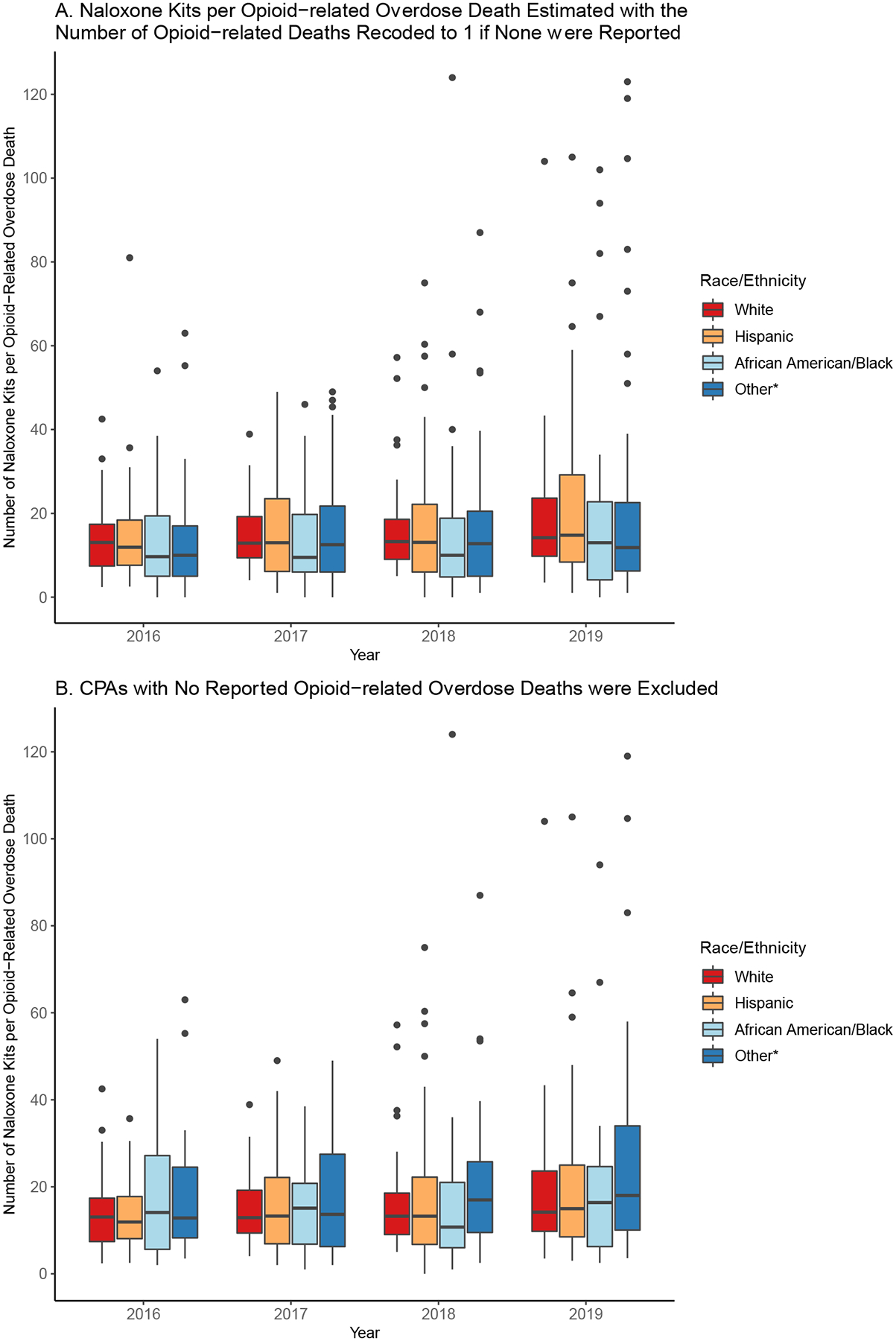
Boxplot of the number of naloxone kits received per opioid-related overdose death by race/ethnicity in each contiguous population area (N=46) between 2016 and 2019 in Massachusetts.
*Other includes American Indian, Asian, Hawaiian/Pacific Islander, Multi-racial and those who refused to answer
Next, we created a map for each race/ethnicity group using the median number of naloxone kits per opioid-related overdose death across all years of the study period (Figure 2). Among all race/ethnicity groups, at least one naloxone kit was distributed in all CPAs with a race/ethnicity-specific opioid-related death rate greater than zero. Over 70% of CPAs had at least ten naloxone kits per opioid-related overdose death among white (non-Hispanic) residents. The distribution of kits per opioid-related overdose death among this population was generally higher in the state’s western region. In contrast, only 46% and 32% of CPAs had at least ten naloxone kits distributed per opioid-related overdose death among Hispanic and African American/Black individuals, respectively. In contrast to white residents, distribution to African American/Black and Hispanic residents was higher in the state’s eastern region.
Figure 2.
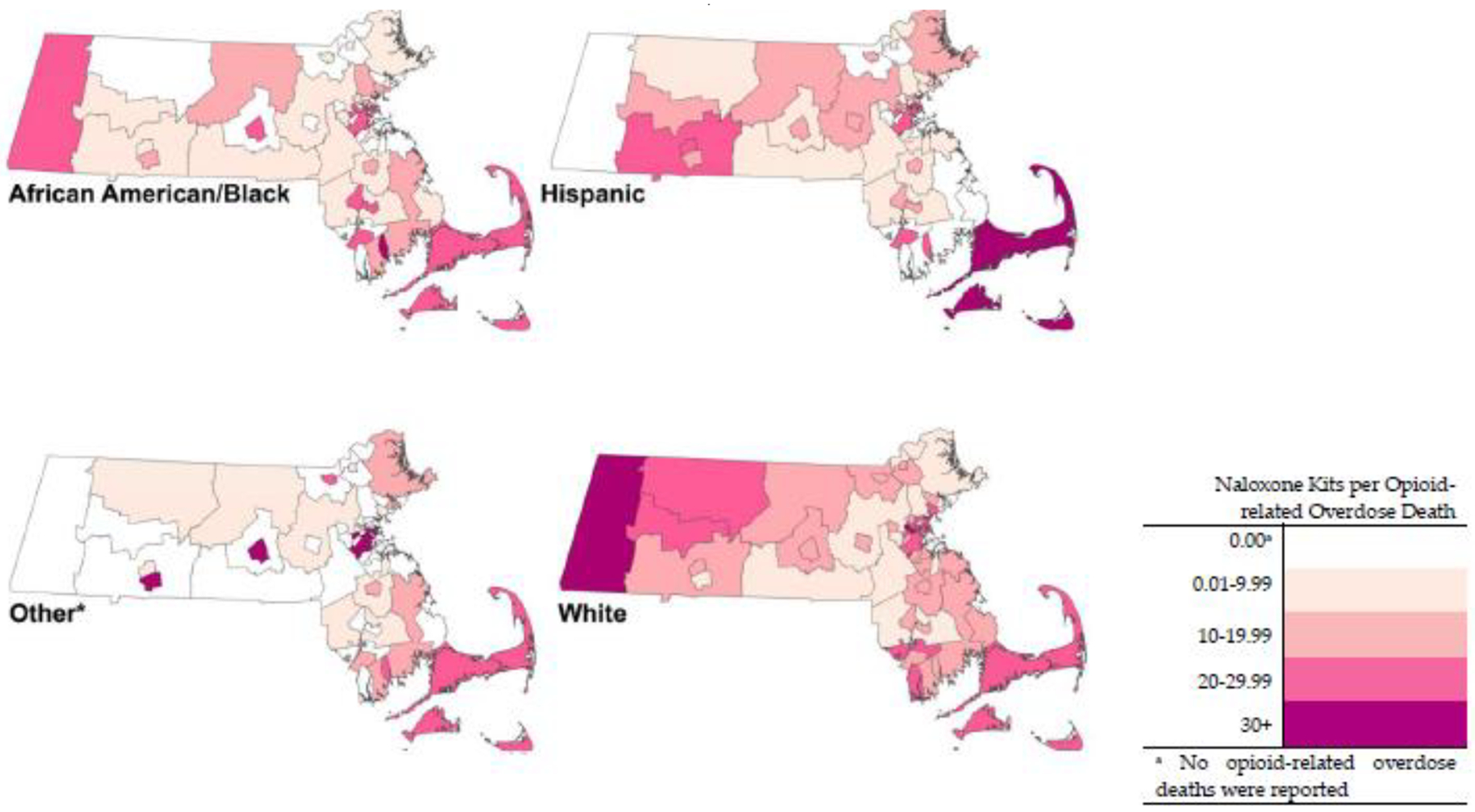
The median number of naloxone kits per opioid-related overdose death among residents in each of 46 contiguous population area of Massachusetts, 2016–2019
*Other includes American Indian, Asian, Hawaiian/Pacific Islander, Multi-racial and those who refused to answer
When we examined naloxone distribution in Boston by neighborhood, we observed greater naloxone distribution among African Americans/Blacks (non-Hispanic) compared to the distribution of naloxone to African Americans/Blacks in the entire state (Figure 3). Forty percent of neighborhoods distributed at least ten naloxone kits for each overdose death to African American/Black residents. For white (non-Hispanic) residents, 87% of neighborhoods distributed at least ten kits per opioid-related overdose death. Among Hispanic residents, the percentage of neighborhoods that distributed at least ten kits per overdose death was the same as the statewide percentage at 46%.
Figure 3.
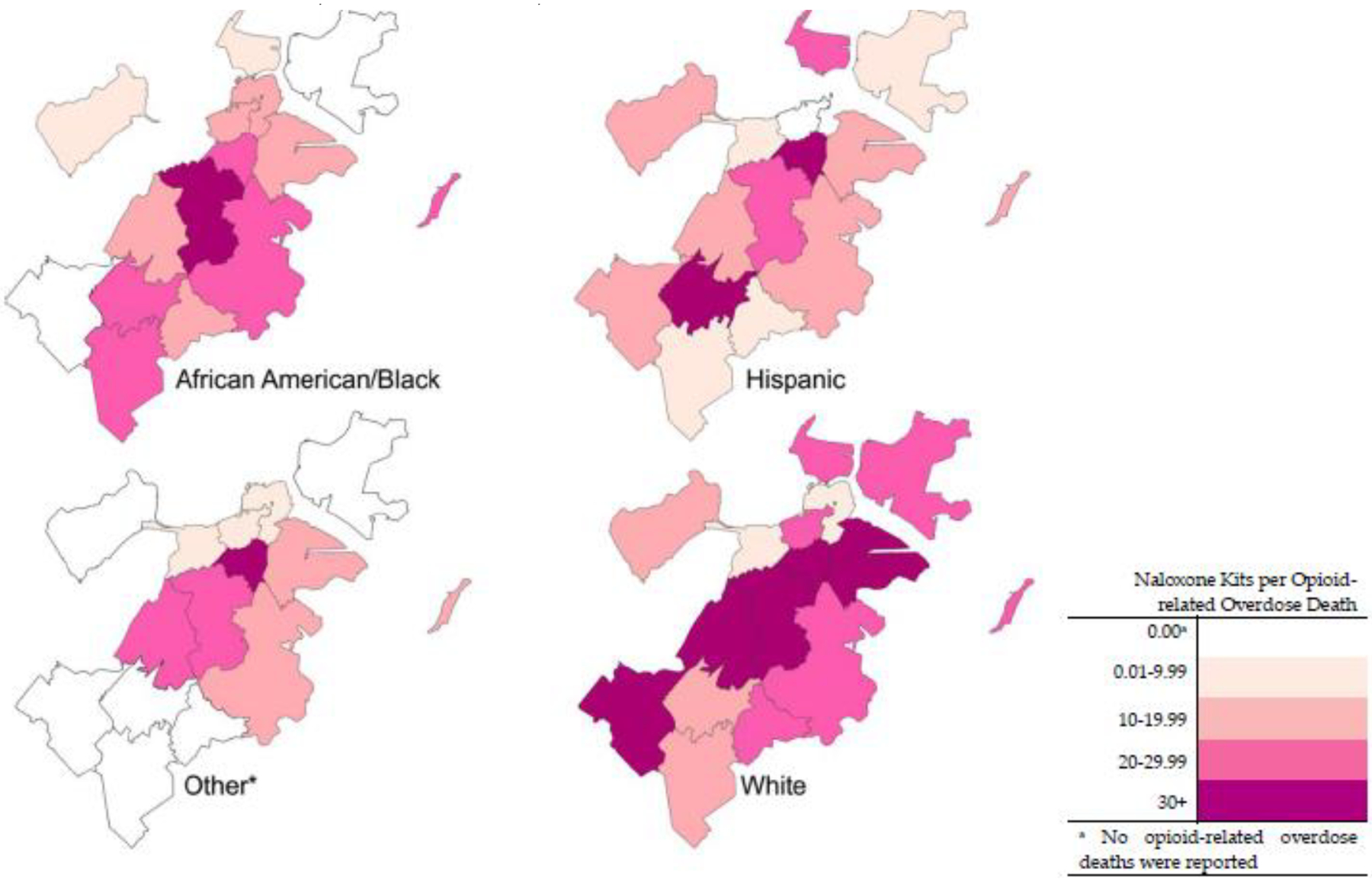
The median number of naloxone kits per opioid-related overdose death among residents in each neighborhoods of Boston, Massachusetts, 2016–2019
*Other includes American Indian, Asian, Hawaiian/Pacific Islander, Multi-racial and those who refused to answer
In the unadjusted GEE model, all race/ethnicity groups had significantly lower naloxone receipt than white (non-Hispanic) residents (Table 2). CPAs with a 4-year opioid-related overdose death rate greater than 30 per 100,000 had a 147% higher rate of naloxone kits distributed than CPAs with an opioid-related overdose rate equal to zero. The percentage of residents in poverty (1.06; 95% CI: 1.04, 1.09) and dissimilarity index (1.51, 95% CI: 0.90, 2.53) in a CPA were positively associated with naloxone distribution. In the adjusted GEE model, the differences between Hispanic and white (non-Hispanic) residents in naloxone receipt continued to be significant (Table 2). The CPA-level opioid-related overdose death rate (1.70, 95% CI: 1.12, 2.56), percentage of residents in poverty (1.07, 95% CI: 1.05, 1.10), and dissimilarity index measuring segregation were also significant in the adjusted model. As for the dissimilarity index, with every one point increase in the percentage of African American (non-Hispanic) residents who need to change residence to reduce segregation, there was a 143% increase in the naloxone receipt rate (2.43, 95% CI: 1.62, 3.65).
Table 2.
Relative ratios of the naloxone kit distribution rate by the race/ethnicity of the recipient among Massachusetts residents using a GEE model with a negative binomial distribution, 2016–2019
| Unadjusted Models RR (95% CI) |
Adjusted Model RR (95% CI) |
|
|---|---|---|
| Race/Ethnicity of Naloxone Recipient | ||
| African American/Black (non-Hispanic) | 0.75 (0.57, 0.99)* | 0.87 (0.65, 1.17) |
| Hispanic | 0.71 (0.54, 0.92)* | 0.78 (0.61, 0.99)* |
| Othera (non-Hispanic) | 0.45 (0.33, 0.59)** | 0.55 (0.40, 0.77)** |
| White (non-Hispanic) | ref | ref |
| Opioid Related Overdose Death Rate (per 100,000) | ||
| 0 | ref | ref |
| 0.01–9.99 | 0.96 (0.45, 2.03) | 1.01 (0.48, 2.13) |
| 10.00–19.99 | 1.58 (0.78, 3.21) | 1.62 (0.80, 3.29) |
| 20.00–29.99 | 0.94 (0.64, 1.39) | 1.02 (0.75, 1.40) |
| 30.00+ | 2.47 (1.60, 3.83)** | 1.70 (1.12, 2.56)* |
| Dissimilarity Index (African American/Black vs. White) | 1.51 (0.90, 2.53) | 2.43 (1.62, 3.65)** |
| % of residents in poverty (per percentage increase) | 1.06 (1.04, 1.09) ** | 1.07 (1.05, 1.10) ** |
Other includes American Indian, Asian, Hawaiian/Pacific Islander, Multi-racial and those who refused to answer
< 0.05;
<0.001
DISCUSSION
In this 4-year, statewide study of community-based naloxone distribution in Massachusetts, we found significant racial/ethnic disparities in naloxone access. This was evaluated using race/ethnicity-specific ratios of naloxone kits per opioid-related overdose deaths across CPAs in Massachusetts. We found that African American/Black (non-Hispanic) and Hispanic racial/ethnic groups had lower rates of naloxone receipt per opioid-related overdose death than white (non-Hispanic) residents. This relationship was seen in descriptive data, boxplots, and maps that examined the number of naloxone kits received per opioid-related overdose death in each racial/ethnic group between 2016 and 2019. We also found some racial/ethnic differences in a GEE model that estimated the rate of naloxone kits received by each racial/ethnic group, adjusting for community poverty levels and racial segregation.
Racial/ethnic minorities had lower rates of receiving community-based OEND naloxone per opioid-related overdose death than white residents across the state, including in Boston neighborhoods. However, African American/Black and Hispanic residents in Boston had a higher median number of naloxone kits per opioid-related overdose death compared to African American/Black and Hispanic residents elsewhere in the state. This could be attributed to OEND programs’ ability to allocate resources more efficiently and equitably in cities/towns such as Boston that are more racially diverse and are heavily impacted by the opioid and overdose crisis (Kerensky and Walley, 2017; Rowe et al., 2016; Walley et al., 2013). In addition to their ability to allocate resources more efficiently, Boston benefits from being the state’s capital and most populated city with a large plurality of the state’s population in the Boston Metro area, which means that there is a concentration of political, financial, and social service capital there in comparison to other municipalities in the state.
We also found that CPAs in Massachusetts and neighborhoods in Boston that were more racially segregated, as measured by dissimilarity index between African American/Black and white individuals, had higher rates of naloxone distributed into those communities. This is consistent with a 2021 study in Massachusetts that found more naloxone was distributed to cities/towns with higher percentages of African American/Black residents (Nolen et al., 2021). Despite that, when examining the racial/ethnic identities of people who received naloxone in those jurisdictions, African American/Black and Hispanic residents were persistently less likely to receive naloxone from OEND programs than white residents. A recent study in San Francisco and Los Angeles found similar results: white individuals were more likely to receive naloxone than racial/ethnic minorities, especially African American/Black individuals (Kinnard et al., 2021). Although racially segregated jurisdictions had higher rates of naloxone receipt, the racial/ethnic distribution of naloxone recipients within those jurisdictions may not reflect equitable racial/ethnic distribution in these communities.
This study is subject to several limitations. First, the CPA configuration chosen could mask inequities that would have been observed at smaller geographical levels. This is attributed to the large number of municipalities with zero race/ethnicity-specific counts of opioid-related deaths, which would cause biased results. Although we did not use a smaller geographic unit, we selected a spatial designation that state stakeholders use, which is a strength of our analysis. Second, we used cumulative counts of naloxone kits over 4 years for our GEE model, versus annual estimates, to ensure sufficient statistical power for the geographic-unit-level analyses. We were, however, able to include annual data in the boxplots that examined the number of naloxone kits per opioid-related overdose death and in maps that estimated the median number of kits per death. Next, although over 70% of naloxone in Massachusetts is distributed from a community-based OEND program (Chatterjee et al., 2022), we were unable to include data for the remaining 30% that was dispensed from a pharmacy-based source as these sources do not provide the race/ethnicity of naloxone recipients. Future studies should assess whether there is racial equity in naloxone use among recipients. This is especially necessary because of the impact of the COVID-19 pandemic on overdose mortality. Studies have suggested that the economic, social, and structural inequities that the African American/Black and Hispanic population experienced in the wake of the COVID-19 pandemic influenced the inequities in overdose mortality and is expected to continue to worsen (Brown et al., 2021; Friedman et al., 2021).
CONCLUSION
We estimated the relationships between naloxone distribution in community-based OEND programs and opioid overdose deaths by race/ethnicity at the individual level, and found that white (non-Hispanic) residents received naloxone at higher rates per opioid-related overdose death than racial/ethnic minority groups, including in jurisdictions with higher concentrations of African American/Black residents where overall naloxone distribution rates were higher. To reduce the racial/ethnic gap in naloxone distribution in the short term, current OEND programs should develop specific initiatives for increasing naloxone distribution to racial/ethnic minorities. Our work demonstrates that simply distributing naloxone through OEND programs operating in racially diverse communities is not sufficient to achieve equitable naloxone receipt among non-white residents. There needs to be changes in practice for assessing equitable naloxone access such as measuring and tracking race/ethnicity-specific naloxone to opioid-related overdose death rations with the goal to understand whether distribution policies and OEND programs are meeting equity goals, and work to improve the categorization of race/ethnicity groups when measuring naloxone equity through the partnership of community-based organizations of communities of people that were either left out or collapsed into other groups. In addition to changes in surveillance, there needs to be efforts towards creating community-informed initiatives that can reach racial/ethnic minorities is necessary for decreasing inequities in naloxone receipt and improving overdose mortality rates. Examples of successful initiatives include collaborations with community-based and faith-based organizations who have a strong relationship with minority communities to develop OEND programs (e.g., Detroit Recovery Project, Bridges to Care and Recovery in St. Louis, Missouri and Amistades, Inc in Tucson, Arizona), and holistic clinics where people who use drugs feel comfortable accessing naloxone but also basic needs service provision and treatment (e.g., Bellevue Hospital holistic addiction clinic in New York City, New York), and employing people at OEND programs that reflect the demographic of the community that they are serving (e.g., peer mentoring at Project RECOVER in Boston, Massachusetts and Connecticut (Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity, 2020a, 2020b). Through the implementation of new policies and practice recommendations and the development of new OEND programs or investing resources in current OEND programs to ensure that they are welcoming, accessible, inclusive, and acceptable to racial/ethnic minorities, inequities in naloxone access can be addressed, and opioid overdose mortality reduced among racial/ethnic minorities.
Supplementary Material
Highlights.
Evaluated racial/ethnic differences in naloxone distribution in Massachusetts
2016–2019, racial/ethnic minorities received less community-based OEND naloxone
Regions with high overdose rates received more naloxone
Despite segregated regions receiving more naloxone, minority residents received less
Funding Sources:
This study was supported by the National Institute on Drug Abuse (U01DA047408, R01CE002999, and P30DA040500).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared
REFERENCES
- Abouk R, Pacula RL, Powell D, 2019. Association between State Laws Facilitating Pharmacy Distribution of Naloxone and Risk of Fatal Overdose. JAMA Intern. Med 179, 805–811. 10.1001/jamainternmed.2019.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad F, Rossen L, Sutton P, 2021. Provisional drug overdose death counts.
- Bailey ZD, Feldman JM, Bassett MT, 2020. How Structural Racism Works — Racist Policies as a Root Cause of U.S. Racial Health Inequities. N. Engl. J. Med 384, 768–773. 10.1056/nejmms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Parmar MKB, Strang J, 2015. Take-home naloxone to prevent fatalities from opiate-overdose: Protocol for Scotland’s public health policy evaluation, and a new measure to assess impact. Drugs Educ Prev Pol 22, 66–76. 10.3109/09687637.2014.981509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop ET, Hopkins B, Obiofuma C, Owusu F, 2020. Racial Disparities in the Massachusetts Criminal System. Criminal Justice Polic Program, Harvard Law School. [Google Scholar]
- Brown P, Watts V, Hanna M, Rizk M, Tucker E, Saddlemire A, Peteet B, 2021. Two Epidemics and a Pandemic: The Collision of Prescription Drug Misuse and Racism during COVID-19. J. Psychoactive Drugs 53, 413–421. 10.1080/02791072.2021.1992048 [DOI] [PubMed] [Google Scholar]
- Chatterjee A, Yan S, Xuan Z, Waye KM, Lambert AM, Green TC, Stopka TJ, Pollini RA, Morgan JR, Walley AY, 2022. Broadening access to naloxone: Community predictors of standing order naloxone distribution in Massachusetts. Drug Alcohol Depend. 230, 109190. 10.1016/j.drugalcdep.2021.109190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WJ, Fang C-C, Shyu R-S, Lin K-C, 2006. Underreporting of illicit drug use by patients at emergency departments as revealed by two-tiered urinalysis. Addict. Behav 31, 2304–2308. 10.1016/j.addbeh.2006.02.015 [DOI] [PubMed] [Google Scholar]
- Davis CS, Carr D, 2015. Legal changes to increase access to naloxone for opioid overdose reversal in the United States. Drug Alcohol Depend. 157, 112–120. 10.1016/j.drugalcdep.2015.10.013 [DOI] [PubMed] [Google Scholar]
- Donnelly EA, Wagner J, Anderson TL, O’Connell D, 2019. Revisiting Neighborhood Context and Racial Disparities in Drug Arrests Under the Opioid Epidemic. Race Justice 2153368719877222. 10.1177/2153368719877222 [DOI] [Google Scholar]
- Emergency Services Program Mobile Crisis Intervention [WWW Document], 2016. Masschusetts Behav. Health Partnersh URL https://www.masspartnership.com/ (accessed 11.17.21).
- Friedman J, Hansen H, Bluthenthal RN, Harawa N, Jordan A, Beletsky L, 2021. Growing racial/ethnic disparities in overdose mortality before and during the COVID-19 pandemic in California. Prev. Med 153, 106845. 10.1016/j.ypmed.2021.106845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gramlich J, 2022. Recent surge in U.S. drug overdose deaths has hit Black men the hardest. Pew Res. Cent URL https://www.pewresearch.org/fact-tank/2022/01/19/recent-surge-in-u-s-drug-overdose-deaths-has-hit-black-men-the-hardest/ (accessed 2.7.22). [Google Scholar]
- Guadamuz JS, Alexander GC, Chaudhri T, Trotzky-Sirr R, Qato DM, 2019. Availability and Cost of Naloxone Nasal Spray at Pharmacies in Philadelphia, Pennsylvania, 2017. JAMA Netw. Open 2, e195388–e195388. 10.1001/jamanetworkopen.2019.5388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen H, 2017. Assisted Technologies of Social Reproduction: Pharmaceutical Prosthesis for Gender, Race, and Class in the White Opioid ‚“Crisis.” Contemp. Drug Probl. 44, 321–338. 10.1177/0091450917739391 [DOI] [Google Scholar]
- Hart CL, Hart MZ, 2019. Opioid Crisis: Another Mechanism Used to Perpetuate American Racism. 10.1037/cdp0000260 [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, 2021. Drug Overdose Deaths in the United States, 1999–2020 8. [PubMed] [Google Scholar]
- Hoopsick RA, Homish GG, Leonard KE, 2021. Differences in Opioid Overdose Mortality Rates Among Middle-Aged Adults by Race/Ethnicity and Sex, 1999–2018. Public Health Rep. 136, 192–200. 10.1177/0033354920968806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS, 2018. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 361, eaau1184. 10.1126/science.aau1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M, Seth P, Scholl L, Wilson N, Davis NL, 2021. Drug overdose deaths involving cocaine and psychostimulants with abuse potential among racial and ethnic groups – United States, 2004–2019. Drug Alcohol Depend. 227, 109001. 10.1016/j.drugalcdep.2021.109001 [DOI] [PubMed] [Google Scholar]
- Kerensky T, Walley AY, 2017. Opioid overdose prevention and naloxone rescue kits: what we know and what we don’t know. Addict. Sci. Clin. Pract 12, 4. 10.1186/s13722-016-0068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri UG, Pizzicato LN, Viner K, Bobyock E, Sun M, Meisel ZF, South EC, 2021. Racial/Ethnic Disparities in Unintentional Fatal and Nonfatal Emergency Medical Services–Attended Opioid Overdoses During the COVID-19 Pandemic in Philadelphia. JAMA Netw. Open 4, e2034878. 10.1001/jamanetworkopen.2020.34878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiang MV, Tsai AC, Alexander MJ, Rehkopf DH, Basu S, 2021. Racial/Ethnic Disparities in Opioid-Related Mortality in the USA, 1999–2019: the Extreme Case of Washington DC. J. Urban Health 98, 589–595. 10.1007/s11524-021-00573-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnard EN, Bluthenthal RN, Kral AH, Wenger LD, Lambdin BH, 2021. The naloxone delivery cascade: Identifying disparities in access to naloxone among people who inject drugs in Los Angeles and San Francisco, CA. Drug Alcohol Depend. 225, 108759. 10.1016/j.drugalcdep.2021.108759 [DOI] [PubMed] [Google Scholar]
- Lassiter MD, 2015. Impossible Criminals: The Suburban Imperatives of America’s War on Drugs. J. Am. Hist 102, 126–140. 10.1093/jahist/jav243 [DOI] [Google Scholar]
- Lim JK, Forman LS, Ruiz S, Xuan Z, Callis BP, Cranston K, Walley AY, 2019. Factors associated with help seeking by community responders trained in overdose prevention and naloxone administration in Massachusetts. Drug Alcohol Depend. 204, 107531–107531. 10.1016/j.drugalcdep.2019.06.033 [DOI] [PubMed] [Google Scholar]
- Massachusetts Department of Public Health, 2021. Opioid-Related Overdose Deaths, All Intents, MA Residents – Demographic Data Highlights.
- Massey DS, Denton NA, 1988. The Dimensions of Residential Segregation. Soc. Forces 67, 281. 10.1093/sf/67.2.281 [DOI] [Google Scholar]
- Mattson CL, Tanz Lauren J., Quinn Kelly, Kariisa Mbabazi, Patel Priyam, Davis Nicole L., 2021. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb. Mortal. Wkly. Rep 70. 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza S, Rivera AS, Hansen HB, 2019. Re-racialization of Addiction and the Redistribution of Blame in the White Opioid Epidemic. Med. Anthropol. Q 33, 242–262. 10.1111/maq.12449 [DOI] [PubMed] [Google Scholar]
- Messner SF, Rosenfeld R, 2012. Crime and the American Dream. Cengage Learning. [Google Scholar]
- Musto DF, 1999. The American Disease: Origins of Narcotic Control. Oxford University Press. [Google Scholar]
- Neighborhood Profiles, 2017. Boston Planning & Development Agency Research Division.
- Nellis A, 2021. The Color of Justice: Racial and Ethnic Disparity in State Prisons. The Sentencing Project. [Google Scholar]
- Nolen S, Zang X, Chatterjee A, Behrends CN, Green TC, Kumar A, Linas BP, Morgan JR, Murphy SM, Walley AY, Yan S, Schackman BR, Marshall BDL, 2021. Community-based Naloxone Coverage Equity for the Prevention of Opioid Overdose Fatalities in Racial/Ethnic Minority Communities in Massachusetts and Rhode Island. Addiction n/a. 10.1111/add.15759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B, 2014. ‘Pharmacy Deserts’ Are Prevalent In Chicago’s Predominantly Minority Communities, Raising Medication Access Concerns. Health Aff. (Millwood) 33, 1958–1965. 10.1377/hlthaff.2013.1397 [DOI] [PubMed] [Google Scholar]
- Ray B, Lowder E, Bailey K, Huynh P, Benton R, Watson D, 2020. Racial differences in overdose events and polydrug detection in Indianapolis, Indiana. Drug Alcohol Depend. 206, 107658. 10.1016/j.drugalcdep.2019.107658 [DOI] [PubMed] [Google Scholar]
- Record K, Sawh L, Reese-McLaughlin N, Pervin A, Anderson A, Wrobel M, 2016. Opioid Use Disorder in Massachusetts: An Analysis of its Impact on the Health Care System, Availability of Pharmacologic Treatment, and Recommendations for Payment and Care Delivery Reform. The Health Policy Commission. [Google Scholar]
- Rowe C, Santos GM, Vittinghoff E, Wheeler E, Davidson P, Coffin PO, 2016. Neighborhood-Level and Spatial Characteristics Associated with Lay Naloxone Reversal Events and Opioid Overdose Deaths. J. Urban Health 93, 117–130. 10.1007/s11524-015-0023-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Schell TL, Wong EC, 2021. Racial/ethnic differences in prescription opioid misuse and heroin use among a national sample, 1999–2018. Drug Alcohol Depend. 221, 108588. 10.1016/j.drugalcdep.2021.108588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shachar C, Wise T, Katznelson G, Campbell AL, 2020. Criminal Justice or Public Health: A Comparison of the Representation of the Crack Cocaine and Opioid Epidemics in the Media. J. Health Polit. Policy Law 45, 211–239. 10.1215/03616878-8004862 [DOI] [PubMed] [Google Scholar]
- Strang J, Powis B, Best D, Vingoe L, Griffiths P, Taylor C, Welch S, Gossop M, 1999. Preventing opiate overdose fatalities with take-home naloxone: Pre-launch study of possible impact and acceptability. Addiction 94, 199–204. 10.1046/j.1360-0443.1999.9421993.x [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity, 2020a. The Opioid Crisis and the Black/African American Population: An Urgent Issue. U.S. Department of Health and Human Services. [Google Scholar]
- Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity, 2020b. The Opioid Crisis and the Hispanic/Latino Population: An Urgent Issue. U.S. Department of Health and Human Services. [Google Scholar]
- US Census Bureau, American Community Survey, 2020. American Community Survey 5-Year Estimates [WWW Document]. URL https://data.census.gov/
- Walley AY, Bernson D, Larochelle MR, Green TC, Young L, Land T, 2019. The Contribution of Prescribed and Illicit Opioids to Fatal Overdoses in Massachusetts, 2013–2015. Public Health Rep. 134, 667–674. 10.1177/0033354919878429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, Ruiz S, Ozonoff A, 2013. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. BMJ Online 346. 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zang X, Macmadu A, Krieger MS, Behrends CN, Green TC, Morgan JR, Murphy SM, Nolen S, Walley AY, Schackman BR, Marshall BD, 2021. Targeting community-based naloxone distribution using opioid overdose death rates: A descriptive analysis of naloxone rescue kits and opioid overdose deaths in Massachusetts and Rhode Island. Int. J. Drug Policy 98, 103435. 10.1016/j.drugpo.2021.103435 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


