Abstract
Objective
We aimed to 1) describe how the UK obesity epidemic reflects a change over time in the proportion of the population demonstrating adverse latent patterns of BMI development and 2) investigate the potential roles of maternal and paternal BMI in this secular process.
Methods
We used serial BMI data between 7 and 17 years of age from 13220 boys and 12711 girls. Half the sample was born in 1958 and half in 2001. Sex-specific growth mixture models were developed. The relationships of maternal and paternal BMI and weight status with class membership were estimated using the 3-step BCH approach, with covariate adjustment.
Results
The selected models had five classes. For each sex, in addition to the two largest normal weight classes, there were “normal weight increasing to overweight” (17% of boys and 20% of girls), “overweight increasing to obesity” (8% and 6%), and “overweight decreasing to normal weight” (3% and 6%) classes. More than 1-in-10 children from the 2001 birth cohort were in the “overweight increasing to obesity” class, compared to less than 1-in-30 from the 1958 birth cohort. Approximately 75% of the mothers and fathers of this class had overweight or obesity. When considered together, both maternal and paternal BMI were associated with latent class membership, with evidence of negative departure from additivity (i.e., the combined effect of maternal and paternal BMI was smaller than the sum of the individual effects). The odds of a girl belonging to the “overweight increasing to obesity” class (compared to the largest normal weight class) was 13.11 (8.74, 19.66) times higher if both parents had overweight or obesity (compared to both parents having normal weight); the equivalent estimate for boys was 9.01 (6.37, 12.75).
Conclusions
The increase in obesity rates in the UK over more than 40 years has been partly driven by the growth of a sub-population demonstrating excess BMI gain during adolescence. Our results implicate both maternal and paternal BMI as correlates of this secular process.
Subject terms: Epidemiology, Risk factors
Introduction
The obesity epidemic is a major public health threat. According to the 2019/20 data from the National Child Measurement Programme in England, 10% of children in Reception (4–5 years) and 21% of children in Year 6 (10–11 years) had obesity [1]. Obesity rates then continue to increase into adulthood [2] due to the marked biological (e.g., decreased insulin sensitivity) and behavioural changes (e.g., decline in physical activity) that occur with puberty and during adolescence [3]. It is well known that the decade of life following the adiposity rebound at 5–7 years of age is a critical period in obesity development [4]. Few studies have, however, used growth mixture modelling to capture and describe the latent class (or classes) of children who share an average body mass index (BMI) trajectory that transitions from non-obese to obese during adolescence [5–10].
Using data from the nationally representative United Kingdom (UK) birth cohort studies, we have previously shown a positive skewing of the BMI distribution at increasingly younger ages in more recently born cohorts [11]. Alternatively, the obesity epidemic can be viewed as a shift over time in the proportion of the population demonstrating obesogenic BMI trajectories. In a recent paper that applied growth mixture modelling to data from three UK birth cohorts, Norris et al revealed how the obesity epidemic partly reflects an increase in the proportion of the population belonging to a latent class characterised by an average BMI trajectory that started in the normal weight range at 11 years but ended in the overweight range at 42 years [12]. Compared to the 1946 birth year cohort, the 1970 cohort (but not the 1958 cohort) had a higher odds of belonging to this class rather than a referent class that was consistently normal weight. The same advanced approach has not been applied using the much more recently born 2001 cohort (in combination with an older cohort or cohorts) to understand secular changes in latent patterns of child-adolescent BMI development from before the obesity epidemic era to present day. Such an analysis would provide important information that cannot be provided by conventional growth curve modelling, an approach which has been widely used to describe cohort differences in mean BMI and obesity prevalence trajectories [11, 13, 14]. By viewing the evolution of the obesity epidemic in this traditional way, one fails to consider the possibility that higher/steeper mean BMI and obesity prevalence trajectories in more recently born cohorts could be the result of complex secular changes in the proportion of the population demonstrating different patterns of development. For example, the 2001 cohort would likely have a higher/steeper mean BMI trajectory than an older cohort, but this could be the result of a secular change towards more children having high-to-average BMI trajectories (e.g., 10% in 2001 cohort; 5% in older cohort), and average-to-high BMI trajectories (e.g., 30% in 2001 cohort; 5% in older cohort), and even consistently low BMI trajectories (e.g., 5% in 2001 cohort; 2.5% in older cohort).
Changes over time in rates of adulthood obesity have broadly mirrored those of childhood obesity, and parental obesity is arguably one the strongest determinants of offspring obesity [15, 16]. Previous analyses in the UK cohorts have demonstrated strong associations of both maternal and paternal BMI with offspring obesity that persisted well into adulthood and were not explained by traditional confounders or offspring lifestyle factors [17–21]. Such traditional analyses, however, impose linear constraints that are a simple representation of the complex way in which parental BMI might be related to offspring BMI trajectories. For example, a one-unit higher maternal BMI might be related to a 0.05 kg/m2/year steeper offspring BMI trajectory on average, but growth mixture modelling might provide additional information that higher maternal BMI is associated with greater odds of their child belonging to a small adolescent-onset of underweight group. A recent paper by Dos Santos et al found that maternal obesity was related to membership of unhealthy latent BMI trajectory classes (e.g., always obese) in the 2001 cohort [22], and similar findings have been reported in other studies [7, 8, 10, 23, 24]. The majority of this literature, however, does not consider paternal BMI and inadvertently contributes to the “imbalance of DOHaD [development origins of health and disease] research towards the study of maternal pregnancy exposures” [25, 26]. The literature also largely comprises studies that have been conducted using data from one cohort of children born at one point in time, and the reported associations do not necessarily tell us anything about how maternal and/or paternal obesity might have contributed to the paediatric obesity epidemic [27].
We aimed to 1) describe how the UK obesity epidemic reflects a change over time in the proportion of the population demonstrating adverse latent patterns of BMI development between 7 and 17 years of age and 2) investigate the potential roles of maternal and paternal BMI in this secular process.
Methods
Sample
The 1958 National Child Development Study (NCDS) is based on 17,638 people born in one week in March 1958 in England, Scotland, and Wales; 920 immigrants born in the same week were incorporated during childhood [28]. The 2001 Millennium Cohort Study (MCS) is based on 18,818 people born between September 2000 and January 2002 who were living in England, Scotland, Wales, or Northern Ireland at age 9 months [29]. Both studies have received ethical approval and obtained informed parental and/or participant consent; this information is available from the study websites and/or cohort profiles.
For inclusion in the present study, participants were required to have at least two values of BMI during the studied age range. The resulting sample comprised 13,220 boys (49.1% from the 2001 MCS) and 12,711 girls (50.1% from the 2001 MCS).
Child BMI data
In the 1958 NCDS, weight and height were measured at data collection sweeps at target ages of 7, 11, and 16 years. In the 2001 MCS, weight and height were measured at data collection sweeps at target ages of 7, 11, 14, and 17 years. All data were collected by trained individuals using similar instruments and measurement protocols. In total, there were 39,184 BMI observations for boys (55.9% from the 2001 MCS) and 38144 for girls (57.1% from the 2001 MCS). Supplementary Tables 1–3 provide detailed description of the BMI data.
Parental BMI data
In the 1958 NCDS, mothers’ weights were self-reported in 1969 (child aged 11 years) and heights were measured in 1958 (child aged 0 years), with missing height data supplemented from 1969 self-reports. Fathers’ weight and heights were both reported in 1969. While all the height data were recorded to the precision of one inch (2.54 cm), “weights were classified into one of 27 groups ranging from 6 stone 4 pounds (39.9 kg) to 19 stone 10 pounds (125.2 kg) in increments of 6 pounds (2.7 kg).” [19] Each parent was assigned a weight equal to the midpoint of their weight group. In the 2001 MCS, maternal and paternal body weights were self-reported, in stones & pounds or kilograms, at the 11-year sweep. Heights were also reported at the 11-year sweep, but the vast majority (95%) of these data were missing. Instead, we used maternal and paternal body heights self-reported, in feet & inches or centimetres, at the first (9-month) sweep. After converting all imperial data to metric, maternal and paternal BMIs were calculated as kg/m2. Weight status was defined as normal weight (<25.0 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30.0 kg/m2).
Covariates
In addition to birth cohort, offspring sex and ethnicity (white British vs other), and parental ages at the birth of the child, we considered three key measures of socioeconomic position. Tenure (own outright or mortgage vs other) was assessed at the 7-year sweep in the 1958 NCDS and at the 9-month sweep in the 2001 MCS. Father’s occupation was assessed at the 11-year sweep in both studies and was classified according to the Registrar General’s Social Class [30]. As in previous publications, for the 2001 MCS study only, we used 2618 observations of mother-figure occupational class when no father-figure was present in the household or when no valid father-figure occupational class data were available [31–33]. The age at which mothers left full time education was assessed at the 16-year sweep in the 1958 NCDS and at the 9-month sweep in the 2001 MCS.
In the 1958 NCDS, it was assumed that both mother and father were natural parents. In the 2001 MCS, the natural mother and natural father did the interviews in most cases. Nonetheless, we restricted all parental data in the 2001 MCS to that from natural parents.
Statistical analyses
Descriptive statistics were produced, stratified by sex, for all children, 1958 NCDS children, and 2001 MCS children.
A separate growth mixture model for each sex was developed to identify distinct groups of individuals who had similar BMI trajectories between 7 and 17 years of age. The base model included a linear trajectory and default specifications in Mplus (i.e., variance and covariance terms, and the residual variance at each time point, freely estimated but constrained to be the same in each class), with the addition of T-scores to account for the fact that measurements were not taken at discrete ages (i.e., not all BMI values were taken at exactly 7, 11, 14, 16, or 17 years of age). Subsequently, model development considered a quadratic function for the trajectory shape, allowing the residual variances to differ across classes, and allowing the intercept variance to differ across classes. For each step of development, models with 1–6 class solutions were run. Supplementary Tables 4 and 5 show how the Bayesian information criterion (BIC) substantially improved with each step of model development. More complex and flexible models (e.g., allowing auto-correlated residuals) were tested but either did not converge or did not improve model fit.
To avoid convergence at local minima [34], the final growth mixture models were fitted specifying up to 1,000,000 random starts (for 30 iterations), of which the best 200,000 models (according to log-likelihood) were run to completion (STARTS = 1,000,000 200,000; STITERATIONS = 30). A summary of the final mixture models, including measures of class separation, is presented in Supplementary Tables 6 and 7. Supplementary Figs. 1a and 2f show the average fitted trajectories, superimposed on the International Obesity Task Force (IOTF) weight status ranges, for each model (i.e., boys or girls) and class solution (e.g., 1–6). The best class solutions were selected based on model fit (e.g., BIC), quality of classification or separation between the classes (e.g., entropy), and plausibility and interpretability of the average trajectories.
To investigate the relationship of auxiliary independent variables (e.g., birth cohort or parental BMI) with class membership we used the 3-step BCH (named after Bolck, Croon, & Hagenaars) approach in Mplus, using full information maximum likelihood (FIML) to handle missing data [35]. Briefly, this approach can be thought of as a multinomial logistic regression which appropriately accounts for the uncertainty in class membership. In addition to estimated odds ratios (OR), we obtained sample statistics (e.g., mean value of each independent variable in any given model) for each class, weighted by estimated class probabilities. All analyses were performed for each sex separately.
Firstly, we ran models to estimate the relationships of birth cohort with class membership. We also did a crude analysis tabulating modal class membership against birth cohort.
Secondly, we estimated the relationships of parental height (cm/10), BMI, and weight status with class membership, considering mothers and fathers, and each exposure, separately. Four sets of models were run: 1) unadjusted, 2) adjusted for birth cohort, 3) testing for effect modification by birth cohort (BMI exposures only), and 4) fully adjusted for maternal or paternal age, tenure, occupational class, maternal age left full-time education, and birth cohort.
Thirdly, we considered maternal and paternal BMI, as well as their interaction, together in fully adjusted models. Because interactions in logistic models test departure from multiplicativity, we also computed and used the Relative Excess Risk due to Interaction (RERI) measure to test departure from additivity [36].
Fourthly, we tested a categorical exposure which considered maternal weight status and paternal weight status together (e.g., both parents had normal weight, mother (but not father) had overweight or obesity, father (but not mother) had overweight or obesity, both parents had overweight or obesity) in fully adjusted models. This analysis was also re-run with the following different groupings: both parents had normal weight, one parent had overweight, both parents had overweight, one or both parents had obesity. Supplementary Tables 8 and 9 describe how these exposures were computed.
As secondary analyses, we investigated the associations of each socioeconomic position variable with class membership, adjusting for birth cohort. In all models in this paper, occupational class and maternal education were entered as ridit scores for parsimony [37]. Presented estimates represent the contrast of the highest socioeconomic group (e.g., professional occupation) compared to the lowest (e.g., unskilled occupation).
Results
Table 1 shows the descriptive statistics. When considering both cohorts combined in the total columns, the prevalence of parental obesity was approximately 11–13% in all instances, while overweight was more common in fathers than mothers (e.g., 40 vs 28%),
Table 1.
Description of the study sample.
| Boys | Girls | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (N = 13,220) | 1958 NCDS (N = 6727) | 2001 MCS (N = 6493) | Total (N = 12,711) | 1958 NCDS (N = 6336) | 2001 MCS (N = 6375) | ||||
| % missing | % missing | ||||||||
| Cohort | 0 | 0 | |||||||
| 1958 NCDS | N (%) | 6727 (50.9) | 6336 (49.9) | ||||||
| 2001 MCS | N (%) | 6493 (49.1) | 6375 (50.1) | ||||||
| Ethnicity | 1.2 | 0.7 | |||||||
| White British | N (%) | 11849 (90.7) | 6435 (98.0) | 5414 (83.4) | 11422 (90.5) | 6129 (98.1) | 5293 (83.0) | ||
| Other | N (%) | 1209 (9.3) | 130 (2.0) | 1079 (16.6) | 1200 (9.5) | 118 (1.9) | 1082 (17.0) | ||
| Mother | |||||||||
| Age (years) | Mean (SD) | 28.2 (5.8) | 5.7 | 27.5 (5.7) | 28.9 (5.8) | 28.2 (5.8) | 5.0 | 27.5 (5.6) | 28.9 (5.8) |
| Height (cm) | Mean (SD) | 162.3 (6.8) | 5.3 | 161.1 (6.4) | 163.5 (6.9) | 162.4 (6.8) | 4.8 | 161.1 (6.4) | 163.7 (7.0) |
| BMI (kg/m2) | Median (IQR) | 24.0 (21.8, 27.3) | 17.3 | 23.6 (21.5, 26.3) | 24.8 (22.3, 28.5) | 24.0 (21.8, 27.1) | 16.8 | 23.4 (21.5, 26.0) | 24.9 (22.3, 28.5) |
| Underweight | N (%) | 285 (2.6) | 203 (3.4) | 82 (1.7) | 293 (2.8) | 204 (3.5) | 89 (1.9) | ||
| Normal weight | N (%) | 6195 (56.7) | 3726 (61.4) | 2469 (50.8) | 6056 (57.3) | 3652 (63.4) | 2404 (49.9) | ||
| Overweight | N (%) | 3022 (27.7) | 1618 (26.7) | 1404 (28.9) | 2882 (27.3) | 1439 (25.0) | 1443 (30.0) | ||
| Obese | N (%) | 1426 (13.1) | 520 (8.6) | 906 (18.6) | 1346 (12.7) | 465 (8.1) | 881 (18.3) | ||
| Father | |||||||||
| Age (years) | Mean (SD) | 31.3 (6.3) | 17.8 | 30.5 (6.4) | 32.2 (6.0) | 31.4 (6.2) | 17.8 | 30.6 (6.3) | 32.4 (6.0) |
| Height (cm) | Mean (SD) | 175.7 (7.6) | 29.2 | 174.5 (7.4) | 177.8 (7.3) | 175.8 (7.6) | 29.1 | 174.5 (7.5) | 177.9 (7.4) |
| BMI (kg/m2) | Median (IQR) | 25.1 (23.1, 27.6) | 31.8 | 24.5 (22.6, 26.6) | 26.8 (24.5, 29.7) | 25.2 (23.1, 27.7) | 31.7 | 24.5 (22.6, 26.6) | 26.8 (24.5, 29.4) |
| Underweight | N (%) | 65 (0.7) | 54 (0.9) | 11 (0.4) | 67 (0.8) | 51 (0.9) | 16 (0.5) | ||
| Normal weight | N (%) | 4299 (47.7) | 3354 (56.8) | 945 (30.4) | 4107 (47.3) | 3187 (57.2) | 920 (29.5) | ||
| Overweight | N (%) | 3625 (40.2) | 2170 (36.8) | 1455 (46.8) | 3553 (40.9) | 2032 (36.5) | 1521 (48.8) | ||
| Obese | N (%) | 1025 (11.4) | 325 (5.5) | 700 (22.5) | 955 (11.0) | 298 (5.4) | 657 (21.1) | ||
| Tenure | 6.8 | 5.8 | |||||||
| Own (outright or mortgage) | N (%) | 5735 (46.6) | 3511 (56.9) | 2224 (36.2) | 5601 (46.8) | 3364 (57.2) | 2237 (36.7) | ||
| Other | N (%) | 6581 (53.4) | 2655 (43.1) | 3926 (63.8) | 6370 (53.2) | 2517 (42.8) | 3853 (63.3) | ||
| ccupational class | 16.0 | 16.1 | |||||||
| I (Professional) | N (%) | 544 (4.9) | 284 (4.7) | 260 (5.2) | 537 (5.0) | 263 (4.6) | 274 (5.6) | ||
| II (Managerial and technical) | N (%) | 3326 (30.0) | 1193 (19.6) | 2133 (42.4) | 3225 (30.1) | 1153 (20.1) | 2072 (42.0) | ||
| IIIN (Skilled non-manual) | N (%) | 1329 (12.0) | 639 (10.5) | 690 (13.7) | 1265 (11.9) | 628 (11.0) | 637 (12.9) | ||
| IIIM (Skilled manual) | N (%) | 3702 (33.3) | 2563 (42.2) | 1139 (22.6) | 3410 (32.0) | 2318 (40.5) | 1092 (22.2) | ||
| IV (Partly-skilled) | N (%) | 1558 (14.0) | 888 (14.6) | 670 (13.3) | 1582 (14.8) | 879 (15.3) | 703 (14.3) | ||
| V (Unskilled) | N (%) | 645 (5.8) | 506 (8.3) | 139 (2.8) | 640 (6.0) | 488 (8.5) | 152 (3.1) | ||
| Maternal age left full-time education | 16.8 | 15.2 | |||||||
| ≥23 | N (%) | 407 (3.7) | 26 (0.5) | 381 (6.2) | 418 (3.9) | 16 (0.3) | 402 (6.6) | ||
| 21–22 | N (%) | 787 (7.2) | 63 (1.3) | 724 (11.8) | 827 (7.7) | 97 (2.1) | 730 (12.0) | ||
| 19–20 | N (%) | 536 (4.9) | 63 (1.3) | 473 (7.7) | 525 (4.9) | 69 (1.5) | 456 (7.5) | ||
| 18 | N (%) | 1090 (9.9) | 112 (2.3) | 978 (15.9) | 1120 (10.4) | 113 (2.4) | 1007 (16.6) | ||
| 17 | N (%) | 1075 (9.8) | 213 (4.4) | 862 (14.1) | 1017 (9.4) | 217 (4.6) | 800 (13.2) | ||
| 16 | N (%) | 2769 (25.2) | 590 (12.1) | 2179 (35.5) | 2706 (25.1) | 556 (11.9) | 2150 (35.3) | ||
| 15 | N (%) | 1892 (17.2) | 1462 (30.0) | 430 (7.0) | 1858 (17.2) | 1421 (30.3) | 437 (7.2) | ||
| 14 | N (%) | 2312 (21.0) | 2258 (46.4) | 54 (0.9) | 2177 (20.2) | 2126 (45.3) | 51 (0.8) | ||
| ≤13 | N (%) | 137 (1.2) | 83 (1.7) | 54 (0.9) | 129 (1.2) | 78 (1.7) | 51 (0.8) | ||
Latent classes
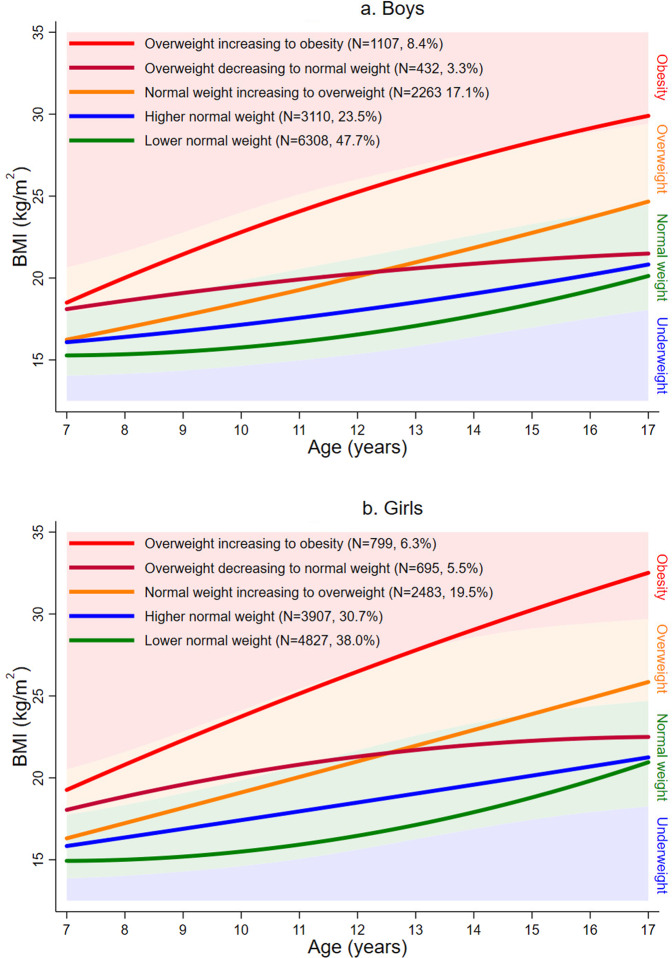
For both boys and girls, a mixture model with five classes provided the best representation of the serial BMI data and the most plausible solution. Figure 1a shows the average trajectories for each latent class for boys; Fig. 1b is for girls. The identified classes were similar for each sex and were thus the same nomenclature was used.
The largest class (47.7% of boys; 38.0% of girls) and second largest class (23.5% of boys; 30.7% of girls) had average trajectories that were consistently in the normal weight range. These classes are referred to as “lower normal weight” and “higher normal weight”, respectively.
The next largest class (17.1% of boys; 19.5% of girls) had an average trajectory that started in the normal weight range but ended in the overweight range. This class is referred to as “normal weight increasing to overweight”.
The next largest class (8.4% of boys; 6.3% of girls) had an average trajectory that started in the overweight range but ended in the obese range. This class is referred to as “overweight increasing to obesity”.
The final and smallest class (3.3% of boys; 5.5% of girls) had a mean trajectory that started in the overweight range but ended in the normal weight range. This class is referred to as “overweight decreasing to normal weight”.
Fig. 1. Average fitted trajectories from the final growth mixture models, superimposed on the IOTF underweight, normalweight, overweight, and obesity ranges.
a Boys. b Girls.
Supplementary Figs. 3a and 4e show the average fitted trajectories and individual observed trajectories for each class. And Supplementary Figs. 5a and 6e show the distributions of the posterior probabilities for assigned class membership.
Using model class assignments, more of the 2001 MCS children than the 1958 NCDS children were in the “normal weight increasing to overweight” class (e.g., 12.4 vs 3.5% for boys) and the “overweight increasing to obesity” class (e.g., 22.1 vs 13.5% for boys) (Table 2). Consequently, and as shown in Table 3, children in the 2001 MCS (compared to the 1958 NCDS) were estimated to have much higher odds of being in these classes (compared to the “lower normal weight” class). For example, girls in the 2001 MCS had 16.44 (11.87, 22.77) times higher odds of being the “overweight increasing to obesity” class and 4.57 (3.82, 4.45) times higher odds of being the “normal weight increasing to overweight” class. Children in the 2001 MCS also had higher odds of being in the “higher normal weight” and “overweight decreasing to normal weight” classes, although these estimates were considerably smaller.
Table 2.
Modal class membership tabulated against birth cohort, with column percentages, for each child sex.
| Boys | Girls | |||
|---|---|---|---|---|
| 1958 NCDS | 2001 MCS | 1958 NCDS | 2001 MCS | |
| Lower normal weight | 3861 (57.4) | 2447 (37.7) | 3047 (48.1) | 1780 (27.9) |
| Higher normal weight | 1605 (23.9) | 1505 (23.2) | 1926 (30.4) | 1981 (31.1) |
| Normal weight increasing to overweight | 831 (12.4) | 1432 (22.1) | 913 (14.4) | 1570 (24.6) |
| Overweight decreasing to normal weight | 197 (2.9) | 235 (3.6) | 309 (4.9) | 386 (6.1) |
| Overweight increasing to obesity | 233 (3.5) | 874 (13.5) | 141 (2.2) | 658 (10.3) |
Table 3.
Odds ratios for class membership according to birth cohort.
| Lower normal weight (referent) | Higher normal weight | Normal weight increasing to overweight | Overweight decreasing to normal weight | Overweight increasing to obesity | |||||
|---|---|---|---|---|---|---|---|---|---|
| % | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | |
| Boys | |||||||||
| Cohort | |||||||||
| 1958 NCDS (referent) | 65.7 | 51.8 | – | 34.0 | – | 50.1 | – | 17.6 | – |
| 2001 MCS | 34.3 | 48.2 | 1.78 (1.45, 2.20) | 66.0 | 3.72 (3.15, 4.39) | 49.9 | 1.91 (1.45, 2.51) | 82.4 | 8.99 (7.14, 11.33) |
| Girls | |||||||||
| Cohort | |||||||||
| 1958 NCDS (referent) | 70.7 | 47.0 | – | 34.6 | – | 49.0 | – | 12.8 | – |
| 2001 MCS | 29.3 | 53.0 | 2.72 (2.22, 3.34) | 65.4 | 4.57 (3.82, 5.45) | 51.0 | 2.51 (1.97, 3.19) | 87.2 | 16.44 (11.87, 22.77) |
Proportions and odds ratios weighted by estimated class probabilities using the 3-step BCH approach in Mplus.
Parental exposures and class membership
The fully adjusted estimates of the relationships of maternal and paternal height (cm/10), BMI, and weight status with class membership are shown in Table 4. The unadjusted and adjusted for birth cohort estimates are shown in Supplementary Tables 10 and 11. There was limited evidence that maternal or paternal height was associated with class membership, with the exception that, in boys, a 10 cm increase in maternal height was related to 0.86 (0.74, 0.99) times lower odds of being in the “overweight increasing to obesity” class (Table 4). Conversely, maternal BMI and paternal BMI were positively related to class membership in all instances, with the estimates being strongest for the “overweight increasing to obesity” contrast followed by the “normal weight increasing to overweight” contrast. As shown in Supplementary Table 12, there was limited evidence that these associations for parental BMI differed between the two birth cohorts. There was, however, some evidence that maternal obesity was more strongly related to odds of being in the “overweight increasing to obesity” class than paternal obesity (Table 4). For example, in boys, maternal obesity was associated with 11.65 (8.39, 16.17) times higher odds while paternal obesity was associated with 6.08 (4.18, 8.84) times higher odds.
Table 4.
Adjusted odds ratios for class membership according to maternal and paternal height, BMI, and weight status.
| Lower normal weight (referent) | Higher normal weight | Normal weight increasing to overweight | Overweight decreasing to normal weight | Overweight increasing to obesity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| x̄ or % | x̄ or % | OR (95% CI) | x̄ or % | OR (95% CI) | x̄ or % | OR (95% CI) | x̄ or % | OR (95% CI) | ||
| Boys | ||||||||||
| Mother | ||||||||||
| Model 1 | Height (cm/10) | 16.21 | 16.21 | 0.87 (0.73, 1.02) | 16.27 | 0.98 (0.86, 1.11) | 16.30 | 1.18 (0.96, 1.46) | 16.23 | 0.86 (0.74, 0.99) |
| Model 2 | BMI (kg/m2) | 23.4 | 25.3 | 1.13 (1.09, 1.17) | 26.1 | 1.16 (1.14, 1.19) | 25.2 | 1.12 (1.08, 1.16) | 28.9 | 1.25 (1.22, 1.29) |
| Model 3 | Weight Status | |||||||||
| Normal weight (referent) | 71.8 | 57.6 | – | 48.7 | – | 55.7 | – | 26.4 | – | |
| Overweight | 22.0 | 30.0 | 1.73 (1.31, 2.24) | 32.9 | 2.16 (1.76, 2.65) | 30.1 | 1.69 (1.20, 2.38) | 35.2 | 3.93 (3.01, 5.14) | |
| Obese | 6.2 | 12.4 | 2.47 (1.64, 3.77) | 18.4 | 3.82 (2.82, 5.19) | 14.2 | 2.62 (1.58, 4.33) | 38.4 | 11.65 (8.39, 16.17) | |
| Father | ||||||||||
| Model 4 | Height (cm/10) | 17.53 | 17.61 | 1.01 (0.86, 1.19) | 17.59 | 0.94 (0.83, 1.07) | 17.56 | 1.05 (0.83, 1.31) | 17.66 | 1.05 (0.89, 1.24) |
| Model 5 | BMI (kg/m2) | 24.6 | 25.6 | 1.08 (1.04, 1.13) | 27.2 | 1.18 (1.14, 1.22) | 25.9 | 1.11 (1.06, 1.17) | 28.5 | 1.22 (1.18, 1.27) |
| Model 6 | Weight Status | |||||||||
| Normal weight (referent) | 60.7 | 46.1 | – | 30.3 | – | 42.4 | – | 26.2 | – | |
| Overweight | 33.1 | 45.4 | 1.64 (1.27, 2.11) | 49.7 | 2.53 (2.02, 3.17) | 43.7 | 1.78 (1.25, 2.52) | 38.9 | 2.03 (1.48, 2.78) | |
| Obese | 6.2 | 8.5 | 1.39 (0.82, 2.38) | 20.0 | 4.15 (2.96, 5.81) | 13.9 | 2.73 (1.57, 4.76) | 34.9 | 6.08 (4.18, 8.84) | |
| Girls | ||||||||||
| Mother | ||||||||||
| Model 7 | Height (cm/10) | 16.16 | 16.29 | 1.10 (0.94, 1.28) | 16.27 | 1.08 (0.95, 1.23) | 16.18 | 0.88 (0.71, 1.09) | 16.31 | 1.12 (0.95, 1.33) |
| Model 8 | BMI (kg/m2) | 23.0 | 24.7 | 1.13 (1.09, 1.17) | 26.9 | 1.24 (1.20, 1.28) | 25.5 | 1.18 (1.14, 1.22) | 29.5 | 1.31 (1.27, 1.35) |
| Model 9 | Weight Status | |||||||||
| Normal weight (referent) | 76.1 | 62.9 | – | 40.0 | – | 54.8 | – | 26.7 | – | |
| Overweight | 18.7 | 28.5 | 1.86 (1.44, 2.41) | 37.1 | 3.54 (2.82, 4.45) | 30.5 | 2.22 (1.64, 3.01) | 32.7 | 4.27 (3.08, 5.91) | |
| Obese | 5.2 | 8.6 | 1.89 (1.18, 3.03) | 22.9 | 6.78 (4.84, 9.50) | 14.7 | 3.69 (2.37, 5.76) | 40.6 | 14.16 (9.49, 21.13) | |
| Father | ||||||||||
| Model 10 | Height (cm/10) | 17.51 | 17.65 | 1.06 (0.91, 1.23) | 17.57 | 0.94 (0.82, 1.08) | 17.62 | 1.08 (0.90, 1.30) | 17.58 | 0.90 (0.74, 1.09) |
| Model 11 | BMI (kg/m2) | 24.3 | 25.6 | 1.10 (1.06, 1.15) | 27.1 | 1.22 (1.18, 1.26) | 26.0 | 1.15 (1.11, 1.20) | 29.6 | 1.31 (1.26, 1.37) |
| Model 12 | Weight Status | |||||||||
| Normal weight (referent) | 63.3 | 47.2 | – | 31.9 | – | 38.1 | – | 18.1 | – | |
| Overweight | 31.3 | 44.4 | 1.65 (1.29, 2.11) | 49.4 | 2.57 (2.04, 3.23) | 51.4 | 2.46 (1.83, 3.31) | 40.9 | 3.00 (1.97, 4.56) | |
| Obese | 5.4 | 8.4 | 1.47 (0.90, 2.40) | 18.7 | 4.29 (2.99, 6.15) | 10.5 | 2.52 (1.45, 4.37) | 41.0 | 10.52 (6.62, 16.73) | |
Means/proportions and odds ratios weighted by estimated class probabilities using the 3-step BCH approach in Mplus, using FIML to handle missing data.
Models adjusted for ethnicity, maternal or paternal age, tenure, occupational class, maternal age left full-time education, and birth cohort.
Table 5 examines maternal and paternal BMI together in fully adjusted models. All the estimates were positive, with 95% CIs that did not cross one, indicating that both maternal BMI and paternal BMI were associated with class membership. There was no evidence of an interaction between maternal and paternal BMI suggesting no departure from multiplicativity. However, all RERI estimates were negative, with confidence intervals that did not cross zero, thereby providing evidence of negative departure from additivity. When considering maternal and paternal weight statuses together, the odds of being in the “overweight increasing to obesity” class was 9.01 (6.37, 12.75) times higher for boys, and 13.11 (8.74, 19.66) times higher for girls, whose parents both had overweight or obesity compared to children whose parents both had normal weight (Table 6). Supplementary Table 13 shows the estimates using the following different groupings: both parents had normal weight, one parent had overweight, both parents had overweight, one or both parents had obesity.
Table 5.
Adjusted odds ratios for class membership according to maternal and paternal BMI and their interaction.
| Lower normal weight (referent) | Higher normal weight | Normal weight increasing to overweight | Overweight decreasing to normal weight | Overweight increasing to obesity | ||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| Boys | ||||||
| Model 1 | Mothers BMI (kg/m2) | – | 1.12 (1.07, 1.17) | 1.15 (1.12, 1.18) | 1.11 (1.07, 1.15) | 1.24 (1.20, 1.28) |
| Fathers BMI (kg/m2) | – | 1.07 (1.02, 1.12) | 1.16 (1.12, 1.20) | 1.11 (1.05, 1.17) | 1.20 (1.16, 1.25) | |
| Interaction | – | 0.99 (0.98, 1.01) | 1.00 (0.99, 1.00) | 1.00 (0.98, 1.01) | 0.99 (0.98, 1.00) | |
| RERI | −0.20 (−0.26, −0.13) | −0.32 (−0.36, −0.27) | −0.22 (−0.29, −0.15) | −0.45 (−0.51, −0.38) | ||
| Girls | ||||||
| Model 2 | Mothers BMI (kg/m2) | – | 1.12 (1.08, 1.17) | 1.22 (1.18, 1.26) | 1.17 (1.13, 1.21) | 1.28 (1.24, 1.33) |
| Fathers BMI (kg/m2) | – | 1.09 (1.05, 1.14) | 1.19 (1.15, 1.24) | 1.14 (1.09, 1.19) | 1.28 (1.22, 1.34) | |
| Interaction | – | 0.99 (0.98, 1.00) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | |
| RERI | −0.23 (−0.29, −0.16) | −0.40 (−0.46, −0.34) | −0.31 (−0.37, −0.25) | −0.56 (−0.64, −0.49) | ||
Odds ratios weighted by estimated class probabilities using the 3-step BCH approach in Mplus, using FIML to handle missing data.
Models adjusted for ethnicity, maternal and paternal age, tenure, occupational class, maternal age left full-time education, and birth cohort.
Mothers BMI and Fathers BMI were each grand mean centred before computing the interaction term.
RERI relative excess risk due to interaction.
Table 6.
Adjusted odds ratios for class membership according to different combinations of maternal and paternal weight status.
| Lower normal weight (referent) | Higher normal weight | Normal weight increasing to overweight | Overweight decreasing to normal weight | Overweight increasing to obesity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | ||
| Boys | ||||||||||
| Model 1 | Both parents’ normal weight (referent) | 49.9 | 32.8 | – | 25.4 | – | 32.1 | – | 15.5 | – |
| Mother (but not father) overweight or obese | 17.3 | 24.1 | 2.15 (1.60, 2.90) | 24.4 | 2.60 (2.03, 3.32) | 21.8 | 1.82 (1.20, 2.77) | 41.4 | 6.47 (4.83, 8.67) | |
| Father (but not mother) overweight or obese | 23.2 | 26.6 | 1.71 (1.29, 2.25) | 26.7 | 2.32 (1.84, 2.92) | 24.2 | 1.64 (1.11, 2.42) | 19.6 | 3.08 (2.23, 4.25) | |
| Both parents overweight or obese | 9.6 | 16.5 | 2.64 (1.84, 3.79) | 23.5 | 5.12 (3.88, 6.72) | 21.9 | 3.53 (2.31, 5.39) | 23.5 | 9.01 (6.37, 12.75) | |
| Girls | ||||||||||
| Model 2 | Both parents’ normal weight (referent) | 54.4 | 37.6 | – | 21.7 | – | 28.7 | – | 17.0 | – |
| Mother (but not father) overweight or obese | 14.4 | 21.4 | 2.20 (1.63, 2.97) | 29.1 | 4.65 (3.54, 6.09) | 24.1 | 3.12 (2.19, 4.43) | 35.9 | 6.51 (4.58, 9.26) | |
| Father (but not mother) overweight or obese | 23.0 | 26.4 | 1.69 (1.31, 2.18) | 22.9 | 2.69 (2.08, 3.49) | 28.8 | 2.36 (1.71, 3.25) | 18.7 | 3.17 (2.16, 4.65) | |
| Both parents overweight or obese | 8.2 | 14.6 | 2.69 (1.88, 3.87) | 26.3 | 8.73 (6.40, 11.91) | 18.4 | 4.24 (2.81, 6.39) | 28.4 | 13.11 (8.74, 19.66) | |
Odds ratios weighted by estimated class probabilities using the 3-step BCH approach in Mplus, using FIML to handle missing data.
Models adjusted for ethnicity, maternal and paternal age, tenure, occupational class, maternal age left full-time education, and birth cohort.
Socioeconomic position and class membership
As shown in Supplementary Table 14, lower socioeconomic position (for each of the three variables considered) was associated with higher odds of belonging to the “overweight increasing to obesity” class (compared to the largest normal weight class).
Discussion
This paper demonstrates the application of growth mixture modelling to serial BMI data pooled from two birth cohort studies, one born in 1958 before the obesity epidemic and one born in 2001 during the obesity epidemic. By using this approach, we were able to describe the secular change in paediatric BMI trajectories in more realistic and holistic terms than just a change in the mean BMI or levels of overweight and obesity. Only a handful of other studies have employed this theoretically interesting and realistic analytical strategy [7, 12, 38]. Most strikingly, we found that more than 1 in 10 children in the 2001 MCS were in the most deleterious “overweight increasing to obesity” class, compared to less than 1 in 30 in the 1958 NCDS. The obesity epidemic in the UK is therefore explained, at least in part, by a dramatic increase in the number of pre-pubertal children with overweight becoming obese during adolescence. This is particularly worrying given that adolescent BMI gains are more strongly related (than childhood BMI gains) to increases in visceral adiposity [39], tissue which plays a role in many pathological processes. Indeed, BMI increase during puberty is more strongly related to cardiovascular mortality than BMI during childhood [40].
Maternal and paternal BMI were associated with latent class membership, with evidence of negative departure from additivity. This means that the combined effect of maternal and paternal BMI was smaller than the sum of the individual effects of these two exposures. Conversely, we found no evidence of departure from multiplicativity. This is in agreement with previous studies, including those using data from the 1970 British Cohort Study (BCS) [10, 20]. This other nationally representative cohort was not used in the present analysis because BMI was only available at 10 and 16 years of age, nearly one-third of the 16-year measurements were self-reported, and the response rate at 16 years was low (for reasons that have been explained elsewhere) [20]. Our reported estimates for maternal BMI and paternal BMI were generally of a similar magnitude, suggesting that, if causal, both exposures are equally important targets to stop the intergenerational transmission of high BMI. Similarly, investigating latent patterns of BMI development between 10 and 42 years of age in the 1970 BCS, Viner et al reported that maternal and paternal BMI were related to 1.10 (1.07, 1.13) and 1.08 (1.04, 1.13), respectively, times higher odds of their child belonging to an “adolescent and young adult-onset obesity” class compared to a “normative” class [10]. These findings do not support the foetal overnutrition hypothesis that, if the intrauterine environment is an independent factor for offspring obesity development (e.g., due to long-lasting biological effects of maternal adiposity during pregnancy on foetal energy metabolism and the endocrine system), the effect of maternal BMI will be stronger than that for paternal BMI [41]. We did find some evidence that maternal obesity was more strongly related to odds of being in the “overweight increasing to obesity” class than paternal obesity, particularly for boys. However, ORs are on a relative scale and this finding is influenced by a lower percentage of fathers than mothers having normal weight (due to a higher percentage of fathers than mothers having overweight) [42]. While some individual studies have found maternal BMI to be more strongly related to childhood BMI than paternal BMI [43, 44], a published systematic review of the literature found limited evidence to support this proposition and thus the foetal overnutrition hypothesis [45].
The most comparable study to ours was conducted by Nedelec et al and published in this journal in 2021 [7]. Those authors developed a sex-combined growth mixture model to describe latent patterns of BMI Z-score change between 2 and 18 years of age using data from 12,040 Finnish children born in either 1966 or 1986. Of the four identified latent classes, the most obesogenic comprised 3.7% of the sample and demonstrated an average trajectory that increased from approximately the 85th (internal) centile to above the 99th centile by 7 years of age, before plateauing. Conversely, for each sex, our “overweight increasing to obesity” class was near the 90th centile of the IOTF charts at 7 years of age, increasing to approximately the 99th centile by 17 years of age. The most recent cohort in our study was born in 2001, while the most recent cohort in the Nedelec et al study was born in 1986. Given what we know about secular trends in BMI trajectories [11], it makes sense that our most obesogenic trajectory class (which mainly comprised children born in 2001) 1) crossed upwards though the centiles while Nedelec et al’s did not and 2) comprised 8.4% of boys and 6.3% of girls while Nedelec et al.’s comprised only 3.7% of boys and girls. The other classes were also not similar between the two studies. In addition to the different populations being studied and the different growth charts used for comparison, this is likely to reflect quite different growth mixture modelling strategies [46, 47]. Further, Nedelec et al only investigated maternal BMI (and not weight status) while we were able to consider the individual and combined associations of maternal and paternal BMI (and weight status) with class membership.
While there are known biological mechanisms through which maternal BMI can influence offspring BMI (e.g., placental function and altered breast milk composition) [48–50], the associations observed in the present study between parental BMI and latent patterns of offspring BMI development are also due to the complex interplay of genetics, epigenetics, and the shared family environment. BMI between 7 and 17 years of age is highly heritable and there will not have been any change in the gene pool during the studied time period, perhaps except for that due to an increase in ethnic diversity [51, 52]. We do, however, know that genetic variants for obesity have stronger effects in obesogenic environments [53, 54]. Such gene-by-environment interactions may partly underlie the strong reported associations of parental obesity with membership of the, predominately 2001 cohort, “overweight increasing to obesity” class. We also know that assortative mating for BMI has increased alongside the obesity epidemic [55]. This phenomenon may have increased genetic predisposition to obesity in the 2001 cohort children, but the (theoretically) stronger tendency of a mother and father to have similar BMI values in the 2001 (compared to 1958) cohort could also influence offspring BMI due to non-genetic factors [56]. Our analysis investigating the associations of parental BMI with latent patterns of offspring BMI development did adjust for traditional confounders, but we did not consider the mediating role of the shared family environment. This is a particularly important consideration for future work as it is modifiable.
The main strength of the paper lies in the data (i.e., 25,931 children, with serial objective BMI measurements, from two birth cohorts) and meticulous development of the growth mixture model. Our model development process considered several age functions for the trajectory shape, removal of default constraints on the growth term variances and covariances, different specifications of the within-class residual variance/error structure, and different autocorrelation structures [46]. Unlike the majority of other BMI growth mixture modelling papers in the literature [57], our analysis addressed all of the points on the Guidelines for Reporting on Latent Trajectory Studies (GRoLTS) Checklist [58]. As the specification of growth mixture models become more refined, it is common for model fit to improve (e.g., lower BIC) but for the degree of separation between the classes to deteriorate (e.g., lower entropy) [47]. This is exactly what we observed, and we acknowledge the limitation that our final models had low entropy (0.55 for boys; 0.52 for girls). We did, however, properly account for the uncertainty in class membership by using the 3-step BCH method of investigating auxiliary variables. Simulation studies have shown that, except in large sample sizes (N ≥ 10,000), estimates (e.g., of associations of auxiliary variables with class membership) using the BCH approach can be biased in situations where the entropy is very low (≤0.5) [59, 60]. The entropy in our models was low, but our estimates our unlikely to be biased (due to uncertainty in class assignment) because our sample size was very large (N~13,000 for each growth mixture model). A common mistake (according to van de Schoot et al) is to consider entropy during model development, ultimately leading to choosing a final model that has good entropy but poor model fit and less informative classes [58]. We did not make this mistake and are confident that our classes approximately reflect “real”, for want of another word, sub-populations of children.
Most of the paternal weight and height data were self-reported. Because people tend to overestimate their height and underestimate their weight, particularly if they are female and/or have obesity [61], corresponding BMI is underestimated. As a result, our estimates might be biased away from the null; the true effects of maternal and paternal BMI on offspring latent BMI class membership might be weaker than reported in the present paper. While both the 1958 NCDS and 2001 MCS were designed to be nationally representative, our sample was limited to approximately 70% of each cohort. This is a relatively large proportion compared to many other published studies using these cohorts. Nonetheless, we do acknowledge that differential selection into our sample may have also biased results [62]. Finally, BMI is a far from perfect index and indicator of adiposity [63, 64]. Some of the differences between classes in mean BMI trajectories might reflect underlying differences in child height, pubertal timing, and body composition. It is also reasonable to question whether part of the observed associations of parental BMI with offspring latent BMI class membership might be driven by intergenerational transmission of stature. However, we think this is unlikely given that 1) height and BMI are negatively correlated in adulthood but positively correlated in much of childhood and adolescence [63] and 2) maternal and paternal height were not strongly associated with class membership in our analyses.
In conclusion, from before to well during the obesity epidemic era in the UK, there has been a four-fold increase in the proportion of children belonging to a sub-population characterised by overweight at 7 years progressing to obesity at 17 years. Our results implicate excess parental BMI as a correlate of this secular change because 1) more than one-third of the mothers and fathers of this sub-population had obesity (and more than one additional third had overweight but not obesity) and 2) maternal and paternal obesity were associated with very higher odds of their children belonging to this sub-population. There has also been a two-fold increase in the proportion of children belonging to a larger sub-population characterised by normal weight at 7 years progressing to overweight at 17 years, but this group is unlikely to represent the “low-hanging fruit” or priority for targeted intervention programmes. In addition to providing further evidence on the need to break the strong intergenerational transmission of obesity risk, our findings emphasise the need for a national adolescent weight gain monitoring programme.
Supplementary information
Acknowledgements
This work was funded by the UK Medical Research Council (WJ New Investigator Research Grant: MR/P023347/1). WJ acknowledges support from the National Institute for Health Research (NIHR) Leicester Biomedical Research Centre, which is a partnership between University Hospitals of Leicester NHS Trust, Loughborough University, and the University of Leicester. SMPP was supported by a UK Medical Research Council Career Development Award (ref: MR/P020372/1). JLB acknowledges support from the Novo Nordisk Foundation (NNF21OC0067346).
Author contributions
WJ conceptualised the study, carried out the analyses, and drafted the initial manuscript. All authors made substantial contributions to the interpretation of the data, revised the manuscript critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Data availability
The datasets analysed during the current study are available in the UK Data Archive repository, https://www.data-archive.ac.uk/.
Code availability
Available from the first author upon request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41366-022-01237-6.
References
- 1.The Health and Social Care Information Centre. The National Child Measurement Programme: England, 2019/20 school year. London, UK: The Health and Social Care Information Centre; 2020.
- 2.Fuller E, Mindell J, Prior G. Health survey for England 2018. London, UK: NHS Digital; 2018.
- 3.Alberga AS, Sigal RJ, Goldfield G, Prud’homme D, Kenny GP. Overweight and obese teenagers: why is adolescence a critical period? Pediatr Obes. 2012;7:261–73. doi: 10.1111/j.2047-6310.2011.00046.x. [DOI] [PubMed] [Google Scholar]
- 4.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59:955–9. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 5.Buscot MJ, Thomson RJ, Juonala M, Sabin MA, Burgner DP, Lehtimaki T, et al. Distinct child-to-adult body mass index trajectories are associated with different levels of adult cardiometabolic risk. Eur Heart J. 2018;39:2263–70. doi: 10.1093/eurheartj/ehy161. [DOI] [PubMed] [Google Scholar]
- 6.Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Body mass index trajectories in childhood is predictive of cardiovascular risk: results from the 23-year longitudinal Georgia Stress and Heart study. Int J Obes. 2018;42:923–5. doi: 10.1038/ijo.2017.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nedelec R, Miettunen J, Mannikko M, Jarvelin MR, Sebert S. Maternal and infant prediction of the child BMI trajectories; studies across two generations of Northern Finland birth cohorts. Int J Obes. 2021;45:404–14. doi: 10.1038/s41366-020-00695-0. [DOI] [PubMed] [Google Scholar]
- 8.Norris T, Mansukoski L, Gilthorpe MS, Hamer M, Hardy R, Howe LD, et al. Distinct body mass index trajectories to young-adulthood obesity and their different cardiometabolic consequences. Arterioscler Thromb Vasc Biol. 2021;41:1580–93. doi: 10.1161/ATVBAHA.120.315782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oluwagbemigun K, Buyken AE, Alexy U, Schmid M, Herder C, Nothlings U. Developmental trajectories of body mass index from childhood into late adolescence and subsequent late adolescence-young adulthood cardiometabolic risk markers. Cardiovasc Diabetol. 2019;18:9. doi: 10.1186/s12933-019-0813-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Viner RM, Costa S, Johnson W. Patterns of BMI development between 10 and 42 years of age and their determinants in the 1970 British Cohort Study. J Epidemiol Community Health. 2019;73:79–85. doi: 10.1136/jech-2018-211051. [DOI] [PubMed] [Google Scholar]
- 11.Johnson W, Li L, Kuh D, Hardy R. How has the age-related process of overweight or obesity development changed over time? Co-ordinated analyses of individual participant data from five United Kingdom birth cohorts. PLoS Med. 2015;12:e1001828. doi: 10.1371/journal.pmed.1001828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Norris T, Hamer M, Hardy R, Li L, Ong KK, Ploubidis GB, et al. Changes over time in latent patterns of childhood-to-adulthood BMI development in Great Britain: evidence from three cohorts born in 1946, 1958, and 1970. BMC Med. 2021;19:96. doi: 10.1186/s12916-021-01969-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graversen L, Howe LD, Sorensen TI, Sovio U, Hohwu L, Tilling K, et al. Body mass index trajectories from 2 to 18 years - exploring differences between European cohorts. Pediatr Obes. 2017;12:102–9. doi: 10.1111/ijpo.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson W, Soloway LE, Erickson D, Choh AC, Lee M, Chumlea WC, et al. A changing pattern of childhood BMI growth during the 20th century: 70 y of data from the Fels Longitudinal Study. Am J Clin Nutr. 2012;95:1136–43. doi: 10.3945/ajcn.111.022269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell JM, McPherson NO. Influence of increased paternal BMI on pregnancy and child health outcomes independent of maternal effects: a systematic review and meta-analysis. Obes Res Clin Pract. 2019;13:511–21. doi: 10.1016/j.orcp.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L, et al. The association between maternal body mass index and child obesity: a systematic review and meta-analysis. PLoS Med. 2019;16:e1002817. doi: 10.1371/journal.pmed.1002817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper R, Hypponen E, Berry D, Power C. Associations between parental and offspring adiposity up to midlife: the contribution of adult lifestyle factors in the 1958 British Birth Cohort Study. Am J Clin Nutr. 2010;92:946–53. doi: 10.3945/ajcn.2010.29477. [DOI] [PubMed] [Google Scholar]
- 18.Power C, Pouliou T, Li L, Cooper R, Hypponen E. Parental and offspring adiposity associations: insights from the 1958 British birth cohort. Ann Hum Biol. 2011;38:390–9. doi: 10.3109/03014460.2011.591827. [DOI] [PubMed] [Google Scholar]
- 19.Lake JK, Power C, Cole TJ. Child to adult body mass index in the 1958 British birth cohort: associations with parental obesity. Arch Dis Child. 1997;77:376–81. doi: 10.1136/adc.77.5.376. [DOI] [PubMed] [Google Scholar]
- 20.Costa S, Johnson W, Viner R. Additive influences of maternal and paternal body mass index on weight status trajectories from childhood to mid-adulthood in the 1970 British Cohort Study. Longitudinal Life Course Studies. 2015;6:147–72. doi: 10.14301/llcs.v6i2.301. [DOI] [Google Scholar]
- 21.Fantin R, Delpierre C, Dimeglio C, Lamy S, Barboza Solis C, Charles MA, et al. Disentangling the respective roles of the early environment and parental BMI on BMI change across childhood: a counterfactual analysis using the Millennium Cohort Study. Prev Med. 2016;89:146–53. doi: 10.1016/j.ypmed.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 22.Dos Santos CS, Picoito J, Nunes C, Loureiro I. Early individual and family predictors of weight trajectories from early childhood to adolescence: results from the millennium cohort study. Front Pediatr. 2020;8:417. doi: 10.3389/fped.2020.00417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norris T, Mansukoski L, Gilthorpe MS, Hamer M, Hardy R, Howe LD, et al. Early childhood weight gain: latent patterns and body composition outcomes. Paediatr Perinat Epidemiol. 2021;35:557–68. doi: 10.1111/ppe.12754. [DOI] [PubMed] [Google Scholar]
- 24.Pryor LE, Tremblay RE, Boivin M, Touchette E, Dubois L, Genolini C, et al. Developmental trajectories of body mass index in early childhood and their risk factors: an 8-year longitudinal study. Arch Pediatr Adolesc Med. 2011;165:906–12. doi: 10.1001/archpediatrics.2011.153. [DOI] [PubMed] [Google Scholar]
- 25.Richardson SS, Daniels CR, Gillman MW, Golden J, Kukla R, Kuzawa C, et al. Society: don’t blame the mothers. Nature. 2014;512:131–2. doi: 10.1038/512131a. [DOI] [PubMed] [Google Scholar]
- 26.Sharp GC, Schellhas L, Richardson SS, Lawlor DA. Time to cut the cord: recognizing and addressing the imbalance of DOHaD research towards the study of maternal pregnancy exposures. J Dev Orig Health Dis. 2019;10:509–12. doi: 10.1017/S2040174419000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mansukoski L, Johnson W. How can two biological variables have opposing secular trends, yet be positively related? A demonstration using timing of puberty and adult height. Ann Hum Biol. 2020;47:549–54. doi: 10.1080/03014460.2020.1795256. [DOI] [PubMed] [Google Scholar]
- 28.Power C, Elliott J. Cohort profile: 1958 British birth cohort (National Child Development Study) Int J Epidemiol. 2006;35:34–41. doi: 10.1093/ije/dyi183. [DOI] [PubMed] [Google Scholar]
- 29.Hansen K. Millennium Cohort Study first, second, third and fourth surveys: a guide to the datasets. London, UK: Centre for Longitudinal Studies, University of London; 2012.
- 30.Bland R. Measuring “social class”: a discussion of the Registrar-General’s Classification. Sociology. 1979;13:283–91. doi: 10.1177/003803857901300209. [DOI] [Google Scholar]
- 31.Bann D, Johnson W, Li L, Kuh D, Hardy R. Socioeconomic inequalities in childhood and adolescent body-mass index, weight, and height from 1953 to 2015: an analysis of four longitudinal, observational, British birth cohort studies. Lancet. Public Health. 2018;3:e194–e203. doi: 10.1016/S2468-2667(18)30045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson W, Bann D, Hardy R. Infant weight gain and adolescent body mass index: comparison across two British cohorts born in 1946 and 2001. Arch Dis Child. 2018;103:974–80. doi: 10.1136/archdischild-2017-314079. [DOI] [PubMed] [Google Scholar]
- 33.Johnson W, Norris T, De Freitas R, Pearson N, Hamer M, Costa S. Is the positive relationship of infant weight gain with adolescent adiposity attenuated by moderate-to-vigorous physical activity in childhood? Evidence from the Millennium Cohort Study. Int J Obes. 2021;45:84–94. doi: 10.1038/s41366-020-00656-7. [DOI] [PubMed] [Google Scholar]
- 34.Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychol Methods. 2006;11:36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- 35.Bolck A, Croon M, Hagenaars J. Estimating latent structure models with categorical variables: one-step versus three-step estimators. Political Anal. 2004;12:3–27. doi: 10.1093/pan/mph001. [DOI] [Google Scholar]
- 36.VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Methods. 2014;3:33–72. [Google Scholar]
- 37.Bross IDJ. How to use ridit analysis. Biometrics. 1958;14:18–38. doi: 10.2307/2527727. [DOI] [Google Scholar]
- 38.Sperrin M, Marshall AD, Higgins V, Buchan IE, Renehan AG. Slowing down of adult body mass index trend increases in England: a latent class analysis of cross-sectional surveys (1992-2010) Int J Obes. 2014;38:818–24. doi: 10.1038/ijo.2013.161. [DOI] [PubMed] [Google Scholar]
- 39.Kindblom JM, Lorentzon M, Hellqvist A, Lonn L, Brandberg J, Nilsson S, et al. BMI changes during childhood and adolescence as predictors of amount of adult subcutaneous and visceral adipose tissue in men: the GOOD Study. Diabetes. 2009;58:867–74. doi: 10.2337/db08-0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ohlsson C, Bygdell M, Sonden A, Rosengren A, Kindblom JM. Association between excessive BMI increase during puberty and risk of cardiovascular mortality in adult men: a population-based cohort study. Lancet Diabetes Endocrinol. 2016;4:1017–24. doi: 10.1016/S2213-8587(16)30273-X. [DOI] [PubMed] [Google Scholar]
- 41.Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11:496–506. doi: 10.1038/oby.2003.69. [DOI] [PubMed] [Google Scholar]
- 42.Kim HY. Statistical notes for clinical researchers: risk difference, risk ratio, and odds ratio. Restor Dent Endod. 2017;42:72–6. doi: 10.5395/rde.2017.42.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lawlor DA, Smith GD, O’Callaghan M, Alati R, Mamun AA, Williams GM, et al. Epidemiologic evidence for the fetal overnutrition hypothesis: findings from the mater-university study of pregnancy and its outcomes. Am J Epidemiol. 2007;165:418–24. doi: 10.1093/aje/kwk030. [DOI] [PubMed] [Google Scholar]
- 44.Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels Longitudinal Study. Pediatr Obes. 2013;8:159–69. doi: 10.1111/j.2047-6310.2012.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patro B, Liber A, Zalewski B, Poston L, Szajewska H, Koletzko B. Maternal and paternal body mass index and offspring obesity: a systematic review. Ann Nutr Metab. 2013;63:32–41. doi: 10.1159/000350313. [DOI] [PubMed] [Google Scholar]
- 46.Gilthorpe MS, Dahly DL, Tu YK, Kubzansky LD, Goodman E. Challenges in modelling the random structure correctly in growth mixture models and the impact this has on model mixtures. J Dev Orig Health Dis. 2014;5:197–205. doi: 10.1017/S2040174414000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sijbrandij JJ, Hoekstra T, Almansa J, Peeters M, Bultmann U, Reijneveld SA. Variance constraints strongly influenced model performance in growth mixture modeling: a simulation and empirical study. BMC Med Res Methodol. 2020;20:276. doi: 10.1186/s12874-020-01154-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fields DA, George B, Williams M, Whitaker K, Allison DB, Teague A, et al. Associations between human breast milk hormones and adipocytokines and infant growth and body composition in the first 6 months of life. Pediatr Obes. 2017;12:78–85. doi: 10.1111/ijpo.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Isganaitis E, Venditti S, Matthews TJ, Lerin C, Demerath EW, Fields DA. Maternal obesity and the human milk metabolome: associations with infant body composition and postnatal weight gain. Am J Clin Nutr. 2019;110:111–20. doi: 10.1093/ajcn/nqy334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kelly AC, Powell TL, Jansson T. Placental function in maternal obesity. Clin Sci. 2020;134:961–84. doi: 10.1042/CS20190266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choh AC, Lee M, Kent JW, Diego VP, Johnson W, Curran JE, et al. Gene-by-age effects on BMI from birth to adulthood: the Fels Longitudinal Study. Obesity. 2014;22:875–81. doi: 10.1002/oby.20517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stunkard AJ, Foch TT, Hrubec Z. A twin study of human obesity. JAMA. 1986;256:51–4. doi: 10.1001/jama.1986.03380010055024. [DOI] [PubMed] [Google Scholar]
- 53.Demerath EW, Choh AC, Johnson W, Curran JE, Lee M, Bellis C, et al. The positive association of obesity variants with adulthood adiposity strengthens over an 80-year period: a gene-by-birth year interaction. Hum Hered. 2013;75:175–85. doi: 10.1159/000351742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rokholm B, Silventoinen K, Tynelius P, Gamborg M, Sorensen TI, Rasmussen F. Increasing genetic variance of body mass index during the Swedish obesity epidemic. PLoS One. 2011;6:e27135. doi: 10.1371/journal.pone.0027135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ajslev TA, Angquist L, Silventoinen K, Gamborg M, Allison DB, Baker JL, et al. Assortative marriages by body mass index have increased simultaneously with the obesity epidemic. Front Genet. 2012;3:125. doi: 10.3389/fgene.2012.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hebebrand J, Wulftange H, Goerg T, Ziegler A, Hinney A, Barth N, et al. Epidemic obesity: are genetic factors involved via increased rates of assortative mating? Int J Obes Relat Metab Disord. 2000;24:345–53. doi: 10.1038/sj.ijo.0801135. [DOI] [PubMed] [Google Scholar]
- 57.Mattsson M, Maher GM, Boland F, Fitzgerald AP, Murray DM, Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes Rev. 2019;20:998–1015. doi: 10.1111/obr.12842. [DOI] [PubMed] [Google Scholar]
- 58.van de Schoot R, Sijbrandij M, Winter SD, Depaoli S, Vermunt JK. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct Equ Model Multidiscip J. 2017;24:451–67.. doi: 10.1080/10705511.2016.1247646. [DOI] [Google Scholar]
- 59.Asparouhov T, Muthen B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Version 11. Mplus Web Notes: No. 21. 2021. www.statmodel.com/examples/webnotes/webnote21.pdf.
- 60.Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Political Anal. 2010;18:450–69. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
- 61.Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001-2006. Prev Chronic Dis. 2009;6:A121. [PMC free article] [PubMed] [Google Scholar]
- 62.Munafo MR, Tilling K, Taylor AE, Evans DM, Davey, Smith G. Collider scope: when selection bias can substantially influence observed associations. Int J Epidemiol. 2018;47:226–35. doi: 10.1093/ije/dyx206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnson W, Norris T, Bann D, Cameron N, Wells JK, Cole TJ, et al. Differences in the relationship of weight to height, and thus the meaning of BMI, according to age, sex, and birth year cohort. Ann Hum Biol. 2020;47:199–207. doi: 10.1080/03014460.2020.1737731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wells JC, Coward WA, Cole TJ, Davies PS. The contribution of fat and fat-free tissue to body mass index in contemporary children and the reference child. Int J Obes Relat Metab Disord. 2002;26:1323–8. doi: 10.1038/sj.ijo.0802077. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analysed during the current study are available in the UK Data Archive repository, https://www.data-archive.ac.uk/.
Available from the first author upon request.