Abstract
Background
Acute mesenteric ischemia (AMI) may present in COVID-19 patients without the classic risk factors of AMI, and the symptoms might confuse physicians, leading to delayed diagnosis and increased mortality. In this manuscript, we report a patient with COVID-19 who presented with AMI as its initial presenting symptom.
Case presentation
A 68-year-old man presented to the emergency room with periumbilical non-radiating pain that had started three days before the admission. He had no defecation or gas passing in the past three days. In the physical exam, the patient had guarding of the abdomen, generalized tenderness, and rebound tenderness. C-reactive protein, Creatine phosphokinase and WBC count were elevate. Abdominal X-ray in the supine position was suggestive of obstruction of the small intestine. Diagnostic laparotomy was performed because of peritonitis and acute abdominal pain. The diagnosis was mesenteric ischemia due to vein thrombosis based on laparotomy and paraclinic findings. In the post-surgery evaluations COVID-19 infection was confirmed based on PCR and chest CT scan.
Discussion
Based on paraclinical, clinical, and diagnostic laparotomy findings, the patient was diagnosed with small bowel obstruction and gangrene due to acute mesenteric ischemia (AMI). But as described, this patient didn't have any history of medical diseases that cause a hypercoagulable state, in the past. While AF was ruled out because his ECG was normal. We concluded that in this patient AMI was due to his infection with COVID-19.
Conclusion
Patients with COVID-19 may not have the typical risk factors for AMI, and AMI diagnosis should be considered in patients presenting with acute abdominal pain, even without the routine risk factors.
Abbreviations: AMI, acute mesenteric ischemia; AF, atrial fibrillation; ACE2, angiotensin-converting-enzyme-2; BP, blood pressure; BPM, beats per minute; COVID-19, Coronavirus Disease 2019; CPK, Creatine phosphokinase; CT, computed tomography; ECG, electrocardiogram; GI, Gastrointestinal; ICU, intensive care units; LUQ, left upper quadrant; NPO, non-per os; PCR, polymerase chain reaction; RR, respiratory rate; RLQ, right lower quadrants; VBG, venous blood gas; WBC, White blood cell
Keywords: Case report, Acute mesenteric ischemia, COVID-19, Acute abdominal pain, Side to side resection anastomosis, General surgery
Highlights
-
•
Acute mesenteric ischemia may present in COVID-19 patients without the classic risk factors of AMI.
-
•
In this manuscript, we report a patient with COVID-19 who presented with AMI as its initial presenting symptom.
-
•
AMI diagnosis should be considered in patients presenting with acute abdominal pain, even without the routine risk factors.
1. Introduction
Coronavirus Disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was first identified in December 2019 in Wuhan, China [1]. The most common COVID-19 symptoms contain fever (85.6 %), cough (65.7 %), fatigue (42.4 %) and dyspnea (21.4%) [2]. However, a significant number of patients experience extrapulmonary symptoms, which can increase morbidity and mortality of COVID-19. Gastrointestinal (GI) symptoms are one of the commonly reported symptoms in patients with COVID-19, which is reported in over two third of patients [3]. Also, about 10 % of patients with COVID-19 only experience GI symptoms, which may confuse the physicians and lead to delayed diagnosis [4], [5]. Impairments in the barrier function of the GI tract, GI inflammation, changes in the microbiota, thromboembolic events, and changes in the metabolism of serotonin are some of the suggested mechanisms leading to GI symptoms in patients with COVID-19 [6]. Also, some medications used for the treatment of COVID-19 can cause GI symptoms [7]. Diarrhea is the most common GI symptom in patients with COVID-19; however, nausea, vomiting, abdominal pain, anorexia, and GI bleeding are also reported in these patients [8].
AMI(acute mesenteric ischemia) is a rare life-menacing surgical emergency with a reported mortality of around 60 % to 80% [7]. AMI is a thromboembolic event reported in very few patients with COVID-19 with a range of clinical characteristics with presenting symptoms ranging from GI or respiratory symptoms to stroke [9]. Timely diagnosis is the cornerstone of successful management of AMI, as these patients require emergent surgical treatment. However, AMI may present in patients without the classic risk factors of AMI, and the symptoms might confuse physicians, leading to delayed diagnosis and increased mortality [9]. Therefore, it is worth studying the characteristics of these patients as it helps improve the physicians diagnosing AMI in the setting of COVID-19. Thus, in this manuscript, we report a patient with COVID-19 who presented with AMI as its initial presenting symptom. This case report was reported according to the SCARE statement guideline [10].
2. Presentation of case
A 68-year-old man presented to the emergency room with periumbilical non-radiating pain that had started three days before the admission and had become worse during this time. The severity of the pain was 10 out of 10. He also had nausea, vomiting, flatus, and no defecation or gas passing in the past three days. He had no history of any diseases and didn't use any medication. The patient lived with his family and reported no history of smoking, alcohol or drug abuse. He had received two doses of the Sinopharm COVID-19 vaccine six months before his admission.
At presentation, the blood pressure (BP) was 160/80 mmHg, temporal artery temperature was 36.5 °C, respiratory rate (RR) was 16 breaths per minute, and pulse rate was 70 beats per minute (BPM). In the physical exam, the patient had guarding of the abdomen, generalized tenderness, and rebound tenderness in the periumbilical and right lower quadrants (RLQ). There were no abnormal findings in heart and lung auscultation. Normal sinus rhythm was evident in the electrocardiogram (ECG). Key laboratory data included C-reactive protein (CRP) was 116 mg/L with leucocytosis (white blood cell was 11,000) and acidosis in arterial blood gas. Creatine phosphokinase (CPK) was 660 μg/L. Results of the other laboratory tests are presented in Table 1.
Table 1.
The laboratory findings of the patient.
| Result-unit in hospital day variables (blood tests) | Day1 | Day3 | Day6 | Day12 |
|---|---|---|---|---|
| Biochemistry | ||||
| Blood sugar mg/dl | 203 | 279 | 147 | 136 |
| Sodium (Na) mEq/L | 141 | 140 | 154 | 136 |
| Potassium (K) mEq/L | 3.5 | 3.7 | 4 | 4.1 |
| Blood urea nitrogen mg/dl (BUN) | 21.8 | 44.45 | 31.59 | 15.07 |
| Creatinine (Cr) mg/dl | 1.03 | 1.39 | 1.25 | 0.99 |
| Hematology | ||||
| White blood cell (WBC) μL/3′10× | 9.3 | 11 | 8.3 | 7.3 |
| Red blood cell (RBC) × 10′6/ μL | 5.47 | 5.03 | 4.26 | 4.33 |
| Hemoglobin (Hb) %g | 16.6 | 15.7 | 13.3 | 13.7 |
| Hematocrit (Hct) % | 49.2 | 45.2 | 39.1 | 38.8 |
| Platelets (Plt) μL/3′10× | 181 | 136 | 154 | 191 |
| Neutrophils % | 88.8 | 90.2 | 84.7 | 79.4 |
| Lymphocytes % | 4.8 | 2.9 | 5.7 | 14.1 |
| Monocyte % | 6.3 | |||
| Eosinophils % | 0 | |||
| Basophils % | 0.1 | |||
| C-reactive protein (CRP) | 166 | 154 | 71 | |
| LDH | 612 | 670 | ||
| PH | 7.44 | 7.39 | 7.44 | |
| PCO2 mmHg | 41.7 | 25.4 | 31.7 | |
| HCO3 mmol/L | 25.1 | 15 | 21.4 | |
| PO2 mmHg | 33.7 | 66.1 | 50.7 | |
| O2SAT % | 64.5 | 93.3 | 87.9 % | |
| PTT, patient time | 35 | 29.1 | 38 | |
| PT, patient time | 18 | 14.2 | 39.7 | |
| PT, control time | 11 | 11 | 11 | |
| INR | 1.6 | 1.26 | 3.5 | |
Important laboratory findings are bold.
On the first day of admission, a chest X-ray showed no lung involvement or air under the diaphragm (Fig. 1). Abdominal X-ray in the supine position presented a fixed intestinal loop and prominent dilatation of a small bowel loop in the left upper quadrant (LUQ) with multiple air-fluid levels. These findings were suggestive of obstruction of the small intestine (Fig. 2).
Fig. 1.

Chest X-ray of the patient.
Fig. 2.

Abdominal X-ray of the patient.
He was prepared for a diagnostic laparotomy on admission day because of peritonitis and acute abdominal pain. This included a non-per os (NPO) diet and bisacodyl enema, 1 g of intravenous ceftriaxone every12 hour, and 500 mg of intravenous metronidazole every 8 h for prophylaxis and resuscitation was done with normal saline and dextrose water 5 %. Meanwhile, his WBC had risen from 9300 on the first day to 17,000 on the second day, and his PH became 7.39 from 7.44 in the venous blood gas (VBG) test. For post-operation care, based on hospital policies to separate intensive care units (ICU) for COVID-19 patients from others, a polymerase chain reaction (PCR) for COVID-19 was performed for the patient. The next day a diagnostic laparotomy was performed by a general surgeon who is a University faculty member of Islamic Azad University of Najafabad. Feces and bloody fluid were seen in the peritoneum. 100 cm from the ligament of Treitz, sixty cm of the gangrenous jejunum was seen. Pulses of mesenteric arteries were detected during surgery, so the jejunal branch of superior mesenteric vein occlusion was suspected. A side-to-side resection-anastomosis of the small intestine was done. Surgery was done without any complications. Pathologic findings showed a transmural hemorrhagic infarction in the jejunum and congestion with hemorrhage in the mesentery, suggesting an occlusion in the mesenteric vein. Based on paraclinical, clinical, and diagnostic laparotomy findings, the patient was diagnosed with small bowel obstruction and gangrene due to acute mesenteric ischemia (AMI) Fig. 3, Fig. 4.
Fig. 3.
Mesenteric tissue with white arrows showing necrosis.
Fig. 4.

Hemorrhage in small intestine mucosal tissue.
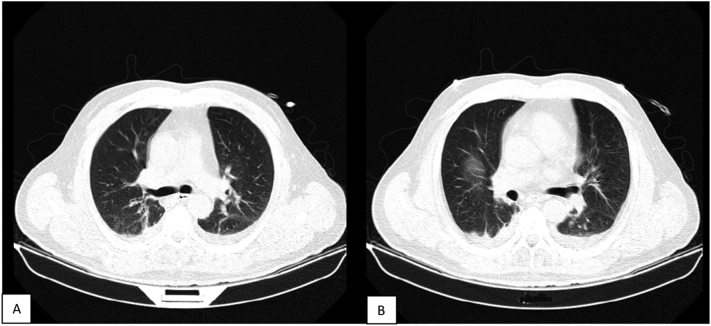
After the surgery, according to his positive PCR test, he was admitted to COVID-19 ICU for post-operation observation. Because of the COVID-19 infection, a computed tomography (CT) of the chest was performed to evaluate the lungs after the surgery. The chest CT scan demonstrates ground glass opacities with air bronchogram and slight pleural effusion in the lung's right and left lower lobes (Fig. 5).
Fig. 5.
A) Chest CT scan indicating the ground glass opacities. B) The patient's chest CT scan indicates ground-glass opacities and pleural effusion.
In the ICU, the therapeutic dose of Heparin and warfarin started to reach an INR above 2. He also received 200 mg of intravenous Remdesivir for five days. After five days, he started per os diet, and his WBC and VBG became normal. He was stable and discharged from the hospital ten days after surgery. He continued anticoagulant therapy with Warfarin for three months. In his follow-up for six months, he did not have complications, and Heparin was discontinued.
Although different conditions can lead to occlusive AMI as described, this patient did not have any history of thromboembolism, vascular events, underlying diseases, and risk factors that cause a hypercoagulable state, except for his positive COVID-19 PCR. The patient had no other vascular event in his six-month follow-up after discontinuing anticoagulant. We concluded that the patient's AMI was due to his infection with COVID-19 because of the hypercoagulable state that occurs in COVID-19 disease.
3. Discussion
The COVID-19 infection has a wide spectrum of presentations based on different risk factors and underlying diseases [11]. The main and most common symptoms are fever, cough, and dyspnea [12]. Gastrointestinal (GI) complications of COVID-19 are nausea, vomiting, abdominal pain, and diarrhea [13]. If Covid-19 disease becomes severe, the inflammatory immune response dysregulation can cause hyperinflammation, tissue damage, and cytokine storm. The cytokine storm and endothelial damage then disbalance the anticoagulation and pro-coagulation state. It tips the balance to a hypercoagulability state. This hypercoagulation causes thrombosis in arteries and veins in different sites of the body and leads to life-threatening complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), and AMI [14]. Another mechanism for AMI occurrence is an attachment of COVID-19 to enterocytes through angiotensin-converting-enzyme-2(ACE2) and triggering the superior mesenteric artery to form thrombosis. AMI presentations are mostly abdominal pain and vomiting [9]. It gets more important considering that the incidence of AMI in patients with COVID-19 who might not have the common risk factors for AMI may confuse the physicians, and lead to delayed diagnosis, and increase the mortality rates in patients.
A thorough search on this topic was performed in PubMed from 2020 to 2022, which yielded 32 results. After excluding irrelevant articles, seven articles are reviewed here. In an observational study by Talar Vartanoglu Aktokmakyan et al., five of the six patients with COVID-19-positive PCR underwent surgery due to mesenteric ischemia. Two had no comorbidities [15]. Suyog Patel et al. did a systematic review including 25,702 COVID-19 patients with gastrointestinal tract symptoms and abdominal pain. CT angiography of the abdomen and pelvis of them showed acute mesenteric. They said that management of AMI includes stabilization of the patient with fluid resuscitation and surgery. They recommend that the preparation of a guideline for COVID-19 patients with severe abdominal pain is needed to suspect AMI in them [13]. A study by P. FRANSVEA et al. included thirty-two COVID-19-positive patients with acute intestinal ischemia. They reported that none of the cases had been vaccinated. The most common comorbidities were hypertension, chronic kidney disease, cardiovascular disease, and diabetes [16]. While our patient did not have any comorbidities and so far had AMI. Bingwen Eugene Fan, in his letter to the editor, analysis some cases and express that COVID-19-associated thromboembolic event continue to cause significant mortality and morbidity. He reviews some previous COVID-19 cases that had thromboembolic events in the recovery phase of infectious. He mentions that they did not have essential risk factors. Because their COVID-19 PCR test was negative in this phase of the disease, they had to rule out other hyper-coagulopathic causes, unlike our case, which had active infection [17]. Two patient's management was described by Ghaith Al Mahruqi et al. They had acute mesenteric ischemia with typical symptoms, including acute respiratory distress syndrome confirmed in CT chest and peritonitis on abdominal physical exam. However, in this case, our patient did not have any clinical respiratory problems, while his CT showed ground-glass opacities suggestive of lung involvement [18]. A case report by Uthayakumar Amaravathi et al. expresses a 45-year-old man presented to the emergency department with severe abdominal pain. The clinical examination was unremarkable, but imaging revealed acute mesenteric ischemia caused by the superior mesenteric artery and superior mesenteric vein occlusion. They suggest that in patients with severe and acute abdominal pain, a chest CT can help physicians think about COVID-19 [19].We considered COVID-19 in our patient as the cause of AMI due to CT findings and positive PCR. Florin Savulescu et al. describe a case of a 60-year-old female patient who received Ad26.COV2-S vaccine for COVID-19 immunization, and after two weeks, she had vaccine-induced immune thrombotic thrombocytopenia (VITT) symptoms with AMI and thrombosis in the splenic-portal vein. While a vaccine can cause VITT, it is essential to consider the time interval between the vaccination and the occurrence of the symptoms [20]. In their case, a two-week interval is justified, but in our case, he had received his second dose of the Sinopharm vaccine six months before. In this period, the symptoms were not attributed to the vaccine. He was at the end of the immunization period, which the second dose of vaccine provides, and he was infected with COVID-19. Therefore, especially during the current COVID-19 pandemic, it should be noted that patients without typical risk factors of AMI may present to the emergency department, and the diagnosis should be considered in patients even without typical risk factors.
4. Conclusion
Even after general vaccination in community, we still have to consider COVID-19 infection and its complex complications. This case again showed the heterogeneous presentations of COVID-19, which has surprised physicians since 2019. While this case had no underlying disease and had received the second dose of the COVID-19 vaccine six months ago, he had peritonitis due to AMI, a complication of a hypercoagulopathic state in COVID-19. He could survive AMI because of the appropriate time of diagnostic laparotomy and resection of the necrotic bowel.
COVID-19 may present a variety of symptoms, including gastrointestinal symptoms. It can also cause life-threatening conditions, such as AMI, which needs emergent treatment. The physicians should take into account that these patients may not have the typical risk factors for AMI. AMI diagnosis should be considered in COVID-19 patients with acute abdominal pain, regardless of a complete COVID-19 vaccination and without the common risk factors as in this case.
Informed consent
We obtained informed consent from patient to report this paper.
Ethical approval
Not applicable, N/A.
Sources of funding
N/A.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Supervision, MB; Roles/Writing - original draft, AS, PM, SS; Writing - review & editing, all authors.
Declaration of competing interest
Authors have no conflict of interest to declare.
References
- 1.Wu F., Zhao S., Yu B., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu Y., Sun J., Dai Z., et al. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J. Clin. Virol. 2020;127(March) doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Redd W.D., Zhou J.C., Hathorn K.E., et al. Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020;159(2):765–767.e2. doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collaborative C . Global Guidance for Surgical Care During the COVID-19 Pandemic. 2020. pp. 1097–1103. (March) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao R., Qiu Y., He J., et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020;5(7):667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin B., Singh R., Ha S.E., Zogg H., Park P.J., Ro S. Pathophysiological mechanisms underlying gastrointestinal symptoms in patients with COVID-19. World J. Gastroenterol. 2021;27(19):2341–2352. doi: 10.3748/wjg.v27.i19.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perisetti A., Goyal H., Gajendran M., Boregowda U. Prevalence , Mechanisms , and Implications of Gastrointestinal Symptoms in COVID-19. Vol. 7. 2020. pp. 1–8. (October) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Editor D. Hematology . Transfusion and Cell Therapy Letter to the Editor COVID-19 and Acute Mesenteric Ischemia : A Review. 3(1) 2019. pp. 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serban D., Tribus L.C., Vancea G., et al. Acute mesenteric ischemia in COVID-19 patients. J. Clin. Med. 2021;11(1) doi: 10.3390/jcm11010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SG The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Chegini V., Hosseini R., Zarei N., et al. COVID-19 presenting as right flank pain in a postpartum woman : a case report. Ann. Med. Surg. 2021;69(July) doi: 10.1016/j.amsu.2021.102770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.da Rosa Mesquita R., Francelino Silva Junior L.C., Santos Santana F.M., et al. Clinical manifestations of COVID-19 in the general population: systematic review. Wien. Klin. Wochenschr. 2021;133(7–8):377–382. doi: 10.1007/s00508-020-01760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel S., Parikh C., Verma D., et al. Bowel ischemia in COVID-19: a systematic review. Int. J. Clin. Pract. 2021;75(12) doi: 10.1111/ijcp.14930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomerak S., Khan S., Almasri M., et al. Systemic inflammation in COVID-19 patients may induce various types of venous and arterial thrombosis: a systematic review. Scand. J. Immunol. 2021;94(5):1–18. doi: 10.1111/sji.13097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vartanoglu Aktokmakyan T., Tokocin M., Meric S., Celebi F. Is mesenteric ischemia in COVID-19 patients a Surprise? Surg. Innov. 2021;28(2):236–238. doi: 10.1177/1553350620962892. [DOI] [PubMed] [Google Scholar]
- 16.Fransvea P., Costa G., Pepe G., Greca A.La, Magalini S., Puccioni C., d’Agostino L., Altieri G., Borello A., Acute V.Cozza G.S. intestinal ischemia in patients with COVID-19: single-centre experience and literature review. Eur. Rev. Med. Pharmacol. Sci. 2022;26:1414–1429. doi: 10.26355/eurrev_202202_28135. [DOI] [PubMed] [Google Scholar]
- 17.Fan B.E. COVID-19-associated thromboembolic events causing acute mesenteric ischaemia. Acad. Radiol. 2020;27(12):1788–1789. doi: 10.1016/j.acra.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al Mahruqi G., Stephen E., Abdelhedy I., Al Wahaibi K. Our early experience with mesenteric ischemia in COVID-19 positive patients. Ann. Vasc. Surg. 2021;73:129–132. doi: 10.1016/j.avsg.2021.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amaravathi U., Balamurugan N., Muthu Pillai V., Ayyan S.M. Superior mesenteric arterial and venous thrombosis in COVID-19. J. Emerg. Med. 2021;60(5):e103–e107. doi: 10.1016/j.jemermed.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Savulescu F., Cirlan C., Iordache-Petrescu M.I., Iordache M., Petrescu A.B., Blajut C. Portal vein and mesenteric artery thrombosis following the administration of an Ad26.COV2-S vaccine-first case from Romania: a case report. Vaccines. 2022;10(11) doi: 10.3390/vaccines10111950. [DOI] [PMC free article] [PubMed] [Google Scholar]