Abstract
Aim
To review and analyse the evidence on the efficacy and safety of non‐pharmacological interventions for preterm infants to relieve endotracheal suctioning (ES) pain.
Design
A systematic review per the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines.
Methods
Six databases were searched with a retrieval strategy. Parallel and crossover randomized controlled trials reporting non‐pharmacological interventions for relieving ES pain in preterm infants were identified from inception to 1 September 2021. The protocol was published in PROSPERO (CRD42021276058).
Results
Ten studies were retrieved, including nine different non‐pharmacological interventions. Seven studies reported that non‐pharmacological interventions in relieving pain were more effective than conventional care during ES, and three trials reported its safety. Due to the heterogeneity of pain assessment tools, time of assessment and population, only Facilitated tucking had sufficient evidence that it is a safe and effective non‐pharmacological intervention.
Keywords: analgesia, endotracheal suctioning, non‐pharmacological interventions, pain, preterm infants
1. INTRODUCTION
Pain is an unpleasant emotional‐sensory feeling caused by actual or potential damage (Usta et al., 2021). It is reported that hospitalized preterm infants routinely suffer a median of 16 invasive procedures per day (Cruz et al., 2016), such as endotracheal suctioning (ES), which is a common and necessary invasive procedure to suck out lung secretions from the tracheobronchial of preterm infants (Taplak & Bayat, 2021). Acute pain caused by ES will negatively affect the effect of respiratory support, further leading to hypoxia, infection, unstable vital signs, etc. (Schults et al., 2021). In addition, repetitive pain exposure can cause a range of adverse effects on neurodevelopment, stress response systems, and pain sensitivity, which can last for life. (Cruz et al., 2016; Guo et al., 2020). Guidelines (Chen et al., 2020; Lim & Godambe, 2017) have emphasized the importance of assessing and managing neonatal procedural pain to reduce any potentially harmful consequences. Over the last few decades, physicians have recognized that infants can be more sensitive to pain and suffer from severe acute and long‐term adverse effects of it. While physician practices in newborn pain management have improved, they remain shortcomings, and there are significant differences between medical centres (Agakidou et al., 2021). Currently, procedural pain in infants can be managed by non‐pharmacological and pharmacological interventions. While pharmacologic treatments have confirmed their effectiveness in relieving pain, their applicability in prematurity is limited and can lead to adverse consequences, such as physiological dependence, liver and kidney toxicity, respiratory depression, and seizures (Perry et al., 2018). In contrast, non‐pharmacologic interventions have given promising results in various routine procedures, but their role in relieving the pain of ES in preterm infants is still under scrutiny.
2. BACKGROUND
Suctioning for preterm infants is a painful procedure and causes changes in vital signs and other parameters (Sinha et al., 2021). Non‐pharmacological pain relief methods such as non‐nutritive sucking, kangaroo care (KC), facilitated tucking (FT), and expressed breast milk (EBM) are short‐impacted, well‐tolerated and can be performed independently by nursing (Fatollahzade et al., 2020). However, current studies on non‐pharmacological pain relief reported inconsistent results. In addition, considering the unclear risks of glucose and sucrose (Gao et al., 2016), it is also crucial to assess the safety of non‐pharmacological interventions for ES pain in preterm infants. Numerous existing reviews have discussed non‐pharmacologic management for the pain of venipuncture (McNair et al., 2019), heel lance (Salvioli et al., 2017) and retinopathy of prematurity (Pirelli et al., 2019), there are currently no published reviews investigating non‐pharmacologic pain management for ES in preterm infants. It is important to summarize existing methods for pain relief to provide reliable answers about their effectiveness and to enhance their use in the care of premature infants. Therefore, the aims of this review are: (1) to examine the use of non‐pharmacologic interventions during ES, (2) to explore the efficacy of non‐pharmacological interventions for ES compared to usual care and (3) to assess the safety of non‐pharmacological interventions for ES.
3. THE STUDY
3.1. Design
This systematic review was per the Preferred Reporting Items for Systematic reviews and Meta‐Analyses guidelines (Page et al., 2021). The protocol had been registered with the International Prospective Register of Systematic Reviews (CRD42021276058).
3.2. Method
3.2.1. Search strategy and study selection
To identify more relevant studies, we developed the search strategies with the help of a librarian and searched the six open databases (Web of Science, PubMed, the Cochrane Library, Embase, PsycNET and CINAHL) from inception to 1 September 2021. Table 1 provided a complete list of search terms in PubMed. For a comprehensive literature search, the researchers also searched the references of key articles.
TABLE 1.
Pubmed search strategy
| #1 | “Infant, premature” [mesh] |
|---|---|
| #2 | “extremely premature” [Title/Abstract] OR “premature infant*” [Title/Abstract] OR “preterm infant*” [Title/Abstract] OR “premature birth” [Title/Abstract] OR “preterm birth” [Title/Abstract] |
| #3 | #1 OR #2 |
| #4 | “Suction” [Mesh] |
| #5 | ((Aspiration*, Mechanical [Title/Abstract]) OR (suction* [Title/Abstract])) OR (Mechanical Aspiration* [Title/Abstract]) |
| #6 | #4 OR #5 |
| #7 | “Pain” [Mesh] |
| #8 | “Analgesia” [Mesh] |
| #9 | (pain* [Title/Abstract]) OR (analgesia [Title/Abstract]) |
| #10 | #7 OR #8 OR #9 |
| #11 | #3 AND #6 AND #10 |
Import all retrieved articles into Endnote software to remove duplicate articles. On the Rayyan website, two independent reviewers according to the eligible criteria scrutinized the abstracts and titles. Full texts of relevant studies were then assessed, and eligible studies were finally included. Any disagreements were recorded and resolved in consultation with a third reviewer.
3.2.2. Inclusion and exclusion criteria
The inclusion criteria were as follows: (a) crossover or parallel randomized controlled trials; (b) infants born before 37 weeks gestation; (c) use non‐pharmacologic interventions to manage infant's pain during ES; (d) the effects of pain relief measured by composite pain scale based on physiological and behaviour, and/or safety of interventions or clinical outcomes assessed; (e) English publications. The exclusion criteria were as follows: (a) premature infants with congenital anomalies, intracranial haemorrhage, seizures or other major diseases (b) use of both pharmacological and non‐pharmacological interventions; (c) duplicate articles or papers from the same patient population; (d) review, case studies, conference reports, letters or qualitative research.
3.2.3. Quality assessment
Two reviewers evaluated the quality of included studies using the Cochrane revised tool (RoB 2.0), which was designed to assess the risk of bias in randomized trials (Higgins et al., 2021). This tool includes five categories (randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results), and each category can be judged as low risk of bias, some concerns, or high risk of bias. Any disagreements were resolved in consultation with a third reviewer.
3.2.4. Data extraction
From eligible studies, two reviewers independently extracted the information, including author, year of publication, country, type of study, sample size, characteristics of participants (gestational age and weight), characteristics of the intervention, measurement of indicators and outcomes. The disagreement was resolved through a discussion with another researcher.
4. RESULTS
4.1. Search results
A total of 282 records were retrieved and screened. After deleting duplicate files, 156 studies were identified, 130 of which were excluded after screening titles and abstracts. Since then, 26 full‐text articles were screened out, and 16 of them have been excluded for various reasons. Finally, only 10 studies were included in this review (Figure 1).
FIGURE 1.
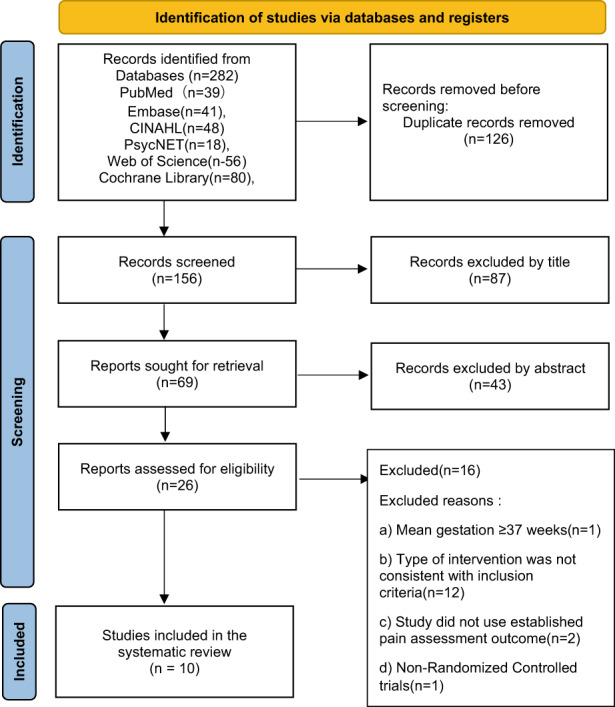
PRIMSA flow diagram
4.2. Characteristics of included studies
Table 2 summarized the characteristics of included studies. The 10 included studies were from Germany (n = 2), Finland (n = 2), Iran (n = 2), Australia (n = 1), India (n = 1), the United States (n = 1) and Turkey (n = 1). All studies were randomized trials with control groups or placebo groups, including intervention with a control group (n = 6), one control group with several intervention groups (n = 2), and all were intervention groups (n = 2). All the studies were published from 2004 to 2021. The sample size of the studies ranged from 20 to 108, the weight of participants was more than 560 grams, and the gestational age ranged from 23 and 37 weeks. In addition, the types of respiratory support were different, including non‐invasive ventilation (Axelin et al., 2009; Rodrigues et al., 2017; Vezyroglou et al., 2015), invasive mechanical ventilation (Alinejad‐Naeini et al., 2014; Fatollahzade et al., 2020; Taplak & Bayat, 2021; Ward‐Larson et al., 2004) and both of them (Axelin et al., 2006; Desai et al., 2017; Mitchell et al., 2013).
TABLE 2.
Characteristics of the included trials
| Author (year) | Country | Design | Intervention type | Participants, setting | Outcome and measurement | Conclusions |
|---|---|---|---|---|---|---|
| Ward‐Larson et al. (2004) | Germany |
Randomized crossover trial |
Facilitated tucking (FT) VS Usual care |
Population:40 VLBW infants with tracheal intubation GA: 23–32 (27.31 ± 2.43) weeks Weight: 560–1,498 (982.30 ± 284.05) g Setting: NICU |
PIPP, SNAP, NTISS |
FT is an effective non‐drug intervention to relieve the pain of tracheal sputum aspiration in very low body weight infants 30 s after the suctioning. |
| Axelin et al. (2006) | Finland |
Randomized crossover trial |
Facilitated tucking by parents (FTP) VS Usual care | Population: 20 preterm infants with one of their parents GA: 24–33 weeks (median 28 weeks) Weight: 690–1920 g (median 950 g) Setting: NICU | NIPS, Time to calm down, Parents' opinions of FTP, | FTP is an effective and safe management method to relieve the pain of sputum aspiration in premature infants during suctioning. |
| Axelin et al. (2009) | Finland |
Randomized placebo controlled crossover trial |
Facilitated tucking by parents (FTP) vs Oral glucose (OG) VS Opioid VS Placebo | Population:20 premature Infants and their parents GA:23–30 (28 ± 2.3) weeks weight: 485–1,570 (1,123 ± 327) g Setting: NICU | PIPP, NIPS, Short‐term adverse effects | OG and FTP are equally effective during heel stick and pharyngeal suctioning exceeding the effect of the opioid, which equaled placebo.FTP is preferable to other pain management methods when both efficacy and safety are considered during the procedure. |
| Mitchell et al. (2013) | USA |
Randomized controlled Crossover trial |
Kangaroo Care (KC) VS Usual care |
Population:38 preterm infants GA: 27–30 weeks weight: >1,000 g Setting: NICU |
PIPP, Salivary cortisol levels | The analgesic or sedative effects of KC were not sustainable or did not exceed the immediate skin‐to‐skin retention time. |
| Alinejad‐Naeini et al. (2014) | Iran |
Randomized controlled crossover trial |
Facilitated tucking (FT) or Usual care |
Population:34 premature infants GA: 29–37 weeks Weight: >1,200 g Setting: NICU |
PIPP | FT significantly reduced the mean PIPP score immediately after suctioning and could be used as a non‐pharmacological method for the pain of suctioning. |
| Vezyroglou et al. (2015) | Germany |
Randomized controlled crossover trial |
Oral glucose (G) or Placebo (P) |
Population: 32 preterm infants GP: GA: 33.6 ± 2.1 weeks Weight:1983 ± 428 g PG: GA:34.4 ± 1.6 weeks Weight:2184 ± 525 gSetting: NICU |
PIPP, Tolerability of the administered drugs |
Late preterm infants in the first days of life did not benefit significantly from analgesia with glucose during oro‐pharyngeal suctioning. Oral 20% glucose is relatively well tolerated during nasal CPAP. |
| Rodrigues et al. (2017) | Australia |
Randomized controlled trial |
Expressed Breast milk (EBM)VS 25% dextrose |
Population: 40 preterm infants Dextrose: GA:31.5 ± 1.82 weeks Weight:1415 ± 367.2 g BM: GA:31.65 ± 1.95 weeks Weight:1481 ± 404.36 g Setting: NICU |
PIPP | EBM and 25%dextrose both could significantly reduce pain during the procedure. The analgesic effect of EBM was sustained. |
| Desai et al. (2017) | India |
Randomized controlled trial |
Expressed Breast milk (EBM) VS Swaddling VS Oral Sucrose (OS) |
Population:108 Preterm neonates BM: GA:32.76 ± 3.96 weeks Weight:1358.52 ± 573.93 g Swadding: GA:33.17 ± 4.86 weeks Weight:1516.75 ± 750.17 g OS: GA:32.91 ± 3.45 weeks Weight:1430.50 ± 648.89 g Setting: NICU |
PIPP | None of the EBM, OS, and Swaddling interventions were significantly effective in relieving the pain during suctioning procedure in preterm neonates on assisted ventilation. |
| Fatollahzade et al. (2020) | Iran |
Randomized controlled crossover trial |
Gentle human touch (GHT) VS Usual care |
Population: 34 Preterm neonates GA:27–34 weeks Weight:>1,200 g Setting: NICU |
PIPP | GHT could reduce the pain immediately after suctioning in premature infants. |
| Taplak and Bayat (2021) | Turkey |
Randomized controlled trial |
Breast milk smell (BMS) VS White noise (WN) VS Facilitated tucking (FT) VS Usual care |
Population: 80 Preterm infants GA: >26 weeks Weight:>1,000 g Setting: NICU |
PIPP‐R, Heart rate, Oxygen saturation |
The PIPP‐R mean scores of the white noise and facilitated tucking groups, which were statistically lower than those of the breast milk smell and control groups, there were significant differences between the groups at 1 min before suctioning procedure. WN and FT could relieve the pain during suctioning procedure in premature infants, but there is no statistical significance. FT could significantly relieve the pain 3 min after suctioning procedure compare with usual care. |
Abbreviations: CPAP: continuous positive airway pressure; GA: Gestational age; NICU: Neonatal Intensive Care Unit; NIPS: Neonatal Infant Pain Scale; NTISS: Neonatal Therapeutic Intervention Scoring System; PIPP: Premature Infant Pain Profile; SNAP: Score for Neonatal Acute Physiology; VLBW: very low birth weight.
Table 3 summarizes the characteristics of the interventions in each study. A total of nine non‐pharmacological interventions were reported: gentle human touch (GHT) (Fatollahzade et al., 2020), FT (Alinejad‐Naeini et al., 2014; Axelin et al., 2006, 2009; Taplak & Bayat, 2021; Ward‐Larson et al., 2004), swaddling (Desai et al., 2017), oral sucrose (Desai et al., 2017), oral glucose (OG) (Axelin et al., 2009; Rodrigues et al., 2017; Vezyroglou et al., 2015), EBM (Desai et al., 2017; Rodrigues et al., 2017), KC (Mitchell et al., 2013), breast milk smell (BMS) (Taplak & Bayat, 2021) and white noise (WN) (Taplak & Bayat, 2021). The timing of the assessment varied from 5 min before the pain procedure to 5 min after the procedure. The outcome indicators included individual vital signs, behavioural response, pain scores, salivary cortisol levels, clinical outcomes, the tolerability of the administered drugs, and parents' perspective.
TABLE 3.
Characteristics of the interventions
| Author (year) | Intervention description | Duration | Observation time | Respiration support |
|---|---|---|---|---|
| Ward‐Larson et al. (2004) | Facilitated tucking (FT): the caregiver ‘hand‐swaddling’ the infant by placing a hand on the infant's head and feet while providing flexion and containment, | FT: during the procedure and 30‐s observation period immediately following the procedure |
T0: 15 s before the procedure T1: 30 s immediately after the procedure |
Invasive ventilation |
| Axelin et al. (2006) | Facilitated tucking by parents (FTP): parent holds by her hands the infant in a side‐lying flexed position offering support and skin contact | FTP: during the procedure, and continued until the infant had calmed down | T0: 1 min before the procedure T1: during the procedure T2: 1 min after the procedure | Non‐invasive ventilation (85% CPAP, 5% extubated), Invasive ventilation (10%) |
| Axelin et al. (2009) |
Facilitated tucking by parents (FTP): parent holds by her hands the infant in a side‐lying flexed position offering support and skin contact Oral glucose (OG): 0.2 ml of 24% glucose Opioid: 0.05 mg/kg of oxycodone Placebo: 0.2 ml of sterile water |
FTP: before the procedure, and continued until the infant had calmed down OG: 2 min before the procedure Opioid: heel lance was conducted 15 min after and endotracheal suctioning 25 min after administration |
T: during the procedure (first 30 s after skin puncture and after the suctioning catheter was set in the infant's mouth) |
Non‐invasive ventilation(CPAP) |
| Mitchell et al. (2013) | Kangaroo Care (KC): kin‐to‐skin on the mother's or father's chest | KC: for a minimum of 2 h daily from day of life five through nine | T: during the procedure | Invasive ventilation, CPAP, nasal cannula flow |
| Alinejad‐Naeini et al. (2014) | Facilitated Tucking: placing the neonate in facilitated tucking position | FT: during the procedure | T: immediately after the procedure | Invasive ventilation |
| Vezyroglou et al. (2015) | Oral glucose (OG): 0.3 ml/kg of 20% glucose | OG:3 min before the procedure | T: during the procedure | Non‐invasive ventilation (CPAP) |
| Rodrigues et al. (2017) | Express Breast milk (EBM): 0.3 ml/kg Dextrose: 0.3 ml/kg of 25% dextrose |
EBM:3 min before procedure Dextrose:3 min before procedure |
T0: before the procedure T1: during the procedure T2: 1 min after the procedure T3: 5 min after the procedure | Non‐invasive ventilation (CPAP) |
| Desai et al. (2017) | Express breast milk (EBM): 2 cc Swaddling: swaddled for 10–15 min Oral Sucrose:2 cc sucrose | EBM: 2 min before procedure Swaddling: 10–15 min before procedure Sucrose: 2 min before procedure | T: during the procedure |
Invasive ventilation (60%) Non‐invasive ventilation (40%) |
| Fatollahzade et al. (2020) | Gentle human touch (GHT): one hand is placed on the neonate's head and the other on the neonate's abdomen | GHT: during the procedure | T: during the procedure | Invasive ventilation |
| Taplak and Bayat (2021) | Breast milk smell (BMS):1 ml of breast milk was dropped on a pet/filter paper and placed 10 cm away from the infant's nose White noise (WN): composed of the mother's womb environment and real heartbeat sounds and relaxing music Facilitated tucking (FT): held in the facilitated tucking position by a nurse working in the service | BMS: 5 min before to 5 min after the suctioning procedure WN: 5 min before to 5 min after the suctioning procedure FT: 5 min before to 5 min after the suctioning procedure |
T0: 5 min before the procedure T1: 3 min before the procedure T2: 1 min before the procedure T3: during the procedure T4: 1 min after the procedure T5: 3 min after the procedure T6: 5 min after the procedure |
Invasive ventilation |
Abbreviation: CPAP: continuous positive airway pressure.
4.3. Quality assessment and bias of the studies
Figure 2 reported the risk of bias. Five studies (Axelin et al., 2009; Mitchell et al., 2013; Rodrigues et al., 2017; Taplak & Bayat, 2021; Vezyroglou et al., 2015) had a low risk of bias, and four studies were judged to raise some concerns (Alinejad‐Naeini et al., 2014; Axelin et al., 2006; Desai et al., 2017; Fatollahzade et al., 2020), and one study (Ward‐Larson et al., 2004) was assessed to have some concerns in two domains (randomization process and measurement of the outcome). However, given that participants included were premature infants and the intervention process was strictly required, we still believed in the reliability of the result.
FIGURE 2.
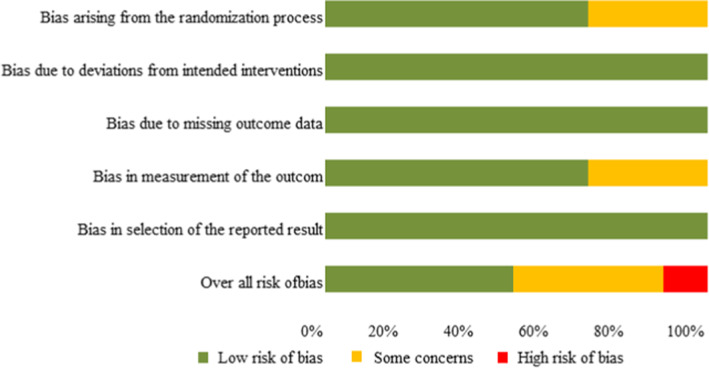
Risk of bias assessment for the RCTs
4.4. Outcome analysis
Focusing on the purpose of this research, we report the results from the following three aspects.
4.4.1. Comparison of the effectiveness between different non‐pharmacological interventions and usual cares
Eight studies compared the effectiveness of non‐pharmacological interventions and usual care to relieve the pain of ES in preterm infants. Touching therapy has been shown to relieve pain in some ways. Seven studies reported three interventions related to touch: FT, GHT and KC. Five studies using FT all reported it was an effective non‐pharmacological intervention to relieve the pain of ES during or after the procedure in premature infants. Four of the studies (Alinejad‐Naeini et al., 2014; Axelin et al., 2006, 2009; Ward‐Larson et al., 2004) showed that FT significantly reduces the score of pain during or immediately after suctioning (p < .05). Axelin et al 's study (Axelin et al., 2006) found that FT significantly reduced NIPS scores during suctioning (p < .001), but the statistically significant difference disappeared 1 min after the suction procedure (p = .084). However, FT could significantly reduce PIPP‐R mean score 1 min before and 3 min after suctioning procedure compare with usual care (p < .05) (Taplak & Bayat, 2021). GHT (Fatollahzade et al., 2020) also can reduce the PIPP score immediately after suctioning in premature infants in an RCT study (p < .002). However, Mitchell. et al. found the KC was not effective after suctioning, and the baseline salivary cortisol levels were also not statistically significant between the groups (p = .49) (Mitchell et al., 2013).
Oral sweet solutions and breast milk have been shown to relieve pain in a single tissue injury procedure. One study (Rodrigues et al., 2017) reported the effects of EBM and dextrose in relieving pain and found that EBM (11.35 ± 3.05 vs 13.45 ± 3.27, p = .04) and 25% dextrose (11.25 ± 2.73 vs 13.20 ± 2.55, p = .02) both can significantly relieve pain during the procedure. In addition, the analgesic effect of EBM remained statistically significant compared to the control group 1 min (p = .02) and 5 min (p = .01) after the procedure. Three studies reported the effects of OG and presented different results. In Axelin et al.'s study, PIPP scores of OG (mean: 11.05 ± 2.31, p = .014) were significantly lower than placebo (mean: 12.4 ± 2.06) during pharyngeal suctioning (Axelin et al., 2009). However, glucose (8.0, KI: 7.1–8.9, p > .05) did not significantly relieve pain in the first few days after birth in late preterm infants compared with placebo (8.6, KI: 7.8–9.4) during oropharyngeal suctioning in the study of (Vezyroglou et al., 2015). In addition, a randomized controlled study comparing the effects between BMS, WN, FT and the usual care group showed no statistical difference in PIPP‐R scores between the groups during the procedure (p = .46) (Taplak & Bayat, 2021), but the PIPP‐R score of WN and FT was statistically lower than the control group 1 min before the procedure (p = .048) (Taplak & Bayat, 2021).
4.4.2. Comparison of the effectiveness of different non‐pharmacological interventions
Four studies assessed the effectiveness of different non‐pharmacological interventions for the pain of ES. One randomized crossover trial (Axelin et al., 2009) analysed the effectiveness of OG, FT, opioid and placebo. The evidence showed that compared with placebo, OG (11.05 ± 2.31, p = .014) and FT by parents (11.25 ± 2.47, p = .034) were both effective in relieving pain during the procedure, surpassing the effectiveness of opioid (11.85 ± 2.80, p = .339), which is not statistically better than placebo (12.40 ± 2.06). In another study comparing multiple interventions using FT (Taplak & Bayat, 2021), the FT group had the lowest mean PIPP‐R score compared to other WN and BMS; and revealed a significant difference in PIPP‐R mean scores 3 min after suctioning procedure (p = .047). In addition, FT and WN groups were more effective in relieving pain more than BMS in premature infants 1 min before the procedure (p = .048). One randomized controlled clinical trial (Desai et al., 2017) evaluated the analgesic effects of three different interventions during suctioning: swaddling, EBM and sucrose. The mean procedural PIPP score for sucrose (11.47 ± 3.23) was lower than the other two groups (EBM: 12.88 ± 3.59; Swaddling: 12.11 ± 3.87), but there was no statistical difference between the three groups (p = .24). Rodrigues. et al. also analysed the effectiveness of EBM for the preterm infant (Rodrigues et al., 2017). The results showed that there was no statistical difference between EBM and glucose during and 1 min and 5 min after the suctioning (p > .05), but the effectiveness of EBM was more durable.
4.4.3. Safety of non‐pharmacological interventions
Three studies examined the safety of non‐pharmacological interventions to relieve the pain of ES in preterm infants. Two of the three trials evaluated the adverse effects of OG compared with placebo. Vezyroglou et al. (2015) found placebo group (58.7%) had a higher incidence of adverse events than OG, but this difference was not statistically significant. In this study, which defined coughing, choking, apnoea, and a 20% deviation from baseline data in breathing, HR and SPO2 as short‐term adverse reactions. However, in another randomized controlled crossover study (Axelin et al., 2009), OG (21.25%) compared with placebo (12.5%) showed more short‐term adverse effects (SatO2 < 85, HR <100). This study also found FT (5%) by the parent group had a lower incidence of short‐term adverse reactions compared with other groups (Axelin et al., 2009). Axelin. et al. assessed the possible impact of parental touch and also concluded that FT by parents not only did not cause pain to premature infants but also can make infants calm down more quickly compared to the control care (5 s vs. 17 s, p = .024) (Axelin et al., 2006).
5. DISCUSSION
This review was conducted to identify non‐pharmacologic interventions to relieve pain during ES in preterm infants and determine their effectiveness and safety. This review revealed that non‐pharmacological interventions in the process of endotracheal suction may be more effective in relieving pain than usual care. Strong evidence that FT is preferable regardless of whether its operator is a nurse or a parent, but some non‐pharmacological interventions were inconsistent in relieving pain in premature infants. Regarding safety still a lack of research, but FT is reliable, the safety of OG is controversial in relieving pain during ES in premature infants.
The review includes the investigation of different types of non‐pharmacological interventions in the process of ES in premature infants. In the current review, compared to usual care, several non‐pharmacological interventions (FT, GHT, Oral sucrose and WN) were exceeded in reducing procedure pain. Although some non‐pharmacological interventions used to relieve pain during ES did not achieve statistical differences compared with usual care such as Swaddling, KC and EBM, their pain scores show a decreasing trend, which has certain implications for future research and clinical practice.
This systematic review also explored the differences in the effectiveness of different non‐pharmacological interventions. There is strong evidence that FT is significantly better than usual care and other non‐pharmacological interventions during and after the ES procedure. Five studies included had evaluated that in different weights, different gestational ages and different populations, the promotion of abdominal folding is significantly better than in others. This finding is consistent with the claim in the literature that FT can reduce pain in infants (Gomes Neto et al., 2020; Hartley et al., 2015). This result can be interpreted with gate control theory in pain control associated with touch. According to this theory, touch causes an endogenous dispersion of endorphins, which helps regulate pain impulses at the spinal cord level and has the effect of relieving the pain (Mathew & Mathew, 2003). In addition, the convenient folding not only supports the baby's position but also imitates the position of the foetus in the womb, providing familiar comfort, promoting physical stability, and reducing pain scores. Not to be ignored, the presence and touch of a caregiver can also relieve pain (Lopez et al., 2015). The effectiveness of GHT and KC in relieving pain can also be explained. As one of the fastest evolving senses in newborns, touch has always been considered to reduce stress and relieve pain. Touching can enhance the activity of the vagus nerve, increase the level of β‐endorphin in the body, and reduce the level of cortisol and adrenaline, thereby reducing pain (Qiu et al., 2017). For KC, the reason why the outcome does not reach statistical significance may be due to the small sample size and the optimal duration (Johnston et al., 2017). In this study, the suction procedure was not performed simultaneously with the intervention. Besides, WN can also effectively relieve pain or relax ventilated preterm infants before the procedure (Taplak & Bayat, 2021), which is similar to the sound familiar to premature babies during the foetal period. WN as a musical therapy had been reported that can lead to slower heart rate, calmer and more regular respiratory rate, and lower blood pressure (Yaman Aktaş & Karabulut, 2016).
In addition, studies on the effects of OG and EBM on pain relief have shown different results. Glucose is one of the most widely studied sweetening solutions, and systematic reviews and meta‐analyses have proved its effectiveness for analgesia during minor surgical pain in neonates (Harrison et al., 2017). However, it is not clear the analgesic effectiveness of glucose on ES. These inconsistent conclusions in our study may be related to the heterogeneity of the included samples, for example, glucose dose, gestational age and type of respiratory support. The two groups of preterm infants received different doses of glucose in different concentrations (0.2 ml of 24% glucose vs. 0.3 ml/kg of 20% glucose) (Axelin et al., 2009; Vezyroglou et al., 2015). Studies have shown that the gestational age is positively associated with oxygen saturation and negatively associated with HR, affecting pain score and thus affecting results (Guo et al., 2020). The subgroup analysis results study by Desai et al. showed that these non‐pharmacological interventions cannot relieve the pain of ES in children using mechanical ventilation, but may be effective in relieving pain in non‐invasive ventilation (Desai et al., 2017). Similarly, respiratory support differed between the two trials (Desai et al., 2017; Rodrigues et al., 2017) using EBM, which may have resulted in different outcomes. Consistent with our findings, previous systematic reviews have suggested that Swaddling (Nelson, 2017) and EBM (Benoit et al., 2017) alone should not be considered an adequate intervention. Future research can use a more scientific and effective combination of non‐pharmaceutical interventions to relieve recurrent procedural pain in preterm infants (Guo et al., 2020). Overall, these findings confirmed the conclusions of previous reviews that non‐pharmacological interventions may provide an evidence base for preventing and managing procedural pain in infants (Perry et al., 2018; Pillai Riddell et al., 2015). These results indicate that non‐pharmacological interventions are promising and effective in relieving ES pain in preterm infants.
This systematic review also summarized each intervention's adverse reactions and clinical outcomes to determine the safety of non‐pharmacological pain interventions. Three trials examined the safety of non‐pharmacological interventions for the pain of ES in preterm infants. FT is preferable, and the safety of glucose interventions is controversial. Similar findings were found in Gomes Neto et al.'s study that FT is quite safe and beneficial for infants of all gestational ages (Gomes Neto et al., 2020). For glucose, the analgesic effects have been demonstrated in several studies (Kassab et al., 2012), but the short‐term and long‐term effects on nerves and development are inconsistent. Moreover, previous studies have mostly described a single mild procedural pain such as a heel puncture. There are few studies on the adverse effects of repeated moderate to severe pain such as ES. Axelin et al.'s study (Axelin et al., 2009) found that compared with opioids (5%) or FT by parents (5%), the short‐term adverse reactions of OG (21.25%) are significantly increased. In another included study (Vezyroglou et al., 2015), OG delivery via nasal CPAP did not cause statistically significant serious adverse reactions, but the study found that the incidence of adverse events in the glucose group was lower than that in the placebo group. In addition, this study also found that the higher the gestational age, the lower the possibility of adverse reactions, which can partly explain the inconsistent results between the two groups. The oropharyngeal function of the premature infant is not fully developed, which makes them more likely to have adverse reactions such as suffocation. Premature babies are at greater risk of swallowing dysfunction due to poor oropharyngeal function (Prabhakar et al., 2019), and are more likely to have adverse reactions such as suffocation. There is a need for replication studies that use similar, clearly defined outcomes in the future.
5.1. Strengths and limitations
To our knowledge, this is the first systematic review of non‐pharmacological interventions for pain during ES in preterm infants and assessing the efficacy and safety. There were several limitations in this review. First, non‐pharmacological interventions used different scoring tools, and different assessment time was used to measure results. These characteristics may have a high degree of heterogeneity affecting the results. Second, due to the small number of included studies and sample sizes for each intervention method, it is impossible to synthesize and compare the effects of each. Third, we only reviewed the research published in English, which limited the generalization of the research results.
6. CONCLUSIONS
This systematic review identified a range of non‐pharmacological interventions used for relieving pain during ES in preterm infants and assess their effectiveness and safety. The key finding demonstrated that non‐pharmacological interventions produced statistically significant pain relief during ES in preterm infants. FT is an effective and safe management method to relieve pain compared to other non‐pharmacological interventions, which nurses can use to manage pain during ES in preterm infants. Due to the diversity of the interventions and the small number of trials per intervention included in this systematic review, the obtained evidence is helpful but cannot be considered robust.
AUTHOR CONTRIBUTIONS
QC, WL, YZ: Made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; QC, WL, YXL: Involved in drafting the manuscript or revising it critically for important intellectual content; QC, WL, YZ, YY, HS, KZ, YXL: Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; QC, WL, YZ, YY, HS, KZ, YXL: Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST
The authors have no conflict of interest to disclose.
ETHICS STATEMENTS
This review did not require ethical approval.
ACKNOWLEDGEMENTS
I am very grateful to my professor, Yuexia Liao, for her guidance and advice during my writing process, which has benefited me a lot. In addition, I am very grateful to my partners (Wen Luo and You Zhou) for their support and criticism, which was instrumental and important in making this paper a reality.
Cai, Q. , Luo, W. , Zhou, Y. , Yin, Y. , Zhu, K. , Shi, H. , & Liao, Y. (2023). Efficacy and safety of non‐pharmacological interventions for endotracheal suctioning pain in preterm infants: A systematic review. Nursing Open, 10, 424–434. 10.1002/nop2.1364
Qian Cai and Wen Luo contributed equally to this article.
REFERENCES
- Agakidou, E. , Tsoni, K. , Stathopoulou, T. , Thomaidou, A. , Farini, M. , Kontou, A. , & Sarafidis, K. (2021). Changes in physicians' perceptions and practices on neonatal pain management over the past 20 years. A survey conducted at two time‐points. Frontiers in Pediatrics, 9, 667806. 10.3389/fped.2021.667806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alinejad‐Naeini, M. , Mohagheghi, P. , Peyrovi, H. , & Mehran, A. (2014). The effect of facilitated tucking during endotracheal suctioning on procedural pain in preterm neonates: A randomized controlled crossover study. Global Journal of Health Science, 6(4), 278–284. 10.5539/gjhs.v6n4p278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelin, A. , Salantera, S. , Kirjavainen, J. , & Lehtonen, L. (2009). Oral glucose and parental holding are preferable to opioid in pain management in preterm infants. The Clinical Journal of Pain, 25(2), 138–145. 10.1097/AJP.0b013e318181ad81 [DOI] [PubMed] [Google Scholar]
- Axelin, A. , Salantera, S. , & Lehtonen, L. (2006). 'Facilitated tucking by parents' in pain management of preterm infants‐a randomized crossover trial. Early Human Development, 82(4), 241–247. 10.1016/j.earlhumdev.2005.09.012 [DOI] [PubMed] [Google Scholar]
- Benoit, B. , Martin‐Misener, R. , Latimer, M. , & Campbell‐Yeo, M. (2017). Breast‐feeding analgesia in infants: An update on the current state of evidence. The Journal of Perinatal and Neonatal Nursing, 31(2), 145–159. 10.1097/jpn.0000000000000253 [DOI] [PubMed] [Google Scholar]
- Chen, R. , Yang, Y. , Shi, Y. , & Feng, Z. (2020). Expert consensus on neonatal pain assessment and analgesia management (2020 edition). Zhongguo Dang Dai Er Ke Za Zhi = Chinese Journal of Contemporary Pediatrics, 22(9), 923–930. 10.7499/j.issn.1008-8830.2006181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz, M. D. , Fernandes, A. M. , & Oliveira, C. R. (2016). Epidemiology of painful procedures performed in neonates: A systematic review of observational studies. European Journal of Pain, 20(4), 489–498. 10.1002/ejp.757 [DOI] [PubMed] [Google Scholar]
- Desai, S. , Nanavati, R. N. , Nathani, R. , & Kabra, N. (2017). Effect of expressed breast milk versus swaddling versus oral sucrose administration on pain associated with suctioning in preterm neonates on assisted ventilation: A randomized controlled trial. Indian Journal of Palliative Care, 23(4), 372–378. 10.4103/IJPC.IJPC_84_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatollahzade, M. , Parvizi, S. , Kashaki, M. , Haghani, H. , & Alinejad‐Naeini, M. (2020). The effect of gentle human touch during endotracheal suctioning on procedural pain response in preterm infant admitted to neonatal intensive care units: A randomized controlled crossover study. The Journal of Maternal‐Fetal and Neonatal Medicine, 35, 1370–1376. 10.1080/14767058.2020.1755649 [DOI] [PubMed] [Google Scholar]
- Gao, H. , Gao, H. , Xu, G. , Li, M. , Du, S. , Li, F. , & Wang, D. (2016). Efficacy and safety of repeated oral sucrose for repeated procedural pain in neonates: A systematic review. International Journal of Nursing Studies, 62, 118–125. 10.1016/j.ijnurstu.2016.07.015 [DOI] [PubMed] [Google Scholar]
- Gomes Neto, M. , da Silva Lopes, I. A. , Araujo, A. , Oliveira, L. S. , & Saquetto, M. B. (2020). The effect of facilitated tucking position during painful procedure in pain management of preterm infants in neonatal intensive care unit: A systematic review and meta‐analysis. European Journal of Pediatrics, 179(5), 699–709. 10.1007/s00431-020-03640-5 [DOI] [PubMed] [Google Scholar]
- Guo, W. , Liu, X. , Zhou, X. , Wu, T. , & Sun, J. (2020). Efficacy and safety of combined nonpharmacological interventions for repeated procedural pain in preterm neonates: A systematic review of randomized controlled trials. International Journal of Nursing Studies, 102, 103471. 10.1016/j.ijnurstu.2019.103471 [DOI] [PubMed] [Google Scholar]
- Harrison, D. , Larocque, C. , Bueno, M. , Stokes, Y. , Turner, L. , Hutton, B. , & Stevens, B. (2017). Sweet solutions to reduce procedural pain in neonates: A meta‐analysis. Pediatrics, 139(1), e20160955. 10.1542/peds.2016-0955 [DOI] [PubMed] [Google Scholar]
- Hartley, K. A. , Miller, C. S. , & Gephart, S. M. (2015). Facilitated tucking to reduce pain in neonates: Evidence for best practice. Advances in Neonatal Care, 15(3), 201–208. 10.1097/anc.0000000000000193 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. , & Welch, V. A. (Eds.). (2021). Cochrane handbook for systematic reviews of interventions version 6.2. John Wiley & Sons. Retrieved from. www.training.cochrane.org/handbook [Google Scholar]
- Johnston, C. , Campbell‐Yeo, M. , Disher, T. , Benoit, B. , Fernandes, A. , Streiner, D. , & Zee, R. (2017). Skin‐to‐skin care for procedural pain in neonates. Cochrane Database of Systematic Reviews, 2(2), Cd008435. 10.1002/14651858.CD008435.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassab, M. I. , Roydhouse, J. K. , Fowler, C. , & Foureur, M. (2012). The effectiveness of glucose in reducing needle‐related procedural pain in infants. Journal of Pediatric Nursing, 27(1), 3–17. 10.1016/j.pedn.2010.10.008 [DOI] [PubMed] [Google Scholar]
- Lim, Y. , & Godambe, S. (2017). Prevention and management of procedural pain in the neonate: An update, American Academy of Pediatrics, 2016. Archives of Disease in Childhood. Education and Practice Edition, 102(5), 254–256. 10.1136/archdischild-2016-311066 [DOI] [PubMed] [Google Scholar]
- Lopez, O. , Subramanian, P. , Rahmat, N. , Theam, L. C. , Chinna, K. , & Rosli, R. (2015). The effect of facilitated tucking on procedural pain control among premature babies. Journal of Clinical Nursing, 24(1–2), 183–191. 10.1111/jocn.12657 [DOI] [PubMed] [Google Scholar]
- Mathew, P. J. , & Mathew, J. L. (2003). Evaluation and treatment of pain in infants. Postgraduate Medical Journal, 79(934), 438–443. 10.1136/pmj.79.934.438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNair, C. , Campbell‐Yeo, M. , Johnston, C. , & Taddio, A. (2019). Nonpharmacologic management of pain during common needle puncture procedures in infants: Current research evidence and practical considerations: An update. Clinics in Perinatology, 46(4), 709–730. 10.1016/j.clp.2019.08.006 [DOI] [PubMed] [Google Scholar]
- Mitchell, A. J. , Yates, C. C. , Williams, D. K. , Chang, J. Y. , & Hall, R. W. (2013). Does daily kangaroo care provide sustained pain and stress relief in preterm infants? Journal of Neonatal‐Perinatal Medicine, 6(1), 45–52. 10.3233/NPM-1364212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, A. M. (2017). Risks and benefits of swaddling healthy infants: An integrative review. MCN: American Journal of Maternal Child Nursing, 42(4), 216–225. 10.1097/nmc.0000000000000344 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ: British Medical Journal/British Medical Association, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry, M. , Tan, Z. , Chen, J. , Weidig, T. , Xu, W. , & Cong, X. S. (2018). Neonatal pain: Perceptions and current practice. Critical Care Nursing Clinics of North America, 30(4), 549–561. 10.1016/j.cnc.2018.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai Riddell, R. R. , Racine, N. M. , Gennis, H. G. , Turcotte, K. , Uman, L. S. , Horton, R. E. , … Lisi, D. M. (2015). Non‐pharmacological management of infant and young child procedural pain. Cochrane Database of Systematic Reviews, 2015(12), Cd006275. 10.1002/14651858.CD006275.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirelli, A. , Savant Levet, P. , Garetti, E. , Ancora, G. , Merazzi, D. , Bellieni, C. V. , & Lago, P. (2019). Literature review informs clinical guidelines for pain management during screening and laser photocoagulation for retinopathy of prematurity. Acta Paediatrica, 108(4), 593–599. 10.1111/apa.14523 [DOI] [PubMed] [Google Scholar]
- Prabhakar, V. , Hasenstab, K. A. , Osborn, E. , Wei, L. , & Jadcherla, S. R. (2019). Pharyngeal contractile and regulatory characteristics are distinct during nutritive oral stimulus in preterm‐born infants: Implications for clinical and research applications. Neurogastroenterology & Motility, 31(8), e13650. 10.1111/nmo.13650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, J. , Jiang, Y. F. , Li, F. , Tong, Q. H. , Rong, H. , & Cheng, R. (2017). Effect of combined music and touch intervention on pain response and β‐endorphin and cortisol concentrations in late preterm infants. BMC Pediatrics, 17(1), 38. 10.1186/s12887-016-0755-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues, L. , Nesargi, S. V. , Fernandes, M. , Shashidhar, A. , Rao, S. P. N. , & Bhat, S. (2017). Analgesic efficacy of Oral dextrose and breast Milk during nasopharyngeal suctioning of preterm infants on CPAP: A blinded randomized controlled trial. Journal of Tropical Pediatrics, 63(6), 483–488. 10.1093/tropej/fmx017 [DOI] [PubMed] [Google Scholar]
- Salvioli, S. , Guidi, M. , & Marcotulli, G. (2017). The effectiveness of conservative, non‐pharmacological treatment, of plantar heel pain: A systematic review with meta‐analysis. Foot (Edinburgh, Scotland), 33, 57–67. 10.1016/j.foot.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Schults, J. A. , Mitchell, M. L. , Cooke, M. , Long, D. A. , Ferguson, A. , & Morrow, B. (2021). Endotracheal suction interventions in mechanically ventilated children: An integrative review to inform evidence‐based practice. Australian Critical Care, 34(1), 92–102. 10.1016/j.aucc.2020.05.003 [DOI] [PubMed] [Google Scholar]
- Sinha, V. , Semien, G. , & Fitzgerald, B. M. (2021). Surgical airway suctioning. In StatPearls. StatPearls Publishing LLC. [PubMed] [Google Scholar]
- Taplak, A. S. , & Bayat, M. (2021). Comparison the effect of breast milk smell, white noise and facilitated tucking applied to Turkish preterm infants during endotracheal suctioning on pain and physiological parameters. Journal of Pediatric Nursing, 56, e19–e26. 10.1016/j.pedn.2020.07.001 [DOI] [PubMed] [Google Scholar]
- Usta, C. , Tanyeri‐Bayraktar, B. , & Bayraktar, S. (2021). Pain control with lavender oil in premature infants: A double‐blind randomized controlled study. Journal of Alternative and Complementary Medicine, 27(2), 136–141. 10.1089/acm.2020.0327 [DOI] [PubMed] [Google Scholar]
- Vezyroglou, K. , Mehler, K. , Kribs, A. , Becker, I. , Langhammer, K. , Roth, B. , & Hunseler, C. (2015). Oral glucose in preterm neonates during oropharyngeal suctioning: A randomized controlled cross‐over trial. European Journal of Pediatrics, 174(7), 867–874. 10.1007/s00431-014-2472-6 [DOI] [PubMed] [Google Scholar]
- Ward‐Larson, C. , Horn, R. A. , & Gosnell, F. (2004). The efficacy of facilitated tucking for relieving procedural pain of endotracheal suctioning in very low birth weight infants. MCN: American Journal of Maternal Child Nursing, 29(3), 151–156. 10.1097/00005721-200405000-00004 [DOI] [PubMed] [Google Scholar]
- Yaman Aktaş, Y. , & Karabulut, N. (2016). The effects of music therapy in endotracheal suctioning of mechanically ventilated patients. Nursing in Critical Care, 21(1), 44–52. 10.1111/nicc.12159 [DOI] [PubMed] [Google Scholar]


