Abstract
Among transgender women living with HIV (TGWLH) in India, little is understood about the mechanisms through which multiple intersecting stigmas impact HIV care engagement, or intervention strategies that might mitigate this impact. We conducted focus groups with TGWLH (N = 30) in three Indian cities and analysed data using theoretical frameworks related to HIV stigma, gender affirmation, and syndemics. Findings revealed that enacted and anticipated stigma due to transgender identity, HIV, or sex work status, and lack of gender affirmation (e.g., misgendering) in healthcare settings delayed ART initiation and promoted care disengagement. Having supportive physicians and counsellors within ART centres and peer outreach workers facilitated ART initiation, adherence, and retention. Findings also revealed that HIV stigma within TGW communities led to concealment of HIV status or syndemic conditions such as depression and alcohol use, thereby affecting care engagement. However, the TGW community itself was also described as a resilience resource, offering emotional, psychological and tangible support that decreased the impact of discrimination on care engagement. HIV care engagement efforts among Indian TGWLH could be strengthened by reducing intersecting stigmas in healthcare settings and within TGW communities, providing gender-affirming and culturally competent healthcare, addressing psychosocial syndemic conditions, and strengthening support within transgender communities.
Keywords: Intersectional stigma, syndemics, HIV care engagement, India, resilience, transgender women
Introduction
Globally, transgender women (TGW) experience a high burden of HIV (Poteat et al., 2016). In India, TGW have an estimated HIV prevalence of 3.1–7.5% (NACO, 2016, 2017a), with wide geographic variations (0.5–23%) (NACO, 2016). Since 2004, antiretroviral treatment (ART) has been available for free through India’s National AIDS Control Programme and in 2017, India introduced a “test and treat” policy to immediately link all persons newly diagnosed with HIV to ART (NACO, 2017b). Evidence suggests that TGW living with HIV (TGWLH) experience suboptimal HIV care continuum outcomes (Jalil et al., 2017; Kalichman et al., 2017; Pina et al., 2018; Reisner et al., 2016). To effectively implement “test and treat” with TGWLH, it is critical to understand the unique challenges faced by this population in their engagement with India’s ART programme.
The challenges faced by TGWLH in accessing HIV care may be understood through complementary theoretical frameworks: (1) the HIV stigma framework (Earnshaw et al., 2013; Reinius et al., 2018; Turan, Budhwani, et al., 2017), which illustrates how HIV-related stigma leads to poor HIV care-related outcomes; (2) syndemic theory (Operario & Nemoto, 2010; Singer & Clair, 2003), which posits that socio-structural forces, including multiple stigmas, lead to co-occurring synergistic epidemics or syndemics of psychosocial health problems affecting care engagement and (3) the gender affirmation framework (Sevelius et al., 2014, 2019), which posits that the lack of or need for gender affirmation influences healthcare-seeking behaviours, including HIV treatment. TGW in India experience rampant discrimination and violence from family, police, healthcare providers and society (Chakrapani et al., 2019; Shaw et al., 2012). Lack of educational and employment opportunities forces some TGW to engage in sex work for survival (Chakrapani et al., 2018; NACO, 2016). Thus, TGWLH face multiple intersecting stigmas based on their gender identity, HIV status, and sex work status, likely influencing care engagement. TGW in India have been shown to experience psychosocial syndemic conditions such as depression, problematic alcohol use and violence victimisation, which in turn increases their HIV risk (Chakrapani et al., 2017; Chakrapani et al., 2019). These syndemic conditions may similarly exist for TGWLH, affecting their engagement with HIV care (Kalichman et al., 2017; Poteat et al., 2016; Sandfort et al., 2019).
The limited data from India show that TGWLH experience barriers accessing ART in public healthcare settings, and face challenges in ART adherence and retention in care (Beattie et al., 2012; Chakrapani et al., 2011). Furthermore, TGW have been shown to have poor access to gender-affirming clinical services, with a lack of qualified healthcare providers (Singh et al., 2014; Srivastava et al., 2021). However, while multiple stigmas likely impact care engagement, limited information is available about how stigmas faced by TGWLH specifically influence HIV care engagement, and what role, if any, gender affirmation plays in HIV treatment engagement. While studies from other countries have shown that limited access to supportive gender-affirming healthcare undermines TGWLH’s engagement with HIV care (Kalichman et al., 2017; Reisner et al., 2017; Sevelius et al., 2014), such information is lacking in India.
We therefore conducted a qualitative study among TGWLH to explore potential pathways between multiple stigmas including discrimination experiences, gender affirmation, syndemic psychosocial health problems, and HIV care engagement.
Methods
Setting and participants
From September to November 2019, we conducted four focus group discussions (FGDs) among TGWLH (two FGDs in Delhi, one each in Mumbai and Hyderabad). Participants were recruited by peer outreach workers of HIV care and support centres, which offer treatment adherence/retention and support services and are managed by community-based organisations (CBOs). Many TGW in these cities have indigenous gender-diverse identities such as hijra and Shiv-Shakti, and often live together in deras/gharanas (clans) with hierarchical social structures – guru (master) and chelas (disciples) (Chakrapani et al., 2018). To capture diverse experiences, maximum variation sampling (e.g., diverse age groups, indigenous gender-diverse identities, engagement in sex work), a subtype of purposive sampling, was used (Patton, 2015).
Data collection
FGDs were conducted in local languages (Hindi, Marathi, and Telugu) by one or more of the authors, co-moderated by trained peer outreach workers. We developed an interview guide informed by three theoretical frameworks (HIV stigma framework (Earnshaw et al., 2013; Reinius et al., 2018; Turan, Budhwani, et al., 2017), syndemic theory (Operario & Nemoto, 2010; Singer & Clair, 2003), and gender affirmation framework (Sevelius et al., 2014, 2019)). It explored stigma and discrimination experiences related to HIV, gender identity, and sex work status; experience of psychosocial problems (e.g., depression, problematic alcohol use); and perceptions and experiences of how discrimination and psychosocial problems were connected, if at all, to HIV treatment initiation and retention. Each FGD ranged from 60 to 90 minutes. Participants received INR 200 (~2.5 USD) for their time. Interviews were audio-recorded and translated into English for data analysis. All participants provided written informed consent. Institutional Review Boards of India HIV/AIDS Alliance and Albert Einstein College of Medicine as well as India’s Health Ministry Screening Committee approved the study.
Data analysis
A codebook was developed based on the aforementioned theoretical frameworks (a priori codes), and from the ideas and constructs identified during data analysis (emergent codes such as legal gender change and its impact on ART access). We used coding and categorising techniques adapted from both framework analysis (Ritchie & Spencer, 1994) and grounded theory approaches (Charmaz, 2014; Corbin & Strauss, 2015). Additionally, we used contiguity-based connecting strategies: a deterministic approach to understand the cause and consequence(s) of an event or phenomenon by locating the relationships among them in the participants’ narratives or among categories (Maxwell, 2012). Illustrative quotes are provided within the main text and in Table 1. The quotes in Table 1 are numbered (e.g., Q1, Q2) in the order in which they appear in the main text.
Table 1.
Additional illustrative quotes highlighting discrimination experiences, gender non-affirmation, and resilience among transgender women living with HIV (TGWLH) in India.
| Domain | Illustrative quotes |
|---|---|
| Discrimination in healthcare settings |
|
| Discrimination within hijra/transgender communities |
|
| Fear of discrimination and non-adherence |
|
| Depression and delay in ART initiation |
|
| Discrimination contributing to depression and alcohol use |
|
| Unmet gender affirmation needs: Family and societal non-acceptance or acceptance |
|
| Resilience and peer support |
|
Results
Participant characteristics
Overall, 30 TGWLH participated in four FGDs. Most participants were either aged 25–30 years (n = 15; 50%) or 18–24 years (n = 11; 36%), 77% identified as hijras (the rest as “transgender woman”), and 37% (n = 11) engaged in sex work. Forty percent (n = 12) had completed higher secondary school or had a college degree.
Stigma and discrimination experiences, and their impact on HIV care engagement
Discrimination in healthcare settings
Participants reported several incidents of discrimination from co-patients (Q1), doctors (Q2), nurses and counsellors (Q3). For example, when waiting for an HIV test result, a nurse told a participant, “[You] will be definitely HIV positive … no need for HIV testing” – a comment highlighting the interconnection between HIV and transgender identity stigmas. Although some participants have had positive experiences with counsellors in ART centres, negative experiences were reported by many, which included a lack of knowledge about TGW and being asked irrelevant questions related to sexual life. For instance, a counsellor at the ART centre asked a participant: “What enjoyment do you get by being a receptive partner?”
Participants reported that very few doctors were both TGW-friendly and culturally and clinically competent (e.g., knowledge about potential interactions between ART and gender-affirming hormones). Most doctors at ART centres, were perceived to be discriminatory – but not necessarily overtly. For example, participants reported that some doctors tried to “keep a distance” (Q2), avoided touching or examining them, and had only brief interactions.
Discrimination within hijra/TGW communities and from birth families
TGWLH reported facing discrimination within their communities due to their HIV status. Participants reported that a person’s HIV status could spread as fast as a “wildfire” within hijra communities, their key support system. In the study cities, deras (place of residence/house of a group of hijras) or gharanas (clans) are generally organised based on the type of work; for example – sex work, doli-badhai (performing in ceremonies by singing, dancing and playing drums) and mangti (asking money for providing blessings). An HIV-positive hijra belonging to doli-badhai or mangti dera, could potentially be expelled to protect dera’s reputation of being “pure” or “divine”, under the assumption that she engages in sex work (Q4). Thus, many TGWLH reported not disclosing their HIV status to even their co-chelas (co-disciples). TGWLH engaging in sex work also reported that sometimes other TGW engaged in sex work would out their HIV status to potential male clients (as other TGW perceive they might contract HIV from clients of TGWLH) – affecting their livelihood. Consequently, these efforts to avoid HIV status disclosure may delay the initiation of and adherence to ART.
Given the high prevalence of both HIV-related enacted and anticipated stigmas, TGW often sought to avoid creating suspicions about their HIV status among peers by skipping medications when visiting peers’ homes or when travelling to other cities to attend trans-community events (Q5, Q6). For TGW diagnosed recently, coming to terms with their HIV diagnosis and dealing with associated depression delayed ART initiation (Q7). Participants also described consuming alcohol to cope with depression resulting from a lack of support from their birth families and societal discrimination (Q8). Thus, discrimination experiences contributed to psychosocial syndemic conditions (e.g., depression and alcohol use) and subsequently ART initiation and non-adherence.
Unmet gender affirmation needs and HIV care engagement
In ART centres, participants recounted incidents of misgendering by healthcare providers and insensitive comments about their gender by cisgender patients. Within the ART centres, names and gender are recorded on medical forms based on their legal identity card. Thus, some TGW were called by their birth-assigned male names (i.e., deadnaming), which hurt and embarrassed them. Participants also reported that some TGWLH who initially registered in the ART centres using birth-assigned names and who subsequently changed their legal name faced interruptions in obtaining medications due to bureaucracy or delay in changing their names in ART centres. Thus, the unmet need for social and legal gender affirmation (Q10) may likely contribute to care disruptions and disengagement.
TGWLH also reported that they usually do not inform physicians in ART centres that they were on feminising hormones (often prescribed by private medical practitioners), as they did not see relevance in sharing that information with ART physicians who were presumed to have inadequate knowledge about hormone therapy and its interactions with ART. It is possible that concerns about interactions between ART and hormones may impact ART adherence, but none of the participants reported such concerns as they might have received information about the lack of interactions from their peers or non-governmental agencies that link them to ART centres.
Gender affirmation outside healthcare settings from family members (Q11, Q12) and partners also appeared to be important to supporting adherence. For instance, a participant reported that after her husband (also living with HIV) left her for a cisgender woman, she became depressed as she believed that her ex-husband did not accept her as a real woman. Thus, the lack of gender affirmation by partners and family led to depression, potentially interrupting ART adherence.
The role of resilience and support in buffering the effects of stigma on HIV care outcomes
Participants’ experiences revealed the presence of resilience at the individual and TGW community levels. At the individual level, resilience was illustrated by several strategies used by TGWLH to adhere to ART: taking medications at night (after household members have gone to sleep), storing ART in unlabelled containers, and telling their guru and co-chelas that the ART were hormone pills. These strategies could also be seen as approaches to protect from HIV status disclosure.
Participants described the TGW community as a resource for resilience, despite also reporting discrimination faced by TGWLH within hijra communities. Participants reported that even if a trans-woman disclosed her HIV status to some of the trusted co-chelas, these co-disciples often do not out her HIV status to other chelas or guru. Some TGWLH were also able to form informal support groups within hijra communities and supported each other in varied ways: exchanging information about HIV care, accompanying other TGWLH to ART centres, supporting one another for adherence (e.g., using code words to remind taking ART when speaking on phone), and offering emotional and material support for HIV care (Q13). A participant from Delhi stated that some hijra gurus supported TGWLH, but most often in secret: “My guru is very supportive. She helps her chela in initiating ART. But she asked me not to disclose my HIV status.” Here, the guru apparently did not want the prestige or reputation of their dera to be affected, especially when dera members are not supposed to engage in sex work – another example of intersecting stigma due to both HIV and sex work status. This occurrence also exemplifies how provision of support can co-occur with stigmatisation.
Finally, participants reported receiving support from peer outreach workers (ORWs) employed in transgender-specific community centres (often supported by the Global Fund) or in HIV outreach interventions supported by India’s National AIDS Control Organisation. Peer ORWs helped TGWLH navigate ART centres and provided adherence counselling. For example, when an ART centre staff demanded an identity card to register a participant, an ORW helped her obtain an identity card expeditiously (Q14) and avoided delays in initiating ART.
Discussion
This qualitative study extends the limited literature on how multiple intersecting stigmas, gender affirmation needs, and syndemic conditions influence HIV care engagement among transgender women living with HIV globally and in India. Findings illustrate the processes by which enacted or anticipated stigma experiences related to gender identity, HIV, sex work, and unmet gender affirmation needs (e.g., misgendering, lack of transgender health competency) in healthcare settings pose challenges to HIV care engagement (Figure 1). Results also showed that discrimination experiences or lack of gender affirmation contributed to the production of inter-connected psychosocial syndemic conditions such as depression and alcohol use, which in turn potentially affects ART adherence and retention in care. Our findings also demonstrate the utility of a novel combination of theoretical frameworks (a modified Earnshaw’s HIV stigma framework, gender affirmation framework, and syndemic theory) in explaining HIV care disengagement among TGWLH in India (Figure 1).
Figure 1.
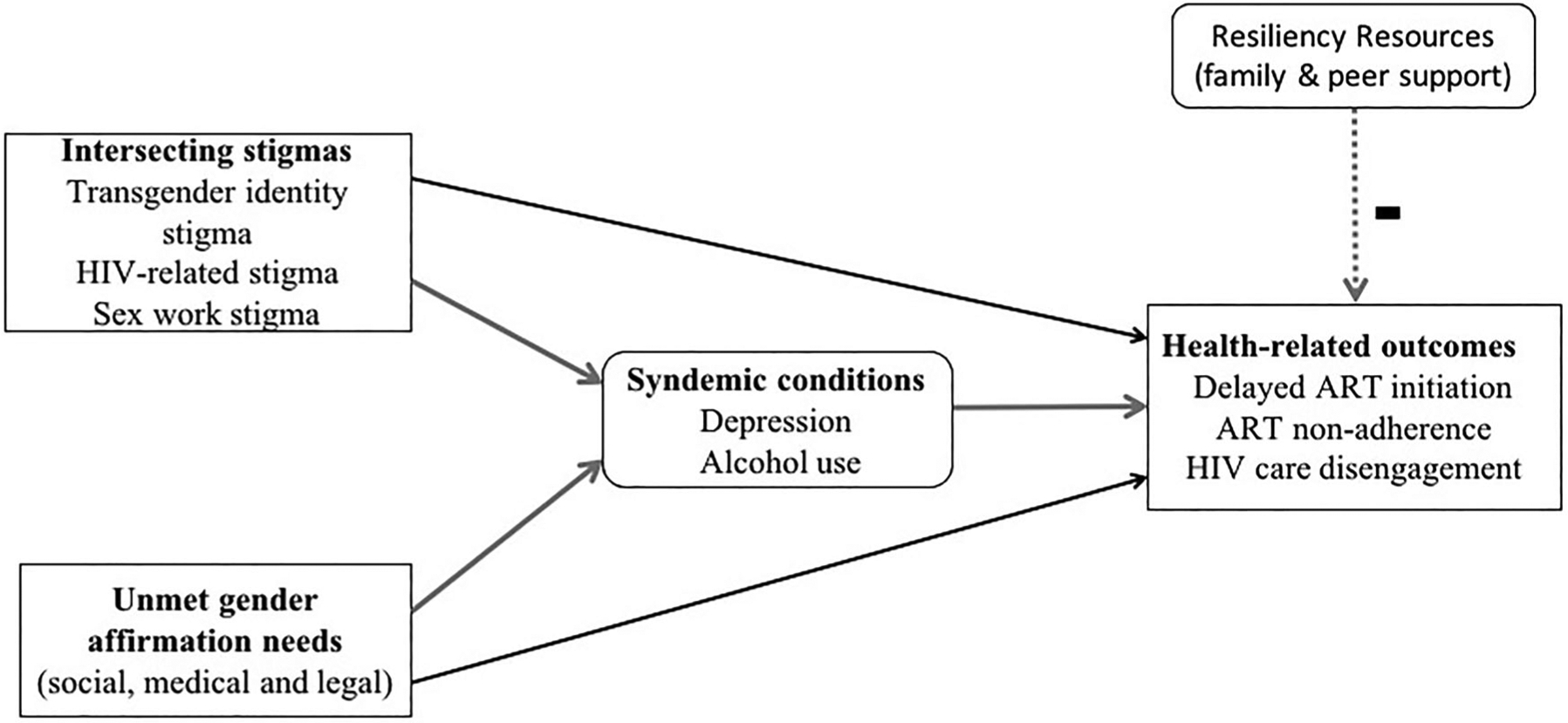
Pathways between multiple and intersecting stigmas, unmet gender affirmation needs, and HIV care engagement among transgender women living with HIV in India: A conceptual model. (Note. Resilience decreases the chances of negative health outcomes).
Intersectional stigma, syndemics production, and HIV care engagement
This study found the presence of multiple intersecting stigmas among TGWLH – transgender identity stigma, HIV-related stigma, and sex work stigma – similar to the intersectional stigma reported in studies among TGW from other countries (Lacombe-Duncan, 2016; Logie et al., 2019). Our findings showed that within TGW communities, TGWLH experienced discrimination. Consequently, fear of discrimination from the TGW community, sometimes their only source of support, also prevents TGWLH from disclosing their HIV status and contributes to delayed ART initiation or non-adherence. We also found that the support offered to TGWLH by the closely-knit, although hierarchical, hijra communities could potentially counter the effects of transgender identity and sex work stigmas – thus, serving as a resilience resource (Woodward et al., 2017).
In line with Stall et al.’s syndemics production model among gay men (Stall et al., 2008), we found that psychosocial syndemic conditions such as depression and problematic alcohol use can result from cumulative experiences of discrimination in healthcare settings and from TGW communities (Figure 1); future research is needed to explore these pathways in detail. Other studies too have reported associations between discrimination experiences, depression, and problematic alcohol use among TGW (Lacombe-Duncan et al., 2019; Nemoto et al., 2011). Similarly, the present study’s finding that syndemic conditions (e.g., depression and problematic alcohol use) can lead to ART non-adherence or HIV care disengagement is consistent with the results from diverse settings (Glynn et al., 2019; Kalichman et al., 2017; Lacombe-Duncan et al., 2019). Although not explicitly reported by the present study’s participants, constant vigilance in keeping one’s HIV status a secret, including hiding antiretrovirals, is likely to be highly stressful – affecting one’s mental health (Turan, Hatcher, et al., 2017), and likely influencing treatment engagement.
Gender affirmation and HIV care engagement
We found that lack of social gender affirmation from healthcare providers (e.g., misgendering), unmet need for medical gender-affirmation procedures (e.g., feminising hormone therapy) in public hospitals (Singh et al., 2014), and problems related to legal gender affirmation (e.g., need for legal identity documents for ART registration) were related to delayed ART initiation (Beattie et al., 2012; Chakrapani et al., 2011) or care interruptions (Figure 1). Studies from high-income countries too have identified similar connections between different types of gender affirmation (social, medical, and legal gender affirmation) and HIV care disengagement (Cicero et al., 2019; Sevelius et al., 2019), underscoring the need to offer gender-affirming care to improve HIV care engagement. Furthermore, we found that the lack of social gender affirmation by partners was linked to depression and this may influence HIV care engagement, an area that warrants further exploration.
Role of resilience
Resilience, the process of overcoming the negative effects of adversity and avoiding the negative trajectories, is not necessarily an individual trait, but also operates at interpersonal and community levels (Fergus & Zimmerman, 2005). Our findings showed that, despite its hierarchical nature and associated power dynamics, hijra communities serve as an important source of resilience for TGWLH, especially as most TGW do not have support from their birth families (Chakrapani et al., 2018). The present study’s findings showed that gurus and co-chelas provide financial support and other tangible support like reminders to take antiretrovirals, and affirm the gender identity of TGW community members. These interpersonal and community-level resilience resources thus seem to partly mitigate the effects of multiple stigmas (from sources outside TGW communities) on ART initiation and retention in care. Our findings are in line with studies from other countries showing that support from TGW communities is an important resilience resource in contributing to better mental health (Puckett et al., 2019) and to access health services (Perez-Brumer et al., 2017). Thus, interventions to enhance support provision from within TGW communities to improve HIV treatment outcomes and the overall wellness of TGW are likely to be effective and efficient, and merit further evaluation.
Limitations
This study has several limitations. We used a purposive sample of TGWLH recruited from urban CBOs that provide HIV-related services. TGWLH not associated with CBOs and those in rural areas may experience a different set of barriers to HIV care than did those in our sample. Future studies would also benefit from conducting in-depth or key informant interviews with healthcare providers and trans-community leaders, providing source and methods triangulation (Denzin & Lincoln, 2018). Future studies on HIV care engagement among TGW also need to consider including additional subgroups of TGWLH (e.g., those not in HIV care, those in rural areas) using longitudinal mixed methods approaches to better understand potential causal pathways we found between multiple stigmas, gender affirmation needs, psychosocial syndemic conditions, and ART initiation and retention in care.
Conclusion
We found that stigmas related to gender identity, sex work, and HIV status either alone or in combination directly or indirectly (through the production of one or more psychosocial syndemic conditions) contribute to delayed ART initiation and care disengagement among TGWLH. Unmet social, medical and legal gender affirmation needs also negatively influence retention in HIV care. Improving HIV care engagement efforts among TGWLH could be efficiently strengthened with interventions to reduce multiple and intersecting stigma at healthcare and transgender community levels by: incorporating screening for and addressing psychosocial syndemic conditions in existing individual-level HIV care interventions; providing gender-affirming and non-discriminatory culturally and structurally competent care in healthcare settings (Metzl & Hansen, 2014); and fostering resilience by increasing support from and solidarity within transgender communities in India.
Acknowledgements
The authors wish to thank the transgender women site leaders and peer outreach workers in Delhi, Mumbai, and Hyderabad; India HIV/AIDS Alliance’s Gender and Sexuality team; and Vihaan Care and Support program teams for their support.
Funding
This work was supported by the United States National Institutes of Health (NIH) grants R21MH118102 and P30AI124414, National Institute of Allergy and Infectious Diseases, National Institute of Mental Health.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Beattie TS, Bhattacharjee P, Suresh M, Isac S, Ramesh BM, & Moses S (2012). Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. Journal of Epidemiology & Community Health, 66(Suppl 2), ii42–ii48. 10.1136/jech-2011-200475 [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Newman AP, & Noronha E (2018). Hijras/transgender women and Sex work in India: From marginalization to social protection. In Nuttbrock LA (Ed.), Transgender Sex work & society (pp. 214–235). Harrington Park Press. [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, & Dubrow R (2011). Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care, 23(12), 1687–1694. 10.1080/09540121.2011.582076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, Logie CH, & Samuel M (2017). Syndemics of depression, alcohol use, and victimisation, and their association with HIV-related sexual risk among men who have sex with men and transgender women in India. Global Public Health, 12(2), 250–265. 10.1080/17441692.2015.1091024 [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Willie TC, Shunmugam M, & Kershaw TS (2019). Syndemic classes, stigma, and sexual risk among transgender women in India. AIDS and Behavior, 23(6), 1518–1529. 10.1007/s10461-018-2373-1 [DOI] [PubMed] [Google Scholar]
- Charmaz K (2014). Constructing grounded theory. Sage. [Google Scholar]
- Cicero EC, Reisner SL, Silva SG, Merwin EI, & Humphreys JC (2019). Health care experiences of transgender adults: An integrated Mixed research literature review. ANS. Advances in Nursing Science, 42(2), 123–138. 10.1097/ANS.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin JM, & Strauss AL (2015). Basics of qualitative research: Techniques and procedures for developing grounded theory. Sage. [Google Scholar]
- Denzin NK, & Lincoln YS (2018). The Sage handbook of qualitative research. Sage Publications, Inc. [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, & Copenhaver MM (2013). HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS and Behavior, 17(5), 1785–1795. 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus S, & Zimmerman MA (2005). Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health, 26(1), 399–419. 10.1146/annurev.publhealth.26.021304.144357 [DOI] [PubMed] [Google Scholar]
- Glynn TR, Safren SA, Carrico AW, Mendez NA, Duthely LM, Dale SK, Jones DL, Feaster DJ, & Rodriguez AE (2019). High levels of syndemics and their association with adherence, viral non-suppression, and biobehavioral transmission risk in Miami, a U.S. City with an HIV/AIDS epidemic. AIDS and Behavior, 23(11), 2956–2965. 10.1007/s10461-019-02619-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalil EM, Wilson EC, Luz PM, Velasque L, Moreira RI, Castro CV, Monteiro L, Garcia ACF, Cardoso SW, Coelho LE, McFarland W, Liu AY, Veloso VG, Buchbinder S, & Grinsztejn B (2017). HIV testing and the care continuum among transgender women: Population estimates from Rio de Janeiro, Brazil. Journal of the International AIDS Society, 20(1), 21873–21873. 10.7448/IAS.20.1.21873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Hernandez D, Finneran S, Price D, & Driver R (2017). Transgender women and HIV-related health disparities: Falling off the HIV treatment cascade. Sexual Health, 14(5), 469–476. 10.1071/SH17015 [DOI] [PubMed] [Google Scholar]
- Lacombe-Duncan A (2016). An Intersectional perspective on access to HIV-related healthcare for transgender women. Transgender Health, 1(1), 137–141. 10.1089/trgh.2016.0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacombe-Duncan A, Bauer GR, Logie CH, Newman PA, Shokoohi M, Kay ES, Persad Y, O’Brien N, Kaida A, de Pokomandy A, & Loutfy M (2019). The HIV care cascade among transgender women with HIV in Canada: A mixed-methods study. AIDS Patient Care and STDs, 33(7), 308–322. 10.1089/apc.2019.0013 [DOI] [PubMed] [Google Scholar]
- Logie CH, Lacombe-Duncan A, Persad Y, Ferguson TB, Yehdego DM, Ryan S, Forrester M, Moses C, & Guta A (2019). The TRANScending love arts-based workshop to address self-acceptance and intersectional stigma among transgender women of color in Toronto, Canada: Findings from a qualitative implementation science study. Transgend Health, 4(1), 35–45. 10.1089/trgh.2018.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JA (2012). A realist approach for qualitative research. Sage. [Google Scholar]
- Metzl JM, & Hansen H (2014). Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine (1982), 103, 126–133. 10.1016/j.socscimed.2013.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NACO. (2016). National IBBS 2014–15: Hijras/Transgender people..
- NACO. (2017a). HIV Sentinel Surveillance: Technical Brief, India 2016–17. National AIDS Control Organisation, Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- NACO. (2017b). Revised guidelines on initiation of antiretroviral therapy (ART). Office memo, National AIDS Control Organisation, Government of India. http://naco.gov.in/sites/default/files/Scan_OM%20CST.pdf [Google Scholar]
- Nemoto T, Bodeker B, & Iwamoto M (2011). Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. American Journal of Public Health, 101(10), 1980–1988. 10.2105/AJPH.2010.197285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, & Nemoto T (2010). HIV in transgender communities: Syndemic dynamics and a need for multicomponent interventions. Journal of Acquired Immune Deficiency Syndromes, 55(Suppl 2), S91–S93. 10.1097/QAI.0b013e3181fbc9ec [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MQ (2015). Qualitative research & evaluation methods: Integrating theory and practice. Sage. [Google Scholar]
- Perez-Brumer AG, Reisner SL, McLean SA, Silva-Santisteban A, Huerta L, Mayer KH, Sanchez J, Clark JL, Mimiaga MJ, & Lama JR (2017). Leveraging social capital: Multilevel stigma, associated HIV vulnerabilities, and social resilience strategies among transgender women in Lima, Peru. Journal of the International Aids Society, 20(1), 21462. 10.7448/IAS.20.1.21462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina C, Dange A, Rawat S, Jadhav U, Arnsten JH, Chhabra R, & Patel VV (2018). Antiretroviral treatment uptake and adherence among men who have sex with men and transgender women with HIV in Mumbai, India: A cross-sectional study. Journal of the Association of Nurses in Aids Care, 29(2), 310–316. 10.1016/j.jana.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T, Scheim A, Xavier J, Reisner S, & Baral S (2016). Global epidemiology of HIV infection and related syndemics affecting transgender people. Journal of Acquired Immune Deficiency Syndromes, 72(Suppl 3), S210–S219. 10.1097/QAI.0000000000001087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puckett JA, Matsuno E, Dyar C, Mustanski B, & Newcomb ME (2019). Mental health and resilience in transgender individuals: What type of support makes a difference? Journal of Family Psychology, 33(8), 954–965. 10.1037/fam0000561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinius M, Wiklander M, Wettergren L, Svedhem V, & Eriksson LE (2018). The relationship between stigma and health-related quality of life in people living with HIV who have full access to antiretroviral treatment: An assessment of Earnshaw and Chaudoir’s HIV stigma framework using empirical data. AIDS and Behavior, 22(12), 3795–3806. 10.1007/s10461-018-2041-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Jadwin-Cakmak L, White Hughto JM, Martinez M, Salomon L, & Harper GW (2017). Characterizing the HIV prevention and care continua in a sample of transgender youth in the U.S. AIDS and Behavior, 21(12), 3312–3327. 10.1007/s10461-017-1938-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, Holland CE, Max R, & Baral SD (2016). Global health burden and needs of transgender populations: A review. The Lancet, 388(10042), 412–436. 10.1016/s0140-6736(16)00684-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie J, & Spencer L (1994). Qualitative data analysis for applied policy research. In Bryman A & Burgess R (Eds.), Analysing qualitative data (pp. 173–194). Routledge. [Google Scholar]
- Sandfort TGM, Dominguez K, Kayange N, Ogendo A, Panchia R, Chen YQ, Chege W, Cummings V, Guo X, Hamilton EL, Stirratt M, & Eshleman SH (2019). HIV testing and the HIV care continuum among sub-Saharan African men who have sex with men and transgender women screened for participation in HPTN 075. PLoS One, 14(5), e0217501. 10.1371/journal.pone.0217501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius J, Chakravarty D, Neilands TB, Keatley J, Shade SB, Johnson MO, Rebchook G, & HRSA SPNS Transgender Women of Color Study Group. (2019). Evidence for the model of gender affirmation: The role of gender affirmation and healthcare empowerment in viral suppression among transgender women of color living with HIV. AIDS and Behavior, 25(Suppl 1), 64–71. 10.1007/s10461-019-02544-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius J, Patouhas E, Keatley JG, & Johnson MO (2014). Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Annals of Behavioral Medicine, 47(1), 5–16. 10.1007/s12160-013-9565-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw SY, Lorway RR, Deering KN, Avery L, Mohan HL, Bhattacharjee P, Reza-Paul S, Isac S, Ramesh BM, Washington R, Moses S, & Blanchard JF (2012). Factors associated with sexual violence against men who have sex with men and transgendered individuals in Karnataka, India. PLoS One, 7(3), e31705. 10.1371/journal.pone.0031705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, & Clair S (2003). Syndemics and public health: Reconceptualizing disease in bio-social context. Medical Anthropology Quarterly, 17(4), 423–441. 10.1525/maq.2003.17.4.423 [DOI] [PubMed] [Google Scholar]
- Singh Y, Aher A, Shaikh S, Mehta S, Robertson J, & Chakrapani V (2014). Gender transition services for hijras and other male-to-female transgender people in India: Availability and barriers to access and use. International Journal of Transgenderism, 15(1), 1–15. 10.1080/15532739.2014.890559 [DOI] [Google Scholar]
- Srivastava A, Sivasubramanian M, & Goldbach JT (2021). Mental health and gender transitioning among hijra individuals: A qualitative approach using the minority stress model. Culture, Health & Sexuality, 23(6), 757–771. 10.1080/13691058.2020.1727955 [DOI] [PubMed] [Google Scholar]
- Stall R, Friedman M, & Catania JA (2008). Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In Wolitski RJ, Stall R, & Valdiserri RO (Eds.), Unequal opportunity: Health disparities affecting gay and bisexual men in the United States (pp. 251–274). Oxford University Press. [Google Scholar]
- Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, & Turan JM (2017). How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS and Behavior, 21(1), 283–291. 10.1007/s10461-016-1451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, & Turan JM (2017). Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American Journal of Public Health, 107(6), 863–869. 10.2105/AJPH.2017.303744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward EN, Banks RJ, Marks AK, & Pantalone DW (2017). Identifying resilience resources for HIV prevention among sexual minority men: A systematic review. AIDS and Behavior, 21(10), 2860–2873. 10.1007/s10461-016-1608-2 [DOI] [PubMed] [Google Scholar]


