Abstract
Introduction
This study aimed to evaluate the lenticule integrity and refractive outcomes of a new technique, Ye’s swing technique, during small-incision lenticule extraction (SMILE).
Methods
This prospective study enrolled patients who underwent the SMILE procedure using a modified technique for lenticule dissection. Per the standard SMILE procedure, the cap cut was opened using a hook, and an anterior dissection was performed with a counterclockwise swing, from 8 to 12 o’clock. A posterior dissection was then performed by swinging counterclockwise, leaving a thin band of the peripheral rim undissected, from 8 to 4 o’clock. The counterclockwise swing was continued to separate the edges of the rim from 4 to 12 o’clock, after which microforceps were used to extract the lenticules. The primary outcome measures were safety and lenticule integrity at the end of the surgery, and the secondary outcome measure was efficacy. Changes in the ocular parameters from the preoperative visit to 1 month postoperative, including uncorrected and corrected distance visual acuity, manifest refraction, lenticule quality, and lenticule residual, were assessed using optical coherence tomography.
Results
A total of 246 patients (490 eyes) with myopia and myopic astigmatism were included in the present study. The dissected lenticules ranged in size from 52 to 148 µm. Postoperatively, the lenticule was completely and successfully extracted in all cases. There was no incisional edge tearing during lenticule separation.
Conclusions
Ye’s swing technique is a safe and effective procedure for lenticule dissection and refractive outcomes. We have now adopted this technique as our routine method for performing the SMILE procedure.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40123-022-00612-w.
Keywords: Small-incision lenticule extraction, SMILE, Myopia, Swing technique, Lenticule tear, Intraoperative complications
Key Summary Points
| The traditional method of lenticule extraction in small-incision lenticule extraction (SMILE) is associated with several intraoperative complications. We therefore evaluated the refractive outcomes of a new technique for lenticule dissection technique, Ye’s swing technique, during SMILE. | |
| The cap cut was opened using a hook, and an anterior dissection was performed with a counterclockwise swing, from 8 to 12 o’clock. A posterior dissection was then performed by swinging counterclockwise, leaving a thin band of the peripheral rim undissected, from 8 to 4 o’clock. The counterclockwise swing was continued to separate the edges of the rim from 4 to 12 o’clock, after which microforceps were used to extract the lenticules. | |
| Postoperatively, the lenticule was completely and successfully extracted in all cases. There was no incisional edge tearing during lenticule separation. | |
| Ye’s swing technique is efficient for lenticule separation and extraction. We have now adopted this technique as our routine method for performing the SMILE procedure. |
Digital Features
This article is published with digital features, including a video abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.21438069.
Introduction
Small-incision lenticule extraction (SMILE) is widely utilized for the correction of myopia and myopic astigmatism because of its efficacy, safety, and predictability [1]. Numerous studies on the SMILE procedure have reported excellent outcomes, such as fewer corneal flap dislocations, better long-term biomechanical stability, and fewer cases of dry eye [2, 3]. Although the entire SMILE procedure is performed using a femtosecond laser, the lenticule is extracted manually, which is technically challenging and can lead to complications [4]. Complications can result in increased corneal stromal damage and inflammation, which lead to delayed visual recovery, diffuse lamellar keratitis, corneal opacity, and poor visual outcomes [5]. Difficulties are frequently encountered during lenticule dissection and extraction, especially in patients with low myopia and for surgeons who are not experienced with the SMILE procedure [3].
Lenticule extraction is traditionally performed by dissecting the anterior and posterior surfaces of lenticule with separated edges [6]. However, intraoperative events reported in two large-scale studies showed an incidence rate of 1.9% (34 of 1500 eyes) for difficult lenticule extractions, 1.8% with small tears at the incision site, 0.3% with cap perforation, 0.1% with major tears [7], and 0.27% (8 of 3004 eyes) with tearing of the lenticule [8]. Numerous modifications to conventional SMILE techniques have been described in an effort to simplify the process of lenticule separation and to minimize complications [9]. Limitations, however, still exist, such as the presence of certain conditions which involve uneven laser scanning during lenticuloschisis [10, 11], an increased risk of cap tearing during lifting and swinging [12], and difficulties in the final segments during sequential segmental lenticular side-cut dissections [13].
In the present study, we describe a new method for lenticule separation and extraction during SMILE, referred to as Ye’s swing technique. This modified technique maintains a residual peripheral rim on the posterior side of the lenticule, which does not exist in the traditional technique. Herein, we describe our modified lenticule dissection and extraction technique, which facilitates the crucial manual step in the procedure, especially in thin lenticules.
Methods
Patients and Clinical Outcomes
This study was part of a prospective audit of consecutive patients who underwent the SMILE procedure between May 2022 and July 2022 by the same refractive surgeon (Y.-F.Y.) at the Eye Hospital of Wenzhou Medical University, Hangzhou. The protocol for the present study followed the tenets of the Declaration of Helsinki, and was approved by the ethics committee at the Eye Hospital of Wenzhou Medical University. Written informed consent was obtained from all participants.
Patients scheduled to undergo SMILE surgery to correct myopia and myopic astigmatism were recruited in this study. The inclusion criteria for this study were myopia of less than 10 D with or without myopic astigmatism, stable refraction for at least 1 year, and corrected distance visual acuity (CDVA) better than 20/25 Snellen refraction. The exclusion criteria for refractive surgery were a corneal thickness of less than 480 μm, suspicion of keratoconus on corneal topography, cataract(s), or ocular inflammation. Patients who wore soft contact lenses were instructed to stop wearing them at least 2 weeks prior to surgery, and patients who wore rigid contact lenses were instructed to stop wearing them at least 4 weeks prior to surgery.
Surgical Technique
The same surgeon (Y.-F.Y.) performed all of the SMILE procedures as previously described [14]. The VisuMax femtosecond laser system with a fixed repetition rate of 500 kHz was utilized for all of the SMILE procedures, using the following parameters: pulse energy 140 nJ; anterior cap depth 110–120 µm; cap diameter 7.5 mm; and side-cut incision position 110° with a width of 2 mm. A lenticule diameter (optical zone) of 6.0–7.0 mm was selected, based on the central corneal thickness and the pupil size in the dark, with no transition zone for spherical errors, and a 0.10 mm transition zone for cylinder errors. Patients aged 18 to 35 years accepted full correction, while for those over 36 years, 0.25–0.75 D undercorrection of sphere error was performed during SMILE surgery.
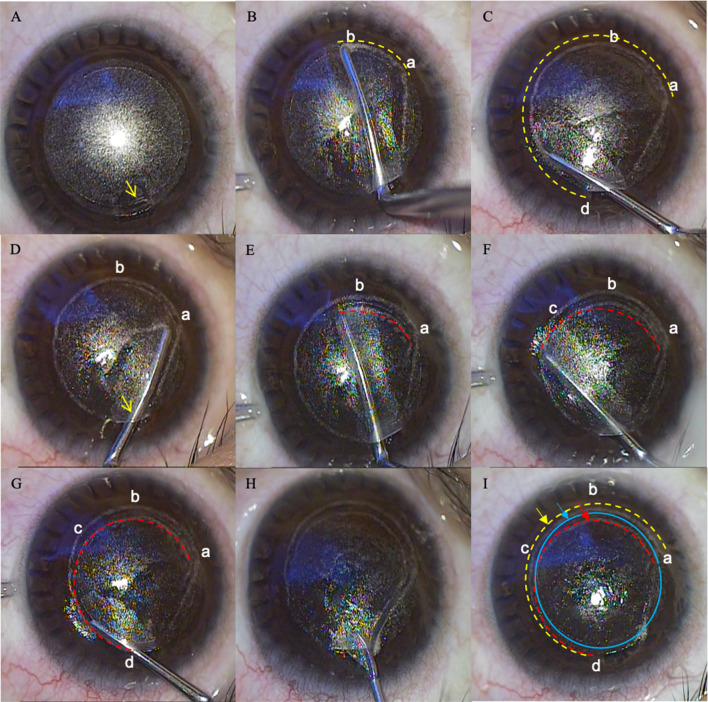
The traditional SMILE technique has been previously described as follows [6]: immediately after completing the femtosecond laser application, the lenticule was extracted after the edges of the anterior and posterior surface were separated. In the modified technique evaluated in the present study, the lenticule was separated and extracted as follows: (1) the cap cut was opened along its entire length from left to right, while the lenticule cut was dissected to only half the length from right to left using a small surgical hook (Suzhou Mingren Medical Equipment Co., Ltd); (2) the anterior dissection was performed counterclockwise from point a (corresponding to 8 o’clock) to point d (corresponding to 12 o’clock), with a swing by a blunt spatula (Intralasik flap spatula, MR-G134T-4, Suzhou Mingren Medical Equipment Co., Ltd), keeping the rest undissected to prevent lenticular movement (Fig. 1B, C); (3) the spatula was used to enter the cleavage plane on the posterior side of the lenticule to perform the partial swing counterclockwise from point a (corresponding to 8 o 'clock) to point c (corresponding to 4 o’clock), leaving a thin undissected band of the peripheral rim (Fig. 1D, E), then continuing the swing towards point d over the margin (Fig. 1F, G); and (4) microforceps (intraocular lens forceps 23G, MR-G116T-4, Suzhou Mingren Medical Equipment Co., Ltd.) were used to grasp the free end of the lenticule, pushing it towards the center of the cornea, and peeling it off gently clockwise in a continuous, circumferential motion (Fig. 1H). In order to ensure that there were no residual fragments left in the pocket after the extraction, the integrity of the lenticule was evaluated. All of the procedures were reversed when performed by left-handed surgeons (See video 1 in the online/HTML version of the manuscript or follow the digital features link under the abstract).
Fig. 1.
Schematic of the spatula separating the lenticule. A The cap cut was along its entire length from left to right, while the lenticule cut was dissected along half its length from right to left by a small surgical hook; B, C the anterior dissection was performed counterclockwise from point a to point d with a swing by a blunt spatula, keeping the rest undissected to prevent lenticular movement; D, E the spatula was used to enter the cleavage plane on the posterior side of the lenticule to perform the partial swing counterclockwise from point a to point c counterclockwise, leaving a thin undissected band of peripheral rim; F, G the swing was continued towards point d over the margin; H the microforceps were used to grasp the free end of the lenticule, push it towards the center of the cornea, and peel it off gently clockwise in a continuous, circumferential motion; and I the anterior lenticule side was cut along the yellow dotted track, while the posterior cut moved along the red dotted track in the lenticule–stroma space. Points a, b, and d represent 8, 6, and 12 o’clock, respectively. The red dotted line represents the movement track of the spatula tip
After surgery, topical 0.5% levofloxacin (Cravit; Santen, Inc.) eye drops were applied four times daily for 1 week, and 0.1% fluorometholone (Allergan, Inc.) eye drops and non-preserved artificial tears were used four times daily for the first week, which was then sequentially reduced to three, two, and one time every week thereafter.
Outcome Measurements
The primary outcome measures were safety and lenticule integrity at the end of the surgery, and the secondary outcome measure was efficacy. All patients underwent a detailed preoperative ophthalmological examination that included the following: an evaluation of the logarithm of the minimum angle of resolution (logMAR) for uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction, slit-lamp examination, intraocular pressure (non-contact tonometer, Topcon, Japan), pupil size (Atlas, Carl Zeiss Meditec, Jena, Germany), Scheimpflug-based corneal topography (Pentacam HR Type 70900, Oculus, Wetzlar, Germany), spectral-domain optical coherence tomography (Optovue RTVue XR Avanti, Optovue Inc., Fremont, CA, USA), and indirect fundoscopy. Experienced optometrists performed the manifest refractions for each patient. The efficacy index (ratio of postoperative UDVA to preoperative CDVA in decimals) and safety index (ratio of postoperative to preoperative CDVA in decimals) were calculated. Efficacy, predictability, stability, and safety were evaluated using standard graphs [15]. Cylinder axes from included left eyes were flipped vertically to avoid the risk of orientation errors. Target-induced astigmatism (TIA) was the astigmatic change that the surgery was expected to induce; surgically induced astigmatism (SIA) was the astigmatic change induced by the surgery in actuality [16].
Once extracted, the lenticule was examined under a microscope to evaluate its integrity, and the duration of the lenticule extraction was recorded on video. Follow-up visits were scheduled at both 1 day and 1 week after surgery. At each visit, the UDVA and CDVA were measured, a slit-lamp exam was performed, manifest refraction and corneal topography measurements were evaluated, and complications were assessed.
Video legend: Ye’s swing technique used during small-incision lenticule extraction surgery (MP4 29861 KB)
Results
Study Population
The modified Ye’s swing technique was successfully performed by the same surgeon in 490 eyes (246 patients) with myopia and myopic astigmatism. The characteristics of those included patients are presented in Table 1. For patients aged 18 to 35 years, the preoperative manifest refraction spherical equivalent ranged from − 1.125 to − 9.75 diopters (D), and the cylinder ranged from 0 to − 5.50 D. The mean optical central corneal thickness (CCT) was 545.23 ± 27.38 µm (range 487–636 µm). The lenticule thickness was 107.28 ± 23.53 µm (range 52–148 µm), with 189 eyes (36.7%) described as thin lenticules (< 100 µm) (Table 1).
Table 1.
Baseline and postoperative parameters of 490 eyes from 246 patients
| Characteristics | Aged 18–35 | n = 406 | Aged over 36a | n = 84 |
|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | |
| Age (years) | 24.15 ± 5.34 | (18 to 35) | 38.79 ± 2.76 | (36 to 46) |
| Right eyes/left eyes | 203:203 | 42:42 | ||
| Preoperative | ||||
| Sphere error (D) | − 4.49 ± 1.60 | (− 9.0 to − 0.25) | − 4.37 ± 1.48 | (− 8.25 to − 0.25) |
| Cylinder error (D) | − 0.91 ± 0.71 | (− 5.5 to 0) | − 0.74 ± 0.71 | (− 3.5 to 0) |
| Spherical equivalent refraction (D) | − 4.95 ± 1.62 | (− 9.75 to − 1.125) | − 4.74 ± 1.39 | (− 8.375 to − 2.0) |
| logMAR CDVA | 0 ± 0 | NA | 0 ± 0 | NA |
| CCT (µm) | 545.23 ± 27.38 | (487 to 636) | 541.95 ± 25.84 | (493 to 612) |
| Optical zone (mm) | 6.64 ± 0.14 | (6 to 6.7) | 6.67 ± 0.12 | (6.0 to 7.0) |
| Lenticule thickness (µm) | 107.28 ± 23.53 | (52 to 148) | 101.54 ± 21.48 | (55 to 141) |
| IOP (mmHg) | 15.06 ± 2.40 | (9.1 to 22.0) | 13.88 ± 2.08 | (8.9 to 19.2) |
| Postoperative | ||||
| Sphere error (D) | 0.25 ± 0.32 | (− 0.75 to 1.0) | 0.08 ± 0.37 | (− 1.0 to 1.25) |
| Cylinder error (D) | − 0.31 ± 0.27 | (− 1.5 to 0) | − 0.27 ± 0.24 | (− 1.0 to 0) |
| Spherical equivalent refraction (D) | 0.10 ± 0.34 | (− 1.0 to 1.0) | − 0.06 ± 0.37 | (− 1.125 to 1.0) |
| logMAR UDVA | − 0.04 ± 0.05 | (− 0.08 to 0.22) | − 0.03 ± 0.07 | (− 0.08 to 0.22) |
| logMAR CDVA | − 0.03 ± 0.05 | (− 0.08 to 0.15) | − 0.02 ± 0.04 | (− 0.08 to 0.09) |
| Efficacy index | 1.12 ± 0.12 | (0.6 to 1.2) | 1.08 ± 0.16 | (0.6 to 1.2) |
| Safety index | 1.07 ± 0.12 | (0.7 to 1.2) | 1.04 ± 0.10 | (0.8 to 1.2) |
Results are expressed as mean ± standard deviation (range)
CCT central corneal thickness, CDVA corrected-distance visual acuity, D diopter, logMAR logarithm of the minimum angle of resolution, SE spherical equivalent, UDVA uncorrected distance visual acuity, NA not available
aPatients aged over 36 years underwent 0.25–0.75 D undercorrection of sphere error during SMILE surgery
Visual Acuity, Efficacy, and Safety
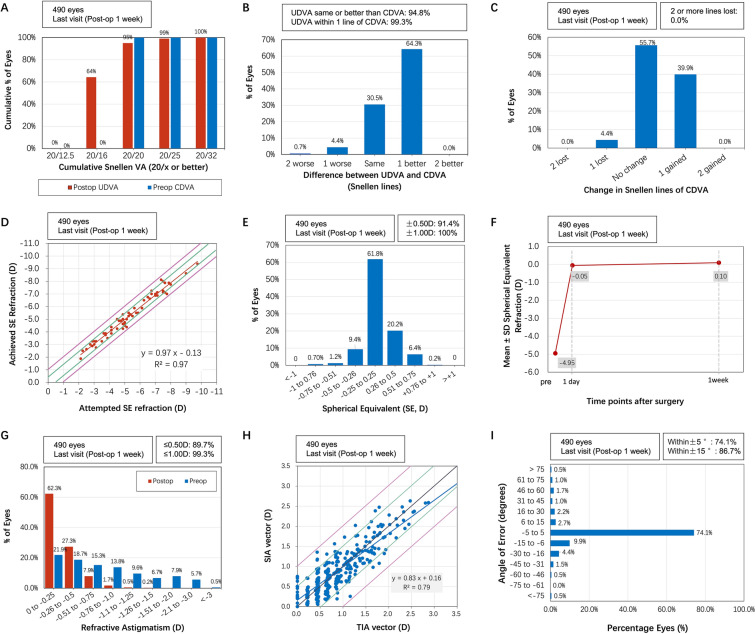
At 1 week postoperatively, all eyes (100%) had UDVA of 20/25 or better (Fig. 2A). The UDVA improved in 261/406 (64.3%) of the treated eyes after SMILE surgery, exhibiting a gain of one or more lines in the 1-week postoperative UDVA (Fig. 2B). Eighteen eyes (4.4%) lost one line of CDVA after surgery (Fig. 2C). At 1 week after SMILE surgery, the mean efficacy index and safety index were 1.12 ± 0.12 and 1.07 ± 0.12 in patients aged 18–35, respectively (Table 1). The linear regression model of attempted SE versus achieved SE achieved an R2 of 97% (Fig. 2D). SE predictability was within ± 0.5 D in 91.4% of eyes after SMILE surgery (Fig. 2E). The predictability of astigmatism correction was 89.7% of eyes within ± 0.5 D (Fig. 2G). Figure 2H showed the linear regression model between the attempted target-induced astigmatism vector (TIA) and the achieved surgically induced astigmatism vector (SIA), with R2 = 0.79 in SMILE group. A total of 301 out of 406 (74.1%) eyes achieved an angle of error (AofE) within ± 5° (P = 0.55; Fig. 2I).
Fig. 2.
Visual outcomes of 406 eyes in 204 patients aged 18 to 35 years after small-incision lenticule extraction (SMILE). A Cumulative 1-week postoperative uncorrected distance visual acuity (UDVA) and preoperative corrected distance visual acuity (CDVA). B Changes in the Snellen lines of postoperative UDVA compared with preoperative CDVA. C Changes in the Snellen lines of postoperative CDVA compared with preoperative CDVA. D Attempted versus achieved changes in SER at 1 week after surgery. E Accuracy of the spherical equivalent refraction (SER) compared with the intended target. F Stability of the SER over 1 week. G Distribution of preoperative and 6-month postoperative cylinders. H Target-induced versus surgically induced astigmatism vectors at 1 week after surgery are shown. I Refractive astigmatism angle of error distribution is shown at 1 week after surgery. D diopters
Lenticule Quality and Complications
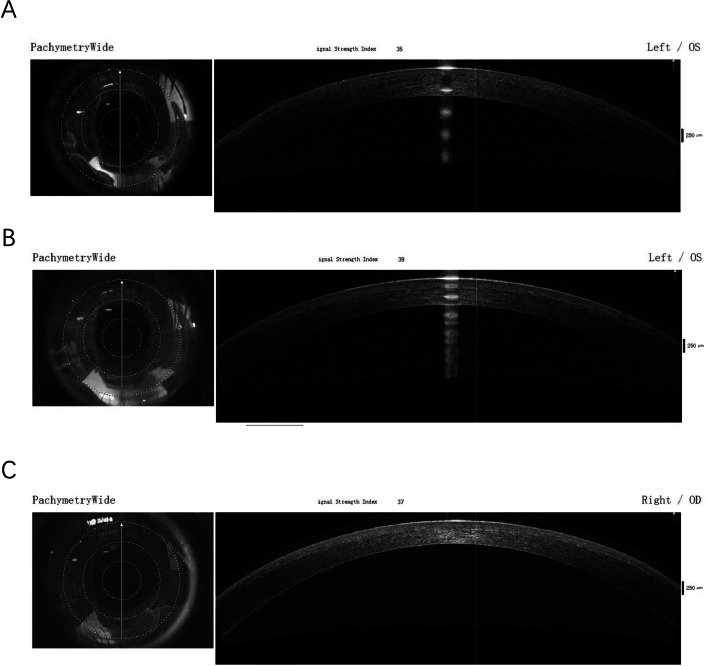
The lenticule was extracted completely and successfully. There were no cases of incisional edge tearing during lenticule separation, nor were any complications observed, such as cap tears, lenticule tears, retained lenticule fragments, or misidentified lenticule planes (Fig. 3). Furthermore, diffuse lamellar keratitis was not observed in the present study, nor were there any cases of epithelial defects, infections, corneal haze, or any other severe complications.
Fig. 3.
Anterior-segment domain optical coherence tomography image of the cornea after SMILE. A A left eye with a lenticule dissection of 52 µm. B A left eye with a lenticule dissection of 100 µm. C A right eye with a lenticule dissection of 143 µm
Discussion
Lenticule dissection and extraction is the most challenging step during the SMILE procedure, and the difficulties suffered in this step may result in cap tears, side-cut tears, retained lenticule or fragments, epithelial defects, irregular interfaces, and delayed visual recovery [8]. In the traditional SMILE procedure, the lenticule is separated from the corneal cap above and the stroma bed below, and then extracted using forceps [17]. In some difficult cases, it is necessary to attempt the separation several times, resulting in more disruption to the corneal tissue and longer operative times [18]. In the present study, we have described a new technique for the SMILE procedure, which leaves a residual peripheral rim on the posterior side of the lenticule. All of the eyes included in the present study underwent this modified SMILE, Ye’s swing technique, and all lenticules were successfully extracted, meaning they were all intact and complete after extraction. This proposed modified technique has several advantages. First, the spatula used to separate the lenticule only needs to be moved twice; therefore, it requires sufficiently less time, which may prevent postoperative corneal edema. Second, in the lower plane, the spatula keeps moving counterclockwise within the edge of the lenticule from 8 to 4 o’clock, allowing the controlled partial separation of the lenticule, which is held in place by a thin, undissected band of the peripheral rim. When the microforceps grasp the freed part of the lenticule, the peripheral rim can be removed with mild resistance using lenticulerrhexis.
Various modifications of the conventional SMILE technique simplify the process of lenticule separation but with some limitations [9]. Zhao et al. [10] introduced the continuous curvilinear lenticulerrhexis (CCL) technique, which simplified the dissection procedure by tearing and extracting the lenticule from the stromal bed in a continuous circumferential manner. Later, Ganesh and Brar [11] described a nondissective approach using only lenticuloschisis. These modifications, however, were limited by certain conditions, especially the high incidence (52.5%) of opaque bubble layer (OBL) formation during the femtosecond laser procedure [19]. Additionally, other studies have evaluated the clinical outcomes of the use of balanced salt solution (BSS) infiltration for dissection and extraction, while interface debris or a hydrated stroma might occur after irrigation [20, 21]. One modified technique for lenticule dissection and extraction, Chung’s swing technique, was described by Kim et al. [12]. There are concerns with this technique, however, about the edge tearing when the spatula ascended to the lenticule–cap interface by lifting and swinging at the 12 to 3 o’clock and the 8 to 11 o’clock positions, which increased the risk of the cap tearing. Another modified technique, sequential segmental terminal lenticular side-cut dissection, breaks up the edge dissection into 4–5 sequential segments to achieve complete lenticular separation and extraction [13]. Lenticular mobility, however, might not allow for the complete dissection of the final segments [13].
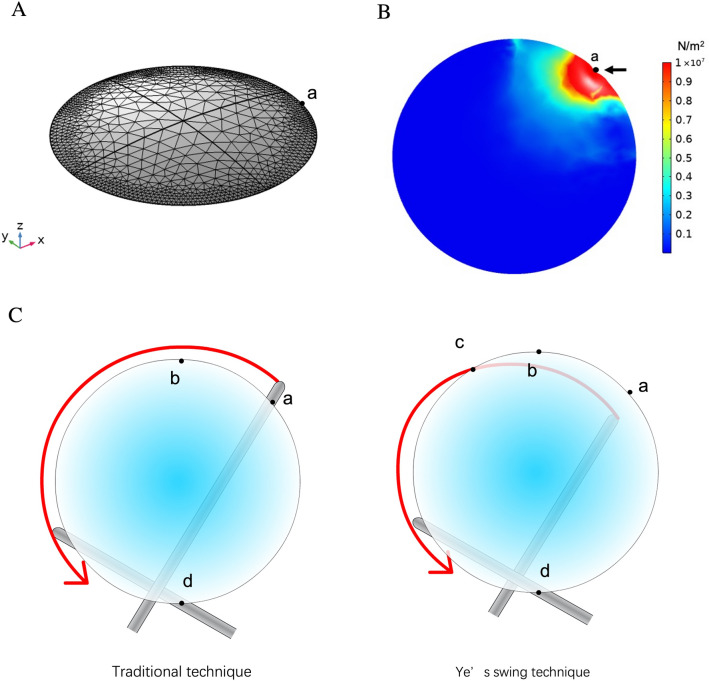
In terms of intraoperative events, margin tears and the resultant partial lenticular extraction may occur when the separation force is larger than the lenticule edge stress. Considering that thinner lenticules are more difficult to dissect and can tear easily, Jacob et al. designed sequential segmental dissection for thin lenticules [13]. Therefore, we established an edge stress model to illustrate the processes based on the finite element analysis software COMSOL Multiphysics 5.5 (COMSOL Inc., Burlington, MA, USA). First, a three-dimensional (3D) shape was created on the basis of the cut lenticle shape, with the thickness of the lenticule being 50–140 μm and the diameter 6.0–6.7 mm (Fig. 4A). Next, we set the material-related physical quantities for the model. The corneal density was set to 1.4 g/mm3, Young’s modulus was 3.8 MPa, and Poisson’s ratio was 0.49. The solid mechanics physics were then added to the geometry model, which was set to a linear elastic material, while the fixed constraints and point loads were set in the model. The point load was set to 0.5 N, acting on the edge of the quarter circle, as shown at point a in Fig. 4B. As shown in our operating model (Fig. 4C), we hypothesized that the movement of the spatula is limited to within the edge of the lenticule, which maintains the patency of the thinnest position. When the spatula moves, the force on the lenticule is less than the tension that which could break the edge of the lenticule; therefore, tearing and damage of the lenticule can be avoided, and the lenticule can be completely extracted. Theoretically, this modified technique minimizes the risk of lenticule tears, while retaining the lenticule or its fragments, particularly in thin lenticules. Further studies are warranted to quantify the manual tension during the dissection and extraction portions of the procedure.
Fig. 4.
An edge stress model based on Ye’s swing technique. A Three-dimensional (3D) shape based on the cut lenticle shape. B Calculated edge stress of point a by model. C Schematic of Ye’s swing technique
The present study has several limitations. First, although this was a prospective study, there was no control group that underwent the traditional SMILE technique. In an ideal situation, the data would be more reliable if the traditional method was performed on one eye and a different technique was performed on the contralateral eye of the same patient. Second, at 1 week after surgery, the refraction was still changing over time until 6 months postoperative, considering the wound healing response of the cornea. Therefore, longer observation periods may be required to determine long-term postoperative outcomes. Third, we assessed lenticule integrity both during surgery and on optical coherence tomography (OCT) scans. We did not quantify microdistortions induced by surgery in Bowman’s layer, although further studies were designed to evaluate these microdistortions in a larger sample size. Fourth, corneal changes, such as inflammatory responses and corneal micromodifications, were not evaluated using confocal microscopy, although confocal microscopy or histologic examination would be helpful to further assess the outcomes of this modified technique.
Conclusion
The modified technique, Ye’s swing technique, is a safe and effective procedure. The modified technique evaluated in the present study allows surgeons to easily separate and extract lenticules with minimal incisional edge tearing. Given the results of the present study, it is reasonable to believe that Ye’s swing technique is a promising new method that could potentially become the primary technique for lenticule extraction during the SMILE procedure.
Acknowledgements
The authors would like to express their deepest gratitude to all of the individuals who participated in the present study, as well as all their colleagues in the Department of Refractive Surgery Center for coordination and logistic arrangements of this study.
Funding
The present work, including the journal’s Rapid Service fee, was supported, in part, by the Science and Technology Plan Project of the Wenzhou Science and Technology Bureau (Y20190638; Yu-Feng Ye).
Author Contributions
Yu-Feng Ye and Shih-Mo Yang provided the conceptualization and design of the study. Jun Zhu and Fen-Fen Li completed the data collection. Fen-Fen Li analyzed and interpreted the data. Jun Zhu and Fen-Fen Li wrote the manuscript. Qi Dai, Dan Cheng, Fang-Jun Bao, Shih-Mo Yang, and Yu-Feng Ye provided critical revisions to the manuscript.
Disclosures
Jun Zhu, Fen-Fen Li, Qi Dai, Dan Cheng, Fang-Jun Bao, Shih-Mo Yang and Yu-Feng Ye all confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
The protocol for the present study followed the tenets of the Declaration of Helsinki, and was approved by the ethics committee of the Eye Hospital of Wenzhou Medical University (No. H2022-002-K-02–01). Written informed consent was obtained from all participants.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Footnotes
Jun Zhu and Fen-Fen Li contributed equally to this paper.
Contributor Information
Shih-Mo Yang, Email: smyang@shu.edu.cn.
Yu-Feng Ye, Email: yyf0571@mail.eye.ac.cn.
References
- 1.Dishler JG, Slade S, Seifert S, Schallhorn SC. Small-incision lenticule extraction (SMILE) for the correction of myopia with astigmatism: outcomes of the United States Food and Drug Administration premarket approval clinical trial. Ophthalmology. 2020;127(8):1020–1034. doi: 10.1016/j.ophtha.2020.01.010. [DOI] [PubMed] [Google Scholar]
- 2.Kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis. Cornea. 2017;36(1):85–91. doi: 10.1097/ICO.0000000000000999. [DOI] [PubMed] [Google Scholar]
- 3.Titiyal JS, Kaur M, Rathi A, Falera R, Chaniyara M, Sharma N. Learning curve of small incision lenticule extraction: challenges and complications. Cornea. 2017;36(11):1377–1382. doi: 10.1097/ICO.0000000000001323. [DOI] [PubMed] [Google Scholar]
- 4.Ang M, Mehta JS, Chan C, Htoon HM, Koh JC, Tan DT. Refractive lenticule extraction: transition and comparison of 3 surgical techniques. J Cataract Refract Surg. 2014;40(9):1415–1424. doi: 10.1016/j.jcrs.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 5.Chan TCY, Ng ALK, Cheng GPM, et al. Effect of the learning curve on visual and refractive outcomes of small-incision lenticule extraction. Cornea. 2017;36(9):1044–1050. doi: 10.1097/ICO.0000000000001246. [DOI] [PubMed] [Google Scholar]
- 6.Li M, Zhou Z, Shen Y, Knorz MC, Gong L, Zhou X. Comparison of corneal sensation between small incision lenticule extraction (SMILE) and femtosecond laser-assisted LASIK for myopia. J Refract Surg. 2014;30(2):94–100. doi: 10.3928/1081597X-20140120-04. [DOI] [PubMed] [Google Scholar]
- 7.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014;121(4):822–828. doi: 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Ma J, Zhang J, et al. Incidence and management of intraoperative complications during small-incision lenticule extraction in 3004 cases. J Cataract Refract Surg. 2017;43(6):796–802. doi: 10.1016/j.jcrs.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 9.Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar AS, Rathi A. Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives. Clin Ophthalmol. 2018;12:1685–1699. doi: 10.2147/OPTH.S157172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao Y, Li M, Yao P, Shah R, Knorz MC, Zhou X. Development of the continuous curvilinear lenticulerrhexis technique for small incision lenticule extraction. J Refract Surg. 2015;31(1):16–21. doi: 10.3928/1081597X-20141218-02. [DOI] [PubMed] [Google Scholar]
- 11.Ganesh S, Brar S. Lenticuloschisis: a "no dissection" technique for lenticule extraction in small incision lenticule extraction. J Refract Surg. 2017;33(8):563–566. doi: 10.3928/1081597X-20170504-09. [DOI] [PubMed] [Google Scholar]
- 12.Kim BK, Mun SJ, Lee DG, Choi HT, Chung YT. Chung's swing technique: a new technique for small-incision lenticule extraction. BMC Ophthalmol. 2016;16(1):154. doi: 10.1186/s12886-016-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacob S, Agarwal A, Mazzotta C, Agarwal A, Raj JM. Sequential segmental terminal lenticular side-cut dissection for safe and effective small-incision lenticule extraction in thin lenticules. J Cataract Refract Surg. 2017;43(4):443–448. doi: 10.1016/j.jcrs.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Li FF, Yang YZ, Bao FJ, Cheng D, Zhu J, Ye YF. Comparison of astigmatic correction with and without cross-axis alignment during small incision lenticule extraction. J Refract Surg. 2022;38(10):624–631. doi: 10.3928/1081597X-20220830-01. [DOI] [PubMed] [Google Scholar]
- 15.Reinstein DZ, Carp GI, Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg. 2014;30(12):812–818. doi: 10.3928/1081597X-20141113-07. [DOI] [PubMed] [Google Scholar]
- 16.Alpins NA. A new method of analyzing vectors for changes in astigmatism. J Cataract Refract Surg. 1993;19(4):524–533. doi: 10.1016/S0886-3350(13)80617-7. [DOI] [PubMed] [Google Scholar]
- 17.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95(3):335–339. doi: 10.1136/bjo.2009.174284. [DOI] [PubMed] [Google Scholar]
- 18.Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-Caban L, Fenzl CR. Small-incision lenticule extraction. J Cataract Refract Surg. 2015;41(3):652–665. doi: 10.1016/j.jcrs.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Liu CH, Sun CC, Hui-Kang Ma D, et al. Opaque bubble layer: incidence, risk factors, and clinical relevance. J Cataract Refract Surg. 2014;40(3):435–440. doi: 10.1016/j.jcrs.2013.08.055. [DOI] [PubMed] [Google Scholar]
- 20.Liu T, Zhu X, Chen K, Bai J. Visual outcomes after balanced salt solution infiltration during lenticule separation in small-incision lenticule extraction for myopic astigmatism. Medicine (Baltimore) 2017;96(30):e7409. doi: 10.1097/MD.0000000000007409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ng ALK, Cheng GPM, Woo VCP, Jhanji V, Chan TCY. Comparing a new hydroexpression technique with conventional forceps method for SMILE lenticule removal. Br J Ophthalmol. 2018;102(8):1122–1126. doi: 10.1136/bjophthalmol-2017-310993. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article/as supplementary information files.