Abstract
Aim
This study examined the mediating effect of circadian rhythm amplitude (LV) and stability (FR) between work stress and sleep quality among Chinese shift‐working nurses (SWNs).
Design
A cross‐sectional study.
Methods
Three‐hundred and seventy‐nine nurses working in shifts were investigated by convenient sampling from six hospitals in Shanghai, China. The mediating effect was analysed using the structural equation model with bootstrapping procedures.
Results
Work stress could directly affect shift nurses' sleep quality and indirectly affect sleep quality through circadian rhythm amplitude and stability. The total indirect effects of work stress on sleep quality accounted for 36.7% of the total effect. The study revealed that poor sleep quality is very common among SWNs, which deserves attention. The mediating effect of the circadian rhythm provides new insights to improve sleep quality, not only by lightening the work stress but also by improving circadian rhythm in SWNs.
Keywords: circadian rhythm, mediation analysis, occupational stress, shift work schedule, sleep quality
1. BACKGROUND
Sleep disturbance among nurses is the most common adverse effect of shift work that provides 24‐hr care for patients (Di Muzio et al., 2020; Han et al., 2016; Zhang et al., 2016). Some previous studies found that 52.1%–83.2% of shift‐working nurses (SWNs) had poor sleep quality in Portugal, Italy and Iran (De Martino et al., 2013; Giorgi et al., 2018; Jafari Roodbandi et al., 2015). It showed that 57%–82.33% of nurses working on changing shifts had poor sleep quality in Taiwan, China, similar to that in studies performed abroad (Lee et al., 2015; Lin et al., 2014). Nurses' physical and mental health, job performance and patient safety were closely related to sleep quality. Studies have shown that nurses with poor sleep quality are highly susceptible to psychological and physiological problems, such as depression, diabetes and coronary heart disease (Dai et al., 2019; Kecklund & Axelsson, 2016). Some studies have also found that nurses with high sleep quality are more efficient and perform better at work, whereas SWNs with sleep problems are more likely to make medical errors and cause patient safety issues (Park et al., 2018; Sun et al., 2019). In addition, job burnout in nurses was strongly associated with poor sleep quality (Giorgi et al., 2018). Therefore, it is vital to recognize the factors that influence sleep quality among SWNs and to adopt targeted measures to improve their sleep quality.
Various factors could influence nurses' sleep quality, such as fatigue, depression, chronic diseases and changes in lifestyle, among which work stress is one factor that cannot be ignored (Dong et al., 2020; Sun et al., 2019). With heavy occupational stress, high conscientiousness and high risk, nurses constantly encounter diseases, traumas and even deaths, so they often face higher work stress (Han et al., 2016). Compared to nurses working in fixed shifts, SWNs are prone to experience work stress (Lin et al., 2015). A long‐term high level of work stress can easily bring about adverse psychological problems such as emotional exhaustion and depression, which will result in sleep disturbance (Kikuchi et al., 2014; Lin et al., 2015). Cross‐sectional studies have found that less work stress was very good for sleep quality in SWNs (Dong et al., 2020; Jafari Roodbandi et al., 2015). A meta‐analysis also pointed out that increased work stress may be a possible cause of increased prevalence of sleep disturbances (Qiu et al., 2020).
Circadian rhythm disruption is also a factor affecting sleep quality (Chaiard et al., 2019; Giorgi et al., 2018; Jafari Roodbandi et al., 2015). Circadian rhythm (CR) refers to periodic changes in human biological and physiological processes over approximately 24 hr that are controlled by the internal clock (Haffen, 2009). The nature of the nursing profession requires nurses to keep 24‐hr shift work and even keep an all‐night vigil sometimes (Dong et al., 2017). This working mode increases the risk of CR disruption among SWNs (Potter et al., 2016). Additionally, long‐term or frequent stress can also lead to CR disruption (Phan & Malkani, 2018). CR disruption has a series of negative effects on individuals, such as job dissatisfaction, absenteeism and sleep disturbance (Bagheri Hosseinabadi et al., 2019; Jafari Roodbandi et al., 2015; Zare et al., 2017). However, individuals with better CR regulation are less likely to develop CR disruption, which in turn leads to fewer negative outcomes. Studies by Folkard and Di Milia et al. found that flexible individuals with high CR stability were better able to eat or sleep at unusual times, and vigorous people with low CR amplitude were better able to cope with insomnia and drowsiness to keep feeling energetic. In general, flexible and vigorous types of people did better in regulating CR and experienced fewer negative effects (Di Milia et al., 2004; Folkard et al., 1979).
As an external factor induced by the nurse's role, work stress cannot be changed in the short term, and thus, it is difficult to improve sleep quality by improving work stress (Keykaleh et al., 2018). Therefore, identification of mediating factors that alleviate the influence of work stress on sleep quality could be an effective strategy for sleep management. According to the above literature, high work stress will lead to CR disruption and poor sleep quality, and CR disruption will also lead to poor sleep quality. Hence, it can be deduced that CR may be a mediator between work stress and sleep quality. This study aimed to (1) determine the level of work stress, CR, and sleep quality of SWNs; (2) identify the relationships between work stress, CR and sleep quality; and (3) verify the mediating effect of CR between work stress and sleep quality. The study will offer some scientific evidence for formulating intervention strategies to improve sleep quality in SWNs.
2. METHODS
2.1. Study design
The study was a cross‐sectional investigation.
2.2. Sample and data collection
Nurses who work in shifts at six hospitals in Shanghai, China, from October 2019–December 2019 were recruited by convenience sampling. Inclusion criteria included: (a) registered and active nurse; (b) working in rotating shifts—a rotating shift referred to work that are not performed between approximately 8:00 to 18:00 as well as rotation between the day shift (from 8:00–16:00), evening shift (from 16:00–24:00 or from 14:00–22:00) and night shift (from 0:00–8: 00) (Lin et al., 2015); and (c) informed consent was signed voluntarily. Exclusion criteria were as follows: (a) presence of psychological disorder, such as depression and anxiety; (b) taking medication that affects sleep; and (c) being pregnant.
A questionnaire was distributed through the online platform SurveyStar (https://www.wjx.cn/). The questionnaire included the following four parts: the purpose and content of the study, an informed consent form, instructions for completing the questionnaire and formal survey content. The detailed steps are as follows. First, with the help of the heads of the nursing department of each hospital, the questionnaire link was distributed to the WeChat group of each department. The person in charge of the department selected the nurses that meet the research requirements and explained the research content and purpose to them. After obtaining informed consent, the selected nurses completed the questionnaire survey independently. Above steps ensure that every participant in our study had informed consent and participated voluntarily. The rule of thumb for sample size was that 10 samples were required per observable variable (Kim & Kim, 2019). The final structural equation model included 22 observed variables. Considering an invalid sample size of 20%, this study required a minimum of 275 samples. The STROBE checklist for cross‐sectional studies was used for reporting this study.
2.3. Measures
2.3.1. Demographic survey form
The contents mainly included the basic information of the participants, such as gender, age, marital status, education, department, professional title and monthly income.
2.3.2. Sleep quality
The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate sleep quality in the last month (Buysse et al., 1989). There are 19 self‐report items in the PSQI, but the last item is not included in the scoring. The 18 self‐report items measure seven factors, and each factor is scored from 0–3. In all cases, a score of “0”indicates no difficulty, while a score of “3”indicates severe difficulty. The cumulative score of each factor is the global score, which ranged from 0–21. The higher the score was, the worse the sleep quality was, and it takes approximately 10 min for patients to complete the questionnaire. Poor sleepers were identified based on a global score of >5. This study utilized a Chinese translation by Liu with the value of Cronbach's alpha was 0.842 and 0.731 in our study (Liu et al., 1996). Notably, the sixth component of the PSQI (use of sleep medication) was assigned a value of 0 and was not included in the structural equation model because the use of medication was excluded from the study.
2.3.3. Work stress
The Chinese Nurses Stressor Scale (CNSS), compiled by Li and Liu (2000) based on China's national conditions, was used to investigate work stress in the study. The CNSS includes the following 35 items and 5 dimensions: (a) nursing specialty and nursing work, (b) time distribution and work quantity, (c) work environment and equipment, (d) nursing care of patients, and (e) management and interpersonal relations. Cronbach's alpha of the scale and five subscales was between 0.80–0.94 in the previous study (Yu, 2007). The responses are from 1 = never to 4 = almost every day. The scale scores from 35–140 points, with 35 to 70 indicating mild stress, 71 to 105 indicating moderate stress and 106 to 140 indicating severe stress. In the present study, the Cronbach's alpha was higher than 0.85 for both the scale and the subscales.
2.3.4. Circadian rhythm
The stability and amplitude of CR were measured by the Circadian Type Inventory (CTI). CTI was originally designed by Folkard et al. (1979) to determine whether an individual could adapt to shift work, and then, it was revised by Di Milia et al. (2004) to an 11‐item scale. The latest version of CTI has 11 items in the following two dimensions: stability and amplitude. In the inventory, the stability is represented by flexible and rigid (FR), as well as the amplitude is languid and vigorous (LV). The Cronbach's alpha was 0.72 for LV and 0.79 for FR, which proves that CTI is reliable similar to other scales used in this study. The responses are from 1 = almost never to 5 = almost always. Nurses with a score of over 18.75 on the stability dimension are considered flexible workers, and nurses with a score of over 22.5 on the amplitude dimension are considered languid workers (Di Milia et al., 2005). Following the revised Brislin translation model, a Chinese version of 11‐item CTI were developed with the consent of the original author before the investigation, which showed good reliability and validity among Chinese medical students. Cronbach's alpha of Chinese version of 11‐item CTI was 0.654 for LV and 0.817 for FR. It showed a good model fit—chi‐square/degrees of freedom ratio (χ 2/df) = 1.833, root‐mean‐square error of approximation (RMSEA) = 0.061, standardized root mean square residual (SRMR) = 0.063, comparative fit index (CFI) = 0.955, goodness‐of‐fit (GFI) = 0.940, adjusted goodness‐of‐fit index (AGFI) = 0.908 and incremental fit index (IFI) = 0.956 in the confirmatory factor analysis. In the present study, Cronbach's alpha was 0.759 (LV) and 0.834 (FR).
2.4. Data analysis
Two researchers checked the returned questionnaires separately and excluded invalid questionnaires before proceeding to the subsequent analysis. The elimination criteria for the questionnaires were as follows: (a) missing answers or filling in the questionnaire randomly; (b) the answers to the questions before and after are contradictory; and (c) the choice of answers shows obvious repetition.
SPSS (version 24) and AMOS Graphics (version 24) (IBM Corp., Armonk, NY, USA) were used to analyse the obtained data. The data were described using mean (M) and standard deviation (SD), and enumeration data were measured using frequency and percentage. The Pearson correlation coefficient was used to analyse the correlations between the studied variables. The structural equation model was adopted to test the intermediate role of the CR between work stress and sleep quality. Considering that indirect effects do not meet the normal distribution conditions, we used AMOS to run a 5,000‐bootstrapping sample. The bias‐corrected (BC) percentile Bootstrap method provided a 95% CI. If the CI did not contain zero, it was considered to be significant (MacKinnon et al., 2002). Moreover, we used goodness‐of‐fit indexes (1 < χ 2/df < 3, AGFI > 0.90, CFI > 0.90, GFI > 0.90, IFI > 0.90, RMSEA < 0.08, SRMR < 0.08, Tucker‐Lewis index (TLI) > 0.90 and Hoelter's critical N (CN) > 200) to confirm the fit of the model (Hu & Bentler, 1998). The value of 0.05 was considered statistically significant.
2.5. Ethics
This study received the approval of the Ethics Committee of the Second Rehabilitation Hospital of Shanghai, China (Approval No. 201903). The purpose and content of the study were provided on the first page of the questionnaire to ensure that everyone who filled in the questionnaire was aware of the purpose and possible risks of the study. All the study participants signed an electronic version of informed consent. The information is kept confidential, and only the research team have access to it.
3. RESULTS
3.1. General characteristics
In total, 423 shift‐working nurses filled out the questionnaires. According to the criteria for excluding questionnaires, 379 (89.6%) questionnaires entered the statistical analysis process. The mean age and length of service of the SWNs were 29.64 (SD = 5.49) years and 8.04 (SD = 6.13) years, respectively. This study showed a higher percentage of female nurses (N = 363, 95.78%), nurses who were married (N = 211, 55.67%), worked in a traditional Chinese medicine hospital (N = 240, 63.32%) and department of internal medicine (N = 141, 37.20%) and surgery (N = 84, 22.16%), and had night shifts (N = 330, 87.07%) (Table 1).
TABLE 1.
General characteristics of participants (N = 379)
| Characteristics | Categories | N | % |
|---|---|---|---|
| Gender | Female | 363 | 95.78 |
| Male | 16 | 4.22 | |
| Education | Junior college degree and below | 153 | 40.37 |
| Bachelor's degree and above | 226 | 59.63 | |
| Marital status | Unmarried | 165 | 43.54 |
| Married | 211 | 55.67 | |
| Divorced | 3 | 0.79 | |
| Has children | Yes | 167 | 44.06 |
| No | 212 | 55.94 | |
| Hospital type | Traditional Chinese medicine hospital a | 240 | 63.32 |
| General hospital | 139 | 36.68 | |
| Working department | Internal medicine | 141 | 37.20 |
| Surgery | 84 | 22.16 | |
| Obstetrics and gynaecology | 13 | 3.43 | |
| Paediatrics | 18 | 4.75 | |
| Emergency | 47 | 12.40 | |
| Intensive care unit | 38 | 10.03 | |
| Others | 38 | 10.03 | |
| Professional title | Nurse | 157 | 41.42 |
| Nurse practitioner | 180 | 47.49 | |
| Nurse‐in‐charge | 42 | 11.08 | |
| Monthly income (RMB) | <8,000 | 211 | 55.67 |
| ≥8,000 | 168 | 44.33 | |
| Having night shift | Yes | 330 | 87.07 |
| No | 49 | 12.93 | |
| Taking a nap | Yes | 76 | 20.05 |
| No | 303 | 79.95 | |
| Circadian rhythm amplitude (LV) | Languid | 181 | 47.76 |
| Vigorous | 198 | 52.24 | |
| Circadian rhythm stability (FR) | Flexible | 26 | 6.86 |
| Rigid | 353 | 93.14 | |
|
Work stress |
Mild stress | 28 | 7.39 |
| Moderate stress | 275 | 72.56 | |
| Severe stress | 76 | 20.05 |
Hospitals that have Traditional Chinese medicine (TCM) characteristics and can provide TCM services.
3.2. Work stress, circadian rhythm and sleep quality of participants
Descriptive statistics for the participants' work stress, CR and sleep quality are displayed in Table 2. Among the 379 SWNs, 28 cases (7.39%) had mild stress, 275 (72.56%) cases had moderate stress, and 76 cases (20.05%) had severe stress (Table 1). Among the subscales of the CNSS, time distribution and work quantity (M = 3.07, SD = 0.64) and nursing specialty and nursing work (M = 2.84, SD = 0.53) scored higher. In terms of CR, the mean score for LV and FR was 22.09 (SD = 3.94) and 12.49 (SD = 3.97), respectively. For LV, 198 cases (52.24%) were of the vigorous type; for FR, 26 cases (6.86%) were of the flexible type (Table 1). The participating SWNs scored 6.80 for sleep quality (SD = 3.16). A total of 143 (37.73%) SWNs had good sleep quality (PSQI < 5). Among the subscales of the PSQI, daytime dysfunction scored the highest (M = 1.85, SD = 0.90).
TABLE 2.
Work stress, circadian rhythm and sleep quality of participants
| Variables | Score range | M | SD |
|---|---|---|---|
| Sleep quality | 0–15 | 6.75 | 3.12 |
| Daytime dysfunction | 0–3 | 1.85 | .90 |
| Sleep latency | 0–3 | 1.40 | .92 |
| Sleep disturbance | 0–3 | 1.29 | .72 |
| Subjective sleep quality | 0–3 | 1.28 | .67 |
| Sleep duration | 0–3 | 0.56 | .67 |
| Habitual sleep efficiency | 0–3 | 0.37 | .75 |
| Use of sleep medication | 0 | 0.00 | .00 |
| Work stress | 35–140 | 94.36 | 17.66 |
| Time distribution and work quantity (TDWQ) | 1–4 | 3.07 | .64 |
| Nursing specialty and nursing work (NSNW) | 1–4 | 2.84 | 0.53 |
| Nursing care of patients (NCP) | 1–4 | 2.79 | .55 |
| Work environment and equipment (WEE) | 1–4 | 2.60 | .71 |
| Management and interpersonal relations (MIR) | 1–4 | 2.30 | .65 |
| Circadian rhythm | 17–55 | 34.57 | 4.83 |
| Circadian rhythm amplitude (LV) | 11–30 | 22.09 | 3.94 |
| Circadian rhythm stability (FR) | 5–25 | 12.49 | 3.97 |
Abbreviations: M, mean; SD, standard deviation.
3.3. Correlational analysis of variables
Significant correlations were found between work stress, sleep quality, LV and FR. Table 3 presents the Pearson correlation coefficients for our research variables.
TABLE 3.
Correlational analysis of variables
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Sleep quality | 1 | |||
| Work stress | 0.398* | 1 | ||
| Circadian rhythm amplitude (LV) | 0.359* | 0.302* | 1 | |
| Circadian rhythm stability (FR) | −0.284* | −0.311* | −0.257* | 1 |
p < .01.
3.4. The mediating role of LV and FR
As depicted in Figure 1, work stress, LV, FR and sleep quality were presented as latent variables in the mediation model. The result demonstrated a good fit (χ 2/df = 2.008, RMSEA = 0.052, SRMR = 0.057, GFI = 0.908, AGFI = 0.886, TLI = 0.927, CFI = 0.935, IFI = 0.936 and CN = 220). Table 4 presents the overall, direct and indirect effects of work stress on sleep quality. Work stress positively predicted sleep quality (0.375, 95% CI [0.193, 0.552]). In addition, work stress indirectly affected sleep quality through mediation of FR and LV, with mediating values of 0.075 (95% CI [0.013, 0.158]) and 0.142 (95% CI [0.071, 0.244]), respectively. No difference was found between the indirect effects of FR and LV (95% CI [−0.189, 0.045]). The overall effect of work stress on sleep quality was 0.592 (95% CI [0.441, 0.747]), and the overall indirect effects accounted for 36.7% (0.217/0.592*100%).
FIGURE 1.
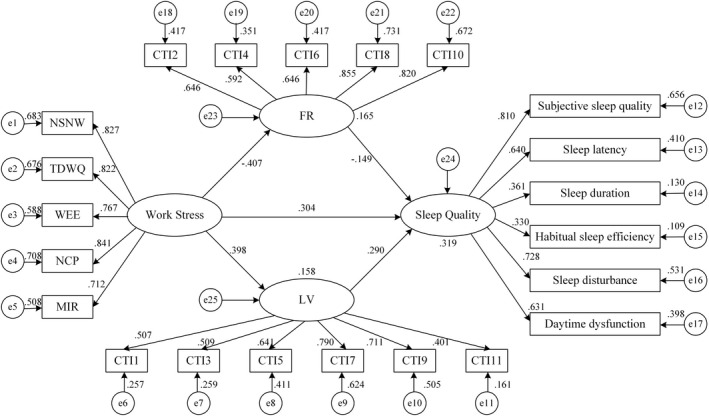
Mediation model of circadian rhythm stability and amplitude. CTI, circadian type inventory; e, residual error; MIR, management and interpersonal relations; NCP, nursing care of patients; NSNW, nursing specialty and nursing work; TDWQ, time distribution and work quantity; WEE, work environment and equipment;
TABLE 4.
Total, direct and indirect effects of the pathway model
| Effects | Product of coefficients | Bootstrapping 95% BC confidence interval | |||
|---|---|---|---|---|---|
| Estimated effect | SE | Z | Lower | Upper | |
| Indirect effect 1: FR as mediator | 0.075 | 0.036 | 2.083* | 0.013 | 0.158 |
| Indirect effect 2: LV as mediator | 0.142 | 0.044 | 3.227* | 0.071 | 0.244 |
| Total indirect effects: FR + LV | 0.217 | 0.054 | 4.019* | 0.124 | 0.337 |
| Difference in indirect effects: FR−LV | −0.068 | 0.060 | −1.133 | −0.189 | 0.045 |
| Direct effects | 0.375 | 0.091 | 4.121* | 0.193 | 0.552 |
| Total effects | 0.592 | 0.076 | 7.789* | 0.441 | 0.747 |
Note: Bias‐corrected bootstrap samples, 5,000.
Abbreviations: BC, bias‐corrected; FR, circadian rhythm stability; LV, circadian rhythm amplitude; SE, standard error; Z, z‐value.
p < .05.
4. DISCUSSIONS
This study explored the mediating effect of CR between SWNs' work stress and sleep quality. The results revealed that work stress was positively related to PSQI, meaning it negatively affected sleep quality. Moreover, the amplitude (LV) and stability (FR) of CR were mediators in the relationship.
4.1. Analysis of work stress, circadian rhythm and sleep quality among SWNs
The present study showed that over 90% SWNs had moderate or higher work stress, higher than that in Yang's study performed in Wuhan city (Yang et al., 2019). Studies found the prevalence of work stress was 78.4% in Iran (Kakemam et al., 2019) and 41.2% in Australia (Maharaj et al., 2018) based on different measuring tools, which was also lower than our finding. In our study, the primary sources of work stress for nurses were found to be time distribution and work quantity and nursing specialty and nursing work, similar to the findings in other studies (Liu & Aungsuroch, 2019). These findings reflect the nurses are sensitive to work stress due to high workload, long work hours and high work requirements (Chen et al., 2020; Liu et al., 2021; Liu & Aungsuroch, 2019). Therefore, nursing managers should take targeted measures to tackle different sources of work stress, effectively arrange the work and create a pleasant working environment for nurses so as to improve their work quality and efficiency and reduce their work stress.
In this study, the proportions of SWNs rated as flexible and vigorous types were 6.86% and 52.24%, respectively. These proportions were lower than those in previous research in Iran (Bagheri Hosseinabadi et al., 2019; Jafari Roodbandi et al., 2015). The low proportions of flexible and vigorous types of SWNs might partly reflect the unreasonable arrangement of shift work in China. As pointed out in Rosa's study, shift work might cause adverse consequences to both nurses' health and nursing work (Rosa et al., 2019). Due to the nature of nursing work and the adverse effect of working in shift, attention should be paid to SWNs' CR, and shift work should be arranged reasonably and effectively according to the type of nurse.
In this study, 62.27% SWNs had poor sleep quality (PSQI > 5), consistent with that in Giorgi et al.'s (2018) and Jafari Roodbandi et al.'s (2015) studies. Notably, a meta‐analysis revealed that 39.2% Chinese healthcare professionals had poor sleep quality (Qiu et al., 2020), which was far lower than our result. Shift work nurses were prone to having poorer sleep quality than nurses in regular shifts. Therefore, the sleep quality of SWNs is worthy of concern.
Compared to standard day work, shift work has been shown to impact on a range of health and safety outcomes, including an increased risk of stress, sleep disturbance, fatigue and chronic diseases (Di Muzio et al., 2020; Ganesan et al., 2019; Rosa et al., 2019). CR disruption is a central feature of shift work, and sleep disturbance is a prevailing health‐related problem caused by shift work (Vogel et al., 2012). Studies have shown that shift nurses are able to recover from shift work after a certain period of rest (Merkus et al., 2015). However, research has failed to determine the amount of recovery needed because the duration of work is an important factor in determining the amount of recovery, that is, longer working hours are attributed to the need for longer recovery time (Ropponen et al., 2018; Wong et al., 2019). In addition, although there will be temporary recovery after rest, to provide patients with 24‐hr care, shift work is inevitable and needs to be maintained for a long time, which will inevitably lead to alterations in SWN's work stress, CR and sleep quality. Similar to previous studies, our study showed that SWNs experienced high work stress and poor sleep quality. Current studies reported the status and effects of work stress, CR disturbance and poor sleep quality in SWNs, but few have explored the relationship among them (Boivin & Boudreau, 2014; Rosa et al., 2019; Vogel et al., 2012). Therefore, to better improve SWNs' sleep quality as well as provide high‐quality nursing for patients, it is necessary to study the relationship between work stress, CR and sleep quality.
4.2. Correlations between work stress, circadian rhythm and sleep quality
As shown by our data, sleep quality was significantly associated with work stress, which was in accordance with earlier findings. Kunzweiler et al. (2016) found that work‐related stress and stress due to irregularly distributed workload significantly affected sleep quality. Studies by Jafari Roodbandi et al. (2015) and Gu et al. (2019) also confirmed that high stress lead to poor sleep quality. As an essential source of stress, work stress acts on the body through factors such as stress response. Such a response can be short‐lived or long‐term (Moreno‐Smith et al., 2010). Frequent or chronic episodes of work stress cause repeated activation of the sympathetic nervous system and adrenal‐cortical system and release various hormones into the body, which may cause sleep disturbances (Roberts & Grubb, 2014). In this study, work stress among SWNs was mainly caused by the nature of nursing work, which is hard to change, and thus, it is difficult to improve work stress. Overall, work stress could directly affect sleep quality. However, considering that a nurse's working environment is difficult to change and a nurse's ability to regulate stress is limited, it is more important to explore the indirect factors that have an effect between work stress and sleep quality.
The study promisingly revealed that greater CR stability and lower CR amplitude were significantly associated with better sleep quality. Shift work nurses who were of the flexible type had better sleep quality in our study, which was congruent with the finding in Jafari Roodbandi et al.'s (2015) study. One possible explanation for the association was that rigid individuals resisted sudden changes in their internal rhythm (like working in a night shift), thereby decreasing their sleep quality (Folkard et al., 1979). Besides, Natvik et al. (2011) found that rigidity was associated with insomnia among shift workers. These findings also revealed that languid SWNs had poor sleep quality, which was inconsistent with Jafari Roodbandi et al.'s (2015) results suggesting that CR amplitude was not related to sleep quality. However, languid people experienced more sleepiness in previous studies(Natvik et al., 2011). The findings could be explained by Di Milia et al.'s (2004) study, which stated that it was more difficult for languid people to overcome sleepiness and lethargy caused by insufficient sleep. In our study, individuals with strong CR ability (flexible and vigorous type) had better sleep quality and were found to be suitable for shift work, in accordance with Di Milia et al.'s (2004) results.
Nurses are one of the largest groups of shift workers. Nurses worldwide must work shift work schedules to provide nursing services around the clock (Shan et al., 2018). There was increasing evidence that shift work could disturb SWNs' sleep or decrease their sleep duration, which had substantial effects on SWNs' job performance, quality of care and patient safety (Wright et al., 2013). Sleep disturbance in SWNs has received widespread attention due to its high prevalence and negative consequences. Studies have proposed several valuable recommendations, such as ensuring sleep hours and a balanced diet at the individual level, as well as establishing a flexible rotating work schedule, and providing a suitable working environment at the management/institutional level (Sun et al., 2019). It has long been known that human circadian rhythms exhibit individual differences in terms of the rhythms' amplitude and stability, which helps to predict how well the nurses tolerate working in shifts to a certain extent (Natvik et al., 2011; Saksvik‐Lehouillier et al., 2012). However, insufficient attention has been given to this area of study (Tahghighi et al., 2017). In our study, sleep quality was not only significantly associated with work stress but also with CR in SWNs, suggesting that nursing managers can provide new ideas for improving sleep quality by explore CR's relationship with work stress and sleep quality.
4.3. Mediating role of LV and FR on work stress and sleep quality
Most importantly, the present study showed that CR amplitude and stability played an intermediate role between work stress and sleep quality in SWNs. Work stress could directly affect SWNs' sleep quality and indirectly affect sleep quality through the CR. SWNs under long‐term stress were more likely to frequently undergo activation of the hypothalamic–pituitary–adrenal axis, which overrode the CR control and disrupted the CR (Phan & Malkani, 2018). However, strong CR in SWNs could reduce the negative impact of work stress, thereby ensuring their sleep quality. The mediating effect of CR implied that intervention programs for CR might improve the sleep quality of SWNs. Therefore, it is advisable for nursing managers to focus on the intermediate role of CR and reduce the impact of work stress on sleep quality by changing the CR of SWNs to provide better care for patients. Measures that can change CR include using bright lights during night shift to suppress the release of melatonin or, if already released, by depleting it to affect CR positively and raising consciousness among nurses(Lok et al., 2019; Sun et al., 2019); melatonin treatment(Zisapel, 2018); napping during a shift (McKenna & Wilkes, 2018); optimization of shift rotations (transferring nurses who cannot deal with shift work to day work(Zare et al., 2017); establishing reasonable and flexible shift scheduling by considering the characteristics of the shift system, such as the length of shifts, the direction and speed of shift rotation, and the length of the recovery period in between two consecutive shifts, etc.(Alfonsi et al., 2021; Di Muzio et al., 2021; Sun et al., 2019)).
4.4. Limitations
This study has some limitations. First, the study could not provide evidence for a cause‐effect relationship between work stress, CR and sleep quality, because it was a cross‐sectional investigation. Second, this study adopted the convenient sampling method, which resulted in limited generalizability of the results. Random sampling research is recommended in future similar studies. Furthermore, only self‐report measures were used in this study, which could produce bias. Multiple methods should be adopted to assess sleep quality in the future. Lastly, the variables that could also SWNs' sleep quality, such as health burden or the use of stimulants, generally understood lifestyle, were not studied, which should be further analysed whether they affect the results in the study.
5. CONCLUSIONS
Poor sleep quality is very common and worthy of concern among SWNs. Our results indicated that work stress was negatively associated with sleep quality, and this relationship was mediated by the CR. The mediating effect of the CR on work stress and sleep quality offers new insights to improve sleep quality, not only by lightening the work stress but also by improving SWNs' CR.
AUTHOR CONTRIBUTIONS
Caiqin Wu: Research design, project administration, funding acquisition, manuscript revision. Songqi Wu: Investigation, data analysis, manuscript writing. Xiaohan Wang: Investigation, manuscript writing. Wenling Fei: Investigation, manuscript writing. Yue Fu: Investigation, manuscript writing.
All authors have agreed on the final version and meet at least one of the following criteria [recommended bythe ICMJE (http://www.icmje.org/recommendations/)]:
• substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
• drafting the article or revising it critically for important intellectual content.
FUNDING INFORMATION
The study was supported by the Xinglin Young Talent Program of Shanghai University of Traditional Chinese Medicine (to Caiqin Wu) and the 12th Innovative activities of college students of Shanghai Traditional Chinese Medicine (2019SHUTCM094).
Wu, S. , Wu, C. , Wang, X. , Fei, W. , & Fu, Y. (2023). Mediating effect of circadian rhythm between work stress and sleep quality in Chinese shift‐working nurses: A cross‐sectional survey. Nursing Open, 10, 560–569. 10.1002/nop2.1322
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Alfonsi, V. , Scarpelli, S. , Gorgoni, M. , Pazzaglia, M. , Giannini, A. M. , & De Gennaro, L. (2021). Sleep‐related problems in night shift nurses: Towards an individualized interventional practice. Frontiers in Human Neuroscience, 15, 644570. 10.3389/fnhum.2021.644570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagheri Hosseinabadi, M. , Ebrahimi, M. H. , Khanjani, N. , Biganeh, J. , Mohammadi, S. , & Abdolahfard, M. (2019). The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. Journal of Clinical Nursing, 28(9–10), 1868–1878. 10.1111/jocn.14778 [DOI] [PubMed] [Google Scholar]
- Boivin, D. B. , & Boudreau, P. (2014). Impacts of shift work on sleep and circadian rhythms. Pathologie‐Biologie, 62(5), 292–301. 10.1016/j.patbio.2014.08.001 [DOI] [PubMed] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F., 3rd , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Chaiard, J. , Deeluea, J. , Suksatit, B. , Songkham, W. , Inta, N. , & Stone, T. E. (2019). Sleep disturbances and related factors among nurses. Nursing & Health Sciences, 21(4), 470–478. 10.1111/nhs.12626 [DOI] [PubMed] [Google Scholar]
- Chen, J. , Li, J. , Cao, B. , Wang, F. , Luo, L. , & Xu, J. (2020). Mediating effects of self‐efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. Journal of Advanced Nursing, 76(1), 163–173. 10.1111/jan.14208 [DOI] [PubMed] [Google Scholar]
- Dai, C. , Qiu, H. , Huang, Q. , Hu, P. , Hong, X. , Tu, J. , Xie, Q. , Li, H. , Ren, W. , Ni, S. , & Chen, F. (2019). The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatric Disease and Treatment, 15, 435–440. 10.2147/NDT.S190689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Martino, M. M. , Abreu, A. C. , Barbosa, M. F. , & Teixeira, J. E. (2013). The relationship between shift work and sleep patterns in nurses. Ciencia & Saude Coletiva, 18(3), 763–768. 10.1590/s1413-81232013000300022 [DOI] [PubMed] [Google Scholar]
- Di Milia, L. , Smith, P. A. , & Folkard, S. (2004). Refining the psychometric properties of the circadian type inventory. Personality and Individual Differences, 36(8), 1953–1964. 10.1016/j.paid.2003.08.003 [DOI] [Google Scholar]
- Di Milia, L. , Smith, P. A. , & Folkard, S. (2005). A validation of the revised circadian type inventory in a working sample. Personality and Individual Differences, 39(7), 1293–1305. 10.1016/j.paid.2005.04.012 [DOI] [Google Scholar]
- Di Muzio, M. , Diella, G. , Di Simone, E. , Novelli, L. , Alfonsi, V. , Scarpelli, S. , Annarumma, L. , Salfi, F. , Pazzaglia, M. , Giannini, A. M. , & De Gennaro, L. (2020). Nurses and night shifts: Poor sleep quality exacerbates psychomotor performance. Frontiers in Neuroscience, 14, 579938. 10.3389/fnins.2020.579938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Muzio, M. , Diella, G. , Di Simone, E. , Pazzaglia, M. , Alfonsi, V. , Novelli, L. , Cianciulli, A. , Scarpelli, S. , Gorgoni, M. , Giannini, A. , Ferrara, M. , Lucidi, F. , & De Gennaro, L. (2021). Comparison of sleep and attention metrics among nurses working shifts on a forward‐ vs backward‐rotating schedule. JAMA Network Open, 4(10), e2129906. 10.1001/jamanetworkopen.2021.29906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, H. , Zhang, Q. , Sun, Z. , Sang, F. , & Xu, Y. (2017). Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry, 17(1), 241. 10.1186/s12888-017-1402-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong, H. , Zhang, Q. , Zhu, C. , & Lv, Q. (2020). Sleep quality of nurses in the emergency department of public hospitals in China and its influencing factors: A cross‐sectional study. Health and Quality of Life Outcomes, 18(1), 116. 10.1186/s12955-020-01374-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkard, S. , Monk, T. H. , & Lobban, M. C. (1979). Towards a predictive test of adjustment to shift work. Ergonomics, 22(1), 79–91. 10.1080/00140137908924591 [DOI] [PubMed] [Google Scholar]
- Ganesan, S. , Magee, M. , Stone, J. E. , Mulhall, M. D. , Collins, A. , Howard, M. E. , Lockley, S. W. , Rajaratnam, S. , & Sletten, T. L. (2019). The impact of shift work on sleep, alertness and performance in healthcare workers. Scientific Reports, 9(1), 4635. 10.1038/s41598-019-40914-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi, F. , Mattei, A. , Notarnicola, I. , Petrucci, C. , & Lancia, L. (2018). Can sleep quality and burnout affect the job performance of shift‐work nurses? A hospital cross‐sectional study. Journal of Advanced Nursing, 74(3), 698–708. 10.1111/jan.13484 [DOI] [PubMed] [Google Scholar]
- Gu, B. , Tan, Q. , & Zhao, S. (2019). The association between occupational stress and psychosomatic wellbeing among Chinese nurses: A cross‐sectional survey. Medicine, 98(22), e15836. 10.1097/MD.0000000000015836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffen, E. (2009). Mesure des rythmes circadiens [measuring circadian rhythm]. L'Encephale, 35(Suppl 2), S63–S67. 10.1016/S0013-7006(09)75536-8 [DOI] [PubMed] [Google Scholar]
- Han, Y. , Yuan, Y. , Zhang, L. , & Fu, Y. (2016). Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatria Danubina, 28(2), 176–183. [PubMed] [Google Scholar]
- Hu, L. T. , & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453. 10.1037/1082-989x.3.4.424 [DOI] [Google Scholar]
- Jafari Roodbandi, A. , Choobineh, A. , & Daneshvar, S. (2015). Relationship between circadian rhythm amplitude and stability with sleep quality and sleepiness among shift nurses and health care workers. International Journal of Occupational Safety and Ergonomics: JOSE, 21(3), 312–317. 10.1080/10803548.2015.1081770 [DOI] [PubMed] [Google Scholar]
- Kakemam, E. , Raeissi, P. , Raoofi, S. , Soltani, A. , Sokhanvar, M. , Visentin, D. , & Cleary, M. (2019). Occupational stress and associated risk factors among nurses: A cross‐sectional study. Contemporary Nurse, 55(2–3), 237–249. 10.1080/10376178.2019.1647791 [DOI] [PubMed] [Google Scholar]
- Kecklund, G. , & Axelsson, J. (2016). Health consequences of shift work and insufficient sleep. BMJ (Clinical Research ed.), 355, i5210. 10.1136/bmj.i5210 [DOI] [PubMed] [Google Scholar]
- Keykaleh, M. S. , Safarpour, H. , Yousefian, S. , Faghisolouk, F. , Mohammadi, E. , & Ghomian, Z. (2018). The relationship between Nurse's job stress and patient safety. Open Access Macedonian Journal of Medical Sciences, 6(11), 2228–2232. 10.3889/oamjms.2018.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi, Y. , Nakaya, M. , Ikeda, M. , Okuzumi, S. , Takeda, M. , & Nishi, M. (2014). Relationship between job stress, temperament and depressive symptoms in female nurses. International Journal of Occupational Medicine and Environmental Health, 27(3), 426–434. 10.2478/s13382-014-0270-z [DOI] [PubMed] [Google Scholar]
- Kim, H. , & Kim, K. (2019). Impact of self‐efficacy on the self‐leadership of nursing preceptors: The mediating effect of job embeddedness. Journal of Nursing Management, 27(8), 1756–1763. 10.1111/jonm.12870 [DOI] [PubMed] [Google Scholar]
- Kunzweiler, K. , Voigt, K. , Kugler, J. , Hirsch, K. , Bergmann, A. , & Riemenschneider, H. (2016). Factors influencing sleep quality among nursing staff: Results of a cross sectional study. Applied Nursing Research: ANR, 32, 241–244. 10.1016/j.apnr.2016.08.007 [DOI] [PubMed] [Google Scholar]
- Lee, C. Y. , Chen, H. C. , Meg Tseng, M. C. , Lee, H. C. , & Huang, L. H. (2015). The relationships among sleep quality and chronotype, emotional disturbance, and insomnia vulnerability in shift nurses. The Journal of Nursing Research: JNR, 23(3), 225–235. 10.1097/jnr.0000000000000095 [DOI] [PubMed] [Google Scholar]
- Li, X. , & Liu, Y. (2000). Job stressors and burnout among staff nurses. Chinese Journal of Nursing, 35(11), 4–8. [Google Scholar]
- Lin, P. C. , Chen, C. H. , Pan, S. M. , Chen, Y. M. , Pan, C. H. , Hung, H. C. , & Wu, M. T. (2015). The association between rotating shift work and increased occupational stress in nurses. Journal of Occupational Health, 57(4), 307–315. 10.1539/joh.13-0284-OA [DOI] [PubMed] [Google Scholar]
- Lin, S. H. , Liao, W. C. , Chen, M. Y. , & Fan, J. Y. (2014). The impact of shift work on nurses' job stress, sleep quality and self‐perceived health status. Journal of Nursing Management, 22(5), 604–612. 10.1111/jonm.12020 [DOI] [PubMed] [Google Scholar]
- Liu, X. , Tang, M. , Hu, L. , Wang, A. , Wu, H. , Zhao, G. , Gao, C. , & Li, W. (1996). Reliability and validity of the Pittsburgh sleep quality index. Chinese Journal of Psychiatry, 29(2), 103–107. [Google Scholar]
- Liu, Y. , & Aungsuroch, Y. (2019). Work stress, perceived social support, self‐efficacy and burnout among Chinese registered nurses. Journal of Nursing Management, 27(7), 1445–1453. 10.1111/jonm.12828 [DOI] [PubMed] [Google Scholar]
- Liu, Y. , Aungsuroch, Y. , Gunawan, J. , & Zeng, D. (2021). Job stress, psychological capital, perceived social support, and occupational burnout among hospital nurses. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 53(4), 511–518. 10.1111/jnu.12642 [DOI] [PubMed] [Google Scholar]
- Lok, R. , van Koningsveld, M. J. , Gordijn, M. , Beersma, D. , & Hut, R. A. (2019). Daytime melatonin and light independently affect human alertness and body temperature. Journal of Pineal Research, 67(1), e12583. 10.1111/jpi.12583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D. P. , Lockwood, C. M. , Hoffman, J. M. , West, S. G. , & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. 10.1037/1082-989x.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj, S. , Lees, T. , & Lal, S. (2018). Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. International Journal of Environmental Research and Public Health, 16(1), 61. 10.3390/ijerph16010061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna, H. , & Wilkes, M. (2018). Optimising sleep for night shifts. BMJ (Clinical Research ed.), 360, j5637. 10.1136/bmj.j5637 [DOI] [PubMed] [Google Scholar]
- Merkus, S. L. , Holte, K. A. , Huysmans, M. A. , van de Ven, P. M. , van Mechelen, W. , & van der Beek, A. J. (2015). Self‐reported recovery from 2‐week 12‐hour shift work schedules: A 14‐day follow‐up. Safety and Health at Work, 6(3), 240–248. 10.1016/j.shaw.2015.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno‐Smith, M. , Lutgendorf, S. K. , & Sood, A. K. (2010). Impact of stress on cancer metastasis. Future Oncology (London, England), 6(12), 1863–1881. 10.2217/fon.10.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natvik, S. , Bjorvatn, B. , Moen, B. E. , Magerøy, N. , Sivertsen, B. , & Pallesen, S. (2011). Personality factors related to shift work tolerance in two‐ and three‐shift workers. Applied Ergonomics, 42(5), 719–724. 10.1016/j.apergo.2010.11.006 [DOI] [PubMed] [Google Scholar]
- Park, E. , Lee, H. Y. , & Park, C. S. (2018). Association between sleep quality and nurse productivity among Korean clinical nurses. Journal of Nursing Management, 26(8), 1051–1058. 10.1111/jonm.12634 [DOI] [PubMed] [Google Scholar]
- Phan, T. X. , & Malkani, R. G. (2018). Sleep and circadian rhythm disruption and stress intersect in Alzheimer's disease. Neurobiology of Stress, 10, 100133. 10.1016/j.ynstr.2018.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter, G. D. , Skene, D. J. , Arendt, J. , Cade, J. E. , Grant, P. J. , & Hardie, L. J. (2016). Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocrine Reviews, 37(6), 584–608. 10.1210/er.2016-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, D. , Yu, Y. , Li, R. Q. , Li, Y. L. , & Xiao, S. Y. (2020). Prevalence of sleep disturbances in Chinese healthcare professionals: A systematic review and meta‐analysis. Sleep Medicine, 67, 258–266. 10.1016/j.sleep.2019.01.047 [DOI] [PubMed] [Google Scholar]
- Roberts, R. K. , & Grubb, P. L. (2014). The consequences of nursing stress and need for integrated solutions. Rehabilitation Nursing: The Official Journal of the Association of Rehabilitation Nurses, 39(2), 62–69. 10.1002/rnj.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ropponen, A. , Härmä, M. , Bergbom, B. , Nätti, J. , & Sallinen, M. (2018). The vicious circle of working hours, sleep, and recovery in expert work. International Journal of Environmental Research and Public Health, 15(7), 1361. 10.3390/ijerph15071361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa, D. , Terzoni, S. , Dellafiore, F. , & Destrebecq, A. (2019). Systematic review of shift work and nurses' health. Occupational medicine (Oxford, England), 69(4), 237–243. 10.1093/occmed/kqz063 [DOI] [PubMed] [Google Scholar]
- Saksvik‐Lehouillier, I. , Bjorvatn, B. , Hetland, H. , Sandal, G. M. , Moen, B. E. , Mageroy, N. , Harvey, A. , Costa, G. , & Pallesen, S. (2012). Personality factors predicting changes in shift work tolerance: A longitudinal study among nurses working rotating shifts. Work and Stress, 26(2), 143–160. 10.1080/02678373.2012.686344 [DOI] [Google Scholar]
- Shan, Z. , Li, Y. , Zong, G. , Guo, Y. , Li, J. , Manson, J. E. , Hu, F. B. , Willett, W. C. , Schernhammer, E. S. , & Bhupathiraju, S. N. (2018). Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: Results from two large US cohorts of female nurses. BMJ (Clinical Research ed.), 363, k4641. 10.1136/bmj.k4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, Q. , Ji, X. , Zhou, W. , & Liu, J. (2019). Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. Journal of Nursing Management, 27(1), 10–18. 10.1111/jonm.12656 [DOI] [PubMed] [Google Scholar]
- Tahghighi, M. , Rees, C. S. , Brown, J. A. , Breen, L. J. , & Hegney, D. (2017). What is the impact of shift work on the psychological functioning and resilience of nurses? An integrative review. Journal of Advanced Nursing, 73(9), 2065–2083. 10.1111/jan.13283 [DOI] [PubMed] [Google Scholar]
- Vogel, M. , Braungardt, T. , Meyer, W. , & Schneider, W. (2012). The effects of shift work on physical and mental health. Journal of Neural Transmission (Vienna, Austria: 1996), 119(10), 1121–1132. 10.1007/s00702-012-0800-4 [DOI] [PubMed] [Google Scholar]
- Wong, K. , Chan, A. , & Ngan, S. C. (2019). The effect of long working hours and overtime on occupational health: A meta‐analysis of evidence from 1998 to 2018. International Journal of Environmental Research and Public Health, 16(12), 2102. 10.3390/ijerph16122102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, K. P., Jr. , Bogan, R. K. , & Wyatt, J. K. (2013). Shift work and the assessment and management of shift work disorder (SWD). Sleep Medicine Reviews, 17(1), 41–54. 10.1016/j.smrv.2012.02.002 [DOI] [PubMed] [Google Scholar]
- Yang, T. , Li, X. , Wang, Y. , Yao, X. , Li, S. , & Yan, H. (2019). Current status and influencing factors of clinical nurses' turnover intention in tertiary grade a hospitals in Wuhan. Chinese Nursing Management, 19(4), 569–574. [Google Scholar]
- Yu, H. (2007). Analysis on reliability and validity of Chinese nurses stressor scale. Chinese Nursing Research, 21(8B), 2090–2093. [Google Scholar]
- Zare, R. , Choobineh, A. , & Keshavarzi, S. (2017). Association of Amplitude and Stability of circadian rhythm, sleep quality, and occupational stress with sickness absence among a gas company employees‐a cross sectional study from Iran. Safety and Health at Work, 8(3), 276–281. 10.1016/j.shaw.2016.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, L. , Sun, D. M. , Li, C. B. , & Tao, M. F. (2016). Influencing factors for sleep quality among shift‐working nurses: A cross‐sectional study in China using 3‐factor Pittsburgh sleep quality index. Asian Nursing Research, 10(4), 277–282. 10.1016/j.anr.2016.09.002 [DOI] [PubMed] [Google Scholar]
- Zisapel, N. (2018). New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British Journal of Pharmacology, 175(16), 3190–3199. 10.1111/bph.14116 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


