Abstract
We present a case of a 61-year-old woman with an atypical non-arteritic anterior ischemic optic neuropathy (NA-AION) as a unique manifestation of COVID-19. Furthermore, the patient worsened after Pfizer-BioNTech COVID-19 vaccine administration. Our findings suggest that NA-AION could result from microangiopathic/thrombotic events that may occur during SARS-CoV-2 infection and/or vaccination against COVID-19. This report sheds light on possible ophthalmologic complications of COVID-19.
Keywords: SARS-CoV-2, optic nerve, vaccine, optical coherence tomography angiography
Introduction
Ischemic optic neuropathy is an acute ischemic disorder of the optic nerve. Ischemic optic neuropathies are categorized into two subtypes: anterior ischemic optic neuropathy (AION) and posterior ischemic optic neuropathy.1
Etiologically, AION can be divided into arteritic AION (A-AION), due to giant cell arteritis (GCA), also known as Horton disease, a systemic inflammatory vasculitis, and non-arteritic AION (NA-AION), usually of multifactorial origin and associated with multiple risk factors, like diabetes mellitus, cardiovascular diseases and obstructive sleep apnea.1 NA-ION is the most common form of ischemic optic neuropathy, characterized by acute, monocular, painless visual loss with optic disc swelling. Its results from hypoperfusion of the short posterior ciliary arteries supplying the optic nerve.1
Coronavirus disease 2019 (COVID-19) pandemic is still raging, and several vaccines for acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are now available.
Few cases of NA-AION have been described in patients with SARS-CoV-2 infection.2,3 However, an association between NA-AION and COVID-19 vaccination has not been reported to date.
We present a case of a 61-year-old woman with an atypical NA-AION as a unique manifestation of COVID-19. The patient worsened after Pfizer-BioNTech COVID-19 vaccine administration.
Case description
On December 21st 2020, a 61-year-old woman experienced severe headache in the periorbital left side followed by a decrease in visual acuity and mydriasis in the left eye. The patient's medical history was unremarkable. Four days after, the patient tested positive for SARS-CoV-2 by nasal and throat swabs, without respiratory symptoms or fever. The patient underwent isolation for COVID-19 until she tested negative for SARS-CoV-2 on 13th January 2021.
On January 27th 2021, the patient sought medical attention due to the persistence of symptoms and was evaluated by an ophthalmologist. Her best-corrected visual acuity was 20/20 for the right eye and 20/25 for the left eye. The intraocular pressure by applanation tonometry was 17 mmHg bilaterally.
Anterior segment examination revealed a left dilated with no reaction to light. Ocular motility examination showed exotropia in the same eye. Otherwise, the neurological examination was unremarkable. There was no temporal tenderness, and temporal artery pulsations were normal.
The fundus examination in the left eye revealed a blurring of the border of the optic disk, while in the right eye was normal.
A magnetic resonance imaging of the brain and orbits with and without contrast was unremarkable.
Several visual fields (VF) were performed with good reliability indices in VF from both eyes.
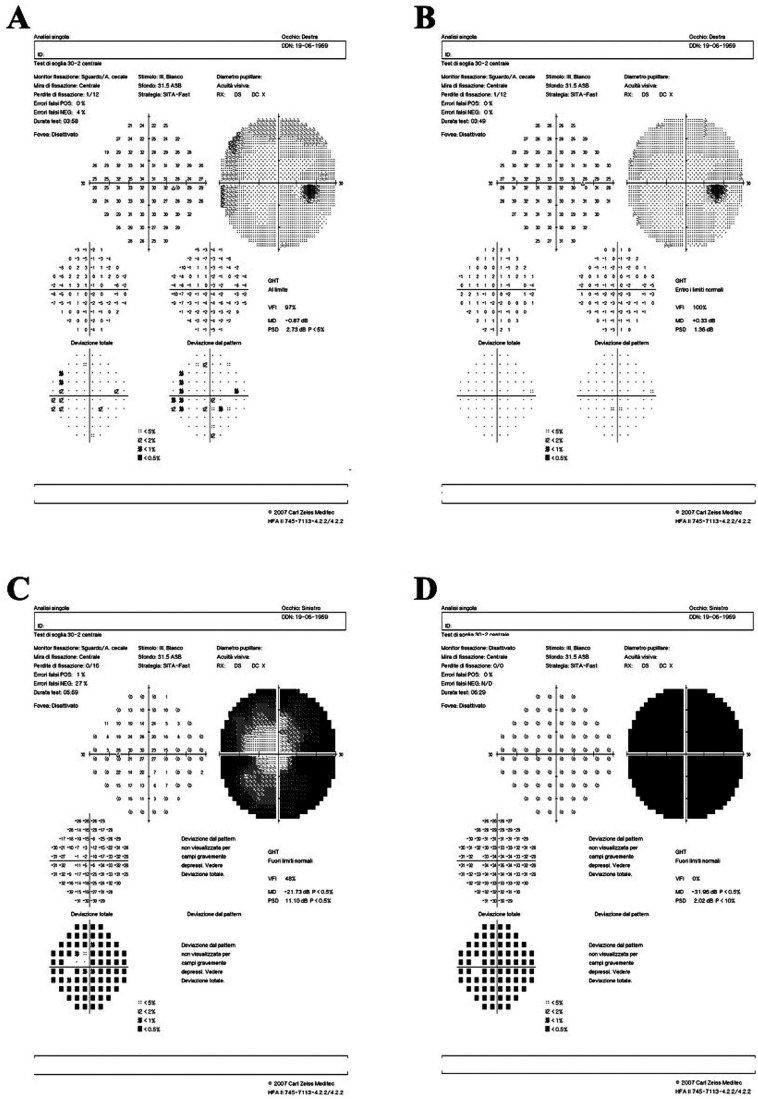
The VF performed at baseline in the right eye (March 31st) (Figure 1, Panel A) showed a moderate reduction in peripheral retinal sensitivity. VF at baseline showed a concentric scotoma in the left eye (Figure 1, Panel C).
Figure 1.
Humphrey visual field (VF) 24–2 testing. Panel A: VF performed on March 31st 2021, showed a moderate reduction in peripheral retinal sensitivity in the right eye. Panel B: VF showed an almost complete recovery of retinal sensitivity in peripheral fields of the right eye. Panel C: VF performed on March 31st 2021, showed marked concentrical reduction of retinal sensitivity in the left eye. Panel D: total loss of visual field in the left eye.
From February 28th 2021, the patient was started on oral prednisone, 50 mg daily, which was tapered and then discontinued in April 2021. Best corrected visual acuity remained stable at 20/20 in the right eye and 20/25 in the left eye.
Blood exams performed on April 4th 2021 showed erythrocyte sedimentation rate (ESR), platelet count within normal limits, and a slightly elevated C-reactive protein (CRP). Extensive screening for infections and autoimmunity was negative, including anti-Aquaporin-4, anti-myelin oligodendrocyte glycoprotein and anti-platelet factor 4 (anti-PF4) antibodies.
On June 2nd 2021, the patient received the first dose of Pfizer-BioNTech COVID-19 vaccine. Two days later, she experienced a further deterioration of visual acuity in the left eye and a severe headache.
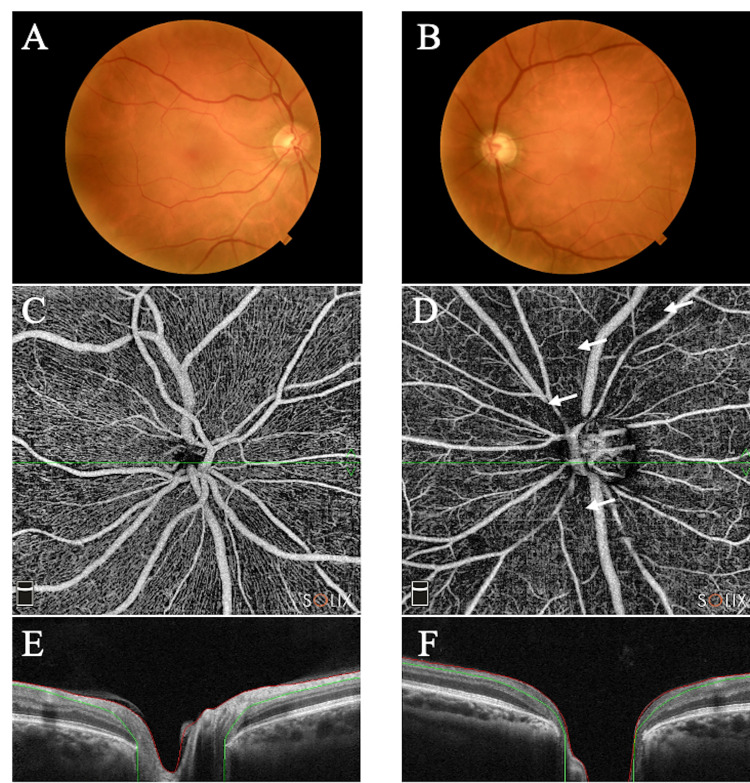
Visual acuity was reduced to light perception in the left eye, remaining stable at 20/20 in the right eye. The retinography of the right eye was normal, while the left eye appeared pale and showed sub-atrophic changes (Figure 2, Panels A-B). VFs performed after vaccination showed an almost complete recovery of retinal sensitivity in peripheral fields of the right eye (Figure 1, Panel B) and total loss of VF in the left eye (Figure 1, Panel D). The optical coherence tomography angiography (OCTA) of the papillary and peri-papillary area was normal on the right eye (Figure 2, Panel C). In contrast, the left eye showed a diffuse reduction of the superficial and deep vascular layer (Figure 2, Panel D).
Figure 2.
Panel A: the retinography of the right eye shows a normal optic nerve. Panel B: the retinography of the left eye shows a normal optic nerve. Panels C-D: optical coherence tomography angiography (OCTA) of the papillary and peri-papillary area in 6 × 6 SOLIX (Optovue) device. The right eye shows a normal vascularization of the superficial and deep vascular layer (Panel C). A diffuse reduction in the left eye is evident mainly in the deep vascular layer (Panel D). White arrows indicate the ischemic area. Panels E-F: normal OCT appearance of the optic nerve head in the right eye and pathologic cupping in the left eye.
A complete GCA work-up was performed: a doppler ultrasound of the left temporal artery and epiaortic vessels, a 18 F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) and a left temporal artery biopsy resulted negative. Thus, the diagnosis of GCA was ruled out. Long-term therapy with acetylsalicylic acid was prescribed. At a six-month follow-up, the patient did not show any further worsening of symptoms, but the amaurosis in the left eye persisted.
Conclusion
NA-AION is a cause of permanent vision loss. Even if the exact pathogenesis remains unclear, it seems to be a multifactorial disease that occurs when the blood supply of the optic nerve is interrupted, leading to hypoperfusion, ischemia and irreversible nerve fiber atrophy1.
Few cases of NA-AION have been described in patients with SARS-CoV-2 infection.2,3
In none of these cases, a NA-AION was the only manifestation of COVID-19. To the best of our knowledge, NA-AION associated with COVID-19 vaccination has not been described to date.
Hypercoagulability and hypoxemia, critical aspects of COVID-19, may play a role in the development of NA-AION, a circulatory insufficiency disease.1,4
Notably, a recent study in patients who recovered from COVID-19 has highlighted that SARS-CoV-2 may target the optic nerve's microvascular network.4
Our case had atypical characteristics because the patient presented with a new-onset headache, while NA-AION is usually painless. Another unusual feature was the involvement of the third cranial nerve. Thus, our first clinical suspicion was a GCA that was ruled out.
Moreover, after the administration of Pfizer-BioNTech COVID-19 vaccine, the patient presented loss of vision in the left eye and headache. This aspect is more difficult to justify, even if thromboembolic events after COVID-19 vaccinations have been extensively reported and have also been related to immune-mediated coagulopathy with anti-PF4.5
The partial involvement of the right eye, as revealed by peripheral retinal sensitivity reduction on VF performed shortly after the first episode, reverted at follow-up, probably due to the timely initiation of steroid treatment.
COVID-19 vaccination is the most effective intervention to reduce severe disease and death caused by SARS-CoV-2 infection. This report aims to shed light on possible ophthalmologic complications of COVID-19 and COVID-19 vaccination. A NA-AION with atypical features such as headache and third cranial nerve involvement may be the only manifestation of SARS-CoV-2 infection.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Consent: Informed consent was obtained from the patient
ORCID iDs: Giulia Amorelli https://orcid.org/0000-0001-5472-2672
Massimiliano Mirabella https://orcid.org/0000-0002-7783-114X
Viviana Nociti https://orcid.org/0000-0001-6016-3141
References
- 1.Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res 2009; 28: 34–62. 2008/12/10. DOI: 10.1016/j.preteyeres.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Rho J, Dryden SC, McGuffey CD, et al. A Case of Non-Arteritic Anterior Ischemic Optic Neuropathy with COVID-19. Cureus 2020; 12: e11950. 2021/01/12. DOI: 10.7759/cureus.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moschetta L, Fasolino G, Kuijpers RW. Non-arteritic anterior ischaemic optic neuropathy sequential to SARS-CoV-2 virus pneumonia: preventable by endothelial protection? BMJ case reports 2021; 14: e240542. DOI: 10.1136/bcr-2020-240542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savastano A, Crincoli E, Savastano MC, et al. Peripapillary Retinal Vascular Involvement in Early Post-COVID-19 Patients. J Clin Med 2020; 9. 2020/09/12. DOI: 10.3390/jcm9092895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cines DB, Bussel JB. SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. The New England journal of medicine 2021; 384: 2254–2256. 2021/04/16. DOI: 10.1056/NEJMe2106315. [DOI] [PMC free article] [PubMed] [Google Scholar]