Abstract
Although cardiovascular mortality in Japan is lower than in other industrialized countries, clinical outcomes in coronary artery disease (CAD) patients with type 2 diabetes mellitus (T2DM) remain poor despite multiple evidence-based drug therapies and interventions. We assumed that part of residual risk in these patients may be attributable to enhanced inflammation, which can be inhibited presumably by colchicine. However, dose-responsiveness of anti-inflammatory effect of colchicine has not been elucidated. Therefore, we designed a multicenter, randomized, double-blinded, parallel-group study to explore the dose-dependent effects of low-dose colchicine on serum high-sensitivity C-reactive protein (hs-CRP) concentration and safety in CAD patients with T2DM and enhanced inflammatory response as a phase 2 study. Enhanced inflammatory response was defined as peripheral white-blood cell count ≥7,000/μL. Patients (N = 63) will be randomly assigned to two doses of colchicine 0.25 mg/day, 0.5 mg/day, or placebo in a 1:1:1 ratio once daily for 12 weeks. Changes in serum hs-CRP levels will be evaluated as the primary endpoint, and changes in flow-mediated vasodilation and plasma myeloperoxidase levels will be evaluated as secondary endpoints. The results of this study will contribute to the development of a protocol for a planned future phase 3 trial to estimate the reduction in CAD. The present study describes the rationale, design, and methods of the trial.
Keywords: Colchicine, High-sensitivity C-reactive protein, Coronary artery disease, Type 2 diabetes, Inflammation
Introduction
In a recent global comparison of ischemic heart disease mortality rates, Japan has the lowest rate among developed countries, along with South Korea and France, and almost half that of the USA [1]. As reported in the Japanese Coronary Artery Disease (JCAD) study, Japanese patients have better short and long-term prognosis in patients with myocardial infarction than in Europe and the USA [2]. However, there remain high-risk patients among Japanese patients with coronary artery disease (CAD). CAD patients with accumulated risk factors, especially type 2 diabetes mellitus (T2DM), are considered to have the same risk as those with secondary prevention, even without a history of myocardial infarction [3], and they are recommended the use of aspirin in the American Diabetes Association guidelines [4].
In our recent cohort study [5], which followed approximately 8,000 Japanese patients with CAD and T2DM for an average of 3.7 years, 18% of patients had a myocardial infarction, stroke, or death. The annual event rate reached 5%, which is defined as a very high risk by the guidelines of the National Cholesterol Education Program in the USA [6]. The Osaka Acute Coronary Insufficiency Study (OACIS), which follows the prognosis of Japanese patients who were hospitalized with acute coronary syndrome (ACS) for about 3 years, reported that in patients complicated with T2DM, the incidence of fatal myocardial infarction was 6.8%, hospitalization for heart failure was 6.1%, and furthermore, major cardiovascular (CV) events including revascularization were over 30% [7]. From these observations, the prognosis of CAD patients complicated with T2DM is still poor in Japan, and therefore, the development of new intervention methods is required.
Although local inflammation in the vascular wall has been thought to play a crucial role in the progression of atherosclerosis and rupture of unstable plaque [8], no probable indicators that reflect the degree of inflammation supported by interventional studies have been developed. Furthermore, there are few reports that atherosclerotic diseases such as ACS could be prevented by suppressing inflammation. When vascular endothelial cells are damaged and activated by various stimuli, circulating leukocytes adhere to the endothelial cells due to the increase in the expression of adhesion molecules, followed by migration into the intima. Migrated leukocytes differentiate into macrophages, take up oxidized LDL via the scavenger receptor, and secrete inflammatory cytokines. This series of processes triggers chronic inflammation of the vascular wall [9], which is thought to occur in the progression of arteriosclerosis, plaque destabilization, or thrombosis. Therefore, leukocyte activation is the most upstream therapeutic target to suppress vascular inflammation. White blood cell (WBC) count is the simplest marker of leukocyte activation, and there exist many reports describing the correlation between WBC count and the occurrence or death of CV events in patients with ACS [10, 11, 12, 13] or chronic stable angina [14, 15, 16, 17] and in the general population [18, 19, 20, 21]. In our cohort study [5], patients with WBC ≥7,700/μL (75th percentile) had a significantly higher risk of CV events (hazard ratio 1.6, 95% confidence interval 1.38–1.85) than those with <5,300/μL (25th percentile). Furthermore, in 344 CAD patients in whom leukocyte activity was measured using a microchannel flow analyzer (HR200, Kowa Co., Ltd), the number of adherent leukocytes in patients with WBC <7000/μL (n = 261) was 5.80 ± 0.19 (mean ± SE)/field of view, which was significantly lower compared to 8.44 ± 0.47/field of view in patients with WBC ≥7,000/μL (n = 83) (p < 0.0001) (unpublished data). These results confirm the previous cohort studies so far, and patients with increased WBCs may have an increased risk of CV events.
Colchicine, commonly used for acute gout attack, is a classical, inexpensive anti-inflammatory drug. It has been reported that colchicine accumulates in leukocytes and suppresses activation due to inhibition of cytoskeletal microtubule formation. This microtubule inhibition prevents leukocyte migration in response to pro-inflammatory factors and chemotaxis after urate crystal phagocytosis. Recent reports have also revealed a new mechanism of action for colchicine, reporting that colchicine suppresses the activation of nucleotide-binding 1, oligomerization domain, leucine rich repeat and pyrin domain containing-3 (NLRP3) inflammasome which can induce IL-1β, a key cytokine in the inflammatory cascade, and IL-18 from its inactive precursor through microtubules [22, 23]. In addition, cholesterol crystals, known as an important player in vascular inflammation, are reported to activate NLRP3 inflammasome formation [24], suggesting that colchicine is a potential candidate drug to suppress vascular inflammatory responses. Clinical studies also suggest the potential role of colchicine in the management of vascular diseases, although it is still controversial. In a randomized controlled trial comparing the effects of placebo and colchicine (1.0 mg/day) on neointimal hyperplasia and in-stent restenosis after bare-metal stent implantation in CAD patients with DM, colchicine significantly suppressed in-stent restenosis compared to placebo [25]. Also, in stable CAD patients, most of whom were treated with aspirin and high-dose statins, colchicine (0.5 mg/day) reduced the risk of CV events by 67% [26]. Contrary, preventing effect of colchicine on restenosis after angioplasty was denied in other studies [27, 28].
Abovementioned observations generally led us to re-evaluate the efficacy of colchicine on vascular inflammation in high-risk CAD patients. Two recent clinical studies using low-dose colchicine (0.5 mg/day), namely, COLCOT trial [29] and LoDoCo2 trial [30], reported a significant reduction in the risk of combined CV events in patients recruited within 30 days after myocardial infarction and in those with chronic coronary disease, respectively. However, both studies showed no reduction in CV death, and there was no significant difference in risk of myocardial infarction alone in the COLCOT trial compared to placebo. One possible reason is that not many subjects with activated WBCs, who are most likely to benefit from colchicine, were included in these studies. Therefore, we designed the phase 2, randomized, double-blinded, placebo-controlled, multicenter, parallel-group comparison trial in CAD patients complicated with T2DM who have increased WBCs (≥7,000/μL). We will also conduct the study with a candidate dose of 0.25 mg, which is less likely to cause dose-dependent diarrhea.
Methods/Design
Trial Design
This is a multicenter, randomized, double-blinded, placebo-controlled, parallel-group comparison trial to determine the effectiveness of colchicine on reduction in high-sensitivity C-reactive protein (hs-CRP) in CAD patients with T2DM and enhanced inflammatory response. The linearity of the dose-response relationship for efficacy and safety is also evaluated. The eligibility criteria are shown in Table 1. Registration, randomization, and data collection are performed using an electronic data capture system. Randomization is performed centrally through the electronic data capture system with a stochastic minimization algorithm to balance treatment assignment within and across hospitals and statin use.
Table 1.
Patient eligibility criteria
| Inclusion criteria:patients who fulfilled all the following criteria were included |
| 1. CAD patients complicated with T2DM(*1) and enhanced inflammatory response(*2) who were clinically stable for the past 3 months |
| 2. Patients aged ≥20 years at the time of consent |
| 3. If patients are women who may become pregnant or men who have not received contraceptive surgery(*3) with a female partner who may become pregnant, patients who agree to conduct appropriate contraception from the start of the study drug until the 90 days after last administration |
| 4. Patients who provide written consent to participate in the trial of their own free will based on a sufficient understanding of the trial following an adequate explanation |
| (*1) CAD is diagnosed by ≥75% stenosis of coronary arteries in coronary angiography; history of ACS and history of coronary artery bypass or percutaneous coronary angioplasty; T2DM is diagnosed by the criteria of The Japan Diabetes Society |
| (*2) Enhanced inflammatory response is defined as WBC count ≥7000/µL |
| (*3) Men who receive contraceptive surgery indicate men who have passed at least 1 year after vasectomy and have documents proving the absence of sperm during ejaculation |
| Exclusion criteria: patients who met any of the following criteria were excluded |
| 1. Patients with a history of hypersensitivity to colchicine preparations |
| 2. Patients with already undertreated with colchicine or patients who took colchicine 30 days before qualification check date |
| 3. Patients with liver cirrhosis |
| 4. Patients with clinically cholestasis |
| 5. Patients with renal dysfunction (eGFR ≤30 mL/min/1.73 m2) |
| 6. Patients with active malignant tumor |
| 7. Patients who take drugs that may interact with colchicine (drugs indicated in package insert) |
| a. Drugs which inhibit CYP3A4: (strongly inhibit) atazanavir, clarithromycin, indinavir, itraconazole, nelfinavir, ritonavir, saquinavir, darunavir, telithromycin, telaprevir; drugs containing cobicistat (modestly inhibit), amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, verapamil |
| b. Drugs which inhibit P-glycoprotein: cyclosporine |
| 8. Patients who take amiodarone or quinidine |
| 9. Patients with apparent infection or inflammatory diseases |
| 10. Smoker |
| 11. Patients who are pregnant, potentially pregnant, or lactating |
| 12. Patients who now participate other clinical trial or participated within 30 days before obtaining consent |
| 13. Patients considered ineligible for any other reason by a study investigator |
CAD, coronary artery disease; T2DM, type 2 diabetes mellitus; ACS, acute coronary syndrome; eGFR, estimated glomerular filtration rate; CYP, cytochrome P450.
Trial Oversight
The principal investigator designed and conducted this study in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan. Protocol and consent forms were reviewed and approved by the Institutional Review Board at the University of the Ryukyus (approved number [104]) as the Central Ethics Committee and each participating center (Table 2) to which important protocol modification and safety information including serious adverse events in this trial are reported. All patients or their legally authorized representatives provided written informed consent before randomization with investigators. All centers are regularly monitored by the University of the Ryukyus, and auditing of Good Clinical Practice for this study is commissioned to a private audit company (Table 2). This trial was registered at UMIN-CTR Clinical Trial (UMIN000029170, https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000033349).
Table 2.
Study oversight
| Role in study | Name | Institution |
|---|---|---|
| Principal investigator | Shinichiro Ueda, MD, PhD | Department of Clinical Pharmacology and Therapeutics, University of the Ryukyus |
|
| ||
| Co-principal investigator | Junya Ako, MD, PhD | Department of Cardiovascular Medicine, Kitasato University School of Medicine |
|
|
||
| Yukihito Higashi, MD, PhD | Department of Cardiovascular Regeneration and Medicine, Hiroshima University | |
|
|
||
| Kazuo Ishikawa, MD | Diabetes Center, Urasoe General Hospital | |
|
|
||
| Shinji Koba, MD, PhD | Division of Cardiology, Showa University School of Medicine | |
|
|
||
| Yuji Kumagai MD, PhD | Clinical Trial Center, Kitazato University Hospital | |
|
|
||
| Koichi Node, MD, PhD | Department of Cardiology, Saga University School of Medicine | |
|
|
||
| Ichiro Sakuma, MD, PhD | Cardiovascular Medicine, Hokko Memorial Clinic | |
|
|
||
| Hiroki Uehara, MD | Department of Cardiology, Urasoe General Hospital | |
|
|
||
| Takanori Yasu, MD, PhD | Department of Cardiovascular Medicine and Nephrology, Dokkyo Medical University Nikko Medical Center | |
|
| ||
| Central review of FMD | Hirofumi Tomiyama, MD, PhD | Department of Cardiology, Tokyo Medical University |
|
| ||
| Statistical analysis | Takeshi Morimoto, MD, PhD, MPH | Department of Clinical Epidemiology, Hyogo College of Medicine |
|
| ||
| Drug manufacture and management | Masahiro Okuda, PhD | Department of Pharmacy, Osaka University Hospital |
|
| ||
| Drug allocation | Hisako Yoshida, PhD | Department of Medical Statistics, Osaka City University |
|
| ||
| Data management and monitoring | Yumi Ikehara, MS, Kaori Une | Clinical Research and Quality Management Center, University of the Ryukyus Hospital |
|
| ||
| EDC system support | Ayumi Shintani, PhD, MPH | Department of Medical Statistics, Osaka City University |
|
| ||
| GCP auditing | Katsumi Ito | A2 Healthcare |
|
| ||
| Measurement of concentration of colchicine and myeloperoxidase | Akiko Mutoh, PhD | Department of Clinical Pharmacology and Therapeutics, University of the Ryukyus |
|
| ||
| Coordinating investigator | Yoshikazu Miwa, MD, PhD | Department of Clinical Pharmacology and Therapeutics, University of the Ryukyus |
FMD, flow-mediated vasodilation; EDC, electronic data capture; GCP, Good Clinical Practice.
Trial Intervention
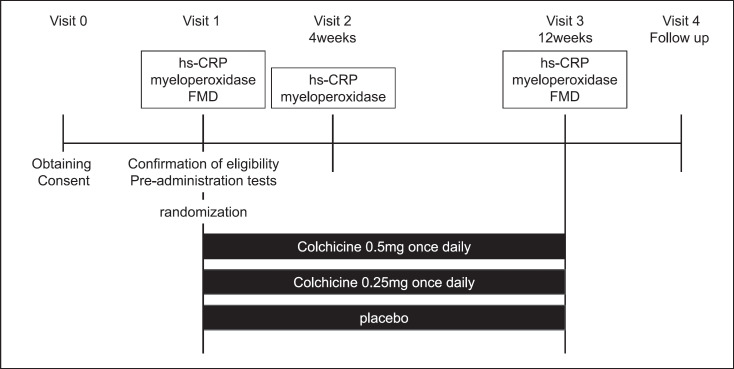
After the qualification check (visit 1), eligible patients randomly receive colchicine (0.5 mg/day), colchicine (0.25 mg/day), or placebo at a ratio of 1:1:1 (Fig. 1). Treatment assignment is concealed from participants or treating physicians. Patients are given drugs orally once per day for 12 weeks. Changes in the medication use as well as other drugs with possible effects on outcome are prohibited. We regularly monitor participants and their physicians for adherence to the study medication/dose at every visit.
Fig. 1.
Trial design. After informed consent is obtained, eligible patients randomly receive colchicine (0.5 mg/day), colchicine (0.25 mg/day), or placebo at a ratio of 1:1:1. Patients are given drugs orally once per day for 12 weeks. FMD; flow-mediated vasodilation.
Outcome Measures
The primary endpoint is the change in hs-CRP from baseline to 4 weeks after administration. Secondary endpoints are the changes in hs-CRP and flow-mediated vasodilation (FMD) from baseline to 12 weeks after administration and plasma myeloperoxidase concentration from baseline to 4 or 12 weeks after administration. Safety outcomes are CV events including death, myocardial infarction, cerebral infarction, admission due to heart failure, and unstable angina and any adverse events systematically reported for 12 weeks, including diarrhea. Safety outcomes are defined in the protocol. Symptoms requiring hospital admission are included according to Good Clinical Practice.
Measurement of Serum hs-CRP
Serum hs-CRP is measured at baseline, 4 and 12 weeks. Blood samples are obtained while fasting or at least 4 h after a meal. Collect 6 mL of venous blood into a plain tube or a blood collection tube with serum separator, leave at room temperature for 30 min, and then centrifuge at 1,200 g for 15 min at 20°C to obtain serum. Dispense 1 mL of serum into 1.5-mL microcentrifuge tubes and freeze at ≤ −20°C until measurement. Measurement shall be conducted by a central inspection agency (SRL Co., Ltd.). Measurement results will not be reported to the implementing medical institution or the principal investigator until data fixation and will be stored at the central measurement period. Measurement of hs-CRP will not be performed during the clinical trial except for this clinical trial.
Measurement of FMD
FMD is measured using a commercially available ultrasound instrument equipped with an online computer-assisted semi-automatic analysis software (EF, Unex Co. Ltd, Nagoya, Japan) at baseline and 12 weeks as described previously [31]. The brachial artery diameter was determined at 21 points in a 3-mm segment of the longitudinal B-mode image. FMD is estimated as the percent increase in the diameter of the brachial artery over the baseline value at maximal dilatation during reactive hyperemia.
Measurement of Plasma Myeloperoxidase Concentration
Plasma myeloperoxidase concentration is measured at baseline, 4 and 12 weeks. After collection of 5 mL of venous blood into an EDTA-2Na tube, mix by inverting 5–6 times, and then centrifuge at 1,500 g at 4°C for 15 min. The plasma sample is ice-cold immediately and stored frozen at ≤−20°C until measurement. Measurement is performed with fluorescent microbead immunoassay (Luminex system).
Other Measurements
Blood pressure, heart rate, complete blood count, and blood chemistry are measured at baseline, 4 and 12 weeks. Electrocardiogram is performed at baseline and 12 weeks. Pregnancy test is done for women who can get pregnant at baseline. Blood samples are obtained while fasting or at least 4 h after a meal. Follow-up is done at the hospital outpatient clinic or referring clinics 3 weeks after the end of treatment.
Data Management
Data management including data entry, coding, security, and storage, including any related processes to promote data quality, is carried out by the University of the Ryukyus. The details are described in the full protocol.
Sample Size and Statistical Analysis
The primary objective of the analysis in this trial is to attest to a linear dose-response relationship. To date, colchicine dose-setting trials using the same index have not been conducted. The previous study [32] compared serum hs-CRP levels between subjects treated with colchicine 1.0 mg/day and those without treatment and reported that hs-CRP levels after 4 weeks of treatment were 1.78 (SD 1.23) mg/dL in the colchicine group and 3.70 (SD 2.30) mg/dL in the non-treated group, respectively. From this result, we estimated that hs-CRP is suppressed to 3.22 mg/L in the 0.25 mg/day treatment group and 2.74 mg/L in the 0.5 mg/day treatment group, respectively, from 3.70 mg/L in the placebo group. Assuming SD of all treatment groups is common and 1.0 mg/dL, and contrast of placebo, 0.25 mg/day, and 0.5 mg/day in treatment groups was 1, 0, −1, we calculated that a total 63 patients are needed with a one-sided alpha of 0.025 and a power of 0.8. If the dose-response relationship reached a peak at 0.25 mg and the resultant contrast was 2-1-1, the power becomes 68% with 63 patients. Considering the dropout cases, the target number of patients was set at 23 patients in each group, resulting in a total of 69 patients.
The statistical analysis plan will be specified before data analysis. The full analysis set (FAS) includes patients who received allocated treatment and provided assessable outcome data. The safety analysis set (SAS) includes patients who received allocated treatment at least once. The per protocol set includes patients who received allocated treatment and for whom planned outcome data as per the protocol are available. The FAS is used for the primary endpoint, and the FAS and per protocol set are used for secondary endpoints. The SAS is used for safety outcomes. Categorical variables are expressed as frequencies with percentages, and continuous variables are expressed as means with SDs or medians with interquartile ranges. All analyses are conducted under the intention-to-treat principle.
For the dose and effect of colchicine, a dose-response line is determined by one-way regression analysis. Effects are assessed by the difference in plasma myeloperoxidase and serum hs-CRP concentration before and after 4 weeks of treatment and the difference in FMD, an index of vascular endothelial function, before and after 12 weeks of treatment. Doses are log transformed, and appropriate hypothetical values for placebo are used. For the changes in other endpoints, a paired t test is used for comparisons of the baseline and follow-up values within the group, and two-sample t tests are used for comparisons between groups. All statistical analyses are performed by a study statistician (T. Morimoto) with the use of JMP (SAS Institute Inc., Cary, NC) or SAS (SAS Institute Inc., Cary, NC) based on the statistical analysis plan. All p values are two-sided, and p < 0.05 is considered significant. For baseline data, missing data are not imputed, and data with missing information are analyzed as they are. Because of the short enrollment and follow-up periods and the estimated low risk of adverse events, no interim analyses are planned.
Discussion
We have developed the phase 2 study protocol examining dose-dependent effects of low doses of colchicine on hs-CRP and safety in CAD patients with T2DM and enhanced leukocyte activation. We are willing to move to the phase 3 study for the approval of colchicine as a drug to reduce CV events in these patients. Our study protocol is characterized by the following: the enrollment of CAD patients with T2DM and enhanced leukocyte activity in order to have the sufficient statistical power and clear evidence for efficacy, setting hs-CRP as the primary endpoint, and testing two low doses of colchicine.
Since the proposal of inflammation hypothesis of atherosclerosis, several clinical trials with anti-inflammatory drugs have been conducted based upon the promising results from animal model of atherosclerosis [33]. These trials, unfortunately, failed to show any significant reduction in risks for CV events [34, 35]. More recently, however, the Canakinumab Anti-inflammatory Thrombosis Outcome Study (CANTOS) found that canakinumab, a monoclonal antibody against IL-1β, significantly reduced recurrent CV events and hs-CRP independent of lipid-level lowering [36]. Results from CANTOS trial suggest that colchicine, which can also inhibit NLRP3 inflammasome-IL-1β pathway as an anti-inflammatory drug, is supposed to similarly reduce CV risk in CAD patients. In fact, COLCOT trial [29] and LoDoCo2 trial [30] showed a significant reduction of risks for CV events in CAD patients. However, both trials failed to reduce the risk of CV death. In addition, unfortunately, the COLCOT trial also failed to reduce the risk of myocardial infarction, and the LoDoCo trial showed a higher risk of all-cause mortality, although not statistically significant. Such unclear results from large-scale clinical trials may result from lower than expected CV risks due to therapeutic interventions based on the background of previous evidence and/or unselected patient population that was not influenced by the drug being studied. The former situation requires a very large sample size or very high-risk population, and for the latter reason, identification and enrollment of patients who are likely to benefit from the study drug should have been enrolled. From these points of view, we will enroll CAD patients with T2DM and enhanced leukocyte activity who carry the highest CV risk in Japan even under the evidence-based optimal medical therapy [5] and are likely to benefit from colchicine for this phase 2 trial and a future phase 3 trial.
Hs-CRP is an established marker of CV disease. Elevated hs-CRP is associated with poor prognosis after ACS, and although controversial, an active role for hs-CRP in atherosclerotic plaque formation and progression has also been proposed. Currently, hs-CRP is considered to be a true CV risk factor as well as low-density lipoprotein cholesterol, and the concept of hs-CRP as a residual inflammatory CV risk is expanding. We set the change in hs-CRP as a primary endpoint because of the previous report indicating that colchicine 1 mg for 4 weeks reduced hs-CRP by about 60% in CAD patients with hs-CRP ≥0.2 mg/dL who received aspirin and statins [26]. Since the main pharmacological effect of colchicine is suppression of leukocyte activation, we also set the changes in leukocyte activation evaluated by the plasma myeloperoxidase concentration as a secondary endpoint. We previously confirmed that leukocyte activation by systemic free fatty acid directly reduces vascular endothelial function via myeloperoxidase, which was increased by leukocyte degranulation [37]. In our clinical study in healthy individuals, colchicine 0.5 mg/day for 1 week suppressed leukocyte activation (adhesion to microchannels) and the increase in plasma myeloperoxidase due to systemic free fatty acid loading (unpublished data). By measuring these markers simultaneously, it is possible to know the effect of colchicine on leukocyte in detail. Although vascular endothelial function measured by FMD is not established as a true surrogate marker in arteriosclerotic disease, many studies showed an association with CV events, and various interventions for arteriosclerosis have been reported a correlation between improvement of vascular endothelial function and risk reduction of clinical endpoint [38, 39, 40]. Therefore, these indices are thought to be appropriate for evaluating the efficacy of colchicine.
Another problem we should solve is the issue of proper dosage of colchicine. The daily dose of 0.5 mg is the approved dose in Japan for familial Mediterranean fever. This dose is less than half the amount used for gout prevention, epicarditis, and Behcet's disease for Caucasians. Although the long-term use of colchicine at doses of 1–2 mg/day has been well documented to be safe and reasonably well tolerated in patients with familial Mediterranean fever [41], we selected low-dose colchicine because we already confirmed its inhibitory effect on leukocyte activation and it has been used in long-term previous studies targeting CAD. However, the occurrence of diarrhea is dose dependent, and chronic administration may accumulate in leukocytes for a long time even at low doses. In a previous study, diarrhea occurred in >10% subjects even at 0.5 mg daily [26]. Considering these issues, a dose-finding study was planned with a lower daily dose of 0.25 mg. To evaluate the linearity of the dose-response relationship, a plan with a daily dose of 0.125 mg was ideal, but it was difficult in terms of formulation production and was abandoned. From the results of our pharmacokinetic study, the half-life of colchicine in neutrophils is 50 h, and the administration period is expected to reach a steady state in about 2 weeks. Therefore, the duration of drug exposure was set at 4 weeks that is sufficient for pharmacological evaluation.
Conclusion
From the points of view discussed above, a double-blinded, randomized, controlled trial investigating the effects of colchicine on hs-CRP levels in CAD patients complicated with T2DM with enhanced inflammatory response was designed.
Statement of Ethics
Protocol and consent forms were approved by the Institutional Review Board at the University of the Ryukyus (approved number [104]) as the Central Ethics Committee and each participating center. All patients or their legally authorized representatives provided written informed consent before randomization. Results from this trial are disseminated through publications and conference presentations to participants, healthcare professionals, and the public. The compensation to those who suffer death or severe damage requiring hospitalization from trial participation is provided from the clinical trial insurance organized by the trial sponsor (University of the Ryukyus).
Conflict of Interest Statement
Dr. Shinichiro Ueda received research grants from Bristol-Myers Squibb and Kowa; non-purpose research grants from Bristol-Myers Squibb, Chugai, MSD, Pfizer, and Takeda; and lecturer's fees from Boehringer Ingelheim and MSD. Dr Yukihito Higashi received consulting fees from Mitsubishi Tanabe related to this study, as well as honoraria and grants from Teijin, Boehringer Ingelheim, MSD, Sanofi, AstraZeneca, Kyowa Hakko Kirin, Takeda, Astellas, Daiichi Sankyo, Mochida, Nihon Kohden, Shionogi, Nippon Sigmax, Sanwa Kagaku Kenkyusho, Unex, and Kao and honoraria from Radiometer, Omron, Sumitomo Dainippon, Otsuka, Torii, Kowa, Fujiyakuhin, Amgen, Nippon Shinyaku, Itamar, Bayer, Eli Lilly, and Ono.
Funding Sources
This study was supported by Japan Agency for Medical Research and Development (AMED) of Japan [171k0201068h001, 181k0201068h002, 191k0201068h003, 201k0201068h004, and 211k0201068h005].
Author Contributions
Yoshikazu Miwa: conception of the study protocol development and preparation of the manuscript; Akiko Mutoh: conception of the study protocol development and planning and preparation of the measurement of myeloperoxidase concentration; Takeshi Morimoto: conception of the study protocol development, design of the statistical analysis methodology, and preparation for conducting research at own institutes; Yumi Ikehara: conception of the study protocol development, preparation of the study protocol, and preparation for conducting research at own institutes; Takanori Yasu, Shinji Koba, Junya Ako, Yukihito Higashi, Masato Kajikawa, Hiroki Uehara, Kazuo Ishikawa, Ichiro Sakuma, Koichi Node, and Yuji Kumagai: conception of the study protocol development and preparation for conducting research at own institutes; Hirofumi Tomiyama: conception of the study protocol development, advice in the preparation of FMD implementation plans, and preparation for conducting research at own institutes; and Shinichiro Ueda: conception of the study protocol development, preparation for conducting research at own institutes, and supervision of research. All authors have given final approval to the manuscript being submitted and agree to take responsibility for all aspects of the work to ensure that any questions regarding its accuracy or completeness are properly investigated and resolved.
Data Availability Statement
The access to the final trial dataset is rigidly restricted to investigators who are authorized by the Steering Committee and any activity is recorded. There are contractual agreements that limit such access for investigators. Confidentiality in the collection of personal information is protected in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
Acknowledgments
We thank Ms. Tamiko Kamitaka, Ms. Saori Hirota, and Ms. Miho Kameda for their data management and monitoring. We also thank Dr. Ayumi Nakamura, Dr. Mitsunori Nishikawa, and Dr. Kouta Kokado for their efforts in drug manufacture and management.
Funding Statement
This study was supported by Japan Agency for Medical Research and Development (AMED) of Japan [171k0201068h001, 181k0201068h002, 191k0201068h003, 201k0201068h004, and 211k0201068h005].
References
- 1.World Health Organization World Health Organization Measurement and health Information. Available from: https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html (accessed February 7, 2022)
- 2.Saito M, Fukami K, Hiramori K, Haze K, Sumiyoshi T, Kasagi H. Long-term prognosis of patients with acute myocardial infarction: is mortality and morbidity as low as the incidence of ischemic heart disease in Japan. Am Heart J. 1987 Apr;113((4)):891–7. doi: 10.1016/0002-8703(87)90049-4. [DOI] [PubMed] [Google Scholar]
- 3.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998 Jul 23;339((4)):229–34. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association 8. Cardiovascular disease and risk management. Diabetes Care. 2016;39((Suppl 1)):S60–71. doi: 10.2337/dc16-S011. [DOI] [PubMed] [Google Scholar]
- 5.Kawabe A, Yasu T, Morimoto T, Tokushige A, Momomura SI, Sakakura K, et al. WBC count predicts heart failure in diabetes and coronary artery disease patients: a retrospective cohort study. ESC Heart Fail. 2021 Oct;8((5)):3748–59. doi: 10.1002/ehf2.13513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grundy SM, Cleeman JI, Bairey Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the national cholesterol education Program adult treatment panel III guidelines. J Am Coll Cardiol. 2004 Aug 4;44((3)):720–32. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Nakatani D, Sakata Y, Mizuno H, Shimizu M, Suna S, Usami M, et al. Impact of diabetes mellitus on rehospitalization for heart failure among survivors of acute myocardial infarction in the percutaneous coronary intervention era. Circ J. 2009 Apr;73((4)):662–6. doi: 10.1253/circj.cj-08-0579. [DOI] [PubMed] [Google Scholar]
- 8.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005 Apr 21;352((16)):1685–95. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 9.Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999 Jan 14;340((2)):115–26. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 10.Pitsavos C, Kourlaba G, Panagiotakos DB, Tsamis E, Kogias Y, Stravopodis P, et al. Does smoking status affect the association between baseline white blood cell count and in-hospital mortality of patients presented with acute coronary syndrome? The Greek study of acute coronary syndromes (GREECS) Int J Cardiol. 2008 Mar 28;125((1)):94–100. doi: 10.1016/j.ijcard.2007.05.030. [DOI] [PubMed] [Google Scholar]
- 11.Barron HV, Harr SD, Radford MJ, Wang Y, Krumholz HM. The association between white blood cell count and acute myocardial infarction mortality in patients ≥65 years of age: findings from the cooperative cardiovascular project. J Am Coll Cardiol. 2001 Nov 15;38((6)):1654–61. doi: 10.1016/s0735-1097(01)01613-8. [DOI] [PubMed] [Google Scholar]
- 12.Cannon CP, McCabe CH, Wilcox RG, Bentley JH, Braunwald E. Association of white blood cell count with increased mortality in acute myocardial infarction and unstable angina pectoris. OPUS-TIMI 16 Investigators. Am J Cardiol. 2001 Mar 1;87((5)):636–639. doi: 10.1016/s0002-9149(00)01444-2. A10. [DOI] [PubMed] [Google Scholar]
- 13.Grzybowski M, Welch RD, Parsons L, Ndumele CE, Chen E, Zalenski R, et al. The association between white blood cell count and acute myocardial infarction in-hospital mortality: findings from the National Registry of Myocardial Infarction. Acad Emerg Med. 2004 Oct;11((10)):1049–60. doi: 10.1197/j.aem.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Hajj-Ali R, Zareba W, Ezzeddine R, Moss AJ. Relation of the leukocyte count to recurrent cardiac events in stable patients after acute myocardial infarction. Am J Cardiol. 2001 Dec 1;88((11)):1221–4. doi: 10.1016/s0002-9149(01)02080-x. [DOI] [PubMed] [Google Scholar]
- 15.Marchioli R, Avanzini F, Barzi F, Chieffo C, Di Castelnuovo A, Franzosi MG, et al. Assessment of absolute risk of death after myocardial infarction by use of multiple-risk-factor assessment equations: GISSI-Prevenzione mortality risk chart. Eur Heart J. 2001 Nov;22((22)):2085–103. doi: 10.1053/euhj.2000.2544. [DOI] [PubMed] [Google Scholar]
- 16.Ndrepepa G, Braun S, Iijima R, Keta D, Byrne RA, Schulz S, et al. Total leucocyte count, but not C-reactive protein, predicts 1-year mortality in patients with acute coronary syndromes treated with percutaneous coronary intervention. Clin Sci. 2009 Apr;116((8)):651–8. doi: 10.1042/CS20080298. [DOI] [PubMed] [Google Scholar]
- 17.Stewart RA, White HD, Kirby AC, Heritier SR, Simes RJ, Nestel PJ, et al. White blood cell count predicts reduction in coronary heart disease mortality with pravastatin. Circulation. 2005 Apr 12;111((14)):1756–62. doi: 10.1161/01.CIR.0000160924.73417.26. [DOI] [PubMed] [Google Scholar]
- 18.Jee SH, Park JY, Kim H-S, Lee TY, Samet JM. White blood cell count and risk for all-cause, cardiovascular, and cancer mortality in a cohort of Koreans. Am J Epidemiol. 2005 Dec 1;162((11)):1062–9. doi: 10.1093/aje/kwi326. [DOI] [PubMed] [Google Scholar]
- 19.Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998 May 13;279((18)):1477–82. doi: 10.1001/jama.279.18.1477. [DOI] [PubMed] [Google Scholar]
- 20.Yarnell JWG, Patterson CC, Sweetnam PM, Lowe GDO. Haemostatic/inflammatory markers predict 10-year risk of IHD at least as well as lipids: the Caerphilly collaborative studies. Eur Heart J. 2004 Jun;25((12)):1049–56. doi: 10.1016/j.ehj.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Brown DW, Giles WH, Croft JB. White blood cell count: an independent predictor of coronary heart disease mortality among a national cohort. J Clin Epidemiol. 2001 Mar;54((3)):316–22. doi: 10.1016/s0895-4356(00)00296-1. [DOI] [PubMed] [Google Scholar]
- 22.Leung YY, Yao Hui LL, Kraus VB. Colchicine -- update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015 Dec;45((3)):341–50. doi: 10.1016/j.semarthrit.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Misawa T, Takahama M, Kozaki T, Lee H, Zou J, Saitoh T, et al. Microtubule-driven spatial arrangement of mitochondria promotes activation of the NLRP3 inflammasome. Nat Immunol. 2013 May;14((5)):454–60. doi: 10.1038/ni.2550. [DOI] [PubMed] [Google Scholar]
- 24.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010 Apr 29;464((7293)):1357–61. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deftereos S, Giannopoulos G, Raisakis K, Kossyvakis C, Kaoukis A, Panagopoulou V, et al. Colchicine treatment for the prevention of bare-metal stent restenosis in diabetic patients. J Am Coll Cardiol. 2013 Apr 23;61((16)):1679–85. doi: 10.1016/j.jacc.2013.01.055. [DOI] [PubMed] [Google Scholar]
- 26.Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. 2013 Jan 29;61((4)):404–10. doi: 10.1016/j.jacc.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 27.O'Keefe JH, Jr, McCallister BD, Bateman TM, Kuhnlein DL, Ligon RW, Hartzler GO. Ineffectiveness of colchicine for the prevention of restenosis after coronary angioplasty. J Am Coll Cardiol. 1992 Jun;19((7)):1597–600. doi: 10.1016/0735-1097(92)90624-v. [DOI] [PubMed] [Google Scholar]
- 28.Freed M, Safian RD, O'Neill WW, Safian M, Jones D, Grines CL. Combination of lovastatin, enalapril, and colchicine does not prevent restenosis after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1995 Dec 1;76((16)):1185–8. doi: 10.1016/s0002-9149(99)80334-8. [DOI] [PubMed] [Google Scholar]
- 29.Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. 2019 Dec 26;381((26)):2497–505. doi: 10.1056/NEJMoa1912388. [DOI] [PubMed] [Google Scholar]
- 30.Nidorf SM, Fiolet ATL, Mosterd A, Eikelboom JW, Schut A, Opstal TSJ, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020 Nov 5;383((19)):1838–47. doi: 10.1056/NEJMoa2021372. [DOI] [PubMed] [Google Scholar]
- 31.Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, et al. Reliability of measurement of endothelial function across multiple institutions and establishment of reference values in Japanese. Atherosclerosis. 2015 Oct;242((2)):433–42. doi: 10.1016/j.atherosclerosis.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 32.Nidorf M, Thompson PL. Effect of colchicine (0.5 mg twice daily) on high-sensitivity C-reactive protein independent of aspirin and atorvastatin in patients with stable coronary artery disease. Am J Cardiol. 2007 Mar 15;99((6)):805–7. doi: 10.1016/j.amjcard.2006.10.039. [DOI] [PubMed] [Google Scholar]
- 33.Fraser H, Hislop C, Christie RM, Rick HL, Reidy CA, Chouinard ML, et al. Varespladib (A-002), a secretory phospholipase A2 inhibitor, reduces atherosclerosis and aneurysm formation in ApoE-/- mice. J Cardiovasc Pharmacol. 2009 Jan;53((1)):60–5. doi: 10.1097/FJC.0b013e318195bfbc. [DOI] [PubMed] [Google Scholar]
- 34.Nicholls SJ, Kastelein JJP, Schwartz GG, Bash D, Rosenson RS, Cavender MA, et al. Varespladib and cardiovascular events in patients with an acute coronary syndrome: the VISTA-16 randomized clinical trial. JAMA. 2014 Jan 15;311((3)):252–62. doi: 10.1001/jama.2013.282836. [DOI] [PubMed] [Google Scholar]
- 35.The STABILITY Investigators. White HD, Held C, Stewart R, Tarka E, Brown R, et al. Darapladib for preventing ischemic events in stable coronary heart disease. N Engl J Med. 2014 May 1;370((18)):1702–11. doi: 10.1056/NEJMoa1315878. [DOI] [PubMed] [Google Scholar]
- 36.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017 Sep 21;377((12)):1119–31. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 37.Azekoshi Y, Yasu T, Watanabe S, Tagawa T, Abe S, Yamakawa K, et al. Free fatty acid causes leukocyte activation and resultant endothelial dysfunction through enhanced angiotensin II production in mononuclear and polymorphonuclear cells. Hypertension. 2010 Jun;56((1)):136–42. doi: 10.1161/HYPERTENSIONAHA.110.153056. [DOI] [PubMed] [Google Scholar]
- 38.Tomiyama H, Yamashina A. Non-invasive vascular function tests: their pathophysiological background and clinical application. Circ J. 2010 Jan;74((1)):24–33. doi: 10.1253/circj.cj-09-0534. [DOI] [PubMed] [Google Scholar]
- 39.Flammer AJ, Anderson T, Celermajer DS, Creager MA, Deanfield J, Ganz P, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012 Aug 7;126((6)):753–67. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Charakida M, Masi S, Lüscher TF, Kastelein JJP, Deanfield JE. Assessment of atherosclerosis: the role of flow-mediated dilatation. Eur Heart J. 2010 Dec;31((23)):2854–61. doi: 10.1093/eurheartj/ehq340. [DOI] [PubMed] [Google Scholar]
- 41.Kallinich T, Haffner D, Niehues T, Huss K, Lainka E, Neudorf U, et al. Colchicine use in children and adolescents with familial Mediterranean fever: literature review and consensus statement. Pediatrics. 2007 Feb;119((2)):e474–83. doi: 10.1542/peds.2006-1434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The access to the final trial dataset is rigidly restricted to investigators who are authorized by the Steering Committee and any activity is recorded. There are contractual agreements that limit such access for investigators. Confidentiality in the collection of personal information is protected in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.