Abstract
Objective:
In the Emergency Department, the physician’s purpose is to rapidly and accurately diagnose the severity of a patient’s condition so that proper treatment can be administered. Therefore, this study pays close attention to the association and prognostic value of blood lactate on different disease outcomes by systematically reviewing recently published studies.
Methods:
The search strategy was developed based on searches in the year 2022 for potential publications including original articles, case reports, and reviews using the following web databases google scholar, PubMed, and Science Direct. A total of 25 studies were identified and reviewed extensively to evaluate the link between mortality and serum lactate levels.
Results:
This literature review presents the strong association of elevated serum lactate levels with the in-hospital mortality rate among emergency department patients.
Conclusion:
These findings suggest that even a moderately raised lactate level in serum can predict the severe outcome in emergency department patients suffering from different conditions. Therefore, early (at the time of administration of hospital) and periodic serum lactate value determination through different techniques and scores is of need and should become part of routine analyses in emergency department to predict and choose therapies that could benefit critically ill patients.
Keywords: Serum lactate, emergency patients, mortality, sepsis, trauma
Introduction
In healthy persons, lactate synthesis and metabolism take place continuously in the brain, stomach, skeletal muscle, and erythrocytes to make sure that blood lactate levels remain around 1 mmol/L.1 In a normal situation, aerobic metabolism transforms pyruvate into ATP molecules by the citric acid cycle. The process is aided by the enzyme pyruvate dehydrogenase, oxygen, glucose, and functional mitochondria. However, when oxygen levels are low anaerobic metabolism get unable to convert pyruvate to Acetyl-CoA by the citric acid cycle. Instead, the enzyme lactate dehydrogenase (LDH) converts pyruvate to lactate, producing two Adenosine Triphosphate (ATP) and lactate molecules.2 Although the lactate shuttle theory also reports the continuous synthesis and consumption of lactate in many cells under both anaerobic and aerobic situations.3
In addition, when lactate level surpasses the clearance mechanism of the body or when clearance metabolism declines or both occur alongside, hyperlactatemia arises.4 Hyperlactatemia can be caused by illnesses associated with raised catecholamine levels, such as asthma, sepsis, shock, trauma, or pheochromocytoma, which cause abnormally increased glycolysis primarily in the muscles to gain energy more quickly. Other etiologies or contributing causes to hyperlactatemia include medicines that inhibit oxidative phosphorylation or acute fulminant liver disease or liver failure that dysfunction lactate removal metabolism.5
Currently, research also suggests that augmented serum lactate level can prognosticate a high risk of mortality, vasopressor requirement, and mechanical ventilation which can lead to intensive care unit (ICU) admission.6 Moreover, even a moderate level of initial lactate in serum indicates shock and organ dysfunction in acute sepsis conditions,7 while elevated lactate levels indicate the complications progression and high death rate in patients with trauma,8 multiple organ failures,9 severe infections (all ages),7,10 cancer,11 and COVID-19 infections.12
Therefore, lactate-guided therapies during the first stage of resuscitation of critically ill patients have lately been presented as a powerful tool for treatment and care.13,14 Although the cutoff lactate levels and lactate clearance varied, lactate-guided resuscitation therapies resulted in a significant reduction in fatality rates when compared to the resuscitation process that was conducted without lactate level monitoring.15 Furthermore, an early percentage decrease of lactate is reported to bring improved outcomes in septic shock patients.16 Likewise, the use of thiamine amino acid in septic shock patients within 24 h hospital administration helps in lactate clearance and reduces the 28-day mortality rate.17 In another large-scale study, an increase in mortality up to ⩾60% was reported because lactate clearance from serum takes more time. However, the study also states that after 6 h of hospital administration, the initial lactate test and lactate clearance test from serum can also independently predict trauma patients’ mortality.18 To summarize, according to a classic study, elevated lactate is considered as a biomarker for identifying critically ill patients in ICU and can predict 100% mortality at >13.3 mmol/L or 120 mg/dL lactate levels.19 However, recent studies showed >2.0–2.5 mmol/L serum lactate level as a predictor for 30-day in-hospital mortality in patients who arrived at the emergency department (ED) and get hospitalized.20–22
Lately, lactate level measurement in serum by using different scores has been examined as a tool for predicting the outcome of emergency patients for accuracy. The study revealed that the combination of different techniques under multiple variables had delivered more precision in predicting mortality rate than the simple lactate level measurements.23 With this knowledge in hand, this systematic analysis correlates the serum lactate level and mortality rate/risk in ED patients, irrespective of the kind of illness or degree of care they are receiving.
Methodology
Study design
This systematic review investigated the predictive role of lactate measurements for mortality in critically ill patients admitted to hospitals’ ED. The data were collected according to set inclusion and exclusion criteria and are represented by following the PRISMA guidelines for systematic reviews.24,25
Data collection
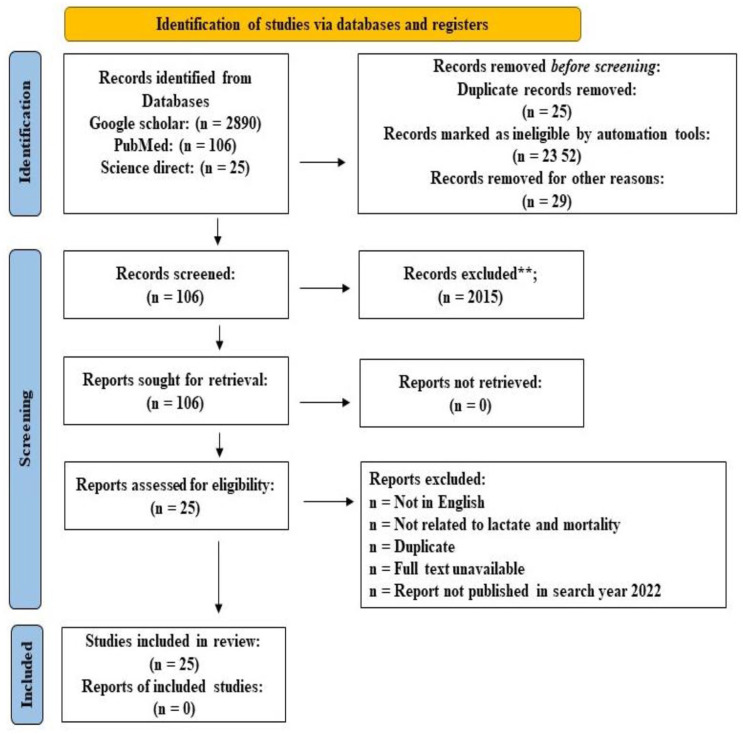
The literature search was conducted with help of renowned search databases, that is, Science Direct, PubMed, Google Scholar, and Web of Science. The databases were searched for literature published in the year 2022 for original articles, case reports, and reviews using the following web terms: lactate, emergency department, mortality, trauma, lactic infections, lactate rate, shock, hyperlactatemia, lactate clearance, and organ failure. Figure 1 illustrates the followed research methodology for data collection.
Figure 1.
Flow diagram of research methodology.
Data inclusion and exclusion criteria
Most recent research on the ED patients who are diagnosed with trauma, sepsis, or other conditions is included in this research. Likewise, research that is not based on the ED of the hospital is also included (i.e. trauma unit, ICU, and operating room). The death rate in hospitalized ED patients with respect to time and their lactate cutoff readings remains of significant interest during the database search. However, after evaluating the titles and abstracts, 25 relevant publications were selected. On basis of the condition of patients; find literature is classified into different sections representing patients with sepsis, patients with trauma, patients undergoing surgeries, patients with cardiac conditions, patients with COVID-19, and others.
Results
Sepsis patients
For 2 decades, sepsis is recognized as one of the most common and lethal conditions for patients with a high mortality rate.26 Recently, various scores based on serum lactate levels have been used frequently to predict in-hospital mortality in ED patients suffering from sepsis. In this regard, Hu et al. used modified, lactate-enhanced, and procalcitonin (PCT)-enhanced versions of the quick sequential organ failure assessment (qSOFA) for mortality rate determination in sepsis patients (n = 936). In predicting in-hospital mortality, the lactate-enhanced qSOFA and modified qSOFA outperformed the qSOFA with the area under the curve (AUC) of 0.740 and 0.731, a sensitivity of 64.36% and 51.40%, and a specificity of 70.78% and 80.96%, respectively.27 Similarly, Guarino et al. used qSOFA, MqSOFA along with lactate assay, and national early warning score (NEWS) to analyze data of sepsis and septic shock patients (n = 556). The author found that MqSOFA, NEWS, and lactate assay scores are more significant predictors of in-hospital mortality than qSOFA, with p < 0.001. However, the NEWS advantage over all other techniques in predicting fatal outcomes was demonstrated by cause-based classification, which included urinary, respiratory, abdominal, mixed, and unknown causes. Also, after Bonferroni’s correction, MqSOFA outperformed qSOFA in respiratory and urinary etiologies.28 Another study determined the detection rate of PCT, sequential organ failure assessment (SOFA), and qSOFA in estimating sepsis and in-hospital mortality in 65-year-old patients referred to the ED. It was found that the PCT test possesses a higher prognostic and predictive capacity for the diagnosis of sepsis than qSOFA and SOFA, with AUC = 0.883 at 95% confidence interval (CI): 0.835–0.931 and p < 0.0001. In addition, the sensitivity and specificity of the PCT test were 71.8% and 89.1%, respectively, at 95% CI (62.36–81.39 and 81.87%–96.45%). For in-hospital mortality, 2 mmol/L of lactate and 0.5 ng/mL of PCT have been reported as cutoff values. Overall, this study also suggests that qSOFA has a poor performance to diagnose sepsis and in-hospital mortality.29
Moreover, lactate rates, the lactate–albumin difference (LAD), and SOFA scores have been assessed for critically ill sepsis patients on hospital arrival, in-hospital mortality, and 90-day survival to evaluate the prognostic performance of the applied test. The report demonstrated the AUC value for predicting LAD mortality was 0.691 (95% CI: 0.663–0.718), lactate was 0.675 (95% CI: 0.646–0.703), and SOFA was 0.716 (95% CI: 0.663–0.718). However, the authors believe that 0.7 seems to be the best threshold for LAD, mentioning its ease of calculation in comparison with SOFA. Furthermore, LAD outperformed maximum lactate levels in terms of predicting in-hospital death and 90-day survival. Overall 20.3% in-hospital mortality rate was noted among patients (n = 2270).30
In the ICU, sepsis is common and subsequently leads to renal failure. A retrospective assessment was conducted on sepsis-related acute kidney injury (AKI) patients (n = 157) receiving continuous renal replacement therapy (CRRT) with a 28-day morbidity endpoint using the public database MIMIC-III. The results revealed that CRRT raises the log(lactate) by 0.041. The joint model also demonstrated a stable relationship between variations in lactate levels and event outcomes, indicating that a one-unit increase in log(lactate) increases the likelihood of 28-day fatality by 2.12. As a result, when offering renal support to a patient with sepsis-related AKI, lactate-control therapies must be given special consideration.31
In a separate study, the relationship between death and initial high blood lactate levels and positive fluid balance 24 h was investigated after admission of children to the pediatric ICU with sepsis and/or septic shock. According to the investigation, children who had leukopenia, an abnormal international normalized ratio, neurologic failure, initial blood lactate >5 mmol/L, mechanical ventilation (p < 0.03), or positive fluid balance (p < 0.001) within 24 h of being admitted to the pediatric ICU had a significantly higher mortality rate.32
Trauma patients
AKI following trauma is related to a longer hospital stay and an increased risk of death. Nasu, Toru, and coworkers verify systolic blood pressure (SBP) and arterial lactate level as predictors of freshly developed AKI after trauma. In the given study, AKI was defined in terms of injury, risk, failure, end-stage kidney disease, and loss of kidney function, based on serum creatinine levels. Patients in the high-risk group had pre-hospital SBP of ⩽126 mmHg and lactate levels of ⩾2.5 mmol/L. The incidence of severe AKI in set injury and failure was significantly higher in the high-risk group, with a 7.75 odds ratio (OR) at 95% CI: 2.33–25.77. As a result, early recognition of high-risk groups for serious AKI following trauma, as well as prompt treatment, may help trauma patients have a better outcome.33
In addition, the clinical value of the lactate-to-albumin ratio (LAR) as a predictor of multiple organ dysfunction syndromes (MODS) and the 30-day mortality rate were determined in patients admitted to the ED with severe trauma (Injury Severity Score ⩾ 16). The results suggest that the rise in the LAR at admission (OR = 1.618, p = 0.028) had been an independent prognosticator of MODS progress. Harrell’s C-index and AUC (0.783, 0.755) demonstrated that LAR could predict MODS and 30-day mortality.34
Until now, LAR scores have not been linked to the prognosis of burned patients’ mortality. In this regard, Dudoignon et al. published a retrospective cohort analysis involving burn patients admitted to the ICU. LAR levels at admission >0.13 were independently linked with 28-day mortality in multivariate analysis accounting for abbreviated burn severity index (ABSI) with OR = 3.98 at 95% CI: 1.88–8.35. Moreover, at p < 0.05, the ability of LAR at admission to distinguish 28-day mortality had 0.81 AUC value at 95% CI: 0.74–0.88, similar to AUC values of SOFA (0.80 at 95% CI: 0.72–0.85) and ABSI (0.85 at 95% CI: 0.80–0.90). The data reveal that a LAR value ⩾0.13 at admission is a simple and reliable measure that is independently related to 28-day mortality for patients with severe burns, but that LAR prediction does not quite perform better than alone lactate level.35
Wang et al. evaluate the value of the Glasgow Coma Scale, blood glucose, LAR, subdural hematoma, intra-parenchymal hemorrhage, and diffuse axonal damage value for mortality prediction in clinical data of moderate-to-severe traumatic brain injury patients (n = 273). The prognostic model was also built using these independent variables. The AUC values for individual lactate, albumin, and LAR were found to be 0.733, 0.740, and 0.780 at 95% CI (0.673–0.794, 0.683–0.797, and 0.725–0.835), respectively. However, the prognostic model had a greater AUC of 0.857 at 95% CI: 0.812–0.901 than LAR (Z = 2.1250, p < 0.05). The study suggests that clinicians can use a prognostic model that includes LAR to assess the probable progression and determine therapy decisions in traumatic brain injury patients.36
Surgical patients
In type, acute aortic dissection; ischemia, and mal-perfusion are major predictors of poor postoperative outcomes, and blood lactate seems to be an effective substitute point-of-care marker of mal-perfusion. As a result, Gemelli et al. investigated the relationship between lactate, in-hospital outcomes, and 1-year survival after type A acute aortic dissection surgery. The authors collected serum lactate values from 128 patients 3 times at p < 0 .01. The results displayed the preoperative, operative, and postoperative; OR = 1.52 at 95% CI: 1.17–2.07, cardiopulmonary bypass completion, OR = 1.34 at 95% CI (1.14–1.64), and 6 h after ICU admission OR = 1.29 at 95% CI: 1.08–1.55. Complications were more common in the raised lactate patient (>2.2 mmol/L), particularly hemofiltration. However, normal and elevated lactate groups have the same 1-year survival rate (p = 0.23). Furthermore, lactate remained a strong predictor of in-hospital mortality at all three-time time points, regardless of Penn Classification status upon admission.37
Kofler et al. studied the perioperative mortality in patients who are going for surgical repair for acute type A aortic dissection. The mortality rate was predicted by a laboratory-based risk score construct with lactates and four other parameters, that is aspartate aminotransferase, alanine aminotransferase, creatinine, and bilirubin values. According to the calculated mortality score, patients (n = 632) were assigned to groups having low (<7), moderate (7–20), and high (>20) risk with a perioperative mortality rate of 8%, 10%, and 24% (p < 0.0001). The laboratory-based risk score revealed an AUC = 0.69 with suitable adjustment. In addition, the multivariable study revealed an independent association with perioperative mortality having OR = 1.509 at 95% CI: 1.042–2.185. Overall, the newly suggested risk score provides doctors with a useful and accurate tool for improving the preoperative risk analysis of patients with acute type A aortic dissection established on easily available and widely obtainable laboratory data.38
Patient with respiratory tract infection
Lee et al. confirm the importance of the LDH to albumin ratio as a reliable marker of mortality in the ED patient having lower respiratory tract infection. The result suggests that LDH/albumin ratio had a larger AUC = 0.808 at 95% CI: 0.757–0.842 and p < 0.001 than albumin-based ratios (C-reactive protein to albumin ratio and LAR), except for blood urea nitrogen/albumin ratio, or severity scales (pneumonia severity index, CURB-65, and modified early warning scores).39
Cardiac patient
For elderly patients hospitalized in the ICU with severe community-acquired pneumonia, myocardial injury can be predicted by LAR. The patients with myocardial injury showed high neutrophil/lymphocyte ratio, neutrophil count, lactate, serum creatinine, and LAR values with a significantly raised mortality rate than the non-myocardial injury patients. Moreover, the author found that the AUC of LAR was 0.737 at 95% CI: 0.620–0.834, with a 1.21 cutoff value, 60.00% sensitivity, and 78.72% specificity, respectively.40
Hsu et al. predicted in-hospital cardiac arrest by evaluating the data retrieved over 7 years in 342 patients admitted to ED. The patient initial serum lactate levels were grouped into normal, moderately, and highly elevated categories on basis of ⩽2 mmol/L, 2 < lactate ⩽ 4, and >4 mmol/L concentrations. The results show that through multivariable analysis, the group with highly raised lactate had an 18-fold augmented risk of having in-hospital cardiac arrest with OR = 18.0 at 95% CI: 11.5–28.2. Moreover, the study also report that the poor lactate-clearance group of patients (<2.5%/h) showed a 7.5-fold higher risk of in-hospital cardiac arrest with OR = 7.5 at 95% CI: 3.7–15.1.41 Moreover, M. Azad and colleagues enrolled 100 patients in their study who had had heart surgery with cardiopulmonary bypass and also reported that ⩾3 mmol/L blood lactate level after 6 h in critical care indicates poor conditions in adult patients.42
COVID-19 infection
LDH is a high-precision biomarker for predicting in-hospital death in COVID-19 patients who are severely ill. Therefore, physicians worldwide have been directed to do the LDH determination to select aids for patients at high risk and to execute more therapies at an earlier stage to save patients’ lives.43 For this purpose, in the reported research, COVID-19 patients (n = 203) LDH serum levels were determined at the time of admission. The author discovered that LDH serum levels of 277.00 U/L as a cutoff value with 58.7% sensitivity and 82.0% specificity for predicting COVID-19 infection severity in patients. In addition, 359.50 U/L cutoff value of the serum LDH levels having 93.8% sensitivity and 88.2% specificity was established for predicting death in COVID-19 patients.44 In another study, lactate and related kinetics measures are beneficial for predicting outcomes in COVID-19-affected critically ill elderly patients (n = 2860). It was reported that 68% of the patient’s serum lactate was <2 mmol/L. However, raised serum lactate was linked with a very high rate of ICU admission and 3-month mortality.45 Moreover, a cohort study was developed to predict conventional oxygen therapy failure by calculating lactate, oxygenation, and temperature (LOT) score in COVID-19 patients. It was found that substantially increased 30-day mortality and conventional oxygen therapy failure arose when the developed score cutoff value reached >5.46
Lactate level in other conditions
In the given study, the MIMIC-IV database was used in another study to investigate the potential of arterial blood lactic acid levels to predict fatality within 28 days of the arrival of severe acute pancreatitis patients in the ICU. Results revealed that patients who died had a high lactic acid concentration in arterial blood within 28 days than surviving patients (p < 0.05). In an adjusted multivariate Cox regression analysis, lactic acid concentration independently predicts all-cause mortality within 28 days of hospitalization with HR = 1.22 at 95% CI: 1.09–1.36, p < 0.001, and area under the ROC curve = 0.741. Moreover, Kaplan–Meier analysis also showed a significance of p < 0.0001 in patients with high lactic acid concentration and raised mortality rate within 28 days. However, there was no significant relationship found between lactic acid concentration and other covariates in all-cause mortality within 28 days of admission (all p > 0.05) in subgroup analysis.47
Gupta, Manoj, and colleagues conducted an observational retrospective cohort study on 163 patients with severe dengue. Basic arterial blood gas parameters, such as pH, bicarbonate, partial pressure of O2 and CO2, and lactate levels, have been evaluated for mortality prediction by comparing values for the survivor and non-survivor dengue patients. On ROC analysis, lactate is the optimum prognostic marker, with an AUC of 88.7% with higher significantly (p < 0.0001) levels other than PCO2 (p = 0.002).48 On the contrary, Dundar, Z.D. report that combining lactate level testing with other physiological measures, notably NEWS, improves the predictive efficacy of tested parameters. Therefore, corresponding lactate levels and NEWS findings are regarded as low-accuracy prognosticators of mortality in severely ill geriatric patients.49
Kim et al. investigated the efficacy of pre-extracorporeal membrane oxygenation (ECMO) lactate in predicting 6-month mortality in patients with acute coronary syndrome having extracorporeal membrane oxygenation. The pre-ECMO lactate level was an independent predictor of 6-month mortality (HR = 1.210, 95% CI: 1.064–1.376, p = 0.004), as Cox regression analysis showed, while pre-ECMO lactate AUC at 95% CI: 0.56–0.72 and p = 0.002 was found to be 0.64. Furthermore, Kaplan–Meier survival analysis revealed that patients having a pre-ECMO lactate level cutoff value of 9.8 mmol/L had a substantially better survival rate at 6 months.50 A study identified arterial cutoff lactate level >1.7 mmol/L as a marker for the rising risk of postoperative complications in the neck and head surgery with 65.38% sensitivity and 66.67% specificity.51
Discussion
In the ED, the physician’s purpose is to rapidly and accurately diagnose the severity of a patient’s condition so that proper treatment can be administered. Therefore, this study pays close attention to the association and prognostic cutoff values of blood lactate, lactic acid, and LDH on different disease outcomes, by systematically reviewing recently published studies in 2022. Practically, every study found a strong link between lactate levels and mortality risk in patients with heterogeneous conditions (Table 1). However, for accuracy in diagnosis, various scores and ratios, such as qSOFA, NEWS, and LAR, are now being used instead of just serum lactate determination.
Table 1.
Summary of selected article in review.
| S. No | Author | Study design | Condition | Outcome |
|---|---|---|---|---|
| 1 | Hu et al.27 | Retrospective observational analysis | Sepsis | Lactate-enhanced qSOFA and MqSOFA have greater in-hospital mortality prediction rate |
| 2 | Guarino et al.28 | Retrospective analysis | Sepsis | MqSOFA, NEWS, and lactate assay scores are more significant predictors of in-hospital mortality than qSOFA |
| 3 | Jaramillo and Pinilla29 | Historical cohort analysis | Sepsis | In the elderly population, qSOFA offer low sepsis diagnostic performance. In-hospital mortality determination of other parameter such as PCT and lactate is also needed |
| 4 | Altun et al.30 | Retrospective analysis | Sepsis | The prognostic LAD performance was better for predicting in-hospital mortality and 90-day survival in adult sepsis patients because of ease in calculability |
| 5 | Wang et al.31 | Retrospective analysis | Sepsis-related AKI | Stable relationship between variations in lactate levels and event outcomes indicates that one-unit rise in log(lactate) increases the likelihood of 28-day fatality by 2.12 |
| 6 | Al-Eyadhy et al.32 | Retrospective analysis | Sepsis and/or septic shock | Children with initial blood lactate >5 mmol/L, along with other conditions, have a higher risk of mortality |
| 7 | Nasu et al.33 | Prospective review | AKI | Patients in the high-risk group had pre-hospital SBP of ⩽126 mmHg and lactate levels of ⩾2.5 mmol/L. |
| 8 | Han et al.34 | Retrospective observational analysis | Multiple organ dysfunction syndrome | LAR could predict multiple organ dysfunction syndrome and 30-day mortality |
| 9 | Dudoignon et al.35 | Retrospective cohort analysis | Burn patient | LAR at admission can distinguish 28-day mortality and had similar AUC values of SOFA and ABSI. Still, LAR prediction does not quite perform better than lactate level alone |
| 10 | Wang et al.36 | Multivariate logistic regression analyses | Severe traumatic brain injury | Non-survivors had higher LAR than survivor. Clinicians can use a prognostic model that includes LAR to assess the progression and determine therapy decisions |
| 11 | Gemelli et al.37 | — | Type A acute aortic dissection | Complications were more common in the raised lactate. Lactate remained a strong predictor of in-hospital mortality at all preoperative, operative, and postoperative points |
| 12 | Kofler et al.38 | Multivariable regression analysis | Surgical repair for acute type A aortic dissection | With laboratory-based risk score construct with lactates and parameters, doctors can accurate analyses the preoperative risks |
| 13 | Lee et al.39 | Multivariable logistic regression | Lower respiratory tract infection | In patients experiencing lower respiratory tract infections, the LDH/ALB ratio may function as an independent predictive indicator for in-hospital mortality |
| 14 | Zhang et al.40 | — | Myocardial injury | In elderly patients with severe community-acquired pneumonia, LAR has a strong predictive value for myocardial damage |
| 15 | Hsu et al.41 | Multivariable analysis | In-hospital cardiac arrest | Elevated lactate levels and inadequate lactate clearance were substantially linked to an increased risk of cardiac arrest in the hospital |
| 16 | Azad et al.42 | Prospective observational study | Heart surgery with cardiopulmonary bypass | High blood lactate level is an independent predictor for worse outcomes in adult patients after cardiac surgery under cardiopulmonary bypass |
| 17 | Dong et al.43 | Single-center retrospective study | COVID-19 | LDH is a predictive biomarker with great accuracy for the prediction of in-hospital mortality in COVID-19 patients |
| 18 | Li et al.44 | Case–control study | COVID-19 | An elevated LDH level at admission is a distinct risk factor for COVID-19 severity and mortality |
| 19 | Bruno et al.45 | Prospective international observation study | COVID-19 | Lactate and its kinetics are useful tools for predicting prognosis in critically ill elderly ICU patients with COVID-19 |
| 20 | Fridman et al.46 | Monocentric cohort study | COVID-19 | High chance of treatment failures and 30-day mortality rate is noticed when lactate, oxygenation, and temperature score is >5 |
| 21 | Wu et al.47 | Retrospective analysis | Severe acute pancreatitis | Patient who died showed a higher lactic acid content in their arterial blood after 28 days than patients who survived. |
| 22 | Gupta et al.48 | Retrospective cohort study | Dengue | In patients with severe dengue, basic arterial blood gas measurements and lactate can be employed as viable prognostic indicators for mortality. |
| 23 | Dundar et al.49 | Retrospective observational study | Critically ill geriatric patients | ED admission lactate level and NEWS are low-accuracy predictors of in-hospital mortality in critically ill geriatric patients. |
| 24 | Kim et al.50 | — | Acute coronary syndrome | In ACS patients having veno-arterial ECMO, a pre-ECMO lactate of 9.8 mmol/L or fewer may indicate a positive prognosis at 6 months. |
| 25 | de Souza et al.51 | Prospective cohort study | Head and neck squamous cell carcinoma | In patients with head and neck squamous cell carcinoma, arterial lactate assessed on the initial postoperative day is a strong predictor of postoperative problems. |
LAD: lactate–albumin difference; SBP: systolic blood pressure; LAR: lactate-to-albumin ratio; AUC: area under the curve; SOFA: sequential organ failure assessment; ABSI: abbreviated burn severity index; LDH: elevated lactate dehydrogenase; ICU: intensive care unit; ACS: Acute coronary syndrome; and ED: emergency department.
Since lactate calculation in the ED is linked to clinical conditions and requirements such as multi-organ failure, injury severity, respiratory problems, hospital stay, emergency operations, mechanical ventilation, and ICU admission, therefore early (at the time of administration of hospital) and periodic (after few hours) lactate level measurements is recommended by all reported studies so that severity of patients can be determined and on basis of that therapies could be recommended for benefit of the patient. Moreover, most studies show that serum lactate determination can become a standard assessment and recommend approximately ⩽2.0 mmol/L lactate levels as the cutoff value for predicting mortality in different conditions.
Limitation
Even though our search was broad and included medical libraries and other published literature, still some findings may get overlooked causing limitations in concluding the role of lactate in the prediction of in-hospital mortality. Furthermore, meta-analysis research would not have been appropriate in this situation due to considerable methodology differences between investigations, as it restricts the understanding of any mutual results. Finally, the quality of the existing literature limits a systematic review outcome, and any selection bias or different treatment for patients could have influenced our findings and reported fatality rates.
Conclusion
These findings suggest that even a moderately raised lactate level in serum can predict the severe outcome in patients under different conditions; thus, clinicians should consider early surveillance of lactate levels for the prognosis of patient condition.
Acknowledgments
The author is thankful to the department of emergency medicine, King Abdul Aziz University, Saudi Arabia, for the continuous support of this review article.
Footnotes
Author’s note: The author has approved the final article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Safinaz M Alshiakh  https://orcid.org/0000-0003-3656-1048
https://orcid.org/0000-0003-3656-1048
References
- 1. Nichol AD, Egi M, Pettila V, et al. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care 2010; 14(1): R25–R29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Juneja D, Singh O, Dang R. Admission hyperlactatemia: causes, incidence, and impact on outcome of patients admitted in a general medical intensive care unit. J Crit Care 2011; 26(3): 316–320. [DOI] [PubMed] [Google Scholar]
- 3. Brooks G. Lactate production under fully aerobic conditions: the lactate shuttle during rest and exercise. Fed Proc 1986; 45: 2924–2929. [PubMed] [Google Scholar]
- 4. Ryoo SM, Kim WY. Clinical applications of lactate testing in patients with sepsis and septic shock. J Emerg Crit Care Med 2018; 2: 14. [Google Scholar]
- 5. Ferreruela M, Raurich JM, Ayestarán I, et al. Hyperlactatemia in ICU patients: incidence, causes and associated mortality. J Crit Care 2017; 42: 200–205. [DOI] [PubMed] [Google Scholar]
- 6. Azevedo LC, Park M, Salluh JI, et al. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study 2013; 17: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med 2009; 37(5): 1670–1677. [DOI] [PubMed] [Google Scholar]
- 8. Freitas AD, Franzon O. Lactate as predictor of mortality in polytrauma. Arq Bras Cir Dig 2015; 28(3): 163–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bakker J, Gris P, Coffernils M, et al. Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg 1996; 171(2): 221–226. [DOI] [PubMed] [Google Scholar]
- 10. Del Portal DA, Shofer F, Mikkelsen ME, et al. Emergency department lactate is associated with mortality in older adults admitted with and without infections. Acad Emerg Med 2010; 17(3): 260–268. [DOI] [PubMed] [Google Scholar]
- 11. Maher SA, Temkit M, Buras MR, et al. Serum lactate and mortality in emergency department patients with cancer. West J Emerg Med 2018; 19(5): 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heldt FS, Vizcaychipi MP, Peacock S, et al. Early risk assessment for COVID-19 patients from emergency department data using machine learning 2021; 11: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial 2010; 182: 752–761. [DOI] [PubMed] [Google Scholar]
- 14. Van den Nouland DP, Brouwers MC, Stassen PM. Prognostic value of plasma lactate levels in a retrospective cohort presenting at a university hospital emergency department. BMJ Open 2017; 7: e011450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017; 43: 304–377. [DOI] [PubMed] [Google Scholar]
- 16. Nguyen HB, Rivers EP, Knoblich BP, et al. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 2004; 32(8): 1637–1642. [DOI] [PubMed] [Google Scholar]
- 17. Woolum JA, Abner EL, Kelly A, et al. Effect of thiamine administration on lactate clearance and mortality in patients with septic shock. Crit Care Med 2018; 46(11): 1747–1752. [DOI] [PubMed] [Google Scholar]
- 18. Odom SR, Howell MD, Silva GS, et al. Lactate clearance as a predictor of mortality in trauma patients. J Trauma Acute Care Surg 2013; 74(4): 999–1004. [DOI] [PubMed] [Google Scholar]
- 19. Peretz DI, Scott HM, Duff J, et al. The significance of lacticacidemia in the shock syndrome. Ann NY Acad Sci 1965; 119: 1133–1141. [DOI] [PubMed] [Google Scholar]
- 20. Park YJ, Kim DH, Kim SC, et al. Serum lactate upon emergency department arrival as a predictor of 30-day in-hospital mortality in an unselected population. PLoS ONE 2018; 13(1): e0190519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Godinjak A, Jusufovic S, Rama A, et al. Hyperlactatemia and the importance of repeated lactate measurements in critically ill patients. Med Arch 2017; 71(6): 404–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Filho RR, Rocha LL, Corrêa TD, et al. Blood lactate levels cutoff and mortality prediction in sepsis: time for a reappraisal. Shock 2016; 46(5): 480–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jo S, Yoon J, Lee JB, et al. Predictive value of the National Early Warning Score–Lactate for mortality and the need for critical care among general emergency department patients. J Crit Care 2016; 36: 60–68. [DOI] [PubMed] [Google Scholar]
- 24. Vincent J-L, Quintairos e, Silva A, Couto L, et al. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care 2016; 20: 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Selçuk AA. A guide for systematic reviews: PRISMA. Turk Arch Otorhinolaryngol 2019; 57(1): 57–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kempker JA, Martin GS. A global accounting of sepsis. Lancet 2020; 395: 168–170. [DOI] [PubMed] [Google Scholar]
- 27. Hu H, Jiang JY, Yao N. Comparison of different versions of the quick sequential organ failure assessment for predicting in-hospital mortality of sepsis patients: a retrospective observational study. World J Emerg Med 2022; 13(2): 114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Guarino M, Perna B, De Giorgi A, et al. A 2-year retrospective analysis of the prognostic value of MqSOFA compared to lactate, NEWS and qSOFA in patients with sepsis. Infection 2022; 50(4): 941–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jaramillo GD, Pinilla MI. Quick sequential organ failure assessment, sequential organ failure assessment, and procalcitonin for early diagnosis and prediction of death in elderly patients with suspicion of sepsis in the emergency department, based on sepsis-3 definition. Gerontology 2022; 68(2): 171–180. [DOI] [PubMed] [Google Scholar]
- 30. Altun GT, Arslantas MK, Dincer PC, et al. Prognostic value of the lactate–albumin difference for predicting in-hospital mortality in critically ill patients with sepsis. Marmara Med J 2022; 35: 61–66. [Google Scholar]
- 31. Wang Z, Zhang L, Xu F, et al. The association between continuous renal replacement therapy as treatment for sepsis-associated acute kidney injury and trend of lactate trajectory as risk factor of 28-day mortality in intensive care units. BMC Emerg Med 2022; 22: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Al-Eyadhy A, Hasan G, Temsah M-H, et al. Initial fluid balance associated outcomes in children with severe sepsis and septic shock. Pediatr Emerg Care 2022; 38: e1112–e1117. [DOI] [PubMed] [Google Scholar]
- 33. Nasu T, Ueda K, Kawashima S, et al. Prediction of early acute kidney injury after trauma using prehospital systolic blood pressure and lactate levels: a prospective validation study. Injury 2022; 53(1): 81–85. [DOI] [PubMed] [Google Scholar]
- 34. Han S, Chung SP, Choa M, et al. The prognostic usefulness of the lactate/albumin ratio for predicting multiple organ dysfunction syndrome in severe trauma. J Korean Soc Emerg Med 2022; 33: 45–60. [Google Scholar]
- 35. Dudoignon E, Quennesson T, De Tymowski C, et al. Usefulness of lactate albumin ratio at admission to predict 28-day mortality in critically ill severely burned patients: a retrospective cohort study. Burns. Epub ahead of print 5 January 2022. DOI: 10.1016/j.burns.2022.01.003. [DOI] [PubMed] [Google Scholar]
- 36. Wang R, He M, Qu F, et al. Lactate albumin ratio is associated with mortality in patients with moderate to severe traumatic brain injury. Front Neurol 2022; 13: 662385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gemelli M, Di Tommaso E, Chivasso P, et al. Blood lactate predicts mortality after surgical repair of type A acute aortic dissection. J Card Surg 2022; 37(5): 1206–1211. [DOI] [PubMed] [Google Scholar]
- 38. Kofler M, Heck R, Seeber F, et al. Validation of a novel risk score to predict mortality after surgery for acute type A dissection. Eur J Cardiothorac Surg 2022; 61: 378–385. [DOI] [PubMed] [Google Scholar]
- 39. Lee BK, Ryu S, Oh SK, et al. Lactate dehydrogenase to albumin ratio as a prognostic factor in lower respiratory tract infection patients. Am J Emerg Med 2022; 52: 54–58. [DOI] [PubMed] [Google Scholar]
- 40. Zhang L, Li Y, Lv C, et al. Predictive value of arterial blood lactate/serum albumin ratio for myocardial injury in elderly patients with severe community-acquired pneumonia. Medicine 2022; 101: e28739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hsu S-H, Kao P-H, Lu T-C, et al. Serum lactate for predicting cardiac arrest in the emergency department. J Clin Med 2022; 11: 403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Azad M, Islam K, Quasem MJ. Evaluation of blood lactate level as predictor of early adverse outcome after cardiac surgery under cardiopulmonary bypass. Bangladesh Heart J 2019; 34: 25–30. [Google Scholar]
- 43. Dong X, Sun L, Li Y. Prognostic value of lactate dehydrogenase for in-hospital mortality in severe and critically ill patients with COVID-19. Int J Med Sci 2020; 17(14): 2225–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li C, Ye J, Chen Q, et al. Elevated lactate dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging 2020; 12: 15670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bruno RR, Wernly B, Flaatten H, et al. Lactate is associated with mortality in very old intensive care patients suffering from COVID-19: results from an international observational study of 2860 patients. Ann Intensive Care 2021; 11: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fridman SE, Di Giampietro P, Sensoli A, et al. Prediction of conventional oxygen therapy failure in COVID-19 patients with acute respiratory failure by assessing serum lactate concentration, PaO2/FiO2 ratio, and body temperature. Cureus 2022; 14(2): e21987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wu M, Shi L, Zhang H, et al. Predictive value of arterial blood lactic acid concentration on the risk of all-cause death within 28 days of admission in patients with severe acute pancreatitis. Postgrad Med 2022; 134: 210–216. [DOI] [PubMed] [Google Scholar]
- 48. Gupta M, Agrawal N, Sharma SK, et al. Study of utility of basic arterial blood gas parameters and lactate as prognostic markers in patients with severe dengue. Cureus 2022; 14(5): e24682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Dundar ZD, Kocak S, Girisgin AS. Lactate and NEWS-L are fair predictors of mortality in critically ill geriatric emergency department patients. Am J Emerg Med 2020; 38(2): 217–221. [DOI] [PubMed] [Google Scholar]
- 50. Kim E, Sodirzhon-Ugli NY, Do Wan Kim KSL, et al. Prediction of 6-month mortality using pre-extracorporeal membrane oxygenation lactate in patients with acute coronary syndrome undergoing veno-arterial-extracorporeal membrane oxygenation. J Chest Surg 2022; 55: 143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. De Souza SP, da Silva Serra MG, dos Santos Oliveira N, et al. Arterial lactate as a predictor of postoperative complications in head and neck squamous cell carcinoma. Epub ahead of print 6 May 2021. DOI: 10.1016/j.bjorl.2021.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]