Abstract
Introduction:
Iodine is one of the crucial micronutrients required for the normal growth of humans from the fetal stage to adulthood through the synthesis of thyroxin (t3) and triiodothyronine (t4) hormones in the thyroid gland for regulation of metabolism, protein synthesis, and brain development. This study aimed to assess iodine status, the impact of knowledge and practice for adequate iodized salt utilization in household levels in North West Ethiopia.
Method:
A population-based cross-sectional study was carried out using multistage sampling among 1398 residents from 28 December 2021 to 30 January 2022. A systematic random sampling technique was used to select the study participants. The collected data were entered into Epi-Data version 3.1 and then exported to STATA/R version 14 for further analysis. An adjusted odds ratio with 95% CI was used to declare statistical significance at p < 0.05.
Result:
The overall mean (±SD) age of participants was 34.9 (±12.8) years. About 678 (48.5%) had 15–80 ppm, 23 (1.6%) had >80 ppm, 533 (38.13%) had 1.1 ppm to 14.9 ppm, and 147 (10.5) had no iodine in salt (0 ppm) after assessed by Rapid Test Kit. Only 48.5% of the sampled household had used adequate iodized salt with ≥15 ppm. The overall burden of goiter was estimated at 11.4/1000 population. Adequate iodized salt utilization was significantly associated with having formal education (adjusted odds ratio = 1.89: 95% confidence interval: 1.4, 2.6, p = 0.001), monthly income ≥5000 ETB/month (adjusted odds ratio = 1.99: 95% confidence interval: 1.5, 2.9, p = 0.001), and good knowledge score (adjusted odds ratio = 1.6: 95% confidence interval: 1.12, 2.6, p = 0.03) were predictors for proper iodized salt utilization.
Conclusion:
Coverage of adequately iodized salt was low and respondents’ formal education, monthly income ≥5000 Ethiopian Birr/month, and good knowledge score were all significantly associated with proper iodized salt utilization. While the prevalence of goiter was not significantly identified as a public health problem as compared in the regions, however, in light of previous iodine deficiency in this region of Ethiopia, the salt iodization program should be done continually.
Keywords: Ethiopia, goiter, iodine, knowledge, practice, salt
Introduction
Iodine is an essential micronutrient in human nutrition and a proper amount is needed in the human diet to ensure good physical growth and neural development.1 When people do not have enough iodine, they cannot make enough thyroxin hormones (T3 and T4),2,3 which has 65% and 59% respective weight of iodine hormones produced from the thyroid gland.4 Human beings required iodine to sustain their regular metabolism, physical growth, and cognitive development. However, IDD with endemic goiters as its main clinical manifestation, brain damage, dwarfism, spontaneous miscarriages, and stillbirth may occur due to inadequate intake.3,4 Globally, nearly 2 billion people suffer from ID with around 50 million having clinical manifestations Children, and pregnant women are more vulnerable to developing ID, and approximately 266 million schoolchildren suffer from ID, with symptoms.4 ID results in goiter, mental retardation, or reduced cognitive function.3,5 Early screening of the iodine status of children is essential to prevent Iodine Deficiency Disorders (IDDs).6 Every year, in under-developing countries, almost 38 million newborns suffered from the enduring impact of neurological associated IDD.7 The mean intellectual Quotient scores are reduced to 13.5 due to iodine deficiency.3 The burden of ID varies from region to zonal levels, and the proportion of the population of school-age children with inadequate iodine (UIC < 100 μg/L) at the national level was found to be 43.4%.8
Global, 35 million people are at risk for IDD, among those 40% have contracted goiter (swelling of the thyroid gland) around the neck.9 The problem is worsening in African countries specifically in Ethiopia, more than 12 million school children suffered from IDD1 with 24.3% and 11.5% palpable and visible goiter respective burdens.1,10 ID-associated goiter is responsible for 24.3% and 11.5% burden of palpable and visible goiter in Ethiopia, respectively.10 The issue is dreadful and ranged for children ≤18 years 41.86% in Amhara regions.11–13 The universal iodized salt initiative recommended daily dose of iodine is based on age class, with 90 µg (RNI) for ≤15 years, and ≥250 µg for all pregnant.9,14 In 2011, Ethiopia was the first among the top ten iodine-deficient countries based on a national median UIC (20–49 μg/L)12 among 148 countries data the study included in the analysis.15
Recently, the practice of adequate iodized salt utilization has increased from 15% in 2011 to 25% in 2016.16 However, it had a significant variation among regions, as the highest reported was 55.2% in Tigray regions, and as lowest reported in Gambela was 9.5%.9,14,16 Despite the government of Ethiopia accepting the 90% universal iodized salt initiative strategy of WHO, through the implementation of universal food fortification, and dietary supplementations, however, only 26% of the households achieved using adequate iodized salt utilization.5,17 The presence of iodine in salt is not enough for preventing IDD. Proper and adequate utilization of iodized salt is necessary as iodine can be lost due to different cooking practices such as pressure cooking, boiling, and shallow frying.3
In 2014, Ethiopia was still one of the 25 most iodine-deficient countries, and only 19.9% of the population was reported to consume iodized household salt.18 Moreover, persistent and significant poverty, poor knowledge, and practice of iodized salt consumption at household levels were responsible for the low coverage at national levels. This study aimed to assess iodine status, and the impact of knowledge and practice for adequate iodized salt utilization at household levels in Debre Markos city, North West Ethiopia.
Objective
Assessing population levels’ knowledge and practice for adequate iodine salt utilization.
Determining levels of iodine concentration among iodine salt utilizer groups.
Assessing the burden of goiter among participants living in selected kebeles.
Methods
Study design, period, and setting
It was a population-based cross-sectional study conducted from 28 December 2021 to January 30, 2022. The town is located 300 km away from the national capital city of Ethiopia and 265 km away from Bahir Dare regional city of the Amhara region.19
Source of population and eligibility criteria
All residents in debre Mark’s (Menkorer) city were the source of the population for this study. Participants whose age was ≥15 years were sampled for an interview as study subjects and included for an interview whereas those who were age ≥15 years and medically ill, and unable to respond were excluded.
Sample size determination
The sample size was calculated based on the formula of z 2 p(1-p)/d2 to derive the minimum required sample size considering the 95% confidence level, a 4% margin of error (d), Preliminary proportions(P1) iodized salt usage 37% from,20 and adding 2.5 design effects for multistage sampling techniques. Eventually, a total sample size of 1398 was derived.
Sampling technique
A multistage with a three-stage sampling process was used to ensure the representation of all residents in Debre Markos Town. The kebeles were considered uniform in characteristics hence they were considered clusters. Six out of twelve total kebeles, the town has a total of 12 kebeles randomly selected by the lottery method, six out of 12 kebeles. Then, in the final stage, systematic random samplings were used to select the households from each selected Kebele by dividing the total household using the sample size interval (K = 3) as shown in Table 1.
Table 1.
Selected households and sampled population from six kebeles of Menkorer city.
| Data collected site | No of household | Sample interval | Sampled household | Sampled population |
|---|---|---|---|---|
| Kabel 01 | 699 | K = 3 | 233 | 233 |
| Kabel 04 | 689 | K = 3 | 229 | 229 |
| Kebel 05 | 726 | K = 3 | 242 | 242 |
| Kebele 08 | 681 | K = 3 | 227 | 227 |
| Kebel 09 | 672 | K = 3 | 234 | 224 |
| Kabel 11 | 702 | K = 3 | 234 | 234 |
| Total | 4269 HHs | K = 3 | 1398 | 1389 |
Variables
Adequate utilization of iodized salt was the dependent variable for this study. Information on the sociodemographic and economic characteristics, drinking water source, and information regarding the usage of iodized salt of the selected participants was obtained by a structured interviewer-administered questionnaire and was counted as independent variables of this study.
For knowledge-related items, the questions contained the category of (“Yes”/“No”). A correct answer was assigned “1” point and an incorrect answer was assigned a “0” point. The total item ranged from 1 to 9. “Good knowledge score” was when the scoring was 5.5 (50% and above) out of 9 items and a score below it indicated a “poor knowledge score” on iodized salt-related beneficiaries and IDDs. This is similar to practice-related items (N = 6). “Good practice score” was when the scoring was 5.5 (50% and above) out of 9 items and a score below it indicated a “poor practice score” on the iodized salt beneficiary and IDDs. The respondents who answered greater than or equal to the mean score listed items have individually experienced knowledge and good practice for iodized salt utilization.
The internal consistency reliability of knowledge and attitude items were checked on 16 pre-tested questionnaires giving a result of Cronbach’s alpha (α = 0.81) and (α = 0.72), respectively.
Operational words
Adequately iodized salt: When we tested the sample salt with the rapid iodine test kit if the iodine content of the household salt sample was ≥15 parts per million (ppm), a deep blue color change was seen and it is called an adequately iodized salt.1
Levels of iodine content determination
To obtain the dietary iodine intake, the 24-h dietary recall method was used with the help of a semi-quantitative Food Frequency Questionnaire as described elsewhere.4,18 The questionnaire was first prepared in English, then translated into the local language (Amharic), and finally, back-translated to English to maintain consistency. Quality assurance mechanisms included training the data collectors and supervisors about the objectives of the project and the data collection processes. Approximately 75–100 g of a salt sample was collected from the participants’ homes and kept in air-tight plastic containers. The samples were stored at room temperature, away from sunlight, until analysis was carried out. Samplings were done from the top, middle, and bottom of the pack bag/containers to ensure the representativeness of the sample by using a moisture-free, clean plastic container.2,21 Briefly, about 15 g of salt was dissolved in distilled water and made up to 50 mL solution. 1 mL of 2 N sulfuric acid and 5 mL 10% potassium iodide were added, which in the presence of iodine was turned yellow. The liberated iodine was titrated against 0.005 M sodium thiosulfate solution using 1 mL of 1% starch indicator near the end of the titration using the formula mg/kg (ppm) iodine = titration volume in mL × 21.15 × Normality of sodium thiosulfate × 1000/salt sample weighting.9,21
Clinical assessment
Two BSC health officer supervisors performed a clinical examination of the neck for goiter for all respondents after being ruled out by graduated BSc nurse data collectors. Goiter classification was done based on the WHO-recommended method.4 Based on that, 0 was graded for no palpable or visible goiter; 1 was graded for palpable, but not visible goiter when the neck is in the normal position; and 2 was graded if swelling in the neck, which is visible when the neck is in a normal position.
Data collection tools and quality controls
Data were collected by using a structured questionnaire interview. The questionnaire was adapted from previous studies in the area,16,21–23 and a 5%(N = 79) pretest was done in Emanuel woreda. The quality of the test kit was assured by internal and external quality control. Two-day data collection training was given to three BSC graduated nurses and two-health officers for the objectives of the study, variables of interest, and maintaining data confidentiality.
Statistical analysis
Questionnaires were checked and coded manually for completeness before being entered into Epi-Date Version 4.2, and then exported to STATA 14.0 for final analysis. Descriptive analysis results were presented in the form of tables, figures, and pie charts. Text using frequencies, and summery and summery statics such as mean (±SD), and percentages were used for final reports. The assumption of the logistic regression model was checked before fitting it to the model. A multivariable logistic regression model was used to assess determinants for proper iodized salt utilization at the household level. An adjusted odds ratio with 95% CI was used to declare statistical significance at p < 0.05.
Result
Sociodemographic characteristics of participants
In this study, 1389 respondents were included for the final analysis and made the overall response rate 99.4%. The majority of 968 (79.61%) of the respondents were female in gender, and 719 (59.13%) of them were married. The overall mean (±SD) age of the participants was found to be 35 (±15.5) years with 471 (33.6%) being found in age groups 26–36 years. During the interview, the majority of 991 (81.50%) respondents were orthodox followers, and ≥451 (37.1%) of them lived with ≥8 family members in a house as shown in Table 2.
Table 2.
Sociodemographic characteristics of respondents’ knowledge, the practice of iodized salt determination in Menkorer city, in North West Ethiopia.
| Characteristics | Categories | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 302 | 21.6 |
| Female | 1096 | 78.4 | |
| Age | ≤25 years | 322 | 23.03 |
| 26–35 | 471 | 33.69 | |
| 36–45 | 382 | 27.3 | |
| ≥46 years | 223 | 15.9 | |
| Marital status | Married | 816 | 58.1 |
| Never in union | 498 | 35.2 | |
| Divorced | 84 | 6.83 | |
| Educational status | Unable to read and write | 150 | 10.3 |
| Complete primary | 40 | 3.13 | |
| Complete high school | 211 | 15.2 | |
| Complete preparatory | 378 | 27.6 | |
| Diploma and above | 617 | 44.4 | |
| Religion | Orthodox | 971 | 79.8 |
| Muslim | 128 | 10.5 | |
| Others | 117 | 9.6 | |
| Occupation | Merchant | 461 | 33.22 |
| Farmer | 370 | 26.4 | |
| Employer | 346 | 24.59 | |
| Student | 221 | 15.7 | |
| Family size | ≤4 | 404 | 29.3 |
| 5–8 | 453 | 33.5 | |
| ≥8 | 451 | 37.1 | |
| TV watching | Yes | 310 | 25.5 |
| No | 906 | 74.5 | |
| Radio listening | Yes | 591 | 57.6 |
| No | 807 | 57.39 | |
| Economic status | ≤1000 ETB/M | 617 44.17 | 44.2 |
| 1000–5000 ETB/M | 375 26.84 | 26.8 | |
| ≥5000 ETB/M | 405 28.99 |
Knowledge of iodized salt utilization
Majority of 1182 (45.4%) participants heard about the importance of iodized salt but not 216 (15.4 %). Nearly two in every five, 522 (37.7%) participants were informed about adequate iodized salt utilization from mass media. More than 1076 (76.97%) respondents know more risk segment population for IDD when did not use adequate iodized salt as shown in Table 3.
Table 3.
Frequency distribution of knowledge status of respondents on iodized salt from 28 December 2021 to 30 January 30 2022.
| Characteristics | Categories | Frequency | Percent |
|---|---|---|---|
| Do you hear about iodized salt here before the importance of it | Yes | 1182 | 84.5 |
| No | 216 | 15.9 | |
| Is there any problem exposing iodized salt to sunlight | Yes | 291 | 20.8 |
| No | 1,107 | 79.2 | |
| Does exposure of iodized salt to moisture have a problem | Yes | 724 | 51.8 |
| No | 674 | 48.2 | |
| Is there any problem might have the washing of iodized salt before cooking | Yes | 917 | 66.5 |
| No | 463 | 33.5 | |
| Do you know goiter is one of the main causes of deficiency of iodine | No | 917 | 65.5 |
| Yes | 481 | 34.4 | |
| Do you know purchasing site for iodized salts | Yes | 1020 | 72.8 |
| No | 378 | 27.1 | |
| Do know animal foods and vegetables are the main sources of iodine | Yes | 1178 | 84.26 |
| No | 220 | 15.74 | |
| Do you know the risk population segment for IDD | Children | 1076 | 76.97 |
| Adult | 422 | 23.1 | |
| Where did you get source information for iodized salt? | I don’t know | 136 | 9.79 |
| School | 315 | 22.5 | |
| Health institution | 145 | 10.4 | |
| Mass media | 522 | 37.4 | |
| Friend | 256 | 18.3 | |
| Other | 23 | 1.65 | |
| Do you know the long-term complication of iodine deficiency | I don’t know | 410 | 29.33 |
| Abortion | 350 | 25.04 | |
| Cretinism | 309 | 22.1 | |
| Goiters | 279 | 19.9 | |
| Mental illness | 50 | 3.58 | |
| Knowledge score | Good knowledge | 879 | 62.88 |
| Poor Knowledge | 519 | 37.12 |
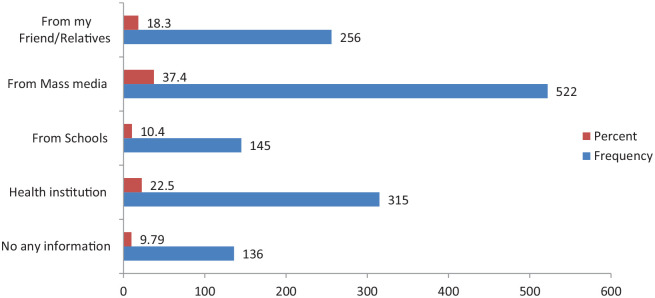
The overall good level of knowledge of participants about the usefulness of iodized salt and the health consequences of IDD was estimated at 879 (62.88%). Furthermore, nearly two in every five of the respondent had information about iodized salt from mass media, but 136 (9.7%) did not have any information about it as shown in Figure 1.
Figure 1.
Source of information about the importance of iodized salt consumption among respondents.
Practice-related questions
Nearly half of the participants 629 (44.99%) mentioned that the salt they were consuming in their homes was usually purchased from mini-shops (grocers) surrounding their homes, while about 380 (27.18%) and 389 (27.83%) of the participants were purchased from Bazar and market, respectively. Majority of 840 (60.1%) participants used iodized salt at the end of cooking dish. The largest proportion of 742 (53.08%) respondents stored their salt in closed containers. The mean practice of iodized salt utilization was found 775 (55.5%) as shown in Table 4.
Table 4.
Frequency distribution of practicing iodized salt utilization among respondents in Menkorer city.
| Characteristics | Categories | Frequency | Percent |
|---|---|---|---|
| How much-iodized salt is used daily | Always | 920 | 65.8 |
| Sometimes | 348 | 24.89 | |
| Never | 130 | 9.3 | |
| What types of salt did you use daily for your cooking dish? | Iodized salt | 858 | 61.8 |
| Common salt | 299 | 21.89 | |
| I don’t know | 241 | 17.3 | |
| Where do you buy iodized salt if you are a user? | Market | 629 | 49.9 |
| Bazar | 380 | 27.18 | |
| Mini-shop | 389 | 28.01 | |
| Where do you put your iodized salt | Packed items | 742 | 53.9 |
| Dry place | 314 | 22.5 | |
| In pastel | 24 | 23.5 | |
| When do you use iodized salt during cooking dish | At beginning | 558 | 39.89 |
| Last of cooking | 840 | 60.11 | |
| How much it is the perceived cost the iodized salt | Expensive | 611 | 43.7 |
| Cheap | 787 | 56.29 | |
| How long can you store the salt and possibly re-used | <2 month | 609 | 43.5 |
| >2 month | 789 | 56.4 | |
| Practice-related score | Good practice | 775 | 55.44 |
| Poor practice | 623 | 44.5 | |
| Iodine test through titrations of rapid test kits | Deep blue | 740 | 52.9 |
| Not colored | 658 | 47.1 |
Levels of iodine concentration from collected salts
About 678 (48.5%) had 15 –80 ppm, 23 (1.6%) had >80 ppm, 533 (38.13%) had 1.1 ppm to 14.9 ppm, and 147 (10.5) had no iodine in salt (0 ppm) after rapid test kit titrations salt sample (RTK). However, of the total, there were no 17 (1.22%) salt samples were not tested (less than 10 g) salt available in a house. The mean (±SD) iodine content of salt from collected Households was found to be 31.9 (±12.8) ppm as shown in Figure 2.
Figure 2.
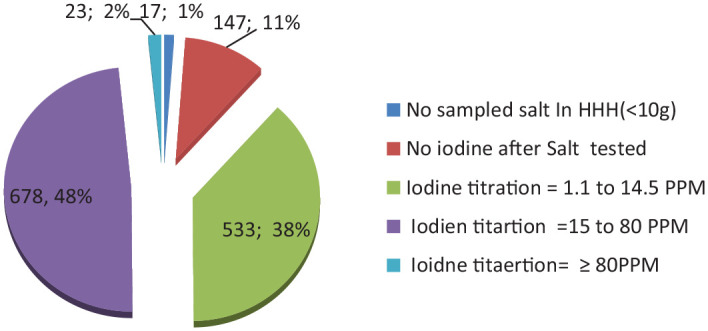
Levels of iodine concentration after sample d salt tested through RTK.
The health burden of a goiter on selected variables
Of the total respondents, 11.4 %(N = 160) (95% CI: 9.87, 13.22) participants had visible goiters. The majority, 118 (73.7%) of these cases were female in gender, and 50 (32.02%) were within ≤25 years of age group. Regarding poor-scored knowledge participants; nearly 8% of 105 (7.5%) had goiter, but doubled reduced this burden among good knowledge-scored participants. The overall grading of goiter was determined as grade 1 was 8.5% and that of grade 2 was 2.4%. The majority 128/160 (80.1%) of the cases did not use iodized salt as shown in Table 5.
Table 5.
Health-related IDD of goiter among residents in Menkorer city in North West Ethiopia.
| Variables | Categories | Burden of Goitre | χ2 | p Value | |
|---|---|---|---|---|---|
| Yes (N = 160) (%) | No (N = 1229) | ||||
| Sex | Male | 42 (3.01) | 1001 (71.6) | 1.47 | 0.94 |
| Female | 118 (8.5) | 237 (16.9) | |||
| Educational status | Formal education | 105 (7.5) | 908 (64.9) | 14.2 | 0.001 |
| No formal education | 57 (4.1) | 330 (23.6) | |||
| Knowledge score | Good Knowledge | 55 (3.8) | 890 (63.6) | 91.1 | 0.01 |
| Poor Knowledge | 105 (7.5) | 348 (24.8) | |||
| Practice score | Good practice | 75 (5.3) | 665 (47.56) | 83.2 | 0.01 |
| Poor practice | 85 (6.1) | 573 (40.9) | |||
| Iodized salt status | Adequate user group (≥15 ppm) | 32 (2.2) | 692 (49.4) | 73.4 | 0.02 |
| Inadequate user groups (≤14 ppm) | 128 (9.1) | 546 (39.1) | |||
Factors associated with adequate iodized salt utilization
Bivariate and multivariable logistic regression analysis was conducted. Finally the model of multivariable logistic regression, three variables were found significantly associated with adequate iodized salt utilization. Accordingly, formal education (AOR = 1.89; 95% CI: 1.4, 2.6, p = 0.001), Monthly income ≥5000 ETB/month (AOR = 1.99; 95% CI: 1.5, 2.9, p = 0.001), and good knowledge score (AOR = 1.6: 95% CI: 1.12, 2.6, p = 0.03) were significantly associated with adequate iodized salt utilization shown as in Table 6.
Table 6.
Bi-variable and multivariable logistic regression for adequate iodized salt utilization in Menkorer city, North West Ethiopia.
| Variable | Categories | Utilization of iodized salt | COR | AOR | p Value | |
|---|---|---|---|---|---|---|
| User | Non-user | |||||
| Sex | Male | 157 (11.2) | 122 (8.7) | Ref | Ref | |
| Female | 594 (42.4) | 525 (37.1) | 1.14 (0.76, 1.3) | 1.2 (0.79, 1.38) | 0.07 | |
| Age | ≤25 years | 240 (17.6) | 196 (14.1) | 1.1 (0.75, 1.4) | 1.17 (0.62, 1.34) | 0.14 |
| 26–35 | 175 (12.5) | 191 (13.6) | 1.2 (0.73, 1.8) | 1.4 (0.94, 1.7) | 0.25 | |
| 36–45 | 197 (14.1) | 139 (9.9) | 1.03 (0.87, 1.6) | 1.3 (0.82, 1.58) | 0.41 | |
| ≥46 year | 240 (17.5) | 121 (8.6) | Ref | Ref | ||
| Family size | ≤5 | 471 (33.6) | 412 (29.5) | 1.18 (0.75, 1.28) | 1.18 (0.75, 1.28) | 0.12 |
| >5 | 253 (18.1) | 262 (18.7) | Ref | Ref | ||
| Mass media attended | Yes | 535 (38.3) | 189 (13.5) | 1.2 (0.9, 1.5) | 1.16 (0.9,1.4) | 0.08 |
| No | 478 (34.2) | 196 (14.2) | Ref | Ref | ||
| Economic status | ≤1000 ETB | 378 (27.1) | 340 (24.3) | Ref | Ref | |
| 1000–5000 ETB | 238 (17.1) | 178 (12.7) | 1.19 (0.92, 1.54) | 1.29 (0.99, 1.6) | 0.05 | |
| ≥5000 ETB | 134 (9.5) | 129 (9.2) | 1.3 (0.9, 1.6) | 1.99 (1.5, 2.9) | 0.01* | |
| Education status | No formal education | 231 (16.5) | 173 (12.3) | Ref | Ref | |
| Had formal education | 520 (37.2) | 474 (33.9) | 1.56 (1.2, 1.9) | 1.8 (1.41, 2.32) | 0.01* | |
| Knowledge score | Good Knowledge | 487 (34.8) | 392 (28.04) | 1.5 (1.3, 2.7) | 1.6 (1.12, 2.6 | 0.03* |
| Poor knowledge | 264 (18.8) | 255 (18.2) | Ref | Ref | ||
| Practice score | Good practice | 428 (30.6) | 347 (24.3) | 1.4 (1.2, 1.8) | 1.02 (0.55, 1.6) | 0.41 |
| Poor practice | 323 (23.1) | 300 (21.4) | Ref | Ref | ||
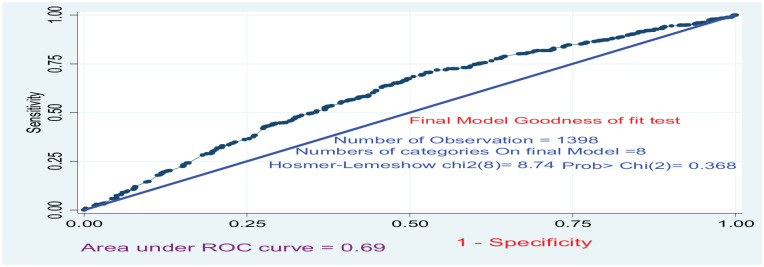
Model goodness of test
The overall goodness-of-fit test for final models of a multivariable logistic regressions model analysis was assessed using the area under the Roc-curve with the following given parameters as shown in the and it is fitted with Hosmer and Lemeshow test as shown in the Figure 3.
Figure 3.
Final model goodness-of-fit test.
Discussion
At the end of the study periods, 905 (64.74%) participants self-reported as they used always-adequate iodized salt at cooking. However, only 48.5% were confirmed with ≥15 ppm iodine content in their daily salt which self-reported as they always used adequate iodized salt utilization. Which is considerably lower than the WHO recommendation levels to be 90%,24 Pradesh Indian 48%,25 Mayhew district (59.7%),26 Dessie town 68.8%,20 Asella town 76.8% in 2016,27 Goba town 57.2%,28 Dega Damot 88.8%29 but higher than previous finding in 33.2% in Gondar,30 33.5% in Addis Ababa,16 and 25.7% in Ziway.26 This might be due to the difference in whether there was a problem in the identification of iodized salt during purchasing from the whole sellers, shops, and others where iodized salt was sold and the lower global and regional levels.10 In fact, in this report, more than 945 (67.6%) participants scored good knowledge about iodine-related beneficiaries but this was divergent from the study where 386 (27.61%) lacked iodized salt in their homes during the interview.
Concerning to health-related burden of goiter in the population was estimated as 11.4/1000. However, which is lower than the previous reported 50.7% North Shewa Zone,9 and 13.6% Hawassa Town.11 This difference might be due to the current improvement in the utilization of iodized salt compared to previously reported studies. On the other hand, the political and logistic problems in the production and distribution of iodized salt could be the main reason for poor regulatory agencies have attributed to inadequate iodized salt utilization and low attributable risk difference on iodized salt utilization.
Regarding the factors associated with adequate iodized salt utilization, the level of education is one factor that facilitates iodized salt utilization.31 Accordingly, participants who have formal education were 1.6 times more likely to use iodized salt as compared to those who did not attend formal education. This is consistent with the previous report on Hote district,32 Laelay Maychew in 2015, Woilata in 2018, Asella in 2016, Sudan in 2017, and Iraq in 2012.16,22,23,31,33,34 Public awareness is necessary for the demand of iodized salt utilization.
Likewise, respondents having a Monthly income ≥5000 ETB/month were nearly two times more likely to use adequate iodized salt as compared with respondents with a monthly income ≤1000 ETB/M. Previously reported studies to reveal that the unavailability (52.2%) of iodized salt is due to the high cost (32%) as the primary reason for not using iodized salt.
In some occasions, the frequent practice of cooking of food can motivate purchasing of iodized salt from shops or markets. This makes directly increased the availability of iodine in cooked food if the daily income did not matter it.
Consistent with previous studies’ reports3,32,35 respondents with good knowledge score had two times more likely to use iodized salt as compared with the counter group. This could be because educated respondents have learned and could read about the importance of iodized salt. In addition, the educated respondent might have the power to better access to mass media that motivates them to utilize iodized salt properly. A significant proportion of the population not used still iodized salt was doing so because of concerns about using it. The most reason for not using iodized salt in every household is the issue of inaccessibility and cost. Each of these barriers could be tacked if and only if edible salts were used in every household.
Limitations of the study
This study ignored knowledge of the whole household members’ iodine status and only interviewed one among them. This effect was ignored during the sample size calculation, and the cross-sectional study design restricts the factors to establish a causal relationship.
Conclusion
In this study, the overall coverage of iodized salt utilization among households was better; however, the proportion of proper utilization remains low, which was 48.5% as compared with universal salt initiative declarations of 90%. Respondents with formal educational status, monthly income ≥5000 ETB/month, and good knowledge score were significantly associated with proper iodized salt utilization. For effective USI and IDD risk reduction, regular inspection and monitoring must be taken barrier on the production and distribution of iodized salt in retailers and purchasers.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121221148612 for Iodine status, impact of knowledge, and practice for adequate iodized salt utilization in house hold at North West Ethiopia by Alebechaw Molla, Mastewal Giza, Fassikaw Kebede and Tsehay Kebede in SAGE Open Medicine
Acknowledgments
We would like also to thank the data collectors and supervisors for their unreserved cooperation during data collection.
Footnotes
Authors’ contributions: FK, MG, and AM conceived the study, supervised the data collection, did the analysis and interpretation, and wrote the full manuscript from the initial to the end. Finally, each author commented, edited the final draft, and approved the final version for submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The Ethical Review Board of Debre Markose University ethically cleared this research to conduct with the protocol (119/011). Written informed consent was taken from the participants and legally authorized representatives of minor participants before the study initiation. The purpose of the study was explained to all study participants, and study was carried out in accordance with relevant guidelines and regulations.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was taken from the participants and legally authorized representatives of minor participants before the study initiation. Purpose of the study was explained to all study participants, and study was carried out in Accordance with relevant guidelines and regulations.
Consent for publication: Not applicable
Trial registration: Not applicable
Data sharing statement: The data set for this research is up on corresponding author with reasonable request.
ORCID iDs: Fassikaw Kebede  https://orcid.org/0000-0002-6117-5272
https://orcid.org/0000-0002-6117-5272
Tsehay Kebede  https://orcid.org/0000-0002-6841-4686
https://orcid.org/0000-0002-6841-4686
Supplemental material: Supplemental material for this article is available online.
Reference
- 1. Girma K, Nibret E, Gedefaw M. The status of iodine nutrition and iodine deficiency disorders among school children in Metekel Zone, northwest Ethiopia. Ethiop J Health Sci 2014; 24: 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Belachew AAT. Effect of iodine deficiency on academic performance of school children in Dawro Zone, Southwest Ethiopia: a prospective cohort study. Nutr Dietary Suppl 2020; 12: 157–166. [Google Scholar]
- 3. Habib MA, Alam MR, Ghosh S, et al. Impact of knowledge, attitude, and practice on iodized salt consumption at the household level in selected coastal regions of Bangladesh. Heliyon 2021; 7: e06747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rahman Khan J, Biswas RK, Sheikh Md T, et al. Factors-associated-with-the-availability-of-iodized-salt-at-household-level-a-case-study-in-bangladesh. Public Health Nutr 2019; 22(10): 1815–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zerfu TA. Magnitude, trends, and determinants of iodized salt availability among households in Ethiopia: analysis of Named Entity Recognition for Hadiyya Language using BiLSTM-CRF ModelNamed entity recognition for Hadiyya language using BiLSTM-CRF ModelEthiopian demographic and health surveys (2000–2016). Nutr Metab Insights 2021; 14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goris JM, Temple VJ, Sumbis J, et al. Iodine status of non-pregnant women and availability of food vehicles for fortification with iodine in a remote community in Gulf province, Papua New Guinea. PLoS One 14(11): e0224229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yeshaw Y, Alem AZ, Tesema GA, et al. Spatial distribution and determinants of household iodized salt utilization in Ethiopia: a spatial and multilevel analysis of Ethiopian demographic and Health survey. BMC Public Health 2020; 20: 1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hailu S, Wubshet M, Woldie H, et al. Iodine deficiency and associated factors among school children: a cross-sectional study in Ethiopia. Arch Public Health 2016; 74: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zeru AB, Muluneh MA, Giorgis KKH, et al. Iodine deficiency disorder and knowledge about benefit and food source of iodine among adolescent girls in the north Shewa zone of Amhara region. J Nutr Metab 2021; 2021: 8892180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Takele L, Belachew T, Bekele T. Iodine concentration in salt at household and retail shop levels in Shebe town, south west Ethiopia. East Afr Med J 2003; 80: 532–539. [DOI] [PubMed] [Google Scholar]
- 11. Girma M, Loha E, Bogale A, et al. Iodine deficiency in primary school children and knowledge of iodine deficiency and iodized salt among caretakers in Hawassa Town: Southern Ethiopia. Ethiop J Health Dev 2012; 26(1): 30–35. [Google Scholar]
- 12. Mesele M, Degu G, Gebrehiwot H. Prevalence and associated factors of goiter among rural children aged 6-12 years old in Northwest Ethiopia: cross-sectional study. BMC Public Health 2014; 14: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hailu S, Wubshet M, Woldie H, et al. Iodine deficiency and associated factors among school children: a cross-sectional study in Ethiopia. Arch Public Health 2016; 74: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mohammed H, Marquis GS, Aboud F, et al. TSH mediated the effect of iodized salt on child cognition in a randomized clinical trial. Nutr Metabolic Insights 2021; 14: 11786388211025352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nega1 AWDTKG. Iodine level of salt and associated factors at household level in Gidami District, Oromia Region, Ethiopia: a cross-sectional study. Nutr Dietary Suppl 2021; 2021: 9–16. [Google Scholar]
- 16. Bazezew MM, Yallew WW, Belew AK. Knowledge and practice of iodized salt utilization among reproductive women in Addis Ababa City. BMC Res Notes 2018; 11: 734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Abebe Z, Tariku A, Gebeye E. Availability of adequately iodized in Northwest Ethiopia: a cross-sectional study. Arch Public Health 2017; 75: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tadesse S, Hymete A, Lieberman M, et al. Iodine status, household salt iodine content, knowledge and practice assessment among pregnant women in Butajira, South Central Ethiopia. PLoS One 2022; 17(11): e0277208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yitayew S, Asemahagn M, Zeleke A. Data management practice and associated factors in East Gojjam Zone, Northwest Ethiopia. Open Med Inf J 2020; 13: 2–7. [Google Scholar]
- 20. Mekonnen TC, Eshete S, Wasihun Y, et al. Availability of adequately iodized salt at household level in Dessie and Combolcha Towns, South Wollo, Ethiopia. BMC Public Health 2018; 18: 1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Senbeta AM, Mamo FT, Desalegn BB, et al. Knowledge and practices of iodized salt utilization, health consequences, and iodine concentration on dietary salts at retailer and households in Jigjiga town, Somali, Ethiopia. Cogent Food Agric 2021; 7. [Google Scholar]
- 22. Tareke AA, Zerfu TA. Magnitude, trends, and determinants of iodized salt availability among households in Ethiopia: analysis of Ethiopian demographic and health surveys (2000-2016). Nutr Metab Insights 2021; 14: 11786388211025342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tariku WB, Mazengia AL. Knowledge and Utilization of Iodized Salt and Its Associated Factors at Household Level in Mecha District, Northwest Ethiopia. J Nutr Metab 2019; 2019: 9763830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alamneh AA, Leshargie CT, Desta M, et al. Availability of adequately iodized salt at the household level in Ethiopia: a systematic review and meta-analysis. PLoS One 2021; 16: e0247106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vasudevan S, Senthilvel S, Sureshbabu J. Knowledge attitude and practice on iodine deficiency disorder and iodine level in salt in retail and vendors among the rural population in south India: a community based observational and descriptive study. Clin Epidemiol Global Health 2019; 7: 300–305. [Google Scholar]
- 26. Aredo MT, Demise HF, Regesu AH. Proper utilization of iodized salt and associated factors among rural community of Hetosa District, Oromia Regional State, South East Ethiopia. Biorxiv 2020. [Google Scholar]
- 27. Hawas S, Lemma S, Mengesha S, et al. Proper utilization of adequatly iodized salt at house hold level and associated factores in Asella Town Arsi Zone Ethiopia: a community based cross sectional study. J Food Process Technol 2016; 7: 573. [Google Scholar]
- 28. Tololu AK, Getahun FA, Abitew DB. Coverage of Iodized Salt and Associated Factors at Household Level in Goba Town, Bale Zone, South East Ethiopia, 2015. Science J Public Health 2016; 4: 346–351. [Google Scholar]
- 29. Afework A, Mulu W, Abate A, et al. Handling and adequacy of iodine at household level: community based cross-sectional survey in Dega Damot District, West Gojjam Zone, Amhara Regional State, Ethiopia. BioRxiv 2019: 586677. [Google Scholar]
- 30. Abebe Z, Tariku A, Gebeye E. Availability of adequately iodized in Northwest Ethiopia: a cross-sectional study. Arch Public Health 2017; 75: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haji Y, Abdurahmen J, Paulos W. Knowledge and perception of consumption of iodized salt among food handlers in Southern Ethiopia. Food Nutr Bullet 2017; 38: 92–102. [DOI] [PubMed] [Google Scholar]
- 32. Bulli AT, Aredo MT, Fekadu H, et al. Proper utilization of iodized salt and associated factors among rural community of Hetosa district, Oromia regional state, South East Ethiopia. BioRxiv. [Google Scholar]
- 33. Kumma WP, Haji Y, 2 Abdurahmen J, et al. Factors affecting the presence of adequately iodized salt at Home in Wolaita, Southern Ethiopia: community based study. Int J Food Sci 2018; 2018: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gemede HF, Tamiru B, Fite MB. Knowledge, practice, and availability of iodized salt and associated factors in Jibat Woreda, West Shoa Zone, Ethiopia. Int J Food Sci 2021; 2021: 5562390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Worku S, Garedew G, Adugna L, et al. Knowledge and utilization of iodized salt and associated factors among households of Fitche Town, Central Ethiopia, 2020: a community based cross-sectional study. JOJ Pub Health 2021; 6(2): 555681. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121221148612 for Iodine status, impact of knowledge, and practice for adequate iodized salt utilization in house hold at North West Ethiopia by Alebechaw Molla, Mastewal Giza, Fassikaw Kebede and Tsehay Kebede in SAGE Open Medicine