Abstract
The use of extracts from the hawthorn plant as cardiovascular agents dates back to the 1st century; recently, they have also been made available online as weight loss aids. Herein, we present a case of intentional intoxication with hawthorn root extract (HRE) in an adult patient that resulted in death. A 20-year-old female patient, who was clinically diagnosed with depression, developed hypotension, bradycardia, and depressed consciousness after ingestion of this extract. An electrocardiogram recorded a sinus arrest with a slow nodal rhythm, which rapidly deteriorated, leading to cardiac arrest. This case report illustrates the potentially fatal consequences of HRE for which the constituents have not yet been characterized. All physicians, especially those in the emergency department, should be aware of the dangerous, even potentially fatal interactions of HRE with prescription medications.
Keywords: Long QT syndrome, Cardiac arrhythmias, Emergency medicine, Sudden cardiac death, Case reports
INTRODUCTION
The use of extracts from the hawthorn plant as cardiovascular agents dates back to the first century and is prevalent even today. Among its cardiovascular effects, hawthorn extracts demonstrate positive inotropic, vasodilatory, and antiarrhythmic effects [1]. Recently, preparations from hawthorn roots have been made available online as weight loss aids [2]. This report depicts a case of intentional intoxication with hawthorn root extract (HRE) in an adult patient that resulted in severe arrhythmia and subsequent death.
CASE REPORT
A 20-year-old female patient arrived at the emergency department (ED) complaining of abdominal pain and nausea. The patient did not have any history of chronic/neurodegenerative disease. Nevertheless, at admission, she was undergoing treatment for depression with amitriptyline, alprazolam, and clozapine. The patient had ingested all three medications simultaneously at 9:00PM, the previous night (12 hours before admission).
She also reportedly ingested two alcoholic drink equivalents (consisting of 24 oz of regular beer) between 10:00PM and 1:00 AM, on the day of admission. On further interrogation, the patient confessed to having ingested an undetermined number of HRE pills. The bottle was stated to contain 90 pills when sealed and was empty when brought to the ED by the patient’s relatives, who estimated that the patient must have ingested over half the tablets in the bottle. Upon examination, the patient was responsive and oriented, with a Glasgow Coma Scale score of 15 points. Vital signs were normal. Routine lab work, including hemogram, renal function, and liver enzymes, were normal. Serum electrolytes were sodium, 142 mEq/L; potassium, 3.8 mEq/L; chloride, 111 mEq/L; magnesium, 2.0 mEq/L. The attending physician advised a gastric lavage (per protocol), and prescribed omeprazole 20 mg intravenous (IV), and ondansetron 4 mg IV.
After 6 hours in the ED, the patient abruptly became pale, and developed diaphoresis and nausea. Vital signs showed a blood pressure (BP) of 70/40 mmHg with pulse rate 30 beats per min (bpm), respiratory rate 20 breaths/min, and O2 saturation 97% on room air. An electrocardiogram (ECG) was obtained (Fig. 1). The patient then received a 500 mL crystalloid fluid bolus and 1 mg atropine IV. Consequently, the pulse rate and BP improved to 80 bpm and 100/60 mmHg, respectively. The patient’s vital signs stabilized, and she also reported symptomatic relief. The ECG showed sinus rhythm with sporadic premature ventricular contractions.
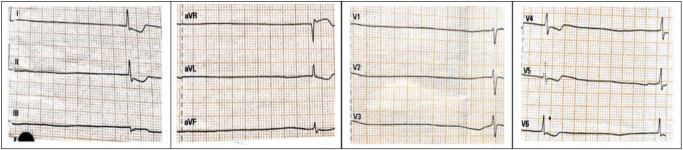
Fig. 1.
Initial electrocardiogram showing sinus arrest with slow nodal rhythm and secondary changes of the ST segment and T wave.
Nevertheless, after 15 minutes, there was a sudden drop in BP and pulse rate to 61/28 mmHg and 30 bpm, respectively. The patient was administered another 250 mL of crystalloid fluid bolus. Fig. 2 shows the ECG findings at this point. However, the patient was unresponsive to fluid resuscitation due to persisting hypotension and bradycardia, and was consequently shifted to the intensive care unit. There, she developed depressed consciousness (Glasgow Coma Scale 13 points, E3 M6 V4). A solution containing 400 mg of dopamine in 250 mL of 5% dextrose, was initially administered at a rate of 5 μg/kg/min and then increased gradually up to 20 μg/kg/min; this led to improvements in pulse rate and BP to 60 bpm and 89/55 mmHg, respectively.
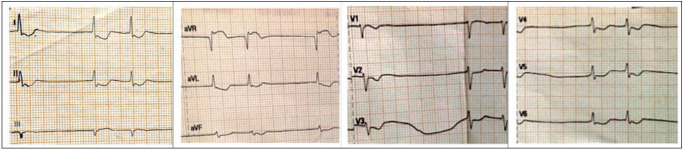
Fig. 2.
Second electrocardiogram showing sinus arrest with nodal rhythm and secondary changes of the ST segment and T wave.
Approximately 40 minutes after her arrival to the intensive care unit, the patient went into a witnessed cardiac arrest. Cardiopulmonary resuscitation was started. The ECG showed ventricular fibrillation. Defibrillation restored rhythm to sinus bradycardia. After a minute passed, the patient sustained a new episode of cardiac arrest. The patient was unresponsive to advanced cardiovascular life support protocols, including lidocaine administration, and was pronounced dead after 20 minutes of effort.
DISCUSSION
This case depicts an extreme consequence of the use of HRE. A plausible mechanism for the fatal arrhythmia in this patient could be a ventricular arrhythmia caused by excessive QT prolongation from an overdose of HRE and its interaction with other medications; consequently, leading to a delay in the cardiac rectifier current (IKr).
Phytochemical analysis shows that epicatechin, aglycons, and glycosides of B-type oligomeric procyanidins, flavanols, phenolic acids, and C-glycosyl flavones are the major bioactive compounds in hawthorn (Crataegus spp.). The beneficial effects of these compounds on the cardiovascular system have been demonstrated through in vitro, animal, and clinical studies [3].
Nevertheless, the adverse events associated with the ingestion of hawthorn extracts are less well known. In a systematic review of 14 trials evaluating hawthorn extract for treating chronic heart failure, 13 trials contained no data on relevant mortality and morbidity, such as cardiac events. Only one trial reported five deaths (three in the active group), but did not provide any details [4]. Another trial with 897 patients, who were treated with HRE, reported the occurrence of cardiac disorders at a frequency of 30% as a side effect. Nonetheless, the authors did not define the cardiac conditions, nor did the report provide further details on the nature of the side effects [5]. Additionally, flowers and leaves are the main components of most hawthorn extracts, with few utilizing the fruits [6], and reports on the use of the roots are rare [2].
The inhibition of IKr is a known effect of hawthorn [1], and this inhibition antecedes the development of torsade de pointes, just as in the congenital long QT syndromes [7]. Although the patient had no history of long QT syndrome, the female sex and the presence of subclinical forms of long QT syndrome mutations are recognized risk factors for drug-induced torsade de pointes [8].
Regarding drug-related QT interval prolongation, both amitriptyline and clozapine (which the patient regularly took without reporting adverse effects) have QT-prolonging capabilities [9]. These two mechanisms, acting either alone or in combination, could have led to the development of the patient’s and subsequent death. Besides, both omeprazole and ondansetron are also reported to prolong the QT interval [10]. Multiple pharmacological targets of hawthorn extracts have been documented [5]. It is worth noting that the patient was under long-term psychiatric treatment with the drugs mentioned above, with good adherence and without reporting any adverse event. It is possible that the patient perceived HRE as safe (due to its so-called “natural” origin), and therefore, decided not to commit a suicidal attempt but only a suicidal gesture. This could provide a possible explanation as to why she did not overdose on her other available medications.
Thus, this might be a cautionary note to physicians regarding their drug choices for patients taking Mexican hawthorn root and other Crataegus spp. In a recent report, the ingestion of HRE in a pediatric patient resulted in clinical manifestations of digoxin intoxication with a false elevation of digoxin serum levels [2]. Clinical trials show that HRE intake is associated with a positive inotropic effect with an increase in ejection fraction of patients with heart failure [5]. Consequently, a digoxin-like effect of hawthorn may have also aggravated the arrhythmogenesis. Unfortunately, we could not obtain any measurement of the serum HRE and digoxin levels, which might have helped in establishing the causal relationship in our case.
Lastly, although the change in plasma sodium and potassium after gastric lavage was not considerable [11], electrolyte disturbances have been documented, which could have further exacerbated the arrhythmogenesis.
In conclusion, this case illustrates the potentially fatal consequences of HRE. We believe that all physicians, especially those in the ED, should be aware of the dangerous, even possibly fatal, interactions of HRE with prescription medications.
Capsule Summary
What is already known
Few herbal medications can have dangerous and even fatal interactions leading to arrhythmia and death.
What is new in the current study
Acute intoxication with hawthorn root extract in an adult patient resulted in arrhythmia and subsequent death.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Brenyo A, Aktas MK. Review of complementary and alternative medical treatment of arrhythmias. Am J Cardiol. 2014;113:897–903. doi: 10.1016/j.amjcard.2013.11.044. [DOI] [PubMed] [Google Scholar]
- 2.Palmer KG, Lebin JA, Cronin MT, Mazor SS, Burns RA. Crataegus Mexicana (Tejocote) exposure associated with cardiotoxicity and a falsely elevated digoxin level. J Med Toxicol. 2019;15:295–8. doi: 10.1007/s13181-019-00727-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang B, Liu P. Composition and health effects of phenolic compounds in hawthorn (Crataegus spp.) of different origins. J Sci Food Agric. 2012;92:1578–90. doi: 10.1002/jsfa.5671. [DOI] [PubMed] [Google Scholar]
- 4.Pittler MH, Guo R, Ernst E. Hawthorn extract for treating chronic heart failure. Cochrane Database Syst Rev. 2008;1:CD005312. doi: 10.1002/14651858.CD005312.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Holubarsch CJ, Colucci WS, Meinertz T, Gaus W, Tendera M. Survival and prognosis: investigation of Crataegus extract WS 1442 in congestive heart failure (SPICE): rationale, study design and study protocol. Eur J Heart Fail. 2000;2:431–7. doi: 10.1016/s1388-9842(00)00109-4. [DOI] [PubMed] [Google Scholar]
- 6.Furey A, Tassell M. Towards a systematic scientific approach in the assessment of efficacy of an herbal preparation: hawthorn (Crataegus spp.) Eur J Heart Fail. 2008;10:1153–7. doi: 10.1016/j.ejheart.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Haverkamp W, Breithardt G, Camm AJ, et al. The potential for QT prolongation and proarrhythmia by non-antiarrhythmic drugs: clinical and regulatory implications. Report on a policy conference of the European Society of Cardiology. Eur Heart J. 2000;21:1216–31. doi: 10.1053/euhj.2000.2249. [DOI] [PubMed] [Google Scholar]
- 8.Paulussen AD, Gilissen RA, Armstrong M, et al. Genetic variations of KCNQ1, KCNH2, SCN5A, KCNE1, and KCNE2 in drug-induced long QT syndrome patients. J Mol Med (Berl) 2004;82:182–8. doi: 10.1007/s00109-003-0522-z. [DOI] [PubMed] [Google Scholar]
- 9.Crouch MA, Limon L, Cassano AT. Clinical relevance and management of drug-related QT interval prolongation. Pharmacotherapy. 2003;23:881–908. doi: 10.1592/phco.23.7.881.32730. [DOI] [PubMed] [Google Scholar]
- 10.Khan Q, Ismail M, Haider I, Ali Z. Prevalence of the risk factors for QT prolongation and associated drug-drug interactions in a cohort of medical inpatients. J Formos Med Assoc. 2019;118(1 Pt 1):109–15. doi: 10.1016/j.jfma.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Benson BE, Hoppu K, Troutman WG, et al. Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol (Phila) 2013;51:140–6. doi: 10.3109/15563650.2013.770154. [DOI] [PubMed] [Google Scholar]