Abstract
Wildfire activity is increasing in parts of the world where extreme drought and warming temperatures contribute to fireprone conditions, including the western United States. The elderly are among the most vulnerable, and those in long-term care with preexisting conditions have added risk for adverse health outcomes from wildfire smoke exposure. In this study, we report continuous co-located indoor and outdoor fine particulate matter (PM2.5) measurements at four skilled nursing facilities in the western United States. Throughout the year 2020, over 8000 h of data were collected, which amounted to approximately 300 days of indoor and outdoor sampling at each facility. The highest indoor 24 h average PM2.5 recorded at each facility was 43.6 μg/m3, 103.2 μg/m3, 35.4 μg/m3, and 202.5 μg/m3, and these peaks occurred during the wildfire season. The indoor-to-outdoor PM2.5 ratio and calculated infiltration efficiencies indicated high variation in the impact of wildfire events on Indoor Air Quality between the four facilities. Notably, infiltration efficiency ranged from 0.22 to 0.76 across the four facilities. We propose that this variability is evidence that PM2.5 infiltration may be impacted by modifiable building characteristics and human behavioral factors, and this should be addressed in future studies.
Keywords: elder health, indoor air quality, long-term care, PM2.5
1 ∣. INTRODUCTION
Elevated ambient air pollution events are linked to poor health outcomes such as stroke, heart disease, lung cancer and chronic respiratory disease representing a major public health challenge in the United States (US) and around the world.1 Contributing sources of air pollution include anthropogenic sources such as oil combustion, vehicular traffic and industrial plants, and natural sources such as wildfires.2 Annual levels of ambient particulate matter (PM) air pollution have been declining over the last several decades in many regions of the United States; an exception to this trend is the northwestern region of the United States, where air quality has worsened due to increased wildfire activity.3 Currently, an estimated 20% of fine particulate annual emissions in the United States are from wildfires,4 with this number being as high as 50% for some western regions.5
Communities exposed to smoke from wildfires often experience extended periods where concentrations of fine PM (PM2.5) are in exceedance of 35 μg/m3, the 24 h ambient air quality standard for the United States.6 For the protection of public health, local and state officials often advise affected populations to remain indoors during wildfire smoke events. However, it is important to consider if these actions alone provide sufficient protection.7 Infiltration of ambient air pollution to the indoor environment is dependent on multiple variables including building structure, engineering and occupancy, and environmental factors such as meteorological and topographical features.8 During periods of poor outdoor air quality and without adequate protective factors in place (e.g., filtration), the Indoor Air Quality can quickly diminish.9 Monitoring indoor PM air pollution levels can provide actionable and timely data to help inform public and occupational health measures even in the absence of specific regulations or building standards from the US Environmental Protection Agency (EPA) or National Institute of Occupational Safety and Health (NIOSH).
The risk for negative health impacts due to poor Indoor Air Quality is also dependent on the characteristics of those who reside in the building. Life stage and preexisting disease are among the most important risk factors for adverse health outcomes related to air pollution exposures.10 Therefore, the long-term care community is of particular interest. Adults over the age of 65 years living in skilled nursing facilities have higher rates of cardiopulmonary morbidities such as chronic obstructive pulmonary disease (COPD) compared with older adults in the general population leaving them at greater risk for exacerbation from inhalation exposures.11 The vulnerability of this population was highlighted by the COVID-19 pandemic, whereby some estimate 30%–40% of the deaths in the United States were represented by those who resided in skilled nursing or long-term care facilities.12,13
Studies investigating Indoor Air Quality exposure among the older adults living in residential homes or retirement communities are relatively limited, and few have focused specifically on PM2.5 in the skilled nursing facility environment, where residents typically require more medical care and have more respiratory-related comorbidities.4,5,14-19 Further studies focusing on vulnerable populations like the elderly are paramount for downwind communities in the western United States that are annually impacted by wildfire smoke. This study presented here aimed to capture real-time indoor fine PM measurements, with a particular focus on PM originating from a wildfire source, in skilled nursing facilities across a broad geographic area within a western US state over a 12 months period.
2 ∣. METHODS
2.1 ∣. Facility participants
Facilities were recruited during education and outreach activities facilitated by the Idaho Health Care Association. At two separate events, administrators and staff were given information about the study. Personnel representing the four participating facilities worked with Boise State University to develop an agreement that would protect the facilities’ anonymity while also allowing for the dissemination of generalizable data. The facilities are geographically dispersed across Idaho and topographically unique, representing three different airsheds. Two facilities are located in southwestern Idaho, one in northwestern Idaho and one in southeastern Idaho.
2.2 ∣. Facility characteristics
The four skilled nursing facilities in the study ranged in building age from approximately 10–50 years old. All buildings in this study were single story and contained operable windows in the resident rooms. The size and usage of the facilities varied with square footage ranging from 15 000 to 30 000 and the number of available beds ranging from 15 to 80. All facilities used a minimum efficiency rating value (MERV) 13 filter; MERVs are derived from a test method developed by the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), and a rating of 13 is given to a filter that removes >75% of particles 0.3–1 μm and >90% of particles 1.0–10 μm.20 The heating, ventilation, and air conditioning (HVAC) systems ranged in installation age from 10 to 50 years with some updates occurring in the interim (Table 1).
TABLE 1.
Facility Characteristics
| Facility | Approximate building age |
Approximate square feet |
Approximate number of beds |
Approximate age of original HVAC (years) |
Approximate age of HVAC update (years) |
HVAC filter rating |
|---|---|---|---|---|---|---|
| SNF 1 | 50 | 30 000 | 80 | 50 | Unknown | MERV 13 |
| SNF 2 | 10 | 15 000 | 15 | 10 | NA | MERV 13 |
| SNF 3 | 50 | 15 000 | 40 | 15 | NA | MERV 13 |
| SNF 4 | 45 | 15 000 | 35 | 45 | 15 | MERV 13 |
Note: Descriptive characteristics collected for four participating skilled nursing facilities, which were recruited in Idaho, USA.
Abbreviations: HVAC, heating, ventilation, and air conditioning; MERV, minimum efficiency reporting value; NA, not applicableSNF, skilled nursing facility.
2.3 ∣. Air quality monitoring
At each of the participating facilities, air quality was monitored indoors and outdoors. The PurpleAir PA-II (PurpleAir, Inc.,) was used for outdoor monitoring and contains two PMS5003 sensors (Plantower,), while the PurpleAir PA-I-Indoor was used for indoor monitoring and contains one PMS5003 sensor. The PMS5003 estimates particle mass concentrations on the principle of light scatter, and these methods are elaborated on further by Sayahi et al.21 The PMS5003 reports both mass concentrations (including PM2.5) and particle counts. The mass concentrations are provided in two data series, which are designated “CF=ATM” and “CF=1,” respectively.22 Mass concentrations are calculated from particle count data using proprietary algorithms developed by the PMS5003 sensor manufacturer, with CF=ATM using “average particle density for outdoor particulate matter” and CF=1 using “average particle density for indoor particulate matter.”23 Data from each sensor were transferred via Wi-Fi in real time to a password-protected private cloud account and were accessed by the research team. Selection of the outdoor location at each facility was based on availability of electrical power and proximity to each skilled nursing facility. Where possible, sensors were sited to avoid direct local exposure sources such as parking lots or drop-off points. The indoor locations were selected to provide a central point within the facility with access to electrical power that were away from commonly opened windows or exterior doors. Similar to outdoor sensors, indoor sensors were sited to avoid direct local exposure sources such as the kitchen. Sensors were positioned 1.5–2 meters above the ground in a position where air could freely circulate under the unit. During the study period, outdoor sensors at two of the facilities failed and were replaced. On several occasions, data were lost for hours up to weeks due to sensor failure, power loss, and Wi-Fi network disconnection.
2.4 ∣. Sensor characteristics
Overall, paired sensors within each outdoor PurpleAir unit had excellent agreement, with correlation coefficients of >0.99. We removed 15 hourly datapoints from one sensor with an apparent malfunction in one sensor that led to paired sensor differences of >100 μg/m3. A further 9 hourly datapoints were removed that had >5 μg/m3 difference and >2 sd percent difference (59%) between paired sensors.
2.5 ∣. Correction factor
A number of studies have evaluated PurpleAir sensors relative to reference monitors and found that PurpleAir overestimates PM2.5 in field settings.22,24-26 We analyzed PurpleAir data from two units that were collocated with an EPA-certified BAM 1020 Continuous Particulate Monitor (Met One Instruments, Inc.,) in Garden City, Idaho, during the month of September of 2020. We compared hourly data from the BAM instrument to PurpleAir data that were corrected using multiple methods.24,25,27 The method with the best performance used a correction factor of 0.714 (Supplement), which was based on studies that have reported the PurpleAir CF=1 channel overestimating PM2.5 by approximately 40% compared with reference monitors.25,28 Based on this literature and our own collocation of PurpleAir sensors with the BAM reference monitor, we corrected all of the PurpleAir data in our analysis by multiplying mean hourly PM2.5 concentrations from the CF=1 data series by 0.714. Further methods and results from the collocation data collection and analysis are presented in the supplemental materials. We note that our rationale for using the same correction factor for both indoor and outdoor PM2.5 is that we are assuming the dominant source of indoor PM2.5 in the facilities is from ambient PM2.5 infiltration (confirmed by results in Table 3). These facilities do not allow smoking and do not have other indoor pollution sources such as wood stoves. Cooking is a potential source of indoor PM2.5, but the PurpleAir monitors were placed in areas to avoid such exposures. Given that indoor pollution sources in the facilities were limited and that there are no indoor correction factors for PurpleAir monitors to our knowledge, it seemed more appropriate to correct both indoor and outdoor PM2.5 concentrations in the same manner rather than to leave the indoor concentrations uncorrected.
TABLE 3.
Outdoor vs Indoor PM2.5 Comparison
| Sampling days |
Outdoor–indoor PM2.5 difference (μg/ m3) Mean (sd) min, median, max |
Outdoor/indoor PM2.5 ratio |
Infiltration efficiency (95% CI) |
|
|---|---|---|---|---|
| All facilities | 1226 | 5.1 (8.4)–1.5, 2.7, 102.4 | 2.5 | 0.55 (0.52, 0.58) |
| Wildfire season | 474 | 7.5 (12.1)–0.5, 3.2, 102.4 | 2.0 | 0.58 (0.54, 0.63) |
| Non-wildfire season | 752 | 3.6 (3.9)–1.5, 2.4, 29.3 | 8.9 | 0.20 (0.19, 0.20) |
| Wildfire day | 88 | 25.3 (19.2) 5.0, 19.9, 102.4 | 1.8 | 0.59 (0.49, 0.71) |
| Non-wildfire day | 1138 | 3.5 (3.6)–1.5, 2.5, 29.3 | 3.7 | 0.29 (0.28, 0.30) |
| Non-wildfire day during wildfire season | 386 | 3.5 (3.0)–0.5, 2.6, 16.7 | 2.5 | 0.43 (0.41, 0.46) |
| Facility 1 | 321 | 6.5 (8.8)–0.2, 3.5, 52.7 | 3.3 | 0.38 (0.35, 0.41) |
| Facility 2 | 321 | 2.3 (3.7)–1.4, 1.0, 29.1 | 1.5 | 0.76 (0.72, 0.79) |
| Facility 3 | 311 | 5.5 (7.9)–1.5, 3.2, 76.3 | 6.3 | 0.22 (0.21, 0.23) |
| Facility 4 | 273 | 6.2 (11.2)–0.1, 3.5, 102.4 | 2.1 | 0.61 (0.57, 0.64) |
Note: Only sampling days with >12 h of hourly data for both indoor and outdoor PM2.5 are included in the table.
Abbreviations: PM2.5, fine particulate matter; sd, standard deviation; CI, confidence interval; Wildfire Season, July through October; Wildfire Day, day with mean 24 h PM2.5 > 21 μg/m3 during wildfire season.
2.6 ∣. Data analysis
Analysis was conducted using R version 4.0.4 (The R Foundation for Statistical Computing,). We evaluated agreement between the two identical sensors in each outdoor PurpleAir unit by assessing differences, percent differences, and correlation coefficients (Pearson and Spearman) for the hourly PM2.5 concentrations from the paired sensors within each unit. Hourly observations (n = 9) were removed from the dataset if the CF=1 PM2.5 concentrations from the paired channels were different by more than 5 μg/m3 and had percent differences larger than two standard deviations.24 Following this evaluation of sensor agreement, we used the mean hourly CF=1 PM2.5 concentration from paired sensors within each outdoor unit for all subsequent analysis. We note that the decision to use hourly data was made for two reasons: (1) the reference monitor used to generate the correction factor produces hourly data and (2) the validated method for calculating infiltration uses hourly data. Only days with 12+ hours of hourly sampling data were included in statistical analysis. We calculated descriptive statistics for indoor and outdoor PM2.5 concentrations (n, mean, sd, minimum [min], median, maximum [max]) overall, by facility, for wildfire season and non-wildfire season, and for wildfire days and non-wildfire days. Based on smoke event notifications from the Idaho Department of Environmental Quality, wildfire season was classified as the months of July through October 2020.29 A suspected wildfire day, hereafter referred to as wildfire day, was classified as a day during wildfire season with mean ambient 24 h PM2.5 (as measured by the outdoor PurpleAir sensor at each facility) greater than 21 μg/m3. A similar threshold to classify a wildfire day has been used previously in multiple studies.30,31 We also conducted sensitivity analyses using other thresholds to classify wildfire days during wildfire season (Table S1).
We calculated infiltration efficiency (Finf) using a previously validated recursive modeling approach.32-34 Finf is defined as the fraction of the outdoor PM2.5 concentration that penetrates to the indoor environment and remains suspended, and is presented as a unitless number between 0 and 1.32 For the calculation, we used paired hourly indoor and outdoor PM2.5 concentrations from the PurpleAir sensors in a model, which states that indoor PM2.5 is equal to a fraction of outdoor PM2.5 from the current hour, a fraction of indoor PM2.5 from the previous hour, and indoor PM2.5 from the current hour. Data were censored to exclude periods with indoor sources of PM2.5 (i.e., periods with a rise in indoor PM2.5 without a subsequent rise in outdoor PM2.5).32,33 Censored data were then used in a linear model with indoor PM2.5 as the outcome variable, outdoor PM2.5 and the previous hour's indoor PM2.5 as predictor variables, and intercept set to 0:
Model coefficients were then used to calculate Finf:
Using the random component superposition (RCS) model developed by Ott et al.,35 we calculated the concentration of indoor particles generated outdoors. As Diapouli et al. suggest36 the RCS model can be used to estimate indoor concentrations as the sum of outdoor- and indoor-generated particle concentrations:
where Cin is the concentration of indoor particles, Cog is the concentration of indoor particles generated outdoors, Cig is the concentration of indoor particles generated indoors, and Cout is the concentration of outdoor particles. From this, we can estimate Cog by simply multiplying Finf by Cout. Allen et al. used similar methods to estimate indoor PM2.5 generated from outdoor sources and percent indoor PM2.5 generated from outdoor sources.32 We multiplied 24-hour outdoor PM2.5 concentrations by the estimated Finf to estimate indoor PM2.5 generated outdoors. We divided this infiltrated concentration by the total 24-hour indoor concentration to estimate percent indoor PM2.5 generated from outdoor sources. If the infiltrated concentration was greater than the measured indoor concentration, the infiltrated concentration was set to equal the measured indoor concentration.32
3 ∣. RESULTS
3.1 ∣. Time series of PM2.5 at four skilled nursing facilities
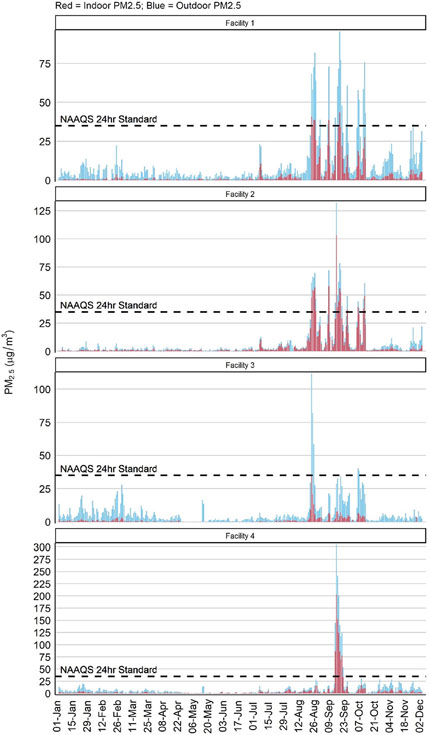
Air samplers were deployed in December 2019, and data for this study were captured from January 1, 2020, through December 1, 2020, yielding approximately 8000 hourly data points (Figure 1). Summary statistics for 24-hour mean PM2.5 are shown in Table 2. Facilities 1–4 had 331, 329, 313, and 276 days of outdoor PM2.5 data and 322, 332, 336, and 336 days of indoor PM2.5 data, respectively. Across all four facilities, the daily outdoor mean PM2.5 for the study period was 8.6 μg/m3 (sd=18.7, median=3.8) and the daily indoor mean PM2.5 was 3.3 μg/m3 (sd=11.3, median=0.7). By contrast, the daily outdoor and indoor mean PM2.5 for all four facilities on wildfire days (defined here as a July to October day with a daily PM2.5 average over 21 μg/m3) was 56.1 μg/m3 (sd=46.5, median=40.3) and 31.1 μg/m3 (sd=32.3, median=21.3), respectively. The highest indoor 24-hour mean PM2.5 recorded for Facilities 1–4 was 43.6 μg/m3, 103.2 μg/m3, 35.4 μg/m3 and 202.5 μg/m3, respectively. All of the highest outdoor and indoor 24-hour mean PM2.5 recorded for each facility occurred during the wildfire season.
FIGURE 1.
Indoor and Outdoor PM2.5, 2020. Time-series graphs represent fine particulate data collected for four skilled nursing facilities in Idaho, USA, from January 1, 2020, through December 1, 2020, where red bars represent data from the indoor sensor, and blue bars represent the outdoor sensor. PM2.5, fine particulate matter; NAAQS, United States Environmental Protection Agency National Ambient Air Quality Standard (35 μg/m3 of PM2.5 for a 24 h period)
TABLE 2.
Summary Statistics for 24 h Mean PM2.5
| Outdoor PM2.5 (μg/m3) |
Indoor PM2.5 (μg/m3) |
|||
|---|---|---|---|---|
| Sampling days | Mean (sd) min, median, max | Sampling days | Mean (sd) min, median, max | |
| All facilities | 1249 | 8.6 (18.7) 0.0, 3.8, 305.0 | 1326 | 3.3 (11.3) 0.0, 0.7, 202.5 |
| Wildfire season | 491 | 15.0 (28.1) 0.3, 5.2, 305.0 | 478 | 7.6 (18.0) 0.0, 2.0, 202.5 |
| Non-wildfire season | 758 | 4.5 (4.9) 0.0, 2.9, 36.1 | 848 | 0.8 (1.1) |
| Wildfire day | 90 | 56.1 (46.5) 21.1, 40.3, 305.0 | 89 | 31.1 (32.3) 3.8, 21.3, 202.5 |
| Non-wildfire day | 1159 | 4.9 (4.8) 0.0, 3.4, 36.1 | 1147 | 1.3 (1.9) 0.0, 0.7, 15.0 |
| Non-wildfire day during wildfire season | 401 | 5.8 (4.7) 0.3, 4.1, 20.7 | 389 | 2.3 (2.6) 0.0, 1.3, 15.0 |
| Facility 1 total | 331 | 9.6 (15.2) 0.3, 4.2, 95.6 | 322 | 3.0 (7.0) 0.0, 0.6, 43.6 |
| Wildfire season | 122 | 17.4 (21.8) 1.2, 7.2, 95.6 | 113 | 7.1 (10.7) 0.2, 2.3, 43.6 |
| Non-wildfire season | 209 | 5.0 (5.5) 0.3, 3.4, 36.1 | 209 | 0.8 (1.2) 0.0, 0.4, 6.8 |
| Wildfire day | 32 | 48.5 (21.4) 21.7, 45.4, 95.6 | 31 | 21.1 (11.6) 4.8, 18.7, 43.6 |
| Non-wildfire day | 299 | 5.4 (5.2) 0.3, 3.7, 36.1 | 291 | 1.0 (1.3) 0.0, 0.5, 6.8 |
| Non-wildfire day during wildfire season | 90 | 6.4 (4.1) 1.2, 4.7, 15.8 | 82 | 1.7 (1.4) 0.2, 1.2, 6.2 |
| Facility 2 total | 329 | 7.0 (14.9) 0.0, 2.1, 132.3 | 332 | 4.6 (11.6) 0.0, 0.9, 103.2 |
| Wildfire season | 123 | 14.9 (22.0) 0.3, 4.5, 132.3 | 119 | 11.3 (17.5) 0.3, 3.1, 103.2 |
| Non-wildfire season | 206 | 2.2 (2.8) 0.0, 1.5, 22.1 | 213 | 0.8 (0.8) 0.0, 0.6, 5.2 |
| Wildfire day | 27 | 50.0 (23.7) 22.9, 46.6, 132.3 | 27 | 38.6 (18.9) 16.4, 37.0, 103.2 |
| Non-wildfire day | 302 | 3.1 (3.6) 0.0, 1.9, 22.1 | 298 | 1.6 (2.3) 0.0, 0.8, 15.0 |
| Non-wildfire day during wildfire season | 96 | 5.0 (4.4) 0.3, 3.2, 18.8 | 92 | 3.3 (3.3) 0.3, 1.8, 15.0 |
| Facility 3 total | 313 | 6.6 (10.4) 0.2, 3.5, 111.7 | 336 | 1.0 (2.7) 0.0, 0.2, 35.4 |
| Wildfire season | 123 | 9.5 (15.2) 0.3, 3.8, 111.7 | 123 | 2.0 (4.2) 0.0, 0.5, 35.4 |
| Non-wildfire season | 190 | 4.7 (4.6) 0.2, 3.2, 28.0 | 213 | 0.4 (0.6) 0.0, 0.1, 3.9 |
| Wildfire day | 17 | 38.6 (24.2) 21.1, 29.4, 111.7 | 17 | 9.0 (8.0) 3.8, 6.6, 35.4 |
| Non-wildfire day | 296 | 4.7 (4.6) 0.2, 3.3, 28.0 | 296 | 0.6 (0.9) 0.0, 0.2, 5.6 |
| Non-wildfire day during wildfire season | 106 | 4.8 (4.6) 0.3, 3.3, 20.7 | 106 | 0.9 (1.2) 0.0, 0.3, 5.6 |
| Facility 4 total | 276 | 11.7 (30.1) 0.2, 5.2, 305.0 | 336 | 4.7 (17.6) 0.0, 1.4, 202.5 |
| Wildfire season | 123 | 18.2 (44.0) 0.5, 6.2, 305.0 | 123 | 10.2 (28.2) 0.0, 2.4, 202.5 |
| Non-wildfire season | 153 | 6.6 (5.3) 0.2, 5.1, 28.1 | 213 | 1.4 (1.4) 0.0, 1.1, 10.1 |
| Wildfire day | 14 | 106.3 (92.3) 22.0, 85.7, 305.0 | 14 | 65.4 (60.9) 8.9, 51.3, 202.5 |
| Non-wildfire day | 262 | 6.7 (5.3) 0.2 5.0, 28.1 | 262 | 2.3 (2.2) 0.0, 1.5, 10.4 |
| Non-wildfire day during wildfire season | 109 | 6.8 (5.3) 0.5, 4.8, 19.2 | 109 | 3.1 (2.8) 0.0, 2.2, 10.4 |
Abbreviations: PM2.5, fine particulate matter; sd, standard deviation; Wildfire Day, Day with mean 24 h PM2.5 > 21 μg/m3 during wildfire season Only sampling days with >12 h of hourly data are included in the table; Wildfire Season, July through October.
3.2 ∣. Influence of outdoor air quality on the indoor environment
To understand how ambient events such as episodes of wildfire smoke impact the indoor environment at skilled nursing facilities, we performed four types of analyses: outdoor to indoor difference in PM2.5, indoor-to-outdoor PM2.5 ratio, infiltration efficiency, and percent indoor PM2.5 generated outdoors (Table 3). The mean outdoor to indoor difference in 24-hour PM2.5 during the entire sampling period ranged across the four facilities from 6.5 μg/m3 (Facility 1) to 2.3 μg/m3 (Facility 2). As expected, facilities with lowest indoor-to-outdoor ratios had lower Finf values. Facility 3 had the highest indoor-to-outdoor ratio at 0.2 and the lowest infiltration efficiency at 0.22, while Facility 2 had the highest indoor-to-outdoor ratio at 0.7 and the highest infiltration efficiency at 0.76. The proportion of indoor PM2.5 generated outdoors was 97.4% or higher across the study. Across the four facilities, infiltration efficiency was higher during the wildfire season compared with non-wildfire season. The indoor daily mean PM2.5 did not go over the 24-hour US National Ambient Air Quality Standard (NAAQS) during the non-wildfire season, but exceedances were observed 28 times (5.7% of wildfire season sampling days) across the four facilities during the fire season (Table 4). Indoor daily averages for every facility went over the ambient NAAQS for PM2.5 at least once; over half of the 28 occurrences took place at Facility 2 (n = 15). Similarly, the indoor daily mean PM2.5 did not go over the 24 h World Health Organization (WHO) standard during the non-wildfire season but exceedances were observed 60 times (12.2% of wildfire season sampling days) across the four facilities during the fire season (Table 4).
TABLE 4.
Days with Indoor and Outdoor PM2.5 Above EPA NAAQS and WHO 24 h Standards
| Outdoor PM2.5 |
Indoor PM2.5 |
|||
|---|---|---|---|---|
| Sampling days | Days with PM2.5 > 35 μg/m3, n (%) | Sampling days | Days with PM2.5 > 35 μg/m3, n (%) | |
| All facilities | 1249 | 53 (4.2) | 1326 | 28 (2.1) |
| Wildfire season | 491 | 52 (10.6) | 478 | 28 (5.9) |
| Non-wildfire season | 758 | 1 (0.1) | 848 | 0 (0) |
| Facility 1 | 331 | 22 (6.6) | 322 | 5 (1.6) |
| Facility 2 | 329 | 18 (5.5) | 332 | 15 (4.5) |
| Facility 3 | 313 | 5 (1.6) | 336 | 1 (0.3) |
| Facility 4 | 276 | 8 (2.9) | 336 | 7 (2.1) |
| Sampling days | Days with PM2.5 > 25 μg/m3, n (%) | Sampling days | Days with PM2.5 > 25 μg/m3, n (%) | |
| All facilities | 1249 | 81 (6.5) | 1326 | 37 (2.8) |
| Wildfire season | 491 | 76 (15.5) | 478 | 37 (7.7) |
| Non-wildfire season | 758 | 5 (0.7) | 848 | 0 (0) |
| Facility 1 | 331 | 29 (8.8) | 322 | 10 (3.1) |
| Facility 2 | 329 | 25 (7.6) | 332 | 18 (5.4) |
| Facility 3 | 313 | 14 (4.5) | 336 | 1 (0.3) |
| Facility 4 | 276 | 13 (4.7) | 336 | 8 (2.4) |
Abbreviations: EPA NAAQS, United States Environmental Protection Agency National Ambient Air Quality Standard (35 μg/m3 of PM2.5 for a 24 h period); Wildfire Season, July through October; PM2.5, fine particulate matter; WHO, World Health Organization (standard is 25 μg/m3 of PM2.5 for a 24 h period) Only sampling days with >12 h of hourly data are included in the table.
In Table S1, we report descriptive statistics for wildfire days and outdoor PM2.5 concentrations using varying thresholds of PM2.5 to define a wildfire day. In general, the number of wildfire days decreased and PM2.5 concentrations increased as the PM2.5 threshold for wildfire days increased. The “non-wildfire day” and “non-wildfire day during wildfire season” means are 4.3 μg/m3 and 3.8 μg/m3, respectively, at a threshold of 10 μg/m3 compared with 5.4 μg/m3 and 7.1 μg/m3, respectively, for a threshold of 30 μg/m3. These results are discussed further below and highlight the need for an objective, validated method to define a wildfire affected day.
4 ∣. DISCUSSION
This study is one of longest continuous air quality monitoring studies among older adults and one of the first focused on wildfire smoke infiltration within a skilled nursing facility environment. Overall, PM2.5 concentrations were higher during wildfire season than during non-wildfire season, and outside the skilled nursing facilities than inside the facilities. However, our results indicate that wildfire smoke impacted the indoor environment at the four skilled nursing facilities to varying degrees. Our findings suggesting that Indoor Air Quality at skilled nursing facilities is a complex yet modifiable risk factors warrant further study due to the vulnerable populations that live in such facilities.
Our comparison of outdoor vs indoor PM2.5 revealed that there was a higher mean difference between outdoor and indoor PM2.5 during wildfire season than during non-wildfire season. However, infiltration efficiency was nearly three times higher during wildfire season than during non-wildfire season across all facilities (Table 3), indicating that Indoor Air Quality is negatively impacted by wildfire activity. The influence of Indoor Air Quality by ambient events was further demonstrated by the high percent of indoor PM2.5 that was generated outdoors, which was nearly 100% for all four facilities. Outdoor vs indoor PM2.5 and infiltration efficiency were also highly variable across the four skilled nursing facilities.
The source of variability in infiltration could be due to external factors, built environment factors, or behavioral factors. There are seasonal trends in particulate infiltration with more outdoor particulate reaching the indoor space in the summer rather than winter; these trends also yield more ultrafine and nanoparticle infiltration in the summer than in the winter.37 Here, we only captured a modest amount of data related to building characteristics. A more thorough examination of built environment factors such as air exchange rates could be helpful in future studies. Finally, human behaviors such as opening and closing windows should be examined. Anecdotally, we were told by facility administrators that residents are asked to keep windows closed when it is exceptionally hot or cold, or when there is a wildfire smoke event, but the residents do have autonomy. Thus, door and window usage could be more closely monitored to gain a better understanding of the impact on smoke PM infiltration.
All facilities reported using MERV 13 filters with their HVAC system, which follows the current guidance from the EPA and the ASHRAE for protecting commercial building occupants from smoke during wildfire events.38 Building ages ranged from approximately 10–50 years, and square footage ranged from approximately 15 000–30 000. With only four facilities in this pilot, it is not feasible to perform a formal analysis of these factors as predictors of infiltration. However, when we look at the relationship between facility age and PM infiltration efficiency (data not shown) we see a modest negative trend suggesting that, within our study, older buildings have better air quality, particularly during wildfire smoke events. Considering the relationship between building size and PM infiltration efficiency (data not shown), we do not see any trend. These relationships should be regarded cautiously until larger-scaled studies can be performed with more robust building characteristics that are measured during the course of the study by trained industrial hygienists and engineers.
Others have evaluated characteristics that influence the safety of being indoors during a biomass burning event. Reisen et al. measured indoor and outdoor air quality for 1 week at 21 residences and found that age and ventilation due to penetration points played a significant role in the infiltration of ambient PM.7 Another study used publicly available data from the PurpleAir sensor network to measure PM2.5 infiltration among 1400 buildings in California.39 In contrast with our results, the authors found that particle infiltration to the indoor environment decreased during wildfire events compared with days not impacted by wildfires. However, even with reduced particle infiltration, mean indoor PM2.5 concentrations were still nearly three times higher on wildfire days than on non-wildfire days. In contrast to skilled nursing facility residents, we speculate that residential inhabitants may choose to open and close their doors and windows less, and may seek additional methods of mitigating poor air quality. Not directly related to wildfire smoke, another group investigated indoor sources of PM such as cooking and cleaning among single family homes in Boston, Massachusetts, and found that air exchange rates influenced the indoor PM concentrations, with higher exchange rates tracking more closely with ambient PM.40
The results of the study presented here are consistent with other groups that have investigated air quality relationships between outdoor and indoor environments where older adults reside. Residential studies in homes of older adults over a 6 months period demonstrate a high correlation between ambient and indoor particulate exposure measured by gravimetric techniques.4,19 Similar results were also seen in a 12 days study conducted in a retirement community, where Buczynska et al. found no significant indoor sources of air pollution but did see a positive relationship between outdoor and Indoor Air Quality.5 Another group recently published an investigation of a single healthcare building during a two-month period of the 2020 wildfire season where they deployed two outdoor and seven indoor PM2.5 sensors.41 Their results indicate that PM2.5 infiltrates the indoor space to a greater degree during a smoke event and is variable by location within the building.
Although we do not directly assess the impact of air quality on health in this study, this is a clear priority for future studies. A growing number of studies among the general populations have evaluated how wildfire smoke events impact health. Bell et al. observed an association between “smoke-wave days” and increased respiratory admissions, 10% for women (4% for men) and 22% for black people (7% for white).42 Yao et al. investigated the emergency health services of British Columbian, Canada, and found that increased PM2.5 was associated with respiratory and cardiovascular-related ambulatory dispatches one hour following exposure during the wildfire seasons of 2010–2015.43
To date, the data specifically relating indoor particulate exposure and health in older adults are limited, but consistent. A series of Italian studies evaluated over 400 individual elder residences and showed that indoor particulate levels were negatively associated with lung function and positively associated with respiratory illness.16 Similarly, Osman et al. showed that pollutants in the indoor environment such as PM2.5 within individual residents’ homes are associated with worse health outcomes among 148 Scottish COPD patients with a mean age of 69 years.17 Perhaps one of the only studies that has considered fine particulate exposure in a skilled nursing facility setting was conducted by Bentayeb et al. as part of the GERIE study in Europe.18 This group measured Indoor Air Quality (PM10 and PM0.1) at 8 facilities and associated the levels with metrics of respiratory distress evaluated by survey and medical examination. Bentayeb et al.’s overall conclusion was that even at low levels of exposure, respiratory health among the elderly in a skilled nursing facility setting was negatively impacted. The authors did not evaluate the indoor versus outdoor sources of the indoor air pollution (personal communication). Notably, these few studies of Indoor Air Quality and elder health were not focused on wildfires as the source of particulate.
In this study, we leveraged low-cost PM sensors and demonstrated their utility in estimating the infiltration of outdoor pollutants in the skilled nursing facility environment. The use of low-cost sensors for assessing exposure in specific settings is gaining traction in the field despite the lower quantitative precision compared with reference monitors. In particular, particle concentrations measured by light-scattering aerosol sensors such as those found in the PurpleAir sensors can vary based on particle density and chemical composition, as well as meteorological conditions during sampling such as relative humidity.24 While we did collocate two PurpleAir sensors with an EPA reference monitor for one month during the study to inform the correction factor used in our analysis, we also acknowledge that using the same correction factor across the full 12 months study period is a limitation in our work. We were also unable to incorporate relative humidity into the correction factor due to malfunctions in the humidity sensors that are built into the PurpleAir units. Future studies should consider collocating low-cost sensors with reference monitors more frequently to incorporate correction factors that can account for seasonal trends and different particle sources, as well as help to identify units that experience calibration drift. Despite these limitations, the portability of low-cost sensors makes them important tools in field research where stationary and high-cost reference monitors are not feasible to use. In addition to higher spatial resolution in field research, our study and others44 demonstrate the utility of low-cost sensors in sampling site-specific air quality levels. With paired indoor/outdoor air pollution concentrations, we can calculate informative metrics such as infiltration efficiency and assess associations between air pollution and health with greater precision.
Specific to wildfire smoke-related low-cost sensor data, one major challenge for the field currently is how to identify a wildfire smoke event. There is currently no standard method for determining a “wildfire day,” and in this study, we used a daily mean PM2.5 cut point of 21 μg/m3 to classify a wildfire day. We chose this value to be consistent with previous studies that have used similar thresholds to classify wildfire days, although these studies used different methods to justify their decision. Doubleday et al. chose a threshold of 20.4 μg/m3 to classify a wildfire day using health-based guidelines and background particulate matter concentrations in the US state of Washington where the study took place.30 Zhou et al. used 21 μg/m3 as a threshold for a wildfire day based on PM2.5 concentrations that correspond to heavy smoke according to the National Oceanic and Atmospheric Administration's Hazard Mapping System.31 Others have used the US EPA’s 24-hour ambient PM2.5 standard (35 μg/m3) to classify a wildfire day,39 or data-driven approaches (98th percentile of daily PM2.5 concentration across western US counties) to classify a wildfire smoke wave.45 Future work would benefit from a standardized method of classifying wildfire-impacted days that can incorporate area-specific information such as background (historical) PM2.5 concentrations that help account for the widely varying geographic and land-use characteristics of wildfire-impacted areas. Such a method will help future research inform the health impacts of wildfire-specific air pollution.
Considering the specificity of our decision to classify a wildfire day as a daily average of PM2.5 over 21 μg/m3 when that day occurs during the specified wildfire season, we do note that this is based on the assumption that wildfire smoke is the dominant source of PM during this period. This assumption is supported for the US state of Idaho by McClure et al., who looked at data from 1988 to 2016 and demonstrated that particulate pollution in the Northwest US primarily comes from wildfires and not from urban sources.3 Thus, we have relatively high confidence in this study classifying a wildfire day as we have. Our selected threshold of 21 μg/m3 was consistent with some prior studies.30,31 We also note that a threshold as low as 10 μg/m3 still showed distinct wildfire day elevations in PM2.5 concentrations (mean 36.9 μg/m3), while non-wildfire days during wildfire season were indistinguishable from non-wildfire season days (mean 4.3 μg/m3 and 3.8 μg/m3, respectively; Table S1). However, we recognize that additional work is necessary to identify region-specific thresholds against an as-yet-unspecified gold standard for designating wildfire days.
We note some limitations in generalizing our findings to other communities. First, the monitoring activity occurred at only four facilities in three Idaho airsheds. It is unlikely that we adequately captured the range of potential variables that could directly or indirectly impact infiltration of ambient air into facilities, including local meteorological and topographical features, as well as building characteristics. Nevertheless, the four monitored facilities are varied in terms of square footage, age of building, and HVAC system. Second, we did not capture day-to-day building usage characteristics and behaviors such as opening windows or human traffic flow through external doors. Given the current public health guidance to stay indoors and seal buildings during wildfire smoke events, we anticipate that these behaviors would be fairly static during such events. However, building-related behaviors could vary considerably by season, and this is a subject that requires further attention. Finally, we used PurpleAir sensors rather than federal reference monitors to measure indoor and outdoor PM air concentrations. As these devices were paired for analysis, we expect that the use of these lower-cost sensors did not adversely impact our determination of I/O and infiltration fraction for each facility.
5 ∣. CONCLUSION
It is well known that ambient air quality impacts from nearby or distant wildfire events can have adverse health impacts on communities. Public health and environmental agencies currently have limited evidence-based recommendations to protect indoor air environments during wildfire events. One proposed strategy includes creating clean air spaces where populations can seek indoor refuge in protected spaces. We show here that such events can impact the indoor environments of skilled nursing facilities that house medically vulnerable populations. Identifying strategies for creating clean air spaces within skilled nursing and similar facilities should be a priority for communities regularly impacted by wildfire smoke events.
Supplementary Material
Practical Implications.
Our study provides evidence warranting future investigation into modifiable factors at skilled nursing facilities that could be addressed to positively influence Indoor Air Quality during wildfire smoke events with the ultimate goal of enhancing the health of residents and staff.
ACKNOWLEDGMENT
The authors thank the administrators and staff at each of the participating facilities and the Idaho Health Care Association for helping to facilitate the relationships that were so important to making this research possible.
Funding information
LM was supported by the Boise State University COBRE (P20GM109095) and the Idaho INBRE (P20GM103408). LM and ST were supported by a Clinical and Translational Research Infrastructure Network Award through the National Institute of General Medical Sciences of the National Institutes of Health (1U54GM104944). CN and EW are supported by the University of Montana Center for Population Health Research (P20GM130418).
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declare they have no conflicts of interest.
ETHICAL APPROVAL
The authors agree to follow the ethical guidelines set by the journal.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
DATA AVAILABILITY STATEMENT
Data from this study involve participating skilled nursing facilities that have requested special protections, which limit the authors’ ability to freely share the data without special permissions.
REFERENCES
- 1.Ambient air pollution. https://www.who.int/teams/environment-climate-change-and-health/air-quality-and-health/ambient-air-pollution
- 2.Adams K, Greenbaum DS, Shaikh R,van Erp AM, Russell AG. Particulate matter components, sources, and health: systematic approaches to testing effects. J Air Waste Manag Assoc. 2015;65:544–558. [DOI] [PubMed] [Google Scholar]
- 3.McClure CD, Jaffe DA. US particulate matter air quality improves except in wildfire-prone areas. PNAS. 2018;115:7901–7906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siponen T, Yli-Tuomi T, Tiittanen P, et al. Wood stove use and other determinants of personal and indoor exposures to particulate air pollution and ozone among elderly persons in a Northern Suburb. Indoor Air. 2019;29:413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buczyńska AJ, Krata A, Van Grieken R, et al. Composition of PM2.5 and PM1 on high and low pollution event days and its relation to indoor air quality in a home for the elderly. Sci Total Environ. 2014;490:134–143. [DOI] [PubMed] [Google Scholar]
- 6.David LM, Ravishankara AR, Brey SJ, et al. Could the exception become the rule? “Uncontrollable” air pollution events in the U.S. due to wildland fires. Environ Res Lett. 2021;16:034029. 10.1088/1748-9326/abe1f3 [DOI] [Google Scholar]
- 7.Reisen F, Powell JC, Dennekamp M, Johnston FH, Wheeler AJ. Is remaining indoors an effective way of reducing exposure to fine particulate matter during biomass burning events? J Air Waste Manag Assoc. 2019;69(5):611–622. 10.1080/10962247.2019.1567623 [DOI] [PubMed] [Google Scholar]
- 8.Leung DYC. Outdoor-indoor air pollution in urban environment: challenges and opportunity. Front Environ Sci. 2015;2:69. [Google Scholar]
- 9.Chen C, Zhao B. Review of relationship between indoor and outdoor particles: I/O ratio, infiltration factor and penetration factor. Atmos Environ. 2011;45:275–288. [Google Scholar]
- 10.Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zarowitz BJ, O’Shea T. Chronic obstructive pulmonary disease: prevalence, characteristics, and pharmacologic treatment in nursing home residents with cognitive impairment. J Manag Care Pharm. 2012;18:598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Girvan G. Nursing Homes & Assisted Living Facilities Account for 38% of COVID-19 Deaths. FREOPP.org. 2021. https://freopp.org/the-covid-19-nursing-home-crisis-by-the-numbers-3a47433c3f70 [Google Scholar]
- 13.Conlen M, et al. Nearly One-Third of U.S. Coronavirus Deaths Are Linked to Nursing Homes. The New York Times. 2020. [Google Scholar]
- 14.Bentayeb M, Simoni M, Norback D, et al. Indoor air pollution and respiratory health in the elderly. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2013;48:1783–1789. [DOI] [PubMed] [Google Scholar]
- 15.Arhami M, MinguillÃ3n MC, Polidori A, Schauer JJ, Delfino RJ, Sioutas C. Organic compound characterization and source apportionment of indoor and outdoor quasi-ultrafine particulate matter in retirement homes of the Los Angeles Basin. Indoor Air. 2010;20:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simoni M, Jaakkola MS, Carrozzi L, Baldacci S, Di Pede F, Viegi G. Indoor air pollution and respiratory health in the elderly. Eur Respir J Suppl. 2003;40:15s–20s. [DOI] [PubMed] [Google Scholar]
- 17.Osman LM, Douglas JG, Garden C, et al. Indoor air quality in homes of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007;176:465–472. [DOI] [PubMed] [Google Scholar]
- 18.Bentayeb M, Norback D, Bednarek M, et al. Indoor air quality, ventilation and respiratory health in elderly residents living in nursing homes in Europe. Eur Respir J. 2015;45:1228–1238. [DOI] [PubMed] [Google Scholar]
- 19.Janssen NAH, de Hartog JJ, Hoek G, et al. Personal exposure to fine particulate matter in elderly subjects: relation between personal, indoor, and outdoor concentrations. J Air Waste Manag Assoc. 2000;50:1133–1143. [DOI] [PubMed] [Google Scholar]
- 20.Us Epa O What is a MERV rating?. 2019. https://www.epa.gov/indoor-air-quality-iaq/what-merv-rating [Google Scholar]
- 21.Sayahi T, Butterfield A, Kelly KE. Long-term field evaluation of the plantower PMS low-cost particulate matter sensors. Environ Pollut. 2019;245:932–940. [DOI] [PubMed] [Google Scholar]
- 22.Tryner J, L'Orange C, Mehaffy J, et al. Laboratory evaluation of low-cost PurpleAir PM monitors and in-field correction using co-located portable filter samplers. Atmos Environ. 2020;220:117067. [Google Scholar]
- 23.PurpleAir FAQ. https://www2.purpleair.com/community/faq#hc-what-is-the-difference-between-cf-1-and-cf-atm
- 24.Barkjohn KK, Gantt B, Clements AL. Development and application of a United States-wide correction for PM2.5 data collected with the PurpleAir sensor. Atmospheric Meas Tech. 2021;14:4617–4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wallace L, Bi J, Ott WR, Sarnat J, Liu Y. Calibration of low-cost PurpleAir outdoor monitors using an improved method of calculating PM2.5. Atmos Environ. 2021;256:118432. [Google Scholar]
- 26.Kelly KE, Whitaker J, Petty A, et al. Ambient and laboratory evaluation of a low-cost particulate matter sensor. Environ Pollut. 2017;221:491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delp WW, Singer BC. Wildfire smoke adjustment factors for low-cost and professional PM2.5 monitors with optical sensors. Sensors. 2020;20:3683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta P, Doraiswamy P, Levy R, et al. Impact of California fires on local and regional air quality: the role of a low-cost sensor network and satellite observations. GeoHealth. 2018;2:172–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hunter SI, Idaho smoke blog. https://idsmoke.blogspot.com/
- 30.Doubleday A, Schulte J, Sheppard L, et al. Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: a case-crossover study. Environmental Health. 2020;19:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou X, Josey K, Kamareddine L, et al. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States. Sci Adv. 2021;7:eabi8789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen R, Larson T, Sheppard L, Wallace L, Liu L- JS. Use of real-time light scattering data to estimate the contribution of infiltrated and indoor-generated particles to indoor air. Environ Sci Technol. 2003;37:3484–3492. [DOI] [PubMed] [Google Scholar]
- 33.Allen R, Wallace L, Larson T, Sheppard L, Liu LJS. Evaluation of the recursive model approach for estimating particulate matter infiltration efficiencies using continuous light scattering data .J Eposure Sci Environ Epidemiol. 2007;17:468–477. [DOI] [PubMed] [Google Scholar]
- 34.Semmens EO, Noonan CW, Allen RW, Weiler EC, Ward TJ. Indoor particulate matter in rural, wood stove heated homes. Environ Res. 2015;138:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ott W, Wallace L, Mage D. Predicting particulate (PM10) personal exposure distributions using a random component superposition statistical model. J Air Waste Manag Assoc. 2000;50:1390–1406. [DOI] [PubMed] [Google Scholar]
- 36.Diapouli E, Chaloulakou A, Koutrakis P. Estimating the concentration of indoor particles of outdoor origin: a review. J Air Waste Manag Assoc. 2013;63:1113–1129. [DOI] [PubMed] [Google Scholar]
- 37.Zauli-Sajani S, Rovelli S, Trentini A, et al. Higher health effects of ambient particles during the warm season: the role of infiltration factors. Sci Total Environ. 2018;627:67–77. [DOI] [PubMed] [Google Scholar]
- 38.Development O of R. Protecting commercial building occupants from smoke during wildfire and prescribed burn events. https://cfpub.epa.gov/si/si_public_record_Report.cfm?dirEntryId=351876&Lab=CPHEA
- 39.Liang Y, Sengupta D, Campmier MJ, et al. Wildfire smoke impacts on indoor air quality assessed using crowdsourced data in California. Proc Natl Acad Sci U S A. 2021;118:e2106478118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abt E, Suh HH, Allen G, Koutrakis P. Characterization of indoor particle sources: a study conducted in the metropolitan boston area. Environ Health Perspect. 2000;108:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen PDM, Martinussen N, Mallach G, et al. Using low-cost sensors to assess fine particulate matter infiltration (PM2.5) during a wildfire smoke episode at a large inpatient healthcare facility. Int J Environ Res Public Health. 2021;18:9811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu JC, Wilson A, Mickley LJ, et al. Who among the elderly is most vulnerable to exposure to and health risks of fine particulate matter from wildfire smoke? Am J Epidemiol. 2017;186:730–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yao J, Brauer M, Wei J, McGrail KM, Johnston FH, Henderson SB. Sub-daily exposure to fine particulate matter and ambulance dispatches during wildfire seasons: a case-crossover study in British Columbi, Canada. Environ Health Perspect. 2020;128:067006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Durkin A, Gonzalez R, Isaksen TB, Walker E, Errett NA. Establishing a community air monitoring network in a wildfire smoke-prone rural community: the motivations, experiences, challenges, and ideas of clean air methow’s clean air ambassadors. Int J Environ Res Public Health. 2020;17:8393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu JC, Wilson A, Mickley LJ, et al. Wildfire-specific fine particulate matter and risk of hospital admissions in urban and rural counties. Epidemiology. 2017;28:77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from this study involve participating skilled nursing facilities that have requested special protections, which limit the authors’ ability to freely share the data without special permissions.