Abstract
Introduction
Chronic myelomonocytic leukemia (CMML) is a rare hematological malignancy bearing of both myelodysplastic syndrome and myeloproliferative neoplasm characteristics. Despite the low incidence, the clinical diagnosis of CMML was difficult and the survival was poor. The optimal first-line therapy for CMML still remains a matter of debate.
Methods
We retrospectively analyzed the clinical characteristics of 66 CMML patients in a single center during the past 10 years and studied the survival status of CMML patients in the real world and the influence of treatment methods on the prognosis of patients.
Results
For the 66 CMML patients, the median age was 60 years old (IQR 47.0–67.0), and an approximately 1.6:1.0 male-to-female ratio was found. CMML-0, CMML-1 and CMML-2 accounted for 13.7% (9/66), 43.9% (29/66) and 42.4% (28/66), respectively. The chromosome abnormality rate was 27.2% (18/66). Gene mutation was detected in 60 patients by sequenced in first-generation with 51.1% (22/43) gene mutations and in NGS with 82.3% (14/17) gene mutations. The top three mutation genes were ASXL1MT (11/60, 18.3%), TET2MT (10/60, 16.7%), and SRSF2 MT (9/60, 15.0%). There were 27 patients in supportive therapy group, and 39 patients in chemotherapy group including patients undergoing HSCT. Patients in chemotherapy group showed better OS than those in the supportive group before and after PSM analysis with p < 0.05. Patients with blast cell in bone marrow ≥10% or WHO CMML-2 benefited more from chemotherapy treatment achieving better OS. Multivariate analysis showed that supportive therapy and intermediate-2/high in CPSS were independent risk factors for OS after PSM.
Discussion
Chemotherapy including hypomethylating agents prolonged overall survival of CMML patients, especially in patients with blast cell ≥10% in bone marrow or WHO CMML-2 comparing with supportive therapy. Sequencing may provide direct insight into the molecular mechanism by detection of gene mutation, enabling personalized treatment in the future.
Keywords: chronic myelomonocytic leukemia, hypomethylating agents, therapy, survival, prognosis
Introduction
Chronic myelomonocytic leukemia (CMML) is a rare, age-related clonal hematological malignancy bearing characteristics of both myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN). Originally, CMML was classified by the French–American–British (FAB) working group as a separate variant of MDS.1 In 2001, the World Health Organization (WHO) classification defined CMML as a new group, referred to as MDS/MPN syndromes combining both MDS and MPN features.2 CMML is characterized by sustained peripheral blood monocytosis (≥1×109/L and ≥10% of WBC differential) and an inherent tendency of 15–20% over 3–5 years for transformation to acute myeloid leukemia (AML).3 In addition to dysplastic and proliferative types, CMML is subclassified into three variants as CMML-0, CMML-1 and CMML-2 based on the percentage of blasts in the peripheral blood and bone marrow.4,5 These groups are also associated with prognostic significance.6 The CMML-specific Prognostic Scoring System (CPSS) uses four variables (FAB and WHO CMML subtypes, erythrocyte transfusion dependence and cytogenetic findings) to classify patients into four risk groups (low, intermediate-1, intermediate-2 and high risk).7 CPSS could predict the survival of CMML patients and the risk of leukemia transformation. Recurrent somatic mutations were very common in CMML patients and have predictive significance for prognosis8 but have not been included in the prediction model at present. Due to the low incidence and lack of research, the optimal first-line therapy for CMML still remains a matter of debate. Hypomethylating agents (HMA) are currently the only Food and Drug Administration (FDA) approved therapy for patients with CMML. In general, objective response rate (ORR) of HMA in CMML patients ranged from 40% to 50% with true complete response (CR) rates of <20%,9 whereas HMA treatment did not confer an overall survival advantage for patients with lower-risk diseases, ie, dysplastic (MD) CMML with <10% blasts and lower risk CPSS.10 Allogeneic hematopoietic stem cell transplantation (Allo-HSCT) remains the only curative treatment option for patients with CMML. However, the median age at diagnosis for CMML was over 70 years in literatures.11 Due to the rather old age and comorbidity, allogeneic hematopoietic stem cell transplantation (HSCT) is not available for most patients when diagnosed. In this study, we retrospectively analyzed the clinical characteristics, bone marrow features, treatment outcomes and prognosis factors of CMML in patients diagnosed in our single center in the past 10 years.
Materials and Methods
Patients
From Jan 2011 to Dec 2020, inpatients with abnormal blood test results in the department of hematology from our single center were retrospectively analyzed. The inclusion criteria of CMML patients diagnosed according to the WHO 2016 criteria were as follows:6 1) Presence of persistent (>3 months) peripheral blood monocytosis >1×109/L, with monocytes constituting ≥10% of the white blood cell count differential; 2) Not meeting WHO criteria for BCR-ABL1 driven chronic myeloid leukemia, essential thrombocythemia, polycythemia vera or primary myelofibrosis; 3) No evidence for PDGFRA or PDGFRB rearrangements, and the absence of FGFR1 rearrangements or the PCM1-JAK2 fusion in the context of concomitant eosinophilia; 4) <20% blasts/blasts equivalent (promonocytes, monoblasts and myeloblasts) in the peripheral blood and bone marrow; 5) Dysplasia in one or more myeloid cell lineages. If myelodysplasia is absent or minimal, the diagnosis of CMML may still be made if the other requirements are met; 6) An acquired clonal cytogenetic or molecular genetic abnormality (TET2, ASXL1, SRSF2 and SETBP1) is present in hemopoietic cells. The exclusion criteria were as follows: 1) Patients with hematological disorders, including benign blood disorders, etc.; 2) patients with age less than 18.
This retrospective study was approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, and was in agreement with the Declaration of Helsinki. The informed consent was waived by the Ethics Committee of Tongji Hospital, and the privacy and confidentiality of the patients were guaranteed. Treatment and follow-up supportive therapy group included hydroxyurea monotherapy, and induction chemotherapy group included hypomethylating agents as decitabine (10mg-20mg/m2/day for 5 days) or azacytidine (75mg/m2/day during 5–7 days, every 28 days), intensive chemotherapy for at least one cycle with HAG (low-dose HHT 1–2 mg/m2 on days 1–14; low-dose Ara-C 10 mg/m2, Q12h on days 1–14 and G-CSF 200 μg/m2, on days 1–14);12 CAG (low-dose cytarabine 10mg/m2, Q12h on days 1–14); aclarubicin 10mg/d on days 1–8, and G-CSF 200 μg/m2 on days 1–14);13 DA (Daunorubicin 45mg/m2 for 3 days and Ara-C 100mg/m2 for 7 days).14 Treatment was determined according to patients’ willingness. Patients enrolled into our study underwent component blood transfusion and anti-infection treatment when necessary. Hematopoietic stem cell transplantation (HSCT) and supportive care were provided in a risk-adapted and priority-based manner. Karyotypes were classified as low risk (normal karyotype and isolated loss of Y chromosome), poor risk (trisomy 8, abnormalities of chromosome 7, and complex karyotype with >3 chromosomal abnormalities) and intermediate risk (all other chromosomal abnormalities) use in CPSS.15 Clonal hematopoiesis was defined as patients with at least one myeloid gene mutation (NPM1, DNMT3A, TET2, SRSF2, TP53, ASXL1, JAK2, FLT3-ITD, IDH1, EZH2, U2AF1, KRAS, SETBP1, RUNX1, ADAMTS13) and a minimum variant allele fraction of >2% in peripheral blood.
Study Endpoints
The primary endpoint was overall survival (OS), which was measured from the time of diagnosis to the time of last follow-up or death of any cause. The secondary endpoint was leukemia transformation. Leukemia transformation was defined as blast cells >20%, and the time to leukemia transformation was measured from the time of diagnosis to the onset of AML according to the WHO 2016 criteria. The endpoint of follow-up was March 2022.
Propensity Score Matching
Propensity score matching (PSM) analysis was used to reduce the bias in treatment selection. Patients in supportive therapy group and chemotherapy group were matched by PSM method as previously described.16 A logistic regression model was applied to calculate the propensity score for an individual given the covariates of age, gender, albumin and bone marrow dysplasia in smear. 1:1 nearest neighbor matching with a caliper of 0.05 and without replacement was used to minimize the conditional bias.
Statistical Analysis
Categorical variables are presented as percentages (%) and analyzed by Chi-square test. Continuous variables are presented as mean ± standard deviation (SD). Student’s t-test was used for normally distributed data, and Mann–Whitney U-test was used for non-normally distributed data. Survival curves before and after PSM were depicted by the Kaplan–Meier method and compared by Log rank test. Univariate and multivariate analysis were performed using Cox proportional hazards regression model. SPSS version 25.0 (SPSS Inc.) was used for statistical analysis.
Results
Baseline Characteristics
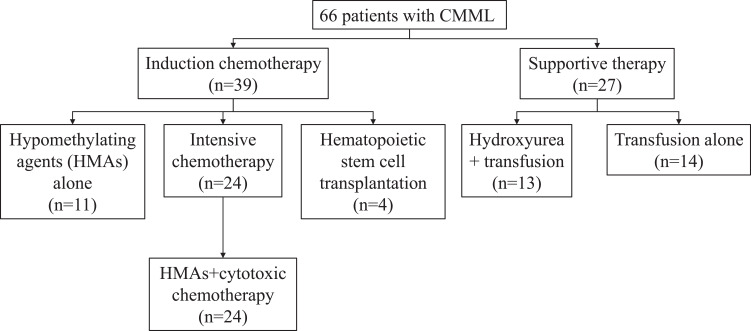
From Jan 2011 to Dec 2020, a total of 8540 patients with abnormal blood test from our single center were retrospectively reviewed. With the inclusion and exclusion criteria, 66 patients with CMML were enrolled into analytic cohort (Supplementary Figure 1). There were 27 patients in supportive therapy group, and 39 patients in chemotherapy group including patients undergoing HSCT (Figure 1).
Figure 1.
Distribution of treatment pattern of 66 patients.
Baseline characteristics of patients before and after PSM are summarized in Table 1. The proportion of patients with decreased level of serum albumin (<30g/L) in supportive therapy group (29.6%) was higher than that in chemotherapy group (10.3%) (p = 0.045). More patients in chemotherapy group (66.7%) presented single/multiple- lineage bone marrow dysplasia in smear, comparing with patients in supportive group (40.7%) (p = 0.037). The other characteristics between two groups were comparable without statistical differences, including age, gender, hematologic parameters, bone marrow morphology, WHO and CPSS score. After PSM analysis, 23 matched pairs were obtained from each group and there were no significant differences among these characteristics in two groups.
Table 1.
Characteristics of the Study Patients Before and After Propensity Score Matching
| Before Propensity Matching | After Propensity Matching | |||||
|---|---|---|---|---|---|---|
| Supportive Therapy (n=27) | Chemotherapy* (n=39) | P | Supportive Therapy (n=23) | Chemotherapy*(n=23) | P | |
| Age (year) (n (%)) | ||||||
| <60 | 11 (40.7%) | 21 (53.8%) | 0.295 | 9 (39.1%) | 12 (52.2%) | 0.375 |
| ≥60 | 16 (59.3%) | 18 (46.2%) | 14 (60.9%) | 11 (47.8%) | ||
| Gender (n (%)) | ||||||
| Male | 17 (63.0%) | 25 (64.1%) | 0.925 | 16 (69.6%) | 16 (69.6%) | 1.000 |
| Female | 10 (37.0%) | 14 (35.9%) | 7 (30.4%) | 7 (30.4%) | ||
| WBC (×109/L) (n (%)) | ||||||
| <13 | 14 (51.9%) | 16 (41.0%) | 0.385 | 14 (60.9%) | 11 (47.8%) | 0.375 |
| ≥13 | 13 (48.1%) | 23 (59.0%) | 9 (39.1%) | 12 (52.2%) | ||
| Hb (g/L) (mean±SD) | 72.137±17.861 | 74.936±19.078 | 0.550 | 74.522±16.393 | 75.891±21.510 | 0.809 |
| Neutrophil count (mean±SD) | 15.394±21.906 | 16.635±23.634 | 0.830 | 13.909±21.109 | 15.666±27.595 | 0.809 |
| Lymphocyte count (mean±SD) | 2.849±2.253 | 4.475±4.820 | 0.071 | 2.335±1.900 | 4.248±5.043 | 0.100 |
| Lymphocyte percent (%) (mean±SD) | 19.430±14.157 | 16.850±11.339 | 0.415 | 19.200±14.061 | 18.500±13.178 | 0.863 |
| PLT (×109/L) (mean±SD) | 90.963±123.101 | 165.869±269.059 | 0.182 | 88.217±132.352 | 133.213±132.528 | 0.255 |
| Albumin (g/L) (n (%)) | ||||||
| <30 | 8 (29.6%) | 4 (10.3%) | 0.045 | 5 (21.7%) | 4 (17.4%) | 0.710 |
| ≥30 | 19 (70.4%) | 35 (89.7%) | 18 (78.3%) | 19 (82.6%) | ||
| Blast cell percent (%) in PB (mean±SD) | 3.296±4.037 | 2.308±2.897 | 0.251 | 3.304±3.936 | 2.022±2.902 | 0.215 |
| Blast cell percent (%) in BM (mean±SD) | 9.370±7.038 | 8.564±4.685 | 0.578 | 8.261±5.045 | 7.891±4.426 | 0.793 |
| Bone marrow dysplasia in smear (n (%)) | ||||||
| Absent | 16 (59.3%) | 13 (33.3%) | 0.037 | 12 (52.2%) | 13 (56.2%) | 0.767 |
| Single/multi-lineage | 11 (40.7%) | 26 (66.7%) | 11 (47.8%) | 10 (43.5%) | ||
| Megakaryocyte dysplasia in smear (n (%)) | ||||||
| Yes | 9 (33.3%) | 20 (51.3%) | 0.149 | 9 (39.1%) | 10 (43.5%) | 0.765 |
| No | 18 (66.7%) | 19 (48.7%) | 14 (60.9%) | 13 (56.2%) | ||
| Bone marrow dysplasia in biopsy (n (%)) | ||||||
| Absent | 13 (48.1%) | 19 (48.7%) | 0.964 | 12 (52.2%) | 14 (60.9%) | 0.552 |
| Single/multi-lineage | 14 (51.9%) | 20 (51.3%) | 11 (47.8%) | 9 (39.1%) | ||
| WHO (n (%)) | ||||||
| CMML-0 | 5 (18.5%) | 4 (10.3%) | 0.313 | 4 (17.4%) | 2 (8.7%) | 0.312 |
| CMML-1 | 9 (33.3%) | 20 (51.3%) | 8 (34.8%) | 13 (56.2%) | ||
| CMML-2 | 13 (48.1%) | 15 (38.5%) | 11 (47.8%) | 8 (34.8%) | ||
| Chromosome karyotype (n (%)) | ||||||
| Normal | 13 (48.1%) | 31 (79.5%) | 0.138 | 14 (60.9%) | 17 (73.9%) | 0.345 |
| Abnormal | 10 (37.0%) | 8 (20.5%) | 9 (39.1%) | 6 (26.1%) | ||
| CPSS (n (%)) | ||||||
| Low | 7 (25.9%) | 17 (43.6%) | 0.392 | 6 (26.1%) | 9 (39.1%) | 0.586 |
| Intermediate-1 | 10 (37.0%) | 14 (35.9%) | 9 (39.1%) | 9 (39.1%) | ||
| Intermediate-2 | 9 (33.3%) | 7 (17.9%) | 7 (30.4%) | 5 (21.7%) | ||
| High | 1 (3.7%) | 1 (2.6%) | 1 (4.3%) | 0 (0%) | ||
Notes: Data are presented as mean±SD or n/N (%). *Chemotherapy group included patients underwent Hematopoietic Stem Cell Transplantation (HSCT).
Abbreviations: WBC, white blood cell; Hb, hemoglobin; PLT, platelet count; CPSS, CMML-specific Prognostic Scoring System; PB, Peripheral blood; BM, bone marrow.
Survival Analysis
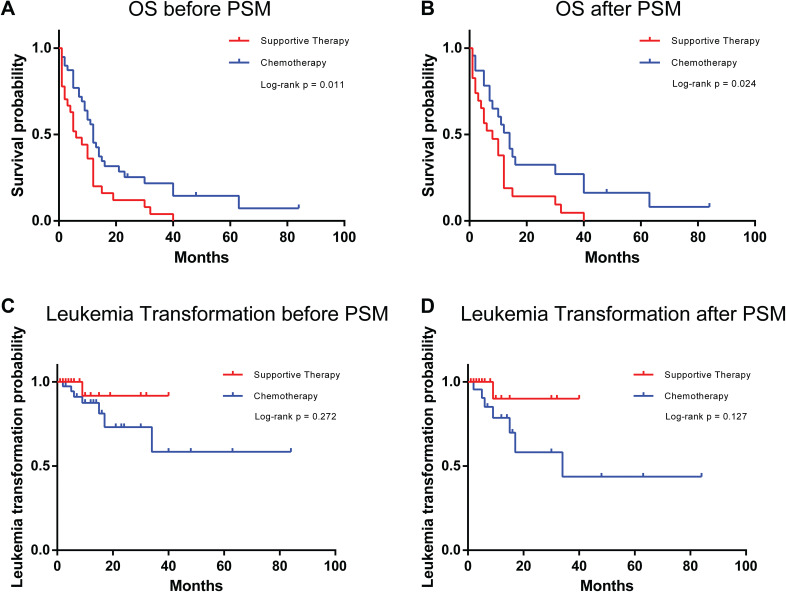
Patients in chemotherapy group showed better OS than those in the supportive group before and after PSM analysis with p < 0.05 (Figure 2A and B). However, there was no statistically significant difference in survival duration without leukemia transformation in both groups before and after PSM analysis with p = 0.272 and p = 0.127, respectively (Figure 2C and D). There was a trend for leukemia transformation in supportive therapy group according to survival curves, but the result was not statistically significant.
Figure 2.
Kaplan–Meier curves of survival and leukemia transformation rates for CMML patients who underwent supportive therapy or chemotherapy (A and B), the Kaplan–Meier curves of OS; (C and D), the Kaplan–Meier curves of leukemia transformation rates.
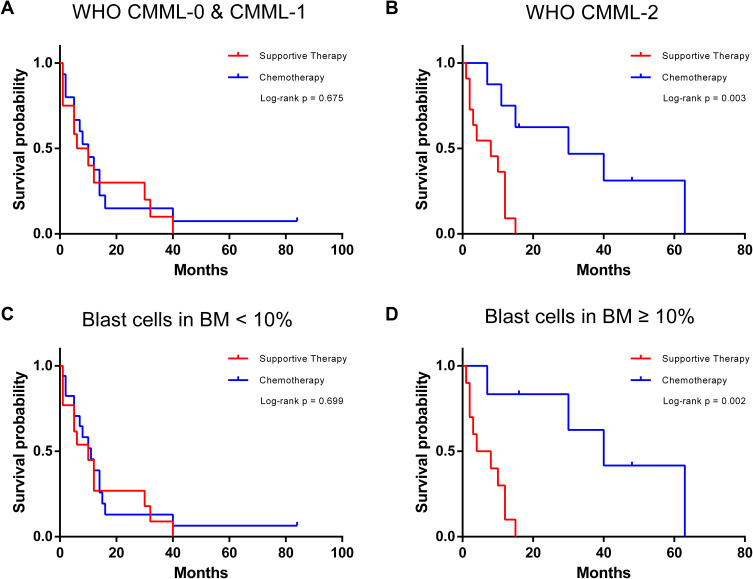
Subgroup analysis of OS showed that specific subgroups may benefit more from chemotherapy treatment (Table 2). For patients with blast cell in bone marrow ≥10% or WHO CMML-2, chemotherapy treatment achieved better OS with p = 0.003 (Figure 3A and B) and p = 0.002 (Figure 3C and D), respectively.
Table 2.
The Risk Analysis for Overall Survival of Patients After Propensity Score Matching Analysis
| Subgroup | Supportive Therapy (n=23) | Chemo- Therapy* (n=23) | Hazard Ratio (95% CI) | P |
|---|---|---|---|---|
| Age (year) | ||||
| <60 | 9 (39.1%) | 12 (52.2%) | 0.512 (0.201–1.308) | 0.162 |
| ≥60 | 14 (60.9%) | 11 (47.8%) | 0.541 (0.222–1.322) | 0.178 |
| Gender | ||||
| Male | 16 (69.6%) | 16 (69.6%) | 0.515 (0.238–1.116) | 0.093 |
| Female | 7 (30.4%) | 7 (30.4%) | 0.443 (0.128–1.536) | 0.199 |
| WBC (×109/L) | ||||
| <13 | 14 (60.9%) | 11 (47.8%) | 0.500 (0.229–1.092) | 0.082 |
| ≥13 | 9 (39.1%) | 12 (52.2%) | 0.557 (0.225–1.379) | 0.206 |
| Hb (g/L) | ||||
| <60 | 6 (26.1%) | 5 (21.7%) | 0.344 (0.083–1.429) | 0.142 |
| ≥60 | 17 (73.9%) | 18 (78.3%) | 0.555 (0.267–1.151) | 0.113 |
| Albumin (g/L) | ||||
| <30 | 5 (21.7%) | 4 (17.4%) | 0.270 (0.030–2.452) | 0.245 |
| ≥30 | 18 (78.3%) | 19 (82.6%) | 0.626 (0.313–1.248) | 0.183 |
| Blast cell in PB (%) | ||||
| <5 | 18 (78.3%) | 21 (91.3%) | 0.576 (0.291–1.139) | 0.113 |
| ≥5 | 5 (21.7%) | 2 (8.7%) | 0.268 (0.031–2.333) | 0.233 |
| Blast cell in BM (%) | ||||
| <10 | 13 (56.5%) | 17 (73.9%) | 0.924 (0.454–1.879) | 0.827 |
| ≥10 | 10 (43.5%) | 6 (26.1%) | 0.082 (0.011–0.636) | 0.017 |
| Bone marrow dysplasia | ||||
| Absent | 12 (52.2%) | 13 (56.5%) | 0.547 (0.266–1.125) | 0.101 |
| Single/multi-lineage | 11 (47.8%) | 10 (43.5%) | 0.440 (0.157–1.235) | 0.119 |
| Megakaryocyte dysplasia | ||||
| No | 14 (60.9%) | 13 (56.5%) | 0.503 (0.217–1.166) | 0.109 |
| Yes | 9 (39.1%) | 10 (43.5%) | 0.379 (0.125–1.145) | 0.085 |
| WHO | ||||
| CMML-0 and CMML-1 | 12 (52.2%) | 15 (65.2%) | 0.866 (0.386–1.943) | 0.727 |
| CMML-2 | 11 (47.8%) | 8 (34.8%) | 0.162 (0.043–0.615) | 0.008 |
| Chromosome karyotype | ||||
| Normal | 14 (60.9%) | 17 (73.9%) | 0.668 (0.352–1.271) | 0.219 |
| Abnormal | 9 (39.1%) | 6 (26.1%) | 0.361 (0.097–1.349) | 0.130 |
| CPSS | ||||
| Low & intermediate-1 | 15 (65.2%) | 18 (78.3%) | 0.619 (0.327–1.172) | 0.141 |
| Intermediate-2 and high | 8 (34.8%) | 5 (21.7%) | 0.360 (0.092–1.413) | 0.143 |
Notes: *Chemotherapy group included patients underwent Hematopoietic Stem Cell Transplantation.
Figure 3.
Kaplan–Meier curves of specific subgroups of CMML patients who underwent supportive therapy or chemotherapy (A and B), the Kaplan–Meier curves of CMML-0 and CMML-1 and CMML-2 patients. (C and D), the Kaplan–Meier curves of blast cell in BM<10% and ≥10% in CMML patients.
Risk Factor Analysis
In the PSM cohort, treatment (p = 0.035), chromosome karyotype (p = 0.011) and CPSS (p = 0.036) were considered as risk factors for OS in univariate analysis with statistical differences (Table 3). Taken into the clinical significance of these variables, age, WBC count, serum albumin, and bone marrow dysplasia in smear were added into multivariate analysis regardless of no significant difference in univariate analysis statistically. Chromosome karyotype was excluded since its risk for OS can be partially reflected by CPSS. Multivariate analysis showed that supportive therapy (p = 0.023), single/multi-lineage of bone marrow dysplasia in smear (p = 0.071) and intermediate-2/high in CPSS (p = 0.010) were independent risk factors for OS after PSM. No risk factor was determined in univariate or multivariate analysis for survival without leukemia transformation after PSM analysis (Supplementary Table 1).
Table 3.
Univariate and Multivariate Analyses of the Relative Risk of Overall Survival After Propensity Score Matching
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Treatment (supportive vs chemotherapy*) | 0.504 (0.267–0.953) | 0.035 | 0.448 (0.225–0.894) | 0.023 |
| Age (year) (<60 vs ≥60) | 1.080 (0.584–1.999) | 0.806 | 1.341 (0.677–2.655) | 0.400 |
| Gender (female vs male) | 0.694 (0.357–1.349) | 0.281 | ||
| WBC (×109/L) (<13 vs ≥13) | 0.851 (0.459–1.578) | 0.609 | 1.449 (0.675–3.111) | 0.342 |
| Hb (g/L) (<60 vs ≥60) | 0.707 (0.343–1.459) | 0.348 | ||
| Albumin (g/L) (<30 vs ≥30) | 0.974 (0.443–2.141) | 0.947 | 1.205 (0.503–2.885) | 0.675 |
| Blast cell in PB (%) (<5 vs ≥5) | 1.087 (0.476–2.484) | 0.843 | ||
| Blast cell in BM (%) (<10 vs ≥10) | 0.806 (0.421–1.542) | 0.515 | ||
| Bone marrow dysplasia in smear (absent vs single/multi-lineage) | 1.702 (0.898–3.229) | 0.103 | 1.916 (0.945–3.882) | 0.071 |
| Megakaryocyte dysplasia (no vs yes) | 1.601 (0.847–3.028) | 0.148 | ||
| WHO (CMML-0 and CMML-1 vs CMML-2) | 0.820 (0.439–1.529) | 0.532 | ||
| Chromosome karyotype (normal vs abnormal) | 2.429 (1.225–4.818) | 0.011 | ||
| CPSS (low and intermediate-1 vs intermediate-2 andhigh) | 2.090 (1.051–4.158) | 0.036 | 3.399 (1.333–8.667) | 0.010 |
Notes: *Chemotherapy group included patients underwent Hematopoietic Stem Cell Transplantation (HSCT).
Discussion
CMML is a clonal neoplastic hematopoietic stem cell disorder characterized by dysplasia, monocytosis, and increased risk of transformation to secondary AML (sAML).6 Diagnosis of CMML is complicated due to overlapping features of MDS and MPN, the high heterogeneity of clinical presentation, and the absence of specific indicators for CMML.17 There are several criteria used in clinic to diagnose CMML, such as persistent absolute monocytosis of ≥1 × 109/L, with monocytes accounting for more than 10% in peripheral blood, dysplasia in one or more bone marrow cell lineage, and the absence of genetic rearrangements in the PDGFRA, FDGFRB, and FGFR1 genes and the PCM1-JAK2 and BCR-ABL1 fusions.17,18
According to the leukocyte count of 13×109/L, CMML is subdivided into myelodysplastic (MD) and myeloproliferative (MP) variants.19 Outcomes of patients with MP CMML are worse than those of patients with MD CMML.20 Among 66 patients with CMML in our center in the past 10 years, CMML-0, CMML-1 and CMML-2 accounted for 13.7%, 43.9% and 42.4%, respectively. As patients in CMML-0 and CMML-1 categories seem to have overlapping cytogenetic features with comparable survival results,21 we analyzed the subtypes for the prognostic value. There was no significant association with the outcomes according the blast percentage in peripheral blood and bone marrow. Univariate and multivariate analysis showed treatments and CPSS are independent risk factors for OS in CPSS patients.
Cytogenetic changes are identified in 20–30% of CMML cases, with the most common alterations including trisomy 8, loss of chromosome Y, abnormalities of chromosome 7 (monosomy 7 and del7q), trisomy 21, and complex karyotype.15,22 In our study of 66 patients, the chromosome abnormality rate was 27.2% (18/66), which was consistent with the literature reports. The type of chromosome abnormalities in CMML patients was similar to MDS except sole del(5q), but the abnormality proportion of CMML patients was lower than MDS of 50%.23 The karyotype provided additional prognostic significance. The Spanish cytogenetic risk stratification system was developed, categorizing patients into three groups: high risk (trisomy 8, chromosome 7 abnormalities, or complex karyotype), intermediate risk (all chromosomal abnormalities, except for those in the high- and low-risk categories), and low risk (normal karyotype or –Y), with 5-year OS of 4%, 26%, and 35%, respectively.24 Among the 18 patients with abnormal karyotype, there were 11 cases with high-risk karyotypes including chromosome 7 or 3 abnormality or complex karyotype. They all died with a median survival of 2 months (range 1–21), which was significantly shorter than those with low or intermediate risk karyotype.
More recently, with the advantages of high throughput, next-generation sequencing (NGS) technologies were widely used to detect the gene mutations in CMML patients. Recurrent somatic mutations were identified in up to 90% CMML patients, involved in DNA methylation, chromatin and histone modification, cell signaling, transcriptional regulation, and RNA splicing.22 In our data of ten years, gene mutation was detected in 60 patients with 43 patients sequenced in first-generation involving common genes and hot spot mutations. The other 17 patients were examined by NGS and 82.3% (14/17) were detected with gene mutations, which was similar to the mutation rate reported in the literature.25 Notably, TP53 mutation was detected in 5 patients (5/17, 29%), with a median survival of 5 months ranging from 1 to 16 months. TP53 mutation was uncommon (<2%) in CMML patients,26 and did not impact OS, but they independently and negatively impacted leukemia-free survival (LFS).27 In AML, mutations of TP53 gene were strongly associated with a complex aberrant karyotype and negative prognostic impact.28 More attention has been paid to the impact of TP53 on the prognosis of MDS patients. TP53 mutations harbor both mono- and biallelic forms, and Elsa Bernard et al concluded that only multi-hit patients with biallelic mutation were associated with complex karyotype, few co-occurring mutations, high-risk presentation and poor outcomes, and monoallelic patients did not differ from TP53 wild-type patients in outcomes and response to therapy.29
In CMML, the most common mutant genes were TET2 (50–60%), SRSF2 (45–50%), ASXL1 (40–45%), N/KRAS (20–30%), RUNX1 (10–20%).30 In our single-center study, the top three mutation genes were ASXL1MT (11/60, 18.3%), TET2MT (10/60, 16.7%), and SRSF2 MT (9/60, 15.0%). The prognostic roles of gene mutations have not been detected in this study due to the limited cases of CMML enrolled, though literatures reported the association of certain gene mutations and poor prognosis in CMML patients.31 ASXL1 gene was involved in histone modification, and patients with ASXL1MT were more likely to have anemia, leukocytosis, extramedullary disease, and high cytogenetic risk according to the Spanish cytogenetic risk stratification system.32 ASXL1 mutations were the only confirmed independent predictors for the patient outcome, which were included in three prognostic models: the Mayo molecular model, Groupe Francophone des Myélodysplasies model, and the CMML-specific prognostic scoring system-molecular model.3 SRSF2 was pre-mRNA spliceosome, and its mutation was rather common. In a meta-analysis, SRSF2MT did not show any prognostic effect on OS of CMML patients, unlike in MDS with an adverse prognostic risk factor.33 As a tumor suppressor, TET2MT lost its suppressive function and frequently occurred in CMML patients. TET2MT patients tended to be older in age, more likely to have dysplastic CMML, a higher number of co-occurring mutations including ASXL1MT and lower-risk stratification. Importantly, TET2MT was associated with a survival advantage, and the adverse prognostic impact of ASXL1MT was partially mitigated by concurrent TET2MT.34
NPM1 and DNMT3A mutations were also common according to our single-center study, with an incidence of 13.3% (8/60). NPM1 mutations are uncommon in CMML, occurring in <5% of cases; however, the CMML cases with a high NPM1 mutational burden were associated with a higher probability of rapid transition to AML (at a median of 5 months) with myelomonocytic (M4) or monocytic (M5) differentiation and a poorer outcome, even treated with chemotherapy.35,36 The incidence of NPM1 mutation in our study was higher than that reported in the literature. Two patients transformed into AML, and 5 patients survived for 3–14 months, and only 1 patient was still alive after 30 months of follow-up.
Therapy should be started when CMML is symptomatic or progressive.37 More particularly, treatment is initiated with hemoglobin <10 g/dL, bone marrow blasts >5%, platelets <100×109/L, progressive leukocytosis >30×109/L, constitutional symptoms (weight loss, fever), and symptomatic splenomegaly or splenomegaly that is palpable ≥5 cm below the left costal margin.38 The aim of CMML treatments is to effectively control the disease in a long-term manner while maintaining the quality of life (QoL) in patients and to prevent clonal evolution and transition to AML. Currently, specific therapy for CMML has not been approved. Most of the available therapeutic approaches are based on MDS and other MPN studies.39 Twenty-seven patients in our study received palliative treatment with supportive care including hydroxyurea reducing leukocyte or blood component transfusion. Thirty-nine patients received chemotherapy containing hypomethylating agents (HMAs), with hydroxyurea in early stage to reduce leukocytes for short time in some patients. In univariate and multivariate analysis, medical treatments were independent risk factors for OS. The chemotherapy including HMAs prolonged the survival of CMML patients (p < 0.05) but did not affect time to transformation to AML. The HMAs, 5-azacitidine (AZA) and decitabine (DEC), may play an important role in the treatment of MP CMML.40–42 HMAs can effectively reduce leukocytosis and improve splenomegaly and extramedullary lesions. For such treatment, the ORR is approximately 50% (30–60%) and CR rate around 17% (10–20%). Most patients achieved a response after 3 cycles of treatment and median OS is about 29 months (12–37 months).38 The recent large multicenter trial showed that patients with higher risk disease, ie, MP CMML, blasts ≥10%, and higher risk CMML according to the CPSS, have significantly better outcomes with HMAs compared with hydroxyurea or intensive chemotherapy.43 In the early stage, the HMAs used by patients in the chemotherapy group were decitabine for the accessibility of drugs. In the later stage of this study, three patients used AZA. In the literature, the response rates of Azacitidine for the patients was similar between 5-day (75mg/m2/day IV for 5 days every 28 days) and 7-day regimens,44,45 the patients using AZA for 5–7 days were included in the study. In the chemotherapy group of 39 patients, 35 patients did not undergo allogeneic HSCT due to the age or lacking a matched donor, in which 11 patients with HMA monotherapy, and 24 patients with HMAs combined intensive cytotoxic chemotherapy, including HAG, CAG, and IA regimen.12–14 Prolonged myelosuppression was still common in CMML patients. Allogeneic HSCT remains the only curative option for CMML patients but has limited applications owing to its toxicity, patient’s age and difficulty in the identification of suitable donors. Allogeneic HSCT in CMML patients had a response rate of 20–40%, a recurrence rate of 20–40%, and 5-year OS of approximately 20% in retrospective studies.46–48 But complete remission at the time of HSCT in CMML patients was the only significant predictive factor of relapse-free and overall survival.49 In our study, four patients underwent HSCT with sibling matched donors and no comorbidities. They were treated with HMAs before transplantation, and 2 patients achieved complete remission with disease-free survival, the other 2 achieved partial remission who still transformed to leukemia, of which one died within ten months after transplantation. Because of only four patients treated with HSCT, it was difficult to compare survival with not-transplanted patients.
In conclusion, CMML patients in chemotherapy group obtained better OS than those in the supportive group before and after PSM analysis. Subgroup analysis of OS showed that specific subgroups (patients with blast cell ≥10% in bone marrow or WHO CMML-2) may benefit more from chemotherapy treatment. In the PSM cohort, treatment, chromosome karyotype and CPSS were considered as risk factors of OS in univariate analysis with statistical differences. Multivariate analysis showed that supportive therapy, single/multi-lineage of bone marrow dysplasia in smear and intermediate-2/high types in CPSS were independent risk factors for OS after PSM. Both first-line and next-generation sequencing provide direct insight into the molecular mechanism of CMML, which may enable future personalized treatment based on gene mutation for specific patient selection.
Funding Statement
This work was supported by Chen Xiao-ping Foundation for the Development of Science and Technology of Hubei Province (Grants No. CXPJJH12000001-2020343 and CXPJJH12000002-2020058) to Dr. Chao Wang.
Highlights
Patients in chemotherapy group achieved better overall survival than those in supportive group before and after propensity score matching (PSM) analysis.
Patients with blast cell in BM ≥ 10% or WHO CMML-2 benefited more from chemotherapy treatment in subgroup analysis.
Univariate and multivariate analysis indicated supportive therapy and intermediate-2/high in CPSS were independent risk factors for overall survival.
Top three mutated genes were ASXL1MT (18.3%), TET2MT (16.7%) and SRSF2MT (15.0%) in our study.
Data Sharing Statement
All data are available in this article.
Ethics Statement
The retrospective study involving human participants was reviewed and approved by the Medical Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. The informed consent was waived by the Ethics Committee of Tongji Hospital as the retrospective study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
- 1.Bennett JM, Catovsky D, Daniel MT, et al. The chronic myeloid leukaemias: guidelines for distinguishing chronic granulocytic, atypical chronic myeloid, and chronic myelomonocytic leukaemia. Proposals by the French-American-British Cooperative Leukaemia Group. Br J Haematol. 1994;87(4):746–754. doi: 10.1111/j.1365-2141.1994.tb06734.x [DOI] [PubMed] [Google Scholar]
- 2.Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100(7):2292–2302. doi: 10.1182/blood-2002-04-1199 [DOI] [PubMed] [Google Scholar]
- 3.Patnaik MM, Tefferi A. Chronic Myelomonocytic leukemia: 2020 update on diagnosis, risk stratification and management. Am J Hematol. 2020;95(1):97–115. doi: 10.1002/ajh.25684 [DOI] [PubMed] [Google Scholar]
- 4.Valent P, Orazi A, Savona MR, et al. Proposed diagnostic criteria for classical chronic myelomonocytic leukemia (CMML), CMML variants and pre-CMML conditions. Haematologica. 2019;104(10):1935–1949. doi: 10.3324/haematol.2019.222059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. doi: 10.1182/blood-2016-03-643544 [DOI] [PubMed] [Google Scholar]
- 6.Arber DA, Orazi A. Update on the pathologic diagnosis of chronic myelomonocytic leukemia. Modern Pathology. 2019;32(6):732–740. doi: 10.1038/s41379-019-0215-y [DOI] [PubMed] [Google Scholar]
- 7.Such E, Germing U, Malcovati L, et al. Development and validation of a prognostic scoring system for patients with chronic myelomonocytic leukemia. Blood. 2013;121(15):3005–3015. doi: 10.1182/blood-2012-08-452938 [DOI] [PubMed] [Google Scholar]
- 8.Elena C, Gallì A, Such E, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. 2016;128(10):1408–1417. doi: 10.1182/blood-2016-05-714030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patnaik MM, Tefferi A. Chronic myelomonocytic leukemia: 2018 update on diagnosis, risk stratification and management. Am J Hematol. 2018;93(6):824–840. doi: 10.1002/ajh.25104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pleyer L, Leisch M, Kourakli A, et al. Outcomes of patients with chronic myelomonocytic leukaemia treated with non-curative therapies: a retrospective cohort study. Lancet Haematol. 2021;8(2):e135–e148. doi: 10.1016/S2352-3026(20)30374-4 [DOI] [PubMed] [Google Scholar]
- 11.Adès L, Sekeres MA, Wolfromm A, et al. Predictive factors of response and survival among chronic myelomonocytic leukemia patients treated with azacitidine. Leuk Res. 2013;37(6):609–613. doi: 10.1016/j.leukres.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 12.Xie M, Jiang Q, Li L, et al. HAG (Homoharringtonine, Cytarabine, G-CSF) regimen for the treatment of acute myeloid leukemia and myelodysplastic syndrome: a meta-analysis with 2314 participants. PLoS One. 2016;11(10):e0164238. doi: 10.1371/journal.pone.0164238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qian SX, Li JY, Tian T, et al. Effect of low-dose cytarabine and aclarubicin in combination with granulocyte colony-stimulating factor priming (CAG regimen) on the outcome of elderly patients with acute myeloid leukemia. Leuk Res. 2007;31(10):1383–1388. doi: 10.1016/j.leukres.2007.02.009 [DOI] [PubMed] [Google Scholar]
- 14.Beran M, Shen Y, Kantarjian H, et al. High-dose chemotherapy in high-risk myelodysplastic syndrome: covariate-adjusted comparison of five regimens. Cancer. 2001;92(8):1999–2015. doi: [DOI] [PubMed] [Google Scholar]
- 15.Such E, Cervera J, Costa D, et al. Cytogenetic risk stratification in chronic myelomonocytic leukemia. Haematologica. 2011;96(3):375–383. doi: 10.3324/haematol.2010.030957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice. Biometrics. 1996;52(1):249–264. doi: 10.2307/2533160 [DOI] [PubMed] [Google Scholar]
- 17.Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114(5):937–951. doi: 10.1182/blood-2009-03-209262 [DOI] [PubMed] [Google Scholar]
- 18.Sangiorgio VFI, Arber DA, Orazi A. How I investigate chronic myelomonocytic leukemia. Int J Lab Hematol. 2020;42(2):101–108. doi: 10.1111/ijlh.13145 [DOI] [PubMed] [Google Scholar]
- 19.Swerdlow SHCE, Harris NL, Jaffe ES, Pileri SA, Stein H. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues Lyon. France: IARC Press; 2017. [Google Scholar]
- 20.Onida F, Beran M. Chronic myelomonocytic leukemia: myeloproliferative variant. Curr Hematol Rep. 2004;3(3):218–226. [PubMed] [Google Scholar]
- 21.Xicoy B, Triguero A, Such E, et al. The division of chronic myelomonocytic leukemia (CMML)-1 into CMML-0 and CMML-1 according to 2016 World Health Organization (WHO) classification has no impact in outcome in a large series of patients from the Spanish group of MDS. Leuk Res. 2018;70:34–36. doi: 10.1016/j.leukres.2018.05.003 [DOI] [PubMed] [Google Scholar]
- 22.Wassie EA, Itzykson R, Lasho TL, et al. Molecular and prognostic correlates of cytogenetic abnormalities in chronic myelomonocytic leukemia: a Mayo Clinic-French Consortium Study. Am J Hematol. 2014;89(12):1111–1115. doi: 10.1002/ajh.23846 [DOI] [PubMed] [Google Scholar]
- 23.Haase D, Germing U, Schanz J, et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood. 2007;110(13):4385–4395. doi: 10.1182/blood-2007-03-082404 [DOI] [PubMed] [Google Scholar]
- 24.Itzykson R, Fenaux P, Solary E. Chronic myelomonocytic leukemia: myelodysplastic or myeloproliferative? Best Pract Res Clin Haematol. 2013;26(4):387–400. doi: 10.1016/j.beha.2013.09.006 [DOI] [PubMed] [Google Scholar]
- 25.Itzykson R, Kosmider O, Renneville A, et al. Clonal architecture of chronic myelomonocytic leukemias. Blood. 2013;121(12):2186–2198. doi: 10.1182/blood-2012-06-440347 [DOI] [PubMed] [Google Scholar]
- 26.Patnaik MM, Tefferi A. Cytogenetic and molecular abnormalities in chronic myelomonocytic leukemia. Blood Cancer J. 2016;6(2):e393. doi: 10.1038/bcj.2016.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patnaik MM, Vallapureddy R, Yalniz FF, et al. Therapy related-chronic myelomonocytic leukemia (CMML): molecular, cytogenetic, and clinical distinctions from de novo CMML. Am J Hematol. 2018;93(1):65–73. doi: 10.1002/ajh.24939 [DOI] [PubMed] [Google Scholar]
- 28.Haferlach C, Dicker F, Herholz H, et al. Mutations of the TP53 gene in acute myeloid leukemia are strongly associated with a complex aberrant karyotype. Leukemia. 2008;22(8):1539–1541. doi: 10.1038/leu.2008.143 [DOI] [PubMed] [Google Scholar]
- 29.Bernard E, Nannya Y, Hasserjian RP, et al. Implications of TP53 allelic state for genome stability, clinical presentation and outcomes in myelodysplastic syndromes. Nat Med. 2020;26(10):1549–1556. doi: 10.1038/s41591-020-1008-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hunter A, Genomic Landscape PE. Risk stratification in chronic myelomonocytic leukemia. Curr Hematol Malig Rep. 2021;16(3):247–255. doi: 10.1007/s11899-021-00613-9 [DOI] [PubMed] [Google Scholar]
- 31.Jian J, Qiao Y, Li Y, et al. Mutations in chronic myelomonocytic leukemia and their prognostic relevance. Clin Transl Oncol. 2021;23(9):1731–1742. doi: 10.1007/s12094-021-02585-x [DOI] [PubMed] [Google Scholar]
- 32.Patnaik MM, Itzykson R, Lasho TL, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014;28(11):2206–2212. doi: 10.1038/leu.2014.125 [DOI] [PubMed] [Google Scholar]
- 33.Arbab Jafari P, Ayatollahi H, Sadeghi R, et al. Prognostic significance of SRSF2 mutations in myelodysplastic syndromes and chronic myelomonocytic leukemia: a meta-analysis. Hematology. 2018;23(10):778–784. doi: 10.1080/10245332.2018.1471794 [DOI] [PubMed] [Google Scholar]
- 34.Coltro G, Mangaonkar AA, Lasho TL, et al. Clinical, molecular, and prognostic correlates of number, type, and functional localization of TET2 mutations in chronic myelomonocytic leukemia (CMML)-A study of 1084 patients. Leukemia. 2020;34(5):1407–1421. doi: 10.1038/s41375-019-0690-7 [DOI] [PubMed] [Google Scholar]
- 35.Peng J, Zuo Z, Fu B, et al. Chronic myelomonocytic leukemia with nucleophosmin (NPM1) mutation. Eur J Haematol. 2016;96(1):65–71. doi: 10.1111/ejh.12549 [DOI] [PubMed] [Google Scholar]
- 36.Vallapureddy R, Lasho TL, Hoversten K, et al. Nucleophosmin 1 (NPM1) mutations in chronic myelomonocytic leukemia and their prognostic relevance. Am J Hematol. 2017;92(10):E614–E618. doi: 10.1002/ajh.24861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Itzykson R, Fenaux P, Bowen D, et al. Diagnosis and treatment of chronic myelomonocytic leukemias in adults: recommendations from the European hematology Association and the European LeukemiaNet. HemaSphere. 2018;2(6):e150. doi: 10.1097/HS9.0000000000000150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kwon J. Diagnosis and treatment of chronic myelomonocytic leukemia. Blood Res. 2021;56(S1):S5–S16. doi: 10.5045/br.2021.2020321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Comprehensive Cancer Network (NCCN) Msv. Available from: https://www.nccn.org/professionals/physician_gls/pdf/mds.pdf. Accessed September 20, 2022.
- 40.Drummond MW, Pocock C, Boissinot M, et al. A multi-centre Phase 2 study of azacitidine in chronic myelomonocytic leukaemia. Leukemia. 2014;28(7):1570–1572. doi: 10.1038/leu.2014.85 [DOI] [PubMed] [Google Scholar]
- 41.Wijermans PW, Rüter B, Baer MR, et al. Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML). Leuk Res. 2008;32(4):587–591. doi: 10.1016/j.leukres.2007.08.004 [DOI] [PubMed] [Google Scholar]
- 42.Santini V, Allione B, Zini G, et al. A Phase II, multicentre trial of decitabine in higher-risk chronic myelomonocytic leukemia. Leukemia. 2018;32(2):413–418. doi: 10.1038/leu.2017.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liapis K, Kotsianidis I. Approaching first-line treatment in patients with advanced CMML: hypomethylating agents or cytotoxic treatment? Front Oncol. 2021;11:801524. doi: 10.3389/fonc.2021.801524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lyons RM, Cosgriff TM, Modi SS, et al. Hematologic response to three alternative dosing schedules of azacitidine in patients with myelodysplastic syndromes. J Clin oncol. 2009;27(11):1850–1856. doi: 10.1200/JCO.2008.17.1058 [DOI] [PubMed] [Google Scholar]
- 45.Martin MG, Walgren RA, Procknow E, et al. A Phase II study of 5-day intravenous azacitidine in patients with myelodysplastic syndromes. Am J Hematol. 2009;84(9):560–564. doi: 10.1002/ajh.21482 [DOI] [PubMed] [Google Scholar]
- 46.Kröger N, Zabelina T, Guardiola P, et al. Allogeneic stem cell transplantation of adult chronic myelomonocytic leukaemia. A report on behalf of the Chronic Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Br J Haematol. 2002;118(1):67–73. doi: 10.1046/j.1365-2141.2002.03552.x [DOI] [PubMed] [Google Scholar]
- 47.Ocheni S, Kröger N, Zabelina T, et al. Outcome of allo-SCT for chronic myelomonocytic leukemia. Bone Marrow Transplant. 2009;43(8):659–661. doi: 10.1038/bmt.2008.366 [DOI] [PubMed] [Google Scholar]
- 48.Park S, Labopin M, Yakoub-Agha I, et al. Allogeneic stem cell transplantation for chronic myelomonocytic leukemia: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Eur J Haematol. 2013;90(5):355–364. doi: 10.1111/ejh.12073 [DOI] [PubMed] [Google Scholar]
- 49.Symeonidis A, van Biezen A, de Wreede L, et al. Achievement of complete remission predicts outcome of allogeneic haematopoietic stem cell transplantation in patients with chronic myelomonocytic leukaemia. A study of the chronic malignancies working party of the European group for blood and marrow transplantation. Br J Haematol. 2015;171(2):239–246. doi: 10.1111/bjh.13576 [DOI] [PubMed] [Google Scholar]