Abstract
Background
Children with acute pneumonia may be vitamin D deficient. Clinical trials have found that prophylactic vitamin D supplementation decreases children's risk of developing pneumonia. Data on the therapeutic effects of vitamin D in acute childhood pneumonia are limited. This is an update of a Cochrane Review first published in 2018.
Objectives
To evaluate the efficacy and safety of vitamin D supplementation as an adjunct to antibiotics for the treatment of acute childhood pneumonia.
Search methods
We searched CENTRAL, MEDLINE, Embase, and two trial registries on 28 December 2021. We applied no language restrictions.
Selection criteria
We included randomised controlled trials (RCTs) that compared vitamin D supplementation with placebo in children (aged one month to five years) hospitalised with acute community‐acquired pneumonia, as defined by the World Health Organization (WHO) acute respiratory infection guidelines. For this update, we reappraised eligible trials according to research integrity criteria, excluding RCTs published from April 2018 that were not prospectively registered in a trials registry according to WHO or Clinical Trials Registry – India (CTRI) guidelines (it was not mandatory to register clinical trials in India before April 2018).
Data collection and analysis
Two review authors independently assessed trials for inclusion and extracted data. For dichotomous data, we extracted the number of participants experiencing the outcome and the total number of participants in each treatment group. For continuous data, we used the arithmetic mean and standard deviation (SD) for each treatment group together with number of participants in each group. We used standard methodological procedures expected by Cochrane.
Main results
In this update, we included three new trials involving 468 children, bringing the total number of trials to seven, with 1601 children (631 with pneumonia and 970 with severe or very severe pneumonia). We categorised three previously included studies and three new studies as 'awaiting classification' based on the research integrity screen. Five trials used a single bolus dose of vitamin D (300,000 IU in one trial and 100,000 IU in four trials) at the onset of illness or within 24 hours of hospital admission; one used a daily dose of oral vitamin D (1000 IU for children aged up to one year and 2000 IU for children aged over one year) for five days; and one used variable doses (on day 1, 20,000 IU in children younger than six months, 50,000 IU in children aged six to 12 months, and 100,000 IU in children aged 13 to 59 months; followed by 10,000 IU/day for four days or until discharge). Three trials performed microbiological diagnosis of pneumonia, radiological diagnosis of pneumonia, or both.
Vitamin D probably has little or no effect on the time to resolution of acute illness (mean difference (MD) −1.28 hours, 95% confidence interval (CI) −5.47 to 2.91; 5 trials, 1188 children; moderate‐certainty evidence). We do not know if vitamin D has an effect on the duration of hospitalisation (MD 4.96 hours, 95% CI −8.28 to 18.21; 5 trials, 1023 children; very low‐certainty evidence). We do not know if vitamin D has an effect on mortality rate (risk ratio (RR) 0.69, 95% CI 0.44 to 1.07; 3 trials, 584 children; low‐certainty evidence). The trials reported no major adverse events.
According to GRADE criteria, the evidence was of very low‐to‐moderate certainty for all outcomes, owing to serious trial limitations, inconsistency, indirectness, and imprecision.
Three trials received funding: one from the New Zealand Aid Corporation, one from an institutional grant, and one from multigovernment organisations (Bangladesh, Sweden, and UK). The remaining four trials were unfunded.
Authors' conclusions
Based on the available evidence, we are uncertain whether vitamin D supplementation has important effects on outcomes of acute pneumonia when used as an adjunct to antibiotics. The trials reported no major adverse events. Uncertainty in the evidence is due to imprecision, risk of bias, inconsistency, and indirectness.
Keywords: Child, Preschool; Humans; Infant; Anti-Bacterial Agents; Anti-Bacterial Agents/adverse effects; Anti-Bacterial Agents/therapeutic use; Community-Acquired Infections; Community-Acquired Infections/complications; Community-Acquired Infections/diagnosis; Community-Acquired Infections/drug therapy; Pneumonia; Pneumonia/complications; Pneumonia/diagnosis; Pneumonia/drug therapy; Pneumonia/prevention & control; Vitamin D; Vitamin D/administration & dosage; Vitamin D/adverse effects; Vitamin D/therapeutic use; Vitamin D Deficiency; Vitamin D Deficiency/complications; Vitamin D Deficiency/drug therapy; Vitamins; Vitamins/administration & dosage; Vitamins/adverse effects; Vitamins/therapeutic use
Plain language summary
Is vitamin D an effective and safe addition to antibiotics for treating children with acute pneumonia?
What is pneumonia, and how can it be treated?
Pneumonia is inflammation (swelling) of the lungs caused by an infection. Treatment for pneumonia includes antibiotics, providing oxygen through a mask, and other supportive therapies. Vitamin D boosts immune defences and reduces excessive inflammation: these effects may help children recover from an episode of pneumonia.
What did we want to find out?
We wanted to find out if vitamin D, taken together with antibiotics, can help children to recover from an episode of pneumonia.
What did we do?
We searched for trials that looked at vitamin D compared with placebo (dummy treatment) in children aged between one month and five years who had pneumonia. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
Study characteristics
We included seven trials involving 1601 children from low‐ and middle‐income countries. In five trials, children received a single large dose of vitamin D when they joined the trial or within 24 hours of admission to hospital. In two trials, children received vitamin D for five days. One trial excluded children with normal vitamin D levels. Two trials reported the cause of children's pneumonia.
Key results
Vitamin D probably has little or no effect on the time it takes children to get better from pneumonia. We do not know if vitamin D has an effect on the time children spend in hospital or the number of children who die. The studies reported no major harmful events.
What are the limitations of the evidence?
We have only moderate confidence in the evidence on the time it took children to recover from pneumonia, because all children in this comparison were from low‐income regions, so the results may not apply to higher‐income populations. We have little confidence in the evidence on death rate, because of the same applicability problem outlined above, and because the result was compatible with both appreciable benefit and harm. We have very little confidence in the evidence on time spent in hospital, because of the same applicability problem outlined above, because the children and health providers in one study knew what the allocated treatment was, and because the results were very inconsistent across the studies included in the comparison.
How up to date is the evidence?
The evidence is current to 28 December 2021.
Summary of findings
Summary of findings 1. Vitamin D compared with placebo for acute childhood pneumonia.
| Vitamin D compared with placebo for acute childhood pneumonia | ||||||
|
Patient or population: children with acute pneumonia Settings: hospital setting Intervention: vitamin D Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Vitamin D | |||||
|
Time to resolution of acute illness (Follow‐up varied from 2 to 14 days) |
Mean time in the control group ranged from 50.8 hours to 119.52 hours. |
Mean time in the intervention group was 1.28 hours less (5.47 hours less to 2.91 hours more). | — | 1188 (5 studies) | ⊕⊕⊕⊝ Moderatea | The appropriate effect measure for time‐to‐event data is hazard ratio; however, the studies reported this information as continuous data. |
|
Duration of hospitalisation (Follow‐up varied from 2 to 14 days) |
Mean duration in the control group ranged from 106.82 hours to 248.4 hours. | Mean duration in the intervention group was from 4.96 hours more (8.28 hours less to 18.21 hours more). | — | 1023 (5 studies) | ⊕⊝⊝⊝ Very lowa,b,c | 3 studies reported median values; we converted them to means and standard deviations. |
|
Mortality rate (Follow‐up time varied from 2 to 14 days) |
97 per 1000 | 94 per 1000 (6 to 1000) |
RR 0.69 (0.44 to 1.07) | 584 (3 studies) |
⊕⊕⊝⊝ Lowa,d | Only 3 trials reported the important outcome of mortality rate. In the remaining studies, either no deaths occurred or the trial authors did not report them. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious indirectness: this comparison only included studies from low‐income regions with high baseline prevalence of vitamin D deficiency (results not generalisable). bDowngraded one level for serious risk of bias concerns: one study had unclear risk of attrition and reporting bias and the other had high risk of performance bias. cDowngraded one level for serious inconsistency: statistical heterogeneity was substantial (I² = 73%) and significant (P = 0.005). dDowngraded one level for serious imprecision: 95% CI includes appreciable harm and benefit.
Background
Description of the condition
Pneumonia is an acute lower respiratory tract infection that primarily affects the lungs. Microscopically, the alveoli are filled with exudative fluid (pus), which compromises breathing and gas exchange in the lungs (Scott 2012). Clinical manifestations of acute childhood pneumonia include cough, fever, breathing difficulty, lower chest wall indrawing, and hypoxia (Das 2021; Scott 2012). The most common aetiological agents are bacteria and viruses (e.g. Streptococcus pneumoniae, Haemophilus influenzae, and respiratory syncytial virus; Mathew 2015).
Risk factors for acute childhood pneumonia include mixed feeding or non‐breastfeeding, undernutrition, indoor air pollution, prematurity, overcrowding, and lack of immunisation against measles (Goyal 2021; Rudan 2008). In 2019, of the 5.3 million deaths of children aged up to five years globally, 49.2% were due to infectious diseases (Perin 2022), and 13.9% (0.74 million) were attributed to pneumonia (Perin 2022).
The management of acute childhood pneumonia includes antibiotics, oxygen therapy, other supportive therapy, and, in severe cases, assisted ventilation (Chee 2022; Lassi 2014; Lodha 2013). Studies investigating the effects in this population of nutritional supplements such as zinc, vitamin A, and vitamin C have produced unfavourable results (Das 2012; Haider 2011a; Haider 2011b; Hemilä 2013; Mathew 2010; Wahed 2008). Similarly, over‐the‐counter medications (e.g. mucolytics and antitussives) have shown no beneficial effects (Chang 2014).
Description of the intervention
Vitamin D is a fat‐soluble vitamin that plays an important role in calcium and phosphorous homeostasis and bone mineralisation (Wagner 2008). There are two types: vitamin D₂ (ergocalciferol), which is derived from plants, and vitamin D₃ (cholecalciferol), which is derived from animals. Vitamin D is primarily synthesised in the skin (as vitamin D₃) after exposure to ultraviolet B radiation; less than 10% is derived from dietary sources (McAllister 2006; Munns 2016). The main form circulating in the blood is 25‐hydroxy‐vitamin D (25(OH)‐D), which is synthesised in the liver, and the active or true hormonal form is 1,25‐dihydroxyvitamin D (1,25(OH)₂‐D or calcitriol), which is synthesised in the kidneys (Munns 2016; Walker 2009). The active form binds to the vitamin D receptor (VDR) present in the nucleus, before orchestrating a wide range of actions in the body (Walker 2009). VDR is present in cells of almost every organ system of the body, including immune cells. The best available parameter to indicate the status of vitamin D in the body is blood 25(OH)‐D level, owing to the long half‐life of this substance. This method is used to define the status of vitamin D in children, as follows (Munns 2016).
Sufficient (50 to 250 nmol/L)
Insufficient (37.5 to 50 nmol/L)
Deficient (37.5 nmol/L or less)
Severely deficient (12.5 nmol/L or less)
Excessive (more than 250 nmol/L)
Most multivitamins (which come in liquid, tablet, and capsule form) include vitamin D as a nutritional supplement (doses vary from 50 IU to 1000 IU). Intramuscular injections may be indicated in special circumstances. The recommended daily dose for children and adolescents is 400 IU. The upper limit should not exceed 2000 IU per day in children aged over one year, and 1000 IU per day in infants aged up to one year. However, children with vitamin D deficiency can receive a daily dose of 1000 IU to 10,000 IU (depending on the child's age) for two to three months to enable the serum vitamin D level to normalise (Munns 2016).
Vitamin D deficiency or insufficiency is prevalent in low‐income countries (Joshi 2014; Kelishadi 2014; Thacher 2012; Torun 2013; Zhang 2013), and also occurs in high‐income countries (Grant 2009; Mansbach 2009; Ward 2007). One 10‐year data series reported 126 cases of vitamin D deficiency rickets in Australia (Robinson 2006), and one two‐year data series reported 104 cases in Canada (Ward 2005). In the USA and the UK, there are no definitive prevalence estimates for vitamin D deficiency rickets. Historical prevalence estimates from the USA indicate increases from 65 instances between 1975 and 1985 to 166 instances between 1986 and 2003 (Weisberg 2004); there were 62 instances between 2004 and 2006 (McAllister 2006; Mylott 2004). Vitamin D deficiency rickets remains a significant public health problem in other parts of the world (Joshi 2014; Wondale 2005).
Variables associated with vitamin D deficiency are: increased urbanisation, time spent indoors, and use of sunscreen; increasing latitude; seasonal change (winter or rainy season); air pollution; prematurity; and malabsorptive disorders (Munns 2016). Vitamin D deficiency substantially increases risk of pneumonia amongst children aged up to five years (Akeredolu 2021; Binks 2014; Najada 2004; Oktaria 2021). Studies have also found a link between single nucleotide polymorphisms (SNPs) of genes related to the VDR, and susceptibility to respiratory syncytial virus infection (Janssen 2007). Few trials that provided vitamin D supplements to children with pneumonia have reported a reduction in recurrent episodes (Manaseki‐Holland 2010; Singh 2019).
How the intervention might work
Vitamin D is thought to boost mucosal immune defences and reduce excessive inflammation (Pfeffer 2012). The immune‐enhancing actions of vitamin D include induction of monocyte differentiation, inhibition of lymphocyte proliferation, stimulation of phagocytosis‐dependent and antibody‐dependent macrophages, and modulation of cytokine and antibody‐producing lymphocytes (Liu 2006; Raloff 2006; White 2008). Hydroxylation of vitamin D to the active form occurs in the kidneys by the enzyme 1‐alpha hydroxylase or CYP27B1; the same hydroxylation pathway also operates in other cells that participate in immune regulation, such as epithelial cells and monocyte‐macrophages (Hewison 2011). In the airways (bronchial epithelial cells), 1‐alpha hydroxylase activity increases in response to any acute insult or inflammatory stimulus (Hansdottir 2008). Cathelicidin is an antimicrobial peptide whose expression is increased over immune cells in response to infection, and the whole cascade depends on vitamin D (Gombart 2005; White 2008). As a result, the vitamin D/cathelicidin‐circuit is activated in acute respiratory tract infections, including pneumonia. Experimental models have shown that vitamin D dampens adaptive immune responses and modulates key elements of innate immune response in dendritic cells following S pneumoniae infection (Olliver 2013). Vitamin D also confers antiviral properties that affect the role of toll‐like receptors (TLR), particularly TLR7 (Alvarez‐Rodriguez 2012).
Some studies have shown that daily vitamin D supplementation has better therapeutic efficacy than large bolus doses for pneumonia, tuberculosis, and fracture in older adults (Heaney 2012; Hollis 2011; Manaseki‐Holland 2012; Martineau 2012; Nielsen 2010). Clinical studies have shown that vitamin D at a higher dose could be immunosuppressive. Kimball 2011 investigated high‐dose vitamin D (10,000 IU per day) and found suppressed proliferative response of peripheral blood monocytes. The findings of Manaseki‐Holland and colleagues supported this finding (Manaseki‐Holland 2012). In one study, large bolus doses (100,000 IU) of vitamin D four times per year in infants led to slightly increased risk of repeat episodes of all types of pneumonia and mortality (Manaseki‐Holland 2010). However, the same study found a 13% reduced risk of clinically defined pneumonia up to three months after vitamin D treatment in children who received a single large bolus dose of 100,000 IU (Manaseki‐Holland 2010). This may mean that the immunological effectiveness of vitamin D is blunted at extremes of dosages (either very high or low therapeutic dose).
Why it is important to do this review
Pneumonia is a leading cause of global mortality in children aged up to five years; more than 90% of deaths occur in low‐income countries (Perin 2022). Although antibiotic therapy is the main treatment for pneumonia, irrational use has contributed to increasing resistance. In addition, most children in low‐income countries have limited access to healthcare facilities. Vitamin D is a relatively simple intervention that may be a helpful addition to standard treatment for acute childhood pneumonia. Due to its low cost and ease of administration, vitamin D can be administered to children with acute pneumonia. Vitamin D, as an adjunct to antibiotics, may help to reduce childhood mortality from pneumonia. In a previous review, we found no role for oral vitamin D supplementation in children aged under five with acute pneumonia (Das 2013). This Cochrane Review includes updated searches to assist healthcare providers in making informed decisions about providing vitamin D for children with acute pneumonia.
Objectives
To evaluate the efficacy and safety of vitamin D supplementation as an adjunct to antibiotics for the treatment of acute childhood pneumonia.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Children aged from one month to five years, hospitalised with a clinical diagnosis of community‐acquired pneumonia (CAP). We defined pneumonia according to the World Health Organization (WHO) acute respiratory infection guidelines (Scott 2012). We defined pneumonia as the presence of age‐specific tachypnoea (more than 60 breaths per minute in children aged up to two months; more than 50 breaths per minute in children aged from two months to 11 months; and more than 40 breaths per minute in children aged from 12 months to 60 months) with or without cough or fever. We defined severe pneumonia as the presence of age‐specific tachypnoea along with lower chest wall indrawing or any of the danger signs (cyanosis, inability to feed, or lethargy). We excluded trials that enrolled children with other debilitating diseases, severe wasting (weight for height z‐score below −3), asthma or other respiratory diseases, hospital‐acquired pneumonia, or postoperative conditions.
Types of interventions
Interventions began after diagnosis of CAP. The interventions consisted of treatment with vitamin D as an adjunct to antibiotics and other supportive measures. The trials compared vitamin D with placebo only. We considered any dose schedule (low or high dose, daily dose or bolus dose, any duration) and any route (oral or injection).
Types of outcome measures
Outcome measures frequently used to determine the clinical efficacy of any acute pneumonia treatment are time to resolution of illness, duration of hospitalisation, treatment failure, adverse events, and mortality.
Primary outcomes
Time to resolution of acute illness
Duration of hospitalisation
We defined time to resolution of acute illness as the time needed to achieve the following parameters from treatment initiation: respiratory rate below age‐specific cutoff, no lower chest indrawing, no danger signs or hypoxia, and ability to feed. These parameters had to be present for at least two consecutive days or 48 hours. We defined duration of hospitalisation as the time period between trial enrolment and discharge.
Secondary outcomes
Time to resolution of tachypnoea
Time to resolution of lower chest wall indrawing
Time to resolution of hypoxia (blood oxygen saturation below 95%)
Time to resolution of fever
Time to resolution of inability to feed or lethargy
Treatment failure rate
Mortality rate
Adverse events (if any)
We defined treatment failure as no reduction in breathing rate after 48 hours compared to the rate recorded at enrolment.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases.
Cochrane Central Register of Controlled Trials (CENTRAL) 2021, Issue 12, part of the Cochrane Library (accessed 28 December 2021), which contains the Cochrane Acute Respiratory Infections (ARI) Group's Specialised Register
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) (1946 to 28 December 2021)
Embase (2010 to 28 December 2021)
We used the search strategy presented in Appendix 1 to search CENTRAL and MEDLINE. The MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE (sensitivity‐ and precision‐maximising version, 2008 revision, Ovid format; Lefebvre 2011; Schünemann 2011). We adapted the search strategy to search Embase (Appendix 2).
Searching other resources
We searched the following clinical trials registries for ongoing trials on 28 December 2021.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov)
WHO International Clinical Trials Registry Platform (ICTRP; www.who.int/clinical-trials-registry-platform)
We also searched the Journal of Orthomolecular Medicine (isom.ca/jom/; 1986 to December 2021), which focuses on dietary supplements for illness. We contacted researchers in the relevant field to identify additional trials that may be eligible for inclusion. We also checked the reference lists of all trials identified.
Data collection and analysis
Selection of studies
Two review authors (RRD, SSN) independently screened titles and abstracts to identify potentially relevant trials. When they could not ascertain relevance from the titles or abstracts, they retrieved the full text for assessment. The same two review authors independently assessed the eligibility of potentially relevant trials by evaluating the full‐text reports and completing eligibility forms designed in accordance with the specified inclusion criteria. They resolved any differences in opinion through discussion or by consulting the third review author (MS) when necessary. We described excluded trials in a Characteristics of excluded studies table, along with reasons for their exclusion. In the case of conference abstracts, if additional data were not forthcoming, we used the information provided in the abstract. We contacted trial authors where we required clarification or additional information.
Research integrity screening
Cochrane defines a problematic study as "Any published or unpublished study where there are serious questions about the trustworthiness of the data or findings, regardless of whether the study has been formally retracted; scientific misconduct will not be the only reason that a study might be problematic; problems may result from poor research practises or honest errors" (Cochrane policy – managing problematic studies). Following suggestions from the Cochrane Research Integrity Editor to identify and handle problematic trials, we changed the inclusion criteria for this update. We considered research integrity of the individual trial as an important eligibility criteria. Some useful tools are available for evaluation of publication integrity, such as the REAPPRAISED checklist (Grey 2020). The Cochrane Pregnancy and Childbirth Group has also developed a data extraction sheet that addresses scientific integrity and trustworthiness (Alfirevic 2021). In addition, there is available implementation guidance on the Cochrane policy of managing potentially problematic trials (Implementation guidance – problematic studies). We used the Cochrane implementation guidance, and adopted the tool described in Popp 2022 and Weibel 2022. Two review authors (RRD, SSN) independently evaluated the newly included trials and previously included trials for research integrity. Trials were eligible if there were no issues related to the following critical criteria.
Retraction notice or expression of concern
Trial registration (as per guidelines of the WHO (WHO 2018) and Clinical Trials Registry – India (CTRI; Shetty 2021)
Ethics committee approval
Plausible trial authorship
Sufficient description of trial methods (e.g. randomisation, blinding, allocation concealment, and loss to follow‐up)
Plausibility of trial results
We excluded trials that were retracted or had expressions of concerns published, and trials published from April 2018 that had not been registered in a trial registry, as per the guidelines of the WHO (WHO 2018) and Clinical Trials Registry – India (CTRI; Shetty 2021). We did not apply the criterion of trial registration to trials published before April 2018, when it was not mandatory to register clinical trials in India. We moved previously included trials to Characteristics of studies awaiting classification if there were issues with the other four criteria listed above, or if the trial authors had not responded to our email queries regarding trial methodology or results.
Data extraction and management
We extracted the following information from each trial using a piloted data extraction form.
Author
Year
Location (country)
Setting (hospital or community)
Method of recruitment
Inclusion criteria
Unit of analysis
Allocation ratio
Risk of bias
Participant data (age, sex, sample size, pneumonia or severe pneumonia)
Intervention (dosage, duration, frequency, and co‐intervention, if any)
Outcomes (outcome definition, valid unit of measurement, time points of collection and reporting)
Loss to follow‐up
Key conclusions
References to other relevant trials
Two review authors (RRD, SSN) independently extracted data from the trials, resolving any discrepancies through discussion or by consulting the third review author (MS). For dichotomous data (e.g. mortality or adverse events), we extracted the number of participants experiencing the condition and the total number of participants in each treatment group. For continuous data (e.g. time to resolution or duration of illness), we used the arithmetic mean and standard deviation (SD) for each treatment group together with the number of participants in each group. If trials reported standard error (SE), we converted it to SD. If trials reported geometric means, we recorded this information and extracted the SD on the log scale. If trials used medians, we derived mean and SD using established methods (Hozo 2005; Luo 2018; Wan 2014). If the report provided a 95% confidence interval (CI) instead of a mean and SD for continuous data, we extracted the mean and SD from the 95% CI.
Assessment of risk of bias in included studies
Two review authors (RRD, SSN) independently assessed methodological quality using the Cochrane risk of bias tool (RoB 1; Higgins 2011). We assessed included trials based on the following six components.
Method of sequence generation
Allocation concealment
Blinding of participants, health providers, and outcome assessors
Incomplete outcome data
Selective outcome reporting
Other biases (including detection bias, e.g. differential effort to locate death records for the intervention and control groups)
We presented findings in risk of bias tables with the review authors' judgement (low, high, or unclear risk of bias) and support for the judgement. We also reported the results in risk of bias graphs. We attempted to contact the trial authors for clarification where data were missing, or where we needed clarification about reporting. A third review author (MS) resolved any disagreements. Further details about the risk of bias tool are provided in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011). Had we identified any cluster‐RCTs, we would have looked for sources of bias originating from differences between individually randomised trials and cluster‐RCTs (e.g. the relationship between allocation concealment and recruitment bias may be greater in cluster‐RCTs).
Measures of treatment effect
We extracted and entered outcome data into Review Manager 5 (RevMan 5) software for statistical analysis (Review Manager 2014). We used the standard methods of the Cochrane Acute Respiratory Infections (ARI) Review Group to synthesise data. Outcomes with continuous data included time to resolution of acute illness; duration of hospitalisation; and time to resolution of tachypnoea, lower chest wall indrawing, hypoxia, fever, and inability to feed or lethargy. For continuous data, we calculated mean differences (MDs) with 95% CIs to estimate the treatment effect. Where trials provided data as medians and ranges, including interquartile ranges (IQRs), we first derived the mean and SD, then calculated the MD and 95% CI. Outcomes with dichotomous data included treatment failure rate, mortality rate, and adverse events rate. For dichotomous data, we calculated risk ratios (RRs) with 95% CIs.
Unit of analysis issues
Trials that randomise units other than individuals (i.e. clusters), should present results with controls for clustering (e.g. robust SEs or hierarchical linear models). We included no cluster‐randomised trials in our review, so we had no unit of analysis issues.
Dealing with missing data
We described missing data, including dropouts, and reported reasons for dropouts. Differential dropout rates can lead to biased estimates of the effect size, and bias may arise if the reasons for dropping out differ across groups. If data were missing, or if trials did not report reasons for dropouts, we contacted the trial authors for further information. When trials performed analyses with only completer data and also analyses that controlled for dropouts (ITT), we extracted the ITT analyses.
Assessment of heterogeneity
We assessed included trials for clinical, methodological, and statistical heterogeneity. We assessed clinical heterogeneity by comparing the distribution of important factors such as trial participants, trial setting, dose and duration of the intervention, and co‐interventions. We evaluated methodological heterogeneity on the basis of factors such as the method of sequence generation, allocation concealment, blinding of outcome assessment, and losses to follow‐up. We used the Chi² test for statistical heterogeneity between trials and considered P ≤ 0.10 as indicating significant heterogeneity. We used the I² statistic to assess the magnitude of heterogeneity, basing our interpretation on the following considerations (Higgins 2011).
0% to 40%: might not be important
30% to 60%: may represent moderate heterogeneity
50% to 90%: may represent substantial heterogeneity
75% to 100%: considerable heterogeneity
The importance of the observed I² value depends on the magnitude and direction of effects, and on the strength of evidence for heterogeneity (e.g. P value from the Chi² test, or CI for I²). Uncertainty in the value of I² is substantial when the number of trials is small.
Assessment of reporting biases
We undertook a comprehensive electronic search and searched trial registries to minimise the effects of publication bias. Had we identified 10 or more trials reporting the primary outcomes, we would have created funnel plots of effect estimates against their SEs (on a reversed scale) using RevMan 5 (Review Manager 2014). However, the primary outcome data were pooled from less than 10 trials, precluding the construction of funnel plots.
Data synthesis
We carried out statistical analyses using RevMan 5 (Review Manager 2014). We performed meta‐analyses using a random‐effects model due to the presence of clinical heterogeneity. We did not include any cluster‐RCTs. We calculated overall effects using inverse variance methods. We presented results as the average treatment effect with 95% CI and Tau² and I² estimates.
Subgroup analysis and investigation of heterogeneity
In this updated review, we conducted subgroup analyses and investigated possible sources and causes of heterogeneity in the pooled analysis of primary outcome measures involving different dose schedules of vitamin D (low or high dose, single bolus or daily dose, oral or parenteral route, duration of less or more than five days). We did not conduct subgroup analysis for population (aged up to one year or one to five years, boys or girls), trial setting (hospital or community, outpatient or inpatient, low‐, middle‐, or high‐income countries), aetiology (bacterial or viral pneumonia), or severity of illness (pneumonia, severe pneumonia, or very severe pneumonia) as there were too few trials.
Sensitivity analysis
In this updated review, we conducted a sensitivity analysis to explore the effect of trial quality on results. This involved excluding trials at risk of bias (selection, performance, detection, attrition, or reporting bias) to assess for any substantive difference to the overall result. We did not investigate the effects of the randomisation unit (individual versus cluster) on the outcomes, as we identified no eligible cluster‐RCTs. We explored the effects of fixed‐effect or random‐effects analyses for outcomes with statistical heterogeneity. We used primary outcomes in sensitivity analyses.
Summary of findings and assessment of the certainty of the evidence
We created a summary of findings table with the following outcomes.
Time to resolution of acute illness
Duration of hospitalisation
Mortality rate
We used the five GRADE considerations (risk of bias, inconsistency, imprecision, indirectness, and publication bias) to assess the certainty of a body of evidence as it related to the trials that contributed data for the prespecified outcomes (Atkins 2004). We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011), employing GRADEpro GDT software (GRADEpro GDT). We justified all decisions to downgrade the certainty of the evidence using footnotes, and made comments to aid the reader’s understanding of the review where necessary. Where it was not possible to carry out a meta‐analysis, we summarised the data for each trial.
Results
Description of studies
Results of the search
After deduplication, we retrieved 1209 records (MEDLINE: 514; CENTRAL: 2; Embase: 690; Google Scholar: 3) in an updated search covering the period July 2018 to December 2021. Two review authors (RRD, SSN) excluded 1201 records based on the title and abstract screen. We retrieved the full‐text reports of the remaining eight records, which corresponded to eight separate trials, and assessed them against our eligibility criteria. We excluded two new trials: one did not study pneumonia specifically (Jadhav 2021), and the other did not report outcomes for acute pneumonia (Singh 2019). Of the six remaining trials, one had been classified as ongoing in the previous version of this review, but had since been published (Chowdhury 2021). The second trial classified as ongoing in the previous version of this review was not recruiting at the time of our updated search and had no update posted since 4 February 2014; it remains in the ongoing category for this update (NCT02054182).
Eligibility screening for research integrity
We re‐assessed all eligible trials for issues related to research integrity. Of the 13 eligible trials (seven included in the previous review and six deemed potentially eligible for inclusion in this update), four passed all the criteria of research integrity screening (Chowdhury 2021; Gupta 2016; Labib 2021; Somnath 2017). Three trials provided no information about registration (Choudhary 2012; Jingi 2018; Manaseki‐Holland 2010). However, as they were published on or before 2018, the trial registration criterion did not apply to them, and as they passed all other criteria of research integrity screening, we included them in this update. The remaining six trials did not meet one or more criteria in addition to trial registration, and were moved to Studies awaiting classification (Bisht 2017; Dhungel 2015; Gaber 2018; Rahmati 2016; Rajshekhar 2016; Shamaoon 2018). See Figure 1.
1.
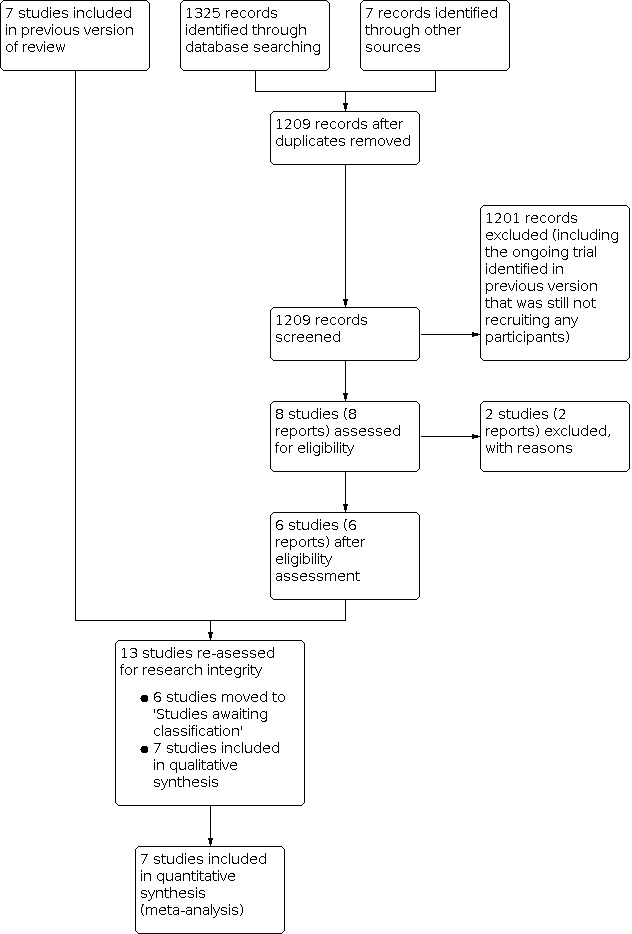
Study flow diagram.
Included studies
We included seven RCTs involving a total of 1601 children (631 with pneumonia and 970 with severe or very severe pneumonia) after applying the research integrity criteria (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021; Manaseki‐Holland 2010; Somnath 2017). See Characteristics of included studies table. All trials were conducted in low‐ and middle‐income countries (LMICs). Participant characteristics, aetiological agents, and prevalence of vitamin D deficiency appeared to be very similar across trials. The trials differed in terms of inclusion criteria and dose and duration of vitamin D use. Three trials received funding: one from the New Zealand Aid Corporation, one from an institutional grant, and one from multigovernment organisations (Bangladesh, Sweden, and UK). The remaining four trials were unfunded.
Choudhary 2012 was a single‐centre trial conducted in India that aimed to determine the role of oral vitamin D supplementation for resolution of severe pneumonia in children. The trial enrolled 200 children (100/100, intervention/control) aged between two months and five years who were hospitalised with WHO‐defined severe pneumonia. Thirty per cent of children in the vitamin D group and 33% of children in the control group had a history of recurrent pneumonia. Five children had clinical evidence of rickets. One‐third of the children had wheezing at enrolment.
Children in the intervention arm received oral vitamin D₃ for five days at a dose of 1000 IU (for those aged up to one year) or 2000 IU (for those aged over one year). Children in the placebo arm received lactose alone. The children received antibiotics in accordance with the Indian Academy of Pediatrics (IAP) 2006 guidelines (IAP 2006). The guidelines recommend the following age‐specific drug combinations.
Infants aged up to three months: cefotaxime/ceftriaxone with or without gentamicin/amikacin as first‐line therapy and co‐amoxyclav plus gentamicin/amikacin as second‐line therapy
Children aged three months to five years: ampicillin/chloramphenicol or ampicillin plus chloramphenicol or co‐amoxyclav as first‐line therapy and co‐amoxyclav or cefotaxime/ceftriaxone as second‐line therapy
Children with staphylococcal infection: in addition to age‐specific treatment combinations, adjuvant therapy with cloxacillin as first‐line therapy and vancomycin/teicoplanin as second‐line therapy
Primary trial outcomes were time to resolution of severe pneumonia (absence of lower chest indrawing, hypoxia, cyanosis, and lethargy with inability to feed). Secondary outcomes were duration of hospitalisation, time to resolution of tachypnoea, chest retraction, and inability to feed.
Chowdhury 2021 was a single‐centre trial conducted in Bangladesh that aimed to determine the role of oral vitamin D supplementation for resolution of severe pneumonia in children. The trial enrolled 197 children (97/100, intervention/control) aged between two months and five years who were hospitalised with WHO‐defined severe pneumonia. Children who presented with severe malnutrition with any sign of pneumonia were also considered to have severe pneumonia. Most children (n = 134, 68%) were infants. Nearly half of children were severely malnourished. Nearly one‐third had a repeat episode of pneumonia. Vitamin D deficiency was present in 21% of children in the intervention group and 35% in the placebo group (P = 0.02).
Children in the intervention arm received oral vitamin D₃ (liquid formulation as Vigantol oil) at a dose of 20,000 IU (for those aged up to six months), 50,000 IU (for those aged between six and 12 months), or 100,000 IU (for those aged between 13 and 59 months) on day 1, followed by 10,000 IU daily thereafter for four days or until discharge. Children in the placebo arm received miglyol oil 812 (vehicle used in Vigantol oil). First‐line parenteral antibiotics included ampicillin and gentamicin. Children who did not respond (no improvement after 48 hours or deterioration of pneumonia signs or symptoms after 24 hours of initiation of antibiotics) were switched to second‐line antibiotics (ceftriaxone and levofloxacin).
Primary trial outcomes were time to resolution of severe pneumonia (absence of tachypnoea, lower chest indrawing, hypoxia or lethargy, cyanosis, convulsion, or inability to feed). Secondary outcomes were duration of hospitalisation, time to resolution of tachypnoea, hypoxia, and chest indrawing.
Gupta 2016 was a single‐centre trial conducted in India that aimed to determine the role of oral vitamin D supplementation for the treatment and prevention of pneumonia in children. The trial enrolled 324 children (162/162, intervention/control) aged between six months and five years who were hospitalised with WHO‐defined severe pneumonia. The prevalence of moderate malnutrition according to the WHO definition was 21.3%. The prevalence of anaemia (haemoglobin below 11 g/dL) was 82.4%. The prevalence of hypocalcaemia was 55.9%, and the prevalence of hypophosphataemia was 31.4%. Vitamin D deficiency was present in 37.6% of children in the vitamin D group and 40.1% of children in the placebo group. Blood culture was positive in 8.6% (Staphylococcus aureus isolated in 8.3%). Around 90% of children had abnormal chest X‐ray findings (consolidation, bilateral patchy opacities, hyperinflation, or minor infiltrates). Wheezing was present in 84.6% of children in the vitamin D group and 78.4% of children in the control group.
Children in the intervention arm received a single oral dose of vitamin D₃ of 100,000 IU on the day of enrolment. Children in the placebo arm received a product similarly prepared and given as a single dose on the day of enrolment. The children received antibiotics according to IAP 2006 guidelines, as specified for Choudhary 2012 (IAP 2006).
Primary trial outcomes were time to resolution of severe pneumonia (time from enrolment to absence of chest indrawing for 24 hours) and proportion of children with recurrent pneumonia over the following six months. Secondary outcomes were change in serum levels of 25(OH)‐D and parathyroid hormone after two weeks and three months of therapy, change in serum levels of cathelicidin and immunoglobulins after two weeks of therapy, duration of hospitalisation, time to complete recovery from pneumonia (normalisation of respiratory rate), fever clearance time, and repeat episodes of pneumonia.
Jingi 2018 was a single‐centre trial conducted in India that aimed to determine if supplementation of oral vitamin D₃ with antibiotics reduced duration of hospitalisation in children with pneumonia. The trial enrolled 80 children (40/40, intervention/control) aged between two months and 60 months who were hospitalised with WHO‐defined acute pneumonia. Severe pneumonia was present in 37.5% of the children randomised; the remainder had pneumonia. Previous pneumonia episodes had affected 17.5% of the children. All children received penicillin G as first‐line antibiotic treatment or cefotaxime as second‐line antibiotic treatment in addition to supportive care.
Children in the intervention arm received a single dose (300,000 IU) of intramuscular vitamin D₃ within 24 hours of admission. Children in the control arm received a sterile water injection. Study outcomes were time to resolution of illness and repeat episodes of pneumonia.
Labib 2021 was a single‐centre trial conducted in Egypt that aimed to determine if supplementation of oral vitamin D₃ with antibiotics reduced the time to resolution of pneumonia in children with pneumonia and insufficient or deficient vitamin D levels. The trial enrolled 191 children (93/98, intervention/control) aged between one month and 12 years who were hospitalised with WHO‐defined acute pneumonia. Severe pneumonia was present in 65% of children randomised; the remainder had pneumonia. More than 46% of children had comorbidities. All children received antibiotics as per the WHO 2014 pneumonia treatment guideline (WHO 2014).
Although Labib 2021 did not comply with our predefined inclusion criteria (it included children up to 12 years of age), we decided to include the trial because the median age and IQR were below five years. This means either there were no children aged over five years, or the number of children aged over than five years was negligible. We felt that excluding the trial (which included children with pneumonia and severe pneumonia) may have introduced bias. We contacted the corresponding authors to request data, but these data were unavailable (Labib 2022 [pers comm]).
Children in the intervention arm received a single dose (100,000 IU) of intramuscular vitamin D₃ within 24 hours of admission. Children in the control arm received a saline injection. Study outcomes assessed were laboratory and biochemical parameters, duration of hospitalisation, time to resolution of illness, and mortality.
Manaseki‐Holland 2010 was a single‐centre trial conducted in Afghanistan that aimed to determine whether oral vitamin D₃ supplementation with antibiotics reduced duration of illness in children with pneumonia. The trial enrolled 453 children (224/229, intervention/control) aged between one month and 36 months with WHO‐defined acute pneumonia treated in outpatient and inpatient settings. Amongst the children randomised, severe pneumonia was present in 17.4% of the intervention group and 15.3% of the placebo group; the remaining children had pneumonia. The trial excluded children with very severe pneumonia. All children received antibiotics as per the WHO Integrated Management of Childhood Illness (IMCI) guidelines: children aged up to two months received intramuscular gentamicin and intramuscular benzylpenicillin, and children aged from two months to five years received oral amoxicillin, or intramuscular chloramphenicol if oral administration was not possible (WHO 2005).
Although Manaseki‐Holland 2010 did not comply with all predefined inclusion criteria (not all children were treated as inpatients), we decided to include the trial because many participants had pneumonia. We felt that excluding the trial (which included children with pneumonia and severe pneumonia) may have introduced bias.
Children in the intervention arm received a single dose (100,000 IU) of oral vitamin D₃ at onset of pneumonia. Children in the placebo arm received olive oil alone. All children received antibiotics according to the national pneumonia treatment protocol based on IMCI guidelines.
Study outcomes were time to recovery (respiratory rate below 40 breaths per minute, no danger signs or subcostal recession, and no fever, for 48 consecutive hours), treatment failure, and pneumonia recurrence.
Somnath 2017 was a single‐centre trial conducted in India that aimed to determine the role of oral vitamin D supplementation on pneumonia in children. The trial enrolled 156 children (78/78, intervention/placebo) aged between two months and five years who were hospitalised with WHO‐defined pneumonia. Very severe pneumonia was present in 10 children (12.8%) in the vitamin D group and 11 children (14.3%) in the control group. Children in the intervention arm received a single dose of oral vitamin D₃ (100,000 IU) on day 1 of admission as cholecalciferol granules mixed with water or milk. Children in the placebo arm received standard therapy. All children received antibiotics according to practice guidelines at the trial centre. The primary trial outcome was duration of hospitalisation (means and SDs obtained from trial authors upon request; Somnath 2022 [pers comm]), and secondary outcomes were time to resolution of fever, complications associated with pneumonia, need for transfer to the paediatric intensive care unit, mortality, and pneumonia recurrence in the following six months.
Excluded studies
We excluded three trials (Jadhav 2021; Singh 2019; Zhou 2016). One trial administered nutritional supplements (vitamin A, vitamin D, zinc, and iron) to children with pneumonia who were nutritionally deficient for these vitamins and minerals (Zhou 2016). Moreover, the trial included children with asthmatic pneumonia. The other two trials mostly focused on prevention of repeat pneumonia episodes, and did not report any outcomes related to the treatment of an acute or current pneumonia episode (Jadhav 2021; Singh 2019).
Studies awaiting classification
See Characteristics of studies awaiting classification. All six trials were generally eligible for inclusion but did not meet the research integrity criteria (Bisht 2017; Dhungel 2015; Gaber 2018; Rahmati 2016; Rajshekhar 2016; Shamaoon 2018). We contacted the trial authors but received only partial responses that could not clarify the issue, or no response at all.
Risk of bias in included studies
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All seven trials used sequentially numbered, sealed envelopes or codes for allocation of participants to the two groups, and were judged at low risk of bias (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021; Manaseki‐Holland 2010; Somnath 2017).
Blinding
Six trials blinded participants and carers and made efforts to prevent unblinding by providing interventions and placebos that were similar in terms of appearance, taste, and colour (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021; Manaseki‐Holland 2010); we judged them at low risk of performance bias. In five of these six trials, investigators broke the code only after administration of the intervention, data collection, follow‐up, and tabulation (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021); we judged them at low risk of detection bias. Manaseki‐Holland 2010 did not describe methods to ensure blinding of outcome assessment, so we judged it at unclear risk of detection bias. Somnath 2017 did not blind participants or personnel and so was at high risk of performance bias; however, risk of detection bias in this trial was low, as outcome assessment was blinded.
Incomplete outcome data
We assessed six trials at low risk of attrition bias (Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021; Manaseki‐Holland 2010; Somnath 2017). In Jingi 2018, 13 children (13.9%) were lost to follow‐up (seven in vitamin D group, six in placebo group). In Chowdhury 2021, 12 children (6.1%) either left against medical advice or were referred to another hospital (five in vitamin D group, seven in placebo group). Manaseki‐Holland 2010 excluded data of 24 children (5.2%) from primary outcome analysis; two of these children (0.4%) had missing or incomplete data. Labib 2021 reported no attrition. Chowdhury 2021 and Gupta 2016 analysed data using the intention‐to‐treat (ITT), and Somnath 2017 analysed using a modified ITT principle (two children in placebo group were found to have tuberculosis and were excluded from analysis). In Choudhary 2012, seven children (3.5%) left against medical advice (number in each group not mentioned), and there was a discrepancy in the number of children with complete outcome data in the table (n = 173) versus the text (n = 193). We therefore judged this trial at unclear risk of attrition bias.
Selective reporting
We assessed four trials as at low risk of reporting bias, as they were registered in clinical trials registries (Chowdhury 2021; Gupta 2016; Labib 2021; Somnath 2017). The remaining trials were not registered and had no available protocols; we judged them at unclear risk of bias.
Other potential sources of bias
There were no other potential sources of bias in the included trials.
Effects of interventions
See: Table 1
Primary outcomes
Time to resolution of acute illness
Five trials reported time to resolution of acute illness (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Manaseki‐Holland 2010). Two trials provided the data as medians and IQRs (Choudhary 2012; Chowdhury 2021). We contacted the corresponding trial authors to request means and SDs, but these data were unavailable (Chowdhury 2022 [pers comm]; Gupta 2016 [pers comm]). We therefore calculated the corresponding mean and SD as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). Vitamin D compared to placebo probably has little or no effect on time to resolution of acute illness (MD −1.28 hours, 95% CI −5.47 to 2.91; I² = 0%; 5 trials, 1188 participants; moderate‐certainty evidence; Analysis 1.1; Table 1).
1.1. Analysis.

Comparison 1: Time to resolution of acute illness, Outcome 1: Time to resolution of acute illness
Subgroup analysis: low‐dose versus high‐dose vitamin D
One trial used low‐dose vitamin D (Choudhary 2012), and four used high‐dose vitamin D (Chowdhury 2021; Gupta 2016; Jingi 2018; Manaseki‐Holland 2010). We do not know if low‐dose vitamin D has an effect on the time to resolution of acute illness (MD 5.19 hours, 95% CI −4.73 to 15.11; 173 participants; Analysis 1.2). High‐dose vitamin D compared to placebo may have little or no effect on the time to resolution of acute illness (MD −2.69 hours, 95% CI −7.31 to 1.94; I² = 0%; 1015 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1: Time to resolution of acute illness, Outcome 2: Time to resolution of acute illness (subgroup analysis: low‐dose versus high‐dose vitamin D)
Subgroup analysis: effect of oral versus parenteral vitamin D
Three trials used oral dose (Choudhary 2012; Chowdhury 2021; Manaseki‐Holland 2010); meta‐analysis of their results indicated that oral vitamin D may have little or no effect on time to resolution of acute illness (MD −0.65 hours, 95% CI −7.42 to 6.12; I² = 20%; 799 participants; Analysis 1.3). Two trials used a parenteral dose of vitamin D (Gupta 2016; Jingi 2018); meta‐analysis of their results indicated that parenteral vitamin D compared to placebo may have little or no effect on time to resolution of acute illness (MD −1.68 hours, 95% CI −7.01 to 3.66; I² = 0%; 389 participants; Analysis 1.3)
1.3. Analysis.

Comparison 1: Time to resolution of acute illness, Outcome 3: Time to resolution of acute illness (subgroup analysis: oral versus parenteral vitamin D)
Duration of hospitalisation
Five trials reported duration of hospitalisation (Choudhary 2012; Chowdhury 2021; Gupta 2016; Labib 2021; Somnath 2017). Four trials provided data as medians and IQRs (Choudhary 2012; Chowdhury 2021; Labib 2021; Somnath 2017). We contacted the corresponding authors to request means and SDs, but these data were unavailable from three trials (Chowdhury 2022 [pers comm]; Gupta 2016 [pers comm]; Labib 2022 [pers comm]). We calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). Somnath 2022 [pers comm] provided means and SDs. We do not know if vitamin D compared to placebo has an effect on duration of hospitalisation (MD 4.96 hours, 95% CI −8.28 to 18.21; I² = 73%; 5 trials, 1023 participants; very low‐certainty evidence; Analysis 2.1; Table 1). Follow‐up varied from two to 14 days.
2.1. Analysis.

Comparison 2: Duration of hospitalisation, Outcome 1: Duration of hospitalisation
Sensitivity analysis: excluding trials with transformed data
We explored the cause of heterogeneity by excluding the three trials that did not provide means and SDs (Choudhary 2012; Chowdhury 2021; Labib 2021). This adjustment reduced statistical heterogeneity but did not change our conclusion (MD −2.99 hours, 95% CI −12.05 to 6.07; I² = 44%; 2 trials, 462 participants; low‐certainty evidence; Analysis 2.2).
2.2. Analysis.

Comparison 2: Duration of hospitalisation, Outcome 2: Duration of hospitalisation (sensitivity analysis: studies with transformed data excluded)
Subgroup analysis: low‐dose versus high‐dose vitamin D
One trial used low‐dose vitamin D (Choudhary 2012); based on the evidence it provided, we do not know if low‐dose vitamin D compared to placebo has an effect on duration of hospitalisation (MD 8.0 hours, 95% CI −0.99 to 16.99; 173 participants; Analysis 2.3). Four trials used high‐dose vitamin D (Chowdhury 2021; Gupta 2016; Labib 2021; Somnath 2017); based on meta‐analysis of their results, we do not know if low‐dose vitamin D compared to placebo has an effect on duration of hospitalisation (MD 5.15 hours, 95% CI −14.29 to 24.59; I² = 76%; 850 participants; Analysis 2.3).
2.3. Analysis.

Comparison 2: Duration of hospitalisation, Outcome 3: Duration of hospitalisation (subgroup analysis: low‐dose versus high‐dose vitamin D)
Subgroup analysis: effect of oral versus parenteral vitamin D
Three trials used oral dose vitamin D (Choudhary 2012; Somnath 2017; Chowdhury 2021); based on meta‐analysis of their results, we do not know if oral vitamin D compared to placebo has an effect on the duration of hospitalisation (MD 0.52 hours, 95% CI −15.51 to 16.54; I² = 64%; 524 participants; Analysis 2.4). Two trials used parenteral dose of vitamin D (Gupta 2016; Labib 2021); based on meta‐analysis of their results, we do not know if parenteral vitamin D compared to placebo has an effect on the duration of hospitalisation (MD 12.34 hours, 95% CI −23.99 to 48.66; I² = 88%; 499 participants; Analysis 2.4).
2.4. Analysis.

Comparison 2: Duration of hospitalisation, Outcome 4: Duration of hospitalisation (subgroup analysis: oral versus parenteral vitamin D)
Secondary outcomes
The follow‐up time for the secondary outcomes varied from two to 14 days.
Time to resolution of tachypnoea
Two trials reported time to resolution of tachypnoea (Choudhary 2012; Chowdhury 2021). Choudhary 2012 presented the data as medians and IQRs; we contacted the corresponding author to request means and SDs, but these data were unavailable (Gupta 2016 [pers comm]). Therefore, we calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). Vitamin D compared to placebo probably has little or no effect on the time to resolution of tachypnoea (MD 4.70 hours, 95% CI −4.48 to 13.88; 2 trials, 368 participants; moderate‐certainty evidence; Analysis 3.1).
3.1. Analysis.

Comparison 3: Time to resolution of tachypnoea, Outcome 1: Time to resolution of tachypnoea
Time to resolution of lower chest wall indrawing
Two trials reported time to resolution of lower chest wall indrawing (Choudhary 2012; Chowdhury 2021). Choudhary 2012 presented the data as medians and IQRs; we contacted the corresponding author to request means and SDs, but these data were unavailable (Gupta 2016 [pers comm]). We therefore calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). Vitamin D compared to placebo probably has little or no effect on time to resolution of lower chest wall indrawing (MD 2.99 hours, 95% CI −4.38 to 10.35; 2 trials, 370 participants; moderate‐certainty evidence; Analysis 4.1).
4.1. Analysis.

Comparison 4: Time to resolution of lower chest indrawing, Outcome 1: Time to resolution of lower chest indrawing
Time to resolution of hypoxia
Two trials reported time to resolution of hypoxia (Choudhary 2012; Chowdhury 2021). Choudhary 2012 presented the data as medians and IQRs; we contacted the corresponding author to request means and SDs, but these data were unavailable (Gupta 2016 [pers comm]). We therefore calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). We do not know if vitamin D compared to placebo has an effect on time to resolution of hypoxia (MD −9.39 hours, 95% CI −29.41 to 10.63; I² = 90%; 2 trials, 370 participants; very low‐certainty evidence; Analysis 5.1).
5.1. Analysis.

Comparison 5: Time to resolution of hypoxia, Outcome 1: Time to resolution of hypoxia
Time to resolution of fever
Three trials reported time to resolution of fever (Choudhary 2012; Gupta 2016; Somnath 2017). Choudhary 2012 presented the data as medians and IQRs; we contacted the corresponding author to request means and SDs, but these data were unavailable (Gupta 2016 [pers comm]). We therefore calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). We do not know if vitamin D compared to placebo has an effect on time to resolution of fever (MD 1.84 hours, 95% CI −2.31 to 6.0; 484 participants; low‐certainty evidence; Analysis 6.1).
6.1. Analysis.

Comparison 6: Time to resolution of fever, Outcome 1: Time to resolution of fever
Time to resolution of inability to feed or lethargy
One trial reported time to resolution of inability to feed or lethargy (Choudhary 2012). Choudhary 2012 presented the data as medians and IQRs; we contacted the corresponding author to request means and SDs, but these data were unavailable (Gupta 2016 [pers comm]). Therefore, we calculated the corresponding means and SDs as per the available statistical methods (Hozo 2005; Luo 2018; Wan 2014). We do not know if vitamin D compared to placebo has an effect on the time to resolution of inability to feed or lethargy (MD 8.0 hours, 95% CI 0.60 to 15.40; 1 trial, 173 participants; very low‐certainty evidence; Analysis 7.1).
7.1. Analysis.

Comparison 7: Time to resolution of inability to feed or lethargy, Outcome 1: Time to resolution of inability to feed or lethargy
Treatment failure rate
Although no trials specifically reported failure rate after 48 hours of treatment, three trials reported treatment response (Choudhary 2012; Chowdhury 2021; Jingi 2018). In Choudhary 2012, 23 (11.5%) children remained in the same condition, and four (2%) children had their condition worsen, but the report provided no description of the groups or the time period. As a result, we were unable to include data from this trial in the meta‐analysis. We do not know if vitamin D compared to placebo has an effect on treatment failure rate (RR 0.77, 95% CI 0.38 to 1.56; 2 trials, 277 participants; low‐certainty evidence; Analysis 8.1).
8.1. Analysis.

Comparison 8: Treatment failure, Outcome 1: Treatment failure
Mortality rate
Three trials reported mortality (Choudhary 2012; Chowdhury 2021; Labib 2021). We do not know if vitamin D compared to placebo has an effect on mortality rate (RR 0.69, 95% CI 0.44 to 1.07; 584 participants; low‐certainty evidence; Analysis 9.1).
9.1. Analysis.

Comparison 9: Mortality rate, Outcome 1: Mortality rate
Manaseki‐Holland 2010 reported three deaths (two in the vitamin D group and one in the placebo group) during the 90‐day follow‐up evaluation of repeated episodes of pneumonia. Because it was not clear if the children died during treatment of the index episode of pneumonia, we contacted the corresponding author for clarification (Manaseki‐Holland 2017 [pers comm]). They confirmed that the children died during the 90‐day follow‐up period (not during the index episode). Accordingly, we did not include mortality data from Manaseki‐Holland 2010 in our analysis.
Adverse events
One trial reported adverse events; these were minor and all occurred in the vitamin D group (Choudhary 2012). We do not know if vitamin D compared to placebo has an effect on the risk of adverse events (RR 4.94, 95% CI 0.24 to 101.48; 173 participants; very low‐certainty evidence; Analysis 10.1).
10.1. Analysis.

Comparison 10: Adverse events, Outcome 1: Adverse events
Discussion
Summary of main results
In this review update, we applied research integrity criteria, and included seven trials involving a total of 1601 children: 631 with pneumonia and 970 with severe or very severe pneumonia (Choudhary 2012; Chowdhury 2021; Gupta 2016; Jingi 2018; Labib 2021; Manaseki‐Holland 2010; Somnath 2017). No trials were conducted in high‐income countries. Participant characteristics, aetiological agents, and prevalence of vitamin D deficiency appeared to be very similar across trials. The trials differed in terms of inclusion criteria and dose and duration of vitamin D use. Three trials received funding: one from the New Zealand Aid Corporation, one from an institutional grant, and one from multigovernment organisations (Bangladesh, Sweden, and UK). The remaining four trials were unfunded.
The appropriate effect measure for time‐to‐event data (time to resolution of acute illness) is hazard ratio, but the trials reported this outcome with continuous data. Only two trials reported vitamin D benefits for children with acute pneumonia (Chowdhury 2021; Labib 2021). In Chowdhury 2021, there was a trend towards reduction in time to recovery from pneumonia and duration of hospitalisation in children with a sufficient serum vitamin D level. Three trials included children with both non‐severe and severe pneumonia, but none reported outcomes separately for children with severe pneumonia (Jingi 2018; Labib 2021; Manaseki‐Holland 2010). Though mortality rate is an important outcome for policy decisions, only three trials reported this outcome (Choudhary 2012; Chowdhury 2021; Labib 2021). The remaining trials did not report any deaths. See Table 1.
We questioned whether vitamin D was ineffective for treating children with acute pneumonia due to real therapeutic ineffectiveness of vitamin D, improper dose or mode of administration, or type or severity of the underlying illness. These are important aspects that should be investigated in future trials.
The included trials differed significantly in vitamin D dose. One trial administered oral vitamin D at a total dose of 5000 IU or 10,000 IU (according to the child's age) over five days (Choudhary 2012). Four trials administered a single bolus dose of 100,000 IU either at the onset of illness or within 24 hours of admission (Gupta 2016; Labib 2021; Manaseki‐Holland 2010; Somnath 2017). Jingi 2018 administered a single bolus dose of 300,000 IU within 24 hours of admission. Chowdhury 2021 administered 20,000 IU to children aged under six months, 50,000 IU to those aged six to 12 months, and 100,000 IU to those aged 13 to 59 months on day 1; followed by 10,000 IU daily for four days or until discharge. As discussed in How the intervention might work, a daily vitamin D supplementation has better therapeutic efficacy than large bolus doses for pneumonia, tuberculosis, and fracture in older adults (Heaney 2012; Hollis 2011; Manaseki‐Holland 2012; Martineau 2012; Nielsen 2010). Clinical studies have shown that at a higher dose, vitamin D could be immunosuppressive, and the immunological effectiveness of vitamin D is blunted at extreme doses (either very high or low therapeutic doses; Kimball 2011; Manaseki‐Holland 2010; Manaseki‐Holland 2012). This conclusion was supported by the findings of various trials that used a daily dose of 1000 IU to 2000 IU per day of vitamin D but did not document any benefit (Bisht 2017; Choudhary 2012; Gaber 2018; Rajshekhar 2016). The doses used in these studies may have been insufficient, considering the high prevalence of vitamin D deficiency along with severe illness (severe pneumonia) in the studied populations. The ideal situation would have been correlation with vitamin D levels measured before and after supplementation.
Two trials reported vitamin D level before and after supplementation, but failed to show any benefit of vitamin D (Gupta 2016; Somnath 2017). However, in Chowdhury 2021, there was a trend towards reduction in time to recovery from pneumonia and duration of hospitalisation in children with a sufficient serum vitamin D level. Another trial found that vitamin D supplementation may reduce mortality risk, time to recovery, and hypoxaemia (Labib 2021). According to National Institutes of Health, the no‐observed‐adverse‐effect level of vitamin D is 2400 IU, and the lowest‐observed‐adverse‐effect level is 3800 IU (NIH Vitamin D Fact Sheet). Future trials may consider use of higher doses with monitoring of toxicity and serum vitamin D level. It is premature to hypothesise about the real therapeutic ineffectiveness of vitamin D because clinical trials are ongoing and results are not yet available.
Although the included trials were conducted in LMICs (Afghanistan, Egypt, and India), only three trials reported prevalence of malnutrition (Chowdhury 2021; Gupta 2016; Jingi 2018). Gupta 2016 reported moderate (grade II) malnutrition but did not specify the prevalence of malnutrition in either the vitamin D or the control group; therefore, it was difficult to examine the effect of vitamin D in malnourished children. Jingi 2018 reported the prevalence of moderate malnutrition in both trial arms, but found no benefit of vitamin D supplementation. Chowdhury 2021 reported severe malnutrition in more than half of the children in both the groups, and found a trend towards reduction of time to recovery from pneumonia and duration of hospitalisation in children with a sufficient serum vitamin D level. Underlying malnutrition may affect the state of immunity and hence blunt the vitamin D effect. Malnutrition also lowers serum vitamin D levels. Furthermore, severe pneumonia may establish a systemic inflammatory response in the host that causes a decrease in the serum vitamin D level (Bang 2011). It would therefore be prudent to trial the level of inflammatory markers along with vitamin D levels in children with non‐severe/severe pneumonia.
No trials reported the aetiology of pneumonia. This is important for any differential therapeutic effect of vitamin D (if any) in bacterial or viral pneumonia. Because there is a seasonal variation in the predominance of aetiological agents (e.g. viruses dominating over bacteria in the rainy season), any trial conducted over a year would be meaningful. This is also important because vitamin D levels may decrease during winter and the rainy season due to less sun exposure. Chowdhury 2021 was conducted over 48 months, Gupta 2016 over 29 months, Jingi 2018 and Somnath 2017 over 12 months, Labib 2021 and Manaseki‐Holland 2010 over three to six months, and Choudhary 2012 did not mention the trial duration.
Viral pneumonia is commonly associated with wheezing. One trial excluded children with wheezing (Manaseki‐Holland 2010). Almost one‐third of children in Choudhary 2012 and more than 80% of children in Gupta 2016 had wheezing. The remaining trials did not report this variable. Recurrent pneumonia affected almost one‐third of children in Choudhary 2012 and Chowdhury 2021, and 17.5% of children in Jingi 2018. These children likely had an underlying immune dysfunction or other problem predisposing them to recurrence. Vitamin D alone may not correct this, resulting in no observable clinical effect or benefit. The timing of vitamin D administration in the course of pneumonia (early versus late) may also have affected outcome measures. Any information regarding the duration of illness prior to initiating vitamin D would be meaningful, but no trial reported this. Likewise, no trials provided information regarding prior antibiotic use. A large proportion of children needing second‐line or broader‐spectrum antibiotics due to severe illness would lead to a reduction in trial power, making it difficult to detect any difference attributable to vitamin D.
Overall completeness and applicability of evidence
We included seven trials, only one of which showed any beneficial effect of vitamin D for children with acute pneumonia. Our results may not be applicable to children with acute pneumonia in high‐income countries, children with HIV or severe malnutrition, and neonates (aged up to one month). At the time of writing this review, we could find no additional or ongoing trials that could provide additional evidence.
Certainty of the evidence
The GRADE assessment showed that the evidence for duration of hospitalisation, time to resolution of hypoxia, inability to feed or lethargy, and adverse events was very low‐certainty. The evidence for mortality rate, treatment failure rate, and time to resolution of fever was low‐certainty. The evidence for time to resolution of acute illness, lower chest indrawing, and tachypnoea was moderate‐certainty (see Table 1). Reasons for downgrading included serious trial limitations (one trial was open‐label), serious inconsistency (statistical heterogeneity), serious indirectness (due to lack of generalisability of trial findings and differing characteristics of the trial population), and serious imprecision (wide 95% CI around the pooled effect, inclusion of no effect, and upper or lower confidence limit crossing the minimal important difference for benefit or harm).
Potential biases in the review process
All included trials measured the effect of vitamin D in childhood pneumonia. It is possible that we missed trials that measured acute respiratory tract infection or lower respiratory tract infection rather than pneumonia specifically, as a secondary outcome. We aimed to avoid this scenario by conducting a wide search and carefully assessing the relevance of each paper identified. We were unable to assess aetiological agents (bacterial or viral) to inform reporting of any beneficial effects of vitamin D, as no included trials reported these data. Furthermore, because no trials measured serum vitamin D levels, we cannot estimate the dose‐response effect in children with acute pneumonia.
Agreements and disagreements with other studies or reviews
We published an earlier systematic review on this topic (Das 2013), which included two trials (Choudhary 2012; Manaseki‐Holland 2010). In the first version of this review (Das 2018), we included seven trials (Choudhary 2012; Dhungel 2015; Gupta 2016; Manaseki‐Holland 2010; Rahmati 2016; Rajshekhar 2016; Somnath 2017). In this update, we moved three previously included trials to Characteristics of studies awaiting classification (Dhungel 2015; Rahmati 2016; Rajshekhar 2016). Our conclusions are unchanged from the previous version of this review.
Authors' conclusions
Implications for practice.
We do not know if vitamin D supplementation as an adjunct to antibiotic treatment has an important effect on any of the measured outcomes in children aged under five years with acute pneumonia. The trials reported no major adverse events. We rated the certainty of the evidence as very low to moderate. Reasons for downgrading included imprecision, risk of bias, inconsistency, and indirectness.
Implications for research.
Future trials may consider use of a higher dosage schedule of vitamin D along with monitoring of toxicity and serum vitamin D level. Investigators should measure baseline and post‐treatment vitamin D levels to correlate the outcome measures with subclinical or clinical vitamin D deficiency. Reported variables should include prevalence of malnutrition, as this may affect the therapeutic effect of vitamin D independently of the illness.
Future trials should also report the level of inflammatory markers along with vitamin D levels in children affected with acute non‐severe or severe pneumonia. It is important to study the aetiology of pneumonia (bacterial, viral, or atypical), and trials should ideally be conducted over one year to include all seasons, because seasonal change can affect vitamin D levels and aetiology of pneumonia.
Future trials should report the duration of illness prior to initiation of therapy with vitamin D, as well as prior antibiotic use, as this can modify recovery. Trial authors should include this information in the baseline data to enable comparison amongst trials.
Future trials should also include a subgroup of children with severe malnutrition, rickets, or both, and a subgroup of children with wheezing.
What's new
| Date | Event | Description |
|---|---|---|
| 28 December 2021 | New citation required but conclusions have not changed | Vitamin D as an adjunct to antibiotics did not benefit children with acute pneumonia. The overall conclusions of vitamin D supplementation in acute pneumonia remain unchanged. |
| 28 December 2021 | New search has been performed | We updated the searches and included three new trials (Chowdhury 2021; Jingi 2018; Labib 2021) with a total of 468 participants, and excluded two new trials (Jadhav 2021; Singh 2019). We moved three previously included trials to Studies awaiting classification (Dhungel 2015; Rahmati 2016; Rajshekhar 2016), and identified three new trials awaiting classification (Bisht 2017; Gaber 2018; Shamaoon 2018). We performed subgroup analysis and sensitivity analysis in this updated review. |
History
Protocol first published: Issue 3, 2015 Review first published: Issue 7, 2018
Acknowledgements
We acknowledge the help and infrastructure provided by the All India Institute of Medical Sciences (AIIMS), Bhubaneswar; and Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh. We thank the following people for commenting on the draft protocol: Ann Fonfa, Denny John, Rakesh Lodha, Pankaj Shah, Viviana Rodriguez, and Michelle Guppy. We also wish to thank the following people for commenting on the draft review: Ruth Day, Janet Wale, Rakesh Lodha, Pankaj Shah, Mark Jones, and Michelle Guppy. Finally, we would like to thank Mohamed Hassan and Sushil Agwan, medical students at Bond University, Australia, for checking the review for quality issues and consistency in reporting for the draft review. We thank Pranita Pradhan, Information specialist, ICMR Advanced Centre for Evidence Based Child Health, PGIMER, Chandigarh, for helping with the literature search for this updated review.
The following people conducted the editorial process for this 2022 update:
Sign‐off Editors (final editorial decision): Mark Jones, Bond University, Australia; Mieke van Driel, University of Queensland, Australia
Managing Editors (provided editorial guidance to authors, edited the draft, invited peer reviewers): Liz Dooley, Bond University, Australia; Fiona Russell, Bond University, Australia
Contact Editor (provided comments and recommended an editorial decision): Michelle Guppy, University of New England, Australia
Copy Editor (copy‐editing and production): Julia Turner
Peer‐reviewers (provided comments and recommended an editorial decision):
Methods review: Rachel Richardson (Associate Editor, Cochrane)
Statistical review: reviewer wished to remain anonymous
Research Integrity Editor: Lisa Bero (Senior Research Integrity Editor, Cochrane)
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
1 exp Pneumonia/ (239521) 2 (pneumon* or bronchpneumon* or pleuropneumon*).tw. (215609) 3 Respiratory Tract Infections/ (41149) 4 (lower respiratory tract infection* or lower respiratory infection* lrti).tw. (7202) 5 or/1‐4 (421099) 6 exp Vitamin D/ (64645) 7 ("vitamin d" or "vit d").tw,nm. (78012) 8 ("vitamin d2" or "vitamin d3").tw,nm. (13632) 9 (ergocalciferol* or cholecalciferol* or calcitriol*).tw,nm. (32666) 10 or/6‐9 (96378) 11 5 and 10 (1262) 12 "2018".yr. (1169392) 13 "2021".yr. (1661342) 14 or/12‐13 (2830734) 15 11 and 14 (554)
Appendix 2. Embase (Elsevier) search strategy
| #13 | #11 AND #12 | 771 |
| #12 | 1054,414 | |
| #12.8 #12.3 NOT #12.7 954412 #12.7 #12.4 NOT #12.6 #12.6#12.4 AND #12.5 #12.5'human'/de AND [embase]/lim #12.4'animal'/de OR 'nonhuman'/de OR 'animal experiment'/de AND [embase]/lim #12.3#12.1 OR #12.2 #12.2random*:ab,ti OR placebo*:ab,ti OR crossover*:ab,ti OR 'cross over':ab,ti OR allocat*:ab,ti OR trial:ti OR (doubl* NEXT/1 blind*):ab,ti AND [embase]/lim #12.1'randomized controlled trial'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp AND [embase]/lim |
||
| #11 | #5 AND #10 | 2,058 |
| #10 | #6 OR #7 OR #8 OR #9 | 16,1899 |
| #9 | ergocalciferol*:ab,ti OR cholecalciferol*:ab,ti OR calcitriol*:ab,ti AND [embase]/lim | 11,129 |
| #8 | 'vitamin d2':ab,ti OR 'vitamin d3':ab,ti AND [embase]/lim | 7,701 |
| #7 | 'vitamin d':ab,ti OR 'vit d':ab,ti AND [embase]/lim | 97,082 |
| #6 | 'vitamin d'/exp AND [embase]/lim | 147,383 |
| #5 | #1 OR #2 OR #3 OR #4 | 430,784 |
| #4 | 'lower respiratory tract infection':ab,ti OR 'lower respiratory tract infections':ab,ti OR 'lower respiratory infection':ab,ti OR 'lower respiratory infections':ab,ti OR lrti:ab,ti AND [embase]/lim | 11,409 |
| #3 | 'lower respiratory tract infection'/de AND [embase]/lim | 13,609 |
| #2 | pneumon*:ab,ti OR pleuropneumon*:ab,ti OR bronchopneumon*:ab,ti AND [embase]/lim | 264,395 |
| #1 | 'pneumonia'/exp AND [embase]/lim | 319,502 |
Data and analyses
Comparison 1. Time to resolution of acute illness.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Time to resolution of acute illness | 5 | 1188 | Mean Difference (IV, Fixed, 95% CI) | ‐1.28 [‐5.47, 2.91] |
| 1.2 Time to resolution of acute illness (subgroup analysis: low‐dose versus high‐dose vitamin D) | 5 | 1188 | Mean Difference (IV, Fixed, 95% CI) | ‐1.28 [‐5.47, 2.91] |
| 1.2.1 Low‐dose vitamin D | 1 | 173 | Mean Difference (IV, Fixed, 95% CI) | 5.19 [‐4.73, 15.11] |
| 1.2.2 High‐dose vitamin D | 4 | 1015 | Mean Difference (IV, Fixed, 95% CI) | ‐2.69 [‐7.31, 1.94] |
| 1.3 Time to resolution of acute illness (subgroup analysis: oral versus parenteral vitamin D) | 5 | 1188 | Mean Difference (IV, Fixed, 95% CI) | ‐1.28 [‐5.47, 2.91] |
| 1.3.1 Oral vitamin D | 3 | 799 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐7.42, 6.12] |
| 1.3.2 Parenteral vitamin D | 2 | 389 | Mean Difference (IV, Fixed, 95% CI) | ‐1.68 [‐7.01, 3.66] |
Comparison 2. Duration of hospitalisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Duration of hospitalisation | 5 | 1023 | Mean Difference (IV, Random, 95% CI) | 4.96 [‐8.28, 18.21] |
| 2.2 Duration of hospitalisation (sensitivity analysis: studies with transformed data excluded) | 2 | 462 | Mean Difference (IV, Fixed, 95% CI) | ‐2.99 [‐12.05, 6.07] |
| 2.3 Duration of hospitalisation (subgroup analysis: low‐dose versus high‐dose vitamin D) | 5 | 1023 | Mean Difference (IV, Random, 95% CI) | 4.96 [‐8.28, 18.21] |
| 2.3.1 Low‐dose vitamin D | 1 | 173 | Mean Difference (IV, Random, 95% CI) | 8.00 [‐0.99, 16.99] |
| 2.3.2 High‐dose vitamin D | 4 | 850 | Mean Difference (IV, Random, 95% CI) | 5.15 [‐14.29, 24.59] |
| 2.4 Duration of hospitalisation (subgroup analysis: oral versus parenteral vitamin D) | 5 | 1023 | Mean Difference (IV, Random, 95% CI) | 3.92 [‐8.57, 16.42] |
| 2.4.1 Oral vitamin D | 3 | 524 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐15.51, 16.54] |
| 2.4.2 Parenteral vitamin D | 2 | 499 | Mean Difference (IV, Random, 95% CI) | 12.34 [‐23.99, 48.66] |
Comparison 3. Time to resolution of tachypnoea.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Time to resolution of tachypnoea | 2 | 368 | Mean Difference (IV, Fixed, 95% CI) | 4.70 [‐4.48, 13.88] |
Comparison 4. Time to resolution of lower chest indrawing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Time to resolution of lower chest indrawing | 2 | 370 | Mean Difference (IV, Fixed, 95% CI) | 2.99 [‐4.38, 10.35] |
Comparison 5. Time to resolution of hypoxia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Time to resolution of hypoxia | 2 | 370 | Mean Difference (IV, Random, 95% CI) | ‐9.39 [‐29.41, 10.63] |
Comparison 6. Time to resolution of fever.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Time to resolution of fever | 3 | 484 | Mean Difference (IV, Fixed, 95% CI) | 1.84 [‐2.31, 6.00] |
Comparison 7. Time to resolution of inability to feed or lethargy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Time to resolution of inability to feed or lethargy | 1 | 173 | Mean Difference (IV, Random, 95% CI) | 8.00 [0.60, 15.40] |
Comparison 8. Treatment failure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Treatment failure | 2 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.38, 1.56] |
Comparison 9. Mortality rate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Mortality rate | 3 | 584 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.44, 1.07] |
Comparison 10. Adverse events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Adverse events | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 4.94 [0.24, 101.48] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Choudhary 2012.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: not reported |
|
| Participants | Setting: hospital inpatient department Country: India Number: 200 (treatment: 100; control: 100) Age: treatment: mean 14.1 (SD 12.2) months; control: mean 13.8 (SD 11.4) months Sex: not reported Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: antibiotics were administered as per the IAP 2006 guidelines (age < 3 months: cefotaxime/ceftriaxone ± gentamicin/amikacin as first line, co‐amoxyclav + gentamicin/amikacin as second line; age 3 months–5 years: ampicillin/chloramphenicol or ampicillin + chloramphenicol or co‐amoxyclav as first line, and co‐amoxyclav or cefotaxime/ceftriaxone as second line. In cases of staphylococcal infection, cloxacillin as first line and vancomycin/teicoplanin as second line was added to age‐specific combination). |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: no funding agency Trial registration: no Ethical approval: obtained Other: investigators did not perform microbiological or radiological diagnosis of pneumonia or measure serum vitamin D₃ levels. Contact with trial authors: email, 24 April 2016. Trial reported medians and IQRs; we requested means and SDs, but this information was unavailable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker, and unlikely that blinding was broken, as the intervention and placebo had in similar appearance, taste, and colour. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Code broken only after intervention, data collection, follow‐up, and tabulation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7 children (3.5%) left against medical advice and could not complete the study (number in each group not mentioned). No mention of ITT. Discrepancy between number of children included in analysis in table (n = 173) and text (n = 193). We wrote to trial authors for clarification, but the data were unavailable. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered, but all outcomes proposed in the methods section were reported. |
| Other bias | Low risk | No other known risks of bias. |
Chowdhury 2021.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 48 months |
|
| Participants | Setting: hospital inpatient department Country: Bangladesh Number: 197 (treatment: 97; control: 100) Age: treatment: median 8 (range 5 to 13) months; control: median 10 (range 5.5 to 14) months Sex: 124 (63%) boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: first‐line parental antibiotics included ampicillin and gentamicin. Children who did not respond (no improvement after 48 hours or deterioration of clinical signs/symptoms of pneumonia after 24 hours of initiation of antibiotics) were switched to second‐line antibiotics ceftriaxone and levofloxacin |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: Government agencies of Bangladesh, Canada, Sweden, and UK Trial registration: registered at ClinicalTrials.gov Ethical approval: obtained Other: the trial reported 4 deaths (3 in vitamin D group and 1 in placebo group) during 6 months' follow‐up of repeat episodes of pneumonia Contact with trial authors: email, 27 February 2022. The trial reported medians and IQRs; we requested means and SDs, but these data were unavailable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker; unlikely that blinding was broken, as intervention and placebo were similar in appearance, taste, and colour. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Code broken only after intervention, data collection, follow‐up, and tabulation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 children (6.1%) lost to follow‐up or referred to another hospital (vitamin D: 5; placebo: 7). ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Trial registered and all relevant outcomes reported. |
| Other bias | Low risk | No other known risks of bias. |
Gupta 2016.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 29 months |
|
| Participants | Setting: hospital inpatient department Country: India Number: 324 (treatment: 162; control: 162) Age: treatment: mean 16.4 (SD 12.9) months; control: mean 16.8 (SD 11.4) months Sex: treatment: 69.7% boys; control: 69.7% boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: antibiotics administered as per IAP 2006 guidelines (age < 3 months: cefotaxime/ceftriaxone ± gentamicin/amikacin as first line, and co‐amoxyclav + gentamicin/amikacin as second line; age 3 months–5 years: ampicillin/chloramphenicol or ampicillin + chloramphenicol or co‐amoxyclav as first line, and co‐amoxyclav or cefotaxime/ceftriaxone as second line. In cases of staphylococcal infection, cloxacillin as first line and vancomycin/teicoplanin as second line was added to age‐specific combination). |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: no funding agency Trial registration: registered retrospectively at CTRI (Clinical Trials Registry – India) Ethical approval: obtained Other: 8.6% of children had positive blood culture (Staphylococcus aureus isolated in 8.3%), and 90.1% of children had abnormal chest X‐ray findings (consolidation, bilateral patchy opacities, hyperinflation, minor infiltrates). Contact with trial authors: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker, and unlikely that blinding was broken, as the intervention and placebo were similar in appearance, taste, and colour. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Code broken only after intervention, data collection, follow‐up, and tabulation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Estimated sample size for outcome of acute pneumonia was 230 (115 in each group), and for recurrent pneumonia, 324 (162 in each group). However, trial authors used data from 314 children (vitamin D: 156; placebo: 158) for both types of pneumonia episodes. |
| Selective reporting (reporting bias) | Low risk | The trial was registered. |
| Other bias | Low risk | No other known risks of bias. |
Jingi 2018.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 12 months |
|
| Participants | Setting: hospital inpatient department Country: India Number: 80 (treatment: 40; control: 40) Age: not reported Sex: 48 (60%) boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: children received antibiotics that included penicillin G (first line) and cefotaxime (second line) along with oxygen and supportive care. |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: no funding agency Trial registration: no Ethical approval: obtained Other: no microbiological diagnosis of pneumonia performed (only blood culture). Only 4% children had normal chest X‐ray. Serum vitamin D level not measured. No report of adverse events or mortality. Contact with trial authors: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker, and unlikely that blinding was broken, as intervention and placebo looked alike. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Code broken only after intervention, data collection, follow‐up, and tabulation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13 children (13.9%) lost to follow‐up (vitamin D: 7; placebo: 6). ITT analysis not performed. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered, but all outcomes proposed in the methods section were reported. |
| Other bias | Low risk | No other known risk of bias. |
Labib 2021.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 5 months |
|
| Participants | Setting: hospital inpatient department Country: Egypt Number: 191 (treatment: 93; control: 98) Age: treatment: median 24 (range 18 to 48) months; control: median 24 (range 10 to 48) months Sex: 136 (71.2%) boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: children received antibiotics according to the national pneumonia treatment protocol based on WHO 2012 guidelines |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: no funding Trial registration: registered retrospectively at ClinicalTrials.gov Ethical approval: obtained Other: microbiological and radiological diagnosis of pneumonia not performed Contact with trial authors: email, 27 February 2022. The trial reported medians and IQRs; we requested means and SDs, but these data were unavailable. We also requested clarification regarding the age of participants, as the median (IQR) age was below 5 years (although the upper age limit was 12 years); these data were also unavailable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence elicited using an Excel spreadsheet. |
| Allocation concealment (selection bias) | Low risk | Closed dark envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker, and unlikely that blinding was broken, as intervention and placebo looked alike. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Code broken only after intervention, data collection, and follow‐up. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Low risk | Trial was registered and relevant outcomes reported. |
| Other bias | Low risk | No other known risk of bias. |
Manaseki‐Holland 2010.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 2 months |
|
| Participants | Setting: hospital outpatient and inpatient department Country: Afghanistan Number: 453 (treatment: 224; control: 229) Age: treatment: mean 13.18 (SD 9.1) months; control: 13.19 (SD 9.2) months Sex: treatment: 57.8% boys; control: 55.6% boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: children received antibiotics according to the national pneumonia treatment protocol based upon Integrated Management of Childhood Illnesses (IMCI) guidelines (age < 2 months: intramuscular gentamicin and intramuscular benzylpenicillin; age 2 months to 5 years: oral amoxicillin or intramuscular chloramphenicol (if oral administration not possible)) |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: New Zealand Aid Corporation. The pharmacy department of Aga Khan University Hospital (Karachi, Pakistan) provided the study medications. Trial registration: not registered Ethical approval: obtained Other: investigators did not perform microbiological or radiological diagnosis of pneumonia or measure serum vitamin D₃ levels. The trial reported 3 deaths (2 in vitamin D group and 1 in placebo group) during the 90‐day follow‐up evaluation of repeat episodes of pneumonia. Contact with trial authors: email, 4 May 2017. Because it was not clear whether the children had died during treatment of the index episode of pneumonia, we contacted the corresponding author; she believed the children had died during the 90‐day follow‐up (not during the index episode). Therefore, we did not use mortality data in the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence generated in an Excel spreadsheet with no restrictions. |
| Allocation concealment (selection bias) | Low risk | Sealed codes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial ensured blinding of participants and caretaker, and unlikely that blinding was broken, as the intervention and placebo were similar in appearance, taste, and colour. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data of 24 (5.2%) children (vitamin D: 13; placebo: 11) were excluded from primary outcome analysis. Of these 24 children, outcome data of 2 children (1 in each group) were unavailable/missing. The remaining 22 children (vitamin D: 12, placebo: 10) were either recovered or lost within 24 hours. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered, but all outcomes proposed in the methods section were reported. |
| Other bias | Low risk | No known other risks. |
Somnath 2017.
| Study characteristics | ||
| Methods | Study design: RCT Study duration: 12 months |
|
| Participants | Setting: hospital inpatient department Country: India Number: 156 (treatment: 78; control: 78) Age: mean 13 months (treatment: 53.8% of children ≤ 12 months, 46.2% > 12 months; control: 47.4% ≤ 12 months, 52.6% > 12 months) Sex: treatment: 69.2% boys; control: 65.8% boys Inclusion criteria
Exclusion criteria
Additional information
|
|
| Interventions | Treatment group
Control group
Co‐interventions: children received standard pneumonia treatment as per the guideline. Details of antibiotics not mentioned. |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding source: institute (JIPMER) Intramural Grant Trial registration: registered at CTRI (Clinical Trial Registry – India). Ethical approval: obtained Other: Investigators did not perform microbiological diagnosis of pneumonia. Only 7% of study population had normal serum, and 71% had deficient level. No adverse events or mortality reported. Contact with trial authors: yes, 4 Aug 2022 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded to the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data analysed using modified ITT principle (2 children in placebo group were found to have tuberculosis after randomisation and were excluded from analysis). As such, the trial authors calculated a total sample size of 140 (70 in each group), but included and analysed 154 children (vitamin D: 78, placebo: 76). |
| Selective reporting (reporting bias) | Low risk | The trial was registered. |
| Other bias | Low risk | No other known risk of bias. |
ALRI: acute lower respiratory tract infection; Hb: haemoglobin; IAP: Indian Academy of Pediatrics; Ig: immunoglobulin; IM: intramuscular; IQR: interquartile range; ITT: intention‐to‐treat; IU: international unit; LAMA: left against medical advice; OH‐D: mono‐hydroxy‐vitamin D; PaO2/FiO2: partial pressure of oxygen divided by fractional inhaled oxygen; PICU: paediatric intensive care unit; pSOFA: paediatric sequential organ failure assessment score; PTH: parathyroid hormone; RCT: randomised controlled trial; SD: standard deviation; SES: socio‐economic status; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Jadhav 2021 | Studied acute respiratory tract infection, not pneumonia or lower respiratory tract infection separately. |
| Singh 2019 | Longitudinal, community‐based study. Vitamin D provided as quarterly boluses until 1 year along with standard treatment of pneumonia. However, the trial authors did not report outcomes for acute pneumonia episodes. |
| Zhou 2016 | Multiple nutrients (iron, zinc, vitamin A, vitamin D) were supplemented in children with nutrient deficiency/malnutrition and pneumonia. The trial included children with asthmatic pneumonia. |
Characteristics of studies awaiting classification [ordered by study ID]
Bisht 2017.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 27 months |
| Participants | Setting: hospital inpatient department Country: India Number: 200 (treatment: 100; control: 100) Age: treatment: mean 16.72 (SD 11.6) months; control: mean 13.98 (SD 11.79) months Sex: 128 (64%) boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: antibiotics administered as per IAP guidelines (age < 3 months: cefotaxime/ceftriaxone ± gentamicin/amikacin as first line, and co‐amoxyclav + gentamicin/amikacin as second line; age 3 months–5 years: ampicillin/chloramphenicol or ampicillin + chloramphenicol or co‐amoxyclav as first line, and co‐amoxyclav or cefotaxime/ceftriaxone as second line. In cases of staphylococcal infection, cloxacillin as first line and vancomycin/teicoplanin as second line was added to the age‐specific combination). |
| Outcomes | Primary
Secondary
|
| Notes | Reason for awaiting classification: registry number not reported; ethics committee approval not reported; baseline details not reported in sufficient detail to assess whether randomisation worked properly; incomplete or missing study flow diagram. Funding source: no funding agency Other: investigators did not perform microbiological or radiological diagnosis of pneumonia or measure serum vitamin D levels. |
Dhungel 2015.
| Methods | Study design: RCT Study duration: 6 months |
| Participants | Setting: hospital inpatient department Country: Pakistan Number: 200 (treatment: 100; control: 100) Age: treatment: mean 8.1 (SD 11.0) months; control: mean 6.9 (SD 10.1) months Sex: 122/200 (61%) boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: children received antibiotics that included cefotaxime, ceftriaxone, ampiclox, clarithromycin, amikacin, vancomycin. Children received either 1 antibiotic or a combination. |
| Outcomes | Primary
Secondary
|
| Notes | Reason for awaiting classification: registry number not reported; ethics committee approval not reported; insufficient reporting of study design (e.g. randomisation) and unclear that study was properly randomised; number of participants in each group inconsistent with the reported randomisation method (e.g. block randomisation); baseline details not reported in sufficient detail to assess whether randomisation worked properly; incomplete or missing study flow diagram; implausible number of children with the condition recruited within the timeframe; implausible study results (e.g. massive risk reduction). Funding source: no funding agency Other: the investigators did not perform microbiological diagnosis of pneumonia. Only 4% of children had normal chest X‐ray. Serum vitamin D₃ level was measured, and those with normal level (> 20 ng/mL) were excluded. No report of adverse events or mortality. Contact with trial authors: no |
Gaber 2018.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: 4 months |
| Participants | Setting: hospital inpatient department Country: Egypt Number: 80 (treatment: 40; control: 40) Age: treatment: mean 8.8 (SD 2.6) months; control: mean 9.1 (SD 4.0) months Sex: 45 (56.3%) boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: treatment included intravenous antibiotics, oxygenation, and antipyretics. Inhalation of bronchodilator was administered according to the treating physician |
| Outcomes | Primary
Secondary
|
| Notes | Reason for awaiting classification: registry number not reported; ethics committee approval and informed consent not reported; insufficient reporting of the study design (e.g. randomisation) and unclear that the study was properly randomised; incomplete or missing study flow diagram; unrealistic response rate or loss to follow‐up. Other: the trial was not registered in any database, and the study protocol was not available. Investigators did not perform microbiological diagnosis of pneumonia or measure serum vitamin D levels. |
Rahmati 2016.
| Methods | Study design: RCT Study duration: 12 months |
| Participants | Setting: hospital inpatient department Country: Iran Number: 100 (treatment: 50; control: 50) Age: treatment: mean 17.6 months; control: mean 16.8 months Sex: treatment: 54% boys; control: 61.2% boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: children received a single antibiotic as ceftriaxone. |
| Outcomes | Primary
|
| Notes | Reason for awaiting classification: insufficient reporting of the study design (e.g. randomisation) and unclear that the study was properly randomised; baseline details not reported in sufficient detail to assess whether randomisation worked properly; incomplete or missing study flow diagram; unrealistic response rate or loss of follow‐up. Funding source: no funding agency Trial registration: registered at ClinicalTrials.gov. Ethical approval: obtained Other: investigators did not perform microbiological diagnosis of pneumonia or measure serum vitamin D₃ levels. No report of adverse events or mortality. Contact with trial authors: emails, 8 November 2017 and 15 November 2017. We asked the trial authors to clarify the outcomes duration of antibiotic therapy and duration of hospitalisation, and the unit (day or hour) for duration of hospital admission. We received no response before 10 January 2018 (Das 2017 [pers comm]) |
Rajshekhar 2016.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Study duration: not reported |
| Participants | Setting: hospital inpatient department Country: India Number: 96 (treatment: 48; control: 48) Age: treatment: mean 1.94 (SD 1.46) years; control: mean 2.08 (SD 1.92) years Sex: 58/96 (60.4%) boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: antibiotics were administered as per the IAP 2012 guidelines and included amoxycillin, amoxyclav, third‐generation parenteral cephalosporins, and macrolides. |
| Outcomes |
Primary
|
| Notes | Reason for awaiting classification: registry number not reported; ethics committee approval not reported; baseline details not reported in sufficient detail to assess whether randomisation worked properly; incomplete or missing study flow diagram. Funding source: no funding agency Other: investigators did not perform microbiological or radiological diagnosis of pneumonia or measure serum vitamin D₃ levels. Meyer Organics Private Ltd. was involved in the randomisation process. Contact with trial authors: email, 3 June 2017. We requested information on study methodology, which the trial authors provided (Rajshekhar 2017 [pers comm]) |
Shamaoon 2018.
| Methods | Study design: RCT Study duration: 6 months |
| Participants | Setting: hospital inpatient department Country: Pakistan Number: 200 (treatment: 100; control: 100) Age: mean 7.5 months Sex: 122 (61%) boys Inclusion criteria
Exclusion criteria
Additional information
|
| Interventions | Treatment group
Control group
Co‐interventions: children received antibiotics according to the national pneumonia treatment guidelines |
| Outcomes | Primary
Secondary
|
| Notes | Reason for awaiting classification: registry number not reported; ethics committee approval not reported; insufficient reporting of the study design (e.g. randomisation) and unclear that the study was properly randomised; baseline details not reported in sufficient detail to assess whether randomisation worked properly; incomplete or missing study flow diagram. Other: the trial was not registered in any database, and the study protocol was not available. The investigators did not perform microbiological diagnosis of pneumonia. Contact with trial authors: no. There was another publication (duplicate) with some change in authors in 2019. |
CAP: community‐acquired pneumonia; CHD: congenital heart disease; IAP: Indian Academy of Pediatrics; IM: intramuscular; IU: international unit; RCT: randomised controlled trial; SD: standard deviation; WHO: World Health Organization.
Characteristics of ongoing studies [ordered by study ID]
NCT02054182.
| Study name | Effect of vitamin D supplementation in young South African children hospitalised with acute lower respiratory infection |
| Methods | RCT |
| Participants | Children aged 1 month–5 years, admitted to hospital with acute lower respiratory tract infection (i.e. bronchiolitis or pneumonia or both) |
| Interventions | Vitamin D: 2500 IU daily from enrolment until hospital discharge |
| Outcomes | Primary: change from baseline in modified Respiratory Distress Assessment Instrument score at hospital discharge Secondary: duration of hospitalisation |
| Starting date | February 2014 |
| Contact information | Winter‐Rose S Nkosi, Univeristy of Limpopo, Medunsa Campus, czawr@webmail.co.za |
| Notes | ClinicalTrials.gov identifier: NCT02054182 |
IU: international units; RCT: randomised controlled trial.
Differences between protocol and review
In the protocol, we indicated that if we found cluster‐randomised trials for inclusion, we would adjust for clustering using the intracluster correlation coefficient (Das 2015). However, we did not identify any cluster‐randomised trials for inclusion.
We previously described an I² threshold of greater than 50% to indicate substantial heterogeneity. For this update, we followed the thresholds provided in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011).
We also indicated in the protocol that we would perform additional analyses (subgroup analysis and sensitivity analysis). We could not perform these analyses in the first version of the review, but did perform them in this update.
In the protocol, we did not describe the research integrity step of study selection. In this review update, eligible studies had to meet specific research integrity screening criteria. We moved three previously included trials to Characteristics of studies awaiting classification (Dhungel 2015; Rahmati 2016; Rajshekhar 2016), and added three new trials to Characteristics of studies awaiting classification (Bisht 2017; Gaber 2018; Shamaoon 2018).
Contributions of authors
Conceiving the review: RRD Co‐ordinating the review: RRD, SSN Undertaking manual searches: RRD, SSN Screening search results: RRD, SSN Organising retrieval of papers: RRD, SSN Screening retrieved papers against inclusion criteria: RRD, MS Appraising quality of papers: RRD, MS Abstracting data from papers: RRD, SSN Writing to authors of papers for additional information: RRD, MS Providing additional data about papers: RRD Obtaining and screening data on unpublished studies: RRD, MS Managing data for the review: RRD, SSN Entering data into Review Manager 5: RRD, SSN Calculating Review Manager 5 statistical data: RRD, MS Performing other statistical analysis not using Review Manager 5: RRD, MS Interpreting data: RRD, MS Making statistical inferences: RRD, MS Writing the review: RRD, SSN, MS Performing previous work that served as the foundation of the present study: RRD, MS Serving as guarantor for the review: RRD Taking responsibility for reading and checking the review before submission: RRD, MS, SSN
Sources of support
Internal sources
-
Acknowledgement, India
We acknowledge all the help and infrastructure provided by the All India Institute of Medical Sciences (AIIMS), Bhubaneswar and Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh.
External sources
-
No Source of support, Other
Not externally supported by any funding agency
Declarations of interest
RRD: has declared that they have no conflict of interest. MS: has declared that they have no conflict of interest. SSN: has declared that they have no conflict of interest.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Choudhary 2012 {published data only}
- Choudhary N, Gupta P. Vitamin D supplementation for severe pneumonia – a randomized controlled trial. Indian Pediatrics 2012;49(6):449-54. [DOI] [PubMed] [Google Scholar]
Chowdhury 2021 {published data only}
- Chowdhury F, Shahid AS, Tabassum M, Parvin I, Ghosh PK, Hossain MI, et al. Vitamin D supplementation among Bangladeshi children under-five years of age hospitalised for severe pneumonia: a randomised placebo controlled trial. PLOS One 2021;16(2):e0246460. [DOI: 10.1371/journal.pone.0246460] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gupta 2016 {published data only}
- Gupta P, Dewan P, Shah D, Sharma N, Bedi N, Kaur IR, et al. Vitamin D supplementation for treatment and prevention of pneumonia in under-five children: a randomized double-blind placebo controlled trial. Indian Pediatrics 2016;53(11):967-76. [DOI] [PubMed] [Google Scholar]
Jingi 2018 {published data only}
- Jingi JK, Patil SS, Desai A. Effect of vitamin D supplementation in under-5 children with pneumonia: a randomized controlled trial. Indian Journal of Child Health 2018;5(4):235-9. [Google Scholar]
Labib 2021 {published data only}
- Labib JR, Ibrahem SK, Ismail MM, Fatah SA, Sedrak AS, Attia MA, et al. Vitamin D supplementation and improvement of pneumonic children at a tertiary pediatric hospital in Egypt: a randomized controlled trial. Medicine (Baltimore) 2021;100(13):e25011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manaseki‐Holland 2010 {published data only}
- Manaseki-Holland S, Qader G, Isaq Masher M, Bruce J, Zulf Mughal M, Chandramohan D, et al. Effects of vitamin D supplementation to children diagnosed with pneumonia in Kabul: a randomised controlled trial. Tropical Medicine and International Health 2010;15(10):1148-55. [DOI] [PubMed] [Google Scholar]
Somnath 2017 {published data only}
- Somnath SH, Biswal N, Chandrasekaran V, Jagdisan B, Bobby Z. Therapeutic effect of vitamin D in acute lower respiratory infection: a randomized controlled trial. Clinical Nutrition ESPEN 2017;20:24-8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Jadhav 2021 {published data only}
- Jadhav S, Khanwelkar C, Jadhav A, Seshla S. Vitamin D supplementation in the prevention of recurrent acute respiratory tract infections in children aged < 5 years. Journal of Medical Sciences 2021;3:129-33. [Google Scholar]
Singh 2019 {published data only}
- Singh N, Kamble D, Mahantshetti NS. Effect of vitamin D supplementation in the prevention of recurrent pneumonia in under-five children. Indian Journal of Pediatrics 2019;86(12):1105-11. [DOI] [PubMed] [Google Scholar]
Zhou 2016 {published data only}
- Zhou W, Zuo X, Li J, Yu Z. Effects of nutrition intervention on the nutritional status and outcomes of pediatric patients with pneumonia. Minerva Pediatrica 2016;68(1):5-10. [PubMed] [Google Scholar]
References to studies awaiting assessment
Bisht 2017 {published data only}
- Bisht A, Pannu MS, Singh N, Singh K, Kumar A, Neki NS. Role of vitamin D supplementation in severe pneumonia in children of age group 2 months to 5 years: a randomized controlled trial. International Journal of Current Research in Medical Sciences 2017;3(8):105-11. [Google Scholar]
Dhungel 2015 {published data only}
- Dhungel A, Alam MS. Efficacy of vitamin D in children with pneumonia: a randomized control trial study. Janaki Medical College Journal of Medical Sciences 2015;3(1):5-13. [Google Scholar]
Gaber 2018 {published data only}
- Gaber MM, Ali FA, Zaghlol KS. The effect of vitamin-D supplementation in severe pneumonia among infants. Medical Journal of Cairo University 2018;86(June):1303-9. [Google Scholar]
Rahmati 2016 {published data only}
- Rahmati MB, Rezapour M, Shahvari SZ. The effects of vitamin D supplementation in respiratory index of severity in children (RISC) of hospitalized patients with community-acquired pneumonia: a double-blind randomized clinical trial. Acta Health Medica 2016;1(3):60-4. [Google Scholar]
Rajshekhar 2016 {published data only}
- Rajshekhar CS, Vanaki R, Badakali AV, Pol RR, Yelamali BC. Efficacy of vitamin D supplementation in the treatment of severe pneumonia in children aged less than five years. International Journal of Contemporary Pediatrics 2016;3(1):96-9. [Google Scholar]
Shamaoon 2018 {published data only}
- Shamaoon M, Maryam, Ahsan M, Ahmad R. Vitamin D and pneumonia; role of vitamin D supplementation in children with pneumonia, a randomised control trial. Professional Medical Journal 2018;25(4):532-7. [DOI: 10.29309/TPMJ/18.4508] [DOI] [Google Scholar]
References to ongoing studies
NCT02054182 {published data only}
- NCT02054182. Effect of vitamin D supplementation in young South African children hospitalized with acute lower respiratory infection. clinicaltrials.gov/ct2/show/NCT02054182 (first received 18 January 2014).
Additional references
Akeredolu 2021
- Akeredolu FD, Akuse RM, Mado SM, Yusuf R. Relationship between serum vitamin D levels and acute pneumonia in children aged 1–59 months in Nigeria. Journal of Tropical Pediatrics 2021;67(1):fmaa101. [DOI: 10.1093/tropej/fmaa101] [DOI] [PubMed] [Google Scholar]
Alfirevic 2021
- Alfirevic Z, Kellie FJ, Stewart F, Jones L, Hampson L, on behalf of Pregnancy and Childbirth Editorial Board . Identifying and handling potentially untrustworthy trials in Pregnancy and Childbirth Cochrane Reviews. Available from: pregnancy.cochrane.org/news/identifying-and-handling-potentially-untrustworthy-trials-pregnancy-and-childbirth-cochrane (accessed 4 October 2022).
Alvarez‐Rodriguez 2012
- Alvarez-Rodriguez L, Lopez-Hoyos M, Garcia-Unzueta M, Amado JA, Cacho PM, Martinez-Taboada VM. Age and low levels of circulating vitamin D are associated with impaired innate immune function. Journal of Leukocyte Biology 2012;91(5):829-38. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al, GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bang 2011
- Bang UC, Novovic S, Andersen AM, Fenger M, Hansen MB, Jensen JE. Variations in serum 25-hydroxy vitamin D during acute pancreatitis: an exploratory longitudinal study. Endocrine Research 2011;36(4):135-41. [DOI] [PubMed] [Google Scholar]
Binks 2014
- Binks MJ, Smith-Vaughan HC, Bar-Zeev N, Chang AB, Andrews RM. Vitamin D insufficiency among hospitalised children in the Northern Territory. Journal of Paediatrics and Child Health 2014;50(7):512-8. [DOI: 10.1111/jpc.12623] [DOI] [PubMed] [Google Scholar]
Chang 2014
- Chang CC, Cheng AC, Chang AB. Over-the-counter (OTC) medications to reduce cough as an adjunct to antibiotics for acute pneumonia in children and adults. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No: CD006088. [DOI: 10.1002/14651858.CD006088.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chee 2022
- Chee E, Huang K, Haggie S, Britton PN. Systematic review of clinical practice guidelines on the management of community acquired pneumonia in children. Paediatric Respiratory Reviews 2022;42:59-68. [DOI: 10.1016/j.prrv.2022.01.006] [DOI] [PubMed] [Google Scholar]
Chowdhury 2022 [pers comm]
- Chowdhury F. Providing data reported in median (IQR) in our trial as mean (SD) [personal communication]. Email to: RR Das 27 February 2022.
Cochrane policy – managing problematic studies
- Cochrane Database of Systematic Reviews: editorial policies. Cochrane policy on managing potentially problematic studies. www.cochranelibrary.com/cdsr/editorial-policies#problematic-studies (accessed 3 October 2022).
Das 2012
- Das RR, Singh M, Shafiq N. Short-term therapeutic role of zinc in children < 5 years of age hospitalised for severe acute lower respiratory tract infection. Paediatric Respiratory Reviews 2012;13(3):184-91. [DOI] [PubMed] [Google Scholar]
Das 2017 [pers comm]
- Das RR. Information needed regarding antibiotic therapy and hospitalisation [personal communication]. Email to: M Rezapour 8 November 2017.
Das 2021
- Das RR, Satapathy AK, Mukherjee A, Goyal JP, Bhat JI, Ratageri VH, et al, Members of The ATU (Acute Respiratory Infection Treatment Unit) Group. Role of clinical criteria and oxygen saturation monitoring in diagnosis of childhood pneumonia in children aged 2 to 59 months. Indian Pediatrics 2021;58(11):1024-9. [PMID: ] [PubMed] [Google Scholar]
Gombart 2005
- Gombart AF, Borregaard N, Koeffler HP. Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxy vitamin D₃. FASEB Journal 2005;19(9):1067-77. [DOI] [PubMed] [Google Scholar]
Goyal 2021
- Goyal JP, Kumar P, Mukherjee A, Das RR, Bhat JI, Ratageri V, et al, Acute Respiratory Infection Treatment Unit Study Group. Risk factors for the development of pneumonia and severe pneumonia in children. Indian Pediatrics 2021;58(11):1036-9. [PMID: ] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version (accessed prior to 19 December 2022). Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available from gradepro.org.
Grant 2009
- Grant CC, Wall CR, Crengle S, Scragg R. Vitamin D deficiency in early childhood: prevalent in the sunny South Pacific. Public Health Nutrition 2009;12(10):1893-901. [DOI] [PubMed] [Google Scholar]
Grey 2020
- Grey A, Bolland MJ, Avenell A, Klein AA, Gunsalus CK. Check for publication integrity before misconduct. Nature 2020;577(7789):167-9. [DOI] [PubMed] [Google Scholar]
Gupta 2016 [pers comm]
- Gupta P. Providing data reported in median (IQR) in our trial as mean (SD) [personal communication]. Email to: RR Das 24 April 2016.
Haider 2011a
- Haider BA, Lassi ZS, Ahmed A, Bhutta ZA. Zinc supplementation as an adjunct to antibiotics in the treatment of pneumonia in children 2 to 59 months of age. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD007368. [DOI: 10.1002/14651858.CD007368.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haider 2011b
- Haider BA, Lassi ZS, Bhutta ZA. Short-course versus long-course antibiotic therapy for non-severe community-acquired pneumonia in children aged 2 months to 59 months. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No: CD005976. [DOI: 10.1002/14651858.CD005976.pub2] [DOI] [PubMed] [Google Scholar]
Hansdottir 2008
- Hansdottir S, Monick MM, Hinde SL, Lovan N, Look DC, Hunninghake GW. Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. Journal of Immunology 2008;181(10):7090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heaney 2012
- Heaney RP. Vitamin D – baseline status and effective dose. New England Journal of Medicine 2012;367(1):77-8. [DOI] [PubMed] [Google Scholar]
Hemilä 2013
- Hemilä H, Louhiala P. Vitamin C for preventing and treating pneumonia. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No: CD005532. [DOI: 10.1002/14651858.CD005532.pub3] [DOI] [PubMed] [Google Scholar]
Hewison 2011
- Hewison M. Antibacterial effects of vitamin D. Nature Reviews Endocrinology 2011;7(6):337-45. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Hollis 2011
- Hollis BW. Short-term and long-term consequences and concerns regarding valid assessment of vitamin D deficiency: comparison of recent food supplementation and clinical guidance reports. Current Opinion in Clinical Nutrition and Metabolic Care 2011;14(6):598-604. [DOI] [PubMed] [Google Scholar]
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
IAP 2006
- Agarwal R, Singh V, Yewale V. RTI Facts. IAP consensus guidelines on rational management of respiratory tract infections in children. Mumbai: Indian Academyof Pediatrics (IAP) 2006.
Implementation guidance – problematic studies
- Cochrane Editorial and Publishing Policy Resource. Policy for managing potentially problematic studies: implementation guidance. documentation.cochrane.org/display/EPPR/Policy+for+managing+potentially+problematic+studies%3A+implementation+guidance (accessed 4 October 2022).
Janssen 2007
- Janssen R, Bont L, Siezen CL, Hodemaekers HM, Ermers MJ, Doornbos G, et al. Genetic susceptibility to respiratory syncytial virus bronchiolitis is predominantly associated with innate immune genes. Journal of Infectious Diseases 2007;196(6):826-34. [DOI] [PubMed] [Google Scholar]
Joshi 2014
- Joshi K, Bhatia V. Vitamin D deficiency in a tropical country – treatment and prevention in children. Indian Journal of Pediatrics 2014;81(1):84-9. [DOI] [PubMed] [Google Scholar]
Kelishadi 2014
- Kelishadi R, Ardalan G, Motlagh ME, Shariatinejad K, Heshmat R, Poursafa P, et al. National report on the association of serum vitamin D with cardiometabolic risk factors in the pediatric population of the Middle East and North Africa (MENA): the CASPIAN-III Study. Nutrition 2014;30(1):33-8. [DOI] [PubMed] [Google Scholar]
Kimball 2011
- Kimball S, Vieth R, Dosch HM, Bar-Or A, Cheung R, Gagne D, et al. Cholecalciferol plus calcium suppresses abnormal PBMC reactivity in patients with multiple sclerosis. Journal of Clinical Endocrinology and Metabolism 2011;96(9):2826-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Labib 2022 [pers comm]
- Labib JR. Providing data reported in median (IQR) in our trial as mean (SD) [personal communication]. Email to: RR Das 27 February 2022.
Lassi 2014
- Lassi ZS, Kumar R, Das JK, Salam RA, Bhutta ZA. Antibiotic therapy versus no antibiotic therapy for children aged two to 59 months with WHO-defined non-severe pneumonia and wheeze. Cochrane Database of Systematic Reviews 2014, Issue 5. Art. No: CD009576. [DOI: 10.1002/14651858.CD009576.pub2] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Liu 2006
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 2006;311(5768):1770-3. [DOI] [PubMed] [Google Scholar]
Lodha 2013
- Lodha R, Kabra SK, Pandey RM. Oral antibiotics versus parenteral antibiotics for severe pneumonia in children. Cochrane Database of Systematic Reviews 2013, Issue 2. Art. No: CD004874. [DOI: 10.1002/14651858.CD004874.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luo 2018
- Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Statistical Methods in Medical Research 2018;27(6):1785-805. [DOI] [PubMed] [Google Scholar]
Manaseki‐Holland 2012
- Manaseki-Holland S, Maroof Z, Bruce J, Mughal MZ, Masher MI, Bhutta ZA, et al. Effect on the incidence of pneumonia of vitamin D supplementation by quarterly bolus dose to infants in Kabul: a randomised controlled superiority trial. Lancet 2012;379(9824):1419-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manaseki‐Holland 2017 [pers comm]
- Manaseki-Holland. Mortality data reported in our trial [personal communication]. Email to: RR Das 4 May 2017.
Mansbach 2009
- Mansbach JM, Ginde AA, Camargo CA. Serum 25-hydroxyvitamin D levels among US children aged 1 to 11 years: do children need more vitamin D? Pediatrics 2009;124(5):1404-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martineau 2012
- Martineau AR. Bolus-dose vitamin D and prevention of childhood pneumonia. Lancet 2012;379(9824):1373-5. [DOI] [PubMed] [Google Scholar]
Mathew 2010
- Mathew JL. Vitamin A supplementation for prophylaxis or therapy in childhood pneumonia: a systematic review of randomized controlled trials. Indian Pediatrics 2010;47(3):255-61. [DOI: 10.1007/s13312-010-0042-1] [DOI] [PubMed] [Google Scholar]
Mathew 2015
- Mathew JL, Singhi S, Ray P, Hagel E, Saghafian-Hedengren S, Bansal A, et al. Etiology of community acquired pneumonia among children in India: prospective, cohort study. Journal of Global Health 2015;5(2):050418. [DOI: 10.7189/jogh.05.020418] [DOI] [PMC free article] [PubMed] [Google Scholar]
McAllister 2006
- McAllister JC, Lane AT, Buckingham BA. Vitamin D deficiency in the San Francisco bay area. Journal of Pediatric Endocrinology and Metabolism 2006;19(3):205-8. [DOI] [PubMed] [Google Scholar]
Munns 2016
- Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global consensus recommendations on prevention and management of nutritional rickets. Journal of Clinical Endocrinology and Metabolism 2016;101(2):394-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mylott 2004
- Mylott BM, Kump T, Bolton ML, Greenbaum LA. Rickets in the Dairy State. Wisconsin Medical Journal 2004;103(5):84-7. [PubMed] [Google Scholar]
Najada 2004
- Najada AS, Habashneh MS, Khader M. The frequency of nutritional rickets among hospitalized infants and its relation to respiratory diseases. Journal of Tropical Pediatrics 2004;50(6):364-8. [DOI] [PubMed] [Google Scholar]
Nielsen 2010
- Nielsen NO, Skifte T, Andersson M, Wohlfahrt J, Søborg B, Koch A, et al. Both high and low serum vitamin D concentrations are associated with tuberculosis: a case-control study in Greenland. British Journal of Nutrition 2010;104(10):1487-91. [DOI] [PubMed] [Google Scholar]
NIH Vitamin D Fact Sheet
- National Institutes of Health (NIH) Office of dietary supplements. Vitamin D fact sheet for health professionals. ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ (accessed prior to 8 June 2017).
Oktaria 2021
- Oktaria V, Triasih R, Graham SM, Bines JE, Soenarto Y, Clarke MW, et al. Vitamin D deficiency and severity of pneumonia in Indonesian children. PLOS One 2021;16(7):e0254488. [DOI: 10.1371/journal.pone.0254488] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olliver 2013
- Olliver M, Spelmink L, Hiew J, Meyer-Hoffert U, Henriques-Normark B, Bergman P. Immunomodulatory effects of vitamin D on innate and adaptive immune responses to Streptococcus pneumoniae. Journal of Infectious Diseases 2013;208(9):1474-81. [DOI] [PubMed] [Google Scholar]
Perin 2022
- Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, Strong KL, et al. Global, regional, and national causes of under-5 mortality in 2000–19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child and Adolescent Health 2022;6(2):106-15. [DOI: 10.1016/S2352-4642(21)00311-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfeffer 2012
- Pfeffer PE, Hawrylowicz CM. Vitamin D and lung disease. Thorax 2012;67(11):1018-20. [DOI] [PubMed] [Google Scholar]
Popp 2022
- Popp M, Reis S, Schießer S, Hausinger RIlona, Stegemann M, Metzendorf M-I, et al. Ivermectin for preventing and treating COVID-19. Cochrane Database of Systematic Reviews 2022, Issue 6. Art. No: CD015017. [DOI: 10.1002/14651858.CD015017.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rajshekhar 2017 [pers comm]
- Rajshekhar C. Blinding and allocation concealment used in our trial [personal communication]. Email to: RR Das 3 June 2017.
Raloff 2006
- Raloff J. The antibiotic vitamin: deficiency in vitamin D may predispose people to infection. Science News 2006;170(20):312-7. [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robinson 2006
- Robinson PD, Högler W, Craig ME, Verge CF, Walker JL, Piper AC, et al. The re-emerging burden of rickets: a decade of experience from Sydney. Archives of Disease in Childhood 2006;91(7):564-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rudan 2008
- Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bulletin of the World Health Organization 2008;86(5):408-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Scott 2012
- Scott JA, Wonodi C, Moïsi JC, Deloria-Knoll M, DeLuca AN, Karron RA, et al. The definition of pneumonia, the assessment of severity, and clinical standardization in the Pneumonia Etiology Research for Child Health study. Clinical Infectious Diseases 2012;54(Suppl 2):109-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shetty 2021
- Shetty NS, Salvi RA, Thatte UM, Gogtay NJ. Has mandatory prospective registration of all studies brought about a change? A 1-year audit of studies registered in the Clinical Trials Registry of India [CTRI] before and after April 1, 2018. Perspectives in Clinical Research 2021;12(2):72-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Somnath 2022 [pers comm]
- Somnath SH. Providing data reported in median (IQR) in our trial as mean (SD) [personal communication]. Email to: RR Das 4 August 2022.
Thacher 2012
- Thacher TD, Fischer PR, Isichei CO, Zoakah AI, Pettifor JM. Prevention of nutritional rickets in Nigerian children with dietary calcium supplementation. Bone 2012;50(5):1074-80. [DOI] [PubMed] [Google Scholar]
Torun 2013
- Torun E, Genç H, Gönüllü E, Akovalı B, Ozgen IT. The clinical and biochemical presentation of vitamin D deficiency and insufficiency in children and adolescents. Journal of Pediatric Endocrinology and Metabolism 2013;26(5-6):469-75. [DOI] [PubMed] [Google Scholar]
Wagner 2008
- Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics 2008;122(5):1142-52. [DOI] [PubMed] [Google Scholar]
Wahed 2008
- Wahed MA, Islam MA, Khondakar P, Haque MA. Effect of micronutrients on morbidity and duration of hospital stay in childhood pneumonia. Mymensingh Medical Journal 2008;17(Suppl 2):S77-83. [PMID: ] [PubMed] [Google Scholar]
Walker 2009
- Walker VP, Modlin RL. The vitamin D connection to pediatric infections and immune function. Pediatric Research 2009;65(5 Pt 2):R106-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wan 2014
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2005
- Ward LM. Vitamin D deficiency in the 21st century: a persistent problem among Canadian infants and mothers. Canadian Medical Association Journal 2005;172(6):769-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2007
- Ward LM, Gaboury I, Ladhani M, Zlotkin S. Vitamin D deficiency rickets among children in Canada. Canadian Medical Association Journal 2007;177(2):161-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weibel 2022
- Weibel S, Popp M, Reis S, Skoetz N, Garner P, Sydenham E. Identifying and managing problematic trials: a Research Integrity Assessment (RIA) tool for randomized controlled trials in evidence synthesis. Research Synthesis Methods 2022 August 29 [Epub ahead of print]. [DOI: 10.1002/jrsm.1599] [DOI] [PMC free article] [PubMed]
Weisberg 2004
- Weisberg P, Scanlon KS, Li R, Cogswell ME. Nutritional rickets among children in the United States: review of cases reported between 1986 and 2003. American Journal of Clinical Nutrition 2004;8(Suppl 6):1697-705. [DOI] [PubMed] [Google Scholar]
White 2008
- White JH. Vitamin D signaling, infectious diseases, and regulation of innate immunity. Infection and Immunity 2008;76(9):3837-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2005
- World Health Organization. Handbook: IMCI integrated management of childhood illness, 2005. Available at: apps.who.int/iris/handle/10665/42939 (accessed 5 October 2022).
WHO 2014
- World Health Organization . Revised WHO Classification and Treatment of Childhood Pneumonia at Health Facilities. Evidence summaries, 2014. Available at: apps.who.int/iris/bitstream/handle/10665/137319/9789241507813_eng.pdf (accessed 5 October 2022).
WHO 2018
- World Health Organization. International standards for clinical trial registries – Version 3.0. Available at: www.who.int/publications/i/item/international-standards-for-clinical-trial-registers (accessed 4 October 2022).
Wondale 2005
- Wondale Y, Shiferaw F, Lulseged S. A systematic review of nutritional rickets in Ethiopia: status and prospects. Ethiopian Medical Journal 2005;43(3):203-10. [PubMed] [Google Scholar]
Zhang 2013
- Zhang W, Stoecklin E, Eggersdorfer M. A glimpse of vitamin D status in Mainland China. Nutrition 2013;29(7-8):953-7. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Das 2013
- Das RR, Singh M, Panigrahi I, Naik SS. Vitamin D supplementation for the treatment of acute childhood pneumonia: a systematic review. ISRN Pediatrics 2013;459160:eCollection 2013. [DOI: 10.1155/2013/459160] [DOI] [PMC free article] [PubMed] [Google Scholar]
Das 2015
- Das RR, Singh M, Naik SS. Vitamin D as an adjunct to antibiotics for the treatment of acute childhood pneumonia. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD011597. [DOI: 10.1002/14651858.CD011597] [DOI] [PMC free article] [PubMed] [Google Scholar]
Das 2018
- Das RR, Singh M, Naik SS. Vitamin D as an adjunct to antibiotics for the treatment of acute childhood pneumonia. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No: CD011597. [DOI: 10.1002/14651858.CD011597.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


