Abstract
Background
Musculoskeletal infections (MSKI), including osteomyelitis and septic arthritis, are among the most common invasive infections in children and have the potential to cause significant morbidity. Guidelines have been developed to optimize care based on clinician-developed endpoints. Patient-centered outcomes have not been defined for children with MSKI. This study identified outcomes most important to caregivers and patients with MSKI.
Methods
This was a single-center prospective qualitative study of children 6 months to 18 years of age hospitalized with MSKI from November 2019 to September 2021. Using design-research methods, patients and caregivers participated in interviews and/or completed journals to describe their experiences during acute infection and recovery from MSKI.
Results
A total of 51 patient/caregivers were approached to participate in the study, 35 of whom declined to participate, resulting in 8 interviews conducted and 14 journals collected from 16 patient/caregivers. From these, a journey map was created highlighting points of stress during the onset of symptoms, through hospitalization, and returning home with new challenges. In addition, patient-centered outcomes were identified. For caregivers, these included managing mental health, managing responsibilities, and receiving support. Both caregivers and patients shared the importance of understanding of treatment plans and responsibilities. For patients, improving mental and physical health was important.
Conclusions
Management of children with MSKI is complex and requires a multidisciplinary team approach. Validation of the outcomes identified and development of a measurement tool are needed. Addressing the patient-centered outcomes we identified in this study can greatly improve the holistic care of children with MSKI.
Keywords: osteomyelitis, patient-centered outcomes, septic arthritis
Using design-research methods, we identified patient-centered outcomes for caregivers and children with MSKI. Outcomes included managing mental health, managing responsibilities, and receiving support for caregivers, shared understanding of treatment plans and responsibilities, improving mental and physical health of the patient.
Musculoskeletal infections (MSKI), which include osteomyelitis and septic arthritis, are among the most common and complex invasive infections in children [1]. Although most children have excellent outcomes [2], serious acute and long-term complications can occur, including metastatic spread of infection, development of chronic infection, pathologic fractures, and limb length discrepancies [2, 3]. Optimal management requires a multidisciplinary team of surgical, medical, and physical therapy specialists. Cooperation and communication among the management team, patients, and caregivers are essential to ensure prompt diagnosis and treatment.
The Infectious Diseases Society of America (IDSA) has developed clinical practice guidelines that outline best practices for children with acute hematogenous osteomyelitis [4]. These guidelines, as well as previous research in pediatric MSKI management, focus on clinician-determined outcomes (eg, length of stay, laboratory values, etc) to decide how the delivery of care is optimized [4–7]. Although clinical endpoints are important, understanding patients’ and caregivers’ perspectives and providing care that is responsive to individual preferences, and values, are essential to deliver the highest quality of care [8]. The need to identify and provide patient-centered care has been recognized in the treatment of patients with invasive infections [9]; however, no such outcomes have been identified for children with MSKI. Therefore, the purpose of this study was to perform qualitative inquiry of children with MSKI and their caregivers to identify outcomes that are important to them during the treatment of and recovery from MSKI.
METHODS
Study Setting and Population
This was a single-center prospective qualitative study. All patients 6 months to 18 years of age, and their caregivers, who were admitted to Riley Hospital for Children (RHC) at Indiana University Health (Indianapolis, IN) with a diagnosis of acute hematogenous osteomyelitis or septic arthritis (as documented by the clinical team) from November 2019 to September 2021 were eligible. Patients and caregivers were excluded if they were unable (eg, language barrier) or unwilling to participate in at least 1 study activity: interview, survey, or journal.
Patient Consent
Written consent was obtained from caregivers and for all patients ≥ 18 years of age. Assent was obtained for children ≥7 years. Those unable or unwilling to give informed consent (or assent for children) were excluded. The study was approved by the Indiana University Institutional Review Board as an expedited study.
Recruitment and Study Design
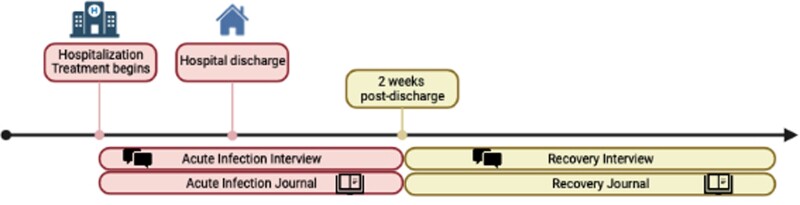
Potential study participants were identified by daily screening of the inpatient pediatric infectious diseases admission list in the electronic medical record. Study team members screened potential participants based on chief complaint and the admission note, without knowledge of MSKI severity or prognostic factors. Eligible children and their caregivers were approached by a study team member to gauge interest in the study. If interested, consent (and assent when appropriate) was obtained by a study team member, and an interview was scheduled (either in-person or via teleconference). Participants were classified as being in 1 of 2 phases of illness (Figure 1): the “acute infection” phase, which was defined as the time of initial hospitalization for MSKI to 2 weeks posthospitalization; and a “recovery” phase, which was defined as >2 weeks up to 12 months posthospitalization. Children and caretakers could participate in an interview during the acute infection phase, the recovery phase, or both. In addition, they could complete a journal during the acute infection phase, the recovery phase, or both. Participants were compensated with a gift card for each study activity completed.
Figure 1.
Musculoskeletal infection (MSKI) treatment timeline and study activities. Participants were classified as being in 1 of 2 phases of illness: the “acute infection” phase, which was defined as the time of initial hospitalization for MSKI to 2 weeks posthospitalization; and a “recovery” phase, which was defined as >2 weeks up to 12 months posthospitalization.
Data Collection
Interviews
Interviews were conducted by study team members (BH and DL) of Research Jam, the Indiana Clinical and Translational Science Institute's Patient Engagement Core. Interviews were conducted in-person (before the coronavirus disease 2019 [COVID-19] pandemic) or via teleconference (during the COVID-19 pandemic). Interviews were conducted jointly and both children and caregivers were encouraged to participate. If the child was not old enough (based on the discretion of the caregiver) or declined to participate, caregivers were relied upon for interview data. Interviews were semistructured, following a guided script. The goal of the interview was to learn patients’ and caregivers’ thoughts, concerns, and experiences through their journey to recovery from MSKI. For patients in the “acute infection phase”, questions centered around thoughts and concerns at the start of symptoms, through diagnosis, and about the treatment plan for discharge. For patients in the “recovery phase”, questions centered around challenges since hospital discharge, daily activities, including work and school, and how the MSKI has impacted daily life. Utilizing a cultural probe method [10], Research Jam created “iconimoes”-predesigned icons to elicit a response from participants in a manner that encouraged them to think outside their first instinctive answer. A cultural probe method is one of a variety of techniques used to gain insight into a participant's unique cultural context before beginning a design process. The facilitator asked the participant a question and then asked them to select an icon tile that represented their answer and to describe why they chose that icon. This method forces the participant to make one of the given options work for their story. It is less important what icon they choose and more important how they use it to tell their story. Iconimoes were used during all interviews, both in person and virtually. Interview sessions lasted 40–60 minutes, were recorded, and notes were made during transcript review. All audio and video recordings as well as text notes were stored securely on Indiana University servers, and no protected health information was stored or maintained as part of the study.
Journals
In addition to interviews, children and caregivers were given journals to capture “in the moment” thoughts and concerns on their own time. Journals had prompt questions to help focus their thoughts, iconimoes, as well as space for open-ended answers. Journals were given for both the acute infection and recovery phases. Before the COVID-19 pandemic, journals were given as a physical notebook. Patients and caregivers were encouraged to document thoughts daily until their follow-up appointment, but no minimum documentation was required. During the COVID-19 pandemic, journals were transitioned to online surveys using Qualtrics survey software (www.qualtrics.com). Qualtrics is a secure data management platform that encrypts data in transit with a high-level security management system to ensure the integrity and confidentiality of personal health information.
Analysis
Qualitative data were collected and analyzed by study team members (BH and DL) using notes taken from the interviews and in raw data from the physical and digital journals. The affinity diagramming method was used to organize data into a hierarchy that revealed common issues and themes [11]. Affinity diagramming is a method of discovering relationships among ideas, then emphasizing and highlighting their likenesses [12]. The diagramming process itself is generative, in that it creates further knowledge about the data. The method's output allows for visualization of larger forged idea patterns and connections. From thousands of discrete data points, a theme or set of themes can be found that point to a more manageable set of patterns. To create the affinity diagram for this analysis session, the individual data points were displayed on Miro, a collaborative whiteboard and virtual workspace (www.miro.com). Data were separated into individual data points or “snippets,” with each snippet on an individual virtual sticky note. The sticky notes were color-coded based on the participant and tagged based on the phase (acute infection or recovery) and the question the note was answering. Physically separating each snippet allowed for easy physical manipulation of singular concepts. The study team then moved the snippets around to create groupings based on relatedness of the content. The team collaboratively worked through the snippets, identifying, discussing, and confirming relationships and connections between them. Once all the snippets were sorted to the team's satisfaction, each group of snippets was given a name, based on its theme.
In addition, modeling was used to identify and detail relationships in the collected data. Modeling involves creating visualizations of the ideas represented in the data [12]. The study team members externalize their mental models for other team members to critique and build upon. The resulting models help the study team and other stakeholders create a shared understanding of the collected data.
RESULTS
We identified 74 patients with MSKI admitted to RHC during the enrollment period. Of those, 5 were excluded due to age less than 6 months, 4 had a language barrier, 14 were unable to be consented because enrollment was paused due to the COVID-19 pandemic (March 2020–June 2020), and 35 declined to participate. Sixteen patient/caregiver participants enrolled and completed at least 1 study activity. Characteristics of the 16 enrolled children with MSKI are shown in Table 1. The majority were White, male, with a median age of 9 years (interquartile range [IQR], 5.75–11.25 years). The median household income by participant zip code was $52 055 (compared to $58 235 for Indiana). The median duration of hospitalization was 8 days (IQR, 5–10 days) and total antibiotics was 47 days (IQR, 30.5–177.5). Nine patients (56.3%) had full recovery without complications. Seven had complications including 5 who developed chronic infections (identified by notation in the medical record of chronic osteomyelitis/infection or radiographic evidence of chronic infection, such as a sequestrum or Brodie's abscess) requiring several months of antibiotics, and 1 requiring limb amputation.
Table 1.
Characteristics of Children With MSKI
| Characteristic | N (%) |
|---|---|
| Age | … |
| Median, years (IQR) | 9 (5.75–11.25) |
| Range, years | 0.75–13 |
| Sex | … |
| Male | 10 (63) |
| Female | 6 (38) |
| Race/Ethnicity | … |
| White, non-Hispanic | 15 (94) |
| Black, non-Hispanic | 1 (6) |
| Type of MSKI | … |
| Osteomyelitis only | 7 (44) |
| Septic arthritis only | 4 (25) |
| Both | 5 (31) |
| Infection-Related Complicationa | … |
| None | 9 (56) |
| Chronic infection | 5 (31) |
| Sepsis | 1 (6) |
| Deep vein thrombosis | 1 (6) |
| Pathologic fracture | 1 (6) |
| Limb amputation | 1 (6) |
Abbreviations: IQR, interquartile range; MSKI, musculoskeletal infection.
Participants could have >1 complication.
A total of 8 interviews were conducted (7 in the acute infection phase and 1 in the recovery phase), and 14 journals were collected (4 in the acute infection phase and 10 in the recovery phase). The median time of study activity completion for the recovery phase was 211 days (range 24 to 360 days). Of the 8 interviews, 1 was conducted with the patient only, 2 were coconducted with the patient and caregiver, and 5 were conducted only with the caregiver. All 14 journals were completed by caregivers. Five participants completed more than 1 study activity, and 2 participants completed at least 1 study activity in both the acute infection and recovery phases.
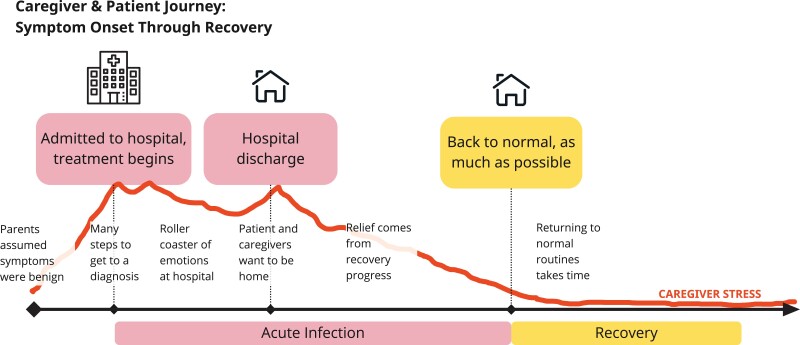
Caregiver/Patient Journey
Based on participant responses, we created a caregiver and patient journey map (Figure 2). Because caregivers of children with MSKI were the primary population engaged in the study activities, the patient and caregiver journey maps are intertwined. Their journey begins with seemingly benign symptoms that are present among a variety of commonplace injuries and illnesses, often leading to a delay in MSKI diagnosis. As the patient's symptoms continue to escalate, caregiver stress increases through diagnosis until treatment begins. Once admitted to the hospital, caregivers and patients experience a range of emotions as they work with many different healthcare professionals, experience the successes and challenges of diagnosis and treatment, often become isolated from the outside world, and desire to return home. Once discharged, the family faces the stresses of caring for a patient without the help of professionals. In addition, the patient may face mobility restrictions that necessitate a caregiver's constant presence. Both patients and caregivers face limits on their ability to engage in their regular activities. It takes time to return to what was previously a physically and mentally normal state and includes adapting previous routines to a life after MSKI.
Figure 2.
Musculoskeletal infection patient and caregiver journey map.
Family-Centered Outcomes
Using responses from the interviews and journals, we identified patient-centered outcomes for caregivers and children with MSKI. These were divided into those “during MSKI” and “post-MSKI”, and categorized by caregiver, shared, and patient outcomes (Table 2). During MSKI included the timeframe while the patient was being medically managed for MSKI (on antibiotics and being followed by infectious diseases, both inpatient and outpatient). Post-MSKI was the time after MSKI medical management was finished. The timing of these phases was different among families because patients had differing severity of MSKI and recovery timeframes.
Table 2.
Caregiver and Patient-Centered Outcomes
| Caregiver Outcomes | Shared Outcomes | Patient Outcomes | |
|---|---|---|---|
| Mental Health | Understanding Treatment Plan | Mental Health | |
| During MSKI | Feelings of excessive guilt Feelings of irritability/anger Depressed mood Feeling overwhelmed Sleep disturbances and fatigue Experiencing memory or concentration issues Excessive worry and obsessive symptom checking |
Both patient and caregiver understand treatment plan Ability to comply with treatment plan (eg, medications, mobility, etc) Comfort with pace of recovery |
Excessive fear of medical procedures |
| Post-MSKI | Relationships with others are negatively affected | Understand long-term effects/limits | Return to normal behavior/mood Long-term mental health effects from experience with MSKI |
| Managing Responsibilities | Managing Responsibilities | Physical Health | |
| During MSKI | Maintain self-care Maintain care for other family members Provide support for the patient |
Establish a routine during treatment Shared recovery responsibilities when age appropriate (eg, dressing change) |
Side effects of treatments (eg, GI upset from antibiotics) Pain control Ability to adhere to mobility limits |
| Post-MSKI | Return to normal work schedule Concerns about finances |
Family can return to normal activities | Return to normal mobility Return to school and activities Return to normal appetite |
| Receiving Support | … | … | |
| During MSKI | Feeling heard and getting questions answered by the medical team Have support outside the hospital (eg, family, friends) |
… | … |
| Post-MSKI | Comfort leaving the patient with other caregivers or alone (if age appropriate) | … | … |
Abbreviations: GI, gastrointestinal; MSKI, musculoskeletal infection.
Several important themes arose during each phase (Table 2). During MSKI, the major themes for caregivers included managing mental health, managing responsibilities, and receiving support. Caregivers reflected on feeling guilty, overwhelmed, having concerns about their ability to provide support for the patient, and feeling supported by the medical team and other social support. Illustrative quotes from caregivers included, “I felt horrible because I didn’t listen when my son said it was so painful.”; “I broke down once we got home. It was just a release of emotions that I had bottled up during the stay in the hospital. I went on antidepressants for a couple months…”. Shared patient and caregiver outcomes included understanding treatment plans and managing responsibilities. Outcomes shared by caregivers and patients focused on comfort with the pace of, and ability to adhere to, the treatment plan as well as the whole family's ability to return to normal activities. Patient outcomes during MSKI included physical effects of treatment and mental health during and after treatment. These outcomes focused on the patient's pain and comfort, side effects of treatment (eg, antibiotics), and fear of medical procedures. During the post-MSKI phase, the same themes persisted, but they were manifested differently, as the patient was no longer receiving medical treatment for MSKI. Details of each theme are highlighted in Table 2.
Caregivers and patients (when able) articulated a need “to be heard” by the care team to address their concerns. In all cases, social workers and case managers were involved to address many of these issues, but often they were not utilized until it became a major stressor for the family. During the hospitalization 75% (12 of 16) were offered a consult by a Child Life specialist. Of these, 11 of 12 accepted the Child Life specialist consult, with the vast majority (9 of 11) addressing coping mechanisms with the medical experience (eg, IV placement, blood draws, procedures), 1 pertaining to pill swallowing and 1 addressing psychosocial needs.
DISCUSSION
In this qualitative study we identified outcomes that are most important to caregivers and patients with MSKI. We identified that the most common outcomes important to caregivers were the ability to manage their mental health and responsibilities and find support. Themes for patients revolved around managing the physical effects of treatment and ability to return to normal activities as well as the mental wellbeing during and after treatment. The outcomes identified in this study are novel and specific to caretaker and children with MSKI, but they are broadly consistent with domains found in widely used, validated patient-centered outcomes tools [13, 14].
We found that these outcomes are not typically assessed and rarely addressed during the management of children with MSKI. Further study to validate these findings and development of a measurement tool for these outcomes are needed. By identifying these outcomes and measuring which are most in need of improvement during the management of children with MSKI, we will be able to target interventions for this population that could impact their overall wellbeing and quality of care.
Addressing the mental health of caregivers and patients during and after the treatment of MSKI is critical to optimize outcomes, both acute and long term. Evidence suggests an association exists between severe infections in children requiring hospitalization and risk of mental health disorders and cognitive ability [15, 16]. The focus of treatment in children with MSKI is often limited to objective clinical measures including fever curve, laboratory markers, and clinical exam. Although these are important for guiding medical therapy, the mental health of caregivers and patients is often overlooked and can have a significant impact on the overall wellness of the patient and family. During our study, caregivers reported (1) feeling guilty about not recognizing the seriousness of their child's symptoms earlier and (2) survivor's guilt leaving the hospital with their child while other families had to stay in the hospital longer or even lost their children. Caregivers also reported feeling fear and anxiety about their child's condition, potential bad outcomes, and feeling overwhelmed by the diagnosis and treatment process. For one caregiver, the mental health impacts prompted the initiation of antidepressant medication. For patients, many of whom were school aged or younger, managing mental health revolved around fear of medical procedures and changes in behavior/personality. The ability to decrease these fears and return to normal behavior were important. These themes highlight the importance of a multidisciplinary approach to treating children with MSKI. Involvement of Child Life specialists and psychologists at admission can play a critical role in decreasing patient's fears and improving the quality of care. In addition, engaging social work and other services to help support caregivers is essential.
For patients, the physical effects of treatment and ability to return to normal activities were also important themes. During MSKI treatment, the patient's comfort level and fear around medical procedures was especially important. Some patients experienced side effects such as allergic reactions to medications and medical dressings. These may seem minor to the clinical team, but they were reported as important to patients. Caregivers reported their children experiencing significant pain before diagnosis and during the treatment and recovery periods. Pain management and attention to treatment-related side effects are important to patients. During the recovery phase, the ability to return to normal activities and mobility was important. For school-aged children, return to school was very important. Assessment of these physical effects by the providers as well as physical therapist are important for optimizing care of children with MSKI.
Many of the themes identified in our study, including caregiver guilt, patient depressed mood, fear, and anxiety, overlap with those found for children with severe, chronic illness such as cancer and asthma [17–19] and are measured using generic pediatric quality-of-life tools [13, 20]. There were several outcomes unique to children with MSKI, however, including ability to adhere to mobility restrictions (especially for toddlers), return to normal mobility and activities, and fear around discharge to home. These novel outcomes are likely a result of the unique nature of MSKIs being sudden in onset, with a common age of infections being <5 years, multiple phases of illness (hospitalization and recovery at home), and the anticipation of full recovery. Our results support the idea of using a patient-centered outcomes measurement tool that integrates both generic and disease-specific quality-of-life measures, enabling comparisons across groups and benchmarking with healthy populations, as well as improving sensitivity for health domains specific for MSKI [14].
There are important limitations to our study. First, this is a single-center study of children at a large, tertiary children's hospital. In addition, although we tried to assess a broad range of patients, our sample size is relatively small, with little racial diversity, possibly limiting generalizability. Finally, 44% of our population had at least 1 complication. This is significantly higher than reported complication rates for pediatric MSKI [21]. This may be a result of self-selection bias because patients with more severe infection may have been more likely to participate. Patients with more mild symptoms, or less severe infection, may not share all of these concerns. Designing tools for more extreme cases, however, allows for increased accessibility without limiting usability to more “typical” cases [2]. Despite these limitations, we believe the results are novel and meaningful.
CONCLUSIONS
In conclusion, management of children with MSKI is complex and requires a multidisciplinary team approach. Further study and validation of these outcomes and development of a measurement tool are needed and planned. Such a tool could be specifically tailored to MSKI, or, since many patient and caregiver experiences are likely shared with the other serious infections, be more broadly applicable to children with a variety of invasive infections. By addressing the caregiver and patient-centered outcomes identified in this study, we can greatly improve the holistic care of these patients.
Acknowledgments
We thank Lisa Parks, Vickie Cater, Cathy Luthman, and the PResNet team.
Financial support. This work was funded by the National Institutes of Health, Agency for Healthcare Research and Quality (1K12HS026390-01; to AEC).
Contributor Information
James B Wood, Center for Pediatric and Adolescent Comparative Effectiveness Research, Indiana University School of Medicine, Indianapolis, Indiana, USA; Ryan White Center for Pediatric Infectious Diseases and Global Health, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Bridget Hawryluk, Indiana Clinical and Translational Sciences Institute's Patient Engagement Core, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Dustin Lynch, Indiana Clinical and Translational Sciences Institute's Patient Engagement Core, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Gina Claxton, Indiana Clinical and Translational Sciences Institute's Patient Engagement Core, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Kelsey Russell, Center for Pediatric and Adolescent Comparative Effectiveness Research, Indiana University School of Medicine, Indianapolis, Indiana, USA.
William E Bennett, Jr., Center for Pediatric and Adolescent Comparative Effectiveness Research, Indiana University School of Medicine, Indianapolis, Indiana, USA Indiana Clinical and Translational Sciences Institute's Patient Engagement Core, Indiana University School of Medicine, Indianapolis, Indiana, USA; Division of Pediatric Gastroenterology, Hepatology and Nutrition, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Sarah E Wiehe, Indiana Clinical and Translational Sciences Institute's Patient Engagement Core, Indiana University School of Medicine, Indianapolis, Indiana, USA; Children's Health Services Research, Indiana University School of Medicine, Indianapolis, Indiana, USA.
Aaron E Carroll, Center for Pediatric and Adolescent Comparative Effectiveness Research, Indiana University School of Medicine, Indianapolis, Indiana, USA.
References
- 1. Arnold JC, Bradley JS. Osteoarticular infections in children. Infect Dis Clin North Am 2015; 29:557–74. [DOI] [PubMed] [Google Scholar]
- 2. Yi J, Wood JB, Creech CB, et al. Clinical epidemiology and outcomes of pediatric musculoskeletal infections. J Pediatr 2021; 234:236–44.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoppe PA, Holzhauer S, Lala B, et al. Severe infections of Panton-Valentine leukocidin positive Staphylococcus aureus in children. Medicine (Baltimore) 2019; 98:e17185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Woods CR, Bradley JS, Chatterjee A, et al. Clinical practice guideline by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America: 2021 guideline on diagnosis and management of acute hematogenous osteomyelitis in pediatrics. J Pediatric Infect Dis Soc 2021; 10:801–44. [DOI] [PubMed] [Google Scholar]
- 5. Copley LA, Kinsler MA, Gheen T, Shar A, Sun D, Browne R. The impact of evidence-based clinical practice guidelines applied by a multidisciplinary team for the care of children with osteomyelitis. J Bone Joint Surg Am 2013; 95:686–93. [DOI] [PubMed] [Google Scholar]
- 6. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr 2015; 169:120–8. [DOI] [PubMed] [Google Scholar]
- 7. Zaoutis T, Localio AR, Leckerman K, Saddlemire S, Bertoch D, Keren R. Prolonged intravenous therapy versus early transition to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics 2009; 123:636–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Institute of Medicine (US) Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US), 2001. doi: 10.17226/10027. [DOI] [PubMed] [Google Scholar]
- 9. Berrevoets MAH, Oerlemans AJM, Tromp M, et al. Quality of outpatient parenteral antimicrobial therapy (OPAT) care from the patient's perspective: a qualitative study. BMJ Open 2018; 8:e024564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gaver B, Dunne T, Pacenti E. Design: cultural probes. Interactions 1999; 6:21–9. [Google Scholar]
- 11. Holtzblatt K, Beyer H. 6—the Affinity diagram. In: Holtzblatt K, Beyer H, eds. Contextual Design. Second Edition. Boston: Morgan Kaufmann, 2017: pp. 127–46. doi: 10.1016/B978-0-12-800894-2.00006-5. [DOI] [Google Scholar]
- 12. Kolko J. Exposing the Magic of Design: A Practitioner's Guide to the Methods and Theory of Synthesis. Oxford Series in Human-Technology Interaction. New York: Oxford University Press, 2011. doi: 10.1093/acprof:oso/9780199744336.001.0001. [DOI] [Google Scholar]
- 13. Luijten MAJ, Haverman L, van Litsenburg RRL, Roorda LD, Grootenhuis MA, Terwee CB. Advances in measuring pediatric overall health: the PROMIS(R) Pediatric Global Health Scale (PGH-7). Eur J Pediatr 2022: 181:2117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001; 39:800–12. [DOI] [PubMed] [Google Scholar]
- 15. Kohler-Forsberg O, Petersen L, Gasse C, et al. A nationwide study in Denmark of the association between treated infections and the subsequent risk of treated mental disorders in children and adolescents. JAMA Psychiatry 2019; 76:271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kohler-Forsberg O, Sorensen HJ, Nordentoft M, McGrath JJ, Benros ME, Petersen L. Childhood infections and subsequent school achievement among 598,553 Danish children. Pediatr Infect Dis J 2018; 37:731–7. [DOI] [PubMed] [Google Scholar]
- 17. Battula M, Arunashekar P, Nagarajan VP. A prospective study to assess the quality of life in children with newly diagnosed asthma and their caregivers using the pediatric asthma quality of life questionnaire. J Prim Care Community Health 2020; 11:2150132720961272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Qual Life Res 1996; 5:35–46. [DOI] [PubMed] [Google Scholar]
- 19. Hinds PS, Wang J, Cheng YI, et al. PROMIS pediatric measures validated in a longitudinal study design in pediatric oncology. Pediatr Blood Cancer 2019; 66:e27606. [DOI] [PubMed] [Google Scholar]
- 20. Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999; 37:126–39. [DOI] [PubMed] [Google Scholar]
- 21. Cavicchio S. Make Your Users Happy By Designing for the Extremes. Available at: https://medium.com/@salvycavicchio/designing-for-extremes-e0d13f84c61e. Accessed 24 March 2022. [Google Scholar]