There was an immediate improvement following Viz.ai implementation for both direct-arriving and telemedicine-transfer thrombectomy cases.
Abstract
BACKGROUND AND PURPOSE:
Comprehensive stroke centers continually strive to narrow neurointerventional time metrics. Although process improvements have been put in place to streamline workflows, complex pathways, disparate imaging locations, and fragmented communications all highlight the need for continued improvement.
MATERIALS AND METHODS:
This Quality Improvement Initiative (VISIION) was implemented to assess our transition to the Viz.ai platform for immediate image review and centralized communication and their effect on key performance indicators in our comprehensive stroke center. We compared periods before and following deployment. Sequential patients having undergone stroke thrombectomy were included. Both direct arriving large-vessel occlusion and Brain Emergency Management Initiative telemedicine transfer large-vessel occlusion cases were assessed as were subgroups of OnHours and OffHours. Text messaging thread counts were compared between time periods to assess communications. Mann-Whitney U and Student t tests were used.
RESULTS:
Eighty-two neurointerventional cases were analyzed pre vs. post time periods: (DALVO-OnHours 7 versus 7, DALVO-OffHours 10 versus 5, BEMI-OnHours 13 versus 6, BEMI-OffHours 17 versus 17). DALVO-OffHours had a 39% door-to-groin reduction (157 versus 95 minutes, P = .009). DALVO-All showed a 32% reduction (127 versus 86 minutes, P = .006). BEMI-All improved 33% (42 versus 28 minutes, P = .036). Text messaging thread counts improved 30% (39 versus 27, P = .04).
CONCLUSIONS:
There was an immediate improvement following Viz.ai implementation for both direct arriving and telemedicine transfer thrombectomy cases. In the greatest opportunity subset (direct arriving large-vessel occlusion-OffHours: direct arriving cases requiring team mobilization off-hours), we noted a 39% improvement. With Viz.ai, we noted that immediate access to images and streamlined communications improved door-to-groin time metrics for thrombectomy. These results have implications for future care processes and can be a model for centers striving to optimize workflow and improve thrombectomy timeliness.
For acute stroke, rtPA is the only approved pharmacologic treatment.1 For nonpharmacologic interventions, neurointerventional radiology procedures have become standard of care for patients with anterior circulation strokes within a 6-hour time window.2,3 Thrombectomy, in appropriately selected patients, is also effective in the extended 6- to 24-hour window.3-5 Thrombectomy is the most effective procedure for reducing functional disability for patients with large-vessel occlusion (LVO).6 Treating facilities such as comprehensive stroke centers assess key time metrics to continually improve quality of care. These metrics include goals of door-to-needle times within 60 minutes in 85% and within 30 minutes in 50% of patients with acute ischemic stroke treated with IV thrombolytics, as well as door-to-device times within 90 minutes (for direct arriving) and within 60 minutes (for transfer) patients.7 Numerous process-improvement workflows have been put in place to help attain these goals for tPA and thrombectomy.8-10 Centers strive to improve door-to-groin and door-to-recanalization times because rapid triage and fast reperfusion times are important predictors of outcome.11 Numerous strategies, including improved processes, transfer enhancements, and direct admission to the angiogram suite, have shown improvements in patients with LVO.12-18 At our comprehensive stroke center, time metrics were not ideal, so continued improvement pathways were needed.
Stroke telemedicine (telestroke) networks are in place to help evaluate patients and transfer those that require a step up in care to thrombectomy-capable centers. Although telestroke improves access and the correctness of decision-making,19 transfers still fare worse than patients who directly arrive to thrombectomy-capable centers due to the added transfer time.20 Although much of this additional time is obligatory given the distance from thrombectomy centers, decreasing transfer time is also a critical goal. Our center has put in place the Brain Emergency Management Initiative (BEMI) transfer pathway for patients evaluated initially at participating telestroke centers that require transfer for possible thrombectomy. This process has enabled a rapid transfer for possible embolectomy by decreasing operational redundancy, and functions well in our telehealth paradigm.17 Although patients arrive quickly because of BEMI, communications between hyperacute teams still remain complex. Nontransfer, direct arriving LVO (DALVO) cases can increase the communication burden because the time window between patient arrival and intervention is compressed (these cases do not allow the additional time buffer of telestroke, which allows mobilization of angiography teams while a patient is being transferred).
Weaknesses often found in stroke-care pathways are poor communication and poor cooperation among health professionals and facilities.21 In acute stroke, communication processes can be complex because numerous teams require timely communication and rapid mobilization for patients with both BEMI and DALVO. Communication pathways place a strong onus on the coordinating provider to ensure that all parties are aware of patient status, destination, and timing. All this would take place during the decision-making process regarding whether the patient was a candidate for transfer (for BEMI cases) or a candidate for neurointervention based on advanced imaging techniques that our comprehensive stroke center has had in place since the initial embolectomy trials in both the standard and extended time windows (for patients with both BEMI and DALVO).4,5,22
In our center, complex pathways, disparate imaging locations, and fragmented communications all highlighted a need for continued improvement in our hyperacute stroke-care pathway. We sought a solution that allowed the following: 1) immediate/mobile access to advanced imaging, 2) advanced CT perfusion mapping to help guide quick interventional decision-making, and 3) a Health Insurance Portability and Accountability Act (HIPAA)–compliant communications platform allowing a coordinated, single-location, secure, text-messaging thread for all care team members to access and be aware of patient status, decision information, and patient destination/location. Our aim was to determine whether we could improve neurointerventional time metrics.
MATERIALS AND METHODS
The Viz neuroimaging platform (Viz.ai; http://viz.ai) was implemented to optimize assessment and synchronize workflow for patients with acute stroke, with additional focus on those patients who may be potential candidates for neurointervention. Using artificial intelligence, this system uses machine learning techniques for automated neuroimaging processing and interpretation. Additional features include real-time, HIPAA-compliant, dynamic viewing of high-fidelity images on mobile devices, group communication messaging, and an artificial intelligence algorithm that automatically identifies suspected LVO strokes on CTA. We transitioned to the use of Viz.ai on January 18, 2021, for clinical care, we maintained research licenses for use of RAPID (iSchemaView).
In an institutional review board–approved Quality Initiative project, we implemented the Viz.ai Implementation of Stroke augmented Intelligence and communications platform to improve Indicators and Outcomes for a comprehensive stroke center and Network (VISIION) pathway for hyperacute stroke assessments for cases of both BEMI and DALVO. This assessed an improvement in times in our comprehensive stroke center. The advanced imaging platform, very similar to our prior experience with RAPID, allowed our hyperacute stroke teams access to images on a secure mobile platform to assess LVO. On-screen tools allowed image rotation in 3D space to better assess vessel morphology as well as review advanced imaging such as CT perfusion maps for cases thought to be potential candidates for neurointervention in the extended window. Providers downloaded the HIPAA-compliant Viz.ai medical tool and used HIPAA-compliant user credentials for access. This secure access allowed review of patient images from our hub facilities (and indirectly from our spoke sites because we already had virtual private network access to these images). The secure text-messaging thread (Fig 1, right) allowed all credentialed participants to access a single point of communication for awareness of patient status, medical issues, and next steps. More than 250 team members were given access, including the stroke team, neurointerventional team, neuroradiology, neurocritical care, charge nurse, transfer center, and house supervisor. Since deployment, additional service areas have been offered access (eg, CT team, angiography team, anesthesia team, and registration team). Providers are able to toggle the setting to “on-call” so as to be aware of cases only when on-shift. It is estimated that only 15–25 providers were actively toggled to on-call during any shift. When a stroke code is called (from either internal or external sites in our network), the stroke provider evaluates the patient and accesses the Viz.ai images on a hand-held device (desktop access was not yet enabled at time of the pilot). The neurointerventional team is contacted using the secure app, and care determinations such as appropriateness for rtPA and thrombectomy are made, including decisions to transfer patients for intervention.
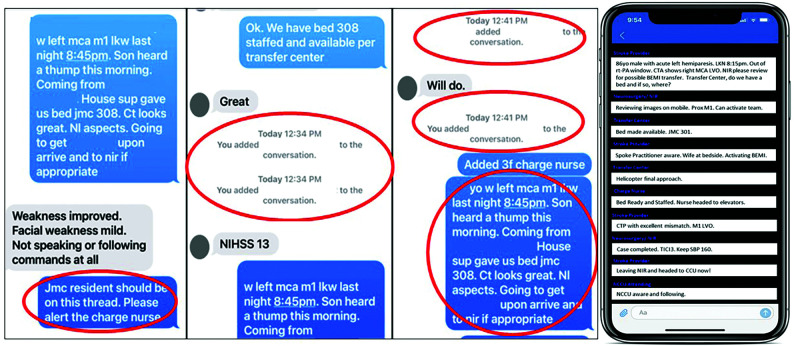
FIG 1.
Team messaging. An encrypted message pre-Viz.ai implementation shows fragmented communication, addition of parties who then have limited data and the need for redundant explanations (left), and a post-Viz.ai implementation example of a secure text-messaging thread with all relevant parties able to view and contribute to a centralized text-messaging thread (right).
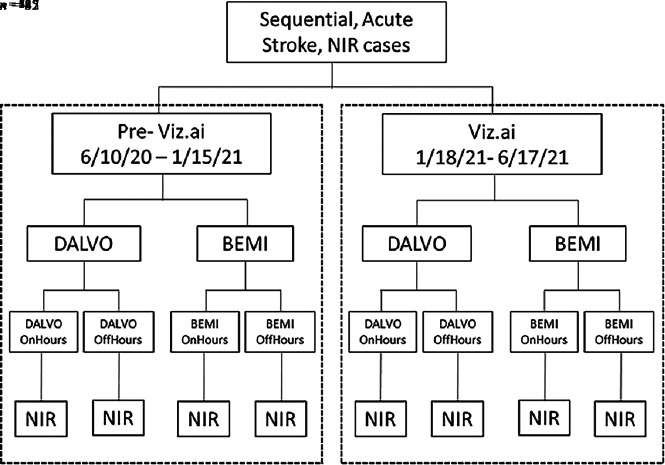
In this initiative, we compared thrombectomy cases from a pre-Viz.ai period (June 10, 2020, to January 17, 2021) with a postdeployment period (January 18, 2021, to June 17, 2021) to assess improved time metrics. Sequential acute stroke cases, requiring embolectomy, were included in this analysis. Cases were further stratified into BEMI (OnHours and OffHours) and DALVO (OnHours and OffHours) on the basis of whether the angiography team was in-house or required activation and mobilization to the hospital (Fig 2). OnHours included weekdays, while OffHours included nights, weekends, and holidays. Comparisons were made for the overall group, for the DALVO and BEMI subgroups, and for the OnHours and OffHours subgroups, comparing the pre- to postimplementation periods. Time outcomes assessed for this initiative included door-to-CT, team activation–to-groin, door-to-groin, door-to-device, and door-to-recanalization. For transfer cases, additional time outcomes were assessed, including spoke code–to-transfer decision, transfer decision–to-hub door, and spoke door–to-groin. To assess whether a quantitative signal could be noted for communication optimization, we assessed text-messaging thread count totals, comparing the first 3 months of the pilot with the second 3 months of the pilot (as well as compared with the last 3 months of our current use of the platform) to assess whether the improved process could be reflected in the number of text messages sent by providers across time. Text-messaging thread counts were defined as the number of specific text entries on a text-message thread for an individual case. The Mann-Whitney U test was used for non-normally distributed data. The Student t test was used for mean comparisons of text-messaging thread counts. Viz.ai had no influence on the direction of results or publication.
FIG 2.
Pre-Viz.ai and postimplementation Viz.ai time periods and case numbers. This nonrandomized, pre-/postassessment design compared pre-implementation cases with postimplementation cases, stratified by DALVO and BEMI subgroups, numbers in each subgroup, and OnHours or OffHours are listed. NIR indicates neurointervention cases.
RESULTS
A total of 82 patients having undergone embolectomy were assessed overall, pre-Viz.ai-versus-post-Viz.ai implementation (47 pre-Viz.ai, 35 post-Viz.ai) (Online Supplemental Data). This pilot assessment included a comparison of 29 DALVO patients (17 versus 12) and 53 BEMI patients (30 versus 23). There were 14 DALVO OnHours cases (7 versus 7), 15 DALVO OffHours cases (10 versus 5), 19 BEMI OnHours cases (13 versus 6), and 34 BEMI OffHours cases (17 versus 17).
For door-to-groin comparisons, DALVO-OffHours had a significant 39% reduction (157 versus 95 minutes, P = .009). DALVO-All showed a significant 32% reduction (127 versus 86 minutes, P = .006). BEMI-All had a significant 33% reduction in median door-to-groin times (42 versus 28 minutes, P = .036). DALVO-OnHours improved 19% (97 versus 79 minutes, P = .201). BEMI-OnHours improved 18% (37 versus 31 minutes, P = .337). BEMI-OffHours improved 38% (45 versus 28 minutes, P = .077). Overall, there was a 22% reduction (50 versus 39 minutes, P = .066) in door-to-groin times after Viz.ai implementation.
We also analyzed other time metric outcomes. For door-to-CT, DALVO-OffHours had a significant 92.2% reduction (25.5 versus 2 minutes, P = .01), and DALVO-All improved 73.2% (20.5 versus 5.5 minutes, P = .002). For hub door–to-device, DALVO-All improved 30.3% (160.0 versus 111.5 minutes, P = .035), and BEMI-All improved 18.6% (59 versus 48 minutes, P = .039). For hub door–to-recanalization, DALVO-All improved 25.9% (162 versus 120 minutes, P = .02) and BEMI-All improved 17.1% (70 versus 58 minutes, P = .042). The remaining results are noted in the Online Supplemental Data. As an additional measure of outcomes, we added the percentage of thrombectomy cases meeting specific targets. Using 90 minutes (for DALVO) and 60 minutes (for BEMI) as targets for the door-to-groin or door-to-device, we noted significance for door-to-groin DALVO-OffHours (0% versus 40%, P = .049), DALVO-ALL (17.65% versus 66.67%, P = .0091), and Overall (63.83% versus 85.71%, P = .028) favoring the implementation, but we only noted significance for similarly timed door-to-device targets for the BEMI-OffHours group (43.75% versus 80%, P = .044).
As a quantifiable measure of whether the new communication strategy was improved, we analyzed the text-messaging thread count totals for all patients who underwent embolectomy in the post-go-live Viz.ai period (Online Supplemental Data). Comparing the text-messaging thread counts from the first 3 months of the pilot with the second 3 months of the pilot, we noted no difference, but comparing the first 3 months of the pilot with the most recent 3 months when we used the communications platform, we noted a statistically significant 30% improvement in text-messaging thread counts per case (38.6 versus 27.2, P = .04). No differences were noted for DALVO or BEMI subgroup comparisons.
DISCUSSION
Our comprehensive stroke center is well-versed in providing time-sensitive decision-making and striving toward optimal treatment time windows for both rtPA and thrombectomy. Published protocols have shown that process/time improvements can correlate with LVO recanalization or good outcome.12-16 We sought a solution that allowed access to advanced CT perfusion mapping and immediate/mobile access to a HIPAA-compliant communications platform for coordination between all care team members to improve our time metrics further. Because there are no definitive data noting whether one algorithm/perfusion map technique is superior to another, assessing for which platform had a more optimal algorithm/ perfusion map technique did not guide a change to the Viz.ai platform.23 Determining differences between perfusion maps and additional imaging tools was beyond the scope of this project. Our aims were solely focused on improving access to imaging and improving communication strategies to afford improved time metrics for thrombectomy cases.
Our DALVO and BEMI pathways begin with the stroke provider evaluating the patient (either in person or via telestroke) for thrombectomy consideration. Images are sent to our advanced imaging tool where CTs and CTAs are reviewed. For the patients with LVO in the 6- to 24-hour window, the perfusion algorithm provides mismatch data for review. Before this pilot, if the patient was a potential thrombectomy candidate, the stroke provider would contact numerous providers via pager, Secure Chat message, cell phone, or encrypted text message. For each team, the stroke provider needed to investigate who was on call and determine that provider’s preferred contact method. The first contact would usually be the neurointerventional provider on-call (to discuss whether the patient was a potential thrombectomy candidate), followed by the Neurocritical Care Unit attending physician and fellow, transfer center, house supervisor, nursing, neuroradiology, stroke team members, and registration teams. At each point, details of the case were discussed, resulting in redundancy and persons not all having the same, most up-to-date information. Most of the time, discussions occurred via telephone contact or alphanumeric texting on pagers forwarded to cellphones. Sometimes text message threads were used (encryption was encouraged to protected health information), depending on individual processes. As noted in Fig 1, left, numerous providers were added at different points in the conversation, and information required repetition throughout the course of the discussion. Because providers may have been communicating via phone, pager, or messaging systems, it was not uncommon for individuals to be left out, it was frequent to not be certain who was the right on-call person, and it was inevitable that some individuals had different information from others as a result of using various noncentralized systems.
On January 18, 2021, our program began using the Via.ai tool. The advanced imaging viewer allowed hand-held smartphone device access to the CT, CTA, and CTP perfusion maps and the ability to review and rotate images using a 3D tool. The embedded communication tool also allowed more coordinated and centralized review regarding treatment decisions, transfer needs, patient status, management, and destination concerns.
Our pilot results noted a robust improvement in door-to-groin, door-to-device, and door-to-recanalization times for many of the groups assessed. Historically, our largest concern was for the DALVO cases because the time from the first interaction until the patient reaches the angiosuite is far more compressed. The telemedicine BEMI cases afford more lead time for angiography teams to arrive at the hub center before the patient arrives. Expectations were that if a large difference was noted, it would be most easily found in DALVO cases at off-hours when the angiography team was not in house and mobilization was required to arrive at the hub. Our results showed a 39% reduction in door-to-groin times for these DALVO OffHours cases. Our interpretation is that the rapid imaging access by relevant teams and coordinated communications among all resulted in quicker decision-to-treat and decision-to-activate the angiography team. Prior analyses reported that there is often significant delay in thrombectomy related to in-hospital time delays, with the greatest delays occurring during the imaging “picture-suite” time windows, which is improved by more parallel processing.24 Our results showed similar door-to-groin time improvements.
In many respects, telemedicine transfers benefit from prehospital notification. Prehospital notification of stroke reduces in-hospital delay because it allows earlier activation of the stroke, imaging, and potentially angiography teams.25,26 As is also noted in our results, this reduction should result in decreased door-to-groin times for BEMI compared with DALVO cases. We did not expect to find significant pre- versus post time differences within the transfer population itself. In our analysis, BEMI telemedicine transfer cases also showed a significant 33% door-to-groin time improvement. Given the small subgroup sizes and smaller effect size seen, we did not show differences in BEMI subgroup analyses based on OnHours or OffHours, and the absolute minutes saved were noted to be less than in DALVO cases (13.5 compared with 41 minutes). This finding was to be expected because the teams had ample opportunity to mobilize ahead of time, resulting in quicker door-to-groin times in BEMI than in DALVO. Overall, a 33% difference in door-to-groin times was still noted in these BEMI transfer cases, resulting in a significant time improvement for these transfers. Door-to-device and door-to-recanalization times showed similar results, lending support to our findings not being due to chance.
Experientially, our teams noted a substantial improvement in communications during this pilot. Stroke providers did not need to access on-call schedules or look up phone numbers to relay time-sensitive information to different services. Just as important, providers did not lose time re-explaining, re-paging, or re-texting information. We were unable to find fewer text-message thread counts comparing the first half of the implementation period with the second half of the implementation period. Reasons may include a small sample size (n = 35) with some comparison groups being as small as 2 samples or because no difference exists. We were unable to compare prepilot text-message thread counts because no standard communication pathways then existed. Providers may have used various systems to communicate. Although it is assumed that absolute numbers of messages transmitted would have been higher in the pre-implementation period, we could only compare early-to-late deployment periods. The final reason may be related to the quality of data transmitted. The ease of communication (with simplified access to all parties) may have been countered by a lower threshold to simply send more messages but of shorter length each. Assessing character counts was beyond the scope of this pilot.
When we assessed a longer experience with the communications platform, that comparison showed 30% fewer text messages being sent per case. This finding is a quantitative surrogate for significantly improved communications. Although this shows improved communications because data were not adjusted for many potentially confounding variables (patients in different time windows, rtPA versus no rtPA, patients who could consent versus requiring surrogate contact and so forth), we think that a longer experience with the platform would help balance any potential variability. However, the noted 30% improvement in text-message thread counts is both clinically and statistically significant. Providers qualitatively report that the ability to access and use a single, secure platform in which all parties on-call can view a real-time, accurate, and longitudinal message string detailing critical patient-related information has improved the provider experience. Because this was a Quality Improvement project, specific provider surveys assessing satisfaction were not instituted. Adjusting for the above variables was beyond the scope of this Quality Improvement project.
This article has some limitations owing to its Quality Improvement design, small sample, and limited scope. Because this project focused only on thrombectomy time metrics, additional research questions could not be included and questions regarding functional outcome metrics could not be addressed. Similarly, the nonrandomized, real-world, pre/post design makes it difficult to prove that the significantly improved time metrics were not the result of other interventions deployed clinically, though we had not implemented any new stroke regimen focused on thrombectomy improvement during this time period. No neurointerventional-specific changes were implemented during this time period, and the small pilot period during which other interventions could have been added make this less likely though not impossible. Concern that improvement was due to more rapid transfers due to our BEMI transfer protocol is unlikely because our BEMI protocol has been unchanged for 6 years.17
Because this project was limited to data already being collected, we were unable to assess provider satisfaction via survey (for qualitative or quantitative improvement in communication) or assess discharge disposition or 90-day outcome (to assess whether the significant time improvement translated to functional outcome). Given the inability to separate our critical variables that resulted in this real-world time improvement, we are unable to determine whether the immediate/mobile access to advanced imaging CT perfusion maps, the advanced ability to rotate images in 3D space for better/quicker image review by stroke or neurointerventional provider, or the streamlined communications portal individually accounted for our time improvement. In all likelihood, it was a combination of the 3, resulting in quicker decision-making because of more streamlined access to advanced imaging and more streamlined communications.
Before our transition to Viz.ai, we used the clinical version of RAPID (not the research version) with an automatic push of results to e-mail on desktop or phone (and some providers had automatic push to a smartphone app as well), but it did not yet have a centralized communication pathway or messaging other than via e-mail notification. Other publications have shown a similar impact of RapidAI (https://www.rapidai.com/) on treatment times in patients with LVO.27 Thus, we cannot determine whether the benefits found were due to the communication platform, the particular method of image viewing, the advanced imaging algorithms, or a combination of the above. The absence of and then implementation of an integrated communications platform may have itself contributed some to our improved communications and improved time metrics. The use of text message count as a surrogate for streamlined communication may not reflect improved communication because more messaging may reflect either better or worse communication depending on the context and content. These software platforms also include numerous alerts making “alert fatigue” a possible concern. Providers can disable or limit the alerts at their discretion. Additional service groups are being added to the platform even a year after deployment, and total user count increasing not decreasing supports the stability and sustainability of the use of the product at our centers. Finally, whether there is sustainability with time or whether this improvement period was only during the initial postimplementation period will be important to investigate.
CONCLUSIONS
Overall, the Viz.ai platform has been shown to benefit both DALVO and BEMI patients at our comprehensive stroke center for door-to-groin, door-to-device, and door-to-recanalization for many of the groups assessed. In the greatest opportunity subset (DALVO-OffHours: direct-arriving patients requiring team mobilization off-hours), we noted a 39% improvement in door-to-groin times. For telemedicine transfer patients, we also noted a 32.5% improvement in the BEMI-All transfer group times. These improved times are likely due to immediate/mobile access to advanced imaging, the advanced CT perfusion mapping to help guide quick neurointerventional decision-making, and a HIPAA-compliant communications platform allowing a coordinated, single-location, secure text-messaging thread for all care team members to access and be aware of patient status, decision information, and patient destination/location. These results support the assertion that quicker decision-making results in more rapid team activation and improved neurointerventional time metrics. Quality Improvement initiatives aimed at improving all time windows from symptom recognition to recanalization should continue to be encouraged.12-16 These results could be a model for other centers that may not already have a robust system in place for DALVO and BEMI cases. Further analysis in a larger data set and assessing sustainability is ongoing.
Ethics Approval
This project was approved by the University of California San Diego institutional review board as a Quality Improvement Initiative.
Acknowledgments
The authors acknowledge Ms Stephanie Rubenstein for her assistance. We would also like to thank the University of California, San Diego Health Enterprise, and the Department of Radiology for supporting operational initiatives designed to improve access to advanced imaging tools to improve patient care.
ABBREVIATIONS:
- BEMI
Brain Emergency Management Initiative telemedicine transfer LVO
- DALVO
direct arriving LVO
- HIPAA
Health Insurance Portability and Accountability Act
- LVO
large-vessel occlusion
Footnotes
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org.
References
- 1.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581–87 10.1056/NEJM199512143332401 [DOI] [PubMed] [Google Scholar]
- 2.Fransen PS, Beumer D, Berkhemer OA, et al. ; MR CLEAN Investigators. MR CLEAN, a multicenter randomized clinical trial of endovascular treatment for acute ischemic stroke in the Netherlands: study protocol for a randomized controlled trial. Trials 2014;15:343 10.1186/1745-6215-15-343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powers WJ, Rabinstein AA, Ackerson T, et al. ; American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2018;49:e46–110 10.1161/STR.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 4.Albers GW, Marks MP, Kemp S, et al. ; DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708–18 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nogueira RG, Jadhav AP, Haussen DC, et al. ; DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11–21 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 6.Saver JL, Goyal M, van der Lugt A, et al. ; HERMES Collaborators. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 2016;316:1279–88 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 7.Target: Stroke Phase III. Introducing Target: Stroke Phase III. https://www.heart.org/en/professional/quality-improvement/target-stroke/introducing-target-stroke-phase-iii. Accessed October 6, 2022
- 8.Grotta JC. tPA for stroke: important progress in achieving faster treatment. JAMA 2014;311:1615–17 10.1001/jama.2014.3322 [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Zhao X, Smith EE, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 2014;311:1632–40 10.1001/jama.2014.3203 [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Rivera V, Salazar-Marioni S, Abdelkhaleq R, et al. Integrated stroke system model expands availability of endovascular therapy while maintaining quality outcomes. Stroke 2021;52:1022–29 10.1161/STROKEAHA.120.032710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyal M, Menon BK, van Zwam WH, et al. ; HERMES Collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 12.Kim SC, Lee CY, Kim CH, et al. The effectiveness of systemic and endovascular intra-arterial thrombectomy protocol for decreasing door-to-recanalization time duration. J Cerebrovasc Endovasc Neurosurg 2022;24:24–35 10.7461/jcen.2021.E2021.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aghaebrahim A, Streib C, Rangaraju S, et al. Streamlining door to recanalization processes in endovascular stroke therapy. J Neurointerv Surg 2017;9:340–45 10.1136/neurintsurg-2016-012324 [DOI] [PubMed] [Google Scholar]
- 14.Frei D, McGraw C, McCarthy K, et al. A standardized neurointerventional thrombectomy protocol leads to faster recanalization times. J Neurointerv Surg 2017;9:1035–40 10.1136/neurintsurg-2016-012716 [DOI] [PubMed] [Google Scholar]
- 15.Panezai S, Meghpara S, Kulhari A, et al. Institution of Code Neurointervention and its impact on reaction and treatment times. J Vasc Interv Neurol 2020;11:1–5 [PMC free article] [PubMed] [Google Scholar]
- 16.Jahan R, Saver JL, Schwamm LH, et al. Association between time to treatment with endovascular reperfusion therapy and outcomes in patients with acute ischemic stroke treated in clinical practice. JAMA 2019;322:252–63 10.1001/jama.2019.8286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Modir R, Meyer D, Hamidy M, et al. Brain emergency management initiative for optimizing Hub-Helicopter Emergency Medical Systems-Spoke Transfer Networks. Air Med J 2020;39:103–06 10.1016/j.amj.2019.10.003 [DOI] [PubMed] [Google Scholar]
- 18.Mendez B, Requena M, Aires A, et al. Direct transfer to angio-suite to reduce workflow times and increase favorable clinical outcome. Stroke 2018;49:2723–27 10.1161/STROKEAHA.118.021989 [DOI] [PubMed] [Google Scholar]
- 19.Meyer BC, Raman R, Hemmen T, et al. Efficacy of site-independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol 2008;7:787–95 10.1016/S1474-4422(08)70171-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goyal M, Jadhav AP, Bonafe A, et al. ; SWIFT PRIME Investigators. Analysis of workflow and time to treatment and the effects on outcome in endovascular treatment of acute ischemic stroke: results from the SWIFT PRIME randomized controlled trial. Radiology 2016;279:888–97 10.1148/radiol.2016160204 [DOI] [PubMed] [Google Scholar]
- 21.Gache K, Leleu H, Nitenberg G, et al. Main barriers to effective implementation of stroke care pathways in France: a qualitative study. BMC Health Serv Res 2014;14:95 10.1186/1472-6963-14-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kidwell CS, Jahan R, Gornbein J, et al. ; MR RESCUE Investigators. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013;368:914–23 10.1056/NEJMoa1212793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray NM, Unberath M, Hager GD, et al. Artificial intelligence to diagnose ischemic stroke and identify large vessel occlusions: a systematic review. J Neurointerv Surg 2020;12:156–64 10.1136/neurintsurg-2019-015135 [DOI] [PubMed] [Google Scholar]
- 24.Mehta BP, Leslie-Mazwi TM, Chandra RV, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc 2014;3:e000963 10.1161/JAHA.114.000963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes 2012;5:514–22 10.1161/CIRCOUTCOMES.112.965210 [DOI] [PubMed] [Google Scholar]
- 26.Patel MD, Rose KM, O’Brien EC, et al. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborative. Stroke 2011;42:2263–68 10.1161/STROKEAHA.110.605857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Kawaz M, Primiani C, Urrutia V, et al. Impact of RapidAI mobile application on treatment times in patients with large vessel occlusion. J Neurointerv Surg 2022;14:233–36 10.1136/neurintsurg-2021-017365 [DOI] [PubMed] [Google Scholar]