Abstract
Background
Attempts have been made to reduce excessive laboratory test ordering; however, the problem persists and barriers to physician involvement in quality improvement (QI) remain. We sought to understand physician participation experience following a laboratory test overuse initiative supported by a QI coalition.
Methods
As part of a larger mixed-methods study, structured virtual interviews were conducted with 12 physicians. The Theoretical Domains Framework (TDF) and the Behavioural Change Wheel (BCW) were used to identify characteristics that influence physician behaviour change for QI leadership and participation and appropriate blood urea nitrogen (BUN) test ordering. A content analysis of physicians’ statements to the TDF was performed, resulting in overarching themes; relevant TDF domains were mapped to the intervention functions of the BCW.
Results
Nine overarching themes emerged from the data. Eight of 14 TDF domains influence QI leadership and participation, and 10 influence appropriate BUN-test ordering behaviours. The characteristics participants described that promoted a change in their QI participation, leadership and appropriate BUN-test ordering were: QI education with hands-on training; physician peer mentorship/support; personnel assistance (QI and analytics) and communication from a trusted/credible physician leader who shares data and insights about the physician role in the initiative, clinical best practice and past project success. Other elements included: a simply designed initiative requiring minimal effort and no clinical workflow disruptions; revised order forms/panels and limiting test-order frequency when laboratory tests are normal. Additionally, various future intervention strategies were identified. For their initial initiative participation, physicians acknowledged coalition leader or member credibility was more important than awareness of the coalition.
Conclusions
Based on physicians’ described perceptions and experiences, coalition characteristics that influenced their QI leadership and participation, and appropriate BUN-test ordering behaviours were revealed; these characteristics aligned to several TDF domains. The findings suggest that these behaviours are multidimensional, requiring a multistrategy approach to change behaviour.
Keywords: healthcare quality improvement, qualitative research, health behavior, leadership
WHAT IS ALREADY KNOWN ON THIS TOPIC
Understanding the behavioural characteristics that influence physician diagnostic test ordering is critical for designing deimplementation interventions that could lead to successful clinical practice change.
WHAT THIS STUDY ADDS
Physician quality improvement (QI) experience and perception of coalition characteristics and interventions that promote QI involvement and a behaviour practice change to reduce excess blood urea nitrogen test ordering, which could be transferable to other forms of testing.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The findings can be used to inform the design of future physician-led QI initiatives about excessive test ordering and strategies to reduce barriers to physician-QI participation and leadership.
Introduction
Laboratory test ordering has been acknowledged as an area where quality improvement (QI) is needed, with recent initiatives focusing on reducing healthcare system costs or improving patient experience and outcomes.1 2 Nevertheless, overuse of laboratory testing persists during hospitalisation, suggesting complex barriers. Additionally, there has been a lack of physician QI leadership and participation, which was found to impact their interest and priority to reduce laboratory testing.3 There is little published evidence about the perceptions of physicians regarding their role and involvement in QI.4
Physician-QI leadership is defined ‘as the active/willing participation of physicians in QI projects that develop a strategic partnership with healthcare operations to improve healthcare delivery, pg6’.5 Reducing laboratory test ordering requires a change in physician behaviour to participate in and lead the initiative; this approach may have broader influence on their colleagues’ ordering practice.6 In 2012, the Choosing Wisely (CW) campaign launched in the USA, aimed to reducing unnecessary tests and treatments in healthcare, has spread to over 20 countries, including Canada.7 In Canada, over 70 medical specialty societies have developed more than 350 recommendations to support conversations about appropriate and necessary treatment. However, ‘recommendations alone will not change practice’, pg4108 and CW suggests incorporating behavioural science tools, such as the Theoretical Domains Framework (TDF), to support interventions aligned with CW recommendations.8
Members of a university Department of Medicine (DoM), in Edmonton, Alberta, Canada, identified healthcare system transformation required physician QI education, engagement and leadership and patient-centred care.9 In 2015, a physician-led coalition—the Strategic Clinical Improvement Committee was developed, uniting the priorities of the DoM and the health zone medicine programme.10 The coalition included 15 DoM physicians from various medicine divisions, six executive directors from the six local hospital medicine programmes, a patient advisor, and a QI consultant. A coalition is the joining of people and organisations, and often involves existing leaders working in strategic pragmatic partnerships to influence outcomes on a particular problem.11 12 The coalition’s aim is to strengthen physician QI capability and involvement in improvement projects; collaboration between hospital medicine programmes and improve patient outcomes and experience.
In 2018, in an internal organisation laboratory test utilisation report, high (>500 tests per month) blood urea nitrogen (BUN) ordering was identified in hospitals, in four health zones (Edmonton, Central, South and North) in Alberta [unpublished]. One coalition QI priority became laboratory test overuse, specifically BUN. Members of the coalition were aware reducing BUN ordering in the hospital setting would require a change in physician behaviour, leadership in the improvement effort and influencing physician colleagues to change their ordering practice.
The research presented herein represents the qualitative phase of a sequential explanatory mixed-methods study. The purpose of this study phase was to gather physician-QI experience to identify the characteristics they perceived as influencing their QI participation (initiative involvement), leadership (champion/lead the initiative) and their reduction in excessive (support appropriate) BUN ordering.
Methodology and methods
Theoretical frameworks
The TDF is a validated behavioural framework based on 128 constructs from 33 psychological theories and consists of 14 domains13: knowledge; skills; beliefs about consequences; beliefs about capabilities; optimism; social/professional role and identity; intention; goals; memory, attention and decision processes; environmental context and resources; social influences; emotion; behavioural regulation and reinforcement.14 15 The TDF expands on the capability, opportunity and motivation conditions of the Behavioural Change Wheel (BCW) known as the COM-B system.13–16 Researchers investigating physician laboratory test ordering in different settings have applied the TDF to understand the determinants of behaviour ‘mechanisms for action/change’ and to identify potential behaviour change interventions.17–19
Study design, team and ethics
A qualitative design incorporating one-to-one structured virtual interviews with physicians in four health zones in Alberta, Canada, was completed after the implementation of a provincial QI initiative to reduce excessive BUN-test ordering. The TDF provided a theoretical perspective for the research findings to be collected, analysed and interpreted.16
The study team comprised of researchers (PM, JM, KS, LD and SM), and a practicing internist (NK). Researcher (PM), the coalition’s QI-consultant provided project management support for the dissemination of the initiative across Alberta and QI guidance to the initiative physician leads. Participants had awareness of and a past relationship with PM in her QI-consultant role.
Patient and public involvement
No patient or public involvement in this study.
Setting
From 2017 to 2019, coalition physician members with or without a multidisciplinary (nurse, unit clerk and medical learners) team at four different hospitals in Edmonton, Alberta, completed QI projects about laboratory test overuse. Aimed at identifying key intervention components to reduce daily laboratory test ordering and BUN testing, a coalition-supported, physician-led multicomponent laboratory test ordering overuse initiative was developed.20 The success of these projects in reducing BUN ordering in hospital medicine units21 led to the December 2019 approval of a provincial initiative to reduce BUN ordering in hospital medicine units and emergency departments, with plans to continue in one Edmonton-health zone hospital and expand to three hospitals in Alberta’s Central, South and North health zones.
The COVID-19 pandemic delayed the spread of the provincial initiative. With frequent hospital disruptions (ie, staff and unit changes, etc), the multicomponent intervention was abridged to one educational presentation (1 hour), the sharing of programme-specific BUN-test data, and the physician lead informally encouraging colleagues. Medicine and emergency physician teams in the four participating hospitals received the educational presentation from either the coalition physician leader, or member, and/or a zone physician leader (not directly aligned with the coalition).
Participants and recruitment
Thirteen hospital medicine and emergency physicians from the four health zones were eligible to participate. Purposively sampled physicians were those who either led or supported a lead physician in the initiative. Researcher (SM) sent 13 individual study invitation emails to each participant’s organisation email address. Participants who responded to the invitation were sent information explaining the study, including consent forms prior to scheduling a 60 min interview. Participants were assigned a study identification number ensuring anonymity.
Data collection
A structured interview guide that included one section for physician general characteristics and another for topic-related open-ended questions aligned to the TDF was developed (online supplemental file A). A physician (dermatologist) researcher reviewed the interview guide; minor word and sentence structure modifications were made to improve question clarity. At a minimum of 3 months postinitiative implementation, PM conducted audio-recorded one-to-one structured interviews via Zoom using Otter Voice Notes and the Zoom recording feature (no video was recorded). At the start of each interview, study information was reviewed, and consent was reaffirmed verbally. Twelve physicians were interviewed over a 6-month period (February to July 2021); study identification-numbered audio recordings resulted.
bmjoq-2022-001965supp001.pdf (218.1KB, pdf)
SM transcribed the recordings verbatim, generating study identification-numbered transcripts. PM independently reviewed all audio recordings to ensure accuracy of the transcripts and JM independently reviewed all final transcripts. Post-transcript development, the audio files were discarded, and transcripts were stored for data protection. SM emailed the transcripts to each participant for review and no participant requested changes or additions.
Data analysis
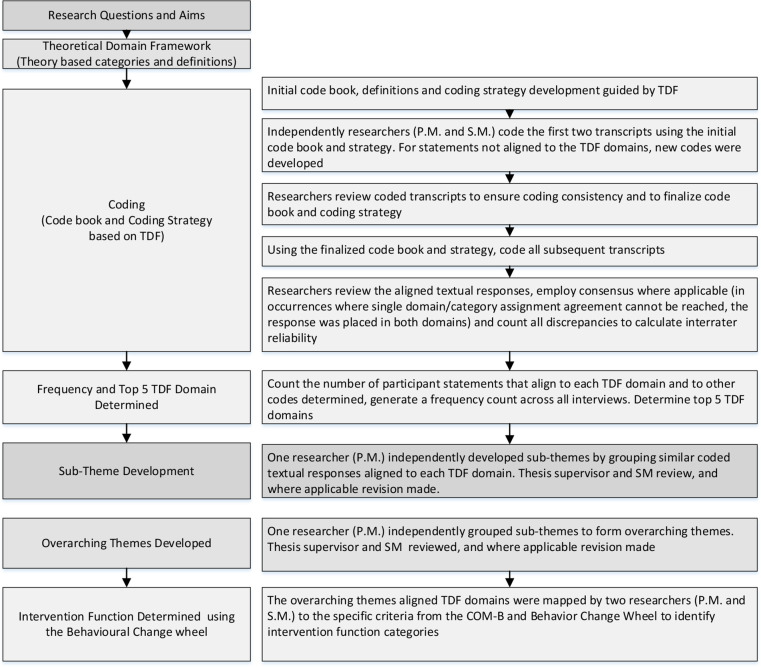
Data analysis occurred concurrently with data collection. A deductive-directed content analysis approach was applied to analyse and interpret the findings.13 14 22 The TDF domains provided the codes, relationships among the codes, and code definitions were used by Cane et al for codebook development.13 22 Data analysis occurred in five steps (figure 1). First, PM and SM independently completed domain coding (ie, selecting segments or passages from the transcript that matched a relevant TDF domain) using NVivo V.12.2. To ensure coding consistency, they reviewed the first two transcripts together; coding discrepancies were addressed using consensus. Relevant data not aligned to the TDF were reviewed and resulted in the addition of three new codes (ie, COVID-19, Connect Care and Unaware of Coalition) that were added to the final codebook confirmed by JM. Subsequently, all transcripts were independently coded by PM and SM, coding discrepancies were resolved using consensus. To determine coding congruence, the interrater reliability coefficient was calculated.23 Second, TDF domains with the highest number of coded phrases were counted.
Figure 1.
Qualitative Study Phase Coding Strategy Diagram. COM-B, Capability, Opportunity, Motivation Behavioural System; TDF, Theoretical Domains Framework.Note. This figure depicts the process used to code, theme, and determine intervention functions.
In steps 3 and 4, PM inductively organised the coded textual statements into domain-specific themes, which were then organised to generate overarching themes.24 25 Two researchers (SM and JM) independently confirmed all themes. Finally, to identify intervention functions influencing behaviours under review, PM and SM mapped the relevant TDF domains aligned to each overarching theme to the COM-B behaviour change model and the BCW.26 Researcher (JM) confirmed the aligned intervention functions.
Rigour
A theory-informed structured approach was employed,13–16 with open-ended, structured interview questions aligned to the TDF, allowing participants to share candidly. Reducing the potential for coercion, correspondence was through SM who was not known to the participants. Creditability was established using the following strategies: a study identification-linking document was developed and accessible to SM only; two researchers independently completed data coding, with a third confirming all findings; PM and SM documented reflective notes clarifying assumptions as part of the coding process; participants were provided the verbatim transcripts for data accuracy; and a detailed research process with raw data (quotes) provide the findings to evaluate and assess transferability.27 The Consolidated Criteria for Reporting Qualitative Research guidelines were followed.28
Results
Participants
Twelve participants were interviewed for 30–35 min; 10 were medicine (urban n=5; rural n=5) and two were emergency physicians (urban n=1; rural n=1) from four health zones in Alberta. Ten participants led the initiative, and two supported a physician colleague’s involvement. Participants were familiar with laboratory test excessive ordering in the hospital setting (n=10) and had awareness of the coalition (n=9). Over half of the participants (n=7) had greater than 10 years of clinical experience and eight reported having less than 10 years of formal administrative/leadership experience. Participants rated their QI knowledge (n=7) and leadership (n=9) as beginner, however, individuals (n=9) noted that the coalition was supportive of QI knowledge development and application. Four reported a positive change in QI knowledge, application or leadership postinitiative involvement. Participants (n=11) reported that they would participate in a QI-initiative supported by the coalition in the future (table 1).
Table 1.
Participant characteristics (n=12)
| Characteristic | Participants (n=12) |
| Hospital geographical region: | |
| Rural (<1 00 000 population) | 6 |
| Urban (>5 00 000 population) | 6 |
| Project physician champion (led the project) | 10 |
| Project physician supporter (supported a physician champion) | 2 |
| Years of clinical experience: | |
| Greater than 10 years | 7 |
| Years of formal administrative or leadership experience: | |
| Less than 10 years | 8 |
| Familiarity of coalition: | |
| Familiar | 9 |
| Familiarity of lab test ordering overuse and BUN test overuse: | |
| Familiar | 10 |
| Pre-project QI knowledge and application: | |
| Beginner | 6 |
| Pre-project QI leadership experience: | |
| Beginner | 9 |
| Coalition supported QI knowledge and application: | |
| Agree | 9 |
| Post-project change in QI knowledge and application or QI leadership: | |
| Improvement | 4 |
| Would you participate in a QI project supported by the coalition in the future? | |
| Yes response | 11 |
| Not applicable response | 1 |
BUN, blood urea nitrogen; QI, quality improvement.
Top five TDF domains
Coding congruence across all interviews and domains had substantial agreement (κ=0.74),23 809 statements from the 12 interviews were coded into 13 TDF domains. Count of the coded TDF domains (>50 coded phrases) determined that the top five domains were social influences; environmental contexts and resources; knowledge; social/professional role and identity and beliefs about capabilities (table 2). No coded data were aligned to the TDF domain memory.
Table 2.
Count of the coded statements, domain-specific themes per TDF domain and participants
| TDF domains | Number of coded statements | Number of domain specific themes per TDF domain | Number of participants (n=12) | |
| 1 | Social influences | 163 | 7 | 12 |
| 2 | Environmental context and resources | 137 | 6 | 11 |
| 3 | Knowledge | 113 | 4 | 11 |
| 4 | Social professional role and identity | 92 | 4 | 12 |
| 5 | Beliefs about capabilities | 56 | 3 | 11 |
| 6 | Goals | 43 | 1 | 8 |
| 7 | Behavioural regulation | 38 | 3 | 9 |
| 8 | Beliefs about consequences | 31 | 3 | 10 |
| 9 | Optimism | 31 | 1 | 11 |
| 10 | Reinforcement | 27 | 1 | 8 |
| 11 | Skills | 22 | 1 | 6 |
| 12 | Intentions | 18 | 1 | 8 |
| 13 | Emotion | 9 | 2 | 5 |
| 14 | Memory | 0 | 0 | 0 |
TDF, Theoretical Domains Framework.
Themes and relevant TDF domains
Thirty-seven TDF domain-specific themes were generated (table 3); these themes are interconnected and were then grouped to form nine overarching themes (online supplemental file B). From these overarching themes, four themes align to the appropriate BUN-test ordering behaviour: (1) trusted local physician leader communicating about QI encourages participation; (2) provide QI-initiative plan/approach, data and physician role (3) order BUN tests mindfully not reflexively or habitually and (4) changing physician behaviour is difficult. Based on these themes, 10 relevant TDF domains were identified: knowledge; beliefs about consequences; beliefs about capabilities; social influences; social/professional role and identity; environmental context and resources, goals; intentions; behavioural regulation and optimism.
Table 3.
TDF domains, domain-specific themes and example quotes
| TDF domains | Domain-specific themes | Examples of interview quotes |
| Social influences | 1.Physician QI mentorship 2.Coalition (SCIC) provides a forum for QI collaboration 3.’Put a physician leader face’ on the LTOO project 4.Coalition physician members spreading and championing the QI project 5.QI recognition 6.QI sharing (social comparison) to encourage QI 7.Urea lab test ordering physician conformity |
‘The biggest bang for the buck is mentorship’ (P9) ‘Integrate physicians into the QI frameworks and organization’ (P2) ‘Led by a trusted, high quality physician, who I know is going to lead the project’ (P11) ‘It is nice that it’s from a physician leader perspective, who shares the QI issues and how they solved it’ (P6) ‘Physician-led projects adds value… in the eyes of other physicians’ (P2) ‘I think having a proof of concept showed in the presentation is excellent because…they did this, okay we can do this here’ (P11) ‘Physicians are educating their learners about the urea test change and why’ (P2) |
| Environmental context and resources | 8.Hospital culture differs 9.Minimal physician project effort, straightforward intervention with minimal workflow impact 10.Provide continual access to experienced support personnel to assist physician-led QI 11.Physician staffing challenges 12.COVID-19/pandemic reduced physician time to champion any additional tasks such as QI 13.Connect Care-IT system rollout/ implementation is a competing priority that reduces physician time to participate in QI activities |
‘Implementation of things that worked in another site may not necessarily work at a different site’ (P7) ‘Change component to the work flow was very minimal, didn’t create a bunch of extra time for physicians’ (P1) ‘It’s the person to assist to get it done, the sharing of abilities and expertise, it’s awesome’ (P10) ‘Chronically understaffed, don’t have physician coverage’ (P7) ‘Expanding the project has been challenging as everyone is extremely tasked with managing patients’ (P3) ‘Now physicians are like, how do I get through my 12-hour shift with a completely new EMR’ (P7) |
| Knowledge | 14.Coalition provided QI education and training encourages physician-led QI 15.LTOO project provides a hands-on QI opportunity 16.‘It is a think tank where physicians can discuss QI topics’ 17.Coalition presentation improved LTOO awareness (utilisation and cost data) |
‘Provided QI workshop with the methodology and the science of improvement that was helpful’ (P3) ‘Just knowing how to be involved with the QI project’ (P8) ‘Bring a problem to the table and brainstorm ways to address’ (P7) ‘Made reasonable sense, seemed logical and well laid out during the presentation’ (P8) and ‘Given numbers to something that we’ve suspected and known’ (P12) |
| Social professional role and identity | 18.Shepherd (chaperone) physician QI leadership role and provide opportunity to lead 19.Physician champion does not view themselves as leading the LTOO project 20.LTOO project aligned to health organisation priorities with support from medical and organisational leaders 21.Competing demands—‘Juggling clinical demands’ |
‘In the past we were asked to participate, today, we are asked to lead’ (P2) and ‘Shepherd physician-led QI projects’ (P10) ‘Knowing somebody else was running it was great’ (P1) and ‘Co-leadership role’ (P10) ‘Project was recognized as a strategic priority provided more credence to the work, it was Choosing Wisely funded also showed that there was professional and organizational priority’ (P5) ‘Physicians don’t have the time to seek the knowledge of QI, also carry out a project when you’re on busy clinical service’ (P2) |
| Beliefs about capabilities | 22.QI is a new skillset for physicians which impacts confidence 23.Lab test ordering is a learnt and ingrained practice 24.Simple Intervention increased confidence to lead QI implementation |
‘I feel very beginner and newbie in terms of QI, its foreign and isn’t a concept that is well ingrained’ (P1) ‘It’s an ingrained [learnt), auto practice; the more physicians are in practice and develop a routine and almost a habit’ (P1) ‘It wasn’t taxing for me, supported my participation’ (P12) and ‘Time commitment for me was little’ (P1) |
| Beliefs about consequences | 25.Anticipated positive intervention implementation effect (reduced urea ordering) 26.Perceived threat to physician choice and freedom—‘being told what to do’” 27.Physician-led QI was competed out |
‘Pretty clean; everyone sees it as a pretty good idea’ (P10) ‘Creates that ivory tower sort of feeling, when you’re just being told what to do …don’t want things imposed on them’ (P7) ‘There is not an appetite for [QI] right now’ (P7) |
| Behavioural regulation | 28.Transition from reflexive/ habitual ordering to mindful (evidence-based, patient required) ordering 29.Sustain physician order behaviour change through data reflection and integration in medical learner curriculum 30.ConnectCare (IT system) standardises the lab order sets and the urea blood test has been removed |
‘I now think about it instead of automatically just running down the list’ (P1) ‘Support ongoing reflection and data collection’ (P1) and ‘Education will need to become integrated into learner curriculum’ (P2) ‘The most effective thing is really just changing the form’ (P3) and ‘Removing choice (urea blood test) from paper and IT order forms’ (P1) |
| Emotion | 31.QI project experience was positive, targeted a grassroots annoying problem, with minimal physician QI effort, motivating physician participation 32.Physicians emotional well-being is impacting their ability to engage in QI |
‘This has been a positive experience’ (P1) and ‘The thoughts and feeling with the project were more that it was grassroots on the ward’ (P6) ‘Trying to provide knowledge or practice change to a group of people who are sort of overworked, trying to sort of balance and survive in their existence’ (P7) |
| Goals | 33.Project goals and benefits were clear and that lab ordering is a patient safety and financial issue | ‘Anyone can understand the goals and for that reason, I think that helped this QI project get traction’ (P11), and ‘Seeing how much we spend in urea blood testing is alarming’ (P6) |
| Skills | 34.Past hands-on QI training and involvement encourages future physician QI involvement | ‘I think having had some formal knowledge of QI processes [helped)’ (P3) |
| Intentions | 35.Meet physicians where they are at with a change idea/concept, share the why to motivate grassroots physicians to improve order behaviour | ‘I think the most importantly, was having a really strong evidence of the ‘Why’.’ (P1) |
| Optimism | 36.Pessimistic—‘Tough to change physician behaviour’ | ‘Have to drag along the rest of the group’ (P10) and ‘I think the barrier would be in general physician behaviour’ (P8) |
| Reinforcement | 37.No incentives for physician QI involvement (funding/grants and remuneration) | ‘You’re never going to get anyone to do anything if they are not remunerated’ (P7) ‘We don’t get paid any extra income for doing QI’ (P12) |
LTOO, Laboratory Test Ordering Overuse; QI, quality improvement; SCIC, Strategic Clinical Improvement Committee; TDF, Theoretical Domains Framework.
bmjoq-2022-001965supp002.pdf (157.5KB, pdf)
Five overarching themes aligned to QI leadership and participation behaviour: (5) QI education and hands-on opportunities support involvement; (6) physician mentorship; (7) coalition functions as a safe peer-to-peer QI community; (8) opportunity to lead, with support, a straightforward QI intervention that requires minimal effort and (9) physician QI involvement competed out. From these themes, eight relevant TDF domains were identified: knowledge; skills; beliefs about capabilities; social influences; social/professional role and identity; environmental context and resources, reinforcement and emotion.
The relevant TDF domains for each overarching theme were linked to the constructs of the COM-B. The following findings are formatted as: the overarching theme in italics; the deductive codes (TDF domains) in bold; the COM-B construct in brackets and the substantiating verbatim participant quotes within quotations.
Theme 1: trusted local physician leader communicating about QI encourages participation
Social influences (Opportunity: Social)
Participants emphasised the importance of associating the QI initiative with a physician leader’s personal characteristics that influence colleague physician behaviour. Characteristics include being easy to get along with, trustworthy, credible and clinically knowledgeable. A participant stated, ‘It definitely helps to have a physician face on the project, the more credible the physician the better, helps to have a good person lead, and [who is] easy to get along with’—P10. Another participant explained the importance of relationships as a motivator for the individual’s initial participation by stating, ‘Relationships do matter, if you know somebody, and you trust them, it’s much more likely to do something that they are suggesting’—P11. Participants expressed the dissemination of the initiative should be completed by a local physician leader who is familiar with the environment and context. A participant stated, ‘It’s really important to have local physicians help to bring it in, as opposed to outside people’—P7.
Theme 2: provide QI-initiative plan/approach, data and physician role
Knowledge (capabilities: psychological), social influences (opportunity: social) goals (motivation: reflective), Beliefs about consequences, intentions and social professional role and identity (motivation: reflective).
Participants appreciated learning about all aspects of the initiative, including the plan/goals, clinical rationale and alignment to organisational strategies, the effect of a past intervention, local BUN data and the physician-QI leadership role. The following quotes illustrate this preference: ‘It was interesting to see how it was approached, what went well, what didn’t and do not need to start from scratch, is really helpful’—P5 and ‘Provided all of the information needed to roll this out, which made it easy to participate’—P1. Participants emphasised the importance of viewing data for their specific clinical programme, two individuals stated: ‘just seeing the data was pretty compelling’—P6; ‘being able to see (BUN) data before and after is a key part of any QI project, and they presented that which helped us understand’—P11.
Theme 3: order BUN tests mindfully not reflexively or habitually
Beliefs about capabilities (motivation: reflective), behavioural regulation (capability: psychological) and social influences (opportunity: social)
Hospital-based physicians admitted ordering BUN was due to ‘habitual ordering’—P12. Another participant reflected, ‘Why do I order urea all the time? I don’t even care what the number is in the vast majority of the cases, why am I doing it’—P11. Participants perceived paper-based order forms with check boxes made ordering easier, suggesting removal of the BUN-test check box and an electronic update of order panels, with provision of regular audit reports, would sustain change. Individuals shared the following perspectives: ‘There is a root cause, urea blood test exists on order sets’—P10; ‘Changing the automatic order sets in the IT-system and actually removing the choice from physicians is probably the number one intervention’—P1; and ‘Ongoing evaluation and review [is needed] to increase focus on mindful ordering’—P2.
Participants recognised the social influences and conformity behaviour regarding BUN ordering, with individuals stating, ‘Some physicians may have felt they had to change as everyone else had’—P2 and ‘We should all be working on trying to improve BUN ordering and if others can do it then we should be able to improve’—P4.
Theme 4: changing physician behaviour is difficult
Optimism, beliefs about consequences (motivation: reflective) and environmental context and resources (opportunity: physical).
Participants were pessimistic about changing ordering practices and mentioned the difficulty to change physician behaviour. One participant shared; ‘I think it’s going to be tough to change physician behaviour’—P8. Another stated, ‘Physicians may perceive a threat to their choice and freedom, and do not like being told what to do’—P7. Optimism about QI participation and initiative leadership was mentioned as being supported by training and personal interest. A participant shared; ‘My optimistic side feels that if we give good QI training that would motivate [physicians] to be more involved and I had enthusiasm and (QI) interest’—P11.
Theme 5: QI education and hands-on opportunities support involvement
Knowledge (capability: psychological), skills (capability: physical) and Beliefs about capabilities (motivation: reflective).
Eleven participants stated that QI was a new skill not taught in their medical training affecting their confidence to participate or lead. One participant stated, ‘QI is a very specific set of skills that may be new to some physicians; when asked to participate or lead projects, the confidence to do that may not be there’—P2. Participants’ perceived QI education including an opportunity for hands-on application supported their involvement in the initiative. Two participants shared: ‘(QI) training created opportunity, awareness and knowledge to engage physicians in this work’—P2 and ‘[QI] knowledge and just knowing how to be involved with the QI project [helped]’—P8.
Theme 6: physician mentorship
Social influences (opportunity: social) and Social professional role and identity (motivation: reflective).
Participants mentioned direct access to and guidance from physician colleagues with QI experience encouraged their leadership. One participant noted, ‘Attaching myself to a physician doing this project was helpful for me to learn and think’—P1. Another stated ‘Having physician partners to support and offer guidance helped with my development and [initiative] implementation’—P5. Additionally, participants reported that they did not perceive themselves as the initiative leader, rather as coleaders or helpers, alleviating the pressure to lead. A participant commented, ‘I don’t see myself as the primary owner of this project, a liaison to help support’—P1.
Theme 7: coalition functions as a safe peer-to-peer QI community
Knowledge (capability: psychological) and Social influences (opportunities: social).
Participants viewed the coalition as a QI community of practice that brings colleague physicians together to share experiences and to obtain advice. This is reflected in the following quotes: ‘Provides both QI knowledge and shares information on physician-led QI activities’—P3; ‘Coalition is a think tank where physicians can discuss QI topics’—P5 and ‘It is a safe environment for sharing as physicians learn and lead QI projects and to work through the struggles with likeminded physicians’—P2.
Theme 8: opportunity to lead, with support, a straightforward QI intervention that requires minimal effort
Environmental context and resources (capability: psychological), beliefs about capabilities (motivation: reflective) and emotion (motivation: automatic).
The initiative provided physicians the opportunity to participate, lead and implement an intervention with minimal workflow impact and effort, along with QI-personnel support. Comments reflecting this include: ‘The intervention was simple, that was attractive to me in terms of my involvement and gave me a level of confidence’—P3; ‘I knew I was going to get a lot of assistance’—P4 and ‘I really like this project narrow focus, supported my confidence to participate’—P11.
Theme 9: physician QI involvement competed out
Environmental context and resources (opportunity: physical), social professional role and identity, beliefs about consequences (motivation: reflection), emotion and reinforcement (motivation: automatic).
The challenge between clinical obligations and the initiative was a common sentiment impacting their involvement. A participant reflected, ‘Physicians finding the time to engage in QI projects while maintaining clinical service is always a juggle, clinical service will take precedent’—P2. Physician staffing challenges and competing priorities were exacerbated by the COVID-19 pandemic and the provincial implementation of an electronic medical record system. A participant explained this viewpoint with the following comment: ‘COVID-19 been in the back of everyone’s collective minds, the heavy clinical workload resulted in my lack of participation in this project, the challenge is QI [has] been competed out’—P7. Other individuals shared, ‘[Physicians are] being pulled to participate in the provincial IT system launch limiting our [availability]’—P3.
The pandemic had an impact on physicians’ emotional well-being, affecting their ability to participate in and lead this initiative. One participant described this limitation as follows: ‘There’s been a huge change in terms of medical staff mentality over the past year we simply do not have the resources to do it and I don’t like to use the word burnout, but people are tired’—P10. Participants expressed concern regarding a lack of remuneration, which they stated affects physician QI involvement. Individuals stated: ‘Physicians are not paid to engage in QI projects and must do so on their own time’—P2 and ‘There is zero financial remuneration for QI’—P10.
Intervention functions
Aligning the relevant TDF domains within the overarching themes to the BCW26 identified future intervention strategies (table 4) that included: (1) education in QI and clinical laboratory medicine; (2) provide hands-on QI opportunities for knowledge and leadership; (3) physician role modelling QI to aspire to or imitate; (4) employ persuasion (a local credible physician) to facilitate participation; (5) provide successful physician-led projects targeting lab test reduction; (6) provide data and human resource support; (7) provide cost data to demonstrate consequence; (8) offer incentives, remuneration and formal physician QI roles to encourage involvement; (9) apply guidelines (laboratory test ordering protocols); (10) restrictions (limit test order frequency when results are normal) and (11) environmental restructuring (modify laboratory order panels/forms) to reduce unnecessary test ordering.
Table 4.
Intervention functions, policies and definitions with examples of participant-identified interventions (based on Michie et al)
| Intervention function | Definition | Examples of identified interventions |
| Education | Increase knowledge or understanding | Offer QI and clinical laboratory educational sessions (clinical best practice); and Apply guidelines (laboratory test ordering protocols) |
| Persuasion | Communication is used to elicit positive or negative emotions, or to stimulate action | Communication from a credible physician leader to encourage behavioural test ordering change and QI project participation |
| Incentivisation | Create expectation of reward | Provide financial reimbursement for physician-led QI |
| Coercion/ consequence | Create expectation of negative consequence, punishment or cost | Provide cost data to demonstrate negative consequence |
| Training | Impart skills | Provide hands-on experiential QI opportunity to apply knowledge and leadership |
| Restriction | Using rules to reduce the opportunity to engage in the target behaviour (or to increase the target behaviour by reducing the opportunity to engage in competing behaviours) | Limit lab test order frequency when results are normal—ie, once per week, etc. |
| Environmental restructuring | Changing the physical or social context | Update paper and IT lab test order forms, to prevent reflexive ordering |
| Modelling | Providing an example for people to aspire to or imitate | Provide examples of past physician-led projects targeting lab test reduction Provide physician QI mentors |
| Enablement | Increasing means/reducing barriers to increase capability or opportunity | Provide support personnel-QI consultant and data analysts Provide frequent audit reports—lab test utilisation data to enable practice change |
| Policies | ||
| Communication/ marketing | Using print, electronic, telephone or broadcast media | Display posters on the hospital units Decision support tools, provided at points of physician ordering to encourage appropriate testing |
| Guidelines | Creating documents that recommend or mandate practice. This includes all changes to service provision | Develop and disseminate laboratory test ordering guidelines. |
| Fiscal | Using the health organisation budgeting processes to reduce or increase the financial cost | Report and disseminate organisational budgetary impacts related lab test ordering |
| Regulation | Establishing rules or principles of behaviour or practice | Implement or adapt as required organisational wide Choosing Wisely recommendations |
| Legislation | Making or changing laws | Prohibit diagnostic testing resource waste, monitored and reported by health organisation |
| Environmental/social planning | Designing and/or controlling the physical or social environment | Engage laboratory medicine and physician professional association leaders in strategic planning regarding lab ordering Engage health organisations human resources dept. regarding formalisation of physician-QI leadership role (job description) |
| Service provision | Delivering a service | Establish formal physician QI leadership role and job description (QI activities have priority) |
QI, quality improvement.
Discussion
This study employed a systematic, theory-based approach to identify behavioural characteristics that were perceived to influence physician QI participation, leadership and appropriate BUN ordering. Eight TDF domains were found to influence QI leadership and participation and 10 TDF domains influenced BUN ordering. Nine overarching themes were generated from 37 domain-specific themes, and 11 intervention functions were identified to inform future initiatives.
Physicians perceived appropriate (reduce excess) BUN-ordering behaviour practice change required a credible physician leader with a multistrategy/initiative approach that includes person-focused (ie, education, laboratory test data, clinical best-practice/guidelines, physician role) and system-focused (ie, paper or IT order form modifications) intervention functions.29 The intervention functions identified in this study corroborate recent evidence that interventions aimed at laboratory testing require multiple strategies.30–32 The use of credible local opinion leaders defined as healthcare providers in a specific area who communicate, role model and provide support for the application of best practice evidence/guidelines have been reported to contribute to project success.33 The QI-initiative educational presentation included the use of social comparison as an additional source of motivation to change behaviour.34 Previous initiative BUN-test reduction data were also included and this was perceived as compelling and meaningful to physicians. This finding paralleled a recent survey reporting physicians in hospitals required data to promote a change in order behaviour.30
Study participants mentioned many barriers to their QI involvement found in literature, including high clinical workload, lack of time, limited QI skills and training, lack of access to data and support from hospital/health organisation administration and lack of financial compensation.4 6 An additional barrier identified in this study was a lack of clarity about the physician QI role and responsibility. From the participants’ interviews, various strategies that enable QI-involvement behaviour change were identified. These include physician coalition leader or member credibility and awareness of, or a past relationship with a coalition member was found to be more important to their initial engagement than knowledge of coalition existence. As well as, providing QI education, personnel and data assistance, experiential QI opportunities that required minimal effort, QI-initiative role clarity, physician mentorship and organisational leadership support were all found to enable physician behaviour change. These strategies/interventions are similar to those reported as important in other physician QI programmes.35–38 The coalition, a peer-to-peer QI community, was perceived as a motivator for behavioural change. A recent study noted, forming a ‘consortium of clinical [physician] QI leaders who both practice clinically and work on the frontlines of QI leadership’, p80039 would increase QI, implementation and dissemination of initiatives among physicians, implying the potential of this approach as a QI engagement strategy.
The TDF and BCW provided a systematic approach to identify the theoretical reasons that change occurs, allowed for cross-checking the allocation of domains,40 and were a good choice for researchers with limited experience with behavioural theories.8 For physician and organisational leaders, these study findings can be used to design future physician-led initiatives about appropriate diagnostic test ordering and to advocate for resources that support strategies to reduce barriers to physician-QI involvement. To gain additional insights, next steps include integrating the study findings with quantitative data (monthly BUN-test order volumes) for each participating hospital.
Limitations
There is a potential for selection bias, participants were the physician leads and supporters, who may have been more motivated towards QI than physicians who did not lead/participate. Participant interviews occurred during the second and third wave of the COVID-19 pandemic; most interviews were shorter than planned and occurred during work hours, which may have affected participants’ response due to competing demands. Investigating multiple behaviours at the same time was challenging to analyse and separate.
Conclusion
The identified characteristics aligned to several TDF domains that influence physician leadership, participation and appropriate BUN-test ordering behaviours, implying these behaviours are multidimensional constructs that require a multistrategy approach to change behaviour. Based on our findings, the key interventions that influence physician behaviour change for QI involvement and appropriate laboratory test ordering were QI education with hands-on training, physician peer mentorship/support, personnel assistance (QI and analytics), communication from a trusted/credible physician leader who shares data, insights about the initiative physician role, clinical best practice and past project success. As well, a simply designed initiative requiring minimal effort with no clinical workflow disruptions, revised order forms/panels and limiting test order frequency when laboratory tests are normal are also important. Future research is needed to determine the effectiveness of the identified interventions and to understand the change management aspects involved in physician-led QI.
Acknowledgments
The authors are grateful to all the physicians who participated in the study and who generously gave their time to share their experiences.
Footnotes
Twitter: @LenoraDuhn
Contributors: PM: led project design, analysis, wrote and reviewed the manuscript and is the guarantor for this work. JM: academic supervisor of PM reviewed all aspects of the study such as design, analysis, and manuscript development. SM: assisted with data collection and analysis. SM, NK, KS, LD and JM: critically reviewed and edited the manuscript. All authors approved the final manuscript.
Funding: Choosing Wisely Alberta grant funded the project titled, ‘The Effectiveness of a Sequenced Multi-component Intervention: Reducing Urea Utilization and Laboratory Test Order Frequency in Alberta’. No award/grant number.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by Queen’s University Health Sciences & Affiliated Teaching Hospitals Research Ethics Board (TRAQ#: 6030885) and University of Alberta Health Research Ethics Board (Pro00106594). Participants gave informed consent to participate in the study before taking part.
References
- 1.Freedman DB. Towards Better Test Utilization - Strategies to Improve Physician Ordering and Their Impact on Patient Outcomes. EJIFCC 2015;26:15–30. [PMC free article] [PubMed] [Google Scholar]
- 2.Jalbert R, Gob A, Chin-Yee I. Decreasing daily blood work in hospitals: What works and what doesn't. Int J Lab Hematol 2019;41 Suppl 1:151–61. ‐. 10.1111/ijlh.13015 [DOI] [PubMed] [Google Scholar]
- 3.Hall A. The (nonfinancial) benefits of reducing unnecessary lab testing. healthcare financial management, 2018. Available: https://api.hfma.org/Content.aspx?id=59162
- 4.Yousefi V, Asghari-Roodsari A, Evans S, et al. Determinants of hospital-based physician participation in quality improvement: a survey of hospitalists in British Columbia, Canada. Global Journal on Quality and Safety in Healthcare 2020;3:6–13. 10.4103/JQSH.JQSH_17_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Aerde J, Dickson G. Accepting our responsibility: A blue print for physician leadership in transforming Canada’s health care system. White Paper, 2017. Available: https://www.canadianhealthcarenetwork.ca/files/2017/02/CSPLWhitepaper2017.pdf
- 6.Mahbooba Z, Chera B, Evarts L. Engaging physicians in quality improvement in a hospital setting: a scoping review. Am J Med Qual 2021;36:328–36. 10.1097/01.JMQ.0000735456.03039.2e [DOI] [PubMed] [Google Scholar]
- 7.Levinson W, Kallewaard M, Bhatia RS, et al. 'Choosing wisely': a growing international campaign. BMJ Qual Saf 2015;24:167–74. 10.1136/bmjqs-2014-003821 [DOI] [PubMed] [Google Scholar]
- 8.Grimshaw JM, Patey AM, Kirkham KR, et al. De-implementing wisely: developing the evidence base to reduce low-value care. BMJ Qual Saf 2020;29:409–17. 10.1136/bmjqs-2019-010060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calder Bateman . University of Alberta department of medicine strategic plan, 2014. Available: https://cloudfront.ualberta.ca/-/media/medicine/departments/medicine/strategic-plan/2014-strategicplanreport.pdf [Accessed 13 Oct 2019].
- 10.Mathura P, Marini S, Spalding K, et al. Physician-led quality improvement: a blueprint for building capacity. CJPL 2022;8:51–8. 10.37964/cr24749 [DOI] [Google Scholar]
- 11.Butterfoss F. Coalitions and partnerships in community health. San Francisco: Jossey-Bass, 2007. [Google Scholar]
- 12.Kelly CS, Meurer JR, Lachance LL, et al. Engaging health care providers in coalition activities. Health Promot Pract 2006;7:66S–75. 10.1177/1524839906287056 [DOI] [PubMed] [Google Scholar]
- 13.Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7:1–17. 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (V1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 15.Sarmast H, Mosavianpour M, Collet J-P, et al. Tdf (theoretical domain framework): how inclusive are TDF domains and constructs compared to other tools for assessing barriers to change? BMC Health Serv Res 2014;14:P81. 10.1186/1472-6963-14-S2-P81 [DOI] [Google Scholar]
- 16.Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017;12:77. 10.1186/s13012-017-0605-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cadogan SL, McHugh SM, Bradley CP, et al. General practitioner views on the determinants of test ordering: a theory-based qualitative approach to the development of an intervention to improve immunoglobulin requests in primary care. Implement Sci 2016;11:102. 10.1186/s13012-016-0465-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patey AM, Islam R, Francis JJ, et al. Anesthesiologists' and surgeons' perceptions about routine pre-operative testing in low-risk patients: application of the theoretical domains framework (TDF) to identify factors that influence physicians' decisions to order pre-operative tests. Implement Sci 2012;7:52. 10.1186/1748-5908-7-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toman I, Mathura P, Kassam N. A multifaceted quality improvement initiative to reduce unnecessary laboratory testing on internal medicine inpatient wards. Canadian Journal of General Internal Medicine 2020;15:30–7. 10.22374/cjgim.v15i2.357 [DOI] [Google Scholar]
- 21.Mathura P, Boettger C, Hagtvedt R, et al. Does admission order form design really matter? A reduction in urea blood test ordering. BMJ Open Qual 2021;10:e001330. 10.1136/bmjoq-2020-001330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayring P. Qualitative content analysis. Forum: qualitative social research. Qualitative Research 2000;1:20 https://www.qualitative-research.net/index.php/fqs/article/view/1089 [Google Scholar]
- 23.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med 2012;22:276–82. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clarke V, Braun V. Thematic analysis. J Posit Psychol 2017;12:297–8. 10.1080/17439760.2016.1262613 [DOI] [Google Scholar]
- 25.Guest G, MacQueen K, Namey E. Introduction to Applied Thematic Analysis. In: Applied thematic analysis. SAGE Publications, Inc, 2014: 3–20. [Google Scholar]
- 26.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.John C, David C. Research design : qualitative, quantitative, and mixed methods approaches. SAGE, 2018. [Google Scholar]
- 28.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 29.Soong C, Shojania KG. Education as a low-value improvement intervention: often necessary but rarely sufficient. BMJ Qual Saf 2020;29:353–7. 10.1136/bmjqs-2019-010411 [DOI] [PubMed] [Google Scholar]
- 30.Bodley T, Kwan JL, Matelski J, et al. Self-Reported test ordering practices among Canadian internal medicine physicians and trainees: a multicenter cross-sectional survey. BMC Health Serv Res 2019;19:820. 10.1186/s12913-019-4639-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nash DM, Garg AX, Brimble KS, et al. Primary care provider perceptions of enablers and barriers to following guideline-recommended laboratory tests to confirm chronic kidney disease: a qualitative descriptive study. BMC Fam Pract 2018;19:192. 10.1186/s12875-018-0879-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bindraban RS, van Beneden M, Kramer MHH, et al. Association of a multifaceted intervention with ordering of unnecessary laboratory tests among caregivers in internal medicine departments. JAMA Netw Open 2019;2:e197577. 10.1001/jamanetworkopen.2019.7577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medves J, Godfrey C, Turner C, et al. Systematic review of practice guideline dissemination and implementation strategies for healthcare teams and team-based practice. Int J Evid Based Healthc 2010;8:79–89. 10.1111/j.1744-1609.2010.00166.x [DOI] [PubMed] [Google Scholar]
- 34.Ryskina K, Jessica Dine C, Gitelman Y, et al. Effect of social comparison feedback on laboratory test ordering for hospitalized patients: a randomized controlled trial. J Gen Intern Med 2018;33:1639–45. 10.1007/s11606-018-4482-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goitein L. Clinician-Directed performance improvement: moving beyond externally mandated metrics. Health Aff 2020;39:264–72. 10.1377/hlthaff.2019.00505 [DOI] [PubMed] [Google Scholar]
- 36.Hoag G. The Physician Quality Improvement initiative: Improving BC’s health care system one project at a time. BC Medical Journal 2019;61:291. [Google Scholar]
- 37.Li J, Hinami K, Hansen LO, et al. The physician mentored implementation model: a promising quality improvement framework for health care change. Acad Med 2015;90:303–10. 10.1097/ACM.0000000000000547 [DOI] [PubMed] [Google Scholar]
- 38.Maynard GA, Budnitz TL, Nickel WK, et al. Mentored implementation: building leaders and achieving results through a collaborative improvement model. The Joint Commission Journal on Quality and Patient Safety 2012;38:301–3. 10.1016/S1553-7250(12)38040-9 [DOI] [PubMed] [Google Scholar]
- 39.Li L, Black WE, Cheung EH, et al. Building psychiatric quality programs and defining quality leadership roles at four academic medical centers. Acad Psychiatry 2020;44:795–801. 10.1007/s40596-020-01317-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McSherry LA, Dombrowski SU, Francis JJ, et al. 'It's a can of worms': understanding primary care practitioners' behaviours in relation to HPV using the theoretical domains framework. Implement Sci 2012;7:73. 10.1186/1748-5908-7-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2022-001965supp001.pdf (218.1KB, pdf)
bmjoq-2022-001965supp002.pdf (157.5KB, pdf)
Data Availability Statement
No data are available.