Abstract
Malocclusion is considered one of the most prevalent oral issues and it is considered one of the major risk factors for dental trauma. Dental trauma is a distressing experience for children, and they can have long-term physical, esthetic, and psychological effects. Hence, the main aim of this retrospective study is to evaluate the association between dental trauma and malocclusion in children. Four hundred and fifty patients between the age of 8 and 17 years during March 1, 2020–February 31, 2021, with Ellis classes 1, 2, and 3 were included in the study. Association of type of fracture with gender and malocclusion was calculated using Chi-square test. In case of Ellis class 1 fracture, 9.1% of the patients had no malocclusion, 21.8% of them had crowding, 11% of them had spacing, and 21.8% of them had anterior protrusion. In case of Ellis class 2 fracture, 4.3% of them had no malocclusion, 6.4% of them had crowding, 2.8% of them had spacing, and 3.6% of them had anterior protrusion. In case of Ellis class 3 fracture, 2.7% of them had no malocclusion, 6.4% of them had crowding, 4.6% of them had spacing, and 4.6% had anterior protrusion. The results were not statistically significant. Children with anterior protrusion and anterior crowding are more prone to severe damage during traumatic dental injuries.
Keywords: Dental trauma, innovative technique, malocclusion, oral health
INTRODUCTION
Children are the victims of the majority of dental complications. Traumatic injuries are distressing, especially when the trauma is associated with the tooth and the supporting tissues. Traumatic dental accidents can harm the teeth and cause esthetic, psychological, social, and therapeutic issues.[1,2] The most serious dental traumatic injuries usually involve one permanent tooth and maxillary central incisors are the most often affected. Fracture involving enamel (Ellis class 1), enamel and dentin (Ellis class 2), and fracture involving enamel and dentin with pulpal involvement (Ellis class 3) are the most common type of dental injury encountered in permanent teeth. Dental traumatic injuries most commonly occur in all genders and are more prone during the ages of 2–4 years and 8–10 years.[3,4] Due to their developmental stage, children are normally more active during these ages and frequently they tend to lack motoric control. As a result, they are often unable to accurately assess velocity and risk.[5]
Regardless of the stage of occlusal formation, malocclusion is more common than normal occlusion in all populations. Malocclusion's predominance is demonstrated by its multifactorial etiology, which includes genetic and environmental causes that all lead to the development of various forms of malocclusion.[5,6] Due to their widespread occurrence and frequency in all parts of the world, oral diseases are considered significant public health issues. Since pain and discomfort are rarely serious, malocclusion has not been extensively studied.[7,8] In terms of pain, quality of living, and social and practical limits, malocclusion has a significant effect on individuals and community. Malocclusion can be caused by genetically determined causes, environmental factors, or, most generally, a result of both inherited and environmental factors. Malocclusion can be a result of local factors, such as bad oral habits, tooth number, form, and developmental abnormalities.[9] Malocclusion has been found to have a negative impact on periodontal hygiene maintenance, implicated in the increase of dental caries, and results in temporomandibular joint disorders. In India, the prevalence of malocclusion varies from 20% to 43%. The concerns of esthetics, self-esteem, age, gender, self-perception of their dental appearance, and peer group norms all influence orthodontic treatment uptake. The main advantages of orthodontic surgery are improved physical function, tissue injury prevention, and cosmetic aspect correction.[10,11]
Earlier studies have demonstrated that nearly one-third of preschoolers suffered from traumatic dental injuries.[12,13] Evaluation of Traumatic dental injuries (TDI) is important, especially in primary dentition due to the potential sequelae in the periapical region, that may adversely affect the developmental process of permanent teeth and occlusal development. Dental injuries are the most common among all facial injuries reported in children. The upper central incisors are the most often affected teeth by injuries, presumably due to their location in the mouth, where they are less secure than the other teeth.[14] Physical characteristics such as an elevated incisal overjet and an anterior open bite have been identified as traumatic dental injuries predisposing factors.[15,16] Furthermore, the occurrence of these anterior malocclusion characteristics may result in feature loss.
The present study is needed to obtain information about the role played by malocclusion in influencing the severity of dental trauma. Moreover, it can be used to assess the importance of orthodontic correction in children. Our research and knowledge have resulted in high-quality publications from our team.[17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]
The main aim and objective of the study are to find out the association between malocclusion and trauma in children.
MATERIALS AND METHODS
Study design
Ethical approval was taken from the institutional review board (IHEC/SDC/PEDO/21/128). The study design was planned and adapted to include all children aged between 8 and 17 years with Ellis classes 1, 2, and 3 fractures. The children were excluded from the study if they did not fall under the inclusion criteria.
Sampling technique
A random sampling technique was adopted in the study to reduce the risk of bias in sampling and all the cases were reviewed by a blind examiner priorly and included in the study.
Data analysis
Data were collected from the patient database with the time framework between March 1, 2020, and February 31, 2021. About 450 orthopantomograms (OPGs) were reviewed by two examiners. The OPGs which met the inclusion criteria were included in the study. Data were cross-verified by another reviewer. The collected data were tabulated under the following parameters:
Patient undergone trauma
Patient with Ellis classes 1, 2, and 3 fracture.
Statistical analysis
Statistical analysis was done using the SPSS version 20.0 (SPSS sofware, IBM, SPSS Statistics for Windows, Armonk, NY: IBM Corp). The variables were coded and imported into statistical software. The categorical variables were expressed in terms of frequency and percentage and bar graphs were plotted. Associations were tested using Chi-square test.
RESULTS
In the male population, 13.6% of the population had no malocclusion, 0.25.4% of them had crowding, 12.7% of them had spacing, and 22% of the male population had anterior protrusion. In case of female patients, 3.6% of them had no malocclusion, 9% of them had crowding, 5.4% of them had spacing, and 8% of them had anterior protrusion. The P value was 0.224 (P > 0.005). The result was statistically not significant [Figure 1].
Figure 1.
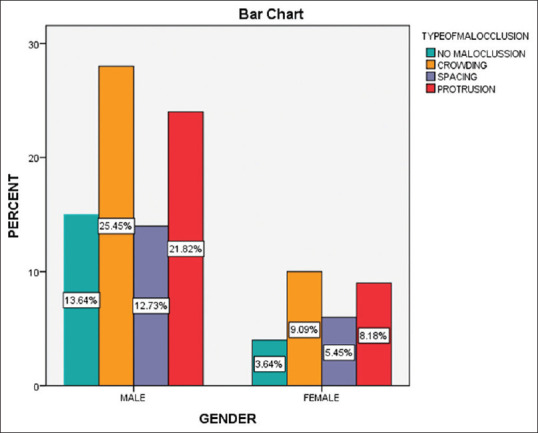
Association of gender to that of type of malocclusion
In case of male patients, 49% of them had Ellis class 1 fracture, 12.8% of them had Ellis class 2 fracture, and 11.8% of them had Ellis class 3 fracture. In case of females, 15.5% of them had Ellis class 1 fracture, 5.5% of them had Ellis type 2 fracture, and 6.4% of them had Ellis type 3 fracture. The P value was 0.731 (P > 0.005). The result was statistically not significant [Figure 2].
Figure 2.
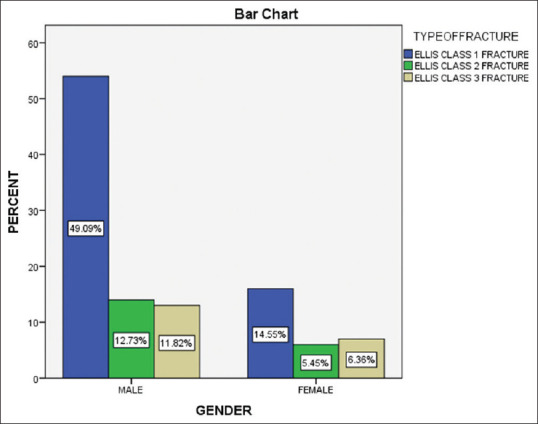
Association between the gender and the type of ellis fracture
In case of Ellis class 1 fracture, 9.1% of the patients had no malocclusion, 21.8% of them had crowding, 11% of them had spacing, and 21.8% of them had anterior protrusion. In case of Ellis class 2 fracture, 4.3% of them had no malocclusion, 6.4% of them had crowding, 2.8% of them had spacing, and 3.6% of them had anterior protrusion. In case of Ellis class 3 fracture, 2.7% of them had no malocclusion, 6.4% of them had crowding, 4.6% of them had spacing, and 4.6% had anterior protrusion. The P value was 0.04 (P > 0.005). The result was statistically not significant [Figure 3].
Figure 3.
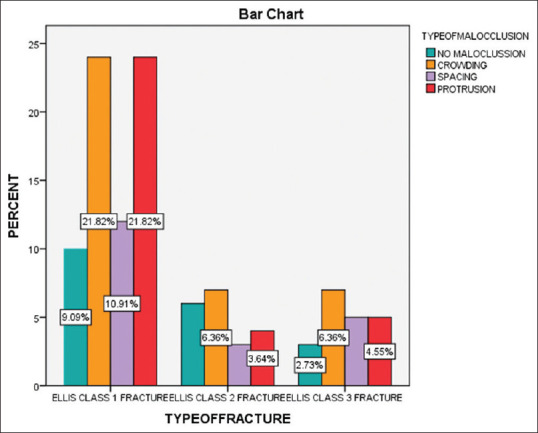
Association of type of malocclusion and type of ellis fracture
DISCUSSION
Dental trauma can result in pain, loss of function, and poor esthetics which may have a direct impact on both the physiological and psychological development of the child. In the present study, most of the dental injuries were encountered in the maxillary anterior. This may be due to the fact that maxillary incisors are usually proclined and which get a direct blow resulting in injury.[32]
Certain occlusal characteristics may predispose a person to trauma by exposing the maxillary anterior teeth to more vulnerable situations. Several research has looked at the link between malocclusion and the occurrence of dental damage in primary teeth. The research, on the other hand, does not clearly indicate a link between the kind of malocclusion and the kind, intensity, and amount of trauma.[33,34] As a result, the current study looked at a group of children with TDI to see if there was a link between malocclusion and the type of trauma to the teeth.
In the present study, male children sustained more injuries than female children. Ellis classes 1, 2, and 3 fractures were seen more in male children than in female children. However, the results were statistically insignificant. Boys are more robust, take more risks, engage in sports and leisure activities, and are aggressive in nature. Thus, they are more prone to fracture.[32]
In the present study, it was found that Ellis class 1 and Ellis class 2 fractures are frequently seen in children with anterior crowding and anterior proclination. Similar results were obtained for Ellis class 3 fracture. Ellis class 3 fractures are more commonly encountered with anterior crowding, anterior proclination, and spacing.
The present study explains the association between malocclusion and trauma in children of age 8–17 years. Hard-tissue injuries were the most prevalent dental injuries in this study. The majority of them were enamel fractures (63.64%) which are similar to other research.[35] Thirty percent of the children undergone traumatic dental injury had anterior protrusion. Children with anterior protrusion had a greater rate of serious damage and trauma affecting numerous teeth than children without open bites, according to the findings of this study. It is likely that children with anterior protrusion have insufficient lip covering, allowing the lips to absorb some of the stress on the anterior teeth in the event of dental trauma. It is similar to previous studies.[1,36] About 34.6% of children who had traumatic dental injury had anterior crowding this is similar to the previous literature.[37]
Limitations
In this study, we have taken only Ellis classes 1, 2, and 3 fractures. More comprehensive studies are required to evaluate the association of malocclusion dental traumatic injuries in primary dentition and permanent dentition.
CONCLUSION
Anterior protrusion and anterior crowding are associated with a significantly higher frequency of severe traumatic dental injuries. This emphasizes the importance of orthodontic correction of malocclusion in children.
Financial support and sponsorship
The present study was supported by the following agencies
Saveetha Institute of Medical and Technical Science
Saveetha Dental College and Hospitals
Saveetha University
Ganga Devi Transports, Madhavaram, Chennai.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author would like to acknowledge the help and support rendered by Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Science, and Saveetha University, Chennai.
REFERENCES
- 1.Bonini GC, Bönecker M, Braga MM, Mendes FM. Combined effect of anterior malocclusion and inadequate lip coverage on dental trauma in primary teeth. Dent Traumatol. 2012;28:437–40. doi: 10.1111/j.1600-9657.2012.01117.x. [DOI] [PubMed] [Google Scholar]
- 2.Feldens CA, Kramer PF, Ferreira SH, Spiguel MH, Marquezan M. Exploring factors associated with traumatic dental injuries in preschool children: A Poisson regression analysis. Dent Traumatol. 2010;26:143–8. doi: 10.1111/j.1600-9657.2009.00858.x. [DOI] [PubMed] [Google Scholar]
- 3.Viegas CM, Scarpelli AC, Carvalho AC, Ferreira FM, Pordeus IA, Paiva SM. Predisposing factors for traumatic dental injuries in Brazilian preschool children. Eur J Paediatr Dent. 2010;11:59–65. [PubMed] [Google Scholar]
- 4.Piovesan C, Guedes RS, Casagrande L, Ardenghi TM. Socioeconomic and clinical factors associated with traumatic dental injuries in Brazilian preschool children. Braz Oral Res. 2012;26:464–70. doi: 10.1590/s1806-83242012000500014. [DOI] [PubMed] [Google Scholar]
- 5.Jorge KO, Moysés SJ, Ferreirae Ferreira E, Ramos-Jorge ML, de Araújo Zarzar PM. Prevalence and factors associated to dental trauma in infants 1-3 years of age. Dent Traumatol. 2009;25:185–9. doi: 10.1111/j.1600-9657.2008.00730.x. [DOI] [PubMed] [Google Scholar]
- 6.De Almeida MR, Pozzobon PA, De Almeida RR, De Almeida P, Da Silva FO. Prevalence of malocclusion in children aged 7 to 12 years. Dent Press J Orthod. 2011;16:123–7. [Google Scholar]
- 7.Thiruvenkatachari B, Harrison J, Worthington H, O'Brien K. Early orthodontic treatment for Class II malocclusion reduces the chance of incisal trauma: Results of a Cochrane systematic review. American Journal of Orthodontics and Dentofacial Orthopedics. 2015;148:47–59. doi: 10.1016/j.ajodo.2015.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Doriguêtto PV, Carrada CF, Scalioni FA, Abreu LG, Devito KL, Paiva SM, et al. Malocclusion in children and adolescents with Down syndrome: A systematic review and meta-analysis. Int J Paediatr Dent. 2019;29:524–41. doi: 10.1111/ipd.12491. [DOI] [PubMed] [Google Scholar]
- 9.Brito DI, Dias PF, Gleiser R. Prevalence of malocclusion in children aged 9 to 12 years old in the city of nova friburgo, rio de Janeiro State, Brazil. Rev Dent Press Ortodontia Ortop Facial. 2009;14:118–24. [Google Scholar]
- 10.Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: A systematic review of quantitative studies. Eur J Orthod. 2015;37:238–47. doi: 10.1093/ejo/cju046. [DOI] [PubMed] [Google Scholar]
- 11.Zhang M, McGrath C, Hägg U. The impact of malocclusion and its treatment on quality of life: A literature review. Int J Paediatr Dent. 2006;16:381–7. doi: 10.1111/j.1365-263X.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 12.Oldin A, Lundgren J, Nilsson M, Norén JG, Robertson A. Traumatic dental injuries among children aged 0-17 years in the BITA study –A longitudinal Swedish multicenter study. Dent Traumatol. 2015;31:9–17. doi: 10.1111/edt.12125. [DOI] [PubMed] [Google Scholar]
- 13.Jesus MA, Antunes LA, Risso Pde A, Freire MV, Maia LC. Epidemiologic survey of traumatic dental injuries in children seen at the Federal University of Rio de Janeiro, Brazil. Braz Oral Res. 2010;24:89–94. doi: 10.1590/s1806-83242010000100015. [DOI] [PubMed] [Google Scholar]
- 14.Shayegan A, De Maertelaer V, Vanden Abbeele A. The prevalence of traumatic dental injuries: A 24-month survey. J Dent Child (Chic) 2007;74:194–9. [PubMed] [Google Scholar]
- 15.Ekanayake L, Perera M. Pattern of traumatic dental injuries in children attending the University Dental Hospital, Sri Lanka. Dent Traumatol. 2008;24:471–4. doi: 10.1111/j.1600-9657.2008.00611.x. [DOI] [PubMed] [Google Scholar]
- 16.Nicolau B, Marcenes W, Sheiham A. Prevalence, causes and correlates of traumatic dental injuries among 13-year-olds in Brazil. Dent Traumatol. 2001;17:213–7. doi: 10.1034/j.1600-9657.2001.170505.x. [DOI] [PubMed] [Google Scholar]
- 17.Rajeshkumar S, Menon S, Venkat Kumar S, Tambuwala MM, Bakshi HA, Mehta M, et al. Antibacterial and antioxidant potential of biosynthesized copper nanoparticles mediated through Cissus arnotiana plant extract. J Photochem Photobiol B. 2019;197:111531. doi: 10.1016/j.jphotobiol.2019.111531. [DOI] [PubMed] [Google Scholar]
- 18.Chen F, Tang Y, Sun Y, Veeraraghavan VP, Mohan SK, Cui C. 6-shogaol, a active constiuents of ginger prevents UVB radiation mediated inflammation and oxidative stress through modulating NrF2 signaling in human epidermal keratinocytes (HaCaT cells) J Photochem Photobiol B. 2019;197:111518. doi: 10.1016/j.jphotobiol.2019.111518. [DOI] [PubMed] [Google Scholar]
- 19.Murugan MA, Arul Murugan M, Jayaseelan V, Jayabalakrishnan D, Maridurai T, Selva Kumar S, et al. Low velocity impact and mechanical behaviour of shot blasted SiC wire-mesh and silane-treated aloevera/hemp/flax-reinforced SiC whisker modified epoxy resin composites. Silicon. 2020;12:1847–56. [Google Scholar]
- 20.Rajagopal R, Padmanabhan S, Gnanamani J. A comparison of shear bond strength and debonding characteristics of conventional, moisture-insensitive, and self-etching primers in vitro. Angle Orthod. 2004;74:264–8. doi: 10.1043/0003-3219(2004)074<0264:ACOSBS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Muthukrishnan S, Krishnaswamy H, Thanikodi S, Sundaresan D, Venkatraman V. Support vector machine for modelling and simulation of heat exchangers. Therm Sci. 2020;24:499–503. [Google Scholar]
- 22.Ezhilarasan D. Oxidative stress is bane in chronic liver diseases: Clinical and experimental perspective. Arab J Gastroenterol. 2018;19:56–64. doi: 10.1016/j.ajg.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Neelakantan P, Sharma S, Shemesh H, Wesselink PR. Influence of irrigation sequence on the adhesion of root canal sealers to dentin: A Fourier transform infrared spectroscopy and push-out bond strength analysis. J Endod. 2015;41:1108–11. doi: 10.1016/j.joen.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Jose J, Ajitha P, Subbaiyan H. Different treatment modalities followed by dental practitioners for Ellis class 2 fracture –A Questionnaire-based survey. Open Dent J. 2020;14:59–65. [Google Scholar]
- 25.Sahu D, Kannan GM, Vijayaraghavan R. Carbon black particle exhibits size dependent toxicity in human monocytes. Int J Inflam 2014. 2014:827019. doi: 10.1155/2014/827019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nandhini NT, Rajeshkumar S, Mythili S. The possible mechanism of eco-friendly synthesized nanoparticles on hazardous dyes degradation. Biocatal Agric Biotechnol. 2019;19:101138. [Google Scholar]
- 27.Wu F, Zhu J, Li G, Wang J, Veeraraghavan VP, Krishna Mohan S, et al. Biologically synthesized green gold nanoparticles from Siberian ginseng induce growth-inhibitory effect on melanoma cells (B16) Artif Cells Nanomed Biotechnol. 2019;47:3297–305. doi: 10.1080/21691401.2019.1647224. [DOI] [PubMed] [Google Scholar]
- 28.Patil SB, Durairaj D, Suresh Kumar G, Karthikeyan D, Pradeep D. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg. 2017;16:312–21. doi: 10.1007/s12663-016-0975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uthrakumar R, Vesta C, Raj CJ, Krishnan S, Das SJ. Bulk crystal growth and characterization of non-linear optical bisthiourea zinc chloride single crystal by unidirectional growth method. Curr Appl Phys. 2010;10:548–52. [Google Scholar]
- 30.Vijayakumar Jain S, Muthusekhar MR, Baig MF, Senthilnathan P, Loganathan S, Abdul Wahab PU, et al. Evaluation of three-dimensional changes in pharyngeal airway following isolated lefort one osteotomy for the correction of vertical maxillary excess: A prospective study. J Maxillofac Oral Surg. 2019;18:139–46. doi: 10.1007/s12663-018-1113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vishnu Prasad S, Kumar M, Ramakrishnan M, Ravikumar D. Report on oral health status and treatment needs of 5-15 years old children with sensory deficits in Chennai, India. Spec Care Dentist. 2018;38:58–9. doi: 10.1111/scd.12267. [DOI] [PubMed] [Google Scholar]
- 32.Dharmani CK, Pathak A, Sidhu HS. Prevalence of traumatic dental injuries to anterior teeth in 8-12-year-old schoolchildren of Patiala City, Punjab, India: An epidemiological study. Int J Clin Pediatr Dent. 2019;12:25. doi: 10.5005/jp-journals-10005-1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goettems ML, Azevedo MS, Correa MB, Costa CT, Wendt FP, Schuch HS, et al. Dental trauma occurrence and occlusal characteristics in Brazilian preschool children. Pediatr Dent. 2012;34:104–7. [PubMed] [Google Scholar]
- 34.Arraj GP, Rossi-Fedele G, Doğramacı EJ. The association of overjet size and traumatic dental injuries –A systematic review and meta-analysis. Dent Traumatol. 2019;35:217–32. doi: 10.1111/edt.12481. [DOI] [PubMed] [Google Scholar]
- 35.Norton E, O'Connell AC. Traumatic dental injuries and their association with malocclusion in the primary dentition of Irish children. Dent Traumatol. 2012;28:81–6. doi: 10.1111/j.1600-9657.2011.01032.x. [DOI] [PubMed] [Google Scholar]
- 36.Agostini BA, Pinto LT, Koehler M, Emmanuelli B, Piovesan C, Ardenghi TM. Trend of traumatic crown injuries and associated factors in preschool children. Braz Oral Res. 2016;30:e112. doi: 10.1590/1807-3107BOR-2016.vol30.0112. [DOI] [PubMed] [Google Scholar]
- 37.Primo-Miranda EF, Ramos-Jorge ML, Homem MA, de Souza DS, Stetler AD, Ramos-Jorge J, et al. Association between occlusal characteristics and the occurrence of dental trauma in preschool children: A case-control study. Dent Traumatol. 2019;35:95–100. doi: 10.1111/edt.12457. [DOI] [PubMed] [Google Scholar]


