Abstract
Saliva is a multilayered secretion. The quality of saliva is just as crucial as the quantity. Saliva is necessary for preserving the integrity of oral structures, personal connections, digestion, and acid–base balance. The acid–base balance in one's oral environment is always being challenged. It happens every time we eat a meal, and when microorganisms are present. At a pH of 5 or 5.5, the demineralization of the enamel and hard tooth structures occurs. This study aimed to raise awareness about the importance of acid–base balance of saliva in dental health. A self-structured questionnaire was prepared to assess the awareness on the importance of acid–base balance in maintaining oral health. The questionnaire consisted of 20 questions, and the results were plotted in a graph. The Chi-square test was employed for evaluating the data, which was done with SPSS software. The study indicated that 91.74% of the participants were aware of the salivary pH in case of healthy gingiva, 34.82% of the respondents were aware of the salivary pH in case of chronic gingivitis, and 20.33% of the respondents were aware of the salivary pH in case of chronic periodontitis. We also correlated our results with gender and year of study. Oral health plays a major role in identifying systemic diseases and hence enough knowledge about various aspects about the oral cavity and its manifestations needs to be created among dental students to ensure that they become efficient dental surgeons in the future. Even though a fair amount of people knew the pH of clinically healthy gingiva, most of them did not know the pH at which periodontitis or gingivitis was caused. Hence, creating awareness about this topic stands vital. Further studies are required for a better understanding of salivary components and how they affect the caries process. The utilization of modified oral molecules as medicinal agents could become a reality with this understanding. Our findings imply that being aware of dietary composition has an impact on acid–base balance. To maintain the correct acid–base balance, more awareness of protein consumption is required.
Keywords: Dental caries, innovative technology, novel method, periodontitis, pH, saliva
INTRODUCTION
Saliva is not a well-known body fluid. It is devoid of the realism of blood, the emotional appeal of tears, and the sincerity of sweat. Saliva is produced by glands that continuously bathe the oral mucosa.[1] It is necessary for preserving the health of mouth tissues. Less saliva production causes not only the rapid deterioration of dental health but also adversely affects the quality of life. A person with dry mouths has a hard time keeping their teeth clean and their dental caries progress quickly.[2]
The factors that favor mineralization can keep the enamel surface integrity as well as the intraoral capacity of mineralization has been increasing scientific interest for decades. At low pH, decay of tooth and enamel demineralization may occur. However, very less importance has been given to the reverse pattern of exchange of minerals inside the oral cavity, which is known as calculus formation. Previously, calculus was considered a key causative factor of periodontitis, however, the interest reduced later.[3] This may be that in experimental conditions, gingivitis can be produced by microbial plaque. Research in periodontics started focusing on periodontitis and microbiology was found to be generated by specific microbes.
There has been a link connecting high salivary pH with periodontitis. As a result, the current hypothesis is that periodontitis patients have a larger intraoral mineralization potential. Furthermore, when comparing periodontitis-affected people to periodontitis-free subjects, it is shown that certain mineralization-promoting factors are more evident in subjects affected by periodontitis. Caries and plaque mineral content have previously been demonstrated to have an inverse relationship. In addition, the concept of an indirect link between dental decay and periodontal disease was previously established.[4] The extensive experience in research and deep knowledge of our team resulted in publications of high quality.[5,6,7,8,9,10,11,12,13,14,15,16]
This study was designed to assess the awareness of the importance of acid–base balance in maintaining oral health and oral hygiene among 200 dental students.
MATERIALS AND METHODS
The research was carried out among dental students from several colleges. In Google Forms, a questionnaire was created. A simple random sampling method was used. Students from several colleges were issued the questionnaire. A signed consent form stating the willingness to participate in the survey was obtained from all the participants. Two hundred responses were received from students (68 boys and 132 girls) from various colleges. The awareness of dental students regarding the significance of acid–base balance of saliva to maintain healthy oral hygiene was assessed and analyzed based on the responses that we received through the questionnaire.
Statistical analysis
SPSS was used to import the data. SPSS version 19 (IBM, India) was used for the analysis. The Chi-square test and descriptive statistics were used to compare the various operations, in which supplemental use of local anesthetic was employed more frequently. The significance threshold was set at 0.05.
RESULTS
Based on the responses that we received through the questionnaire, the following results were formulated. The analyzed results were expressed as bar graphs [Figures 1-8].
Figure 1.
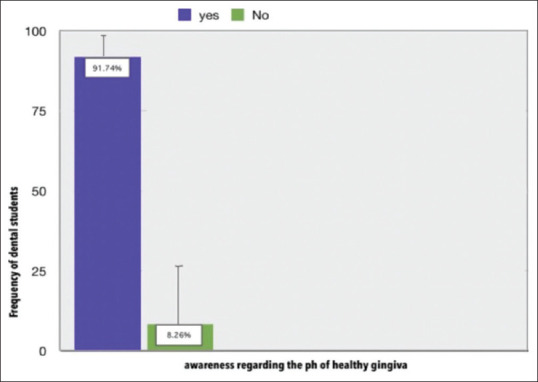
Graph represents the awareness regarding the pH of saliva in the case of clinically healthy gingiva being 7.06 ± 0.04 among dental students. X-axis indicates if the dental students who responded to the study were aware of pH of saliva in case of clinically healthy gingiva or not and Y-axis indicates the frequency of students who were aware and students who were not aware of the pH of clinically healthy gingiva
Figure 8.
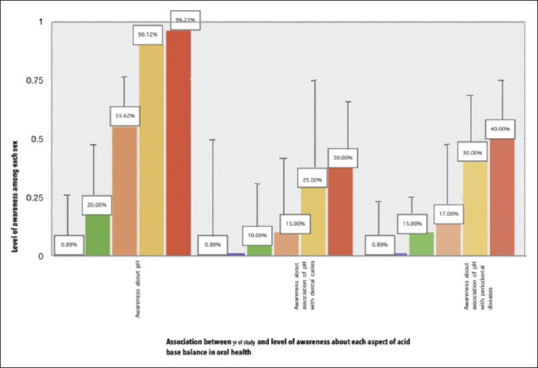
Graph represents the correlation of different aspects of saliva and oral health with year of study. X-axis indicates the influence of various aspects of acid–base imbalance of saliva on dental caries and periodontitis among dental students between different years of study. Y-axis indicates the level of awareness in each aspect of salivary acid–base balance between different years of study. Considering all the aspects of saliva and oral health, BDS interns were the most aware of all
Figure 2.
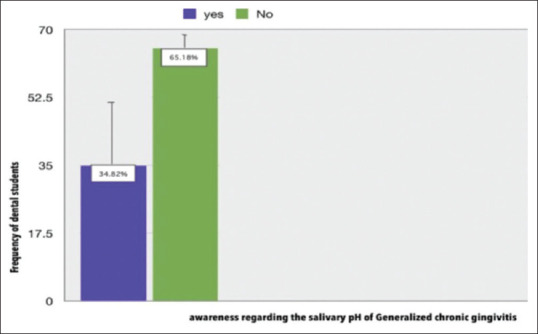
Graph represents the awareness regarding the pH of saliva in case of generalized chronic gingivitis being 7.24 ± 0.10 among dental students. X-axis indicates if the dental students who responded to the study were aware of pH of saliva in case of generalized chronic gingivitis or not and Y-axis indicates the frequency of students who were aware and students who were not aware of the pH of generalized chronic gingivitis
Figure 3.
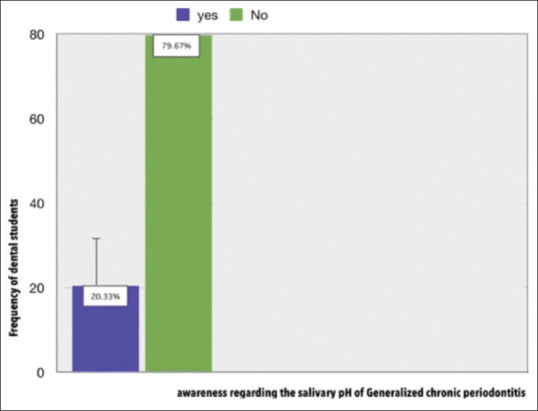
Graph represents the awareness regarding the pH of saliva in case of generalized chronic periodontitis being 6.85 ± 0.11 among dental students. X-axis indicates if the dental students who responded to the study were aware of pH of saliva in case of generalized chronic or not and Y-axis indicates the frequency of students who were aware and students who were not aware of the pH of Generalized chronic periodontitis
Figure 4.
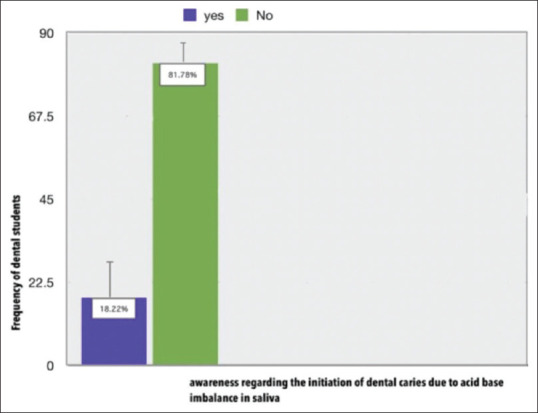
Graph represents the awareness regarding the effect of acid base imbalance of saliva on initiating dental caries. X-axis indicates if the dental students who responded to the study were aware of the effect of acid–base imbalance of saliva on initiating dental caries and Y-axis indicates the frequency of students who were aware and students who were not aware of the effect of acid–base imbalance of saliva on initiating dental caries
Figure 5.
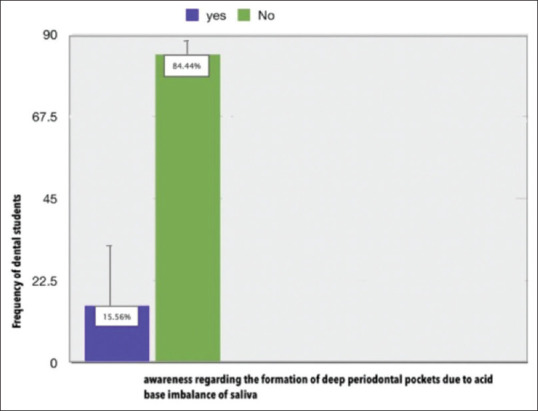
Graph represents the awareness regarding the effect of acid–base imbalance of saliva on the formation of deep periodontal pockets. X-axis indicates if the dental students who responded to the study were aware of the effect of acid–base imbalance of saliva on the formation of deep periodontal pockets and Y-axis indicates the frequency of students who were aware and students who were not aware of the effect of acid–base imbalance of saliva on the formation of deep periodontal pockets
Figure 6.
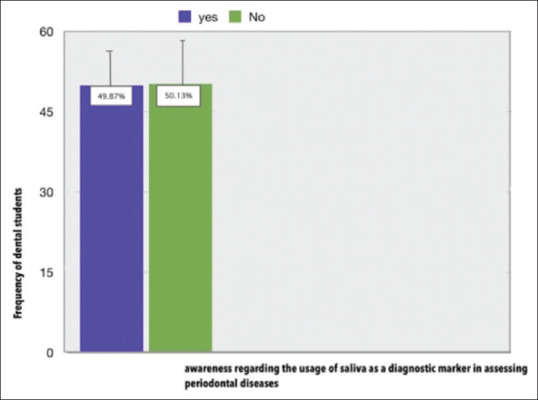
Graph represents the awareness regarding the usage of saliva as diagnostic marker in assessing periodontal disease. X-axis indicates if the dental students who responded to the study were aware of the usage of saliva as diagnostic marker in assessing periodontal disease and Y-axis indicates the frequency of students who were aware and students who were not aware of the usage of saliva as a diagnostic marker in assessing periodontal disease
Figure 7.
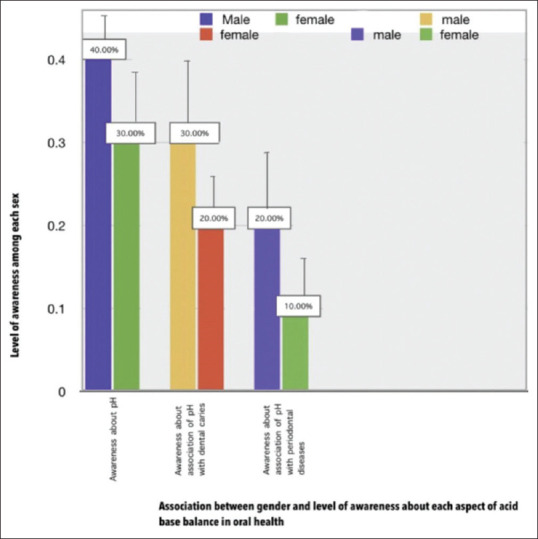
Graph represents the correlation of different aspects of saliva and oral health with gender. X-axis indicates the influence of various aspects of acid–base imbalance of saliva on dental caries and periodonitis among dental students between both the sex. Y-axis indicates the level of awareness in each aspect of salivary acid–base balance among each sex
DISCUSSION
The question of whether the two oral illnesses, periodontitis and dental caries, are affected by salivary pH has been debated for at least 50 years. High periodontal index scores in the caries-free population reflect an irregular change in salivary pH in these patients, according to epidemiologic studies.[17] Sewon et al. have demonstrated that the oral mineralization potential of saliva plays a vital role in periodontal health and illness in a series of research dating back to 1990.
Mineralization-promoting variables are known to help keep enamel surfaces in good shape, and intraoral mineralization capability has piqued scientists’ interest for decades. Enamel demineralization and dental deterioration may occur in the presence of a low plaque pH.[18]
According to the results of our current survey, dental students’ understanding of the importance of salivary pH and acid–base balance in sustaining oral health is still lacking.
This is in line with the findings of a study by Sewn et al., who found a link between high pH and periodontitis and assessed dentistry community awareness of the issue.[19]
We compared the levels of awareness among dentistry students on several aspects of acid–base balance in preserving oral health in our research.[20] Our findings included a statistical analysis of dental students’ knowledge of salivary pH, its impact on periodontal disorders, and its impact on dental caries progression. This is in line with the findings of research by Dong et al., which suggest that parameters such as the frequency of acidogenic episodes, rather than the degree of acidogenicity during any given episode, may be more relevant in caries progression.[21]
In our research, we discovered that the least amount of people is aware of the impact of acid–base balance on periodontal pockets.[22] This is in line with the findings of Axelsson and Lindhe, who investigated the impact of regulated oral hygiene techniques on caries and periodontal disease in adults and concluded that dental caries and periodontal disease are the outcomes of poor oral hygiene.
In this study, we looked at dentistry students’ lack of understanding of the impact of acid–base imbalance on the evolution of deep pockets into widespread chronic periodontal disease. This is in line with the findings of Sewn et al., who found that people with periodontitis have more intact molars and teeth than people without the condition.
As a result, the current hypothesis is that periodontitis patients have a larger intraoral mineralization potential. When comparing periodontitis-affected participants to periodontitis-free people, Sewn et al. 1990 found that certain mineralization-promoting factors are more prevalent in periodontitis-affected subjects.
We also correlated our findings with gender and year of study in this study. Furthermore, numerous studies imply that gender differences in caries resistance and the percentage of healthy teeth are related to the remineralization capability of their saliva.
Subjects having decreased salivary mineralization parameters, particularly salivary inorganic phosphate and calcium, less pH, and decreased flow rate, on the other hand, have an increased risk in developing dental caries because of the acidogenic property of the plaque and more readily enamel demineralization occurs, resulting in fewer intact teeth.
As a result of our findings, we believe that increasing awareness of the critical function of acid–base balance in preserving oral health is required, not only among dentistry professionals but also among the general public, to achieve a caries-free population in the future.[23]
CONCLUSION
The current study emphasizes the possible link between levels of awareness on salivary parameters, oral hygiene, and diseases including dental caries and periodontitis, which mostly affect humans and require future investigation. The utilization of modified oral molecules as medicinal agents could become a reality with this understanding. Our findings imply that being aware of dietary composition has an impact on acid–base balance. To maintain the correct acid–base balance, more awareness of protein consumption is required.
Financial support and sponsorship
This study was supported by the following agencies:
Saveetha Dental College
SIMATS, Saveetha University
3 states health care.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank all the students who participated in this survey.
REFERENCES
- 1.Gowdappa Doddawad V, Shivananda S, Madhu B, Gurupadayya BM, Vidya CS, Jayaraj BS. Assessing physical and chemical properties of saliva among tuberculosis patients on anti-tuberculosis treatment –An observational study. J Clin Tuberc Other Mycobact Dis. 2022;28:100322. doi: 10.1016/j.jctube.2022.100322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nimma V, Talla H, Poosa M, Gopaladas M, Meesala D, Jayanth L. Influence of hypertension on pH of saliva and flow rate in elder adults correlating with oral health status. J Clin Diagn Res. 2016;10:C34–6. doi: 10.7860/JCDR/2016/16799.8888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woelber JP, Al-Ahmad A, Alt KW. On the pathogenicity of the oral biofilm: A critical review from a biological, evolutionary, and nutritional point of view. Nutrients. 2022;14:2174. doi: 10.3390/nu14102174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim MJ. The relation of amount of the saliva secretion rate and saliva pH on taking 2 liters of water per a day. Korean Soc Oral Health Sci. 2019;7:70–6. [Google Scholar]
- 5.Veeraraghavan VP, Hussain S, Balakrishna JP, Dhawale L, Kullappan M, Ambrose JM, et al. Acomprehensive and critical review on ethnopharmacological importance of desert Truffles: Terfezia claveryi, Terfezia boudieri, and Tirmania nivea. Food Rev Int. 2021;37:1–20. [Google Scholar]
- 6.Sathya S, Ragul V, Veeraraghavan VP, Singh L, Niyas Ahamed MI. An in vitro study on hexavalent chromium [Cr (VI)] remediation using iron oxide nanoparticles based beads. Environ Nanotechnol Monit Manag. 2020;14:100333. [Google Scholar]
- 7.Yang Z, Pu M, Dong X, Ji F, Priya Veeraraghavan V, Yang H. Piperine loaded zinc oxide nanocomposite inhibits the PI3K/AKT/mTOR signaling pathway via attenuating the development of gastric carcinoma In vitro and in-vivo studies. Arab J Chem. 2020;13:5501–16. [Google Scholar]
- 8.Rajendran P, Alzahrani AM, Rengarajan T, Veeraraghavan VP, Krishna Mohan S. Consumption of reused vegetable oil intensifies BRCA1 mutations. Crit Rev Food Sci Nutr. 2022;62:1222–9. doi: 10.1080/10408398.2020.1837725. [DOI] [PubMed] [Google Scholar]
- 9.Barma MD, Muthupandiyan I, Samuel SR, Amaechi BT. Inhibition of Streptococcus mutans antioxidant property and cytotoxicity of novel nano-zinc oxide varnish. Arch Oral Biol. 2021;126:105132. doi: 10.1016/j.archoralbio.2021.105132. [DOI] [PubMed] [Google Scholar]
- 10.Samuel SR. Can 5-year-olds sensibly self-report the impact of developmental enamel defects on their quality of life? Int J Paediatr Dent. 2021;31:285–6. doi: 10.1111/ipd.12662. [DOI] [PubMed] [Google Scholar]
- 11.Samuel SR, Kuduruthullah S, Khair AM, Shayeb MA, Elkaseh A, Varma SR. Dental pain, parental SARS-CoV-2 fear and distress on quality of life of 2 to 6 year-old children during COVID-19. Int J Paediatr Dent. 2021;31:436–41. doi: 10.1111/ipd.12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang Y, Rajendran P, Veeraraghavan VP, Hussain S, Balakrishna JP, Chinnathambi A, et al. Osteogenic differentiation and mineralization potential of zine oxide nanoparticles from Scutellaria baicalensis on human osteoblast-like MG-63 cells. Mater Sci Eng C. 2021;119:111656. doi: 10.1016/j.msec.2020.111656. [DOI] [PubMed] [Google Scholar]
- 13.Veeraraghavan VP, Periadurai ND, Karunakaran T, Hussain S, Surapaneni KM, Jiao X. Green synthesis of silver nanoparticles from aqueous extract of Scutellaria barbata and coating on the cotton fabric for antimicrobial applications and wound healing activity in fibroblast cells (L929) Saudi J Biol Sci. 2021;28:3633–40. doi: 10.1016/j.sjbs.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mickymaray S, Alfaiz FA, Paramasivam A, Veeraraghavan VP, Periadurai ND, Surapaneni KM, et al. Rhaponticin suppresses osteosarcoma through the inhibition of PI3K-Akt-mTOR pathway. Saudi J Biol Sci. 2021;28:3641–9. doi: 10.1016/j.sjbs.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teja KV, Ramesh S. Is a filled lateral canal –A sign of superiority? J Dent Sci. 2020;15:562–3. doi: 10.1016/j.jds.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Theertha M, Sanju S, Priya VV, Jain P, Varma PK, Mony U. Innate lymphoid cells: Potent early mediators of the host immune response during sepsis. Cell Mol Immunol. 2020;17:1114–6. doi: 10.1038/s41423-020-0383-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boehlke C, Rupf S, Tenniswood M, Chittur SV, Hannig C, Zierau O. Caries and periodontitis associated bacteria are more abundant in human saliva compared to other great apes. Arch Oral Biol. 2020;111:104648. doi: 10.1016/j.archoralbio.2020.104648. [DOI] [PubMed] [Google Scholar]
- 18.Lingström P, Moynihan P. Nutrition, saliva, and oral health. Nutrition. 2003;19:567–9. doi: 10.1016/s0899-9007(03)00062-5. [DOI] [PubMed] [Google Scholar]
- 19.Xu F, Laguna L, Sarkar A. Aging-related changes in quantity and quality of saliva: Where do we stand in our understanding? Journal of Texture Studies. 2019;50:27–35. doi: 10.1111/jtxs.12356. [DOI] [PubMed] [Google Scholar]
- 20.Iorgulescu G. Saliva between normal and pathological. Important factors in determining systemic and oral health. J Med Life. 2009;2:303–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Atukorallaya DS, Ratnayake RK. Oral mucosa, saliva, and COVID-19 infection in oral health care. Front Med (Lausanne) 2021;8:656926. doi: 10.3389/fmed.2021.656926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mandal Y, Jha K, Jnaneswar A. Biomarkers in saliva as diagnostic tool in early diagnosis of oral submucous fibrosis. J Prim Care Dent Oral Health. 2021;2:8. [Google Scholar]
- 23.Oliveby A, Lagerlöf F, Ekstrand J, Dawes C. Influence of flow rate, pH and plasma fluoride concentrations on fluoride concentration in human parotid saliva. Arch Oral Biol. 1989;34:191–4. doi: 10.1016/0003-9969(89)90007-1. [DOI] [PubMed] [Google Scholar]


