Abstract
Background:
Hypertension (HTN) accounts for one in five deaths of American women. Major societies worldwide aim to make evidence-based recommendations for HTN management. Sex- or gender-based differences exist in epidemiology and management of HTN; in this study, we aimed to assess sex- and gender-based language in major society guidelines.
Materials and Methods:
We reviewed HTN guidelines from four societies: the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), the European Society of Cardiology (ESC), and the Eighth Joint National Committee (JNC8). We quantified the sex- and gender-based medicine (SGBM) content by word count in each guideline as well as identified the gender of guideline authors.
Results:
Two of the four HTN guidelines (ACC, ESC) included SGBM content. Of these two guidelines, there were variations in the quantity and depth of content coverage. Pregnancy had the highest word count found in both guidelines (422 words in ACC and 1,523 words in ESC), which represented 2.45% and 3.04% of the total words in each guideline, respectively. There was minimal coverage, if any, of any other life periods. The number of women authors did not impact the SGBM content within a given guideline.
Conclusions:
Current HTN management guidelines do not provide optimal guidance on sex- and gender-based differences. Inclusion of sex, gender identity, hormone therapy, pregnancy and lactation status, menopause, and advanced age in future research will be critical to bridge the current evidence gap. Guideline writing committees should include diverse perspectives, including cisgender and transgender persons from diverse racial and ethnic backgrounds.
Keywords: hypertension, sex, gender, disparity, guideline, women's health, transgender
Introduction
It has been estimated that up to 26% of the world's adult population has hypertension (HTN),1 and sex- or gender-based differences exist in the epidemiology and management of HTN.2–4 For example, there is a significant difference in the prevalence of HTN between men and women globally: 31% of men versus 25.3% of women carry the diagnosis of HTN.5 HTN prevalence also varies by geographic distribution; in 2010, the highest HTN prevalence for men was in Europe and Central Asia, reaching 38.8%, whereas the highest HTN prevalence for women was in sub-Saharan Africa, reaching 36.3%.5
This difference of incidence of HTN among men and women also varies by phase of life. The incidence of HTN is higher among men in younger age groups5; however, the incidence rate is higher among women after menopause.6,7 Estrogen has a protective effect on arterial stiffness; estrogen induces vasodilatation, inhibits vascular remodeling processes, and modulates specific pathways such as the renin–angiotensin aldosterone system and the sympathetic system.2 Given decline in estrogen levels in menopause, the higher incidence of HTN among menopausal women is not surprising.
HTN is a leading cause of morbidity and mortality, accounting for one in five deaths among American women,8,9 and HTN affects women in all phases of life. Certain sex-specific conditions, such as menopause, the use of hormonal contraception or hormone replacement therapy, and sex-specific disorders such as preeclampsia, are associated with a particular risk for HTN in women.10,11 In addition, there are specific characteristics relating to risk factors and the primary prevention of HTN in various populations of women: teenage and young adult women, pregnant women, women who use oral contraceptives, assisted reproductive technologies, or hormone replacement therapy, lactating women, and menopausal or older women.10–12 Specific modifiable risk factors for a lower risk of incident HTN have been described in a cohort of more than 83,000 women and include normal weight, physical exercise, correct dietary approach, modest alcohol intake, moderate use of analgesics, and intake of supplemental folic acid.13
Management of some of these modifiable risk factors of HTN has revealed sex- and/or gender-based differences. For example, dietary differences and lifestyle modifications in the treatment of HTN may have a different impact on men compared with women.14 In a study among young adults, alcohol consumption was identified as a risk factor for HTN in women but not in men.14 And, while high-salt diet has been associated with the risk of HTN in both men and women, another study revealed that salt sensitivity was associated with all-cause mortality in men but not in women.15 Furthermore, some data suggest that emotional dietary support from family members is associated with better adherence to short-term sodium restriction for African American girls compared with boys.16 Response to medications may also differ between men and women. Although efficacy in the prevention of cardiovascular outcomes does not seem to differ between men and women in large trials, calcium channel blockers appear to be particularly effective for blood pressure control in women.17
Whether women in past studies were universally cisgender (sex and gender concordance) is unknown due to lack of data collection of sex assigned at birth and of gender identity in most studies. While knowledge regarding risk of HTN for transgender individuals is limited, some existing data point to differences in the risk for cardiovascular outcomes in transgender (sex and gender discordance) individuals, highlighting the importance of better characterization of gender identity in research. A large cohort study using Behavioral Risk Factor Surveillance System data from 2014 to 2017 demonstrated that transgender men were twice as likely to have a history of myocardial infarction compared with cisgender men and four times as likely compared with cisgender women.18 Transgender women were twice as likely to have myocardial infarction compared with cisgender women, without an increased risk compared with cisgender men.
Reasons for this increased risk may be multifactorial. One study showed that transgender men on gender-affirming hormone therapy who reported greater stress had increased high-sensitivity C-reactive protein levels and reduced nocturnal blood pressure reduction.18 A systematic review of the effects of testosterone therapy on transgender men found an increased risk for HTN in some studies and no effect in other studies.19 Another observational study showed a protective effect of progestin on transgender women.20 Overall, lack of consistent data collection of gender identity and exogenous hormone therapy in existing research limits generalizable knowledge to inform cardiovascular care for transgender and nonbinary individuals. For the remainder of the article, we will only use the terms cisgender or transgender in describing the existing literature when clearly reported.
Major societies worldwide aim to make evidence-based recommendations on the management of HTN. The current article examines existing HTN guidelines and quantifies sex- and gender-specific language use and content in the prevention, screening, and management of hypertensive disorders in these guidelines. We hypothesized that use of the terms, sex and/or gender, as well as related evidence would be minimal despite the known sex and/or gender differences in the prevalence of HTN, risk factors, and response to therapy. Additionally, we sought to determine if presence or proportion of female guideline authors influenced the presence of sex- and/or gender-specific guidance.
Materials and Methods
Authors of this article are members of the Sex and Gender Health Collaborative (SGHC) Scholarship Committee. The SGHC exists within the American Medical Women's Association (AMWA) and was created to foster a sex and gender approach to education and clinical practice. The Scholarship Committee is made up of 11 women health care providers and/or researchers (8 physicians, 1 pharmacist, and 2 PhD researcher) whose goal is to further scholarship in this area.
Before undertaking this review, the scholarship committee met several times and outlined the process for review. Our authors include physicians in the fields of emergency medicine (T.E.M. and A.J.M.), family medicine and public health (M.H.), internal medicine (M.R., I.T., and J.T.), pulmonary medicine (G.B.), and nephrology (B.O.M.) and have expertise in managing patients with cardiovascular disease. In addition, all SGHC scholarship committee authors are national content experts in sex- and gender-based medicine and have all participated actively in continuing medical education on the importance of sex and gender content in medical education and clinical practice guidelines.
Following a focused review of the literature, study authors came to an agreement on nine key topic areas: prevention/screening, presentation/diagnosis, chronic treatment/management, emergency/urgency treatment, outcomes related to chronic HTN, outcomes related to emergency HTN, pregnancy, lactation, and transgender care. We identified whether sex- and gender-based medicine (SGBM) content appeared in the most recently published HTN guidelines from four separate major specialty societies: the 2018 American College of Cardiology (ACC),21 the 2013 American College of Emergency Physicians (ACEP),22 the 2018 European Society of Cardiology (ESC),23 and the 2014 Eighth Joint National Committee (JNC8).24
We described and quantified the SGBM content in each of the four guidelines. First, each of the guidelines was reviewed for exact matches of the nine content areas as well as any content related to women, female gender, pregnant, or lactating persons. For each of the nine SGBM topic areas, the total number of words pertaining to that topic within each guideline was calculated by two study authors per guideline (ACC—G.B. and B.O.M.; ACEP—T.E.M. and A.J.M.; JNC8—I.T. and J.T.; ESC—M.H. and M.R.). Each pair of authors independently reviewed each guideline to minimize any inaccuracies due to human error and to avoid potential reviewer bias, although reviewer bias was not anticipated to be an issue given the inherent objective nature of our review criteria.
Before statistical analysis, the two reviewers assigned to a given guideline discussed and addressed any discrepancies in their data review. Then, for each of the four guidelines, descriptive statistics (median values, ranges) were calculated for SGBM word count across all nine topic areas. Median values and ranges, rather than means, were used due to the small number of word counts that were identified in the nine areas. Then, for each of the nine topic areas, total word counts were calculated for all four guidelines. The percentage of total word count dedicated to the SGBM content for each topic area was also calculated.
We also collected data on author gender. Each specialty society lists the authors of its guidelines. We performed an internet search on each author and categorized authors as women or men from the use of pronouns in any publications by and/or about a given author (he/his/his or she/her/hers), LinkedIn Profiles where authors may have displayed stated gender and or preferred pronouns, and gender expression from profile photos. Consensus by this article's authors was utilized when gender was not clear from the above sources. The percentage of women authors for each of the four guidelines was calculated and reported.
All summary statistics and graphs were conducted in R version 4.1.1.25 Comparisons in percentages of women authors were conducted using comparisons of proportions test.
Results
Of the four guidelines we selected for inclusion in this study, two guidelines did not mention sex or gender at all (ACEP, JNC8). Of the two guidelines that included the SGBM content (ACC, ESC), the word count for subtopic areas ranged from 72 to 422 (median 147) for ACC and from 48 to 1,563 (median 60) for ESC (Table 1).
Table 1.
Number of Words Related to Sex- and Gender-Based Content by Category and Guideline
| ACC | ACEP | JNC8 | ESC | Total | |
|---|---|---|---|---|---|
| Prevention/screening | 72 | 0 | 0 | 50 | 122 |
| Presentation/diagnosis | 93 | 0 | 0 | 95 | 188 |
| Chronic treatment/management | 250 | 0 | 0 | 60 | 310 |
| Emergency/urgency treatment/management | 0 | 0 | 0 | 0 | 0 |
| Outcomes with chronic HTN | 147 | 0 | 0 | 0 | 0 |
| Outcomes with emergent/urgent HTN | 0 | 0 | 0 | 0 | 0 |
| Pregnancy | 422 | 0 | 0 | 1563 | 1985 |
| Lactation | 0 | 0 | 0 | 48 | 48 |
| Trans health care | 0 | 0 | 0 | 0 | 0 |
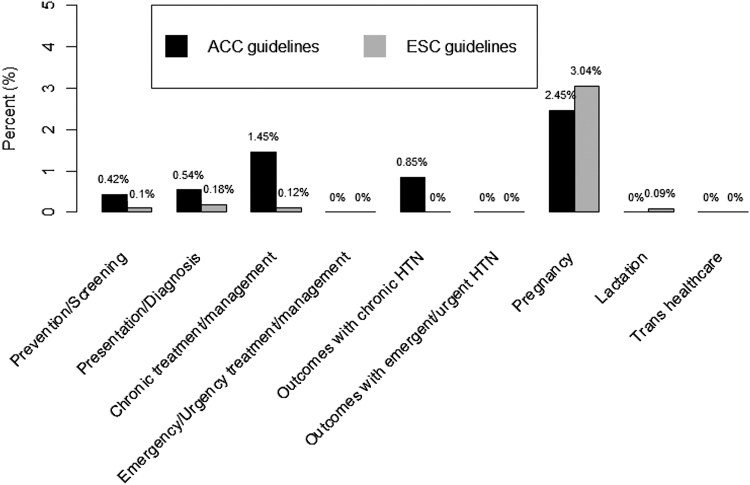
Of the two guidelines which included the SGBM content, there were variations in the quantity and depth of content coverage (Table 1). Pregnancy was the category with the highest word count found in both the ACC (422) and ESC guidelines (1,523), which represented 2.45% and 3.04% of the total number of words in the ACC and ESC guidelines, respectively. The next highest word count for the SGBM content was in the category of chronic treatment and management of HTN (250 words in ACC, 60 words in ESC), which represented 1.45% and 0.12% of the total words in the ACC and ESC guidelines, respectively. A discussion of lactation was only mentioned in one of the four guidelines (ESC) and only included 45 words, despite potential nuances in pharmacotherapy in lactating women. The remaining categories and total word counts are presented in Table 1, and the percentages of word count for each category are presented in Figure 1.
FIG. 1.
Percentage of word count of the SGBM content for ACC21 and ESC guidelines.23 ACC, American College of Cardiology; ESC, European Society of Cardiology; SGBM, sex- and gender-based medicine.
The percentage of women authors ranged from 0% (ACEP writing group) to 33% (ACEP oversight committee)22 (Table 2). The two guidelines that did have the SGBM content (ACC and ESC) had 0% and 10.7% women authors, respectively, whereas the two guidelines that did not have any SGBM content (JNC8 and ACEP) had 23.5% and 28.6% women authors, respectively. There was no statistically significant association between the percentage of women authors and the presence of SGBM content. All pairwise comparisons of the percentages of women authors between guidelines were not statistically significant, with all p > 0.05 (data not shown).
Table 2.
Number of Total and Female Authors per Guideline
| Guideline | Total no. of authors | No. of female authors | Percentage of female authors |
|---|---|---|---|
| ESC | 28 | 3 | 10.7 |
| ACC | 21 | 6 | 28.6 |
| JNC8 | 17 | 4 | 23.5 |
| ACEP writing committee | 5 | 0 | 0 |
| ACEP oversight committee | 21 | 7 | 33.3 |
Discussion
This study is the first to our knowledge to examine the SGBM content in national and international guidelines on the management of HTN in adults. It is noteworthy that only two of the four guidelines (ACC, ACEP, JNC8, and ESC) reviewed included SGBM language pertaining to women and HTN. In addition, in the two guidelines that did include SGBM guidelines specific to women (ACC, ESC), the percentage of the SGBM content was quite small (≤3%).
Not surprisingly, the content area with the highest percentage of content and greatest area of SGBM inclusion was pregnancy. Hypertensive disorders of pregnancy are now a recognized risk factor for long-term cardiovascular disease and chronic HTN.26 Furthermore, the management of HTN in pregnancy is unique in terms of choice of medications, target blood pressure, the impact of delivery on management of HTN, and the potential impact of HTN and blood pressure control on perinatal maternal and fetal/neonatal outcomes.
Despite potential nuances in pharmacotherapy in lactating women, a discussion of lactation was only mentioned in one of the four guidelines (ESC) and only included 45 words. There was no mention of SGBM as it pertains to the care of transgender persons on hormonal therapy in any of the guidelines.
There are implications of the lack of SGBM content beyond the fact that there are no/limited guidelines that are specific for cisgender women or transgender persons. Guidelines are often used by insurance organizations and companies to dictate what is considered appropriate care and coverage for health services. Guidelines are also typically used to develop “standard of care” protocols in medical centers and other professional organizations and therefore are often followed very closely by practicing health care workers.27 Guidelines and professional organization recommendations are also often used to identify knowledge gaps and drive research and further studies.
The lack of more specific SGBM guidelines by these respected and widely followed medical organizations creates challenges for health care providers and researchers at all levels.28 The United States Preventive Services Task Force (USPSTF) recently published a recommended approach to addressing sex and gender when making recommendations for clinical preventive services28; we suggest applying a similar approach to clinical management guidelines.
Many knowledge gaps persist, including the contribution of hypertensive disorders in pregnancy to cardiovascular disease risk, the contribution of hormone replacement to blood pressure, and blood pressure targets for older women. It would be appropriate to have the SGBM content that is not only gender-specific but also age-specific in cisgender women/those assigned female at birth given that the prevalence of HTN is higher in perimenopausal and menopausal women. Future research should include diverse populations and standard collection of data including sex assigned at birth, gender identity, exogenous hormone use, current pregnancy and gestational timing, and lactation status to address gaps in the current evidence base. Future research should also report on heterogeneity of prevalence, risk reduction strategies (i.e., lifestyle, pharmacotherapeutic), screening (i.e., ideal age), diagnosis, treatment (i.e., pharmacotherapeutic and pharmacodynamic differences in medication use, adherence), treatment effects, and patient outcomes stratified by sex and gender.
The proportion of women authors of a given guideline was not associated with the presence of sex- and gender-specific content, which is similar to findings previously published by Tong et al.29 Sardar et al. reviewed the representation of women in the ACC/American Heart Association Guideline Writing Committees and highlighted the importance of including women authors in cardiology guidelines.30 Specifically, authors emphasized that including more women authors has the potential to help identify knowledge gaps pertaining to sex- or gender-specific data, diversify the perspective of the writing group, and increase attention to the need for recommendations specific to women. We propose including a specific section on sex- and gender-related content in every clinical practice guideline, so that readers are aware that sex- and gender-related issues were considered.
A strength of this study is the multidisciplinary perspectives of the study team and their expertise in sex and gender medicine. The study is descriptive in nature and is focused on the presence or absence of sex- and/or gender-specific information; thus, no statistical associations can be extrapolated.
Conclusions
Overall, our study found a considerable lack of sex- and gender-based content in HTN management guidelines. Clinical guidelines currently do not provide optimal guidance for cisgender women or transgender persons. Insurance plans are unlikely to cover services that are not included in guidelines, and clinicians cannot provide appropriate care management without evidence-based guidance. Thus, inclusion of sex, gender identity, hormone therapy, pregnancy, and lactation status in future research will be critical to bridge the current evidence gap. Finally, representation matters; our findings point to continued gender disparities in authorship and suggest that changes need to be made with regard to the inclusion of diverse authors in clinical practice guideline writing committees. It is critical that guideline committees include diverse perspectives, including those of cisgender and transgender women and men from diverse racial and ethnic backgrounds.
Acknowledgment
The authors of this article are members of the Scholarship Committee of the Sex and Gender Health Collaborative of the American Medical Women's Association.
Authors' Contributions
All authors affirm to participating in the writing and reviewing of this article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
T.E.M. is funded by a grant from the National Heart, Lung, and Blood Institute (NHLBI). G.B. has received grant funding from the National Heart, Lung, and Blood Institute (NHLBI). HL-R01130702. M.H. is currently funded by the Health Resources and Services Administration (HRSA) GRANT #U1QHP28730. Mandi Pratt-Chapman Currently funded by CDC U01DP00639, CDC NU58DP00646, NCI 5R01CA203604-REVISED, NCI R25CA265802, NCI U24 CA271246, and NIH R34MH128046.
References
- 1. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 2. Di Giosia P, Giorgini P, Stamerra CA, Petrarca M, Ferri C, Sahebkar A. Gender Differences in epidemiology, pathophysiology, and treatment of hypertension. Curr Atheroscler Rep 2018;20:13. [DOI] [PubMed] [Google Scholar]
- 3. Doumas M, Papademetriou V, Faselis C, Kokkinos P. Gender differences in hypertension: Myths and reality. Curr Hypertens Rep 2013;15:321–330. [DOI] [PubMed] [Google Scholar]
- 4. Song JJ, Ma Z, Wang J, Chen LX, Zhong JC. Gender differences in hypertension. J Cardiovasc Transl Res 2020;13:47–54. [DOI] [PubMed] [Google Scholar]
- 5. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: Analysis of the 2010–2014 Korea National Health and Nutrition Examination Survey. PLoS One 2017;12:e0178334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Asgari S, Moazzeni SS, Azizi F, et al. Sex-specific incidence rates and risk factors for hypertension during 13 years of follow-up: The Tehran lipid and glucose study. Glob Heart 2020;15:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation 2016;133:187–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics—2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:480–486. [DOI] [PubMed] [Google Scholar]
- 10. Brahmbhatt Y, Gupta M, Hamrahian S. Hypertension in premenopausal and postmenopausal women. Curr Hypertens Rep 2019;21:74. [DOI] [PubMed] [Google Scholar]
- 11. Turbeville HR, Sasser JM. Preeclampsia beyond pregnancy: Long-term consequences for mother and child. Am J Physiol Renal Physiol 2020;318:F1315–F1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wenger NK, Arnold A, Bairey Merz CN, et al. Hypertension across a woman's life cycle. J Am Coll Cardiol 2018;71:1797–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA 2009;302:401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim JS, Kim CG. Gender differences in hypertension treatment and control in young adults. J Nurs Res 2020;28:e88. [DOI] [PubMed] [Google Scholar]
- 15. Bursztyn M, Ben-Dov IZ. Sex differences in salt-sensitivity risk approximated from ambulatory blood pressure monitoring and mortality. J Hypertens 2013;31:900–905. [DOI] [PubMed] [Google Scholar]
- 16. Wilson DK, Ampey-Thornhill G. The role of gender and family support on dietary compliance in an African American adolescent hypertension prevention study. Ann Behav Med 2001;23:59–67. [DOI] [PubMed] [Google Scholar]
- 17. Muiesan ML, Salvetti M, Rosei CA, Paini A. Gender differences in antihypertensive treatment: Myths or legends? High Blood Press Cardiovasc Prev 2016;23:105–113. [DOI] [PubMed] [Google Scholar]
- 18. Dubois LZ. Associations between transition-specific stress experience, nocturnal decline in ambulatory blood pressure, and C-reactive protein levels among transgender men. Am J Hum Biol 2012;24:52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Velho I, Fighera TM, Ziegelmann PK, Spritzer PM. Effects of testosterone therapy on BMI, blood pressure, and laboratory profile of transgender men: A systematic review. Andrology 2017;5:881–888. [DOI] [PubMed] [Google Scholar]
- 20. Pyra M, Casimiro I, Rusie L, et al. An observational study of hypertension and thromboembolism among transgender patients using gender-affirming hormone therapy. Transgend Health 2020;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 22. Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM. Clinical policy: Critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013;62:59–68. [DOI] [PubMed] [Google Scholar]
- 23. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Eur Heart J 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 24. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 25. R Core Team: R. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2021. [Google Scholar]
- 26. Paauw ND, Lely AT. Cardiovascular sequels during and after preeclampsia. Adv Exp Med Biol 2018;1065:455–470. [DOI] [PubMed] [Google Scholar]
- 27. Spellberg B, Wright WF, Shaneyfelt T, Centor RM. The future of medical guidelines: Standardizing clinical care with the humility of uncertainty. Ann Intern Med 2021;174:1740–1742. [DOI] [PubMed] [Google Scholar]
- 28. Caughey AB, Krist AH, Wolff TA, et al. USPSTF approach to addressing sex and gender when making recommendations for clinical preventive services. JAMA 2021;326:1953–1961. [DOI] [PubMed] [Google Scholar]
- 29. Tong I, Griffin B, Trott J, Romano M, Stein AB, Madsen TE. The proportion of women authors and the inclusion of sex and gender content among the American College of Cardiology Clinical Practice Guidelines, 2008–2018. J Womens Health (Larchmt) 2021;30:1616–1625. [DOI] [PubMed] [Google Scholar]
- 30. Sardar P, Kundu A, Poppas A, Abbott JD. Representation of women in American College of Cardiology/American Heart Association Guideline Writing Committees. J Am Coll Cardiol 2018;72:464–466. [DOI] [PubMed] [Google Scholar]