Abstract
Background:
Patients with limited English proficiency (LEP) experience lower quality end-of-life (EOL) care. This inequity may have been exacerbated during the COVID-19 pandemic.
Objective:
Compare health care utilization, EOL, and palliative care outcomes between COVID-19 decedents with and without LEP during the pandemic's first wave in Massachusetts.
Methods:
Retrospective cohort study of adult inpatients who died from COVID-19 between February 18, 2020 and May 18, 2020 at two academic and four community hospitals within a greater Boston health care system. We performed multivariable regression adjusting for patient sociodemographic variables and hospital characteristics. Primary outcome was place of death (intensive care unit [ICU] vs. non-ICU). Secondary outcomes included hospital and ICU length of stay and time to initial palliative care consultation.
Results:
Among 337 patients, 89 (26.4%) had LEP and 248 (73.6%) were English proficient. Patients with LEP were less often white (24 [27.0%] vs. 193 [77.8%]; p < 0.001); were more often Hispanic or Latinx (40 [45.0%] vs. 13 [5.2%]; p < 0.001); and less often had a medical order for life-sustaining treatment (MOLST) on admission (15 [16.9%] vs. 120 [48.4%]; p < 0.001) versus patients with English proficiency. In the multivariable analyses, LEP was not independently associated with ICU death, ICU length of stay, or time to palliative care consultation, but was independently associated with increased hospital length of stay (mean difference 4.12 days; 95% CI, 1.72–6.53; p < 0.001).
Conclusions:
Inpatient COVID-19 decedents with LEP were not at increased risk of an ICU death, but were associated with an increased hospital length of stay versus inpatient COVID-19 decedents with English proficiency.
Keywords: coronavirus-19, COVID-19, limited English proficiency, palliative care
Introduction
The coronavirus-19 (COVID-19) pandemic disproportionately impacted historically minoritized racial and ethnic groups, especially during the early stages of the pandemic.1–5 Studies have shown that U.S. communities with a larger proportion of foreign-born noncitizens, especially monolingual Spanish speakers in the Latinx community, experienced higher COVID-19 infection rates.3,6 Consequently, patients with limited English proficiency (LEP) sustained higher rates of COVID-19-related hospitalization and mortality,7 but little is known about end-of-life (EOL) care and palliative care outcomes among COVID-19 decedents with LEP.
Before the pandemic, LEP was associated with lower quality EOL care. Patients with LEP were more likely to receive intensive life-sustaining treatment at EOL when admitted to the intensive care unit (ICU),8 receive worse symptom management,9 experience lower quality serious illness communication,10,11 and report poorer prognostic awareness and inadequate understanding of their diagnosis.9 In addition, approximately 30% of U.S. health care systems lacked adequate language services,12 and many medical interpreters reported feeling uncomfortable and inadequately trained to interpret EOL communication.13
The COVID-19 pandemic may have further exacerbated health care inequities among patients with LEP at the EOL for multiple reasons, including increased demand for interpreter services, lack of clinician linguistic diversity, and communication barriers resulting from infection control practices.14–16 Although highlighted in the lay press, little has been published in the academic literature about EOL care quality among COVID-19 patients with LEP.16 Therefore, we conducted a retrospective cohort study to identify differences in health care utilization, palliative care, and EOL outcomes between COVID-19 patients with LEP and COVID-19 patients with English proficiency who died in the hospital during the pandemic's first wave.
Materials and Methods
Study design, setting, and participants
We performed a retrospective cohort study of adult (≥18 years old) inpatients who died of COVID-19 at two tertiary academic hospitals and four community hospitals within a greater Boston health care system during the pandemic's first wave. We analyzed inpatient deaths between February 18, 2020 and May 18, 2020 when COVID-19 deaths reached its apex in Massachusetts.17 We identified the COVID-19 decedent cohort by combining manual chart review and querying the electronic health record (EHR) using a data extraction tool called Epic Reporting Workbench. Two reviewers (I.S.C. and S.M.S.) conducted manual chart reviews to confirm cause of death and excluded patients who died in the outpatient setting or patients with unknown primary language (Fig. 1).
FIG. 1.
Flow diagram for patient inclusion criteria.
Our study focused on inpatient deaths since most COVID-19 deaths in the United States occurred in the hospital.18,19 LEP was the primary exposure and was defined as a self-reported primary language other than English listed in the EHR.8,20–22 The Mass General Brigham Institutional Review Board approved the study as nonhuman subjects research.
Outcomes
Primary and secondary outcomes are based on population-based quality indicators for EOL care.23,24 The primary outcome was place of death (ICU vs. non-ICU). For our primary outcome, we dichotomized place of death variables into ICU vs. non-ICU by consolidating the categories (inpatient palliative care, general ward, and emergency room) into a single non-ICU variable, and we excluded observations that had an unclear location. Secondary outcomes included hospital and ICU length of stay, time to initial goals-of-care documentation and palliative care consultation, mechanical ventilator or extracorporeal membrane oxygenation (ECMO) utilization, cardiopulmonary resuscitation (CPR) attempts, changes in code status from time of admission to time of death, and time from initial palliative care consultation to time of death.
Data collection
From the EHR, we extracted patient demographic variables (age, sex, race, ethnicity, insurance status, religion, self-reported primary language, body mass index [BMI], smoking history, comorbidities), hospital characteristics (academic vs. community), and health care utilization outcomes (hospital and ICU length of stay). We conducted a manual chart review of the patient's terminal hospitalization to collect the remaining patient variables of interest: completed medical orders for life-sustaining treatment (MOLST) on date of admission (i.e., hospital day 0), life-sustaining treatment utilization (mechanical ventilation and ECMO initiation and discontinuation and any CPR attempts), code status on admission and at time of death, and palliative care delivery outcomes (timing of inpatient palliative care consultation and goals-of-care documentation).
We constructed a keyword library to identify goals-of-care documentation by searching for keywords and abbreviations using a free-text search function in the EHR. This keyword library is partially based on a previously validated taxonomy25 and the presence of a structured module in the electronic health care record designed to capture advance care planning (ACP) documentation that uses the Serious Illness Conversation Guide as a template.26,27 Reviewers conducted a structured query for the following terms for each patient: “goals,” “healthcare proxy,” “HCP,” “advanced care planning,” “ACP,” “serious illness,” “discuss,” “prefer,” “conversation,” “home,” “hospice,” “nursing home,” “long term care,” “assisted living,” “skilled nursing facility,” “SNF,” “rehab,” and “dispo.”
Reviewers then identified progress notes that addressed at least one of the following domains: patient values and goals; prognosis or illness understanding; EOL care planning; or clarifying or expressing code status preferences; or desire for other life-sustaining treatments or procedures.28 If the keyword search did not generate any relevant documentation, the reviewer would filter notes by author type (i.e., palliative care, social work, chaplain, and case management). If the reviewers could not identify the relevant documentation after filtering notes, then they would indicate “no documentation.”
In the setting of ambiguous documentation during the manual chart review (e.g., whether a progress note reflected an actual goals-of-care documentation), the two reviewers (I.S.C. and S.M.S.) discussed the case to achieve consensus. If consensus could not be reached, then a third reviewer (D.M.L.) adjudicated.
Statistical methods
We reported numbers (percentages) for categorical variables and investigated associations between categorical variables using Pearson's chi-squared test or Fisher's exact test when cell counts were <5. We reported continuous variables as medians (interquartile ranges [IQRs]) and used Wilcoxon rank-sum tests to assess for associations. A two-sided p value <0.05 was considered statistically significant.
We conducted multivariable analyses of binary outcomes and continuous outcomes using a logistic regression model and linear regression models, respectively. We only performed multivariable analyses on outcomes that were statistically significant on univariable analyses and had sufficient sample sizes that precluded model overfitting.29 We conducted a univariable screen to identify asymmetry in patient and hospital characteristics between patients with LEP and English proficiency and included variables in the model if p < 0.05. Based on these criteria, we conducted multivariable analyses on our primary outcome (place of death) and secondary outcomes (time to initial palliative care consultation, hospital length of stay, and ICU length of stay).
To prevent model overfitting, we also combined subcategories with low cell sizes of the following variables: race, insurance, and religion. For race, we combined Asian, American Indian, and Other into a single variable Other. For insurance, we combined Self-Pay, Dual Coverage, and Other into the variable Other. For religion, we combined Muslim, Jewish, Buddhist, Not Affiliated, No Preference, or Other into the variable non-Christian.
Historically minoritized racial, ethnic, and linguistic groups have reported lower quality care than whites,30 and patient-reported primary language is a known effect modifier on race and health care quality.31,32 Therefore, we conducted sensitivity analyses separately examining race and ethnicity as an interaction term with primary language to determine if there was effect modification by race, ethnicity, and language on the primary outcome. We performed statistical analyses using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Patient characteristics
Among 359 patients who died of COVID-19 from February 18, 2020 to May 18, 2020, we identified 343 patients who died in the hospital and excluded 6 patients due to unknown self-reported primary language (Fig. 1). The final sample included 337 patients total, of which 89 (26.4%) patients had LEP, and 248 (73.6%) were English proficient (Table 1). Most patients with LEP spoke Spanish (44 [49.4%]), Haitian-Creole (14 [15.7%]), and Russian (11 [12.4%]).
Table 1.
Patient Characteristics of COVID-19 Inpatient Decedents by English Proficiency Status
| Total deaths (n = 337) | English proficient (n = 248) | LEP (n = 89) | p Valuea | |
|---|---|---|---|---|
| Age, median (IQR), years | 77.5 (68.0–87.3) | 77.3 (67.8–88.0) | 77.9 (68.9–85.4) | 0.59 |
| Male | 194 (57.6) | 147 (59.3) | 47 (52.8) | 0.29 |
| Race | <0.001 | |||
| White | 217 (64.4) | 193 (77.8) | 24 (27.0) | |
| Black | 58 (17.2) | 36 (14.5) | 22 (24.7) | |
| Asian | 9 (2.7) | 2 (0.8) | 7 (7.9) | |
| Otherb | 38 (11.3) | 9 (3.6) | 29 (32.6) | |
| Unknown | 15 (4.5) | 8 (3.2) | 7 (7.9) | |
| Ethnicity | <0.001 | |||
| Hispanic or Latinx | 53 (15.7) | 13 (5.2) | 40 (45.0) | |
| Non-Hispanic | 261 (77.5) | 217 (87.5) | 44 (49.4) | |
| Unknown | 23 (6.8) | 18 (7.3) | 5 (5.6) | |
| Primary language | <0.001 | |||
| English | 248 (73.6) | 248 (100.0) | 0 (0) | |
| Spanish | 44 (13.1) | 0 (0) | 44 (49.4) | |
| Haitian Creole | 14 (4.2) | 0 (0) | 14 (15.7) | |
| Russian | 11 (3.3) | 0 (0) | 11 (12.4) | |
| Portuguese | 3 (0.9) | 0 (0) | 3 (3.4) | |
| Italian | 3 (0.9) | 0 (0) | 3 (3.4) | |
| Chinese-Cantonese | 3 (0.9) | 0 (0) | 3 (3.4) | |
| Vietnamese | 3 (0.9) | 0 (0) | 3 (3.4) | |
| Portuguese Creole | 2 (0.6) | 0 (0) | 2 (2.2) | |
| Khmer | 2 (0.6) | 0 (0) | 2 (2.2) | |
| French | 1 (0.3) | 0 (0) | 1 (1.1) | |
| Tagalog | 1 (0.3) | 0 (0) | 1 (1.1) | |
| Somali | 1 (0.3) | 0 (0) | 1 (1.1) | |
| Polish | 1 (0.3) | 0 (0) | 1 (1.1) | |
| Insurance | <0.001 | |||
| Medicare | 213 (63.2) | 182 (73.4) | 31 (34.8) | |
| Medicaid | 32 (9.5) | 17 (6.9) | 15 (16.9) | |
| Private | 25 (7.4) | 18 (7.3) | 7 (7.9) | |
| Self-pay | 3 (0.9) | 2 (0.8) | 1 (1.1) | |
| Dual coverage | 60 (17.8) | 26 (10.5) | 34 (38.2) | |
| Other | 4 (1.2) | 3 (1.2) | 1 (1.1) | |
| Religion | 0.002 | |||
| Christian | 248 (73.6) | 178 (71.8) | 70 (78.7) | |
| Muslim | 3 (0.9) | 2 (0.8) | 1 (1.1) | |
| Jewish | 24 (7.1) | 18 (7.3) | 6 (6.7) | |
| Buddhist | 3 (0.9) | 0 (0) | 3 (3.4) | |
| Otherc | 46 (13.7) | 42 (16.9) | 4 (4.5) | |
| Unknown | 13 (3.9) | 8 (3.2) | 5 (5.6) | |
| Weightd | 0.70 | |||
| Obese (35 > BMI ≥ 30) | 57 (17.3) | 43 (17.8) | 14 (16.1) | |
| Morbidly obese (BMI ≥ 35) | 41 (12.5) | 32 (13.2) | 9 (10.3) | |
| Smoking history | <0.001 | |||
| Positive historye | 143 (42.4) | 127 (51.2) | 16 (17.9) | |
| Never smoker | 129 (38.3) | 81 (32.7) | 48 (53.9) | |
| Unknown | 65 (19.3) | 40 (16.1) | 25 (28.1) | |
| Comorbidities | ||||
| Coronary artery disease | 105 (31.2) | 84 (33.9) | 21 (23.6) | 0.07 |
| CHF | 97 (28.8) | 79 (31.9) | 18 (20.2) | 0.04 |
| Hypertension | 268 (79.5) | 198 (79.8) | 70 (78.7) | 0.81 |
| COPD or asthma | 88 (26.1) | 73 (29.4) | 15 (16.9) | 0.02 |
| Chronic kidney disease | 160 (47.5) | 125 (50.4) | 35 (39.3) | 0.07 |
| Cirrhosis | 11 (3.2) | 9 (3.6) | 2 (2.3) | 0.73 |
| Diabetes mellitus | 150 (44.5) | 104 (41.9) | 46 (51.7) | 0.11 |
| Active malignancy | 32 (9.5) | 23 (9.3) | 9 (10.1) | 0.82 |
| Dementia | 132 (39.2) | 98 (39.5) | 34 (38.2) | 0.83 |
| MOLST on admission | <0.001 | |||
| DNR/DNI | 80 (23.7) | 72 (29.0) | 8 (9.0) | |
| Full code | 43 (12.8) | 36 (14.5) | 7 (7.9) | |
| Partial DNR | 12 (3.6) | 12 (4.8) | 0 (0) | |
| None | 202 (60.0) | 128 (51.6) | 74 (83.2) |
Data are expressed as n (%) unless otherwise indicated.
Univariable comparison using Pearson's chi-squared test or Fisher's exact test when cell counts were <5 for categorical variables and Wilcoxon rank-sum test for continuous variables.
Includes American Indian and Other.
Includes Not Affiliated, No preference, or Other.
Weight data for eight patients are missing.
Includes former and current smokers.
BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; DNR, do-not-resuscitate, DNI, do-not-intubate; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range; LEP, limited English proficiency; MOLST, medical order for life-sustaining treatment.
In the univariable analyses, patients with LEP were less often white (24 [27.0%] vs. 193 [77.8%]; p < 0.001) but were more often of Hispanic or Latinx ethnicity (40 [45.0%] vs. 13 [5.2%]; p < 0.001) (Table 1). Patients with LEP were more often insured with Medicaid (15 [16.9%] vs. 17 [6.9%]; p < 0.001) or dual coverage insurance (34 [38.2%] vs. 26 [10.5%]; p < 0.001); less often reported other religion (4 [4.5] vs. 42 [16.9]; p = 0.002); more often were never smokers (48 [53.9%] vs. 81 [32.7%]; p < 0.001); and less often had a diagnosis of congestive heart failure (CHF) (18 [20.2%] vs. 79 [31.9%]; p = 0.04) or chronic obstructive pulmonary disease or asthma (15 [16.9%] vs. 73 [29.4%]; p = 0.02). Patients with LEP less often had a completed MOLST on admission (15 [16.9%] vs. 120 [48.4%]; p < 0.001), and among those who completed a MOLST, fewer patients had orders for do-not-resuscitate (DNR) and do-not-intubate (DNI) (8 [9.0%] vs. 72 [29.0%]) compared to patients with English proficiency.
Palliative care and EOL outcomes
In the univariable analyses, patients with LEP more often died in the ICU (55 [61.8%] vs. 87 [35.1%]; p < 0.001) and more often received CPR (9 [10.1%] vs. 9 [3.6%]; p = 0.04) than patients with English proficiency (Table 2). The number and timing of initial goals-of-care conversations were similar in both groups, and there was no difference in the number of patients who received palliative care consultations.
Table 2.
Hospitalization Characteristics of COVID-19 Inpatient Decedents by Level of English Proficiency
| Total deaths (n = 337) | English proficient (n = 248) | LEP (n = 89) | p Valuea | |
|---|---|---|---|---|
| Place of death | ||||
| ICU | 142 (42.1) | 87 (35.1) | 55 (61.8) | <0.001 |
| Inpatient palliative care | 63 (18.7) | 46 (18.6) | 17 (19.1) | |
| General ward | 118 (35.0) | 103 (41.5) | 15 (16.9) | |
| ER | 12 (3.6) | 10 (4.0) | 2 (2.3) | |
| Unclear location | 2 (0.6) | 2 (0.8) | 0 (0) | |
| HPM consultation | 208 (61.7) | 148 (59.7) | 60 (67.4) | 0.20 |
| Time to initial consult, median (IQR), days | 3 (1–7)b | 3 (0–7)c | 5 (2–9)d | 0.02 |
| Time from initial consult to patient death, median (IQR), days | 4 (2–9)b | 4 (2–8)c | 6 (2–13)d | 0.06 |
| Goals-of-care conversation | 327 (97.0) | 239 (96.4) | 88 (98.9) | 0.47 |
| Time to initial documentation, median (IQR), days | 1 (0–4)e | 1 (0–3)f | 1 (0–6)g | 0.06 |
| Code status change | <0.001 | |||
| Full code to CMO or DNR/DNI | 137 (40.7) | 82 (33.1) | 55 (61.8) | |
| Partial code to CMO or DNR/DNI | 30 (8.9) | 25 (10.1) | 5 (5.6) | |
| Prior/unknown to CMO or DNR/DNI | 9 (2.7) | 7 (2.8) | 2 (2.3) | |
| Full code to partial DNR | 15 (4.5) | 7 (2.8) | 8 (9.0) | |
| DNR/DNI to CMO | 101 (30.0) | 87 (35.1) | 14 (15.7) | |
| No change | 37 (11.0) | 33 (13.3) | 4 (4.5) | |
| Unable to determine | 8 (2.4) | 7 (2.8) | 1 (1.1) | |
| CPR performed | 18 (5.3) | 9 (3.6) | 9 (10.1) | 0.04 |
| Code status concordant | 17 (5.0) | 9 (3.6) | 8 (9.0) | |
| Code status discordant | 1 (0.3) | 0 (0) | 1 (1.1) | |
| Hospital length of stay, median (IQR), days | 9 (4–15) | 8 (4–13) | 13 (6–19) | <0.001 |
| ICU admission or transfer | 204 (60.5) | 131 (52.8) | 73 (82.0) | <0.001 |
| ICU length of stay, median (IQR), days | 7.4 (1.9–14.0) | 5.3 (1.1–11.1) | 10 (4–16) | <0.001 |
| Mechanical ventilation or ECMO | 141 (69.1) | 81 (61.8) | 60 (82.2) | 0.003 |
| Time on mechanical ventilation or ECMO, median (IQR), days | 11 (5–18) | 10 (5–18) | 13.5 (7.0–19.5) | 0.08 |
| Hospital type | 0.002 | |||
| Academic | 200 (59.4) | 135 (54.4) | 65 (73.0) | |
| Community | 137 (40.7) | 113 (45.6) | 24 (27.0) | |
| Admission month | 0.22 | |||
| March | 14 (4.2) | 9 (3.6) | 5 (5.6) | |
| April | 272 (80.7) | 197 (79.4) | 75 (84.3) | |
| May | 51 (15.1) | 42 (16.9) | 9 (10.1) |
Data are expressed as n (%) unless otherwise indicated.
Univariable comparison using Pearson's chi-squared test or Fisher's exact test when cell counts were <5 for categorical variables and Wilcoxon rank-sum test for continuous variables.
Unable to calculate time to initial consult for seven patients who were transferred from an outside hospital.
Unable to calculate time to initial consult for four patients who were transferred from an outside hospital.
Unable to calculate time to initial consult for three patients who were transferred from an outside hospital.
Unable to calculate time to initial documentation for eleven patients who were transferred from an outside hospital.
Unable to calculate time to initial documentation for six patients who were transferred from an outside hospital.
Unable to calculate time to initial documentation for five patients who were transferred from an outside hospital.
CMO, comfort measures only; CPR, cardiopulmonary resuscitation; ER, emergency room; HPM, hospice or palliative medicine; ICU, intensive care unit.
However, patients with LEP more often received later palliative care consultations than patients with English proficiency (5 days [2–9 days] vs. 3 days [0–7 days]; p = 0.02). More patients with LEP transitioned from a code status of full code on admission to comfort measures only (CMO) or DNR/DNI at time of death (55 [61.8%] vs. 82 [33.1%]; p < 0.001) and less often transitioned from DNR/DNI to CMO (14 [15.7%] vs. 87 [35.1]; p < 0.001) compared to patients with English proficiency.
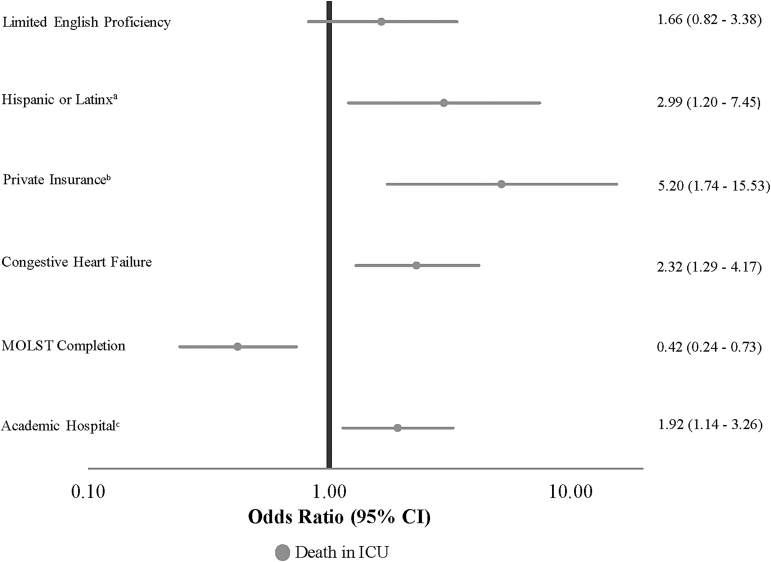
Figure 2 and Supplementary Table S1 shows the final multivariable model for odds of dying in the ICU adjusted for patient and hospital characteristics that were significant in the univariable models. LEP was not independently associated with dying in the ICU, but Hispanic or Latinx ethnicity, private insurance, CHF, or a terminal hospitalization in an academic hospital were significantly associated with death in the ICU. Conversely, a completed MOLST on admission was independently associated with non-ICU death. There was no significant association between race and primary language or ethnicity and primary language in our sensitivity analyses (Supplementary Table S2).
FIG. 2.
Forest plot for variables independently associated with the primary outcome: death in ICU. Multivariable model was adjusted for primary language, race, ethnicity, insurance, religion, smoking history, history of CHF and COPD, MOLST completion on admission, and hospital type. Note: aReference is Non-Hispanic or Non-Latinx ethnicity. bReference is Medicare. cReference is Community Hospital. CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; MOLST, medical order for life-sustaining treatment.
Figure 3 and Supplementary Table S3 show the multivariable analysis for time to initial palliative care consultation. LEP was not associated with later palliative care consultation compared to patients with English proficiency. Other race was associated with later palliative care consultation compared to White race, whereas a completed MOLST on admission and a terminal hospitalization in an academic hospital were associated with earlier palliative care consultations.
FIG. 3.
Forest plot for variables independently associated with secondary outcomes. Secondary outcomes include time to initial palliative care consultation, hospital length of stay, and ICU length of stay. Multivariable models were adjusted for primary language, race, ethnicity, insurance, religion, smoking history, history of CHF and COPD, MOLST completion on admission, and hospital type. Note: aReference is White race. bReference is Medicare. cReference is Never Smoker. dReference is Community Hospital.
Health care utilization outcomes
In the univariable analyses, patients with LEP more often died in an academic hospital (65 [73.0%] vs. 135 [54.4%]; p = 0.002) and experienced a longer hospital length of stay before death (13 days [6–19 days] vs. 8 days [4–13 days]; p < 0.001] (Table 2). During their hospitalization, patients with LEP were admitted or transferred to the ICU more often (73 [82.0%] vs. 131 [52.8%]; p < 0.001) and had a longer ICU length of stay (10 days [4–16 days] vs. 5.3 days [1.1–11.1 days]; p < 0.001). Patients with LEP more often received mechanical ventilation or ECMO (60 [82.2%] vs. 81 [61.8%]; p = 0.003), but there was no difference on time spent on mechanical ventilation or ECMO.
In the multivariable analyses, LEP was associated with a longer hospital length of stay (mean difference 4.12 days; 95% CI, 1.72–6.53; p < 0.001) compared to patients with English proficiency (Fig. 3 and Supplementary Table S4). Private insurance (mean difference 3.43 days; 95% CI, 0.20–6.65; p = 0.04) and academic hospitals (mean difference 2.34 days; 95% CI, 0.61–4.07; p = 0.008) were also associated with a longer hospital length of stay, whereas other insurance (mean difference −2.90 days; 95% CI, −5.12 to −0.67; p = 0.01) and MOLST on admission (mean difference −3.07 days; 95% CI, −4.85 to −1.28; p < 0.001) were associated with a shorter length of stay. LEP was not associated with ICU length of stay, but positive smoking history and a terminal hospitalization at an academic hospital were associated with a longer length of stay (Fig. 3 and Supplementary Table S4).
Discussion
During the pandemic's first wave, differences in EOL care existed between COVID-19 patients with LEP and COVID-19 patients with English proficiency who died in the inpatient setting in the greater Boston area. LEP was independently associated with an increased hospital length of stay but not with ICU length of stay, death in the ICU, or timing of palliative care consultations. In our univariable analyses, more patients with LEP had a code status of full code on admission and received life-sustaining treatment (i.e., CPR and mechanical ventilation) versus patients with English proficiency. The reasons for these findings are likely multifactorial and may include individual factors (i.e., personal EOL preferences influenced by varying levels of acculturation), interpersonal factors (i.e., barriers that impeded effective communication), and structural factors (i.e., racism and discrimination toward patients with LEP).
The degree of acculturation among immigrant populations has been shown to influence preferences for life-sustaining treatment.33–37 For example, recent immigrants are more likely to die in the ICU and receive invasive care compared with long-standing residents.36 Although we did not measure acculturation directly, primary language designation is a reliable proxy for acculturation.38–40 In our study, more patients with LEP designated a code status of full code on admission and more often received CPR compared to English proficient patients. This finding possibly reflects cultural attitudes toward EOL care among patients less acculturated to the dominant cultural narrative in the United States regarding EOL care (i.e., a “good death” means less invasive life-sustaining treatment at the EOL).41
However, because a universally accepted definition of a “good death” does not exist,42 simply acculturating to dominant social norms around EOL care does not automatically equate to high-quality palliative care. To improve palliative care delivery to patients with LEP, additional research is needed to better understand less acculturated patients' perceptions of quality EOL care and why a trend toward higher intensity care at EOL exists.
In addition to facing pandemic-specific challenges (i.e., prognostic uncertainty around COVID-19, visitor restrictions, and reduced time spent in patient rooms to minimize infectious risk and personal protective equipment use),43–45 patients with LEP likely faced challenges related to clinician-patient language discordance. Clinician-patient language discordance has long been associated with poor outcomes, including less health education for patients, worse interpersonal care, lower patient-reported satisfaction with care, and increased hospital length of stay.8,46–48 In palliative care, the linguistic and cross-cultural complexities of navigating language discordant conversations around EOL care are well established.49–51 Therefore, even though the timeliness of palliative care consultation and goals-of-care conversations were similar between LEP and English proficient groups, the inherent difficulties of language discordant EOL conversations may have added an extra layer of difficulty to achieve timely and effective shared decision-making for patients with LEP.
However, because our study lacks data on key stakeholders' experiences, additional work that examines these stakeholders' experiences is needed to determine whether language discordance impacted shared decision-making and thus hospital length of stay.
Structural racism and discrimination—macro-level conditions that limit opportunities, resources, power, and well-being of individuals and populations based on race/ethnicity, primary language, and other statuses52—may have also contributed to increased hospital length of stay among COVID-19 decedents with LEP. Structural racism and discrimination toward patients with LEP embody many forms, e.g., inadequate insurance enrollment support leading to higher rates of uninsured patients among individuals with LEP and “hidden curricula” within health care organizations that lead to a passive indifference towards the needs of patients with LEP.53,54 Lack of interpreter availability is a ubiquitous form of structural racism and discrimination in our health care system12,55 and is an established predictor of increased hospital length of stay.48
However, because our study lacks data on interpreter utilization, any association between hospital length of stay and interpreter access is inferential. That said, the increased demand for medical interpreters during the initial COVID-19 surge in greater Boston was well reported and forced health care systems to adapt and create innovative service lines to meet this need.56–58
There are several limitations to our study. First, our study took place within one health care system, which limits generalizability. However, we analyzed data from multiple hospitals from within the system and adjusted for such differences in our multivariable analyses. Second, we may have lacked power to identify all pertinent differences among the two groups due to our sample size. Third, we were unable to assess when and if an interpreter was present during patient encounters. Fourth, the level of English proficiency among health care proxy agents and family members was unknown, which could have influenced patient outcomes. Fifth, we did not measure acculturation directly via validated ethnographic surveys or qualitative interviews, which limits attribution of our findings to this phenomenon.
Sixth, our demographic categories for race and ethnicity may differ from race and ethnicity categories utilized by the U.S. Census. This variability in taxonomy reflects the lack of standardization of how the social constructs of race and ethnicity have been defined and implemented across EHRs. Seventh, our study used accepted quality indicators that approximate the quality of EOL care delivered, but additional qualitative data or bereaved caregiver input is necessary to understand the quality of EOL care delivered to COVID-19 decedents with LEP in greater detail. Finally, we dichotomized religion into Christian versus non-Christian in our multivariable analyses due to our small sample size. We acknowledge that diverse religions constitute the non-Christian subcategory, which makes it difficult to interpret the findings of this subanalysis.
Conclusion
Our findings suggest that differences in EOL care occurred between COVID-19 inpatient decedents with LEP and COVID-19 inpatient decedents with English proficiency in a greater Boston health care system during the first wave of the pandemic. LEP was independently associated with increased hospital length of stay but not death in the ICU. However, limitations in the study design preclude attribution of these findings to a specific phenomenon, but may include individual, interpersonal, and structural factors. Additional research is needed to understand which factors were the primary drivers of differences in EOL care delivery that led to increased hospital lengths of stay among inpatient COVID-19 decedents with LEP.
Supplementary Material
Authors' Contributions
I.S.C. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: I.S.C., S.M.S., and D.M.L. Acquisition, analysis, or interpretation of data: all authors. Drafting of the article: I.S.C. Critical revision of the article for important intellectual content: all authors. Statistical analysis: I.S.C. and D.M.L. Administrative, technical, or material support: I.S.C. Supervision: D.M.L.
Funding Information
Dr. Chua reports receiving funding from IBM Watson Health for work related to artificial intelligence in oncology. Dr. Levine reports receiving funding from IBM Watson Health to study COVID-19 safety, separate from present work. Dr. Shi reports receiving funding from the Harvard Translational Research in Aging Training Program, T32AG023480.
Author Disclosure Statement
No competing financial interests exists.
Supplementary Material
References
- 1. Moore JT, Ricaldi JN, Rose CE, et al. : Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020–2022 States, February-June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1122–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wadhera RK, Wadhera P, Gaba P, et al. : Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA 2020;323:2192–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Figueroa JF, Wadhera RK, Lee D, et al. : Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood) 2020;39:1984–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Martinez DA, Hinson JS, Klein EY, et al. : SARS-CoV-2 positivity rate for Latinos in the Baltimore-Washington, DC region. JAMA 2020;324:392–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention: COVID-19 weekly cases and deaths per 100,000 population by age, race/ethnicity, and sex. 2021. https://covid.cdc.gov/covid-data-tracker/?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcases-updates%2Fcases-in-us.html#demographicsovertime (Last accessed April 3, 2021).
- 6. Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, et al. : Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Ann Epidemiol 2020;52:46–53 e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Karmakar M, Lantz PM, Tipirneni R: Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open 2021;4:e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barwise A, Jaramillo C, Novotny P, et al. : Differences in code status and end-of-life decision making in patients with limited English proficiency in the intensive care unit. Mayo Clin Proc 2018;93:1271–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Silva MD, Genoff M, Zaballa A, et al. : Interpreting at the end of life: A systematic review of the impact of interpreters on the delivery of palliative care services to cancer patients with limited English proficiency. J Pain Symptom Manage 2016;51:569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thornton JD, Pham K, Engelberg RA, et al. : Families with limited English proficiency receive less information and support in interpreted intensive care unit family conferences. Crit Care Med 2009;37:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pham K, Thornton JD, Engelberg RA, et al. : Alterations during medical interpretation of ICU family conferences that interfere with or enhance communication. Chest 2008;134:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schiaffino MK, Nara A, Mao L: Language services in hospitals vary by ownership and location. Health Aff (Millwood) 2016;35:1399–1403. [DOI] [PubMed] [Google Scholar]
- 13. Schenker Y, Fernandez A, Kerr K, et al. : Interpretation for discussions about end-of-life issues: Results from a National Survey of Health Care Interpreters. J Palliat Med 2012;15:1019–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Presa LR and Bowen A: Lost in translation: How language barriers can add anguish and complicate care for COVID-19 patients who don't speak English. November 15, 2020. https://www.chicagotribune.com/coronavirus/ct-life-coronavirus-english-second-language-spanish-speaking-patients-20201115-qi26k6ixnjejhoe4umnkh6bn3y-story.html (Last accessed April 5, 2021).
- 15. Aguilera J: Coronavirus patients who don't speak english could end up ‘unable to communicate in their last moments of life’. April 15, 2020. https://time.com/5816932/coronavirus-medical-interpreters (Last accessed April 5, 2021).
- 16. Shen MJ, Maciejewski PK, Tergas AI, et al. : Inequities in end-of-life care among immigrant patients exaggerated by the COVID-19 pandemic. J Pain Symptom Manage 2021;62:e3–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Commonwealth of Massachusetts: COVID-19 response reporting. 2021. https://www.mass.gov/info-details/covid-19-response-reporting (Last accessed June 1, 2021).
- 18. Chuzi S, Molsberry R, McCabe ME, et al. : Distribution in place of death for COVID-19-related mortality in the United States. J Am Geriatr Soc 2020;68:1917–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chua IS, Shi SM, and Levine DM: Place of death and end-of-life care utilization among COVID-19 decedents in a Massachusetts health care system. J Palliat Med 2021;24:322–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ngai KM, Grudzen CR, Lee R, et al. : The association between limited English Proficiency and Unplanned Emergency Department revisit within 72 hours. Ann Emerg Med 2016;68:213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Qureshi MM, Romesser PB, Jalisi S, et al. : The influence of limited English proficiency on outcome in patients treated with radiotherapy for head and neck cancer. Patient Educ Couns 2014;97:276–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parker MM, Fernández A, Moffet HH, et al. : Association of patient-physician language concordance and glycemic control for limited-English proficiency Latinos with type 2 diabetes. JAMA Intern Med 2017;177:380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Earle CC, Park ER, Lai B, et al. : Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol 2003;21:1133–1138. [DOI] [PubMed] [Google Scholar]
- 24. Grunfeld E, Urquhart R, Mykhalovskiy E, et al. : Toward population-based indicators of quality end-of-life care: Testing stakeholder agreement. Cancer 2008;112:2301–2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lindvall C, Lilley EJ, Zupanc SN, et al. : Natural language processing to assess end-of-life quality indicators in cancer patients receiving palliative surgery. J Palliat Med 2019;22:183–187. [DOI] [PubMed] [Google Scholar]
- 26. Bernacki R, Hutchings M, Vick J, et al. : Development of the serious illness care program: A randomised controlled trial of a palliative care communication intervention. BMJ Open 2015;5:e009032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paladino J, Bernacki R, Neville BA, et al. : Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: A cluster randomized clinical trial of the Serious Illness Care Program. JAMA Oncol 2019;5:801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lakin JR, Koritsanszky LA, Cunningham R, et al. : A systematic intervention to improve serious illness communication in primary care. Health Affairs 2017;36:1258–1264. [DOI] [PubMed] [Google Scholar]
- 29. Lever J, Krzywinski M, and Altman N: Points of significance: Model selection and overfitting. Nat Methods 2016;13:703–704. [Google Scholar]
- 30. Weech-Maldonado R, Morales LS, Elliott M, et al. : Race/ethnicity, language, and patients' assessments of care in Medicaid managed care. Health Serv Res 2003;38:789–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Seid M, Stevens GD, and Varni JW: Parents' perceptions of pediatric primary care quality: Effects of race/ethnicity, language, and access. Health Serv Res 2003;38:1009–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nguyen D and Reardon LJ: The role of race and English proficiency on the health of older immigrants. Soc Work Health Care 2013;52:599–617. [DOI] [PubMed] [Google Scholar]
- 33. Grace Yi EH: Does acculturation matter? End-of-life care planning and preference of foreign-born older immigrants in the United States. Innov Aging 2019;3:igz012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Matsumura S, Bito S, Liu H, et al. : Acculturation of attitudes toward end-of-life care: A cross-cultural survey of Japanese Americans and Japanese. J Gen Intern Med 2002;17:531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wright AA, Stieglitz H, Kupersztoch YM, et al. : United states acculturation and cancer patients' end-of-life care. PLoS One 2013;8:e58663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yarnell CJ, Fu L, Manuel D, et al. : Association between immigrant status and end-of-life care in Ontario, Canada. JAMA 2017;318:1479–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. DeSanto-Madeya S, Nilsson M, Loggers ET, et al. : Associations between United States acculturation and the end-of-life experience of caregivers of patients with advanced cancer. J Palliat Med 2009;12:1143–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lee S, Nguyen HA, and Tsui J: Interview language: A proxy measure for acculturation among Asian Americans in a population-based survey. J Immigr Minor Health 2011;13:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kang S-M: Measurement of acculturation, scale formats, and language competence: Their implications for adjustment. J Crosscult Psychol 2006;37:669.—693. [Google Scholar]
- 40. Pew Research Center: Hispanic trends: Assimilation and language. March 19, 2004. https://www.pewresearch.org/hispanic/2004/03/19/assimilation-and-language (Last accessed May 7, 2021).
- 41. Jackson VA, Sullivan AM, Gadmer NM, et al. : “It was haunting…”: Physicians' descriptions of emotionally powerful patient deaths. Acad Med 2005;80:648–656. [DOI] [PubMed] [Google Scholar]
- 42. Steinhauser KE, Christakis NA, Clipp EC, et al. : Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284:2476–2482. [DOI] [PubMed] [Google Scholar]
- 43. Leiter RE: Reentry. N Engl J Med 2020;383:e141. [DOI] [PubMed] [Google Scholar]
- 44. Cook DJ, Takaoka A, Hoad N, et al. : Clinician perspectives on caring for dying patients during the pandemic: A mixed-methods study. Ann Intern Med 2021;174:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Frampton S, Agrawal S, and Guastello S: Guidelines for family presence policies during the COVID-19 pandemic. JAMA Health Forum 2020;1:e200807. [DOI] [PubMed] [Google Scholar]
- 46. Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. : Providing high-quality care for limited English proficient patients: The importance of language concordance and interpreter use. J Gen Intern Med 2007;22 Suppl 2(Suppl 2):324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. John-Baptiste A, Naglie G, Tomlinson G, et al. : The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med 2004;19:221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lindholm M, Hargraves JL, Ferguson WJ, et al. : Professional language interpretation and inpatient length of stay and readmission rates. J Gen Intern Med 2012;27:1294–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Norris WM, Wenrich MD, Nielsen EL, et al. : Communication about end-of-life care between language-discordant patients and clinicians: Insights from medical interpreters. J Palliat Med 2005;8:1016–1024. [DOI] [PubMed] [Google Scholar]
- 50. Butow PN, Lobb E, Jefford M, et al. : A bridge between cultures: Interpreters' perspectives of consultations with migrant oncology patients. Support Care Cancer 2012;20:235–244. [DOI] [PubMed] [Google Scholar]
- 51. Silva MD, Tsai S, Sobota RM, et al. : Missed opportunities when communicating with limited English-proficient patients during end-of-life conversations: Insights from Spanish-speaking and Chinese-speaking medical interpreters. J Pain Symptom Manage 2020;59:694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. National Institute on Minority Health and Health Disparities: Structural racism and discrimination. https://www.nimhd.nih.gov/resources/understanding-health-disparities/srd.html (Last accessed January 29, 2022).
- 53. Kenison TC, Madu A, Krupat E, et al. : Through the veil of language: Exploring the hidden curriculum for the care of patients with limited English proficiency. Acad Med 2017;92:92–100. [DOI] [PubMed] [Google Scholar]
- 54. Foiles Sifuentes AM, Robledo Cornejo M, Li NC, et al. : The role of limited English proficiency and access to health insurance and health care in the affordable care act era. Health Equity 2020;4:509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Butkus R, Rapp K, Cooney TG, et al. : Envisioning a better U.S. health care system for all: Reducing barriers to care and addressing social determinants of health. Ann Intern Med 2020;172:S50–s59. [DOI] [PubMed] [Google Scholar]
- 56. Knuesel S, Chuang W, Olson E, et al. : Language barriers, equity, and COVID-19: The impact of a novel Spanish language care group. J Hosp Med 2021;16:109–111. [DOI] [PubMed] [Google Scholar]
- 57. Bebinger M: With Latinos dying at higher rates from COVID, Brigham and Women's Hospital Intervenes. 2021. https://www.wbur.org/commonhealth/2021/01/29/mass-general-brigham-covid-community-intervention (Last accessed June 15, 2021).
- 58. Herzberg EM, Barrero-Castillero A, and Matute JD: The healing power of language: Caring for patients with limited English proficiency and COVID-19. Pediatr Res 2022;91:526–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.