Abstract
Timely and accurate detection of Group B Streptococcus (GBS) carriage in pregnant women allows for targeted peripartum prophylaxis. Replacing culture-based screening by molecular biology assays enables faster results obtention, better targeted antibiotic prophylaxis, and reduces the laboratory workload. Here, we present a comparative analysis between a Loop Mediated Isothermal Amplification assay (HiberGene GBS kit) and culture (gold-standard). The HiberGene GBS kit showed a sensitivity of 97.9% and a specificity of 96.8% compared with culture. The limit of detection was estimated at 103 cfu/ml and results were obtained within 30 min. HiberGene GBS assay can be used for peripartum GBS screening and targeted antibiotic prophylaxis provided sample processing can be swiftly performed around the clock.
Keywords: Group B streptococci, LAMP assay, Intrapartum prophylaxis, Early onset neonatal sepsis, Screening, Pregnancy
Introduction
Group B streptococci (GBS) belongs to the commensal vaginal and rectal flora and is present in 10 to 30% of women [1]. In pregnant women, this colonization is the primary risk factor for neonatal infections referred to as GBS early-onset disease (EOD). Prevention is based on intrapartum antibiotic prophylaxis (IAP) for GBS carriers, who are screened at 35–37 weeks of pregnancy using a culture-based approach. This strategy (screening and treatment) has been shown to efficiently reduce the incidence of EOD from 1.8 to 0.22 cases per 100 births [1]. Alternatively, a risk factor strategy, including previous delivery with invasive GBS disease, GBS bacteriuria during the current pregnancy, rupture of amniotic membranes for ≥ 18 h, birth at less than 37 weeks, and known GBS positive status during a previous pregnancy, can be used, at the expense of a lower efficacy [2]. Ideally, determination of maternal GBS carriage should be performed during the peripartum phase in order to permit the most adequate administration of the prophylactic treatment. Indeed, it has been shown that GBS carriage fluctuates during the pregnancy and more particularly from 35 to 37 weeks and the onset of labor. Reversion of 35–37 weeks GBS carriage occurs in about 10% of the cases and about 4% of negative GBS carriers are detected as positive at the onset of labor [3]. The use of molecular assays for GBS peripartum screening allows for targeting the correct population with analytical performances equivalent to culture [4].
Numerous commercially available PCR-based assays are now available including the Cepheid® Xpert® GBS that can be performed in the delivery room [4–7]. Here, we present a comparative analysis between the HiberGene Group B Streptococcus LAMP assay versus culture including a backup broth.
Material and methods
Vagino-rectal swabs (ESwabs, Copan CE 0103, Brescia, Italy) were collected during the period of April 2021 to February 2022 in 153 patients and sent to the clinical bacteriology laboratory of Geneva University Hospitals. GBS detection by culture was performed on the WASPLab using CHROMID® Strepto B chromogenic agar plates (GBS CHROMID®, BioMérieux, Marcy l'Etoile, France) and a broth-enriched media (Copan, 476CE.A), which was systematically inoculated on another chromogenic agar after 24 h of growth. Suspect pink colonies were identified by matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF/MS) (MBT Compass 4.1, Bruker Daltonics, Bremen, Germany) according to the manufacturer’s instructions.
As molecular-based assay, we used HiberGene HGGBSR2204, according to the manufacturer’s instructions. The HiberGene GBS kit is a LAMP-based assay performed in isothermal condition and thus made to be dispensed from a thermocycling unit, with the advantage of being more robust than PCR [8]. In brief, the vagino-rectal swabs used for the culture on agar plates were eluted in the appropriated buffer, and 80μL were lysed at room temperature for 20 min. The samples were denatured for 5 min at 105 °C and 25 μL added into each vial of the reaction strips prior to loading on the HiberGene GBS kit for GBS amplification. Control experiments using the Cepheid® Xpert® GBS were performed according to the manufacturer recommendation.
Assessment of the limit of detection (LOD)
Real-time PCR positivity is based on fluorophore detection and expressed in cycling units, whereas for the LAMP assay is based on a more rapid target DNA amplification, shifting the turbidity of the amplification reaction and detected in minutes. To estimate the LOD of the HiberGene GBS assay, vagino-rectal ESwabs were spiked with GBS colony concentrations ranging from 3 × 102 to 3 × 107 cfu/ml. The time to positivity was plotted in minutes against the colony-forming unit/milliter (cfu/ml) as determined by vial cell counting on Columbia agar after overnight incubation. The LOD was derived from the lowest cfu/ml concentration correlating with a positive LAMP amplification.
Results and discussion
Among the 153 specimens tested for GBS carriage, 48 (31%) were positive by culture. This rate does not reflect the real incidence, as we had selected 30 positive specimens for our analysis to test its clinical sensitivity. For this reason, the negative and positive predictive values cannot be calculated from our data. Among the 48 positive specimens, only 47 were taken in consideration due to one non-interpretable result of the Hibergene LAMP assay (Table 1, error). The sensitivity of the HiberGene GBS kit was 97.9% (95% [CI 88.9–99.6%]) corresponding to 46/47 positive specimens. The specificitey was 96.8% (95% CI [91.1–98.9%]) corresponding to 92/95 negative culture-based specimens (Table 1). The three false positive results were assessed using the Cepheid® Xpert® GBS kit, which returned negative and were therefore considered as “true” false-positive results. The performance of the Hibergene assay is therefore comparable with other commercialized GBS PCR assays, i.e. Cepheid® Xpert® GBS and GenomEra® GBS PCR, with the advantage of having a faster turnaround time than PCR assays [7, 9].
Table 1.
Number of specimens according to the test results. Error: inconclusive result of the HiberGene GBS test due to technical error
| HiberGene PCR | Culture | ||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 46 | 3 | 49 |
| Negative | 1 | 92 | 93 |
| Error | 1 | - | 1 |
| Total | 48 | 95 | 153 |
Additionally, we found that the LAMP assay was able to detect specimens that revealed positive by enrichment broth, showing that the LAMP assay can accurately perform on low inocula. To evaluate the low inoculum detection by the LAMP assay and the issue of false positive detection, we investigated the LOD. The LOD corresponded to 103 cfu/ml and a time of positivity of 27.1 ± 0.5 min (Fig. 1). Occasionally, specimens with 102 cfu/ml returned positive but duplicates provided unreproducible data (data not shown). The serial dilutions spanning from 103 to 107 cfu/ml showed a consistent and linear decrease in time to positivity (Fig. 1). These data demonstrated that the LOD of the HiberGene GBS kit was equivalent to other commercially available molecular-based assays [9].
Fig. 1.
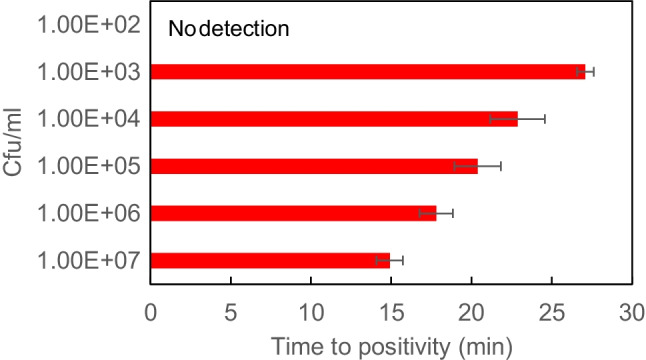
Negative clinical specimens were spiked with serial dilutions of GBS at concentrations ranging from 102 to 107 colony-forming units per ml (cfu/ml). The time to positivity measured by HiberGene GBS kit is expressed in minutes (min). Measurements were made in triplicate and errors expressed as SEM
The HiberGene GBS assay is an accurate and rapid test, requiring less laboratory skills and time than culture. Compared to existing PCR assays, it has the advantage of a lower price but needs to be executed by laboratory technologists. This implies having a diagnostic laboratory operating on a 24 hours basis to benefit from this rapid turn-around time. GBS carriage results should be available to allow targeted intra-partum prophylaxis and for at least 4 hours. Cepheid® Xpert® has been shown to allow for correct prophylaxis in the same number of women than antenatal culture but targeting the highest risk population [4]. As the HiberGene GBS assay performs faster or at least as fast as the Cepheid® Xpert®, this suggests that the HiberGene GBS can be utilised to rapidly and accurately detect GBS carriage in pregnant women provided laboratory staff is available at the vicinity and analyzing around the clock.
Author contribution
GZ and MT designed and conceptualized the study. MT performed the analysis, compiled, analyzed the data, and wrote the manuscript. JS and BMT reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
Open access funding provided by University of Geneva This study was performed by using internal funding.
Declarations
Ethics approval
In accordance with local ethical committee, routine clinical laboratories of our institution may use biological sample leftovers for method development after irreversible anonymization of data. The official name of the ethics committee is “Commission cantonale d’éthique de la recherche (CCER)” https://www.hug-ge.ch/ethique.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Russell NJ, et al. Maternal colonization with group B Streptococcus and serotype distribution worldwide: systematic review and meta-analyses. Clin Infect Dis. 2017;65(2):S100–S111. doi: 10.1093/cid/cix658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu Y, Lin XZ. Updates in prevention policies of early-onset group B streptococcal infection in newborns. Pediatr Neonatol. 2021;62(5):465–475. doi: 10.1016/j.pedneo.2021.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Hussain FN, et al. The accuracy of group beta Streptococcus rectovaginal cultures at 35 to 37 weeks of gestation in predicting colonization intrapartum. AJP Rep. 2019;9(3):e302–e309. doi: 10.1055/s-0039-1697655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Tejada BM, et al. Intrapartum Group B streptococcus detection by rapid polymerase chain reaction assay for the prevention of neonatal sepsis. Clin Microbiol Infect. 2011;17(12):1786–1791. doi: 10.1111/j.1469-0691.2010.03378.x. [DOI] [PubMed] [Google Scholar]
- 5.Curry A, et al. Evaluation of hibergene loop-mediated isothermal amplification assay for detection of group B streptococcus in recto-vaginal swabs: a prospective diagnostic accuracy study. Clin Microbiol Infect. 2018;24(10):1066–1069. doi: 10.1016/j.cmi.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Gao K, et al. Diagnostic performance of various methodologies for group B Streptococcus screening in pregnant woman in China. Front Cell Infect Microbiol. 2021;11:651968. doi: 10.3389/fcimb.2021.651968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nielsen SY, Moller JK, Khalil MR. A comparison of GenomEra(R) GBS PCR and GeneXpert (R) GBS PCR assays with culture of GBS performed with and without broth pre-enrichment. Eur J Clin Microbiol Infect Dis. 2020;39(10):1945–1950. doi: 10.1007/s10096-020-03934-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Francois P, et al. Robustness of a loop-mediated isothermal amplification reaction for diagnostic applications. FEMS Immunol Med Microbiol. 2011;62(1):41–48. doi: 10.1111/j.1574-695X.2011.00785.x. [DOI] [PubMed] [Google Scholar]
- 9.Ramesh Babu S, et al. Screening for group B Streptococcus (GBS) at labour onset using PCR: accuracy and potential impact - a pilot study. J Obstet Gynaecol. 2018;38(1):49–54. doi: 10.1080/01443615.2017.1328490. [DOI] [PubMed] [Google Scholar]


