Abstract
Population demand, healthcare resourcing, and transportation linkage are considered as major determinants of spatial access to health care. Temporal changes of the 3 determinants would result in gain or loss of spatial access to health care. As a remarkable milestone achieved by Targeted Poverty Reduction Project launched in China, the significant improvements in spatial access to health care served as an ideal context for investigating the relative contributions of these 3 determinants to the changes in spatial access to health care in a rural county. A national level poverty-stricken county, Chishui county from Guizhou province, China, was chosen as our study area. The enhanced two-step floating catchment area model and the chain substitution method were employed for analysis. The relative contributions of the 3 determinants demonstrated variations with villages. The relative contributions of healthcare resourcing were positive in all villages as indicated by sharp increases in healthcare resources. Population changes and transportation infrastructure expansion had both negative and positive effects on spatial access to health care for different villages. Decisionmakers should take into account the duration of travel time spent between where people live, where transport hubs are located, and where healthcare services are delivered in the process of formulating policies toward rural healthcare planning. For villages with poorly-established infrastructure, the optimization of population distribution and healthcare resourcing should be considered as the priority. A stronger marginal effect would be induced by transportation infrastructure expansion with increased spatial accessibility. This study provides empirical evidences to inform healthcare planning in low- and middle-income countries.
Keywords: rural health, enhanced two-step floating catchment area (E2SFCA) method, health services accessibility, chain substitution method, China
What do we already know about this topic?
Population demand, healthcare resourcing, and transportation linkage are considered as major determinants of spatial access to health care.
How does your research contribute to the field?
Under the constraints of limited resources, understanding the relative contributions made by each particular local factor to temporal changes in spatial accessibility of health care has great potential to inform health-related policy making procedures as well as investment-related decision making at the governmental level, especially for low- and middle-income countries confronted with similar situations.
What are your research’s implications toward theory, practice, or policy?
Decisionmakers should take into account the duration of travel time spent between where people live, where transport hubs are located, and where healthcare services are delivered throughout the process of formulating policies toward rural healthcare planning.
Background
Universal health coverage (UHC) was firstly proposed by World Health Organization in 2005,1 and has been widely pursued by countries around the world.2,3 Ensuring equitable access to health care is the cornerstone of UHC.4,5 It has been widely recognized that inaccessibility of health care would hinder residents from obtaining desired healthcare outcomes,6 especially for the impoverished residents or those living in remote rural areas.7,8 To date, quite a number of countries have taken actions to move toward UHC, such as Jamkesmas project in Indonesia, National Health Fund (NHF) project in Jamaica, and Seguro Popular project in Mexico.9
Qualification and assessment of access to health care is a critical approach for monitoring progress toward UHC as well as for future healthcare planning.10 Access to health care can be measured from both spatial and non-spatial dimensions.11 The former emphasizes geographic barriers between population demand and healthcare resources, while the latter refers to the actual utilization of medical services under the impacts of various economic and sociocultural factors.12 As a critical component and effective indicator in the evaluation of health equity, spatial accessibility has been widely used to inform policy-making procedures and healthcare-related program development.13
Spatial accessibility of health care can be evaluated by multiple measurements, which can be divided into 5 categories, namely container, coverage, minimum distance, travel cost, and gravity as suggested by Talen.14 As Geographical Information System (GIS) has been used to examine spatial patterns and utilization of health care, the two-step floating catchment area (2SFCA) method, one of the gravity models, gained great popularity among various spatial accessibility measurements.15 -17 In this method, population demand, healthcare resourcing, and transportation linkage are considered as significant determinants of spatial access to health care. The method enables the possibility of looking at the role of population demand and transportation linkage as important forces for spatial access to health care, perhaps as important as healthcare resourcing.
These 3 local factors associated with spatial access to health care, namely population demand, healthcare resourcing, and transportation linkage, are not fixed.18,19 Instead, they change over time at different paces, leading to gain or loss of spatial accessibility of health care.20 For instance, migration of people, relocation and replenishment of healthcare resources, and transportation infrastructure expansion could all affect spatial access to health care. Nevertheless, the contributions of each region-specific factor to the changes would vary due to different paces of change.
Under such context, it’s rather essential to associate the overall changes in spatial accessibility of health care with the unique contributions of each single local factor. By doing so, we would have an in-depth understanding of the constantly changing spatial patterns of health care delivery in terms of which local factor has posed the most or least impacts on improving residents’ spatial access to health care. Under the constraints of limited resources, understanding the relative contributions made by each particular local factor to temporal changes in spatial accessibility of health care has great potential to inform health-related policy making procedures as well as investment-related decision making at the governmental level, especially in low- and middle-income countries confronted with similar situations.21
To the best of our knowledge, only one existing study has analyzed the relative contribution made by each one of the 3 local factors to the changes in spatial access to health care, which employed chain substitution method to measure local factor impacts on spatial accessibility of physicians in Florida, USA.20 Given large disparities embedded in the patterns and improvements of spatial access to health care between developed countries and less developed countries,22 it’s necessary and urgent to add new evidence into this field via conducting relevant research in less developed countries. As a remarkable milestone achieved by Targeted Poverty Reduction Project over the past few years, the significant improvements in spatial access to health care served as an ideal context for us to explore the relative contributions of the 3 determinants to the changes in spatial access to health care in a rural county.
At the end of 2015, China launched a new round of nationwide poverty reduction projects, named “Tuo Ping Gong Jian (Targeted Poverty Reduction).” The central government aimed to eliminate extreme poverty in rural China by 2020.23 Considering the main causes of poverty in China, the government gave special attention to ensuring access to safe housing,24 compulsory education,25 and basic medical services26 among the poverty-stricken population and released a variety of policies to achieve the goal. By the end of 2020, 35 000 new settlement communities and 2.66 million new housing units have been built for resettling the impoverished families from inhospitable areas, while 59 000 km of new roads have been constructed in the impoverished regions. Moreover, 30 000 medical students have started working for impoverished areas as doctors after accomplishing free training programs. Moreover, 3700 key clinical departments have been established with the assistance of health workers from leading hospitals.27 These initiatives have brought about dramatic changes in population distribution, transportation infrastructure and healthcare resourcing among impoverished regions in China,28 thus providing us a fantastic opportunity to assess the unique contributions made by each region-specific factor to the overall temporal changes in spatial accessibility of health care.
Detailed data on the population, healthcare resourcing and transportation infrastructure were collected from a poverty-stricken county in China as the study area. The enhanced two-step floating catchment area (E2SFCA) model was utilized to calculate spatial access to health care provided by healthcare institutions. The chain substitution method was further employed to quantify the relative contributions of 3 local factors.
Rural Health Care and Accessibility
The Challenges of Rural Healthcare Access
Rural residents have experienced limited access to health care. Goins et al29 classified barriers to health care into 5 dimensions, including limited healthcare supply, the lack of quality health care, transportation difficulties, social isolation, and financial constraints. The first 3 dimensions reflect major obstacles posed on the process of seeking medical services, which measures the potential for patients to receive a certain quality and quantity of care in the existing healthcare system, while the last 2 aspects reflect the barriers to obtaining revealed care delivery. The definition “revealed care delivery,” as opposite to the “potential” one, refers to the fact that the access to medical services that patients actually obtained in the reality would be affected by multiple factors, such as economic status, region-specific norms and values in rural areas and other factors.16 For the first 2 major barriers we proposed earlier, the limited and low-quality healthcare services are mainly induced by the shortage of health professionals in rural areas, where the majority of healthcare professionals tend to move to higher-level hospitals in order to improve their compensation and living conditions, as well as to have more opportunities for career development. As to transportation difficulties, several leading factors have been proposed in this regard, including (1) traveling out of town for specialty care, (2) poor marked roads, (3) limited public transportation, and (4) inhospitable terrain or weather. In terms of social isolation, it has to be noted that under the context where residents are largely affected by rural norms and values, lots of time and efforts would have to be spent in order to improve the current situation. The last one, financial constraints, refers to the considerable financial burden posed by medical costs on patients’ affordability of obtaining medical services. As reported by the current literature, the heavy financial burden posed by medical costs has resulted in financial hardship for millions of people living in low-and middle-income countries.30
These barriers mentioned above exactly reflect the true situation of rural China, where village doctors have been confronted with major challenges in providing various types of public health services to meet the demand of residents. In addition, the health professional labor force in rural China mainly consists of village doctors with nearly half of them aged 50 years old and above, which further undermines the efficiency and quality of healthcare delivery.31 As reported by a recently accomplished national survey led by China’s National Bureau of Statistics which engaged more than 300 million residents living in impoverished counties, 80.3% of people whose household members didn’t manage to access health services in a timely manner over the past year reported that they were “too far away from a health facility,” while another 14.6% percent of people reported financial hardship as the major factor.32
Accessibility Measures Used in Health Care
Penchansky and Thomas have grouped access to health care into 2 spatial (availability and accessibility) and 3 aspatial (affordability, acceptability, and accommodation) aspects, known as “the five As.”33 It is difficult to measure aspatial accessibility because it can be pretty hard to obtain the data reflective of the actual health service utilization patterns of patients. Spatial accessibility, which only requires the spatial information of the patients and healthcare institutions as well as road network, is easier to measure and increasingly used in health planning. There are several ways to measure spatial accessibility, including (1) provider-to-population ratio (PPR), (2) travel barriers to the nearest provider, (3) average travel barriers to a group of providers, and (4) gravity models.34 The provider-to-population ratio, which directly calculates the ratio of resource supply to demand within a given administrative area, is widely used in China because it is easy to calculate and understand. However, PPR does not reflect the real-world situation, given the disparities in healthcare accessibility within administrative units and patients’ cross-border service-seeking behaviors.35 The second and third measurements belong to the shortest path analysis, depending on the distance or time spent by the patient to the healthcare organizations. In contrast to the PPR, shortest path analysis takes into account the location information of both supply and demand sides. Gravity models give consideration not only to the location and spatial interactions between supply and demand but also to the size of the supply and demand, enabling a more accurate measurement of the configuration of the healthcare facilities.36
Among the gravity models, a representative one typically adopted in this study field is the Two-Step Floating Catchment Area (2SFCA) method. The major limitation of this method is that it does not take into account the variability of spatial accessibility within the search radius.37 As a solution to this issue, the Enhanced Two-Step Floating Catchment Area (E2SFCA) method divides each catchment into multiple sub-catchments and applies different weights to each sub-catchment to simulate the distance decay effects.38 Some critics have pointed out that the E2SFCA method overestimates the needs of patients and does not make allowance for the competitive relationships among hospitals. The Enhanced Three-Step Floating Catchment Area (E3SFCA) method was then proposed to further address this issue.39 In addition, Luo incorporated the Huff model into floating catchment area methods to explore the probability of people’s choice of healthcare service locations.40 The above methods offer a variety of ways to measure spatial accessibility and are widely used among different regions around the world.41 -43
Data and Methods
Study Area
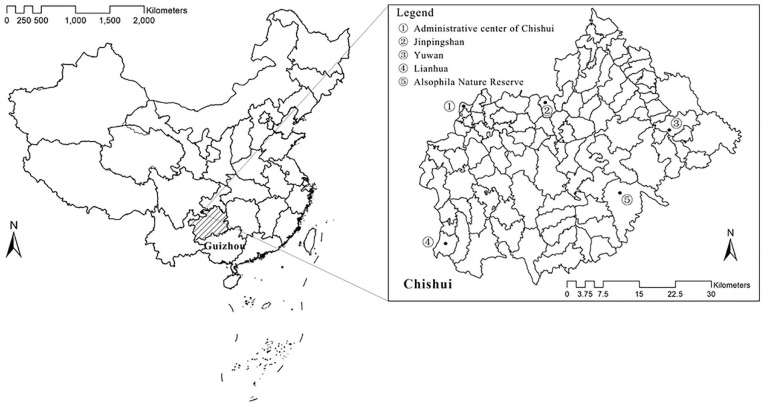
A national level poverty-stricken county, Chishui county from Guizhou province, China, was chosen as our study area. Chishui is a county located in Guizhou Province in Southwest China (Figure 1), with a total population of over 310 100 in 2014 and an area of 1862 km2.44 In 2014, the per capita disposable income of urban residents and rural residents in Chishui was 21 722, and 8350 RMB,45 which were both lower than the national averages of the corresponding population groups.46 Chishui developed vigorous socioeconomic and infrastructures during the implementation of the Targeted Poverty Reduction Project and raised out of poverty at the end of 2017. During this period of 2014 to 2017, the population distribution, healthcare resourcing, and transportation infrastructure have been changed and thus resulted in a variation in spatial access to health care.
Figure 1.
The geographic location of Chishui, Guizhou province, China.
Note. Administrative center of Chishui, Jinpingshan Village, Lianhua Village, Yuwan Village which would mention subsequently were marked in the followed graph.
Data and Preprocessing
The data used in this study were collected from multiple sources: (1) data of population distribution retrieved from the Bureau of the Statistics of Chishui; (2) data healthcare resourcing retrieved from the Health Commission of Chishui; and (3) data of transportation infrastructure retrieved from the Department of Transportation of Chishui. These 3 datasets were available for the years 2014 and 2017. The population data was accurate to the village level, while the data on healthcare resourcing was reported at the facility level, including health facility name, address, and the number of health professionals, doctors, nurses, and hospital beds.
We used ArcGIS 10.5 to build a GIS database to contain all data collected from multiple resources. We processed the village population data into 230 m × 230 m grid data.47 Grid data were used for calculating spatial accessibility of health care for each raster population. When calculating the travel time of residents to the point of health care, the centers of the grids were regarded as residential locations. Each type of road was set up with a specific speed based on the Highway Technical Standards and the actual situation in China. Specifically, we set 60km/h for county roads, 40 km/h for township roads, and 30 km/h for village roads. Residents are confined to walking to the closest road at 5 km/h before traveling by vehicles.48
Enhanced Two-Step Floating Catchment Area Method
We used the Enhanced two-step Floating Catchment Area Method (E2SFCAM) to measure the spatial access to health care, as it applies weights to different travel time zones to account for a distance-decay effect.49 It involves 3 basic steps:
| (1) |
| (2) |
| (3) |
Firstly, calculate the healthcare resources provided by healthcare institutions supply-to-population ratio Rj, searching all population locations (i) within the catchment area (Dr) using the decay function (f(dij)) from healthcare institutions j (includes general hospitals, specialist hospitals, township health centers, and village clinics). Sj is the health professionals or doctors or nurses or beds of healthcare institutions j. dij is the travel time between population locations i and healthcare institutions j.
Secondly, calculate the spatial access for the population in grid i. Similarly, for the healthcare institution j in the spatial catchment, the ratio Rj is weighted by the decay function (f(dij)). Following former literature, the decay function is calculated via equation (4).47,50,51 The Gaussian function, which was introduced on the decay function in our study, can continuously account for the distance decay of accessibility within a catchment and remove the burden of determining the number of zones, thus reasonably simulating the spatial relationship between supply and demand.51 -53 The less time it spends between the healthcare institution j and population location i, the higher the weight is. The maximum catchment area for healthcare institutions is considered 90 minutes.47 The “golden hour” is the term often used in trauma or emergency care to suggest that an injured or sick person must receive definitive treatment within the first 60 minutes from the time of injury or appearance of symptoms. Following the suggestion, 60 minutes travel time is usually set up as the maximum catchment area.54 -56 Given the fact that Chishui was still a poor rural area where the travel burden of seeking care was supposed to be heavier than average, 90 minutes was set up in our study as the maximum catchment according to evidences from the relevant literature.
| (4) |
We used ArcGIS 10.5 to obtain travel times between the healthcare institutions and the population location, and further calculated the spatial access of each grid and village using R 4.0.3.
Chain Substitution Method
The chain substitution method (CSM) was utilized to quantify the relative contributions of 3 local factors to changes in spatial access to health care. This method was initially used to estimate the impacts of different factors on regional economic change,57,58 and then adapted to spatial access studies.20,59,60 We used this method to quantify the impacts of population demand, healthcare resourcing, and transportation linkage on spatial access in the process of rapid developments in Chishui. The application of the chain substitution method is valid when the substitution factors vary independently.61 Therefore, we examined the correlation between the substitution factors before starting. Given that the policies were usually implemented by the administrative divisions, such as village, township, county, city, and province, we used the village as the analysis unit when decomposing the factors’ contribution in our study.
The replacement order for the chain substitution method would follow 2 principles: (1) quantitative factors would be replaced first, followed by qualitative factors; (2) the replacement order of the factors would be arranged according to their importance degree, with more important factors replaced prior to less important ones.61 Following the 2 principles, the factor substitution order would be based on the specific analysis. Considering health service utilization initially derived from patient demand, then the provision of health services fulfilling the patient demand, until to the connection between the supply and demand sides, the replacing order in our analysis was arranged as follows: the population, healthcare institutions, and road network. This sequence was also adopted by the 3 relevant studies from the current literature.20,59,60
Firstly, calculate spatial access to health care of village V at time T by a generic function of 3 local factors, denoted as :
| (5) |
Where represent population demand, healthcare resourcing, and transportation linkage of village V at time T, respectively.
Secondly, calculate the impact of population demand on spatial access by substituting the population demand at time T + 1 replacing that at time T, as follows:
| (6) |
Similar to the way above, then replace healthcare resourcing and transportation linkage with their values at time T + 1 in turn, respectively.
| (7) |
| (8) |
When all factors are replaced by the value at time T + 1, the computed result of the function is the value of spatial access at time T + 1, denoted as .
Thirdly, calculate the absolute contributions of different factors, including population demand I (∆PV), healthcare resourcing I (∆HV), and transportation linkage I (∆LV). The detailed process is as follows:
| (9) |
Lastly, to compare the relative contributions and convert to the standardized impacts into percentages, as shown in follow:
| (10) |
The higher the percentage, the more important the factor is in explaining the variation in spatial access to health care. A positive value means that the factor leads to an increase in spatial access, while a negative value means that the factor leads to a decrease in spatial access.
Results
Changes of Population Distribution, Healthcare Resourcing, and Transportation Infrastructure
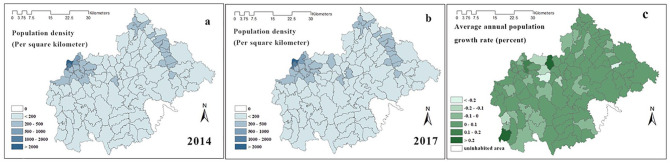
From 2014 to 2017, the total population of Chishui grew from 310 088 to 310 775. Figure 2 shows the population density in 2014 and 2017. The population distribution patterns were similar in both 2014 and 2017 (see Figure 2a and b). The number of populations had a slight fluctuation in most villages, except for Lianhua Village and Jinpingshan Village where the average annual population growth rates exceeded 0.2% (see the darkest colored part in Figure 2c). In addition to the natural growth or decline of the population in each village, population relocation was also a significant contributor to the changed patterns of population distribution at the village level. We found that most residents were clustered in villages around the administrative center, while in the eastern part, the residents mainly resided in villages along the country roads.
Figure 2.
Population density in (a) 2014, (b) 2017, and (c) average annual population growth rate.
Note. The villages with the darkest colors in (c) are Lianhua Village and Jinpingshan Village.
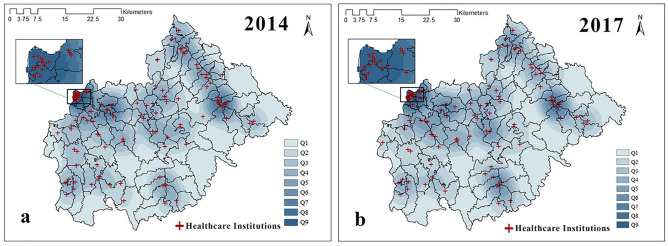
Figure 3 shows the distribution of healthcare institutions across Chishui from 2014 to 2017. The healthcare institutions were mainly located near the administrative center. From 2014 to 2017, the number of healthcare institutions slightly increased. In 2014, the total number of healthcare institutions was 134, including 12 hospitals, 22 township health centers, and 100 village clinics. In 2017, the total number of healthcare institutions increased to 136 with 2 newly constructed hospitals added into the region.
Figure 3.
Geographic distribution of healthcare institutions in Chishui in (a) 2014 and (b) 2017.
Note. Q1 to Q9 represent the cluster degree of healthcare institutions based on Kernel Density Analysis in ArcGIS 10.5, higher numbers indicate higher cluster degree.
Healthcare resources provided by healthcare institutions increased rapidly from 2014 to 2017. Table 1 shows the growth trends of different types of healthcare resources. The number of nurses had the fastest growth rate, while the number of hospital beds had the slowest growth rate but produced the largest amount of growth in quantity.
Table 1.
The Changes of Healthcare Resources From 2014 to 2017.
| Different kinds of healthcare resources | 2014 | 2017 | Annual growth rate (%) |
|---|---|---|---|
| Health professionals | 1380 | 2073 | 14.53 |
| Doctors | 372 | 603 | 17.47 |
| Nurses | 484 | 897 | 22.83 |
| Beds | 1863 | 2652 | 12.49 |
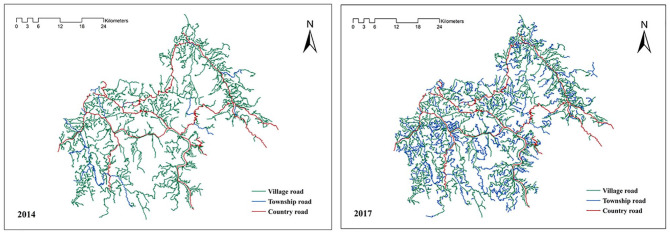
The construction of transportation infrastructure in Chishui has been significantly improved over the study period. In 2014, the total length of the transportation network was 2485 km, which increased by 1228 to 3687 km in 2017. Compared to that of 2014, both village and township road constructions have been expanded by the end of 2017. Figure 4 shows the changes in the transportation network from 2014 to 2017.
Figure 4.
The comparison of transportation infrastructure between (a) 2014 and (b) 2017 in Chishui.
Spatial Access to Health Care Over Time
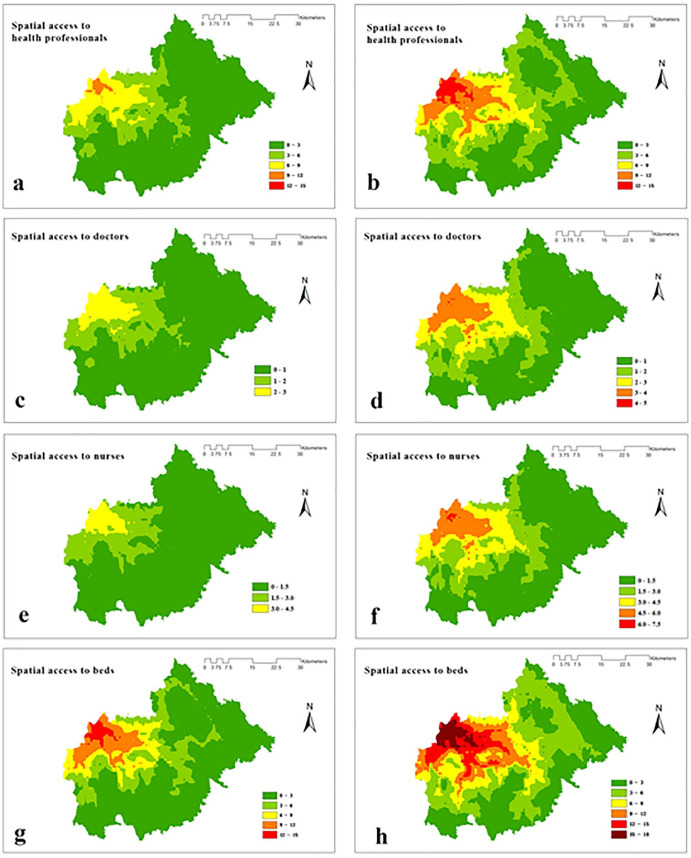
Figure 5 shows the spatial access to health care in the county during the period of 2014 and 2017. From 2014 to 2017, spatial access to health care in the administrative center remained at a good level, with gradually improved spatial accessibility of medical services among the surrounding outskirts. In general, spatial access to all kinds of healthcare resources in the county increased substantially from 2014 to 2017, with an increase of 2.22 health professionals, 0.74 doctors, 1.33 nurses, and 2.53 hospital beds per thousand residents respectively. Spatial access to health professionals and beds in the eastern region demonstrated a significant increase. Spatial access to healthcare resources of Chishui county and its villages were shown in Table 2. Spatial access to all kinds of healthcare resources showed considerable improvement in almost all villages.
Figure 5.
Spatial access to health professionals (a), doctors(c), nurses(e), and beds(g) in 2014 and spatial access to health professionals(b), doctors(d), nurses(f), and beds(h) in 2017.
Table 2.
Spatial Access to Health Care (per thousand residents).
| Spatial access | County | Villages | |||||
|---|---|---|---|---|---|---|---|
| Max | Min | Median | Q1 | Q3 | IQR | ||
| Health professionals | |||||||
| 2014 | 4.45 | 9.31 | 0.53 | 2.14 | 1.53 | 4.92 | 3.40 |
| 2017 | 6.68 | 13.16 | 0.76 | 3.58 | 2.35 | 7.98 | 5.63 |
| Doctors | |||||||
| 2014 | 1.20 | 2.54 | 0.13 | 0.54 | 0.37 | 1.37 | 1.01 |
| 2017 | 1.94 | 3.92 | 0.17 | 1.02 | 0.60 | 2.36 | 1.76 |
| Nurses | |||||||
| 2014 | 1.56 | 3.60 | 0.11 | 0.51 | 0.32 | 1.75 | 1.43 |
| 2017 | 2.89 | 5.98 | 0.27 | 1.38 | 0.80 | 3.51 | 2.71 |
| Beds | |||||||
| 2014 | 6.01 | 12.90 | 0.48 | 2.71 | 1.87 | 6.67 | 4.78 |
| 2017 | 8.54 | 16.71 | 0.90 | 4.50 | 2.98 | 10.36 | 7.42 |
Note. Q1 = first quartile; Q3 = third quartile; IQR = interquartile range.
Relative Contributions of Local Factors
We found that the independence between 2 substitution factors was weak. Although the correlation among different healthcare resources was strong, it did not influence the results. The specific values are shown in Table 3.
Table 3.
Correlation Coefficients Among 3 Major Factors.
| Population demand | Healthcare supply | Road network density | ||||
|---|---|---|---|---|---|---|
| Health professionals | Doctors | Nurses | Beds | |||
| Population demand | 1 | - | - | - | - | - |
| Healthcare supply | ||||||
| Health professionals | 0.236 | 1 | - | - | - | - |
| Doctors | 0.157 | 0.729 | 1 | - | ||
| Nurses | 0.132 | 0.701 | 0.841 | 1 | - | |
| Beds | 0.127 | 0.700 | 0.841 | 0.998 | 1 | - |
| Road network density | 0.058 | 0.007 | 0.137 | 0.122 | 0.116 | 1 |
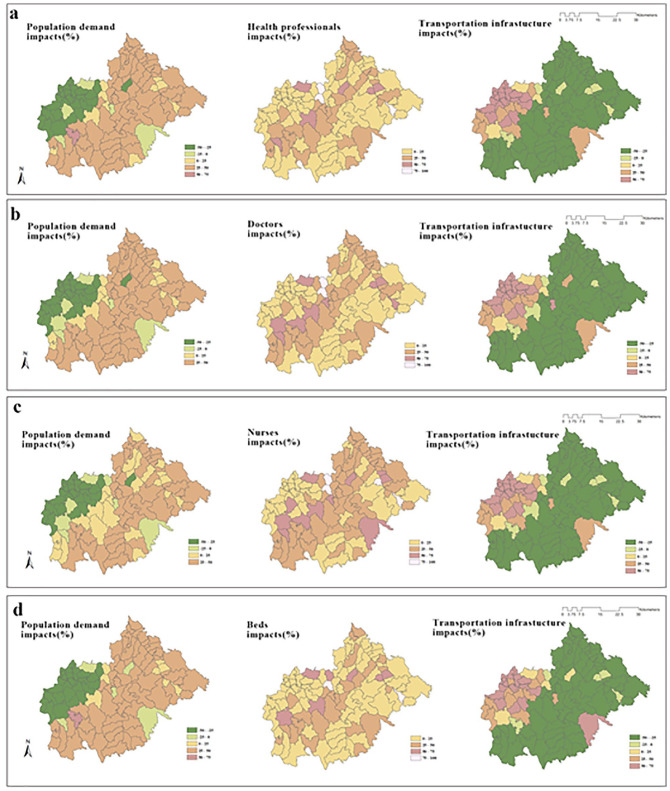
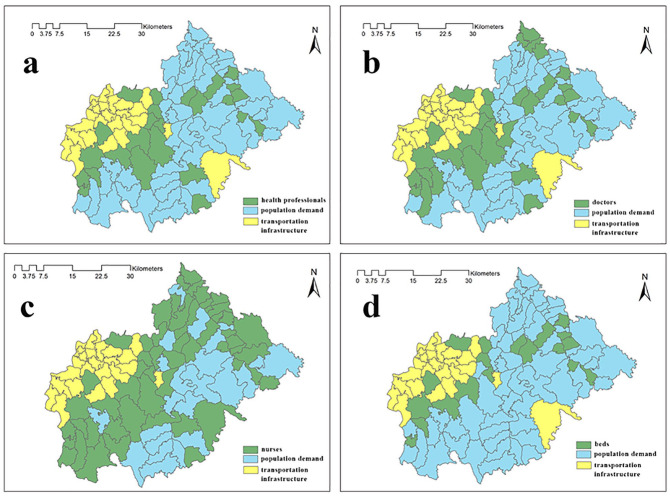
Figure 6 shows the relative contributions of 3 local factors to the improvements in spatial access to health professionals, doctors, nurses, and beds at the village level. Among different villages, the patterns of the relative contributions of the 3 local factors showed apparent variations. Population changes had both negative and positive effects on spatial access to health care for villages. In the villages with a relatively large population size surrounding the administrative center, the relative contributions of population demand were negative, while on the outskirts the relative contributions of population demand were positive. The relative contributions of healthcare resourcing were all positive due to the sharp increases in the absolute numbers of healthcare resources. The increases of healthcare resources posed more impacts (25%-75%) on the outskirts compared with villages around the administration center (0%-25%). Both negative and positive effects on the changes in spatial access to health care were observed as the result of the expansion of the road network.
Figure 6.
Relative contributions of the 3 local factors to spatial access to health professionals (a), doctors (b), nurses (c), and beds (d)for villages.
Figure 7 shows the main positive contributor to the spatial accessibility of different types of healthcare resources. For about 25% of villages, transportation infrastructure made the greatest contributions (50%-75%) to the increases in spatial access to health care. For the other 75% of villages, healthcare resourcing and population demands were the main positive contributors. The growth rate of nurses was found to be the fastest among all types of healthcare resources, which served as the predominant contributor to increased healthcare resourcing among 52% of all villages. In contrast, the growth rate of hospital beds presented to be the slowest, which only served as the primary determinant of increased healthcare resourcing among 19% of all villages. Villages where transportation infrastructure expansion served as the main contributor to improved spatial access to health care were mainly clustered around the administrative center.
Figure 7.
The main positive contributor to spatial accessibility of health professionals (a), doctors (b), nurses (c), and beds (d) for villages.
Discussion
China has been confronted with limited spatial access to health care in its impoverished rural areas.62,63 Quite a number of previous studies have highlighted the lack of timely access to health care in rural China as a critical issue to be addressed at the governmental level to inform health-related policy-making procedures. Prior to the implementation of the Targeted Poverty Reduction Project, nearly 400 000 impoverished residents in China were not able to have timely access to seeking medical services as reported in 2014, for which the locations of healthcare institutions being too far away from residential areas was the major obstacle in the process of medical service utilization.64 Since the initiation of the Targeted Poverty Reduction Project at the end of 2015 a series of strategies has been adopted by the Chinese government to raise residents living below the national poverty line out of poverty by the end of 2020, which included ensuring residents’ access to basic medical services.23 The significant increase in spatial access to health care in Chishui over the past few years, as a remarkable milestone achieved by the Targeted Poverty Alleviation Project, has validated the effectiveness of those interventions implemented among those impoverished regions.
Understanding the Contributions of 3 Factors
The positive and negative impacts of population change on spatial access to health care are explainable. Specifically, population growth naturally increases residents’ demand for healthcare services, leading to intensified competition for limited healthcare resources, which further results in the reduction of spatial accessibility of healthcare. In previous studies where regression models were adopted, higher population density was typically found to be associated with increased spatial accessibility of healthcare.65,66 Such phenomenon is reflective of a balance between the supply and population demand, which means that people tend to move to places where they have better access to health care or living conditions, while the delivery of healthcare services tends to be clustered in places with greater demand. However, these results ignored the fact that residents’ competition for limited healthcare resources would be intensified by increased population demand, thus leading to reduced spatial accessibility of health care.
The sharply increased amount of healthcare resources distributed across Chishui could be attributed to the successful implementation of the health poverty alleviation project, which is an essential component of the Targeted Poverty Alleviation Project. As we all know, retaining and recruiting health professionals in rural and remote areas is a difficult and challenging task,67,68 as most health workers would choose to move to higher-level healthcare institutions located in more developed areas instead of working for rural and remote areas with dis-satisfactory compensation, limited career development opportunities as well as poor living conditions.69 Under the Health Poverty Alleviation Project, China has made considerable investments in increasing its healthcare resources to facilitate the development of impoverished rural areas, while efforts have also been made by the government to improve the medical service capacity of healthcare institutions via increasing healthcare workforce through education, regulation, financial incentives, management and social systems support.70 For example, quite a number of healthcare professionals and medical students have been hired as prospective general practitioners to work for rural and remote areas based on the employment contracts that would exempt tuition fees needed throughout students’ medical training programs. Meanwhile, experienced doctors and nurses from several leading hospitals in developed areas have been assigned to different rural healthcare institutions to provide one-on-one assistance in the establishment of key clinical departments as well as the introduction of medical projects.
The impacts of transportation infrastructure on changes in spatial access to health care produced interesting findings that the magnitude of transportation infrastructure impacts in our study presented to be greater than those reported in previous studies.59,60 This is not difficult to understand as in previous studies, transportation infrastructure had little change over the study periods, while in our study area the construction of the transportation network has undergone tremendous changes during the 4 years. The slogan “build the road first if you want to become rich” (yao xiang fu, xian xiu lu) is prevailing in rural China, which indicates that the enhancement of transportation infrastructure construction should be addressed as a top priority in order to achieve poverty alleviation in poverty-stricken counties in China. As part of our findings, both positive and negative effects of transportation infrastructure on spatial access to health care among rural villages were observed. One plausible explanation is that transportation infrastructure expansion has enabled residents to seek medical services from a wider range of medical institutions, while such improved transportation construction has also intensified residents’ competition for limited health services.20,59,60 In our study, the transportation infrastructure expansion seems to be more beneficial in villages that previously had better spatial access to health care.
Comparison With Relevant Studies
There are even less evidences from the current literature that can be directly compared to the findings of our study. For example, a decomposition of Florida’s accessibility contribution, using the same methodology as ours, found that increased physicians was the main factor that contributors to healthcare accessibility improvement, especially in the first 10 years, when 95% of study regions had increased physicians as the most significant contributor to improved regional healthcare accessibility.20 In contrast, we found that in the short term in Chishui, population distribution, health resources, and road networks were similarly dominant as contributors to healthcare accessibility across the entire study area. This was mainly because Florida’s policies implemented at the time of study were mainly focused on attracting healthcare workers to places where there was a shortage of resources, which failed to involve other demographic, transport interventions. Two other studies used the same approach to decompose dynamic accessibility in metropolitan areas, but instead of healthcare accessibility, they decomposed food accessibility and green park accessibility respectively.59,60 These 2 studies both arrived at a conclusion that population change and food/green park resources posed greater impacts on accessibility compared with transportation infrastructure. This is slightly different from our findings, probably due to the differences between urban and rural characteristics, namely metropolitan areas already have well-connected communities with densely populated population, whereas rural areas have a dispersed population and poorly-developed transportation network.
Implications for Rural Health Care
Most of health reforms have been oriented toward spatial accessibility outcomes under, ignoring the role of the 3 factors on changes in spatial accessibility.71,72 Despite the eventual success of the reform, it remains unknown which specific policy interventions actually posed effective impacts to result in desired outcomes. There were also lessons learned from the current literature regarding reform-induced failures, such as a study in Portugal that reported the reduction of accessibility in its rural areas after the implementation of the health reform as an undesired consequence. The authors attributed this to not taking into account the duration of travel time spent between where people live, where transport hubs are located, and where emergency services are delivered.73 This again highlights the importance that policymakers should consider not only the amount of healthcare resources, but also the connections between population distribution, health resources, and transport networks.
To achieve the universal goal of improving equity in spatial access to health care,36 more attention has been paid to rural and remote areas among worldwide nations,56 with a relatively sparse population, fragile transportation infrastructures and limited healthcare resourcing.29 However, how to effectively improve spatial access to health care in those underdeveloped areas with limited financial resources remains a tough issue for low- and middle-income countries. Decisionmakers should take into account the duration of travel time spent between where people live, where transport hubs are located, and where healthcare services are delivered throughout the process of formulating policies toward rural healthcare planning. It should be noted that in practice, well-planned investments should be made by decision-makers under financial constraints in order to achieve the optimal outcome that balances all those 3 dimensions, namely population layout, resource allocation, and transport infrastructure. According to our study, in areas with underdeveloped transportation infrastructure and inadequate healthcare resources, the priority task is to optimize the population distribution to be tailored for the allocation of healthcare resources while increasing the total amount of medical resources across those regions. In contrast, in the areas where the population distribution and healthcare resource allocations are properly matched, the enhancement of regional transportation infrastructure construction should be considered as a more effective approach.
The COVID-19 pandemic has created an unprecedentedly challenging climate for healthcare resource allocation, especially in rural areas, where residents previously had poor access to quality healthcare as well as well-constructed transportation networks are now more likely to suffer from the pandemic.42 It has been reported by recent studies that healthcare resource availability is potentially associated with COVID-19 mortality.74 Under such context, the optimization of healthcare resource allocation should be oriented toward well-balanced geographic distributions of healthcare resources and residential areas, as well as access to transport networks. Under financial constraints, it is rather essential that prudent investments be made to achieve the optimal layout for population and resource distribution, as well as easily accessible transportation networks.
Several limitations should be noted in our study. Firstly, potential spatial access was calculated in our research without considering patients’ preference for healthcare institutions, which might be influenced by the quality of healthcare resources provided by healthcare institutions as well as varied socioeconomic status of patients.75 Secondly, measuring healthcare accessibility should typically take into account the impacts posed by multiple essential dimensions embedded in healthcare resources. However, considering that a comprehensive index cannot reflect the impacts that each particular policy actually posed on healthcare accessibility, we instead conducted separate analyses on each dimension embedded in the regional healthcare resources to produce more meaningful outcomes to help understand the respective contribution of each dimension investigated. Thirdly, due to the in-availability of relevant data, we were not able to conduct a cost-benefit analysis for the 3 local factors to make our conclusions more convincing. Despite all these limitations, the study provides an opportunity to understand the trends of spatial access to health care over space and time as well as the impact of the 3 local factors on spatial access, which is expected to provide evidence-based implications to inform policy making procedures in terms of improving residents’ spatial accessibility of health care in a particular region based on predominant factors identified. The findings are also expected to provide empirical evidence for low- and middle-income countries confronted with similar situations.
Conclusions
This study examined the improvements in spatial access to health care in Chishui from 2014 to 2017 as well as the relative contributions of 3 local factors (population demand, healthcare resourcing, transportation linkages/infrastructure) on the changes in spatial accessibility over the study period. As a remarkable milestone achieved by the Targeted Poverty Reduction Project, residents’ spatial access to health care was significantly improved from 2014 to 2017. For different villages, the patterns of the relative contributions of the 3 local factors showed apparent variations. Specifically, the sharp increase in healthcare resources among all villages indicated that the relative contributions of healthcare resourcing posed positive impacts on residents’ spatial access to health care across the entire study area. In contrast, population changes and transportation infrastructure expansion posed both negative and positive effects on spatial access to health care for different villages. The dominant factor affecting changes in accessibility was not necessarily supply, but also demand and transportation. Limited by financial constraints, the predominant factors associated with regional spatial access to health care should be highlighted as priority aspects to be improved during policy-making procedures based on region-specific conditions. For example, for villages with poorly-established transportation infrastructure, the optimization of population distribution and healthcare resourcing should be considered as the priority. In contrast, the expansion of transportation infrastructure should be adopted as the priority strategy in areas with relatively good spatial accessibility as the marginal effects induced by such a strategy would become stronger with increased spatial accessibility. Especially during the COVID-19 pandemic, which has created an urgent need for improving healthcare accessibility. Decision-makers should take into account the duration of travel time spent between where people live, where transport hubs are located, and where healthcare services are delivered in the process of formulating policies toward rural healthcare planning. This study offers new insights into the relative contribution of local factors to temporal changes in spatial access to health care in impoverished and rural areas, which is expected to provide evidence-based implications to inform healthcare planning procedures in low- and middle-income countries.
Acknowledgments
We thank Yili Yang, Xiuli Wang, Chao Song, Xiaoshuang Zhao, Yufan Deng, Peiya Cao from Sichuan University for their valuable and technical suggestions.
Footnotes
Authors’ Contributions: JP conceived the study. LC analyzed the relevant data and wrote the first draft of the manuscript. JP and CC contributed to the interpretation of the results and manuscript revision. JP, CC, LC, TC, and TL revised the manuscript. All the authors approved the final version.
Availability of Data and Materials: The data that support the findings of this study are available from the Chishui Health and Family Planning Bureau and the Chishui Office of Poverty Alleviation and Development, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Health Commission of Chishui.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Foundation of China under Grant No. 72074163, The National Social Science Fund of China Grant No. 21ZDA104, Taikang Yicai Public Health and Epidemic Control Fund, Bill & Melinda Gates Foundation Grant No. OPP1178967, Sichuan Science and Technology Program Grant No. 2022YFS0052, Chengdu Federation of Social Science Association under Grant No. ZZ05, China Postdoctoral Science Foundation under Grant No. 2020M683298.
Ethics Approval and Consent to Participate: This study has been approved by the ethics committee of Sichuan University, China, and the approval number is K2018087. Data applied in our analysis were secondary data and extracted by corresponding government departments or from publicly available yearbooks, and no human participants were involved. The authors obtained all necessary administrative permission from the Health Commission of Chishui to access data used in this study.
Consent for Publication: Not applicable.
ORCID iDs: Lingwei Chen  https://orcid.org/0000-0002-6335-6421
https://orcid.org/0000-0002-6335-6421
Tianjiao Lan  https://orcid.org/0000-0003-4373-3477
https://orcid.org/0000-0003-4373-3477
References
- 1. WHO. Sustainable health financing, universal coverage and social health insurance. 2005. Accessed August 21, 2021. http://apps.who.int/iris/bitstream/handle/10665/20383/WHA58_33-en.pdf;jsessionid=82ED582BA6CC3E9E96ECE617C72A055B?sequence=1
- 2. Bloom G, Katsuma Y, Rao KD, Makimoto S, Yin JDC, Leung GM. Next steps towards universal health coverage call for global leadership. BMJ. 2019;365:l2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shan L, Wu Q, Liu C, et al. Perceived challenges to achieving universal health coverage: a cross-sectional survey of social health insurance managers/administrators in China. BMJ Open. 2017;7(5):e014425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Birn AE, Nervi L. What matters in health (care) universes: delusions, dilutions, and ways towards universal health justice. Global Health. 2019;15:0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goddard M, Smith P. Equity of access to health care services: theory and evidence from the UK. Soc Sci Med. 2001;53(9):1149-1162. [DOI] [PubMed] [Google Scholar]
- 6. Tian F, Pan J. Hospital bed supply and inequality as determinants of maternal mortality in China between 2004 and 2016. Int J Equity Health. 2021;20(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192-1204. [DOI] [PubMed] [Google Scholar]
- 8. Moodley J, Ross E. Inequities in health outcomes and access to health care in South Africa: a comparison between persons with and without disabilities. Disabil Soc. 2015;30(4):630-644. [Google Scholar]
- 9. World Bank Group. GOING UNIVERSAL: How 24 developing countries are implementing universal health coverage reforms from the bottom up. 2015. Accessed August 21, 2021. https://www.worldbank.org/en/topic/universalhealthcoverage/publication/going-universal-how-24-countries-are-implementing-universal-health-coverage-reforms-from-bottom-up
- 10. Song Y, Tan Y, Song Y, et al. Spatial and temporal variations of spatial population accessibility to public hospitals: a case study of rural—urban comparison. GISci Remote Sens. 2018;55(5):718-744. [Google Scholar]
- 11. Tang JH, Chiu YH, Chiang PH, Su MD, Chan TC. A flow-based statistical model integrating spatial and nonspatial dimensions to measure healthcare access. Health Place. 2017;47:126-138. [DOI] [PubMed] [Google Scholar]
- 12. Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131-146. [DOI] [PubMed] [Google Scholar]
- 13. Gu X, Zhang L, Tao S, Xie B. Spatial accessibility to healthcare services in metropolitan suburbs: the Case of Qingpu, Shanghai. Int J Environ Res Public Health. 2019;16(2):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Talen E. Neighborhoods as service providers: a methodology for evaluating pedestrian access. Environ Plann B-Plann Des. 2003;30(2):181-200. [Google Scholar]
- 15. Fransen K, Neutens T, De Maeyer P, Deruyter G. A commuter-based two-step floating catchment area method for measuring spatial accessibility of daycare centers. Health Place. 2015;32:65-73. [DOI] [PubMed] [Google Scholar]
- 16. Luo W, Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago Region. Environ Plann B Plann Des. 2003;30(6):865-884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang X, Yang H, Duan Z, Pan J. Spatial accessibility of primary health care in China: a case study in Sichuan Province. Soc Sci Med. 2018;209:14-24. [DOI] [PubMed] [Google Scholar]
- 18. Ahmed S, Adams AM, Islam R, Hasan SM, Panciera R. Impact of traffic variability on geographic accessibility to 24/7 emergency healthcare for the urban poor: a GIS study in Dhaka, Bangladesh. PLoS One. 2019;14(9):e0222488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paul J, Edwards E. Temporal availability of public health care in developing countries of the Caribbean: an improved two-step floating catchment area method for estimating spatial accessibility to health care. Int J Health Plann Manage. 2019;34(1):e536-e56. [DOI] [PubMed] [Google Scholar]
- 20. Yang J, Mao L. Understanding temporal change of spatial accessibility to healthcare: an analytic framework for local factor impacts. Health Place. 2018;51:118-124. [DOI] [PubMed] [Google Scholar]
- 21. Cerf ME. Health worker resourcing to meet universal health coverage in Africa. Int J Healthc Manag. 2021;14(3):789-796. [Google Scholar]
- 22. Iyer HS, Flanigan J, Wolf NG, et al. Geospatial evaluation of trade-offs between equity in physical access to healthcare and health systems efficiency. BMJ Glob Health. 2020;5(10): e003493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Central Government of the People’s Republic of China. Decision on winning the fight against poverty. 2015. Accessed May 4, 2021. http://www.gov.cn/xinwen/2015-12/07/content_5020963.htm
- 24. The State Council of the People’s Republic of China. China’s policy of relocating poor people from inhospitable areas. 2018. Accessed November 17, 2021. https://www.ndrc.gov.cn/fzggw/jgsj/dqs/sjdt/201803/t20180330_1050716.html?code=&state=123
- 25. The State Council of the People’s Republic of China. The Ministry of Education and other six departments issued a notice on the 13th five-year plan for poverty alleviation through education. 2016. Accessed November 17, 2021. http://www.gov.cn/xinwen/2016-12/29/content_5154106.htm#1
- 26. The State Council of the People’s Republic of China. Guidelines on implementing Health Poverty Alleviation Projects. 2016. Accessed November 17, 2021. http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/33978/34697/xgzc34703/Document/1481192/1481192.htm
- 27. The State Council Information Office of the People’s Republic of China. Poverty alleviation: China’s experience and contribution. 2021. Accessed May 4, 2021. http://www.gov.cn/zhengce/2021-04/06/content_5597952.htm
- 28. Pan J, Chen C, Yang Y. Building a global community of shared future free from poverty. Glob Health J. 2021;5(3):113-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T. Perceived barriers to health care access among rural older adults: A qualitative study. J Rural Health. 2005;21(3):206-213. [DOI] [PubMed] [Google Scholar]
- 30. Knaul FM, Arreola-Ornelas H, Méndez-Carniado O, et al. Evidence is good for your health system: policy reform to remedy catastrophic and impoverishing health spending in Mexico. Lancet. 2006;368(9549):1828-1841. [DOI] [PubMed] [Google Scholar]
- 31. Li X, Cochran C, Lu J, et al. Understanding the shortage of village doctors in China and solutions under the policy of basic public health service equalization: evidence from Changzhou. Int J Health Plann Manage. 2015;30(1):E42-E55. [DOI] [PubMed] [Google Scholar]
- 32. National Bureau of Statistics of the People’s Republic of China. China rural poverty monitoring report. 2018. Accessed November 13, 2022. https://t.cnki.net/kcms/article/abstract?v=szG_SvYQhKwsa3maN7KEfbFV7cw2XoewNBDL3xPyK7X45XqqXR1nTDQWAy2u8Uy3Dsy0Wdr9FChLJ8ZVnKcIdIjTHjPgiT0Y0o5D_fOMMM8sEP1v_hhsfQ==&uniplatform=NZKPT
- 33. Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127-140. [DOI] [PubMed] [Google Scholar]
- 34. Guagliardo MF. Spatial accessibility of primary care: concepts, methods, and challenges. Int J Health Geogr. 2004;3(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Luo W, Whippo T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place. 2012;18(4):789-795. [DOI] [PubMed] [Google Scholar]
- 36. Wang X, Seyler BC, Han W, Pan J. An integrated analysis of spatial access to the three-tier healthcare delivery system in China: a case study of Hainan Island. Int J Equity Health. 2021;20(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McGrail MR. Spatial accessibility of primary health care utilising the two step floating catchment area method: an assessment of recent improvements. Int J Health Geogr. 2012;11:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Langford M, Fry R, Higgs G. Measuring transit system accessibility using a modified two-step floating catchment technique. Int J Geogr Inf Sci. 2012;26(2):193-214. [Google Scholar]
- 39. Wan N, Zou B, Sternberg T. A three-step floating catchment area method for analyzing spatial access to health services. Int J Geogr Inf Sci. 2012;26(6):1073-1089. [Google Scholar]
- 40. Luo J. Integrating the Huff model and floating catchment area methods to analyze spatial access to healthcare services. Trans GIS. 2014;18(3):436-448. [Google Scholar]
- 41. Ghorbanzadeh M, Kim K, Ozguven EE, Horner MW. A comparative analysis of transportation-based accessibility to mental health services. Transp Res D-Transp Environ. 2020;81:102278. [Google Scholar]
- 42. Kim K, Ghorbanzadeh M, Horner MW, Ozguven EE. Identifying areas of potential critical healthcare shortages: a case study of spatial accessibility to ICU beds during the COVID-19 pandemic in Florida. Transp Policy. 2021;110:478-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pan J, Zhao H, Wang X, Shi X. Assessing spatial access to public and private hospitals in Sichuan, China: the influence of the private sector on the healthcare geography in China. Soc Sci Med. 2016;170:35-45. [DOI] [PubMed] [Google Scholar]
- 44. Liu Z, et al. Zunyi yearbook. 2015. Accessed August 22, 2021. https://navi.cnki.net/knavi/yearbooks/YZYNJ/detail
- 45. Statistic Bureau of Chishui. Statistical communique on the national economic and social development of Chishui City in 2017. 2018. Accessed August 22, 2021. http://www.gzchishui.gov.cn/ztzl/tzcs/tzhj/rkjy_5150334/202003/t20200320_55376422.html
- 46. National Bureau of Statistics. Resident income and consumer spending in 2014. 2014. Accessed September 18, 2021. https://data.stats.gov.cn/easyquery.htm?cn=A01&zb=A010301&sj=201412
- 47. Chen T, Pan J. The effect of spatial access to primary care on potentially avoidable hospitalizations of the elderly: evidence from Chishui City, China. Soc Indic Res. 2022;160:645-665. [Google Scholar]
- 48. Pan J, Liu H, Wang X, Xie H, Delamater PL. Assessing the spatial accessibility of hospital care in Sichuan Province, China. Geospat Health. 2015;10(2):384. [DOI] [PubMed] [Google Scholar]
- 49. Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place. 2009;15(4):1100-1107. [DOI] [PubMed] [Google Scholar]
- 50. Shi L. The impact of primary care: a focused review. Scientifica. 2012;2012:432892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shi X, Alford-Teaster J, Onega T, Wang D. Spatial access and local demand for major cancer care facilities in the United States. Ann Assoc Am Geogr. 2012;102(5):1125-1134. [Google Scholar]
- 52. Dai D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place. 2010;16(5):1038-1052. [DOI] [PubMed] [Google Scholar]
- 53. Nakamura T, Nakamura A, Mukuda K, Harada M, Kotani K. Potential accessibility scores for hospital care in a province of Japan: GIS-based ecological study of the two-step floating catchment area method and the number of neighborhood hospitals. BMC Health Serv Res. 2017;17:438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Huang Y, Meyer P, Jin L. Spatial access to health care and elderly ambulatory care sensitive hospitalizations. Public Health. 2019;169:76-83. [DOI] [PubMed] [Google Scholar]
- 55. McGrail MR, Humphreys JS. The index of rural access: an innovative integrated approach for measuring primary care access. BMC Health Serv Res. 2009;9:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wang X, Pan J. Assessing the disparity in spatial access to hospital care in ethnic minority region in Sichuan Province, China. BMC Health Serv Res. 2016;16:399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Balakrishnan N. Methods and Applications of Statistics in Business, Finance, and Management Science. John Wiley & Sons; 2010. [Google Scholar]
- 58. Vaninsky AY. The Factor Analysis of Economic Activity. Moscow. Finance and Statistics (In Russian); 1984. [Google Scholar]
- 59. Hu L, Zhao C, Wang M, Su S, Weng M, Wang W. Dynamic healthy food accessibility in a rapidly urbanizing metropolitan area: socioeconomic inequality and relative contribution of local factors. Cities. 2020;105:102819. [Google Scholar]
- 60. Li Z, Wei H, Wu Y, Su S, Wang W, Qu C. Impact of community deprivation on urban park access over time: understanding the relative role of contributors for urban planning. Habitat Int. 2019;92:102031. [Google Scholar]
- 61. García-Vidal G, Pérez-Campdesuñer R, Sánchez-Rodríguez A, Martínez-Vivar R. Chain substitution and successive approximation method: throughput analysis at SMEs. Int J Eng Bus Manag. 2019;11:1-12. [Google Scholar]
- 62. Meng Q, Zhang J, Yan F, Hoekstra EJ, Zhuo J. One country, two worlds—the health disparity in China. Glob Public Health. 2012;7(2):124-136. [DOI] [PubMed] [Google Scholar]
- 63. Song S, Yuan B, Zhang L, et al. Increased inequalities in health resource and access to health care in rural China. Int J Environ Res Public Health. 2018;16(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. National Bureau of Statistics of the People’s Republic of China. China rural poverty monitoring report. 2015. Accessed June 10, 2021. https://navi.cnki.net/KNavi/YearbookDetail?pcode=CYFD&pykm=YPKJC&bh=
- 65. Liu S, Qin Y, Xu Y. Inequality and influencing factors of spatial accessibility of medical facilities in rural areas of China: a case study of Henan Province. Int J Environ Res Public Health. 2019;16(10):1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hu S, Song W, Li C, Lu J. A multi-mode Gaussian-based two-step floating catchment area method for measuring accessibility of urban parks. Cities. 2020;105:102815. [Google Scholar]
- 67. Shah TI, Milosavljevic S, Bath B. Measuring geographical accessibility to rural and remote health care services: challenges and considerations. Spat Spatiotemporal Epidemiol. 2017;21:87-96. [DOI] [PubMed] [Google Scholar]
- 68. Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet. 2017;390(10112):2584-2594. [DOI] [PubMed] [Google Scholar]
- 69. Meng Q, Yuan J, Jing L, Zhang J. Mobility of primary health care workers in China. Hum Resour Health. 2009;7:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. The State Council of the People’s Republic of China. National healthcare policy announcement of strategic plan on national healthcare service system (2015-2020). 2015. Accessed August 2, 2021. http://www.gov.cn/zhengce/content/2015-03/30/content_9560.htm
- 71. Jamtsho S, Corner R, Dewan A. Spatio-temporal analysis of spatial accessibility to primary health care in Bhutan. ISPRS Int J Geo Inf. 2015;4(3):1584-1604. [Google Scholar]
- 72. Reshadat S, Saedi S, Zangeneh A, et al. Spatial accessibility of the population to urban health centres in Kermanshah, Islamic Republic of Iran: a geographic information systems analysis. East Mediterr Health J. 2015;21(6):389-395. [DOI] [PubMed] [Google Scholar]
- 73. Lopes HS, Ribeiro V, Remoaldo PC. Spatial accessibility and social inclusion: the impact of Portugal’s last health reform. Geohealth. 2019;3(11):356-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and healthcare resource availability. Lancet Glob Health. 2020;8(4):E480-E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hu H, Jian W, Fu H, Zhang H, Pan J, Yip W. Health service underutilization and its associated factors for chronic diseases patients in poverty-stricken areas in China: a multilevel analysis. BMC Health Serv Res. 2021;21(1):707. [DOI] [PMC free article] [PubMed] [Google Scholar]