Abstract
Introduction
Patients with generalized myasthenia gravis (gMG) experience functional impairment due to MG symptoms. This study aimed to assess, from the patient perspective, the symptoms, impacts, and treatment goals of individuals diagnosed with gMG.
Methods
Semi-structured, in-depth concept-elicitation interviews were conducted with 28 individuals diagnosed with gMG in the United States.
Results
Participants reported gMG symptoms that affected many body regions and functions, with an average of 16 symptoms per participant. The most frequently reported symptoms were eyelid drooping (93%), physical fatigue (89%), symptoms affecting the legs (82%), difficulty breathing (82%), and difficulty holding head up (82%). Nearly all participants (96%) reported fluctuations in symptoms and severity. Participants’ most bothersome symptoms were blurry/double vision (43%), breathing difficulties (36%), all-over fatigue (36%), and swallowing problems (29%). Impacts on physical functioning included an inability to participate in hobbies/sports, need for increased planning, and difficulties performing activities of daily living. All participants reported emotional impacts and impacts on their work and finances. Their treatment goals included reduced fatigue and weakness, improved symptom stability, and minimization of the impact of symptoms, in particular the emotional impact.
Conclusions
The fluctuating and unpredictable nature of gMG symptoms was found to have a substantial impact on patients’ emotional, social, and economic well-being. Participants’ goals for symptom management suggest that greater focus is needed to help them quickly resume a normal lifestyle by achieving symptom stability. Impacts of fluctuating and unpredictable symptoms are difficult to measure, but it is important to consider symptom fluctuation as well as ongoing symptomatology when making treatment decisions, and to recognize the impact of uncontrolled symptoms on patients, their partners/caregivers, and family/friends. These factors are often not reflected in burden/cost-of-illness studies.
Keywords: Burden, Fatigability, Fatigue, Impact, Myasthenia gravis, Qualitative research, Symptoms, Treatment
Plain Language Summary
The aim of this study was to understand—from the patient’s point of view—the range of generalized myasthenia gravis (gMG) symptoms that they experience, which symptoms bother them most, and which symptoms have the greatest impact on everyday life, as well as patients’ treatment goals. Researchers asked these questions in one-on-one interviews with 28 people in the US who have gMG. Study participants reported living with symptoms that come and go, and are sometimes severe, making it difficult to lead a normal life. The most frequently reported symptoms were eyelid drooping (reported by 93% of study participants), physical fatigue (89%), symptoms affecting the legs (82%), difficulty breathing (82%), and difficulty holding head up (82%). The symptoms that bothered patients most were difficulties with vision (43%), problems breathing (36%), all-over fatigue (36%), and trouble swallowing (29%). Participants reported that gMG symptoms affected physical functioning, making it hard to participate in hobbies/sports, increasing the amount of planning needed to conduct their daily lives, and hindering their ability to do day-to-day activities (like driving, eating, and bathing). All participants reported that they were affected emotionally, and that the symptoms of gMG impacted their ability to work and their financial well-being. Participants’ treatment goals included reducing fatigue and weakness, making symptoms more stable, and reducing the impact of symptoms, particularly emotional impacts. These responses reveal the extensive effects of gMG symptoms on patients’ daily lives and highlight that symptom stability is especially important to people with gMG.
Key Summary Points
| Why carry out this study? |
| Myasthenia gravis is a rare, chronic autoimmune disease characterized by muscle weakness and fatigability, resulting in functional impairment. |
| While the symptoms of generalized myasthenia gravis (gMG) are well known, patients’ lived experience of the disease—the symptoms that bother them most, the impact of the fluctuating and unpredictable nature of different symptoms on their daily lives, and their treatment goals—has not been adequately documented. |
| The aims of this study were to systematically document the symptoms and impact of gMG from the patient’s perspective, and to understand their treatment goals. |
| What was learned from the study? |
| Patients reported that they live with persistent symptomatology as well as fluctuations in symptom presence and severity; the most bothersome symptoms were difficulties with vision, breathing, all-over fatigue, and swallowing. |
| The fluctuating nature of symptoms has an impact on patients’ emotional, social, and economic well-being. |
| Patients’ treatment goals included symptom management (reduce weakness, consistent control of disease manifestations) and minimizing the impact of symptoms, particularly the emotional impact. |
| The degree of fluctuation in gMG symptoms, and the impact of this fluctuation on an individual patient’s life, may not be evident in routine clinical visits, but should be regularly monitored in order to more comprehensively understand the patient’s unmet needs and treatment goals. |
Introduction
Myasthenia gravis (MG) is a rare chronic autoimmune disease with a variable course [1–3]. The prevalence of MG ranges from 14.0 to 36.1 cases per 100,000 population [4, 5]. MG can occur at any age, but onset tends to occur at a younger age in women (under 40 years of age) and at an older age in men (over 60 years) [6]. Overall, approximately 15% of patients with MG only experience weakness of the extra-ocular muscles (manifesting as double vision and/or drooping eyelids), while approximately 85% present with or will progress to generalized disease (gMG), in which the face, neck, hands, and/or limbs are also affected [1, 3, 7]. More frequent symptoms of gMG include head drop, difficulty talking, chewing, and swallowing, poor hand grip, inability to use arms and legs, and respiratory issues [3, 6–9].
A 2021 study found that a third of patients with gMG were dissatisfied with their current symptom state. This dissatisfaction was associated with disease severity, disease length (duration of the disease), depression, fatigue, and lower MG-related quality of life [10]. Another 2021 study—a large cross-sectional study conducted in Sweden (n = 1,077)—found that 47% of patients were unsatisfied with their symptom state [11]. In an earlier study in Germany, many patients—despite receiving treatment—reported MG-related impairments that particularly affected mobility, mental well-being, and quality of life [12]. Health-related quality of life is reported to be markedly lower in patients with MG compared with the general population [12, 13].
The purpose of this study was to better understand—from a patient perspective—the symptoms, impacts, and treatment goals of individuals diagnosed with gMG, with an emphasis on the symptoms identified by participants as most bothersome.
Methods
Study Design and Population
This was a qualitative, cross-sectional, non-interventional study involving in-depth, individual telephone or webcam concept-elicitation interviews with 28 people living with gMG. It was conducted, following US Food and Drug Administration (FDA) guidance on patient-focused drug development, to determine the gMG-related symptoms, impacts, and treatment goals that are important to patients [14–16]. As per the FDA guidance, the target population is defined as the group of patients whose experience is being investigated. Such studies therefore do not use matched controls because the objective is to hear directly from people living with the disease. Patients—in this case, patients living with gMG—serve as the experts on their condition because of their lived experience. For qualitative studies, sample size determination is often based on concept saturation, which means the point at which no new important concepts relevant to the research question are emerging from interviews [17]. The rationale for this focus on saturation comes from research that has “repeatedly demonstrated lack of agreement, often markedly so, on the severity and frequency of signs and symptoms when patient-reported and non-patient-reported measures are compared” [14].
All study materials were reviewed and approved by an independent review board (New England Independent Review Board; NEIRB Study #1286397). Owing to the minimal-risk nature of this study, the independent review board approved a waiver of documented consent. Participants were provided with a consent document, which was reviewed in detail by the interviewer at the start of the interview; consent (including consent for publication of anonymized responses) was freely given, specific, informed, and unambiguous, and was provided verbally.
This study employed a purposive sampling strategy. Purposive sampling is a non-probability sampling method which allows for the research team to use their knowledge of the research objectives and the population of interest to identify participants who are appropriate for the study [14], taking into account important factors such as age, sex, and disease duration. This design strategy was selected based on the objective of understanding the breadth of the patient experience, and the range of impacts associated with the broad array of symptoms. The sampling strategy is among those recommended by the US FDA in their guidance regarding collection of comprehensive and representative input for patient-focused drug development [14]. Patients were identified for recruitment for the study through a variety of sources, including patient advocacy groups (Myasthenia Gravis Foundation of America [MGFA], MGFA New England, and Myasthenia Gravis of the Heartland) and referral resources from the sponsor’s own patient network. The patient advocacy groups announced the study via their websites, e-mail lists, and social media platforms, and interested patients contacted a third-party recruitment company for screening and scheduling.
Eligible participants were aged 18 years or older, US residents, and comfortable reading and communicating in English. They were required to have been told by their doctor that they had gMG, and to be receiving at least one of the following treatments for their gMG: anti-acetylcholinesterase, azathioprine, tacrolimus, corticosteroid, cyclophosphamide, cyclosporine, intravenous or subcutaneous immunoglobulin, methotrexate, mycophenolate mofetil, plasmapheresis (plasma exchange), rituximab, or eculizumab. Patients with only ocular disease were excluded to better understand the breadth of MG symptoms that affect all muscle groups.
Semi-Structured Interview Process
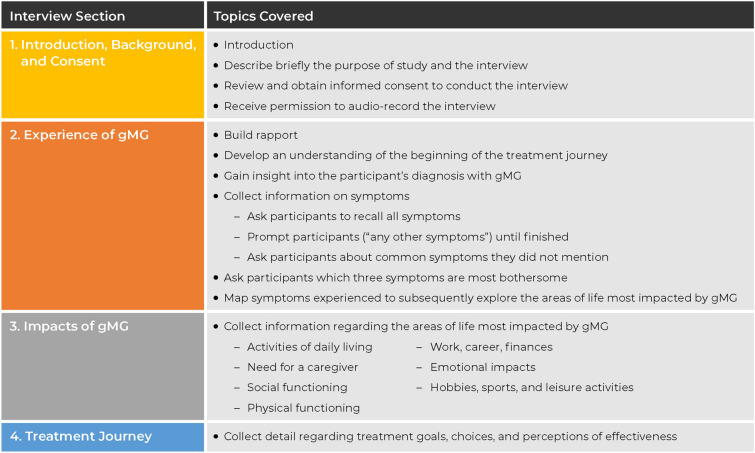
Concept elicitation in health-measurement research is a qualitative method in which the interviewer asks the participant open-ended questions about the symptoms, impacts, and other aspects of their condition to characterize the patient experience [17–21]. Each interview followed a standardized, semi-structured interview guide developed specifically for this study. Due to the heterogeneity of the condition, the interview guide was intentionally broad, in order to ensure that symptoms and impacts were not missed. Interviewers began by asking about the participant’s experience of their diagnosis and all symptoms since diagnosis. Participants were asked to list their symptoms, and interviewers used the probe, “Anything else?” until the participant said “No.” Interviewers then used a comprehensive list of symptoms to inquire about symptoms that had not yet been mentioned by the participant. After completing this inquiry, if fatigue was identified as a symptom, participants were asked additional fatigue-related questions. Finally, all participants were asked to identify their three most bothersome symptoms. Participants were also asked to describe the impact of their symptoms on their lives, and were subsequently asked about their treatment experiences over the previous year and to identify their goals for treatment. The interview structure is summarized in Fig. 1.
Fig. 1.
Summary of interview structure. gMG generalized myasthenia gravis
The interview concluded with verbal administration of the Myasthenia Gravis–Activities of Daily Living (MG-ADL) profile. This tool captures information on ocular dysfunction (two items), oropharyngeal dysfunction (three items), respiratory dysfunction (one item), and extremity dysfunction (two items) over a 7-day recall period. Each item is graded on a four-point severity scale from 0 (normal) to 3 (most severe), with the total score ranging from 0 to 24. Higher scores indicate greater severity of symptoms [22]. All interviews were audio recorded and recordings were transcribed verbatim. Following completion of the interview, participants received an honorarium as compensation for their time.
Coding and Analysis
Participants’ descriptions of their experiences of gMG were coded using content thematic analysis [23] in accordance with grounded theory analysis methods, whereby concepts and themes emerge from participants rather than imposing an a priori theory [24–26]. The one exception to this was the code for fatigability, which was not specifically named by either the interviewers (to avoid using jargon) or the participants (because it is not common vernacular among patients). Instead, researchers coded for this concept based on patient descriptions of their symptoms according to the definition of fatigability provided by Barnett et al. [27].
The initial codebook was developed during the interview process and was based on a review of the field notes before receipt of transcripts. To begin the coding and analysis process, three researchers (two of whom also conducted the interviews) independently coded four transcripts. The researchers met to discuss coding, one transcript at a time. Any discrepancies in coding were resolved through review of relevant data and discussion, and adjustments were made as needed to the codebook and code definitions. Once the researchers were coding consistently, the remaining transcripts were divided into three groups and each group of transcripts was coded by one of the researchers. All coding was later reviewed by the study principal investigator (who was one of the three researchers), and any issues or questions arising from the data were resolved via data review and discussion. Data were reviewed and coded using NVivo 12 Plus qualitative data analysis software (QSR International Pty Ltd, 2018; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home).
Saturation of concepts was reached across all participants, indicating that the number of interviews was sufficient and that additional interviews would not result in further concepts of interest. This was assessed by examining concepts across five sets of five interviews, and a sixth set of three interviews. Of the 93 unique concepts (i.e., codes), transcript set 1 generated 70 codes, set 2 generated an additional ten codes, set 3 generated an additional six codes, and the remaining three sets generated a total of seven new codes. Overall, 75% of codes were generated in set 1 and 92% of codes were generated in the first three sets. The two concepts identified in the sixth (final) set were symptoms (twitches and frozen muscles), neither of which was identified by participants as being among their top three most bothersome symptoms. This suggests that conducting 28 interviews was sufficient to reach saturation, and that further interviews would not have resulted in additional themes. The specific concepts that emerged during the interviews (e.g., driving, running errands, cooking) were inductively grouped into more general categories [e.g., activities of daily living (ADLs)].
Results
Study Population
Table 1 provides the characteristics of the study population, which included 18 women and ten men. The majority of participants were White (93%), aged between 35 and 69 years (64%), and had some college education or a college degree (86%). MG-ADL scores ranged from 0 to 13 (mean 5.54; standard deviation 3.55).
Table 1.
Demographic and clinical characteristics of study participants
| Characteristic | All (n = 28) |
|---|---|
| Age, n (%) | |
| 18–34 years | 6 (21) |
| 35–50 years | 9 (32) |
| 51–69 years | 9 (32) |
| 70+ years | 4 (14) |
| Sex, n (%) | |
| Male | 10 (36) |
| Female | 18 (64) |
| Education, n (%) | |
| High school diploma or GED | 4 (14) |
| Some college but no degree | 7 (25) |
| Associate degree or technical certificate | 5 (18) |
| Bachelor’s degree | 8 (29) |
| Graduate degree | 4 (14) |
| Race/ethnicity, n (%) | |
| Black or African American | 1 (4) |
| Hispanic/Latino/Spanish | 1 (4) |
| White | 26 (93) |
| Region, n (%) | |
| Midwest | 9 (32) |
| Northeast | 11 (39) |
| South | 4 (14) |
| Southwest | 2 (7) |
| West | 2 (7) |
| Time since MG diagnosis, n (%) | |
| 0–1 year | 5 (18) |
| 2–5 years | 4 (14) |
| 6–9 years | 7 (25) |
| 10–15 years | 6 (21) |
| 16–20 years | 0 |
| > 20 years | 6 (21) |
| MG-ADL total score, mean (SD) | 5.54 (3.55) |
GED General Educational Development test, MG myasthenia gravis, MG-ADL Myasthenia Gravis-Activities of Daily Living, SD standard deviation
Symptom Experience
Body Regions and Symptom Types
The symptoms reported by participants (n = 28) affected many body regions and functions (Fig. 2), with an average of 16 symptoms per participant since symptom onset. The most frequently reported symptoms or areas affected were eyelid drooping (93%), physical fatigue (89%), symptoms affecting legs (82%), difficulty breathing (82%), and difficulty holding head up (82%) (Table 2).
Fig. 2.
Body areas affected by generalized myasthenia gravis, as reported by study participants
Table 2.
Most common symptoms identified spontaneously and via probing in participants (n = 28), and representative quotes
| Symptom type (spontaneous/probed)a | Total no. of participants (%) | Direct quote |
|---|---|---|
| Blurry or double vision (21/1) | 22 (79) | They thought I only had a—a lazy eye … but then it was clear my double vision started changing all the time. I didn't see exactly two images and they weren't in the exact same places. So, for instance, sometimes they were diagonal. Sometimes they were side by side. ID 34 |
| Arms (20/2) | 22 (79) | Like one thing we did in my kitchen when I was first diagnosed was, we put all the heavy dishes sort of waist level so that I wasn’t reaching up high to pull them down and just dropping them on myself … So, we totally rearranged my kitchen so that it was easier for me so that my muscles wouldn’t fatigue reaching up high and stuff like that. ID 01 |
| Cognitive impairment (19/0) | 19 (68) | I’ll think of something I want to do, and I’ll finish up what I was doing, and I says, “What was it I want to do anyway?” I can’t remember what I was going to go do. ID 05 |
| Legs (19/4) | 23 (82) | But when [symptoms] are really bad, I’ve had issues with walking. I can’t walk without assistance. Today, I still can’t walk without assistance. I need a cane or a walker or I lose my balance. ID 42 |
| Eyelid drooping (18/8) | 26 (93) | Yeah, I have, uh, [Laughs] eyelid droopiness … a lot. It’s kind of … hard to look in the mirror because … I’m used to seeing my eyes being open wide. And I look in the mirror, it looks like I’m like falling asleep, but I’m not. ID 23 |
| Swallowing (18/3) | 21 (75) | But when you pick up a, a glass of water or milk or something, you drink like you normally do. And those muscles just can’t push it down and it’s, it’s just stuck … There’s been times I have not been able to cough it up … you sometimes have to make yourself throw up because sometimes, something will be obstructing your throat. ID 62 |
| Breathing (17/6) | 23 (82) | I got real short of breath … I was having trouble walking from my car to the hospital when I was working … and then it would just be, if I was in a big conversation it’d be, when I was talking, I would just run out of breath … again, trying to walk for any period of time, I’d have to stop to catch my breath. ID 48 |
| Fatigue physical (16/9) | 25 (89) | The overall feels like I have no energy left. And when I know I have no energy left, I know I need to rest and hopefully in an hour, maybe take a nap, as long as it’s cold and I’m comfortable, I can rest. ID 44 |
| Chewing (15/7) | 22 (79) | I couldn’t keep my mouth, my lips closed. I couldn’t control my tongue so I would bite it a lot or the side of my cheeks and stuff like that. So yeah, that was kind of all with the eating, not being able to eat thing. ID 16 |
| Holding head up (14/9) | 23 (82) | Um, and so, I kind of—that’s kind of what brought it to my mind. Like, I’m holding my head not because I’m bored but my—I can’t hold it up. ID 33 |
| Fatigue all over (14/6) | 20 (71) | Uh, it’s usually all over … It’s just extremely just heavy, don’t want to move, feel like an elephant’s on my chest sometimes. ID 16 |
| Speech (13/7) | 20 (71) | I would often get tongue-tied and I would often feel like I just couldn’t, I couldn’t enunciate, or I couldn’t speak. I’ve always been able to speak fairly well. ID 62 |
| Lower facial muscles (11/7) | 18 (64) | The corners of my mouth, the muscles are giving way and I just drool all the time. It means my face—you know, with some hanging stuff on it all the time, I have to continually watch it because it just runs all the time. ID 66 |
| Eye muscle weakness (9/12) | 21 (75) | And I gave up driving for six months because I decided it wasn’t real safe to drive around like this holding an eye lid up. I can’t drive more than a few hours or my eye lid start drooping … I can’t even … close my eyes and rest because the muscle is so weak it won’t stay closed. So, I actually have to put my hand on top of my eye lids to hold them closed. ID 01 |
| Hands (9/11) | 20 (71) | My hands—from, like, my elbows to my hands were shaky and I couldn’t … even grab the door to open it. It was too weak to grab the … door handle to … turn it. ID 54 |
| Voice quality and tone (7/12) | 19 (68) | This is, uhm, very important to me when I’m on, uh, calls, videos, meetings where if my representation is altered, it—it now reduces that perception in my own mind. And uh, I—and that’s hard. That’s really hard because I’m representing my company in the role that I play. And if I’m talking to a chief science officer and I can’t get the right words out of my mouth, this is not good. ID 03 |
| Fingers (5/11) | 16 (57) | Uhm, some days I can do like, uhm, let’s say—I—I do arts and crafts. Uhm, some days I can do like a little paint-by-number thing and then the next day I can’t even like grip my pencil—or my hands are shaky because I’m trying to do detail and I can’t even do that. ID 12 |
| Mental fatigue (4/9) | 13 (46) | I know I have the energy. I know I have it, but mentally I just can’t bring myself to do anything. It’s just like—it—the m-mental fatigue is more of a—uh, depressive episode without being depressed, if that makes any sense. ID 12 |
| Spasms (4/7) | 11 (39) | My hands will twitch sometimes, but it’s always the right eye, it’s always that weak, weak side. I don’t have any twitching in the left, it’s always in the right … and my hands and arms will twitch sometimes too. And leg cramps. I get terrible leg cramps. ID 62 |
| Pain in specific location (4/5) | 9 (32) | Just other than my neck gets sore from time to time … I don’t have much range of motion. ID 66 |
| Fatigue in specific location (3/5) | 8 (29) | There are days where my strength is, you know, good enough that I can eat the salad. But then there are other days when I probably take two or three mouthfuls and I’m so tired of chewing or trying to chew that it’s just not worth it. ID 42 |
| Pain all over (3/0) | 3 (11) | Like I’ll get up from the couch and my shoulders will hurt, my arms will hurt, and my legs will hurt and I just kind of stand there to stabilize myself and then move at that point and it kind of lessens. ID 17 |
aNumber of participants who spontaneously reported this symptom/reported this symptom when probed
The majority of participants (93%) experienced fatigability (i.e., tiring more quickly than usual when performing common tasks). Of the body regions, the arms (54%) and legs (50%) were most commonly associated with fatigability.
“If it’s off the ground, I won’t pick up something heavy because there’s a lot of legs involved. And I know just one lift might fatigue me for, like, an hour.” ID 541
Most of the participants reported (either spontaneously or following interviewer probes) physical fatigue (89%) and weakness (86%).
“I’ve had weakness in my back that was so bad. I thought I had an issue with my heart but really, I just, I couldn't even hold my ribcage right.” ID 34
Unlike weakness, in which a specific muscle or muscle group was involved, physical fatigue was experienced throughout the body as a global feeling of exhaustion.
“I just feel completely exhausted like I just ran a marathon.” ID 16
“It doesn’t just start in one spot and then work its way wherever. It’s all over.” ID 44
Some participants also reported mental fatigue (46%). All of those who identified mental fatigue also recalled experiences of physical fatigue and were able to make a distinction between the two. Being mentally tired, too exhausted to think, or unable to mentally motivate oneself was sometimes directly associated with physical fatigue. For example, experiencing physical fatigue for several days in a row could be mentally draining. However, mental fatigue was also sometimes independent of (or a precursor to) physical fatigue and could be the result of concentrating for too long. In some instances, mental fatigue was associated with depression or stress, and in others the experience was independent of emotions.
“I know I have [the energy], but mentally I just can’t bring myself to do anything. It’s just like—it—the m-mental fatigue is more of a—uh, depressive episode without being depressed.” ID 12
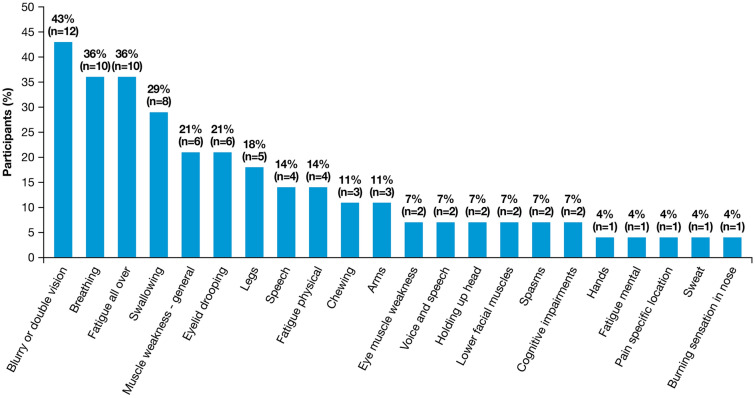
Most Bothersome Symptoms
When asked to identify their three most bothersome symptoms or body regions, some participants identified only one or two, and others described a tie between symptoms. Rather than force participants into a choice, the interviewers asked additional questions regarding all symptoms that were identified as most bothersome and analyzed these results. The symptoms that participants identified as most bothersome were blurry or double vision (43%), difficulty breathing (36%), all-over fatigue (36%), and swallowing impairments (29%), followed by general muscle weakness (as distinct from fatigue) and eyelid drooping (both 21%) (Fig. 3). Of those who reported all-over fatigue as one of their three most bothersome symptoms (n = 10), one participant also gave general muscle weakness as a separate most bothersome symptom.
Fig. 3.
Most bothersome myasthenia gravis symptoms and affected body regions, as reported by study participants. Participants were asked to identify their top three most bothersome symptoms or body regions and could nominate a symptom, a body region, or both when they identified the experiences that were most bothersome. Number of patients reporting a symptom as one of their top three most bothersome is shown in brackets above the corresponding bar
Although ‘blurry or double vision’ was among the topmost bothersome symptoms reported, the overall bothersomeness (and impact) of ocular symptoms was often dependent on the participant’s lifestyle and/or the type of ocular symptom. For instance, mild double vision could be very bothersome and disruptive to those who were still working and/or still driving, but participants in retirement and/or no longer driving did not always report double vision as bothersome.
Symptom Fluctuations and Triggers
In addition to underlying persistent symptomatology, most patients (96%) reported that the presence and/or severity of symptoms often fluctuated over the course of a day or from one day to another. Fluctuation was reported for fatigue, weakness, blurry or double vision, difficulty swallowing, and difficulty breathing.
“One of my first symptoms was double vision, and it—it would pop in and out. There was no rhyme or reason to it. It was just popping in and out.” ID 37
Fatigability, which includes fluctuation by definition, was associated with all body regions and symptom types. Many participants also identified other triggers that caused symptoms to fluctuate. Hot or humid weather was reported to trigger both general physical fatigue and muscle weakness, resulting in participants avoiding outdoor activities and lowering home thermostats. Dietary choices triggered chewing or swallowing symptoms, often because certain food consistencies or textures (which differed for different participants) could make eating more difficult. Stress, anxiety, and high-pressure life events (e.g., work conflicts) could also exacerbate symptoms.
While the breadth of symptoms experienced by patients with gMG has been noted in previous studies, the interview methodology in this study revealed an important aspect of symptom fluctuations and symptom recall. Every participant reported at least one additional symptom or body region when probed, after stating that they had provided a complete list of their symptoms (Table 2). Upon confirming the initially omitted symptom or body region, they explained that their recall difficulty was a result of becoming accustomed to their gMG, or because a symptom fluctuated.
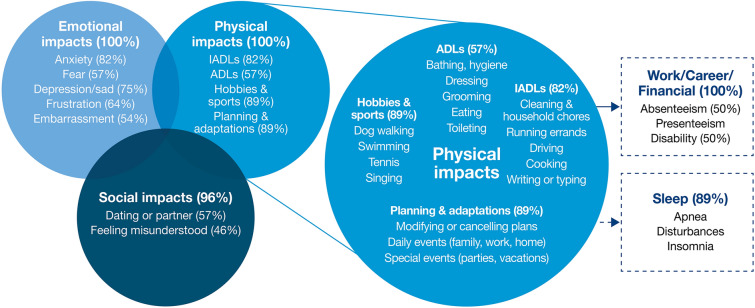
Impact of Symptoms
Participants reported the impacts of symptoms and these were subsequently grouped into three main domains of life: physical functioning, emotional functioning, and social functioning. These impacts were often interrelated, and participants tended to describe simultaneous experiences in these domains (Fig. 4). Symptoms also affected other life domains, including sleep; work, career, and finances; and independence (i.e., need for assistance). At times, participants were unable to identify an association between a specific symptom and a specific impact. Representative quotes from the participants illustrating the overall impact of MG symptoms on aspects of their lives are provided in Table 3.
Fig. 4.
Impacts of generalized myasthenia gravis symptoms, as reported by study participants. ADL activity of daily living, IADL instrumental activity of daily living
Table 3.
Impact of myasthenia gravis symptoms on aspects of participants’ lives
| Impact | Direct quote |
|---|---|
| Physical functioning (n = 28) | And when I’d fall, I couldn’t get up unless I was right next to something that I could use to help me get up. I would have to call my daughter-in-law, and she would have to leave work and come home and help me get up. Because I would … fall in the middle of the living room floor … I would have to make my way crawling, literally, only I couldn’t get up and crawl. It was more of a GI Joe crawl to get to my phone. ID 64 |
| Work, career, finances (n = 28) | And, so it’s very costly. Okay. My insurance covers 80% of it, so I would have to pay the other 20%. And I don’t even make enough money in social security to pay the 20%. ID 67 |
| Emotional (n = 28) | I do—I do get depressed. Because I do feel like the idea that something has been taken away from me. ID 03 |
| Social functioning (n = 27) | We’ve … canceled a lot of plans with, like, extended family or friends that we have that we’ll go on their house for dinners or just playdates kind of things. And it can be right up until time to leave to where we got to call and say, “Hey, we can’t do it.” You know, “[participant’s name] is not feeling good.” Or, I’ll call and say, “I’m not up to it tonight.” I’ve always had to rearrange vacation plans in time for it. Just because, I’m not feeling up to it. That pretty much cancels things. ID 54 |
| Planning (n = 25) | And the term I use quite a bit is I have to be very “planful” … if I want to do something, or we’re going out for a doctor’s appointment … I know that I will have to take a nap when I get home. If I work downstairs in our office, then I will definitely have to take a nap after that. And like when we were going on vacation, the whole vacation would be planned around a nap in the afternoon, in terms of the tours and that type of thing. ID 17 |
| Sleep (n = 25) | A lot of it, I think, was just my being scared that I didn’t want to die in my sleep. I didn’t want to stop breathing or not be able to breathe, or choke or something. That was a big part, I think, why I didn’t want to go to sleep. Then, I just have a hard time sleeping at night. I’m really restless. I think I’m just so fatigued and then I would finally fall asleep at the wee hours of the morning, usually. But … I’m noticing a little difference in that now since I’ve been on the treatments that I’ve been on that I’m able to go to sleep a little bit earlier at night. ID 46 |
| Independence (n = 18) | My mom is my caregiver. She [helps me] every day … doing my laundry, helping me maintain my room clean, because I try to keep it as clean as possible so I don’t bump into things, so I’m able to walk in my room without really needing my cane if I can do it … cooking for me. I can’t carry plates and cups because—in case I fall or something … So she’ll help me with that. She takes me to my appointments … She’s there for me whenever I need her. ID 44 |
Impact on Physical Functioning
The symptoms of gMG resulted in impacts on physical functioning for all participants (100%) across the following domains: gross motor impairment (93%), fine motor impairment (46%), balance impairment (29%), difficulty performing ADLs (i.e., basic self-care activities such as bathing, dressing, grooming, eating, and using the bathroom) (57%) and instrumental ADLs (i.e., activities with aspects of cognitive and social functioning that are necessary for independent functioning in the community, such as shopping, cooking, housework, and managing finances) (82%), inability to participate in hobbies or sports (89%), and a need for increased planning to accomplish daily activities and/or participation in social activities (89%) (Fig. 4).
Gross motor impairments included an inability to walk short or long distances, climb stairs, or stand up from a seated position without assistance or support, and difficulty lifting or carrying items. Fine motor impairments included difficulty grasping objects or a loss of grip strength (e.g., turning a doorknob, holding a pen or paintbrush, using a fork or knife). Overall balance was also affected by gMG symptoms. Some participants needed constant ambulatory support (a cane or walker), while others noticed their balance fluctuated and, as a result, were overall much more cautious when moving about, sometimes holding a railing or using a wall for support.
“So, I was having problems with my legs. Again, falling on the steps or … or tripping, or, you know. I had no, no like special perception where my feet were. I would kick stuff in the hallway or, you know, trip over things.” ID 31
Limitations in performing ADLs were common. Participants had difficulty washing their hair, and often needed to rest after taking a shower. Getting dressed, grooming, and eating all presented similar challenges because it was difficult for participants to manage buttons, pull up pants, hold a hairbrush, or grasp eating utensils while experiencing limited fine motor control. Some had difficulty using the bathroom independently (getting on and off the toilet) during periods of extreme muscle weakness. Additionally, gMG symptoms limited participants’ ability to complete chores around the house, drive, run errands, cook, and write or type. Limitations in both ADLs and instrumental ADLs were often associated with a loss of independence.
“… other things would be like I don’t wear a lot of stuff with buttons, because my hands are having issues. It’s hard for me to put them in … Or, something so stupid and small … but even like leggings or jeggings, like something that doesn’t have, they just slide on. Sometimes my hands are not strong enough to pull them up.” ID 58
Participation in hobbies and sports was challenging and often too difficult to continue as a result of gMG symptoms. This included the abandonment of team and individual sports, such as ball sports, running, cycling, and swimming, and activities and hobbies including traveling, crafting, and singing.
“The woodworking always has been one of my passions … I have built so many things. And I can’t do that anymore.” ID 42
Disruptions to plans and careful planning of activities were common themes. This included having to prepare for and manage the logistics of day-to-day tasks, such as appointments, grocery shopping, cleaning, cooking, or working. It also entailed planning for potential adjustments during an activity, breaking an activity into smaller segments, or pacing an activity and taking breaks to make things more manageable, conserve energy, or minimize symptoms. Last-minute modifications or cancellations meant that some no longer intended to go to special events (e.g., vacations or family gatherings) due to the unpredictability of their gMG symptoms. Others were very thoughtful and intentional in their planning of events and vacations, to ensure they could attend and/or participate.
“And the term I use quite a bit is I have to be very ‘planful’ … if I want to do something, or we’re going out for a doctor’s appointment or whatever it is, I know that I will have to take a nap when I get home. If I work downstairs in our office, then I will definitely have to take a nap after that. And like when we were going on vacation, the whole vacation would be planned around a nap in the afternoon, in terms of the tours and that type of thing … So much more conscious of uh, what I do, and the ramifications.” ID 17
Impact on Mental and Emotional Health
Emotional impacts as a result of gMG were reported by all participants (100%) and included anxiety (82%), depression/sad (75%), frustration (64%), ambivalence (50%), stress (32%), and discomfort (18%) (Fig. 4). The symptoms of gMG were described as being “emotionally draining” and many participants described an overarching sense of sadness that was often—but not always—tied to stress and anxiety. Anxiety presented as a state of fear and worry, sometimes associated with specific gMG symptoms (e.g., difficulty breathing, double vision, eyelid drooping, muscle weakness) and at other times related to lack of treatment availability and costs of treatment.
“I do—I do get depressed. Because I do feel like the idea that something has been taken away from me.” ID 03
“A lot of it, I think, was just my being scared that I didn’t want to die in my sleep. I didn’t want to stop breathing or not be able to breathe, or choke or something. That was a big part, I think, why I didn’t want to go to sleep.” ID 46
Some participants were frustrated by the way gMG impacted their functioning and quality of life. Feelings of denial, embarrassment, guilt, a loss of control, and a tendency to withdraw because of gMG were common and often connected to stigma in social situations. Alternatively, gMG was occasionally described with ambivalence and neutrality, with some viewing the condition (or particular aspects of the condition) as a hurdle to deal with and accept as a part of life.
Impact on Social Functioning
Impacts on social functioning (96%) included difficulties dating, feeling misunderstood by friends and family, feeling uncomfortable and anxious in social situations, and skipping or avoiding social events altogether (Fig. 4). Dating experiences were difficult, with concerns around how a potential partner would cope with gMG and whether the participant would be a burden on a partner (i.e., placing the partner in the position of caregiver).
“You know, the desire to date … but there’s a fear factor that goes in and it’s mostly—it’s an unrealistic fear. But it—it’s there because I—want to be honest and up front, but it’s like, ‘Hey, how ya doing. I’ve got an incurable disease. How are you?’ That’s not usually a good way to open up a conversation, so …” ID 03
Anxiety was common at social gatherings, as were concerns over being judged or pitied by strangers who might not recognize gMG and judge speech issues as drunkenness or assess drooping facial muscles as signs of a stroke. Additionally, social time with family and friends was also difficult to enjoy when others did not understand how debilitating gMG could be. Canceling or avoiding social gatherings to prevent overexertion or exacerbation of symptoms was common.
“Well, it's impacted things with friends because like I said, my … my mindset on things have changed a bit like seeing friends is something to fear and worry about.” ID 34
Impact on Sleep
Sleep disturbances were reported by 89% of participants (Fig. 4). They had difficulty falling asleep and were often unable to get an uninterrupted night’s sleep due to pain or muscle cramps, trouble breathing, or side effects of medications.
“I noticed it more when I was sleeping. Uhm, I think, again, that was like the hard swallowing, the hard time swallowing thing. I u-used to have to sleep propped up a little bit because I would wake up and I’d be choking on my spit. And then I’d just feel like I couldn’t breathe.” ID 16
Those who associated sleeping difficulties with their gMG took naps to catch up on their sleep, although a few also used nighttime sleep aids such as sleeping pills. Participants who were diagnosed with sleep apnea reported use of continuous or bi-level positive airway pressure devices to aid with sleep and nighttime breathing. A few (24%) who reported trouble sleeping were uncertain how closely related this was to their gMG. Despite being a common issue, participants did not detail the ways in which sleep disturbances affected other areas of life, nor did they discuss improved sleep later in the interview as an important treatment goal.
Impact on Work, Career, and Finances
All participants said symptoms of gMG impacted aspects of their work, career, and finances (Fig. 4). Some were unable to work because of their gMG, whereas those who were working said they missed work as a result of gMG treatments, hospitalizations, or symptom flares. In addition to limiting participants’ ability to work full time, gMG reduced overall productivity and often required work modifications such as spreading tasks over multiple days or resting between tasks. Younger participants tended to change or modify college plans or switch career paths, while older participants instead passed on promotions or prematurely ended a career to pursue a different job or retire.
“Because there’s a lot of walking involved, you know, all around the school and there’s days where walking down one hallway is too much. So, I’ve had to go home.” ID 54
“Well main thing is I had to give up on my dream of being an animal [care]taker at a zoo.” ID 16
Financial impacts of gMG included receiving social security or disability as a primary source of income, relying on a family member’s income to pay bills, and the high costs of gMG treatment.
“And, so it’s very costly. Okay. My insurance covers 80% of it, so I would have to pay the other 20%. And I don’t even make enough money in social security to pay the 20%.” ID 67
Impact on Independence
One participant relied on a formal paid caregiver for assistance. All others who needed assistance (64%) relied on informal caregivers such as a spouse/partner, family member, or friend. Those with informal caregivers relied on them for intermittent assistance with driving, cooking, cleaning, running errands, and carrying objects. While some were grateful for the help when needed, most expressed a desire to stay as independent as possible, and only asked for help when necessary.
“My mom is my caregiver. She [helps me] every day … doing my laundry, helping me maintain my room clean, because I try to keep it as clean as possible so I don’t bump into things, so I’m able to walk in my room without really needing my cane if I can do it … cooking for me … I can’t carry plates and cups because—in case I fall or something … So she’ll help me with that. She takes me to my appointments.” ID 44
Treatment Goals
The two main categories of treatment goals identified through patient interviews were symptom management (82%) and minimizing the impact of symptoms (71%). The most common goal for symptom management was reduced fatigue or weakness (39%), followed by achieving consistent control of disease manifestation—often referred to by participants as achieving “stability” or a “new baseline” (25%)—and remission/cure (18%).
“Right now, right now the realistic goal is—I would say—is to not be any worse than I am now. You know, just kind of keep things stabilized and stay there. Not have these ups and downs.” ID 05
“If—if a new therapy came out that addressed that [fatigue], it would—it would turn my life around.” ID 03
The most common treatment goal for managing the impact of symptoms was to reduce the emotional impacts (18%). This was especially true for participants who noticed any kind of emotional upset or distress that could further exacerbate their symptom(s) and those who were uncertain about treatment efficacy. The next most common treatment goal related to impact was a return to former activities, including hobbies, sports, leisure, and travel (14%). A general desire to get back to a normal life, without detailing the specifics, was identified by 14% of participants.
“Um, I mean, my ideal goal would be to become what I would define as normal. Being realistic, uh, I would say my goal is just to kind of stabilize.” ID 17
Discussion
This qualitative study used one-on-one concept-elicitation interviews to identify all gMG symptoms experienced by participants; to collect details regarding the most bothersome symptoms and the impacts of symptoms on participants’ daily lives; and to identify the specific symptoms and impacts that participants would like to be addressed by their treatments. The intent of the study was to gain insights into patients’ lived experiences of gMG; as such, the findings represent symptoms and impacts experienced by participants over the entire course of their disease. The particular symptoms and impacts that participants found most bothersome were highly dependent on their lifestyle and how well or poorly their gMG was managed, providing additional evidence of the diversity of the gMG experience. Although individuals experiencing ocular symptoms were not excluded from the study, the design was not intended to focus on ocular MG. Many participants described experiencing ocular symptoms; however, no comparisons were made as this was not the study objective.
Participants reported that the severity (or presence/absence) of a symptom could vary during the course of the day or across days, and that this fluctuation and unpredictability had substantial impacts. This is consistent with other research reporting that the unexpected exacerbation of symptoms following a state of remission was sometimes discouraging to patients and accentuated the limitations caused by their MG [28].
The burden associated with detailed planning around daily activities and special events in order to cope with the variability of gMG symptoms was a common aspect reported by participants in this study. Despite careful planning, many mentioned having missed important life events because of gMG, reflecting the persistent impairment in functioning that is an undercurrent to the fluctuation of symptoms. This was also noted in the recent analysis by Law et al., who suggested that, because of muscle weakness, patients with MG “have to make continuous assessments and trade-offs in all aspects of their life” [28]. An important next step in this research will be to explore the coping strategies used by patients with gMG when their symptoms are stable and when they are unstable.
The findings concerning the impacts of gMG on emotional well-being, mental health, and work are also in accordance with a recent matched-pairs analysis that compared the subjective experience of patients with MG with that of the general population [13]. The study, conducted in Germany, found that physical health, mental health, and health-related quality of life were considerably lower in patients with MG, with impacts on economic and social aspects and patients’ emotional well-being. The authors of the study suggested that when describing and measuring the burden of the disease, it is important to take a holistic view that accounts for functional impairment, depression, anxiety, fatigue, and limitations on social functioning [13].
An adverse impact of MG on employment has been reported in previous research, including reduced participation in the labor market, increased absenteeism and sick leave, and increased patient-reported hardship among those who are employed [12, 29–32]. In addition to the economic burden imposed by unemployment, involuntary exclusion from the labor market is detrimental to overall health and is associated with increased morbidity, premature mortality, and greater use of medical services [33–37].
This is, to the best of our knowledge, the first qualitative study of its kind to systematically collect information about the treatment goals of people living with gMG after a detailed exploration of symptom types, affected body regions, and disease impacts. Data from the current study suggest that, when treating patients with gMG and assessing potential therapies, it is important for physicians to be aware of the heterogeneous experience of persistent physical functioning impairment that is punctuated, for many patients, by ongoing fluctuations in gMG symptoms. Physicians also need to be aware of how gMG impacts the daily lives of patients. Very few studies have examined the patient’s experience of the impact of MG symptoms and its treatment [28, 38]; a comprehensive picture of an individual’s symptoms, their variability, and their impact is needed to help guide choices regarding the optimal therapy pathway for that person.
As other authors have previously suggested [10], the findings from this study reinforce that instead of focusing exclusively on objective measurements of symptoms and treatments, taking a broader, more patient-centered approach to managing gMG is likely to optimize patient satisfaction with treatment. Instruments such as the MG-ADL profile and the revised 15-item Myasthenia Gravis Quality of Life questionnaire are currently used in clinical trials (and sometimes in clinical practice) to measure gMG symptoms and their impacts. However, these instruments do not assess the wider consequences of symptoms for patients and their caregivers. Furthermore, although gMG is recognized by patients and physicians to be a fluctuating disease superimposed on a background of continuous symptom burden, most available assessment tools fail to take into account the variable nature of the disease or the impact of symptom fluctuations. An important next step would be to carefully evaluate the existing gMG assessment tools against the symptoms and impacts commonly reported by participants in this study.
Although this study gathered valuable patient insights about symptoms, impacts, and treatment goals, there are some limitations. Two-thirds of the participants were female and all were from the US, which may affect the generalizability of the findings to the wider population. The purposive selection strategy did not aim to ensure geographic diversity; however, although the sample was skewed to the northeast of the US, geographic representation also included all other regions. All diagnoses and treatment types were self-reported and not confirmed by a clinician. This was mitigated by using a screening questionnaire at the time of recruitment that included the following from the patient: a detailed treatment history, including discussion and approximate date of gMG diagnosis, and information on current and previous treatments for gMG. Participants’ responses often implied an effect on caregivers and family; direct evidence of this impact was not solicited in this study. Future research focused on the impact of the symptoms on patients and their caregivers would provide insight into the holistic impacts of gMG.
Both disease symptoms and side effects/burdens from treatment negatively affect patients’ mental status (emotion, mood, anxiety/depression and cognitive function) and social activities; ideally, disease severity and treatment type and intensity should therefore be taken into account in assessing a treatment goal of gMG [39]. This is particularly important as participants sometimes had difficulty disentangling gMG symptoms from those of other conditions (e.g., depression) and medication side effects (e.g., cramps, spasms). However, such detailed assessment was not possible in the context of the patient interviews in this study. Finally, although associations between specific symptoms and specific impacts were often indicated by participants in the interviews (e.g., blurry vision and the impact on driving), the study did not aim to investigate potential links. An area of future research that could inform the treatment of individuals with gMG would be a systematic assessment of the specific symptoms associated with particular impacts. Due to the potential for recall bias, individuals were only asked to discuss treatments received over the past year.
Despite these limitations, the study design had many strengths, including a rigorous qualitative research design that followed guidance and standards from the US FDA [14] and the International Society for Pharmacoeconomics and Outcomes Research [40]. Although participants were predominantly female and white, the sample was diverse with respect to age, education, MG-ADL score, and the type, duration, and combination of treatments, all of which helped broaden the range of patient experiences that were captured in the study. Saturation was carefully tracked and assessed, confirming that the sample size warranted the reporting of results. Although all participants were from the US, and patients’ lived experiences might be expected to vary by country, the findings from this study were in agreement with those from a recent international patient-led analysis that included patients from six European countries as well as the USA [28].
Conclusions
This qualitative study provides valuable insights into patients’ lived experience with gMG, giving a comprehensive overview of gMG symptoms and their impacts. In addition to the impact of physical weakness caused by gMG, participants’ descriptions indicated that symptom fluctuation as well as the continuous symptomatology substantially affected their lives, with consequences for emotional, social, and economic well-being. Participants’ treatment goals for symptom management suggest that greater focus needs to be placed on helping patients with gMG resume a normal stable lifestyle as soon as possible, by achieving the treatment targets of overall symptom stability and reduced fatigue and weakness. Increased awareness of the patient-perceived burden of gMG, as well as patients’ treatment goals, is critical to guide patient–clinician interactions and to inform other decision-makers, such as payers, to ensure access to effective treatments for patients living with gMG. Although some of the effects of gMG symptomatology may not be easy to measure, it is important to consider both fluctuating and persistent symptoms when making treatment decisions and to recognize the impact of uncontrolled symptoms on patients, their partners/caregivers and family/friends; these factors are often not reflected in burden/cost-of-illness studies.
Acknowledgements
The authors thank the participants who were involved in this study. Nancy Law passed away during development of the manuscript and her co-authors gratefully acknowledge her contribution to the paper, and to the MG community. The authors also thank Adrian Kielhorn, Giorgio Giannattasio, and Sivani Paskaradevan (Alexion, AstraZeneca Rare Disease) for critical review of the manuscript.
Funding
Financial support for the conduct of the research and for editorial assistance in preparation of the article, and the Rapid Service fee, were provided by Alexion, AstraZeneca Rare Disease, Boston, USA.
Editorial Assistance
Editorial assistance in development of the article was provided by Deirdre Carman and Duncan Porter of Piper Medical Communications, funded by Alexion, AstraZeneca Rare Disease.
Author Contributions
Concept and design: Kristi Jackson, Anju Parthan, Miranda Lauher-Charest, Lynne Broderick; conducting interviews: Kristi Jackson, Lynne Broderick; coding and analysis: Kristi Jackson, Lynne Broderick, Miranda Lauher-Charest; consultation on interview discussion guide, analysis, interpretation of interview responses: Carolina Barnett, Nancy Law; drafting of manuscript: Kristi Jackson, Anju Parthan, Miranda Lauher-Charest, Lynne Broderick, Carolina Barnett, Nancy Law. All authors read and approved the final manuscript.
Prior Presentation
Data from this study were presented at the 7th Congress of the European Academy of Neurology, Vienna, Austria, June 19–22, 2021; and at the Myasthenia Gravis Foundation of America Congress, Aurora, CO, USA, October 13, 2021.
Disclosures
Kristi Jackson, Miranda Lauher-Charest, and Lynne Broderick are employees of QualityMetric, which received funding for this study from Alexion, AstraZeneca Rare Disease. Anju Parthan was an employee of Alexion, AstraZeneca Rare Disease at the time the study was conducted and analyzed, and is now affiliated with FibroGen. Nancy Law received honoraria from UCB, argenx, and Momenta Pharmaceuticals (now Janssen). Carolina Barnett has received research grants from MGNet, the US Department of Defense, Muscular Dystrophy Canada, Grifols, and Octapharma; she has been a member of an advisory board for Alexion, AstraZeneca Rare Disease, Sanofi, and argenx, and has provided consultancy to Akcea, Takeda, and CSL; she did not receive compensation for this study.
Compliance with Ethics Guidelines
All study materials were reviewed and approved by an independent review board (New England Independent Review Board; NEIRB Study #1286397). Owing to the minimal-risk nature of this study, the independent review board also approved a waiver of documented consent. Participants were provided with a consent document, which was reviewed in detail by the interviewer at the start of the interview; consent (including consent for publication of anonymized responses) was freely given, specific, informed, and unambiguous, and was provided verbally.
Data Availability
The datasets presented in this article are not readily available because the data used were obtained from one-to-one interviews with patients. Alexion, AstraZeneca Rare Disease will consider requests for disclosure of study participant-level data provided that participant privacy is assured through methods such as data de-identification, pseudonymization, or anonymization (as required by applicable law), and if such disclosure was included in the relevant study informed consent form or similar documentation.
Footnotes
References
- 1.Conti-Fine BM, Milani M, Kaminski HJ. Myasthenia gravis: past, present, and future. J Clin Invest. 2006;116(11):2843–2854. doi: 10.1172/jci29894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howard JF., Jr Myasthenia gravis: the role of complement at the neuromuscular junction. Ann N Y Acad Sci. 2018;1412(1):113–128. doi: 10.1111/nyas.13522. [DOI] [PubMed] [Google Scholar]
- 3.Melzer N, Ruck T, Fuhr P, et al. Clinical features, pathogenesis, and treatment of myasthenia gravis: a supplement to the Guidelines of the German Neurological Society. J Neurol. 2016;263(8):1473–1494. doi: 10.1007/s00415-016-8045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai CH, Tseng HF. Nationwide population-based epidemiological study of myasthenia gravis in Taiwan. Neuroepidemiology. 2010;35(1):66–71. doi: 10.1159/000311012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Westerberg E, Punga AR. Epidemiology of myasthenia gravis in Sweden 2006–2016. Brain Behav. 2020;10(11):e01819. doi: 10.1002/brb3.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Neurological Disorders and Stroke. Myasthenia gravis fact sheet. 2020. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Myasthenia-Gravis-Fact-Sheet. Accessed 16 June 2021.
- 7.Gilhus NE, Tzartos S, Evoli A, et al. Myasthenia gravis. Nat Rev Dis Primers. 2019;5(1):30. doi: 10.1038/s41572-019-0079-y. [DOI] [PubMed] [Google Scholar]
- 8.Schneider-Gold C, Hagenacker T, Melzer N, Ruck T. Understanding the burden of refractory myasthenia gravis. Ther Adv Neurol Disord. 2019;12:1756286419832242. doi: 10.1177/1756286419832242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dresser L, Wlodarski R, Rezania K, Soliven B. Myasthenia gravis: epidemiology, pathophysiology and clinical manifestations. J Clin Med. 2021;10:2235. doi: 10.3390/jcm10112235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen LK, Jakobsson AS, Revsbech KL, Vissing J. Causes of symptom dissatisfaction in patients with generalized myasthenia gravis. J Neurol. 2021;268:3086–3093. doi: 10.1007/s00415-021-10902-1. [DOI] [PubMed] [Google Scholar]
- 11.Petersson M, Feresiadou A, Jons D, et al. Patient-reported symptom severity in a nationwide myasthenia gravis cohort: cross-sectional analysis of the Swedish GEMG study. Neurology. 2021;97(14):e1382–e1391. doi: 10.1212/wnl.0000000000012604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Twork S, Wiesmeth S, Klewer J, Pöhlau D, Kugler J. Quality of life and life circumstances in German myasthenia gravis patients. Health Qual Life Outcomes. 2010;8:129. doi: 10.1186/1477-7525-8-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lehnerer S, Jacobi J, Schilling R, et al. Burden of disease in myasthenia gravis: taking the patient's perspective. J Neurol. 2021;269:3050–3063. doi: 10.1007/s00415-021-10891-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Food and Drug Administration. Patient-focused drug development: collecting comprehensive and representative input. Guidance for industry, Food and Drug Administration staff, and other stakeholders. 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-collecting-comprehensive-and-representative-input. Accessed 30 June 2020.
- 15.US Food and Drug Administration. Patient-focused drug development: methods to identify what is important to patients. Guidance for industry, Food and Drug Administration staff, and other stakeholders. 2022. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-methods-identify-what-important-patients. Accessed 3 Mar 2022.
- 16.US Food and Drug Administration. CDER patient-focused drug development. 2022. https://www.fda.gov/drugs/development-approval-process-drugs/cder-patient-focused-drug-development. Accessed 3 Mar 2022.
- 17.Patrick DL, Burke LB, Gwaltney CJ, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–977. doi: 10.1016/j.jval.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Cheng KKF, Clark AM. Qualitative methods and patient-reported outcomes: measures development and adaptation. Int J Qual Methods. 2017;16(1):1609406917702983. doi: 10.1177/1609406917702983. [DOI] [Google Scholar]
- 19.Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park: Sage Publications; 1990. [Google Scholar]
- 20.Creswell JW. Qualitative inquiry and research design: choosing among five approaches. Los Angeles: SAGE Publications; 2013. [Google Scholar]
- 21.Wolf JA, Niederhauser V, Marshburn D, LaVela SL. Defining patient experience. Patient Exp J. 2014;1(1):7–19. [Google Scholar]
- 22.Wolfe GI, Herbelin L, Nations SP, et al. Myasthenia gravis activities of daily living profile. Neurology. 1999;52(7):1487–1489. doi: 10.1212/wnl.52.7.1487. [DOI] [PubMed] [Google Scholar]
- 23.Assarroudi A, Heshmati Nabavi F, Armat M, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs. 2018;23:42–55. doi: 10.1177/1744987117741667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research: Princeton: Recording for the Blind & Dyslexic; 2008.
- 25.Corbin JM, Strauss AL. Basics of qualitative research: techniques and procedures for developing grounded theory. 3. Los Angeles: Sage Publications; 2009. [Google Scholar]
- 26.Turner-Bowker DM, Lamoureux RE, Stokes J, et al. Informing a priori sample size estimation in qualitative concept elicitation interview studies for clinical outcome assessment instrument development. Value Health. 2018;21(7):839–842. doi: 10.1016/j.jval.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 27.Barnett C, Bril V, Kapral M, Kulkarni A, Davis AM. A conceptual framework for evaluating impairments in myasthenia gravis. PLoS ONE. 2014;9(5):e98089. doi: 10.1371/journal.pone.0098089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Law N, Davio K, Blunck M, Lobban D, Seddik K. The lived experience of myasthenia gravis: a patient-led analysis. Neurol Ther. 2021;10(2):1103–1125. doi: 10.1007/s40120-021-00285-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frost A, Svendsen ML, Rahbek J, et al. Labour market participation and sick leave among patients diagnosed with myasthenia gravis in Denmark 1997–2011: a Danish nationwide cohort study. BMC Neurol. 2016;16(1):224. doi: 10.1186/s12883-016-0757-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guastafierro E, Tramacere I, Toppo C, et al. Employment in myasthenia gravis: a systematic literature review and meta-analysis. Neuroepidemiology. 2020;54(4):304–312. doi: 10.1159/000506310. [DOI] [PubMed] [Google Scholar]
- 31.Harris L, Aban IB, Xin H, Cutter G. Employment in refractory myasthenia gravis: a Myasthenia Gravis Foundation of America Registry analysis. Muscle Nerve. 2019;60(6):700–706. doi: 10.1002/mus.26694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagane Y, Murai H, Imai T, et al. Social disadvantages associated with myasthenia gravis and its treatment: a multicentre cross-sectional study. BMJ Open. 2017;7(2):e013278. doi: 10.1136/bmjopen-2016-013278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathers CD, Schofield DJ. The health consequences of unemployment: the evidence. Med J Aust. 1998;168(4):178–182. doi: 10.5694/j.1326-5377.1998.tb126776.x. [DOI] [PubMed] [Google Scholar]
- 34.Voss M, Nylén L, Floderus B, Diderichsen F, Terry PD. Unemployment and early cause-specific mortality: a study based on the Swedish twin registry. Am J Public Health. 2004;94(12):2155–2161. doi: 10.2105/ajph.94.12.2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. CMAJ. 1995;153(5):529–540. [PMC free article] [PubMed] [Google Scholar]
- 36.Modini M, Joyce S, Mykletun A, et al. The mental health benefits of employment: results of a systematic meta-review. Australas Psychiatry. 2016;24(4):331–336. doi: 10.1177/1039856215618523. [DOI] [PubMed] [Google Scholar]
- 37.Waddell G, Burton K, Aylward M. Work and common health problems. J Insur Med. 2007;39(2):109–120. [PubMed] [Google Scholar]
- 38.Keer-Keer T. The lived experience of adults with myasthenia gravis: a phenomenological study. Australas J Neurosci. 2015;25(1):40–6. 10.21307/ajon-2017-112.
- 39.Utsugisawa K, Suzuki S, Nagane Y, et al. Health-related quality-of-life and treatment targets in myasthenia gravis. Muscle Nerve. 2014;50(4):493–500. doi: 10.1002/mus.24213. [DOI] [PubMed] [Google Scholar]
- 40.Harrington RL, Hanna ML, Oehrlein EM, et al. Defining patient engagement in research: results of a systematic review and analysis: report of the ISPOR Patient-Centered Special Interest Group. Value Health. 2020;23(6):677–688. doi: 10.1016/j.jval.2020.01.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets presented in this article are not readily available because the data used were obtained from one-to-one interviews with patients. Alexion, AstraZeneca Rare Disease will consider requests for disclosure of study participant-level data provided that participant privacy is assured through methods such as data de-identification, pseudonymization, or anonymization (as required by applicable law), and if such disclosure was included in the relevant study informed consent form or similar documentation.