Abstract
This report describes a case of a newly diagnosed 49-year-old HIV patient, who presented with decreased visual acuity and retinal lesions characterized by ischemia at the level of the deep retinal capillary plexus, documented with optical coherence tomography (OCT), OCT angiography, fluorescein angiography, and visual fields testing. These lesions closely resembled the morphologic and clinical characteristics of late paracentral acute middle maculopathy. The presence of these lesions suggests that HIV microangiopathy can potentially affect both superficial and deep retinal capillary plexuses.
Keywords: Paracentral acute middle maculopathy, PAMM, HIV, HIV Retinopathy
Introduction
PAMM is a clinical and imaging finding attributed to ischemia of the intermediate (ICP) and deep (DCP) retinal capillary plexuses. Early lesions appear slightly grayer than cotton wool spots, while in spectral-domain optical coherence tomography (OCT), they present as hyper-reflective, band-like lesions from the junction of the inner nuclear layer (INL) and the outer plexiform layer to the full extent of the INL. They resolve gradually, leaving behind areas of INL atrophy (late lesions), accounting for the persistent paracentral scotomas experienced by the patients [1, 2].
PAMM may develop in association with retinal vascular diseases, including diabetic retinopathy, hypertensive retinopathy, central or branch retinal vein occlusion, arterial occlusions, sickle cell retinopathy, or Purtscher retinopathy. Other associations include occlusive retinal vasculitis, post-upper respiratory infection, post-H1N1 vaccination, use of vasopressor medication, sickle cell disease, hypovolemia, migraine, and COVID-19 infection [2–5]. The underlying pathophysiologic mechanism seems to be an ischemic insult on the DCP-ICP, bi-planar capillary system, located at the inner and outer borders of the INL [1, 2, 6].
HIV retinopathy is detectable in up to 70% of AIDS patients, usually as asymptomatic microangiopathy with features similar to diabetic retinopathy (cotton wool spots, retinal hemorrhages, telangiectasias, microaneurysms, or capillary no perfusion areas) [7]. We present the case of a newly diagnosed HIV patient with retinal lesions characterized by ischemia at the level of the deep retinal capillary plexus, closely resembling the morphologic and clinical characteristics of late paracentral acute middle maculopathy. The CARE checklist has been completed by the authors for this case report, attached as online supplementary (for all online suppl. material, see www.karger.com/doi/10.1159/000528408).
Case Report
A 49-year-old Caucasian male was admitted to the Patras University Hospital, presenting with a 10-day history of fever, severe headache, and dizziness. Cerebrospinal fluid examination revealed cryptococcal meningitis. The patient was also diagnosed with pulmonary tuberculosis and HIV infection, with a CD4 count of 45 cells/µL and HIV viral load of 873,083 copies/mL. Upon diagnosis, treatment with liposomal amphotericin B, fluconazole, and antituberculosis agents was commenced.
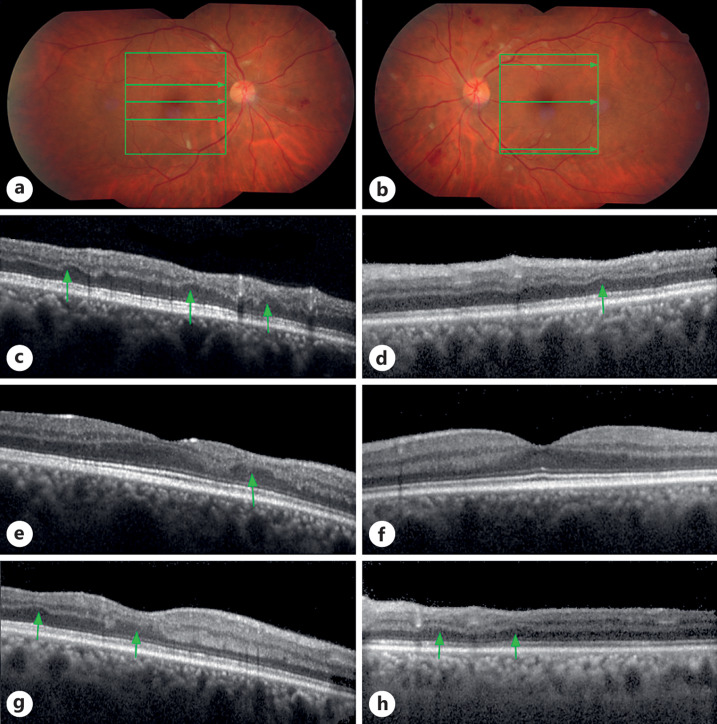
After 7 weeks of treatment and before initiation of antiretroviral therapy (commenced 2 months after the admission), the patient complained of a decrease in visual acuity affecting the right eye and was referred to the ophthalmology department. There was no history of previous ocular disease or surgery, and the patient’s best corrected visual acuity (BCVA) was 9/10 OD and 10/10 OS. Anterior segment evaluation was unremarkable. Dilated fundus examination revealed cotton wool spots and pre- and intraretinal hemorrhages in both eyes compatible with HIV retinopathy (Fig. 1a, b).
Fig. 1.
Color fundus and OCT imaging: HIV retinopathy and INL thinning. a Right eye at presentation: cotton wool spots, pre-, and intraretinal hemorrhages. OCT scan frame and scan lines are presented as green square and arrows. b Left eye at presentation: cotton wool spots, pre-, and intraretinal hemorrhages, extending in a larger region than in the right eye but respecting the macula. c, e, g OCT scans of the right eye, revealing areas with INL thinning (arrows), including the macula. Scan lines are presented in A above as green arrows. d, f, h OCT scans of the left eye, revealing areas with INL thinning (arrows), respecting the macula. Scan lines are presented in B above as green arrows.
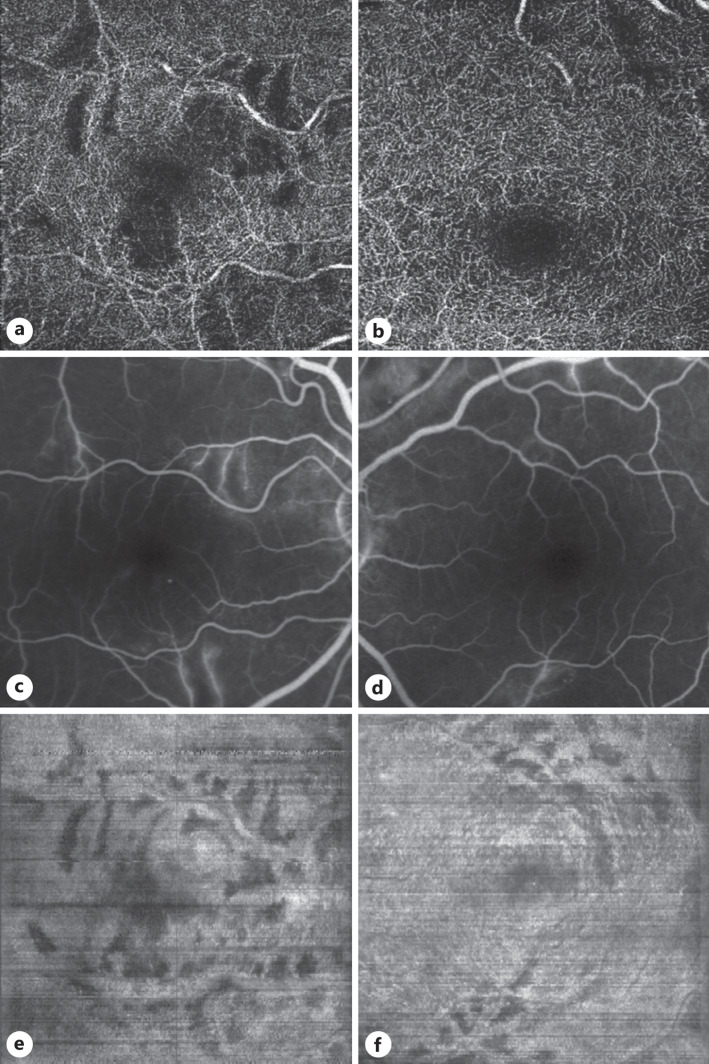
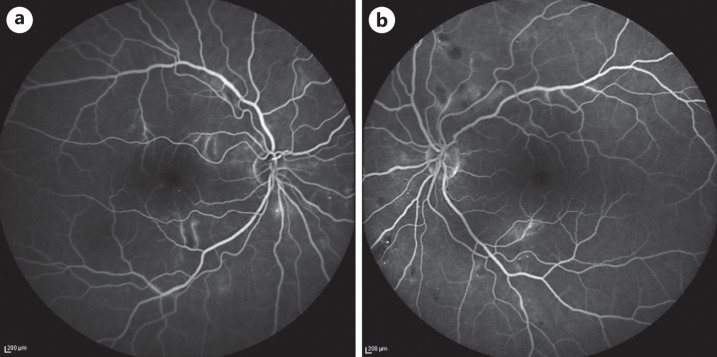
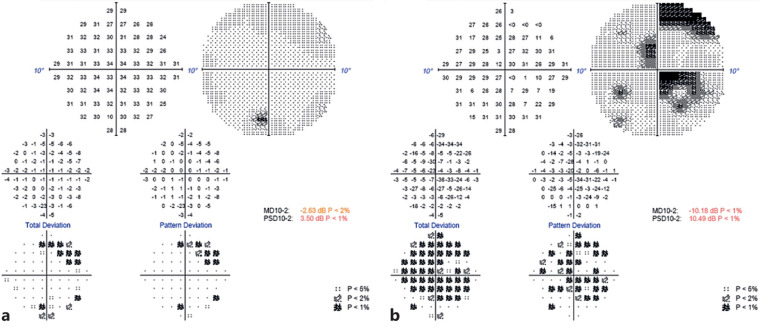
Spectral-domain OCT (SD-OCT, Spectralis HRA + OCT; Heidelberg Engineering GmbH, Heidelberg, Germany) revealed the presence of INL thinning below the fovea in OD in the parafoveal area in OD and OS (Fig. 1c–h). OCT angiography (OCTA; Triton Swept Source OCT, Topcon) revealed areas of DCP ischemia devoid of capillaries (Fig. 2a, b). Fluorescein angiography revealed microaneurysms and areas of late leakage in both eyes (Fig. 2c, d and 3a, b). Visual field (VF) testing (Zeiss Humphrey Field Analyzer 3) documented the presence of central (OD) and paracentral (OD and OS) scotomas (Fig. 4a, b).
Fig. 2.
En face OCT reconstruction, OCT angiography, and FA. a, b OCT angiography at the level of the deep capillary plexus. The areas devoid of capillaries coincide with the areas of thinning in a and b above, indicating the conjunction of DCP ischemia with the late PAMM-like lesions. c, d Enlarged images of the FA, to facilitate the comparison with the en face reconstructed images and OCT angiography. e, f En face OCT reconstruction at the INL-OPL level with concurrent shadow removal revealing dark areas of INL thinning consistent with late PAMM lesions. FA, fluorescein angiography; OPL, outer plexiform layer.
Fig. 3.
Full (55°) view of late-phase FA. Evident microaneurysms and areas of late leakage in both eyes. a Right eye. b Left eye. FA, fluorescein angiography.
Fig. 4.
VFs (SITA Fast, 10–2). a Left eye. b Right eye.
Discussion
In our patient, along with the classical manifestations of HIV microangiopathy, we detected areas of focal INL atrophy, fulfilling the morphologic and VF characteristics of late-stage PAMM [8–10]. The early stage of these lesions was not detected, possibly because the patient failed to pay attention and timely report ocular manifestations due to other severe and life-threatening symptoms.
OCTA revealed areas of deep retinal capillary plexus (DCP) ischemia, devoid of capillaries (Fig. 2a, b), coinciding and presenting the same pattern with the areas of the late PAMM-like lesions. Central and/or paracentral scotomas characteristic of late PAMM lesions were detected on the VFs in both eyes (Fig. 4a, b).
To better localize these late PAMM-like lesions, we performed an en face SD-OCT reconstruction at the INL-outer plexiform layer level with concurrent shadow removal based on a technique we have already described [11]. The involved retina presented in a branch and leaf-like pattern; areas of thinning located between branching retinal arteries but not below them (Fig. 2e, f). It seems that the proximity to major vessels may play a protective role securing sufficient perfusion pressure to the underlying DCP-ICP.
Although PAMM has not been directly associated with HIV retinopathy, the detected lesions are consistent with late PAMM. The exact pathogenic mechanism remains to be elucidated, though an increase in plasma viscosity, immune complex deposition, rigidity of circulating neutrophils, and direct infection of the vascular endothelium by HIV, alone or in combination, are all probable. The distinct possibility that these findings could be related to the systemic infection, as seen in sepsis, cannot be excluded, but seems unlikely as the clinical presentation is not fully compatible with cryptococcal or tuberculous retinal lesions.
It seems that HIV infection can potentially affect all the retinal capillary plexuses: the SCP in the form of cotton wool spots, and the ICP and DCP in the form of PAMM-like lesions. Since the aforementioned late PAMM-like lesions can only be documented with SD-OCT and OCTA imaging, and parafoveal lesions may not cause apparent symptoms, we suggest that detailed imaging should be performed in all HIV patients presenting with HIV retinopathy, as the prevalence, importance, and clinical correlations of these lesions in HIV patients are still unknown.
Statement of Ethics
Ethical approval is not required for this study in accordance with local or national guidelines. Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images. This report does not contain any personal information that could lead to the identification of the patient.
Conflict of Interest Statement
The authors report no conflicts of interest to declare.
Funding Sources
No funding sources of any kind to declare.
Author Contributions
Menelaos Kanakis initially examined and followed up the patient’s ophthalmologic manifestations, processed OCT images, and drafted the manuscript. Ilias Georgalas performed OCTA data analysis and critically revised the manuscript. Vassilios Kozombolis critically revised and finalized the manuscript. Alexandra Lekkou treated the patient as infectious disease specialist and critically revised the manuscript. Efthymios Karmiris edited video files and critically revised the manuscript. Panagiotis Stavrakas combined the data and critically revised the manuscript. The final version of the manuscript was approved by all authors. Authors attest that they meet the current ICMJE criteria for authorship.
Funding Statement
No funding sources of any kind to declare.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.
Supplementary Material
References
- 1. Rahimy E, Sarraf D. Paracentral acute middle maculopathy spectral-domain optical coherence tomography feature of deep capillary ischemia. Curr Opin Ophthalmol. 2014 May;25(3):207–12. 10.1097/ICU.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 2. Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral acute middle maculopathy: what we knew then and what we know now. Retina. 2015 Oct;35. (10); p. 1921–30. 10.1097/IAE.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 3. Chen X, Rahimy E, Sergott RC, Nunes RP, Souza EC, Choudhry N, et al. Spectrum of retinal vascular diseases associated with paracentral acute middle maculopathy. Am J Ophthalmol. 2015 Jul;160(1):26–34.e1. 10.1016/j.ajo.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 4. Ilginis T, Keane PA, Tufail A. Paracentral acute middle maculopathy in sickle cell disease. JAMA Ophthalmol. 2015 May;133(5):614–6. 10.1001/jamaophthalmol.2014.6098. [DOI] [PubMed] [Google Scholar]
- 5. Castro CS, Ferreira AS, Silva NP, Lume MR, Furtado MJ. Paracentral acute middle maculopathy after COVID-19 disease: multimodal evaluation. Retin Cases Brief Rep. 2022 Jul 15. 10.1097/ICB.0000000000001301. [DOI] [PubMed] [Google Scholar]
- 6. Sarraf D, Rahimy E, Fawzi AA, Sohn E, Barbazetto I, Zacks DN, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013 Oct;131(10):1275–87. 10.1001/jamaophthalmol.2013.4056. [DOI] [PubMed] [Google Scholar]
- 7. Bittencourt MG, Agbedia OO, Liu HT, Annam R, Sepah YJ, Leder HA, et al. Ocular complications of HIV/AIDS in the era of HAART. Expert Rev Ophthalmol. 2012;7(6):555–64. 10.1586/eop.12.65. [DOI] [Google Scholar]
- 8. Shah A, Rishi P, Chendilnathan C, Kumari S. OCT angiography features of paracentral acute middle maculopathy. Indian J Ophthalmol. 2019 Mar;67(3):417–9. 10.4103/ijo.IJO_1249_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maltsev DS, Kulikov AN, Burnasheva MA, Freund KB. Vascular microanatomy of small resolved paracentral acute middle maculopathy lesions. Ophthalmol Retina. 2021 Sep;5(9):928–34. 10.1016/j.oret.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 10. Scharf J, Freund KB, Sadda S, Sarraf D. Paracentral acute middle maculopathy and the organization of the retinal capillary plexuses. Prog Retin Eye Res. 2021 Mar;81:100884. 10.1016/j.preteyeres.2020.100884. [DOI] [PubMed] [Google Scholar]
- 11. Kanakis MG, Giannouli K, Andreanos K, Papaconstantinou D, Koutsandrea C, Ladas I, et al. Capillary nonperfusion and photoreceptor loss in branch retinal vein occlusion: spatial correlation and morphologic characteristics. Retina. 2017 Sep;37(9):1710–22. 10.1097/IAE.0000000000001410. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.