Abstract
Study Design:
Multicentric retrospective study, Level of evidence III.
Objective:
The objective of this multicentric study was to analyze the prevalence and risk factors of early postoperative complications in adult spinal deformity patients treated with fusion. Additionally, we studied the impact of complications on unplanned readmission and hospital length of stay.
Methods:
Eight spine centers from 6 countries in Latin America were involved in this study. Patients with adult spinal deformity treated with fusion surgery from 2017 to 2019 were included. Baseline and surgical characteristics such as age, sex, comorbidities, smoking, number of levels fused, number of surgical approaches were analyzed. Postoperative complications at 30 days were recorded according to Clavien-Dindo and Glassman classifications.
Results:
172 patients (120 females/52 males, mean age 59.4 ± 17.6) were included in our study. 78 patients suffered complications (45%) at 30 days, 43% of these complications were considered major. Unplanned readmission was observed in 35 patients (20,3%). Risk factors for complications were: Smoking, previous comorbidities, number of levels fused, two or more surgical approaches and excessive bleeding. Hospital length of stay in patients without and with complications was of 7.8 ± 13.7 and 17 ± 31.1 days, respectively (P 0.0001).
Conclusion:
The prevalence of early postoperative complications in adult spinal deformity patients treated with fusion was of 45% in our study with 20% of unplanned readmissions at 30 days. Presence of complications significantly increased hospital length of stay.
Keywords: adult spinal deformity, postoperative complications, readmission, hospital length of stay, clavien-dindo classification
Introduction
Adult spinal deformity (ASD) is a degenerative condition that is associated with pain, disability and low quality of life.1-3 Surgical treatment is indicated after failure of nonoperative management and involves decompression, fusion and global balance restoration that can improve patient satisfaction.4-6 However, complications associated with surgical treatment of ASD remains relatively high7-9 and increase morbidity, hospital length of stay (LOS), unplanned readmissions and mortality rates with consequent increase in health costs. 10
The report of complications in spine surgery, on the other hand, is heterogeneous due to the lack of a unified, universally accepted system, the terms minor and major complications by Glassman is usually employed, being mainly descriptive. 11 Recently, Clavien and Dindo developed a five-grade classification system of postoperative complications based on severity and management to address a complication,12-14 this classification has been used in general surgery and rapidly extended to other surgical specialties. In spine surgery, this system has been employed in few studies.8,15-17 However, this classification has not been universally accepted in spine surgery and the relationship with hospital length of stay and readmission in ASD is not clearly understood.
The objectives of this study are to report, through a multicentric registry in Latin America, the prevalence of postoperative complications at 30 days in ASD patients treated with fusion surgery using the Clavien-Dindo classification and to analyze the impact of postoperative complications on hospital LOS and unplanned readmission. In addition, we evaluated the prevalence of complications according to Glassman and described the main complications.
Material and Methods
This is a retrospective multicentric registry that involved 8 Spine centers from 6 countries in Latin America (Argentina, Brazil, Uruguay, Chile, Colombia and Mexico) from January 2017 to December 2019. Institutional review board was obtained prior initiation of registry (IRB 00010193), no informed consent was required for this study. Inclusion criteria were as follows: ≥18 years old patients with ASD defined as having at least one of the following radiological findings: Thoracic, lumbar or thoracolumbar scoliotic curve with a cobb angle of ≥ 20°, sagittal vertical axis (SVA) of ≥ 60 millimeters, pelvic tilt (PT) of ≥ 20°, thoracic kyphosis of ≥ 60°, surgically treated with fusion surgery of ≥ 3 levels with/without associated decompression surgery, anterior, posterior and double approach were also included, with a minimal follow-up of 6 months.
Patients with history of previous or active postoperative spinal infection, active oncologic conditions or incomplete registry were excluded from the analysis.
Descriptive characteristics were reported as age, sex, American Society of Anaesthesiology (ASA) grade. Comorbidities were also collected, such as: obesity, defined as body mass index of ≥ 30, diabetes, cardiac (uncontrolled hypertension, history of myocardial infarction, coronary artery disease), pulmonary (asthma, chronic obstructive pulmonary disease COPD) and active smoking status. Surgical variables included: number of level fused, surgical approach (posterior, anterior, double), primary or revision surgery, surgical duration (minutes), preoperative and postoperative albumin, hematocrit and hemoglobin.
Definition of Complications
Complications were defined according to Dindo et al 12 as any deviation from the normal postoperative course. Complications were recorded using the modified Clavien-Dindo classification for postoperative complications of Orthopaedic and Spine surgery (Table 1) 17 and Glassman classification. 11
Table 1.
Classification of Surgical Complications According to Dindo-Clavien Adapted to Orthopedic Surgery.
| Gender | Definition |
|---|---|
| I | Non-life-threatening complication that requires transient medication and resolves within the next 72 h. |
| II | Requiring pharmacological intervention for at least 72 h, or
Active observation without interventions.
|
| III | Requiring surgical, endoscopic, or radiographic
intervention
|
| IV | Life-threatening complication requiring IC/ICU
management
|
| V | Death |
Primary outcomes were overall prevalence of complications, complication distribution according to Clavien-Dindo and Glassman, hospital LOS and unplanned readmission up to 30 days.
Statistical Analysis
Categorical variables were described as their absolute and relative frequency with percentages. The quantitative variables were described as mean and standard deviation (SD) or median and interquartile range (IQR) according to the observed distribution. Comparisons among the categorical variables were made between the different groups (with and without complication), based on degree of complication with a global chi-square. The quantitative variables (age, hospital stay, number of levels fused, surgical time) were compared between the groups of complication yes/no or degrees of complication with a t test or Wilcoxon according to the distribution of the observed variable. It was considered a significant association if P < .05.
The statistical analysis was performed with the software Minitab18 y RStudio Version 1.1.383
Results
Between January 2017 and December 2019, 192 ASD patients surgically treated in the participating centers were included. 15 patients did not meet one or more inclusion criteria and were excluded, 5 patients were also excluded for incomplete registry. A total of 172 ASD patients were analyzed (120 females/52 males) with a mean age and SD of 59.4 ± 17.6. Regarding postoperative complications at 30 days, 78 patients suffered at least one complication (45.6%) based on Clavien-Dindo classification, overall hospital LOS was of 11.9 ± 23 days and unplanned readmission was observed in 35 patients (20.3%).
Prevalence of Complications According to Clavien-Dindo and Glassman
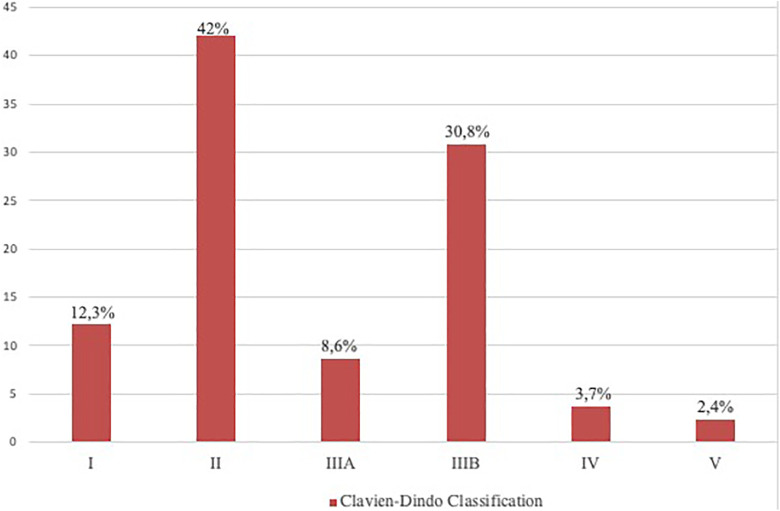
Figures 1 and 2 show distribution of complications according to Clavien-Dindo and Glassman.
Figure 1.
Distribution of postoperative complications according to Clavien-Dindo Classification, type II complications were the most common (42%) followed by IIIB (30.8%).
Figure 2.
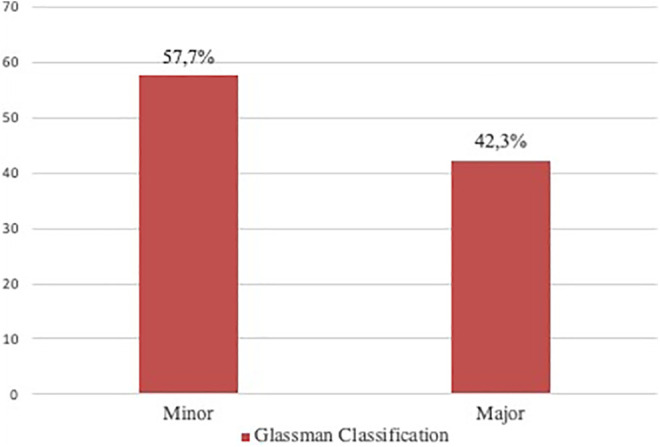
Distribution of complications according to Glassman, 57% were considered minor complications and 43% were major.
Table 2 shows relative and absolute frequency of complications.
Table 2.
Absolute and Relative Frequency of Complications and Hospital Length of Stay.
| Complication | Number | Percentage | Hospital LOS (mean and SD) |
|---|---|---|---|
| Excessive bleeding* | 17 | 21.8 | 10 ± 7.8 |
| Deep wound infection | 15 | 19.2 | 37.3 ± 41.8 |
| Radicular symptoms/ excessive pain | 8 | 11.1 | 12.2 ± 9 |
| Fracture/PKJ | 7 | 8.9 | 71 ± 79.4 |
| Wound hematoma/Seroma | 5 | 6.4 | 9 ± 5.7 |
| Implant mispositioning** | 4 | 5.1 | 12 ± 5.1 |
| Incidental Dural tear | 4 | 5.1 | 32.7 ± 38.9 |
| Deep vein thrombosis | 3 | 3.8 | 7.5 ± 4 |
| Wound dehiscence | 3 | 3.8 | 6.3 ± 2.3 |
| Overall medical complications | 30 | 38,4 | 8.8 ± 6.4 |
| Overall surgical complications | 48 | 61,5 | 33.5 ± 48.7 |
* Excessive bleeding that required non-scheduled transfusion.
**Implant mispositioning that required reoperation.
Baseline and Surgical Characteristics in Patients With and Without Complications
Table 3 shows baseline and surgical characteristics of patients with and without complications, as we can observe in the table, significant differences were observed in the presence of comorbidities (P 0.006), smoking (P 0.027), number of levels fused (P 0.04), need of more than a single approach (P 0.003) and postoperative hemoglobin (P 0.004).
Table 3.
Baseline and Surgical Characteristics in Patients With and Without Complications.a
| No complication group (N: 93) | Complication group (N: 78) | P | |
|---|---|---|---|
| Age (mean/ SD) | 57.5 (18.1) | 61.5 (15.8) | 0.173 |
| Sex (female %) | 73.6 | 75.8 | 0.624 |
| ASA | - | - | 0.078 |
| Comorbidities (%) | 42 | 58 | 0.006 |
| Smoking (%) | 42.3 | 57.7 | 0.027 |
| Surgical duration (min) | 300.7 (120) | 339 (145) | 0.063 |
| Number of levels fused | 5.7 (3.8) | 6.6 (3.8) | 0.04 |
| Primary surgery (%) | 52.9 | 47.1 | 0.638 |
| Posterior single approach (%) | 60.6 | 39.4 | 0.003 |
| Preoperative Hemoglobin (gr/dl SD) | 13.7 (1.4) | 13.6 (1.3) | 0.516 |
| Postoperative Hemoglobin (gr/dl SD) | 12 (4.4) | 10.8 (3.2) | 0.004 |
| Preoperative albumin (gr/dl SD) | 3.9 (0.4) | 4.1 (0.5) | 0.472 |
| Preoperative Hematocrit (%) | 41.1 (3.9) | 41.3 (3.9) | 0.745 |
| Postoperative Hematocrit (%) | 32 (6.7) | 31.2 (5.1) | 0.107 |
aBold numbers illustrate statistical significant differences.
30-Day Unplanned Readmission
Table 4 illustrates overall 30-day readmission and reoperation rates. In addition, main causes of readmission were mentioned.
Table 4.
30-Days Readmission Rate and Main Causes.
| n | % | |
|---|---|---|
| Overall 30-day readmission | 35 | 100 |
| Wound infection | 15 | 42.8 |
| Implant failure/Proximal junctional kyphosis | 7 | 20 |
| Incidental dural tear | 3 | 8.5 |
| Postoperative pain requiring readmission | 8 | 22.8 |
| Wound dehiscence | 2 | 5.7 |
| Overall 30 day-reoperation* | 26 | 74.3 |
* Reoperation at 30 days from the patients readmitted to the hospital.
Hospital LOS
Mean hospital stay in patients without complications was of 7.8 ± 13.7 days (median 5; IQR 4-7), while patient with complications had a mean stay of 17 ± 31.1 days (median 8.5; IQR 6-15). There were significant differences in terms of hospital length of stay between both groups (P 0.0001).
Mean and SD hospital LOS according to Clavien-Dindo classification was a follow:
Type I: 6.5 ± 4.6 days; Type II: 8.3 ± 5.3 days; Type IIIA: 13.5 ± 7.9 days; Type IIIB: 33.6 ± 51 days; Type IV: 65 ± 55 days and Type V: 16 ± 16.9 days.
Based on Glassman, hospital LOS in minor and major complications was of 15 ± 9.8 days and 63 ± 73.8 days, respectively.
Discussion
Surgical treatment of adult spine deformity has been associated with a relative high range of complications, and it is a challenge for surgeons and institutions.
Our study showed a 30-day surgical complication rate of 45% according to Clavien-Dindo classification, 42% of these complications were considered major using Glassman classification. We also found a significant increase in hospital LOS in patients with complications compared to non-complicated cases. Finally, the 30-day unplanned readmission was of 20%.
The importance of reporting complications in clinical studies relies on different aspects; first, it allows knowing the prevalence of these events. Regarding prevalence of complications, Smith et al 18 found a 52% of perioperative complications in a prospective multicentric study of ASD patients, 53% of these complications were considered minor and 47% were major. In our study, the prevalence was slightly lower with similar distribution in terms of minor and major complications. In another study, Soroceanu et al 19 examined medical complications in 448 surgical ASD patients and found 26% of complications. Smoking, hypertension and long history of spinal symptoms were the main predictors for medical complications. In our study, smoking status and comorbidities were factors associated with complications, but the prevalence of medical complications was of 17%, which is lower than the reported by the author. Regarding risk factors, smoking status, patient comorbidities and number of levels fused were significantly associated with surgical complications, compared to those without. Similar risk factors are found in the literature.20-21 It is worth mentioning that neither duration of smoking nor number of cigarettes per day were analyzed in our study.
We found that excessive bleeding leading to postoperative anemia requiring non-programed transfusion was the most common non-surgical complication. Furthermore, we found significant differences in postoperative hemoglobin. Patients with complications presented lower values of hemoglobin compared to those without complications. Excessive bleeding can be associated with complications and increased hospital LOS.22-24 There are different methods to estimated blood loss, 25 we decided to use difference between preoperative and postoperative hemoglobin as a more reliable parameter according to Purvis et al. 26 Low levels of hemoglobin are related to delayed wound healing, especially when combined with risk factors such as low oxygenation, higher age, diabetes, obesity, alcoholism, smoking, and poor nutrition status. Those are important factors to determine patient’s frailty index. A better understanding of the influence of these combined factors in complex spinal surgery in adults, such as spinal deformities, may lead to therapeutics that improve wound healing. An extensive work on identifying adult patients with indication for complex spinal surgery that will most likely present complications on early postoperative period has been done in the last decade. 27 This amount of data will hypothetically lead us on the decision making of which patient should we do surgery. Although there are considerable rates of complications, surgery for adult spinal deformity has been shown to be beneficial even after long time follow up. 28 In the light of health economics and programs to lower costs in health care, we should clearly understand the benefits of operating patients with adult spinal deformity and avoid complications that frequently increase final treatment cost.
In our study, we found significant higher hospital LOS in patients with complications compared to non-complication group. Wound infection and proximal junctional kyphosis were the main causes for 30-days readmission. Similar results were found in previous studies.16,29,30 We had 20% of unplanned readmission at 30-days, Schairer 31 found 8.4% of unplanned readmission after fusion in ASD patients. Similarly, De la Garza Ramon et al 32 reported 11% of 30-day readmission after 3 column osteotomies for ASD patients and 8% of reoperation rate. Manoharam et al 33 and Lee et al. 34 had 7.5% and 7% readmission, respectively. Readmission causes in our study were similar with wound infection and proximal junctional kyphosis as the main reasons, however, we found higher readmission rate in our study, probably due to the prevalence of major complications, which represented 43% of the total complications. While wound infections are not only related to the surgical procedure itself, but to a number of risk factors as stated before, proximal junctional kyphosis is mostly related to suboptimal preoperative surgical planning. As we better understand patients’ global alignment and abnormal parameters in adult spinal deformity, we can better plan spinal correction goals before surgery. 35 Poor bone quality, Parkinson disease, infection, smoking are well known risk factors for proximal junctional failure in spine surgery, but an unbalanced or hyper corrected spine is now considered as one of the main reasons for implant and junctional failure.36,37
Our study has some limitations. First, this is a retrospective analysis from electronic medical records of 8 institutions in Latin America and selection bias could be present as there could be patients not properly included in the analysis due to its retrospective nature. However, since all institutions included are equipped with electronic medical records and we demanded a short follow-up to our objective, we believe that most of the patients included were properly recorded. Another limitation is related to the institutions included in the analysis. Although all 8 centers are tertiary level with expertise in the treatment of ASD, we cannot extrapolate these results to the entire continent population. However, since this is the first multicentric registry for ASD patients in South America, this constitutes a positive inflexion point for many surgeons and institutions in our region to foster multicentric analysis and improve teamwork among different centers.
Knowing the impact of complications on spine surgery in patients’ quality of life, hospital readmission and length of stay is important for to the patient, surgeons and healthcare institutions and understanding the main risk factors will lead to decreasing rate of complications and improvement of surgical management.38-40 Efforts should be spent on identifying patients that are at higher risk for complication in complex spine surgery. Prospective multicentric registry is mandatory in our region in order to stablish homogeneous records of complications, through a unified system and focus of effort in identifying risk factors for complication, decreasing complications and improving postoperative outcomes in ASD patients.
Conclusion
Patients with adult spinal deformity undergoing surgical treatment presented a 45% of complication rate and 20% unplanned readmission rate at 30 days. Risk factors for complications in ASD surgery were presence of comorbidities, smoking, number of levels fused and need for more than a single approach. The presence of complications significantly increased Hospital LOS. Longer term follow-up studies would be helpful to understand the role of risk factors as well as the impact of complications on postoperative outcomes.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Gaston Camino-Willhuber, MD  https://orcid.org/0000-0002-5684-7679
https://orcid.org/0000-0002-5684-7679
Alfredo Guiroy, MD  https://orcid.org/0000-0001-9162-6508
https://orcid.org/0000-0001-9162-6508
Nelson Astur, MD  https://orcid.org/0000-0002-2608-2118
https://orcid.org/0000-0002-2608-2118
Murilo Daher, MD  https://orcid.org/0000-0001-9589-5596
https://orcid.org/0000-0001-9589-5596
Baron Zarate-Kalfopulos, MD  https://orcid.org/0000-0002-0630-2662
https://orcid.org/0000-0002-0630-2662
Ratko Yurac, MD  https://orcid.org/0000-0003-3603-6294
https://orcid.org/0000-0003-3603-6294
Emiliano Vialle, MD  https://orcid.org/0000-0003-1157-4889
https://orcid.org/0000-0003-1157-4889
References
- 1.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population . Spine (Phila Pa 1976). 2005;30(9):1082–1085. doi:10.1097/01.brs.0000160842.43482.cd [DOI] [PubMed] [Google Scholar]
- 2.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013;38(13):E803–E812. doi:10.1097/BRS.0b013e318292b7b9 [DOI] [PubMed] [Google Scholar]
- 3.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024–2029. doi:10.1097/01.brs.0000179086.30449.96 [DOI] [PubMed] [Google Scholar]
- 4.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery . Spine (Phila Pa 1976). 2010;35(25):2224–2231. doi:10.1097/BRS.0b013e3181ee6bd4 [DOI] [PubMed] [Google Scholar]
- 5.Takemoto M, Boissière L, Vital JM, et al. Are sagittal spinopelvic radiographic parameters significantly associated with quality of life of adult spinal deformity patients? Multivariate linear regression analyses for pre-operative and short-term post-operative health-related quality of life. Eur Spine J. 2017;26(8):2176–2186. doi:10.1007/s00586-016-4872-y [DOI] [PubMed] [Google Scholar]
- 6.Pizones J, Moreno-Manzanaro L, Sánchez Pérez-Grueso FJ, et al. Restoring the ideal Roussouly sagittal profile in adult scoliosis surgery decreases the risk of mechanical complications. Eur Spine J. 2020;29(1):54–62. doi:10.1007/s00586-019-06176-x [DOI] [PubMed] [Google Scholar]
- 7.Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D. Study group on scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976). 2012;37(8):693–700. doi:10.1097/BRS.0b013e31822ff5c1 [DOI] [PubMed] [Google Scholar]
- 8.Klineberg EO, Passias PG, Poorman GW, et al. Classifying complications: assessing adult spinal deformity 2-year surgical outcomes. Global Spine J. 2020;10(7):896–907. doi:10.1177/2192568220937473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J. 2003;3(6):496–501. doi:10.1016/s1529-9430(03)00426-1 [DOI] [PubMed] [Google Scholar]
- 10.McCarthy I, Hostin R, O’Brien M, Saigal R, Ames CP. Health economic analysis of adult deformity surgery. Neurosurg Clin N Am. 2013;24(2):293–304. doi:10.1016/j.nec.2012.12.005 [DOI] [PubMed] [Google Scholar]
- 11.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32(24):2764–2770. doi:10.1097/BRS.0b013e31815a7644 [DOI] [PubMed] [Google Scholar]
- 12.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi:10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–526. [PubMed] [Google Scholar]
- 14.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi:10.1097/SLA.0b013e3181b13ca2 [DOI] [PubMed] [Google Scholar]
- 15.Willhuber GC, Stagnaro J, Petracchi M, et al. Short-term complication rate following orthopedic surgery in a tertiary care center in Argentina. SICOT J. 2018;4:26. doi:10.1051/sicotj/2018027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Camino Willhuber G, Elizondo C, Slullitel P. Analysis of postoperative complications in spinal surgery, hospital length of stay, and unplanned readmission: application of Dindo-Clavien classification to spine surgery. Global Spine J. 2019;9(3):279–286. doi:10.1177/2192568218792053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Camino Willhuber G, Slullitel P, Taype Zamboni D, et al. validation of a modified Clavien-Dindo classification for postoperative complications in orthopedic surgery. Rev Fac Cien Med Univ Nac Cordoba. 2020;77(3):161–167. Published 2020 August 21. doi:10.31053/1853.0605.v77.n3.27931 [DOI] [PubMed] [Google Scholar]
- 18.Smith JS, Klineberg E, Lafage V, et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine. 2016;25(1):1–14. doi:10.3171/2015.11.SPINE151036 [DOI] [PubMed] [Google Scholar]
- 19.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976). 2016;41(22):1718–1723. doi:10.1097/BRS.0000000000001636 [DOI] [PubMed] [Google Scholar]
- 20.Martin CT, Gao Y, Duchman KR, Pugely AJ. The impact of current smoking and smoking cessation on short-term morbidity risk after lumbar spine surgery. Spine (Phila Pa 1976). 2016;41(7):577–584. doi:10.1097/BRS.0000000000001281 [DOI] [PubMed] [Google Scholar]
- 21.McCunniff PT, Young ES, Ahmadinia K, Ahn UM, Ahn NU. Smoking is associated with increased blood loss and transfusion use after lumbar spinal surgery. Clin Orthop Relat Res. 2016;474(4):1019–1025. doi:10.1007/s11999-015-4650-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khanna R, Harris DA, McDevitt JL, et al. Impact of anemia and transfusion on readmission and length of stay after spinal surgery: a single-center study of 1187 operations. Clin Spine Surg. 2017;30(10):E1338–E1342. doi:10.1097/BSD.0000000000000349 [DOI] [PubMed] [Google Scholar]
- 23.Elsamadicy AA, Adogwa O, Vuong VD, et al. Association of intraoperative blood transfusions on postoperative complications, 30-day readmission rates, and 1-year patient-reported outcomes. Spine (Phila Pa 1976). 2017;42(8):610–615. doi:10.1097/BRS.0000000000001803 [DOI] [PubMed] [Google Scholar]
- 24.Blackburn CW, Morrow KL, Tanenbaum JE, DeCaro JE, Gron JM, Steinmetz MP. Clinical outcomes associated with allogeneic red blood cell transfusions in spinal surgery: a systematic review. Global Spine J. 2019;9(4):434–445. doi:10.1177/2192568218769604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pennington Z, Ehresman J, Molina CA, et al. A novel predictive model of intraoperative blood loss in patients undergoing elective lumbar surgery for degenerative pathologies [published online ahead of print June 27, 2020]. Spine J. 2020;S1529-9430(20)30825-1. doi:10.1016/j.spinee.2020.06.019 [DOI] [PubMed] [Google Scholar]
- 26.Purvis TE, Goodwin CR, Molina CA, Frank SM, Sciubba DM. Percentage change in hemoglobin level and morbidity in spine surgery patients. J Neurosurg Spine. 2018;28(3):345–351. doi:10.3171/2017.7.SPINE17301 [DOI] [PubMed] [Google Scholar]
- 27.Reid DBC, Daniels AH, Ailon T, et al. Frailty and health-related quality of life improvement following adult spinal deformity surgery. World Neurosurg. 2018;112: e548–e554. doi:10.1016/j.wneu.2018.01.079 [DOI] [PubMed] [Google Scholar]
- 28.Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP. Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine. 2018;28(2):194–200. doi:10.3171/2017.6.SPINE17357 [DOI] [PubMed] [Google Scholar]
- 29.Blumberg TJ, Woelber E, Bellabarba C, Bransford R, Spina N. Predictors of increased cost and length of stay in the treatment of postoperative spine surgical site infection. Spine J. 2018;18(2):300–306. doi:10.1016/j.spinee.2017.07.173 [DOI] [PubMed] [Google Scholar]
- 30.Yeramaneni S, Gum JL, Carreon LY, et al. Impact of readmissions in episodic care of adult spinal deformity: event-based cost analysis of 695 consecutive cases. J Bone Joint Surg Am. 2018;100(6):487–495. doi:10.2106/JBJS.16.01589 [DOI] [PubMed] [Google Scholar]
- 31.Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976). 2013;38(19):1681–1689. doi:10.1097/BRS.0b013e31829c08c9 [DOI] [PubMed] [Google Scholar]
- 32.De la Garza Ramos R, Nakhla J, Echt M, et al. Risk factors for 30-day readmissions and reoperations after 3-column osteotomy for spinal deformity. Global Spine J. 2018;8(5):483–489. doi:10.1177/2192568217739886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM. Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J. 2016;16(7):862–866. doi:10.1016/j.spinee.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 34.Lee NJ, Lenke LG, Cerpa M, et al. The 90-day reoperations and readmissions in complex adult spinal deformity surgery [published online ahead of print September 3, 2020]. Global Spine J. 2020;2192568220953391. doi:10.1177/2192568220953391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lafage R, Beyer G, Schwab F, et al. Risk factor analysis for proximal junctional kyphosis after adult spinal deformity surgery: a new simple scoring system to identify high-risk patients. Global Spine J. 2020;10(7):863–870. doi:10.1177/2192568219882350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duan PG, Mummaneni PV, Rivera J, et al. The association between lower Hounsfield units of the upper instrumented vertebra and proximal junctional kyphosis in adult spinal deformity surgery with a minimum 2-year follow-up. Neurosurg Focus. 2020;49(2): E7. doi:10.3171/2020.5.FOCUS20192 [DOI] [PubMed] [Google Scholar]
- 37.Zhao J, Chen K, Zhai X, Chen K, Li M, Lu Y. Incidence and risk factors of proximal junctional kyphosis after internal fixation for adult spinal deformity: a systematic evaluation and meta-analysis [published online ahead of print May 19, 2020]. Neurosurg Rev. 2020;10.1007/s10143-020-01309-z. doi:10.1007/s10143-020-01309-z [DOI] [PubMed] [Google Scholar]
- 38.Dekutoski MB, Norvell DC, Dettori JR, Fehlings MG, Chapman JR. Surgeon perceptions and reported complications in spine surgery. Spine (Phila Pa 1976). 2010;35(9 Suppl):S9–S21. doi:10.1097/BRS.0b013e3181d830de [DOI] [PubMed] [Google Scholar]
- 39.Smith JS, Shaffrey CI, Ames CP, Lenke LG. Treatment of adult thoracolumbar spinal deformity: past, present, and future. J Neurosurg Spine. 2019;30(5):551–567. doi:10.3171/2019.1.SPINE181494 [DOI] [PubMed] [Google Scholar]
- 40.Núñez-Pereira S, Pellisé F, Vila-Casademunt A, et al. Impact of resolved early major complications on 2-year follow-up outcome following adult spinal deformity surgery. Eur Spine J. 2019;28(9):2208–2215. doi:10.1007/s00586-019-06041-x [DOI] [PubMed] [Google Scholar]