Abstract
Study Design:
A retrospective study of prospectively collected radiographic and clinical data.
Objective:
This study aims to investigate the relationship between endplate morphology parameters and the incidence of cage subsidence in patients with mini-open single-level oblique lateral lumbar interbody fusion (OLIF).
Methods:
We included 119 inpatients who underwent OLIF from February 2015 to December 2017. A total of 119 patients with single treatment level of OLIF were included. Plain anteroposterior and lateral radiograph were taken preoperatively, postoperatively, and during follow-up. The correlation between disc height, endplate concave angle/depth, cage position and cage subsidence were investigated. Functional rating index (Visual Analogue Scale for pain, and Roland Morris Disability Questionnaire) were employed to assess clinical outcomes.
Results:
Cage subsidence was more commonly seen at the superior endplates (42/119, 35.29%) than at the inferior endplates (6/119, 5.04%) (p < 0.01). More importantly, cage subsidence was significantly less in patients with superior endplates that were without concave angle (3/20, 15%) than with concave angle (37/99, 37.37%) (p < 0.05). Cage subsidence correlated negatively with preoperative anterior disc height (r = −0.21, p < 0.05), but positively with disc distraction rate (r = 0.27, p < 0.01). Lastly, the distance of cage to the anterior edges of the vertebral body showed a positive correlation (r = 0.26, p < 0.01).
Conclusions:
This study for the first time demonstrated that endplate morphology correlates with cage subsidence after OLIF. Since relatively flat endplates with smaller concave angle significantly diminish the incidence of subsidence, the morphology of cage surface should be taken into consideration when designing the next generation of cage. In addition, precise measurement of the disc height to avoid over-distraction, and more anteriorly placement of the cage is suggested to reduce subsidence.
Keywords: oblique lateral lumbar interbody fusion, lumbar fusion, cage positioning, lumbar lordosis, disc degenerative disease
Introduction
Lumbar interbody fusion with bone graft and various types of cage has been the choice of surgical treatment of degenerative lumbar spine diseases. 1 The mini-open oblique lateral lumbar interbody fusion (OLIF) technique, first reported in 2012, 2 uses a window between the lateral border of major vessels and psoas muscle to access the target disk obliquely. 3 With a small anterior-lateral skin incision, OLIF not only spares the lumbar para-spinal musculature, improves postoperative mobility, and decreases chronic muscle pain; but more importantly, OLIF employs an enlarged cage within the predominant load-bearing column of the spine to enable indirect posterior decompression of the neural elements. Thus, the impact of the degree of cage subsidence on the clinical outcome could be significantly higher in OLIF compared to other techniques with a posterior approach, in which decompression is achieved directly.
Cage subsidence often occurs as a result of axial compressive loading to the cage-endplate interface and leads to a gradual loss of disc/foraminal height, column lordosis, neuroforaminal stenosis, and recurrence of radiculopathy. Factors reported as causes of postoperative cage subsidence in various intervertebral fusions involving OLIF are reduced bone mineral density (BMD), 4 cage designs (titanium/ narrow cage),5,6 cage positions (anteriorly/ centrally positioned),7,8 endplate violation,9,10 old age, 11 dosage of bone morphogenic protein, 12 and the presence or absence of supplemental fixation.13,14 However, few reports to date have focused on the effects of pre-operative endplate morphology on the incidence of cage subsidence.
Several studies on endplate morphology15-17 indicate that the structural ductility of human vertebrae is sensitive to endplate surface topography, and that the stiffness of the endplate boundary layer and surface topography are associated with the brittleness of vertebral bodies. Furthermore, previous studies on the contact area between the cage and endplate have led to the recommendation of using larger devices to increase the interface contact, which increases the load to failure and may reduce cage subsidence in OLIF procedures. 16 However, these above studies did not devise new ways to predict cage subsidence. The purpose of current study is to determine the relationship between endplate morphology and cage subsidence uniquely in patients accepted single level OLIF procedure. Results gained from this study could help in finding a feasible method to predict cage subsidence and gathering evidence for future cage designment.
Materials and Methods
Patient Information
This retrospective review study was approved by the Institutional Review Board. The study included patients who underwent OLIF and received follow-up cares at 3 institutes (Sir RunRun Shaw Hospital, Lishui Center Hospital, Jiaxing Hospital of Zhejiang General Corps of Armed Police Forces) from February 2015 to December 2017. The total number of patients was 119, comprised of 49 male and 70 female, with a mean age of 62.35±7.79 years at the time of surgery. Preoperative diagnosis was degenerative kyphoscoliosis in 32 patients, spondylolisthesis in 37 patients, degenerative lumbar canal stenosis in 38 patients, and discogenic low back pain in 12 patients. Inclusion criteria were as follow: (1) no history of prior spinal surgery; (2) no emergency operation; (3) age above 18; (4) sufficient knowledge to complete the questionnaires; (5) indication for OLIF; and (6) absence of concomitant spinal disease. Exclusion criteria comprised of (1) previous lumbar surgery; (2) patients with isthmic spondylosethesis; (3) patients with iatrogenic endplate interruption; (3) BMD< −2.5 or a history of osteoporotic fractures; (4) indications other than OLIF; and (5) concomitant neoplastic, metabolic, or severe general/infectious disease.
OLIF Procedure
The surgical approach of OLIF procedure has been modified by our group, namely anterior-inferior psoas approach (AIP approach, manuscript accepted by Orthopaedic Surgery). Briefly, the patient was placed in the lateral decubitus position on the right side, and the central point of target IVD space was identified under fluoroscopic guidance. A transverse skin incision approximately 4 cm in length was made from the midpoint of the target IVD for single level OLIF procedure. Three muscular layers of the abdominal wall: the external oblique, the internal oblique, and the transversalis were bluntly split along the direction of muscle fibers. Then the retroperitoneal space was bluntly dissection and the peritoneum were mobilized anteriorly using retractors to expose the anterior border of the psoas. The intervertebral disc was identified by retracting the anterior border of psoas posteriorly using Cobb under direct visualization and the psoas muscle was dissected from the disc surface and retracted posteriorly. The guide pin, probe, sequential dilators, and the tube retractor were sequentially placed on the disc space vertically, and the retractor was fixated to the upper vertebral body with a pin. Discectomy was performed, endplate preparation was performed using a rasp and various curettes to remove all the cartilage and make parallel the entire disc space. A peek cage (mostly 45 mm wide, with 6° angled, Clydesdale Spinal System; Medtronic Sofamor Danek, Minneapolis, MN, UAS) filled with artificial bone (Wright, Tennessee, USA) was inserted vertically into the intervertebral space. Finally, the wound was irrigated thoroughly and conventionally closed by intradermal suture.
Radiographic Measurements
All patients were given pre- and post-operative radiologic examination, and then at 3, 6, and 12 months. Standing anteroposterior and lateral plain x-ray were taken at every follow-up. Measurements were analyzed with Image J 1.46 (National Institutes of Health, http://rsbweb.nih.gov/ij/download.html) with software for embedded region of interested. Radiographic assessment was independently performed by 2 spinal surgeons (Z.H. and D.H.) blinded to the study information. A third reviewer (Z.Z.) was available for adjudication in case of a disagreement. The endpoint of follow-up was set either at 12-month post-operation, or when a cage subsidence of more than 3 mm was identified. 18
Land markers, including the anterior (A), posterior (P), and concave apex (Ca) points of the vertebral body on the lateral view, were manually selected. The angle made by the A-Ca and Ca-P lines were considered the endplate concave angle, and a perpendicular line drawn from Ca to AP, the endplate concavity depth was deduced.19,20
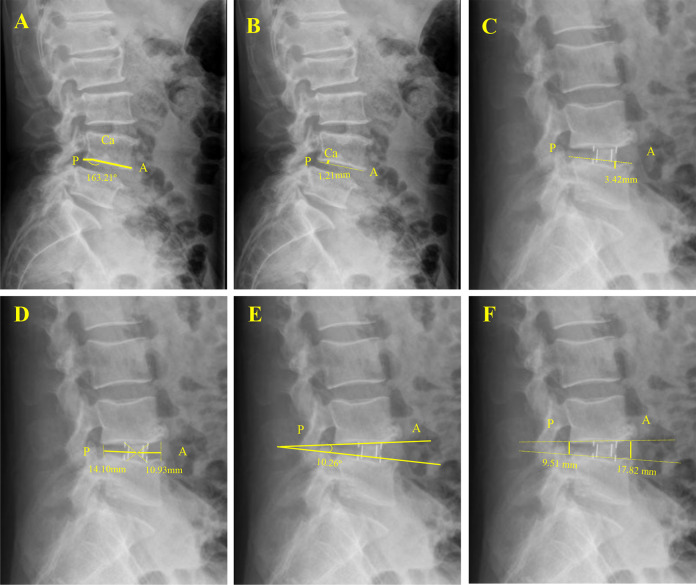
Endplate parameters were determined as follow (Figure 1):
Figure 1.
Measurement of vertebral endplate concave angle (A), vertebral endplate concave depth (B, solid line), cage subsidence (C), cage position (D, solid line), segmental lordosis (E), and disc height (F, solid line) on lateral X-ray films. Landmarks in midsagittal plane: A is anterior rim of the endplate, P is posterior rim of the endplate, Ca is endplate concave apex.
The endplate sagittal concave angle (ECA), was determined from the obtuse angle formed by the rims (A and P) of the endplate and Ca on the lateral plane; endplate concavity depth (ECD) was measured from the concavity apex (Ca) to the line connecting the anterior (A) and posterior (P) margins of the endplate;
Radiographic subsidence was measured from the vertebral endplate to the caudal or cranial margin of the cage;
Disc height at each side of the anterior/posterior border of the vertebra (DH) and segmental lordosis [SL] (angulation between the superior and inferior endplates facing each other) was measured in the lateral view;
Cage location (CL) was defined as the distance from the anterior/posterior end of endplate of the vertebral body to the center of the cage;
Clinical Assessment
For clinical outcome assessment, the Visual Analogue Scale (VAS) score was determined for back pain, along with the Roland-Morris Disability Questionnaire (RMDQ) 21 evaluation, to assess back pain and disability. Each clinical assessment was obtained before surgery and at each follow-up. Endpoint of follow-up was set as either 12 months after surgery or when a subsidence was confirmed. Patients with a significant cage subsidence (>3 mm) with or without clinical complains (recurrent pain, recurrent neurological symptoms, or a significant decline of clinical outcome) were re-evaluated for further treatment, including pedicle screw fixation and additional posterior decompression.
Statistical Analysis
Data was expressed as mean ± standard deviation (SD) for continuous variables, and number (percentage) for categorical variables. Statistical evaluation was performed with SPSS software version 20.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics (means and standard deviations) were obtained for quantitative variables. Characteristics between the groups with subsidence of cage and that without subsidence (yes or no) were compared by the 2 independent samples t-test for continuous variables, and the Fisher’s exact test for categorical variables. Pearson correlation coefficient was used to evaluate the statistical significance of possible trends (anterior/posterior disc height, lumbar lordosis, distance of cage to anterior/posterior edge with subsidence). The significance level was set at P < 0.05.
Results
Demographic Data
A total of 119 patients (49 male and 70 female), with a mean age at surgery of 62.35±7.79 years were included in the analysis, with a mean follow up of 10 ± 1.76 months. All patients underwent single level OLIF procedure, with treatment sites varied from L1 to L5. Cage subsidence were divided into superior- and inferior endplate groups. Of the 119 patients, cage subsidence occurred in 6 female patients (8.57%) of inferior endplate, 25(35.71%) female and 17(34.69%) male patients of superior endplate during postoperative follow up (Table 1). The incidence of cage subsidence in the inferior group was higher in female than in male (P < 0.05), but no significant difference was found in the superior group (P = 0.68). Cage subsidence was not associated with age (p = 0.77)
Table 1.
Patients Information.
| Patients | Total (n = 119) | Subsidence | ||
|---|---|---|---|---|
| Yes | No | P Value | ||
| Age (yrs.) | 62.35±7.79 | 59.32±9.17 | 62.93±7.41 | 0.77 |
| Inferior Endplates | ||||
| Male | 49 | 0(0%) | 49(100%) | |
| Female | 70 | 6(8.57%) | 64(91.43%) | |
| P Value | 0.04 | |||
| Superior Endplates | ||||
| Male | 49 | 17(34.69%) | 32(65.31%) | |
| Female | 70 | 25(35.71%) | 45(64.29%) | |
| P Value | 0.68 | |||
Radiological Results
The analysis of subsidence in endplates at varying treatment levels is presented in Table 2. Subsidence was more common at the superior endplate of treatment levels (42/119, 35.29%) than the inferior endplates (6/119, 5.04%) (p < 0.01). More importantly, when the endplate concave angle was 180° with a flat surface at each side of treatment levels, the incidence of cage subsidence decreased (inferior 0/20, 0%; superior 3/20, 15%), compared to that of endplate with concave angles (inferior 8/99, 8.08%; superior 37/99, 28.2%), with a significant difference in the superior endplate group (P < 0.05). The endplate concave angle (superior: r = −0.197, p < 0.05; Superior: r = −0.43, p < 0.01) negatively correlated with cage subsidence, indicating that a smaller angle increases cage subsidence risk. However, the endplate concave depth did not correlate with cage subsidence (superior: r = 0.173, p = 0.06; Superior: r = 0.149, p = 0.11) (Table 3). Furthermore, the preoperative anterior disc height negatively (r = −0.21, p < 0.05) correlated with the superior cage subsidence, while the disc distraction rate (r = 0.27, p < 0.01) (calculated by the rate of disc height pre-/post-operatively) was positively correlated. This result indicated that a lower pre-operative anterior disc height, with more post-operative disc distraction, was associated with an increase in cage subsidence. The distance of the cage to both edges of the vertebral body showed a positive correlation anteriorly with the superior endplate (r = 0.26, p < 0.01), indicating a more anteriorly positioned cage is associated with a decrease in the occurrence of superior cage subsidence. Cage subsidence neither correlated with the SL pre- or post-operatively, nor with SL correction.
Table 2.
Endplate Concave Angle and Cage Subsidence.
| Endplates | (Total n = 119) | Yes (n = ) | No (n=) |
|---|---|---|---|
| Inferior | 119 | 6(5.04%) | 113(94.96%) |
| Superior | 119 | 42(35.29%) | 77(64.71%) |
| P Value | 0.00 | ||
| Concave Angle | |||
| Inferior | |||
| =180° | 20 | 0 (6.5%) | 20 (100%) |
| <180° | 99 | 8(8.08%) | 91 (91.92%) |
| P Value | 0.22 | ||
| Superior | |||
| =180° | 20 | 3 (15%) | 17 (85%) |
| <180° | 99 | 37(37.37%) | 62 (62.63%) |
| P Value | <0.05 |
Table 3.
Correlations of Endplate Morphology Parameters and Cage Positions to Cage Subsidence.
| Values | Pearson Coefficient (r value) | ||
|---|---|---|---|
| Cage Subsidence | / | 1 | |
| Endplate concave angle | |||
| Inferior (°) | 162.25±9.73 | -0.197* | |
| Superior (°) | 164.16±13.92 | -0.43** | |
| Endplate concave Depth | |||
| Inferior (mm) | 2.61±1.80 | 0.173 | |
| Superior (mm) | 2.00±1.93 | 0.149 | |
| Anterior disc height | |||
| Superior Endplate |
Inferior Endplate |
||
| Pre-op (mm) | 10.51±3.73 | -0.48 | -0.21* |
| Distraction rate | 1.56±0.65 | -0.12 | 0.27** |
| Posterior disc height | |||
| Superior Endplate |
Inferior Endplate |
||
| Pre-op (mm) | 5.21±2.56 | 0.22 | -0.15 |
| Distraction rate | 1.61±0.94 | -0.52 | 0.26 |
| Segmental Lordosis | |||
| Superior Endplate |
Inferior Endplate |
||
| Pre-op (°) | 7.72±4.39 | -0.74 | -0.76 |
| Correction rate | 2.06±2.31 | 0.42 | -0.32 |
| Distance to Anterior (mm) | 15.61±7.60 | 0.10 | 0.26** |
| Distance to Posterior (mm) | 14.88±0.60 | 0.71 | 0.14 |
*:P < 0.05; **:P < 0.01.
Clinical Outcomes
Among the 119 patients, 48 were confirmed to have cage subsidence, and pedicle screw fixation with/without posterior decompression was considered only for patients who were symptomatic (including recurrent or newly onset low back pain or radiculopathy). All patients claimed satisfactory symptom relief at the end of their follow-up. Clinical outcomes were measured by both VAS and RMDQ scores. Overall, patients showed a statistically significant improvement in both their VAS score and RMDQ score postoperatively (p < 0.01, Table 4). Interestingly, clinical outcome was not significantly affected by the occurrence of cage subsidence.
Table 4.
Clinical Outcomes.
| Subsidence | |||
|---|---|---|---|
| Yes | No | p Value | |
| VAS | |||
| Pre-op | 60.79±8.38 | 62.75±9.98 | 0.19 |
| Final follow-up | 18.16±6.28 | 18.75±7.30 | 0.36 |
| p Value | 0.00 | 0.00 | |
| RMDQ | |||
| Pre-op | 16.95±1.54 | 17.64±1.51 | 0.08 |
| Final follow-up | 5.47±1.93 | 5.12±1.97 | 0.47 |
| p Value | 0.00 | 0.00 | |
Discussion
The primary objective of this study was to determine the correlation of endplate morphology with cage subsidence in patients that underwent OLIF. This study found that patients with a concaved endplate were more vulnerable to cage subsidence, when compare to patients with a flat endplate.
The minimally invasive OLIF through a retroperitoneal anterior-inferior psoas (AIP) approach is a safe and effective alternative to anterior, lateral, or posterior approaches for lumbar fusion. Advantages of the OLIF22,23 include indirect neurological decompression with a less invasive approach, minimal blood loss, shorter operation times, less wound issues, placement of a larger cage, and earlier patient mobilization. In addition, normal stabilizing ligaments and psoas are not sacrificed or interrupted compared to other interbody techniques. In OLIF, larger cages are used that span across the vertebral ring apophysis, and this has been reported to increase load tolerance for failure and mitigate endplate violation. However, cage subsidence after OLIF is still frequently seen.
Subsidence is defined as the sinking of an object with a greater elasticity modulus (e.g., cage or spacer) into an object with a lower elasticity modulus (e.g., vertebral body).24,25 In our study, cage subsidence was diagnosed if the cage sank into the adjacent vertebral body by 3 mm or more. 18 Causes of subsidence are multifactorial, which could be related to the surgical technique, implant material/morphology, endplate preparation and bone quality of patients. 26 Among these factors, endplate morphology is one of the most concerning.
Various reports indicate that cage migration is affected by endplate morphology, size, shape, and elasticity modulus.2,7,8,27-29 Increasing mismatch angle between implant and vertebral endplate is an important factor leading to cage subsidence. 29 Consequently, the incidence of subsidence in the clinical setting could be reduced by ensuring that both the prosthetic and bony endplates are well apposed at the end of surgery. 29 Grant JP et al. 30 suggested an important role for surface nonuniformities of the endplate in the failure of a vertebrae, but without giving a clear relationship between the 2. Our current data showed a significantly lower cage subsidence rate on endplates without any concavity (angle = 180°), especially at the superior side. We believe a “flat endplate” will have better interface contact with an OLIF cage with surface that were currently used by us. This is because a well-matched endplate-cage surface lead to more even distribution of stress and a larger area of endplate coverage, which result in a reduction in cage subsidence. Hasegawa et al. 5 also demonstrated that a larger area of endplate coverage improved resistance to subsidence. On the other hand, a concaved endplate (angle <180°) or irregularly shaped endplate reduces the contact area between the cage and the endplate surface. The smaller the surface contact area, the higher the stress on the endplate, and hence more cage subsidence. 2 Meanwhile, endplate concave angle negatively correlated with cage subsidence, indicating a magnitude dependent manner of endplate morphology to cage subsidence. This was confirmed by a positive correlation between the endplate concave depth and cage subsidence, though not statistically significant (Table 3).
Another controversial issue concerning cage subsidence is the cage position. In general, lumbar posterior endplate regions are stronger than anterior ones. Anatomical studies also have shown that the density and thickness of the vertebral endplate increase toward the periphery. A biomechanical study demonstrated that a dorso-lateral placement of interbody cages in combination with a pedicle screw system results in a 20% higher failure loads than a central cage placement. 8 However, in our OLIF patients with the AIP approach, it was more difficult to place the cage as posteriorly as it could be achieved via a posterior approach. Our data showed that the distance of the cage to the anterior edge of the vertebral body positively correlated to cage subsidence. In other words, a more anteriorly placed cage will decrease the occurrence of cage subsidence. With the center of the endplate being the weakest region in lumbar endplates, both the density and thickness of the endplate have been shown to increase toward the periphery. 9 We suggested that the anterior region is also ideal for cage placement, and surgeons could place interbody devices anteriorly to achieve stronger interface properties.
It has been well accepted that anterior placement of large OLIF cage resulted in better correction of LL, while posterior placement may produce more satisfactory indirect decompression. Even though the increased cage lordotic angle seen in anterior placement may provide better stability and reduce the risk of cage damage, in vitro biomechanical analysis indicated it may increase the risk of subsidence.27,28 Here we investigated if the correction of LL by anterior cage placement influences the occurrence of cage subsidence in our OLIF patients. Our results showed that neither pre-/post-operative LL, nor LL correction influenced the cage subsidence in our patient’s series (Table 3).
Over-distraction is another important factor for subsidence, it was reported that disk space distraction could result in cage subsidence in anterior cervical and lumbar fusion cases.1,31,32 However, to the best of our knowledge, few researches have demonstrated this phenomenon in the lumbar region. Our data demonstrated a significantly positive correlation between disc distraction and cage subsidence. This was further confirmed by the data that the pre-operative anterior disc height negatively correlated to cage subsidence. These results suggested that attention should be paid to avoid over-distracting the disc space in OLIF patients, and an obvious loss of pre-operative disc height should be taken into consideration.
In our current study of 119 patients, cage subsidence was diagnosed in 42 (35.3%) cases with superior endplates, and in only 6 (5.0%) cases with inferior endplates. In other words, the superior endplate was more vulnerable to cage subsidence when comparing to its inferior counterpart. Our result is similar to previous reports that topographical parameters of the superior endplate, rather than the inferior endplate, have a significant association with stiffness, strength, or ductility parameters. 20 The inferior endplates have been reported to be stronger and thicker than the superior endplates in lumbar discs. 30 Interestingly, no subsidence on both ends of endplates was found in our case series. We believe this is because of an initial subsidence either end will release the stress at the endplate-cage interface and preclude subsidence at the opposite end.
Our study suffered from several potential limitations. First, this was a retrospective study with a relatively limited cohort that might be insufficiently powered to detect statistical differences between subgroups. Second, the study did not assess the bone mineral density, which is important but has been well-investigated in previous studies. Finally, patients were not stratified into specific subgroups according to the target lumbar disks, which may reveal vertebral-specific outcomes. Future studies are required to address these concerns.
Conclusion
Our study for the first time demonstrated that OLIF patients with a flat endplate showed less cage subsidence than patients with a concaved endplate. Our results strongly suggested that more emphasis should be placed on endplate preparation and cage placement in patients with a concaved endplate. Moreover, the morphology of convex surface should be taken into consideration when designing the new generation of cage. Due to the limitation of an AIP approach, it is difficult to place the cage onto the strongest posterior region. Thus, anterior placement of cage could be an ideal alternative in OLIF procedure.
Footnotes
Availability of Data and Material: The datasets generated and/or analyzed during the current study are available.
Consent for Publication: The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This article does not contain any studies with human participants or animals performed by any of the authors. The Institutional ethical board of this university has reviewed and approved this study.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shunwu Fan, MD  https://orcid.org/0000-0001-5853-0678
https://orcid.org/0000-0001-5853-0678
References
- 1.Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abbushi A, Cabraja M, Thomale UW, Woiciechowsky C, Kroppenstedt SN. The influence of cage positioning and cage type on cage migration and fusion rates in patients with monosegmental posterior lumbar interbody fusion and posterior fixation. Eur Spine J. 2009;18(11):1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jin J, Ryu KS, Hur JW, Seong JH, Kim JS, Cho HJ. Comparative study of the difference of perioperative complication and radiologic results: MIS-DLIF (minimally invasive direct lateral lumbar interbody fusion) versus MIS-OLIF (minimally invasive oblique lateral lumbar interbody fusion). Clin Spine Surg. 2018;31(1):31–36. [DOI] [PubMed] [Google Scholar]
- 4.Oh KW, Lee JH, Lee JH, Lee DY, Shim HJ. The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg. 2017;30(6):E683–e689. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa K, Abe M, Washio T, Hara T. An experimental study on the interface strength between titanium mesh cage and vertebra in reference to vertebral bone mineral density. Spine (Phila Pa 1976). 2001;26(8):957–963. [DOI] [PubMed] [Google Scholar]
- 6.Lee JH, Jeon DW, Lee SJ, Chang BS, Lee CK. Fusion rates and subsidence of morselized local bone grafted in titanium cages in posterior lumbar interbody fusion using quantitative three-dimensional computed tomography scans. Spine (Phila Pa 1976). 2010;35(15):1460–1465. [DOI] [PubMed] [Google Scholar]
- 7.Briski DC, Goel VK, Waddell BS, et al. Does spanning a lateral lumbar interbody cage across the vertebral ring apophysis increase loads required for failure and mitigate endplate violation. Spine (Phila Pa 1976). 2017;42(20):E1158–e1164. [DOI] [PubMed] [Google Scholar]
- 8.Labrom RD, Tan JS, Reilly CW, Tredwell SJ, Fisher CG, Oxland TR. The effect of interbody cage positioning on lumbosacral vertebral endplate failure in compression. Spine (Phila Pa 1976). 2005;30(19):E556–561. [DOI] [PubMed] [Google Scholar]
- 9.Hou Y, Yuan W, Kang J, Liu Y. Influences of endplate removal and bone mineral density on the biomechanical properties of lumbar spine. PLoS One. 2013;8(11):e76843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tatsumi R, Lee YP, Khajavi K, Taylor W, Chen F, Bae H. In vitro comparison of endplate preparation between four mini-open interbody fusion approaches. Eur Spine J. 2015;24(suppl 3):372–377. [DOI] [PubMed] [Google Scholar]
- 11.Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 2006;88(12):2714–2720. [DOI] [PubMed] [Google Scholar]
- 12.Vaidya R, Weir R, Sethi A, Meisterling S, Hakeos W, Wybo CD. Interbody fusion with allograft and rhBMP-2 leads to consistent fusion but early subsidence. J Bone Joint Surg Br. 2007;89(3):342–345. [DOI] [PubMed] [Google Scholar]
- 13.Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003;12(5):513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. ScientificWorldJournal. 2012;2012:456346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grosland NM, Goel VK. Vertebral endplate morphology follows bone remodeling principles. Spine (Phila Pa 1976). 2007;32(23):E667–673. [DOI] [PubMed] [Google Scholar]
- 16.Nekkanty S, Yerramshetty J, Kim DG, et al. Stiffness of the endplate boundary layer and endplate surface topography are associated with brittleness of human whole vertebral bodies. Bone. 2010;47(4):783–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satake K, Kanemura T, Yamaguchi H, Segi N, Ouchida J. Predisposing factors for intraoperative endplate injury of extreme lateral interbody fusion. Asian Spine J. 2016;10(5):907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He W, He D, Sun Y, et al. Standalone oblique lateral interbody fusion vs. combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet Disord. 2020;21(1):184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen H, Zhong J, Tan J, Wu D, Jiang D. Sagittal geometry of the middle and lower cervical endplates. Eur Spine J. 2013;22(7):1570–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duran S, Cavusoglu M, Hatipoglu HG, Sozmen Ciliz D, Sakman B. Association between measures of vertebral endplate morphology and lumbar intervertebral disc degeneration. Can Assoc Radiol J. 2017;68(2):210–216. [DOI] [PubMed] [Google Scholar]
- 21.Fan S, Hu Z, Hong H, Zhao F. Cross-cultural adaptation and validation of simplified Chinese version of the Roland-Morris Disability Questionnaire. Spine (Phila Pa 1976). 2012;37(10):875–880. [DOI] [PubMed] [Google Scholar]
- 22.Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A. The Oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. 2016;474(9):2020–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 2012;6(2):89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hakalo J, Wronski J, Ciupik L.[Subsidence and its effect on the anterior plate stabilization in the course of cervical spondylodesis. Part I: definition and review of literature]. Neurol Neurochir Pol. 2003;37(4):903–915. [PubMed] [Google Scholar]
- 25.Kao TH, Wu CH, Chou YC, Chen HT, Chen WH, Tsou HK. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg. 2014;134(10):1343–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Le TV, Baaj AA, Dakwar E, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37(14):1268–1273. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Z, Fogel GR, Liao Z, Sun Y, Liu W. Biomechanical analysis of lumbar interbody fusion cages with various lordotic angles: a finite element study. Comput Methods Biomech Biomed Engin. 2018;21(3):247–254. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Z, Fogel GR, Liao Z, Sun Y, Sun X, Liu W. Biomechanical evaluation of four surgical scenarios of lumbar fusion with hyperlordotic interbody cage: a finite element study. Biomed Mater Eng. 2018;29(4):485–497. [DOI] [PubMed] [Google Scholar]
- 29.Mohammad-Shahi MH, Nikolaou VS, Giannitsios D, Ouellet J, Jarzem PF. The effect of angular mismatch between vertebral endplate and vertebral body replacement endplate on implant subsidence. J Spinal Disord Tech. 2013;26(5):268–273. [DOI] [PubMed] [Google Scholar]
- 30.Grant JP, Oxland TR, Dvorak MF. Mapping the structural properties of the lumbosacral vertebral endplates. Spine (Phila Pa 1976). 2001;26(8):889–896. [DOI] [PubMed] [Google Scholar]
- 31.Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN. Effects of disc height and distractive forces on graft compression in an anterior cervical discectomy model. Spine (Phila Pa 1976). 2002;27(22):2441–2445. [DOI] [PubMed] [Google Scholar]
- 32.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3(1):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]