Abstract
Background
To achieve patient-centric quality care in neuro-oncology, all aspects of the disease and its impact on quality survival need to be considered. This includes the psychological consequences of a brain tumor diagnosis and subsequent life-altering experiences. Far too often the voice of our patients is unheard. Empowering patients to advocate for their own psychological needs is essential.
Methods
Data were derived from four focus groups with adult patients with brain tumors (N = 15; Mage = 46 years, 53% female). A trained moderator led each 90-min group and posed semi-structured questions regarding patients’ care needs throughout their neuro-oncological disease trajectory. Emphasis was placed on the quality of life and distress reduction. Common themes were identified via thematic content analysis using NVivo software. A high inter-rater reliability (Mkappa = 0.92, range = 0.85–0.93) was achieved. Two themes are presented here: Emotional Response to Stressors and Existential Considerations.
Results
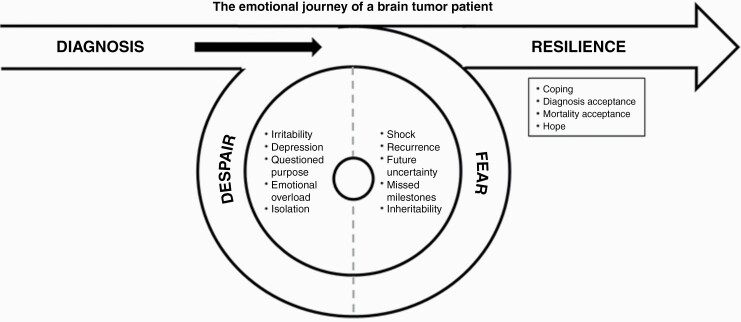
Of the two themes presented, 14 codes emerged. Codes were classified into three broad categories: Fear, Despair, and Resilience. The frequency of each category ranged from 31.4% to 34.7%. Example quotes and a discussion of each category follows.
Conclusions
It is imperative that we include the patient perspective in the development of neuro-oncology programs, thereby considering the quality of survival in addition to quantity. Neuro-oncology quality care must be driven by our patients' experiences and should integrate support for emotional distress while promoting resilience throughout this life-threatening illness.
Keywords: brain tumor, despair, fear, resilience, quality of life
A brain tumor diagnosis immediately changes one’s life. Too often, neuro-oncology programs focus solely on tumor stabilization and management of neurologic and physical effects, neglecting the emotional and behavioral consequences of a brain tumor diagnosis and subsequent life-altering experiences for both the patient and their loved ones. To achieve true patient-centric care in neuro-oncology, we must take into consideration all aspects of the disease and its impact on quality survival.
The literature documents high rates of both psychological and cancer-related distress in those diagnosed with brain tumors,1–6 and while the quantitative research assessing emotional impact is growing, the voice of our patients is often lost in scientific definitions or clinical conceptualizations. In a recent investigation exploring quality care in neuro-oncology, focus groups were used to provide a platform for brain tumor patients to describe their neuro-oncology journey, engage in interactive conversations, and speak openly about their quality care needs throughout the disease trajectory.7 The research team identified six essential themes from patient discussions, including two themes that were psychological in nature: Emotional Response to Stressors and Existential Concerns. These findings emphasized the pervasiveness of emotional distress in neuro-oncology and reiterated the importance of psychological support throughout the disease. The present paper explores these themes in greater detail in order to shed light on the specific psychological concerns impacting patients during this life-altering disease.
Methods
Participants were recruited from an NCI-designated cancer center in January of 2021. Eligibility requirements include: (1) primary brain tumor diagnosis (any grade) confirmed by medical records; (2) age ≥18 years; (3) telehealth capability with reliable internet access; (4) surgical treatment ≥2 weeks; and (5) no indication of major cognitive impairment (Telephone Interview for Cognitive Status [TICS]8; score >21 required). Participants were all aware of their brain tumor diagnosis, but did not need to indicate awareness of prognosis to participate. Four focus groups were held via a secure telehealth platform from February to April 2021. The moderator (ARL), a clinical neuropsychologist, conducted the focus groups (90-min each) using semi-structured interview questions to guide the discussion. The semi-structured interview format allowed for the use of probes to explore participant responses while maintaining consistency across groups. Following each group discussion, participants completed online self-report psychological questionnaires using a secure online data collection system (REDCap).9 Participants were compensated $40 for their completion of the focus group and the online questionnaires. Approval for this study was obtained from the ethics committee of Virginia Commonwealth University and Massey Cancer Center (HM20020548).
All study staff (neuropsychologists, clinical psychology graduate trainees, and medical students) had been exposed to qualitative research methods and/or the outlined steps for thematic content analysis by Braun and Clarke.10 Focus group recordings were transcribed and uploaded to NVivo software.11 Using the codebook created by the study team, each transcript was coded by two study staff. For consistency and content integrity, the moderator (ARL) coded all four group transcripts. All code allocations were reviewed for agreement across transcripts, and identified discrepancies were resolved between coders through discussion to ensure reliability. Text was recoded if consensus determined appropriate. Inter-rater reliability was excellent across all four focus groups (MKappa = 0.92, range = 0.85–0.93). Frequencies and means for demographic data, medical variables, and self-reported distress measures were obtained using SPSS v27 to describe participants and contextualize their responses.12 Detailed methodology including recruitment, procedures, and analysis for this study is reported elsewhere.7 In-depth analyses of themes specific to the patient’s emotional journey are presented here (ie, Emotional Response to Stressors and Existential Concerns).
Results
Participants
For this study, 20 patients with brain tumors showed initial interest to participate, 18 agreed to screening, and 17 met eligibility criteria. A total sample of 15 patients consented and participated in the focus groups. Most participants were female (53%), White (93%), middle-aged (Mage = 45 years; range = 18–76), married (67%), and college-educated (60%). Cognitive capacity was evenly distributed between those with intact cognition (47%) and those with mild impairments (53%). Most participants had private insurance (80%), and all had access to a primary care provider (100%). There was a relatively even distribution of diagnoses: glioblastoma (33%), astrocytoma (27%), and oligodendroglioma (33%). Most participants had high-grade tumors (73%) located in the right hemisphere (67%) and frontal lobe (67%). All participants had undergone surgical intervention, 80% received radiation therapy, and 87% received chemotherapy treatment. Average time since diagnosis was 44 months (range = 5–178), with 53% being within the first 2 years of diagnosis. Four participants had a history of progression (27%) at the time of enrollment. Overall, the sample had mild depression, mild generalized anxiety, moderate death anxiety, and moderate fear of cancer recurrence. The full demographic, tumor-related, and distress profiles of the sample are reported elsewhere.7
Thematic Content Analysis Findings
Fourteen codes within the Emotional Response to Stressors and the Existential Concerns themes emerged. Average kappa for these two themes was 0.95 (range = 0.85–1.00). Codes were classified into three broad categories: Fear (33.9% of coded content; initial shock, tumor recurrence, future uncertainty, missed milestones, and inheritability; Table 1), Despair (34.7% of coded content; irritability, depression, questioned purpose, emotional overload, and isolation; Table 2), and Resilience (31.4% of coded content; coping, diagnosis acceptance, acceptance of mortality, and hope; Table 3).
Table 1.
Fear direct quote sampling
| Initial Shock | “I think especially with the shock of the diagnosis, just trying to figure out… You sit here with this friggin’ book saying make your decision. You can choose your surgery, you can choose your blah blah blah. It is just…wait a second, your life has just changed.”(52-year-old female; astrocytoma) “After my initial shock, I was fine. And then I got a new surgery and a new shock.”(42-year-old male; glioblastoma) |
| Tumor Recurrence | “It would be nice if I had support on the days of my MRI, regardless of the result, because I don’t get the results that day. But it’s just the anticipation of going in for something that I know could go poorly or not…That day where I know I’m not going to find the answer that day, and I’m just waiting.”(27-year-old female; glioblastoma) “At first, I was frightened. Any time I got a little headache, I was like oh my God, it’s back. It’s back…But you can’t live thinking like that all the time.”(39-year-old female; oligodendroglioma) |
| Future Uncertainty | “People could tell you, okay, you have twelve months to live and then you could go on living five plus years, more. So, it’s kind of like against the odds, against the statistics and the findings and all these things, anything could happen.”(27-year-old female; glioblastoma) “And that’s average. Some people are less, some people are more. When you hear that, you’re thinking, am I going to be more or am I going to be less?”(39-year-old female; oligodendroglioma) |
| Missed Milestones | “The thing that worries me the most is, how long can I stick around to help raise my kids? What are those milestones that I’m going to miss out on? Or, you know, maybe I don’t get to see everything.”(39-year-old male; oligodendroglioma) “I want to see my grandbabies graduate from high school, graduate from college if they go to college, get married and have their first- I want to be a great-grandmother. I don’t know if I’ll live that long and that does scare me.”(54-year-old female; oligodendroglioma) |
| Inheritability | “But my biggest fear then was ‘Is it hereditary?’ Something I can pass to my children, to my siblings, to their children? That was my biggest fear. Not for myself. Whatever is in store for me is in store for me. But I was so afraid somebody else could get it.”(43-year-old female; oligodendroglioma) “Maybe there is something genetic about this. We just don’t know yet. That’s certainly one of the most worrisome things for me is, can I pass this down?”(39-year-old male; oligodendroglioma) |
Table 2.
Despair direct quote sampling
| Irritability | “I have a problem with remembering certain words…I’ll get frustrated because I don’t remember a simple word that I should know. I get frustrated and I get angry…and I just feel like I’m stupid.”(48-year-old female; astrocytoma) “I don’t have the patience anymore, with this disease or whatever… One frustrating thing in my life is family members…They’ve said, 'Mom, you’ve changed…you don’t have patience anymore.' And I say, 'Yeah, I probably have changed.'(54-year-old female; oligodendroglioma) |
| Depression | “I thought there was a good chance, if I did live through the surgery, that I might become a vegetable, which was terrifying, or I might die. It was so depressing.” (39-year-old female; oligodendroglioma) “I lost my independence. I lost my will to finish school. At one point, I lost my will to even live. I just didn’t care. I lost my friends and my daughter moved in and I’m no longer independent, I have to rely on somebody to do just about anything… So, it’s not normal.”(48-year-old female; astrocytoma) |
| Questioned Purpose | “But now it’s so disappointing just to stop my life. It’s like alright, what do I do now? I took a drawing class at the museum and I’m trying to work with some nonprofits to help them. But to find some reason for purpose is hard.”(56-year-old male; glioblastoma) “It was like the end of the world as I knew it, as it was. I was twenty-four years old. I was like, what is there now?”(39-year-old female; oligodendroglioma) |
| Emotional Overload | “I have a similar issue with noise. Sound can really set me off. Not all the time, but sometimes if I go to a place, there’s a bunch of kids running around just everywhere. I just got to go to a room and close the door and just be by myself.”(56-year-old male; glioblastoma) “For me, I’ve been struggling with anxiety. It’s just the ruminating thoughts in your head over and over again.”(27-year-old female; glioblastoma) |
| Isolation | “There’s a whole group of people that I haven’t told because I didn’t want to deal with the sympathy, and I didn’t want to have to explain to people.”(76-year-old male; glioblastoma) “Honestly, I need more support than I did, and that is a lot more difficult. It’s taken me two years of therapy to get to the point of being able to say that and ask for help.”(39-year-old male; astrocytoma) |
Table 3.
Resilience direct quote sampling
| Coping | “It’s even just little things, walking my dog around the neighborhood, little moments of joy… I want to go look at the moon. Go water these plants and look at the moon, relax myself and enjoy this moment. And I did. And it was really, really nice.”(39-year-old male; astrocytoma) “Coping with today, the here and now, not coming up with some plan for a ‘new normal’ bullshit.”(39-year-old female; oligodendroglioma) “So, my mindset has always been 'I’m living life large' and I call it L3- living life large.”(54-year-old female; oligodendroglioma) |
| Diagnosis Acceptance | “[It’s not] going to be normal again. And I’m fine with that. Honestly, at this point, I embrace it. This is who I am. I’m okay. I’m okay with this. This is part of my story.”(39-year-old male; astrocytoma) “The main thing that I notice on a regular basis is loss of words. My vocabulary has gotten bad. I have much better memory about things longer ago than I do about recent things. And it doesn’t really bother me because, you know, it’s just part of the game.”(76-year-old male; glioblastoma) |
| Acceptance of Mortality | “That’s what all the sudden the future was. I was still thinking about the future, but it wasn’t hope or life. It was death and finality and how to make it easier for my daughter when I pass. Whether it be two or five years.” (48-year-old female; astrocytoma) “I think [end-of-life] has to be discussed. Right now, we’re going through setting up the will. We’re putting our affairs in order… We’ll be done with it and then we can go on with our happy lives.”(42-year-old male; glioblastoma) |
| Hope | “How do you define hope? It’s important to think positively and hope for the best despite the odds… It would be hard getting through each day if you didn’t think that way.”(27-year-old female; glioblastoma) “Hope is key.”(42-year-old male; glioblastoma) |
Fear
Most participants reported shock upon learning of their diagnosis. Many discussed the rapid onset of their disease—from symptom exposure (eg, seizure and debilitating headache), to hospitalization and neuroimaging, to neurosurgery and pathological diagnosis confirming a brain tumor—all taking place within a few days. Participants struggled to comprehend the reality of their diagnosis and the instantaneous life detour resulting thereafter, creating a sense of impending doom. Following slight adjustments as time passed, participants discussed the effect of prognosis uncertainty and the fear of the tumor progressing, an omnipresent concern, never fully allowing them to put the diagnosis behind them. Participants also spoke of the recurring threatening anticipation surrounding their neuroimaging days (eg, scanxiety) and a newfound hypervigilance of any symptoms that may signal progression (eg, headache). Participants also conversed about their struggles with uncertainty. For example, many discussed their challenges with statistical prognoses (ie, mean overall survival), understanding their tumor would eventually recur, just not knowing when or what their future may hold. This distress related to uncertainty is in constant battle with their desire for optimism. Participants discussed trying to maintain hope that they will beat the odds, exceed the average, and live out their previously identified life goals; however, while participants acknowledged medical literacy as important, some explained that becoming knowledgeable of brain tumor statistics put an end to their future directives and dreams. Instead of their own potential, many began to think of their eventual (early) demise and the lives of their loved ones without them. There was commonality in the fear of missing future milestones—such as graduations, weddings, and births. Many questioned if their illness would prevent them from personal accomplishments (eg, having children and finding a life partner) or being present for upcoming family occasions (eg, dancing with their son on their his wedding day, taking a trip with their grandchildren). Finally, some expressed concerns of this disease being genetic, eventually impacting their offspring (ie, inheritability).
Despair
Irritability was the most common emotional response discussed among focus groups. Participants described becoming easily frustrated and having a newly present “short fuse.” This was particularly apparent when discussing posttreatment cognitive changes; participants expressed ongoing aggravation with their anomic aphasia, immediate memory loss, and distractibility. Irritability is presented as both external (eg, yelling or verbally blaming others) and internal expressions (eg, becoming frustrated with oneself, feeling stupid). Symptoms of depression were also a highly prevalent conversation topic. Participants discussed sadness about their diagnosis and the possibility of a shortened lifespan. They described being distressed about their loss of independence and the subsequent burden on their caregivers, with some even noting a fluctuating will to live. A shared theme among participants was the challenge of redirecting goals and finding purpose following diagnosis. Participants described feeling as though their life was stopped instantaneously, such that they began to question their meaning in life and contribution to society. Many discussed their difficulties with adjustment—an emotional milestone never fully achieved. Additionally, participants reiterated the feeling of being emotionally overloaded; overwhelmed by others’ sympathy or pity, overloaded by sensory stimuli, and especially inundated with the high frequency of medical appointments now consuming their daily calendars. For some participants, these various feelings of grief and despair led to isolation. Participants described withholding information about their diagnosis or prognosis, refusing support—especially from those who were identified as acquaintances prior to diagnosis—and having difficulty acknowledging how or when to ask for help after pushing those who offered initial support away.
Resilience
Nevertheless, participants also discussed their coping strategies, including living in the present moment, despite the aforementioned distress.While participants acknowledged the importance of planning for the future, many discussed focusing on the present as a way to mitigate the overwhelming nature of this life-threatening illness. The use of spirituality throughout their journey was also common; participants noted incorporating daily devotionals into their routine, joining faith-based community groups, and having belief in a higher power or that there is a purpose to this illness. Beyond focusing on the present moment, there were underlying messages of acceptance across group members. Participants openly discussed how they would not allow the diagnosis to define their life story, but, instead, accept that the diagnosis would be interwoven throughout their next chapters. An important component of acceptance was accepting one’s own mortality, and patients described coming to the realization that an early demise was likely in the concluding paragraph. Often this acceptance of mortality was demonstrated by a willingness to plan and discuss end-of-life matters, sorting out their affairs before it was too late. Throughout the focus group discussions, participants laughed together, they cried together, and they discussed that while life-changing and distressing, the overall effects of their brain tumor were manageable. They were survivors. They shared stories of strength, of persistence, of encouragement—a few even shared mantras with the group as a mark of legacy to one another. Their determination to continue fighting was strong. In this way, each group concluded with messages of hope: Hope for strength, hope for one another, and hope for an eventual cure.
Discussion
The goal of this qualitative study was to elucidate quality care directions for future comprehensive neuro-oncology programs. This study extends the previously identified themes,7 with an opportunity of providing a platform for our brain tumor patients to describe their psychological journey in relation to their Emotional Response to Stressors and Existential Concerns. Participants’ responses suggest that brain tumor patients experience three broad psychological categories: Fear, Despair, and Resilience (Figure 1). For many, the response of fear immediately followed diagnosis, trailed shortly behind by thoughts and feelings of despair. Nevertheless, patterns of resilience are shown throughout. Most importantly, these experiences appear to be nonlinear and very personal, with many describing a cyclic journey with no set time course for their distress patterns. In order to ensure quality patient-centric neuro-oncology care, comprehensive programs must integrate support for emotional distress and promote adjustment and resilience throughout this life-threatening illness for both the patient and their loved ones. Current neuro-oncology programming needs to be improved. Recommendations based on patients' distress descriptions are provided below.
Fig. 1.
The emotional journey of a brain tumor patient.
Discussion of Themes
Fear
Participants in the focus group endorsed feeling fearful about their present (eg, shock of diagnosis and current scans) and future (eg, tumor progression and uncertainty). Moreover, their fears extended to include the ones they love most (eg, missed milestones and inheritability). These types of fears may be classified as existential in nature, such that they are related to a loss of meaning, fear of burdening others, and potential suffering and death.13 Recent quantitative literature in neuro-oncology similarly depicts this identified theme of Fear: Patients with brain tumors consistently report significant rates of generalized anxiety, death anxiety, and fear of cancer recurrence.4,5,14 The corroboration of patient-described and investigator-measured distress in the form of Fear provides an even stronger call for treatment in this population.
Future neuro-oncology programming may consider a multifaceted approach for treating this type of distress. For generalized symptoms of anxiety, including shock and routine scanxiety, patients with brain tumors may benefit from concrete, cognitive-behavioral strategies (eg, relaxation training and cognitive restructuring).15 However, for the progression-related fears or fears of uncertainty, more specialized psychotherapies have been developed and may be better indicated.16 Notable interventions include Fear of Recurrence Therapy (FORT)17 and Conquer Fear,18 which go above and beyond basic cognitive-behavioral strategies and utilize attention training, mindfulness, metacognitive therapy, values clarification, existentialism, and psycho-education to address patients’ fears of recurrence. However, it is important to note that neither of these treatments has included patients with brain tumors, a population that might have a nuanced experience of fear of recurrence given the dismal prognostics and neurologic triggers of distress. Therefore, an investigation of the fear of recurrence treatment in neuro-oncology is warranted.
Finally, patients’ fears related to their loved ones, including possible missed milestones and questions of inheritability, may be best discussed as a family or dyad. One existential intervention, which addresses concerns related to the patient’s future and legacy, may be particularly well-suited to tackle these types of patient concerns. Managing Cancer and Living Meaningfully (CALM) was designed to include the patient’s loved ones19 and has been shown to be feasible, acceptable, and preliminarily effective in reducing death anxiety in patients with brain tumors.20 Overall, in order to discern which treatment is most appropriate, routine distress screening and patient preferences will need to be incorporated into future neuro-oncology programming to effectively manage the variety of patients’ experienced fears.
Despair
In addition to the fears and anxieties that plague patients with brain tumors, participants’ conversations also reflected an underlying sense of despair which manifests in various ways. For some, this grief and despair take the forms of irritability, a lack of patience, frustration with physical and cognitive changes, and emotional overload. Others may internalize their despair, experience depressive symptoms, grieve a loss of purpose, and isolate themselves from others—even their loved ones. Previous research has also identified similar aspects of despair. Increased irritability has been noted across cancer diagnoses, with patients with frontal lobe tumors particularly susceptible to personality changes and loss of emotional control.21 Moreover, an estimated 15%–20% of glioma patients are thought to develop major depressive symptoms within eight months after diagnosis,22 with higher rates of clinical diagnosis than other oncology populations.23,24
Neuro-oncology programs should frequently assess for increased irritability, depression, and suicidality to ensure that supportive services are offered as appropriate. The Depression subscale of the Hospital Anxiety and Depression scale and the Patient Health Questionnaire-9 have both been validated for use as screening tools for patients with brain tumors.25 The patient may desire pharmacologic treatment for their emotional distress. Retrospective studies indicated that selective serotonin inhibitors (SSRIs) do not adversely affect survival for patients with glioblastoma26; however, potential adverse drug interactions and increased seizure activity while taking antidepressants have yet to be systematically explored in this population.21
Psychotherapeutic interventions should also be implemented within neuro-oncology programs. As previously mentioned, Managing Cancer and Leaving Meaningfully (CALM) addresses patients’ existential concerns and changes in relationships with themselves and others.19 CALM has been shown to successfully decrease depressive symptoms in a mixed-cancer sample27 and more recently, in a small sample of primary brain tumor patients.20 Additionally, Making Sense of a Brain Tumor (MSoBT) is a psychosocial intervention that combines cognitive rehabilitation, neuropsychological feedback, and psychotherapy—has been found to lead to decreased depressive symptoms both during treatment and at a 6-month follow-up.28 Although irritability has not yet been assessed as a particular outcome of this intervention, cognitive rehabilitation strategies may help patients feel more empowered and less overwhelmed by their cognitive deficits, as posttreatment cognitive changes were the leading frustration described by our focus group participants.
Resilience
Throughout each focus group, participants shared messages of incredible resilience, coping, acceptance, and hope. Prior research suggests that resilience and effective coping skills are associated with increased quality of life and decreased distress from uncertainty among patients with brain tumors.29 Participants in our groups reported several active problem-focused coping strategies, including planning for end-of-life and finding new activities to foster a sense of purpose. Mindfulness-based interventions have also been shown to foster problem-focused coping and reduce stress in cancer patients;30 the participants similarly echoed the importance of being mindful, living in the present moment, and taking pleasure in small milestones or gains. Spirituality has been quantitatively associated with greater quality of life in brain tumor patients, and several participants used prayer and belief in a higher power as a means of accepting their diagnosis.31
In addition to addressing symptoms of emotional distress (eg, fear and despair), psychosocial interventions should foster patients’ resilience and encourage positive coping. In a review of positive psychology interventions for patients with breast cancer, five major types of interventions were found: mindfulness-based therapies, meaning-making interventions, written expression of positive emotions, psycho-spiritual interventions, and hope interventions.32 These interventions were associated with improved quality of life and well-being and might be worth exploring as part of future neuro-oncology care.32 Meaning-making, hope, and other positive components are also integrated within CALM19 and MSoBT;28 however, further research is needed to understand how the positive aspects of these therapies specifically impact patients with brain tumors.
Strengths and Limitations
The focus group format of the current study afforded a unique opportunity to explore the emotional journey of a brain tumor diagnosis in the patient's own words. Moreover, their level of reported emotional distress (mild-to-moderate) mirrors previous findings in neuro-oncology, suggesting a generalizable sample.5 However, the voice of those of minority status, particularly regarding racial identity, was underrepresented in this sample. It is important to note that cultural differences have been found regarding cancer-related emotional reactions,33 and thus, the emotional reactions described above may manifest differently in more diverse samples. Future research will need to actively include voices of the underserved, who have worse outcomes given systematic disparities in care.34 Additionally, the voice of brain tumor caregivers needs equal representation in neuro-oncology comprehensive care programming, as we know this disease affects not only the patient, but those who love them as well. Psychological impact of the disease is strongly influenced by several patient-related and disease-related factors, including patient coping style, stage of disease, recurrence, and treatments. These variables need continued investigation. Additional strengths and limitations of the present study are reported elsewhere.7
Conclusion
This study examined two themes identified by brain tumor patients as important components to quality care: Emotional Reaction to Stressors and Existential Concerns. Three categories within these two themes emerged: Fear, Despair, and Resilience. Participants shared their present and current anxieties in addition to their external and internal grief. Importantly, through the burden of these described distress experiences, a shared theme of resilience held strong. Future neuro-oncology programming should consider a multifaceted approach for treating the aforementioned emotional distress of brain tumor patients. To achieve this, psychotherapeutic interventions must stop purposely excluding those diagnosed with brain tumors35 and begin ensuring intervention suitability for this vulnerable population. Moreover, future research should take a closer look at those that express resilience over time in order to discern factors that foster adjustment. Our patients have made it clear: Quality, patient-centric neuro-oncology care includes comprehensive programs that integrate support for emotional distress and promote adjustment and resilience throughout this life-threatening illness. Current neuro-oncology programming needs to be improved.
Acknowledgments
Thank you to our patients who shared their voices on quality care in neuro-oncology.
Contributor Information
Ashlee R Loughan, School of Medicine, Virginia Commonwealth University, Richmond, Virginia, USA; Massey Cancer Center, Richmond, Virginia, USA.
Morgan Reid, Department of Psychology, Virginia Commonwealth University, Richmond, Virginia, USA.
Kelcie D Willis, Massey Cancer Center, Richmond, Virginia, USA; Department of Psychology, Virginia Commonwealth University, Richmond, Virginia, USA.
Sarah Barrett, School of Medicine, Virginia Commonwealth University, Richmond, Virginia, USA.
Karen Lo, School of Medicine, Virginia Commonwealth University, Richmond, Virginia, USA.
Funding
Supported by Massey Cancer Center – Cancer Prevention and Control Research Accelerator Monies.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Ethics Approval
Approval was obtained from the ethics committee of Virginia Commonwealth University and Massey Cancer Center (HM20020548). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1. Fox SW, Lyon D, Farace E. Symptom clusters in patients with high-grade glioma. J Nurs Scholarsh. 2007;39(1):61–67. [DOI] [PubMed] [Google Scholar]
- 2. Litofsky NS, Farace E, Anderson F, et al. . Depression in patients with high-grade glioma: results of the glioma outcomes project. Neurosurgery. 2004;54(2):358–66; discussion 366. [DOI] [PubMed] [Google Scholar]
- 3. Kilbride L, Smith G, Grant R. The frequency and cause of anxiety and depression amongst patients with malignant brain tumours between surgery and radiotherapy. J Neurooncol. 2007;84(3):297–304. [DOI] [PubMed] [Google Scholar]
- 4. Loughan AR, Aslanzadeh FJ, Brechbiel J, et al. . Death-related distress in adult primary brain tumor patients. Neurooncol Pract. 2020;7(5):498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Loughan AR, Husain M, Ravyts SG, et al. . Death anxiety in patients with primary brain tumor: Measurement, prevalence, and determinants. Palliat Support Care. 2021;19(6):672–680. [DOI] [PubMed] [Google Scholar]
- 6. Braun S, Aslanzadeh FJ, Thacker L, Loughan A. Examining fear of cancer recurrence in primary brain tumor patients and their caregivers using the actor-partner interdependence model. Psycho‐Oncology. 2021;30:1120–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Loughan AR, Reid M, Willis KD, et al. . The burden of a brain tumor: guiding patient centric care in neuro-oncology. J Neurooncol. 2022;1(3):1–12. [DOI] [PubMed] [Google Scholar]
- 8. Fong TG, Fearing MA, Jones RND, et al. . The telephone interview for cognitive status: creating a crosswalk with the mini-mental state exam. Alzheimers Dement. 2009;5(6):492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 11. QSR International Pty Ltd. NVivo. 2020. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home [Google Scholar]
- 12. IBM Corp. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. 2020. [Google Scholar]
- 13. An E, Lo C, Hales S, Zimmermann C, Rodin G. Demoralization and death anxiety in advanced cancer. Psychooncology. 2018;27(11):2566–2572. [DOI] [PubMed] [Google Scholar]
- 14. Braun SE, Aslanzadeh FJ, Thacker L, Loughan AR. Examining fear of cancer recurrence in primary brain tumor patients and their caregivers using the Actor-Partner Interdependence Model. Psychooncology. 2021;30(7):1120–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Greer JA, Park ER, Prigerson HG, Safren SA. Tailoring cognitive-behavioral therapy to treat anxiety comorbid with advanced cancer. J Cogn Psychother. 2010;24(4):294–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Butow PN, Turner J, Gilchrist J, et al. . Randomized trial of ConquerFear: a novel, theoretically based psychosocial intervention for fear of cancer recurrence. J Clin Oncol. 2017;35(36):4066–4077. [DOI] [PubMed] [Google Scholar]
- 17. Maheu C, Lebel S, Courbasson C, et al. . Protocol of a randomized controlled trial of the fear of recurrence therapy (FORT) intervention for women with breast or gynecological cancer. BMC Cancer. 2016;16(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Butow PN, Bell ML, Smith AB, et al. . Conquer fear: protocol of a randomised controlled trial of a psychological intervention to reduce fear of cancer recurrence. BMC Cancer. 2013;13(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodin G, Lo C, Rydall A, et al. . Managing cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018;36(23):2422–2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Loughan AR, Willis KD, Braun SE, et al. . Managing cancer and living meaningfully (CALM) in adults with malignant glioma: a proof-of-concept phase IIa trial. J Neurooncol. 2022;157:447–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Boele FW, Rooney AG, Grant R, Klein M. Psychiatric symptoms in glioma patients: from diagnosis to management. Neuropsychiatr Dis Treat. 2015;11:1413–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rooney AG, Carson A, Grant R. Depression in cerebral glioma patients: a systematic review of observational studies. J Natl Cancer Inst. 2011;103(1):61–76. [DOI] [PubMed] [Google Scholar]
- 23. Arnold SD, Forman LM, Brigidi BD, et al. . Evaluation and characterization of generalized anxiety and depression in patients with primary brain tumors. Neuro Oncol. 2008;10(2):171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Linden W, Vodermaier A, MacKenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141(2-3):343–351. [DOI] [PubMed] [Google Scholar]
- 25. Pranckeviciene A, Bunevicius A. Depression screening in patients with brain tumors: a review. CNS Oncol. 2015;4(2):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Caudill JS, Brown PD, Cerhan JH, Rummans TA. Selective serotonin reuptake inhibitors, glioblastoma multiforme, and impact on toxicities and overall survival: the mayo clinic experience. Am J Clin Oncol. 2011;34(4):385–387. [DOI] [PubMed] [Google Scholar]
- 27. Lo C, Hales S, Jung J, et al. . Managing cancer and living meaningfully (CALM): phase 2 trial of a brief individual psychotherapy for patients with advanced cancer. Palliat Med. 2014;28(3):234–242. [DOI] [PubMed] [Google Scholar]
- 28. Ownsworth T, Chambers S, Damborg E, et al. . Evaluation of the making sense of brain tumor program: a randomized controlled trial of a home-based psychosocial intervention. Psychooncology. 2015;24(5):540–547. [DOI] [PubMed] [Google Scholar]
- 29. Pan CJ, Liu HC, Liang SY, et al. . Resilience and coping strategies influencing the quality of life in patients with brain tumor. Clin Nurs Res. 2019;28(1):107–124. [DOI] [PubMed] [Google Scholar]
- 30. Mehta R, Sharma K, Potters L, Wernicke AG, Parashar B. Evidence for the role of mindfulness in cancer: benefits and techniques. Cureus. 2019;11(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Randazzo DM, McSherry F, Herndon JE, et al. . Spiritual well-being and its association with health-related quality of life in primary brain tumor patients. Neurooncol Pract. 2021;8(3):299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Casellas-Grau A, Font A, Vives J. Positive psychology interventions in breast cancer. A systematic review. Psychooncology. 2014;23(1):9–19. [DOI] [PubMed] [Google Scholar]
- 33. Zhang AY, Gary F, Zhu H. Exploration of depressive symptoms in African American cancer patients. J Ment Health. 2015;24(6):351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. National Brain Tumor Society. Quick Brain Tumor Facts. https://braintumor.org/brain-tumor-information/brain-tumor-facts/. Published 2022. Accessed March 16, 2022. [Google Scholar]
- 35. Loughan AR, Lanoye A, Aslanzadeh FJ, et al. . Fear of cancer recurrence and death anxiety: unaddressed concerns for adult neuro-oncology patients. J Clin Psychol Med Settings. 2021;28(1):16–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.