In this journal, the reports of Li et al.1 and Zhou et al.2 attract our attention and interest, which demonstrated that the Coronavirus disease 2019 (COVID-19) pandemic has an impact on the Haemophilus influenzae and Streptococcus pneumoniae infection in children. However, no data was available regarding the changes of Mycoplasma pneumoniae (M. pneumoniae) prevalence in children before and after COVID-19 pandemic in Henan, China.
M. pneumoniae is a bacterium that can cause illness by damaging the lining of the respiratory system.3 M. pneumoniae infection is one of the most common causes of community acquired pneumonia (CAP) in children. Up to 10% of M. pneumoniae-infected children developed pneumonia.4 M. pneumoniae was mainly transmitted by respiratory droplets formed by people infected with M. pneumoniae infection when they coughed or sneezed. COVID-19 is a highly infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that may result in life-threatening complications.5 To prevent the spread of SARS-CoV-2, strict intervention measures were implemented, such as wearing masks, keeping social distance, limiting crowd gathering and restricting outdoor activities. Theses control measures may also have an impact on the spread of M. pneumoniae in children. Analyzing the local data of children with M. pneumoniae infection before and after the COVID-19 pandemic can provide evidence-based strategies for the prevention of M. pneumoniae infection in children.
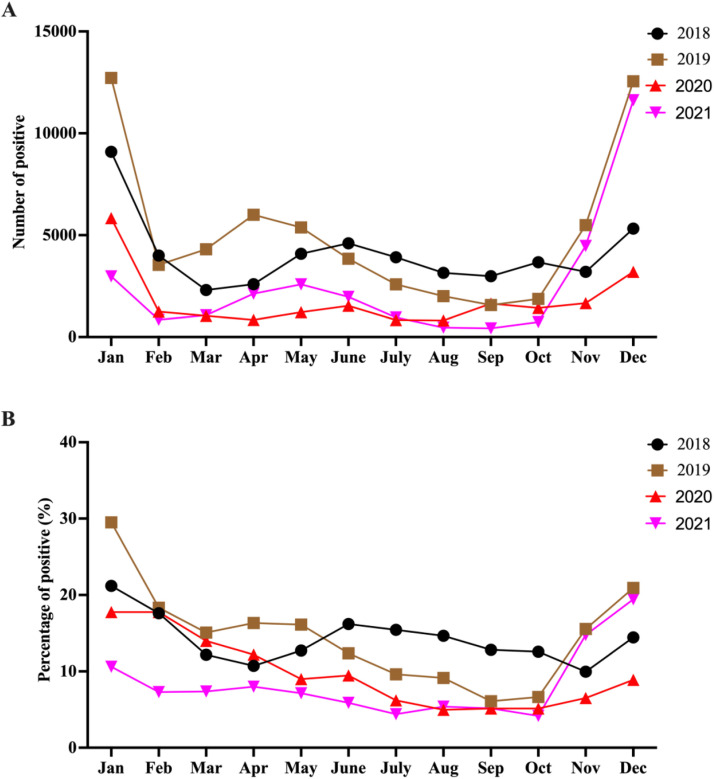
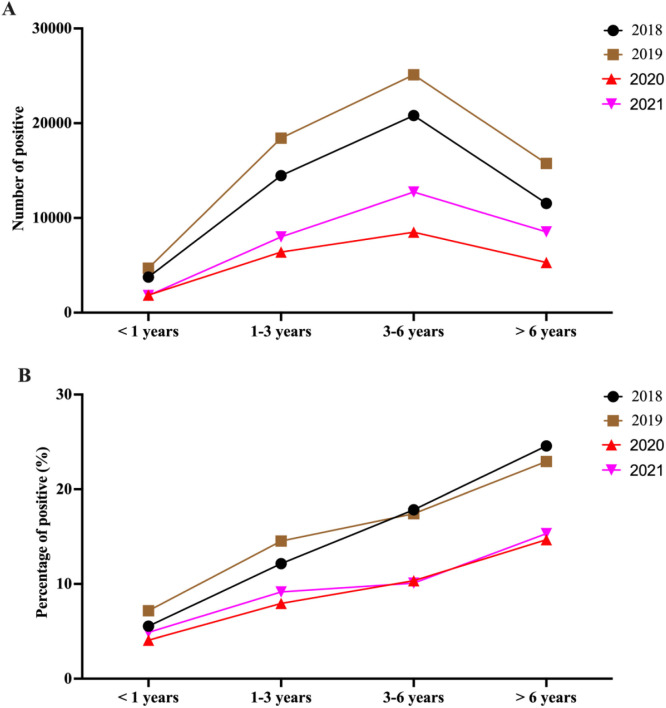
Therefore, we conducted a retrospective study to investigate the changes of M. pneumoniae prevalence in children before and after COVID-19 pandemic in Henan, China. A total of 1,259,697 children aged 1days to 18 years who came to Henan Children's Hospital (Zhengzhou, China) for M. pneumoniae IgM testing from 2018 to 2021 were enrolled in this study. As shown in Fig. 1 , the positive number and rate of children with M. pneumoniae infection decreased in 2020 and 2021, compared with the same period in 2018 and 2019 (Except that in November and December 2020). Our data also showed that the peak of M. pneumoniae infection occurred in January and December. Meanwhile, we further divided the children into four groups according to age (0-1years, 1-3years, 3-6 years and > 6 years). As shown in Fig. 2 , the positive number and rate of children infected with M. pneumoniae in all age groups decreased in 2020 and 2021, compared with that in 2018 and 2019. The number of children aged 3-6 years with M. pneumoniae infection is the largest. Of note, the positive rate of children infected with M. pneumoniae infection increased with age.
Fig. 1.
The positive number and rate of M. pneumoniae infection in children from 2018 to 2021.
Fig. 2.
The number of positive and positive rates of M. pneumoniae infection in children by age group from 2018 to 2021.
In conclusion, our data showed that COVID-19, as well as well as its prevention and control measures, decreased the positive number and rate of children with M. pneumoniae infection in 2020 and 2021. Maintaining effective and continuous surveillance is very important for the prevention of M. pneumoniae infection in children aged > 3 years, especially in December and January.
This study had several strengths. First, it is a large study with more than 1 million children undergoing M. pneumoniae IgM testing, reporting 162,338 children with M. pneumoniae infection. Second, children aged 1 day to 18 years old were enrolled in this study. This study also has a few limitations. First, this was a cross-sectional study, and we did not track the future clinical outcomes. Second, this was a single-center study conducted in Henan, China. The results may differ in other regions.
Declaration of Competing Interest
The authors declare no conflict of interests.
References
- 1.Li Y, Guo Y, Duan Y. Changes in streptococcus pneumoniae infection in children before and after the COVID-19 pandemic in Zhengzhou, China. J Infect. 2022;85(3):e80–e81. doi: 10.1016/j.jinf.2022.05.040. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou J, Zhao P, Nie M, Gao K, Yang J, Sun J. Changes of Haemophilus influenzae infection in children before and after the COVID-19 pandemic, Henan, China. J Infect. 2022 doi: 10.1016/j.jinf.2022.10.019. Oct 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang Z, Li S, Zhu C, Zhou R, Leung PHM. Mycoplasma pneumoniae infections: pathogenesis and vaccine development. Pathogens. 2021;10(2) doi: 10.3390/pathogens10020119. Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krafft C, Christy C. Mycoplasma pneumonia in children and adolescents. Pediatr Rev. 2020;41(1):12–19. doi: 10.1542/pir.2018-0016. Jan. [DOI] [PubMed] [Google Scholar]
- 5.Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020;41(12):1100–1115. doi: 10.1016/j.it.2020.10.004. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]