Abstract
The emergence of the COVID-19 pandemic necessitated rapid expansion of telehealth as part of healthcare delivery. This study compared HIV-related no-shows by visit type (in-person; video; telephone) during the COVID-19 pandemic (April 2020–September 2021) from the Data for Care Alabama project. Using all primary care provider visits, each visit’s outcome was categorized as no-show or arrived. A logistic regression model using generalized estimating equations accounting for repeat measures in individuals and within sites calculated odds ratios (OR) and their accompanying 95% confidence interval (CI) for no-shows by visit modality. The multivariable models adjusted for sociodemographic factors. In-person versus telephone visits [OR (95% CI) 1.64 (1.48–1.82)] and in-person versus video visits [OR (95% CI) 1.53 (1.25–1.85)] had higher odds of being a no-show. In-person versus telephone and video no-shows were significantly higher. This may suggest success of telehealth visits as a method for HIV care delivery even beyond COVID-19.
Keywords: HIV, Telehealth, No shows, Visit modality, Retention in care
Introduction
The World Health Organization declared COVID-19 a global pandemic on Mar 11, 2020 [1]. This unforeseen onset of the COVID-19 pandemic necessitated rapid expansion of telehealth as part of healthcare delivery. While telehealth was offered as one option in some healthcare delivery systems prior to the COVID-19 pandemic, others relied mostly or only on face-to-face communication [2, 3]. The onset of the COVID-19 pandemic, therefore, put an added burden on these facilities by causing them to shift all or most of their face-to-face appointments to telehealth [4, 5]. This rapid transition in the way healthcare was delivered was not only an extensive adjustment for the clinic but also for the physicians and patients.
Previous studies assessing retention in HIV care among different visit modalities during COVID-19 have shown mixed results. While some studies have shown better retention in care outcomes with telehealth visits compared with in-person visits [5–7], others have shown in-person visits to have better retention in care outcomes versus telehealth [4]. Additionally, since most facilities serving PWH transitioned almost fully to telehealth after the emergence of the COVID-19 pandemic, many studies assessing retention in care outcomes by visit modality (i.e., in-person or telehealth) used the pre-COVID period as the reference and as a substitute for in-person visits. Moreover, most studies compared retention in care between in-person and telehealth visits without distinguishing between video and telephone visits. Additionally, most previously conducted studies looking at the association between visit modality and HIV retention in care during the COVID-19 pandemic were conducted in areas other than the Southern US, which left a gap in the literature assessing this relationship among PWH living the Southern US, an area disproportionally impacted by the HIV epidemic [8]. Moreover, comparing the information and communication technologies, such as internet, computers, cellphones, and fixed-line telephones, most of the Southern states have shown to have the lowest technology access as compared to the rest of the US [9].
This mixed evidence on the association between visit modality and retention in HIV care during the COVID-19 pandemic, the dearth of literature distinguishing between video and telephone visits, and the lack of findings from the Southern US highlight the importance of conducting additional studies looking at this relationship. Therefore, the objective of this study was to assess HIV primary care appointment no-shows by three visit modalities (in-person, video, and telephone) during the early COVID era (Apr20–Sep21). This study used a longitudinal multi-site data sample from PWH in Alabama, one of the Southern states with low technology access. Although, a recent study conducted in Birmingham, Alabama, found a large proportion of PWH owning a smartphone [10], these results may not be generalizable state-wide as 82% of the countries in Alabama are considered rural [11], which may face the challenges associated with mobile reception and internet connectivity. Currently, there are six recommended methods to measure HIV retention in care, but only no-shows have shown to be independently associated with all-cause mortality [12–14]. Lastly, to assess the difference in the likelihood of having a no-show among sociodemographic groups for each visit modality, we also assessed the association between sociodemographics with no-shows for in-person, video, and telephone visits.
Methods
A retrospective cohort study design used all scheduled primary care provider (PCP) visits (arrived and no-shows) between April 1, 2020 to September 30, 2021 from the Data for Care-Alabama (D4C) project [15]. The PCP visits did not include urgent care visits. D4C is a consortium of seven HIV care facilities across the State of Alabama, which include the University of Alabama at Birmingham (UAB) 1917 Clinic (Birmingham), UAB Family Clinic (Birmingham), Health Services Center (Anniston), Thrive Alabama (Huntsville), Medical Advocacy and Outreach (Montgomery), University of South Alabama (Mobile), and Unity Wellness Center (Opelika). All sites have been routinely reporting client-level data for D4C since 2019 on sociodemographics, HIV viral loads, CD4 counts, and scheduled HIV-related PCP appointments. To be eligible for this study, individuals that had at least one scheduled PCP visit with data on visit modality associated with that visit were included. Since one site did not report visit modality, data from only six sites was included for this analysis. One site offered telehealth prior to the onset of the COVID-19 pandemic.
Visit Scheduling Practices Around the Onset of the COVID-19 Pandemic
After the onset of the COVID-19 pandemic, although most visits were shifted to telehealth, in-person visits (42% of our study sample in Q2 2020) were still reserved for some PWH (new patients, those with complicated medical history, those without reliable access to phone/cellular/internet, and those who preferred in-person visits). Additionally, the move to telehealth was quickly reversed as most individuals returned to in-person visits (72% to 98% from Q3 2020 to Q3 2021) even in the pre-vaccine era. While visit modality was not captured prior to April 2020, visit modality was routinely recorded in the scheduling system from April 1st, 2020. Incase visit modality was changed (ex. video to telephone or in-person to video), this information was updated in the scheduling system. Most commonly, video calls transitioned to telephone calls in real-time due to technological barriers. In-person visits were rescheduled to video visits mostly in advance and individuals were contacted prior to the visit ensuring comfortability with a telehealth visit and availability of internet. While video calls were the preferred telehealth method by providers for replacing in-person visits, telephone calls were carried out if the individuals preferred telephone over video call or lacked access to internet.
Outcome, Exposure, and Covariate/Confounder Variables
The outcome variable, no-show, for each visit was categorized as a dichotomous variable. The exposure variable, visit modality, was categorized as in-person, video, and telephone visits. A set of covariates were included: Age and annual income were included as continuous variables, whereas self-reported gender was categorized as male, female, and transgender, which included male-to-female, female-to-male, unspecified transgender; self-reported race/ethnicity was categorized as White, Black, Asians, Native Hawaiians/Pacific Islanders, American Indians or Alaska Natives, and mixed race. Due to small proportions all races other than white and Black, they were categorized together as “Other”; self-reported housing status was categorized as stable/permanent temporary (example, staying at a friend’s or relative’s place), and unstable (example, eviction or foreclosure). Due to their small numbers, temporary and unstable housing were grouped together; self-reported HIV risk factor, which includes all potential transmission risks was categorized as men who have sex with men (MSM), heterosexual contact, injection drug use (IDU), hemophilia/coagulation disorder, receipt of blood transfusion, blood components or tissue, perinatal transmission, and MSM/IDU. Due to small proportions, all HIV risk factors other than MSM and heterosexual contact, they were categorized together as “Other”; and pre-COVID-19 telehealth site indicator, which indicated if a site offered telehealth prior the COVID-19 pandemic.
Statistical Analysis
Descriptive statistics were calculated for individuals having 0 and ≥ 1 no-show during the total study period with the covariates/confounders. Frequencies and proportions were calculated for categorical variables, and median and interquartile range were calculated for continuous variables. For the multivariable analysis, crude odds ratios (OR), adjusted OR (AOR), and their accompanying 95% confidence intervals (CI) were calculated with logistic regression models using generalized estimating equations accounting for repeat measures in individuals and within sites. First, the overall no-shows were calculated for video and telephone visits using in-person visits as reference; comparison between telephone and video visits was also made. Next, no-shows by visit modality were calculated for the study period divided into six quarters [Q2 2020 (Apr 1–Jun 30), Q3 2020 (Jul 1–Sep 30), Q4 2020 (Oct 1–Dec 31), Q1 2021 (Jan 1–Mar 31), Q2 2021 (Apr 1–Jun 30), Q3 2021 (Jul 1–Sep 30)] to assess trends over time for the association. In addition, no-shows for the three visit modalities were compared among the six quarters keeping Q2 2020 (beginning of the pandemic) as reference. Lastly, to compare the association between sociodemographics and no-shows for each visit modality, three separate models were set (one for each visit modality) to assess the relationship between the sociodemographics and no-shows. All adjusted models were controlled for the covariates/confounders and site. All analyses were carried in SAS 9.4. [16].
Results
A total of 7712 individuals had ≥ 1 scheduled PCP visits with information on visit modality. After excluding individuals with missing data on age (n = 182), gender (n = 57), race/ethnicity (n = 46), housing status (n = 243), income (n = 144), and HIV risk factor (n = 179), 6861 unique individuals were included. The study population was predominantly Black (68.4%) and male (69.7%) with a median age of 45 years. Overall, 57.4% individuals had 0 no-shows, and 42.7% had ≥ 1 no-show during the study period. The bivariate analysis showed that individuals that had ≥ 1 no-show during the study period were more likely to be younger, Black, have lower median annual income, and have temporary/unstable housing (Table 1). The range of no-shows among individuals with ≥ 1 no-show was one to 12 for in-person, one to six for video visits, and one to seven for telephone visits.
Table 1.
Descriptive characteristics of the study population at baseline (n = 6861)
| Variables | % | 0 No-shows 3935 (57.4%) |
≥ 1 No-shows 2926 (42.7%) |
|---|---|---|---|
| Age | – | 49 (36, 58) | 41 (31, 52) |
| Income‡ | – | 1928 (600, 10,908) | 1017 (9, 9528) |
| Gender† | |||
| Men | 69.7 | 2742 (69.7) | 2043 (69.8) |
| Women | 29.6 | 1173 (29.8) | 855 (29.2) |
| Transgender | 0.7 | 20 (0.5) | 28 (1.0) |
| Race/ethnicity† | |||
| White | 29.4 | 1326 (33.7) | 688 (23.5) |
| Black | 68.4 | 2508 (63.7) | 2188 (74.8) |
| Other | 2.2 | 101 (2.6) | 50 (1.7) |
| Housing status† | |||
| Permanent/stable | 93.7 | 3780 (96.1) | 2648 (90.5) |
| Temporary/unstable | 6.3 | 155 (3.9) | 278 (9.5) |
| HIV risk factor† | |||
| MSM | 49.3 | 1958 (49.8) | 1421 (48.6) |
| Heterosexual | 45.5 | 1796 (45.6) | 1324 (45.3) |
| Other | 5.3 | 181 (4.6) | 181 (6.2) |
| Site | |||
| 1 | 47.7 | 1995 (50.7) | 1278 (43.7) |
| 2 | 3.6 | 124 (3.2) | 126 (4.3) |
| 3 | 13.7 | 631 (16.0) | 311 (10.6) |
| 4 | – | ||
| 5 | 25.8 | 925 (23.5) | 843 (28.8) |
| 6 | 2.9 | 113 (2.9) | 85 (2.9) |
| 7 | 6.3 | 147 (3.7) | 283 (9.7) |
‡Median (interquartile range); †N (%)
p-value were calculated using Cochran-Mantel–Haenszel test for categorical and Kruskal–Wallis test for continuous variables
Transgender includes individuals transgender, transgender male-to-female, and transgender female-to-male
Other race includes Asian, Native Hawaiian/Pacific Islander, American Indian or Alaska Native, and Other (including mixed race)
Other risk factor includes Injection drug use (IDU), hemophilia/coagulation disorder, receipt of blood transfusion, blood components, or tissue, perinatal transmission, and MSM/IDU
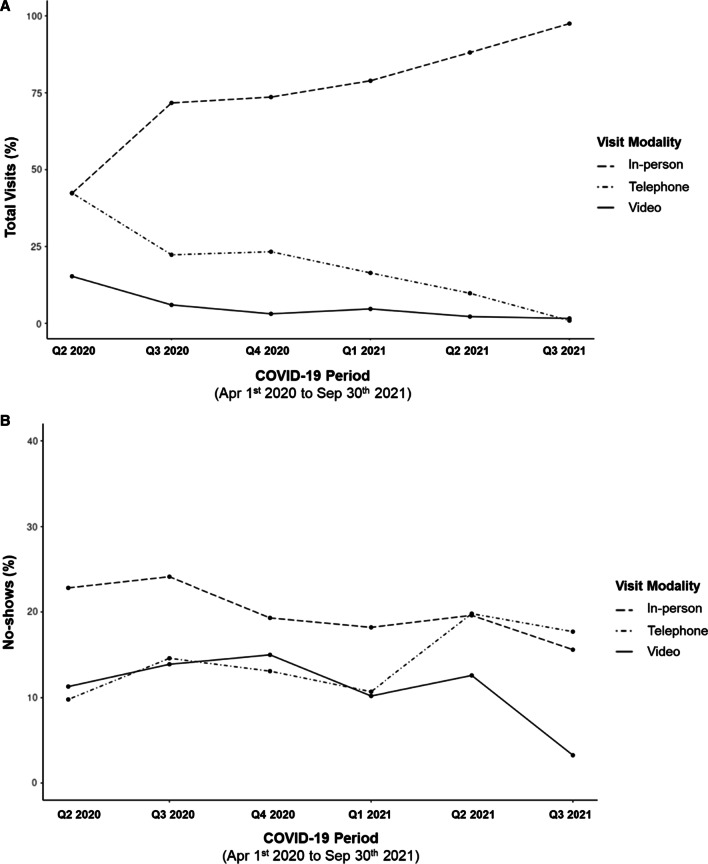
A total of 27,969 visits were included during the study period (arrived: 81.7%; no-show: 18.3%). Of the total visits, 73.6% were in-person, 5.4% were video, and 21.0% were telephone visits, and their overall no-show rates were 20.4%, 12.2%, and 12.6%, respectively. Figure 1A depicts the change in the proportion of scheduled PCP visits for in-person, video, and telephone visits modality during the study period divided into six aforementioned quarters and showed that, at the beginning of the study, most visits were conducted using telehealth (Video: 15.3%; Telephone: 42.4%); however, the proportion of in-person visits and telephone visits were almost identical (43.3% vs. 42.4%). Telehealth visits were steadily replaced by in-person visits from 42.3% in Q2 2020 to 81.7% in Q3 2021. This was accompanied by a decrease in telephone and video visits, from 42.4% and 15.3% in Q2 2020 to only 16.1% and 2.3% in Q3 2021, respectively. Figure 1B shows the change in the proportion of no-shows by visit modality for the study period divided into six quarters and showed that the no-show rates were consistently highest for in-person visits compared to telehealth visits (video and telephone). The no-show rates for video visits were comparable to that of telephone visits for the majority of the study period.
Fig. 1.
A Trends over time for proportion of scheduled visits by visit modality. B Trends over time for proportion of no-shows by visit modality
The multivariable analysis showed that compared to in-person visits, telephone visits had 39% lower odds [AOR (95% CI) 0.61 (0.55, 0.68)] of being a no-show, whereas video visits had 34% lower odds [AOR (95% CI) 0.66 (0.54, 0.80)] of being a no-show (Table 2); no differences were observed between video and telephone visits. Table 3 shows the association between visit modality and no-shows for each of the six quarters and mirrors the trends seen in Fig. 1B where, compared to in-person visits, telephone visits had significantly lower odds of being a no-show throughout the study period with the exception of Q2 2021; the difference in the odds of no-show for in-person versus telephone visits was the highest at the beginning of the study and decreased as the study progressed. Moreover, compared to video visits, in-person visits had lower odds of being a no-show in only Q2 2020, Q3 2020, and Q1 2021. Lastly, the odds of being a no-show for video visits and telephone visits were similar throughout the study period.
Table 2.
Comparison of No-Show by Visit Modality (In-person vs. Video and Telephone & Video vs. Telephone) During COVID-19 (April 1, 2020 to September 31, 2021)
| Visit type | Odds of no-shows versus 0 no-shows | |||
|---|---|---|---|---|
| Video and telephone versus in-person | Video versus telephone | |||
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.61 (0.52, 0.71) | 0.66 (0.54, 0.80) | 1.07 (0.89, 1.27) | 1.08 (0.87, 1.33) |
| Telephone | 0.57 (0.52, 0.63) | 0.61 (0.55, 0.68) | Reference | Reference |
| In-person | Reference | Reference | – | – |
aLogistic regression model using generalized estimating equations accounting for repeat measures in individuals and within sites
bAdjusted for age, race/ethnicity, gender, income, housing status, HIV risk factor, and pre-COVID-19 telehealth site indicator
cBold denotes statistical significance (p < 0.05)
Table 3.
Comparison of no-show visit modality (in-person vs. video and telephone and video vs. telephone) during COVID-19 by Quarter (April 1, 2020 to September 31, 2021)
| Visit type | Video and telephone versus in-person | Video versus telephone | ||
|---|---|---|---|---|
| Q2 2020 (Apr 1 to Jun 30) | ||||
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.48 (0.37, 0.62) | 0.47 (0.36, 0.61) | 1.26 (0.95, 1.68) | 1.23 (0.92, 1.64) |
| Telephone | 0.38 (0.31, 0.46) | 0.38 (0.31, 0.47) | Reference | Reference |
| In-person | Reference | Reference | – | – |
| Q3 2020 (Jul 1 to Sep 30) | ||||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.58 (0.41, 0.82) | 0.60 (0.42, 0.85) | 1.11 (0.76, 1.63) | 1.10 (0.74, 1.64) |
| Telephone | 0.53 (0.43, 0.65) | 0.54 (0.43, 0.68) | Reference | Reference |
| In-person | Reference | Reference | – | – |
| Q4 2020 (Oct 1 to Dec 31) | ||||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.89 (0.55, 1.45) | 0.95 (0.58, 1.56) | 1.37 (0.82, 2.30) | 1.44 (0.85, 2.45) |
| Telephone | 0.65 (0.52, 0.80) | 0.66 (0.53, 0.82) | Reference | Reference |
| In-person | Reference | Reference | – | – |
| Q1 2021 (Jan 1 to Mar 31) | ||||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.56 (0.37, 0.82) | 0.55 (0.36, 0.82) | 1.07 (0.69, 1.67) | 1.08 (0.68, 1.70) |
| Telephone | 0.52 (0.41, 0.65) | 0.51 (0.40, 0.65) | Reference | Reference |
| In-person | Reference | Reference | – | – |
| Q2 2021 (Apr 1 to Jun 30) | ||||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.65 (0.38, 1.09) | 0.65 (0.38, 1.12) | 0.57 (0.33, 1.01) | 0.59 (0.33, 1.04) |
| Telephone | 1.12 (0.81, 1.41) | 1.11 (0.87, 1.41) | Reference | Reference |
| In-person | Reference | Reference | – | – |
| Q3 2021 (Jul 1 to Sep 30h) | ||||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Video | 0.76 (0.47, 1.23) | 0.84 (0.50, 1.41) | 1.17 (0.70, 1.94) | 1.25 (0.73, 2.15) |
| Telephone | 0.66 (0.53, 0.81) | 0.67 (0.53, 0.83) | Reference | Reference |
| In-person | Reference | Reference | – | – |
aLogistic regression model using generalized estimating equations accounting for repeat measures in individuals and within sites
bAdjusted for age, race/ethnicity, gender, income, housing status, HIV risk factor, and pre-COVID-19 telehealth site indicator
cBold denotes statistical significance (p < 0.05)
When comparing the no-shows for each visit modality among the six quarters (Table 4), the findings for in-person visits showed that, compared to Q2 2020, no-shows were similar in Q3 2020 but were significantly lower in Q4 2020, Q1 2021, and Q2 2021; no difference in no-shows was observed between Q2 2020 and Q3 2021. For video visits, no differences in no-shows were observed in Q3 2020, Q4 2020, Q1 2021, Q2 2021, and Q3 2021 when compared with Q2 2020. For telephone visits, compared to Q2 2020, no-shows were higher in Q3 2020, Q4, 2020, Q2 2021, and Q3 2021; no difference in no-shows was observed between Q2 2020 and Q1 2021.
Table 4.
Association between no-shows for each visit modality by time
| Variables | No-show vs 0 no-show Adjusted OR (95% CI) |
||
|---|---|---|---|
| In-person | Video | Telephone | |
| Time | |||
| Q2 2020 | Reference | Reference | Reference |
| Q3 2020 | 1.11 (0.96, 1.28) | 1.42 (0.93, 2.16) | 1.58 (1.22, 2.06) |
| Q4 2020 | 0.80 (0.70, 0.93) | 1.63 (0.95, 2.80) | 1.39 (1.09, 1.79) |
| Q1 2021 | 0.76 (0.66, 0.87) | 0.89 (0.56, 1.41) | 1.02 (0.77, 1.34) |
| Q2 2021 | 0.80 (0.69, 0.91) | 1.10 (0.62, 1.98) | 2.31 (1.76, 3.04) |
| Q3 2021 | 0.92 (0.80, 1.06) | 1.64 (0.94, 2.87) | 1.61 (1.24, 2.10) |
aLogistic regression model using generalized estimating equations accounting for repeat measures in individuals and within sites
bAdjusted for age, race/ethnicity, gender, income, housing status, HIV risk factor, and pre-COVID-19 telehealth site indicator
cBold denotes statistical significance (p < 0.05)
Table 5 shows the relationship between sociodemographics and no-shows for each visit modality, separately. For in-person visits, older age (AOR [95% CI] 0.98 [0.97, 0.98]), female (AOR [95% CI] 0.83 [0.74, 0.93]), white (AOR [95% CI] 0.83 [0.75, 0.92]), Other race group (AOR [95% CI] 0.52 [0.38, 0.71]), those with permeant/stable housing person (AOR [95% CI] 0.53 [0.46, 0.60]), and MSM (AOR [95% CI] 0.82 [0.73, 0.92]) had lower odds of having a no-show. For video visits, the odds of having a no-show were only lower for those with permeant/stable housing (AOR [95% CI] 0.37 [0.20, 0.69]). For telephone visits, the odds of having a no-show were only lower for older age (AOR [95% CI] 0.98 [0.97, 0.98]) and other race group (AOR [95% CI] 0.41 [0.21, 0.80]).
Table 5.
Association between no-shows and sociodemographics by visit modality
| Variables | No-show vs 0 no-show Adjusted OR (95% CI) |
||
|---|---|---|---|
| In-person | Video | Telephone | |
| Age | 0.98 (0.97, 0.98) | 0.99 (0.97, 1.00) | 0.98 (0.97, 0.98) |
| Income (Unit = $100,000) | 1.00 (1.00, 1.00) | 0.72 (0.23, 2.27) | 0.71 (0.40, 1.28) |
| Gender | |||
| Men | 1.20 (1.07, 1.35) | 1.62 (0.93, 2.81) | 1.23 (0.98, 1.54) |
| Transgender | 1.92 (1.28, 2.87) | 1.61 (0.18, 14.1) | 0.65 (0.20, 2.11) |
| Women | Reference | Reference | Reference |
| Race/ethnicity | |||
| White | 0.83 (0.75, 0.92) | 0.93 (0.64, 1.34) | 0.91 (0.74, 1.12) |
| Other | 0.52 (0.38, 0.71) | 0.34 (0.04, 2.67) | 0.41 (0.21, 0.80) |
| Black | Reference | Reference | Reference |
| Housing status | |||
| Permanent/stable | 0.53 (0.46, 0.60) | 0.37 (0.20, 0.69) | 0.80 (0.52, 1.23) |
| Temporary/unstable | Reference | Reference | Reference |
| HIV risk factor | |||
| MSM | 0.82 (0.73, 0.92) | 0.68 (0.41, 1.13) | 0.81 (0.64, 1.02) |
| Other | 0.93 (0.76, 1.14) | 1.05 (0.51, 2.18) | 1.32 (0.88, 1.97) |
| Heterosexual | Reference | Reference | Reference |
aLogistic regression model using generalized estimating equations accounting for repeat measures in individuals and within
bBold denotes statistical significance (p < 0.05)
cTransgender includes individuals transgender, transgender male-to-female, and transgender female-to-male
dOther race includes Asian, Native Hawaiian/Pacific Islander, American Indian or Alaska Native, and Other (including mixed race)
eOther risk factor includes Injection drug use (IDU), hemophilia/coagulation disorder, receipt of blood transfusion, blood components, or tissue, perinatal transmission, and MSM/IDU
Discussion
This study showed telehealth visits (either video or telephone) to be the most common method of HIV healthcare delivery at D4C-participating clinic sites around the onset of the COVID-19 pandemic. However, as the pandemic progressed, most telehealth visits were replaced by in-person visits to the point that in-person visits accounted for 81.7% of total visits by the study end. Moreover, in-person visits had the highest rates throughout the study period, whereas telephone and video no-shows remained fairly stable. Noteworthy, the range of telehealth (video and telephone) no-shows was significantly smaller than in-person no-shows among individuals with ≥ 1 no-shows, which may suggest a lower likelihood of individuals missing a telehealth visit as compared to an in-person visit. Interestingly, around the onset of the COVID-19 pandemic, while the proportion of in-person and telephone visits were almost identical, telephone visits had a much lower no-show rate compared to in-person visits. While this significant difference between telephone and in-person no-shows may be due to the stay-at-home orders around the onset of COVID-19 pandemic, this difference persisted as in-person no-shows were significantly higher than the telephone no-shows by the end of the study period. When comparing the in-person visits versus video visits, no-shows were higher around the beginning of the study and became similar as the COVID-19 pandemic progressed.
The findings from this study were in line with those from previous studies. A study conducted at the Johns Hopkins HIV Clinical Cohort assessing completion of at least one scheduled in-person visit during a pre-pandemic period (September 1, 2019–March 15, 2020) versus completion of at least one scheduled telehealth visit during a pandemic period (March 16, 2020–Septempber 30, 2020) showed a higher rate of visit completion associated with telehealth visits in the pandemic period [5]. While the visits in the John Hopkins study temporarily shifted almost completely from in-person to telehealth after the onset of the COVID-19 pandemic, a comparison of in-person visits with telehealth visits during the pandemic period could not be made [5]. The John Hopkins study, however, did compare the visit completion among video and telephone visits during the pandemic period and found a much higher rate of visit completion for telephone visits when compared with video visits [5]. Our study did not find such evidence, as no statistically significant difference in the odds of being a no-show was observed among telephone and video visits in all quarters of the study period. Similarly, another study conducted in Chicago, Illinois, compared appointment attendance among telehealth visits (distinction between video and telephone visits not made) with in-person visits during the pandemic (Mar20–May21) and found that telehealth appointments had a higher appointment attendance compared to in-person appointments [6]. Previous studies have shown missed visits and kept visits to capture distinct behaviors among PWH [18] and although our study measured missed visits instead kept visits as done in John Hopkins and Chicago studies, we found similar trends among the two retention in care measurement types i.e. telehealth visits were less likely be missed visits (our study) and more likely to be kept visits (other studies).
When examining the trends in no-shows through the study period for each visit modality separately, it was seen that no-shows associated with in-person visits were higher around the beginning of the COVID-19 pandemic, after which no-show rates became significantly lower. Interestingly, in-person no-show rate around the end of the study period was found to be similar to that at the beginning of the COVID-19 pandemic. Similar to our findings, a study conducted in Africa (Tanzania, Uganda, Kenya, and Nigeria) found that PWH were less likely to be adherent to their HIV clinic visits (in-person visits) during the early phases of the COVID-19 pandemic compared with later in the pandemic [19]. Moreover, it was noteworthy to see that, even though the number of scheduled video visits declined as the study progressed (15.3% to 2.3%), the rate of no-shows remained similar throughout the study period compared to that at the onset of the COVID-19 pandemic. Lastly, while the no-show rate decreased among in-person visits and remained similar for video visits through the course of the study, no-show rates for telephone visits became higher as the study progressed compared to the beginning of the study period; this was coupled with the substantial decrease in number of scheduled telephone visits from the beginning of the study (42.4%) to the end of the study (16.1%).
Our study also found differences among sociodemographic groups to be most commonly associated with missing in-person visits. We found that younger age, Black and Other race group versus White, male and transgender versus cisgender female, those with temporary/unstable versus permanent/stable housing, and those reporting heterosexual contact as their HIV risk factor versus MSM were more likely to have an in-person no-show. This was similarly seen in the Chicago study, which showed that Black PWH and PWH with unstable housing arrangements had lower in-person appointment attendance [6].
Regarding video visits, while previous studies have indicated Black compared to White PWH and male compared to female PWH to be less likely to complete a video visit [5, 7, 17], our study did not find any differences in missing a video visit by race/ethnicity or gender. However, we did find PWH with temporary/unstable housing to be more likely to miss a video visit compared to PWH with stable housing arrangement. This may be due to the lack of telehealth access among those with temporary/unstable housing arrangement. While ensuring telehealth access may not be straightforward among homeless PWH, other efforts, such as ensuring telehealth access among shelters, day sites, etc., may be placed in order to minimize this inequity. When examining telephone visits, younger versus older and Black versus “Other” race PWH were more likely to have a no-show. In line with this, a qualitative study exploring experiences associated with telehealth use among older PWH (> 50 years) found older individuals to prefer telephone visits over video visits [20]. These results, which illustrate more sociodemographic differences in retention in care outcomes for in-person versus telehealth visits, suggest that telehealth visits may help ameliorate some of the structural barriers that contribute to health disparities.
Around the onset of the COVID-19 pandemic, telehealth visits (video and telephone) accounted for the majority of scheduled visits. This trend was, however, seen to change as the pandemic progressed, and most telehealth visits were replaced by in-person visits. Interestingly, it was seen that no-shows were higher for in-person visits and similar between telephone and video visits. Among telehealth visits, it was noteworthy that a substantially higher number of telephone visits were conducted as compared with video visits. Moreover, as the pandemic progressed, the no-shows for in-person visits decreased, remained similar for video visits, and increased for telephone visits, relative to the start of the pandemic.
Strengths and Limitations
This study was conducted using data from six HIV care facilities across the State of Alabama. The demographics of our study population are representative of PWH in Alabama making the findings generalizable to PWH in Alabama, as well as PWH living in areas similar to Alabama, especially in the Southern US, which faces the disparities associated HIV as well as technology access [8, 9]. While there were strengths associated with this study, there were also a few limitations. As sites report data quarterly, visit modality was added as a new reporting variable after the onset of the COVID-19 pandemic. Data on visit modality, therefore, first started being reported Q2 2020 (Apr20) onwards. Due to this, we were unable to assess no-shows with visit modality for the COVID-19 period between March 11, 2020, the onset of the COVID-19 pandemic, and March 31, 2020. Moreover, most of our covariates were self-reported and not validated. In addition, due to lack of data availability, we were unable to adjust for any COVID-19-related variables or the multiple COVID-19 waves which may have limited our ability to fully understand the findings. Moreover, although our analysis adjusted for sites’ pre-COVID telehealth access, we were unable to control for other factors that may have differed among sites (example access to video/telephone), which may have impacted the no-shows. Additionally, although we studied the no-show trends as the COVID-19 pandemic progressed among each visit modality, we did not assess this trend at an individual level. Moreover, our analysis did not assess the variance at an individual level or at a site level. Additionally, due to data availability restrictions, we were unable to assess in details the rescheduled visits in which the visit modality switched i.e. visit modality of the scheduled visits being different from the visit modality of the completed visit. Furthermore, our study population was predominantly from the MSM and heterosexual contact HIV risk factor categories, which may limit the generalizability of these findings to those reporting IDU or other HIV risk factors. Moreover, lack of substantial statistically significant findings associated with video visits may be due to the low statistical power associated with this group as a result of its small number. Lastly, the lag between the data being recorded and being available for analysis limited our ability to report the most up-to-date trends.
Conclusion
Findings from our study showed that, during the COVID-19 pandemic, HIV-related no-shows were impacted by visit modality. While in-person visits had higher no-show rates than telephone and video visits around the onset of the COVID-19 pandemic, no-show rates for video visits were similar to telephone visits. As the pandemic progressed, an increase in scheduled in-person visits was associated with a decrease in the no-shows within this visit modality. While both video and telephone visits decreased as the pandemic progressed, no-shows increased relative to the start of the pandemic for telephone visits and remained similar for video visits. Additionally, it was seen that while the association of no-shows with visit modality for in-person visits differed significantly among different sociodemographic groups, most groups had similar likelihood of having a no-show for telephone and video visits. In summary, even though the no-shows were higher for in-person visits when compared with telephone and video visits, no-shows within in-person visits significantly decreased as the COVID-19 pandemic progressed. Additionally, despite decreasing number of video and telephone visits, the no-shows within telephone visits were seen to increase and remain similar for video visits as the study progressed. Regardless, telehealth visits had lower no-show rates than in-person visits, which may suggest the success of telehealth in terms of achieving the desired HIV care outcomes during the COVID-19 pandemic.
Author Contributions
MS led study conception and design with consultation of MM. Material preparation and analysis were performed by MS. The first draft of the manuscript was written by MS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was a part of CDC PS18-1802 grant.
Data Availability
Data supporting the findings of this study are available from the corresponding author on request.
Code Availability
Code used for this study is available from the corresponding author on request.
Declarations
Conflict of interest
The authors have no conflict of interest.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University of Alabama at Birmingham.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Coronavirus disease 2019. Geneva: WHO; 2020. [Google Scholar]
- 2.Lawal FJ, Rao A, Vazquez JA. 1010. Effective management of HIV in rural Georgia using telemedicine. Open Forum Infect Dis. 2020;7(Suppl 1):S533. doi: 10.1093/ofid/ofaa439.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohl ME, Richardson K, Rodriguez-Barradas MC, et al. Impact of availability of Telehealth Programs on Documented HIV viral suppression: a cluster-randomized program evaluation in the Veterans Health Administration. Open Forum Infect Dis. 2019 doi: 10.1093/ofid/ofz206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auchus IC, Jaradeh K, Tang A, Marzan J, Boslett B. Transitioning to Telehealth during the COVID-19 pandemic: patient perspectives and attendance at an HIV clinic in San Francisco. AIDS Patient Care STDS. 2021;35(7):249–254. doi: 10.1089/apc.2021.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Nahal WG, Shen NM, Keruly JC, et al. Telemedicine and visit completion among people with HIV during the coronavirus disease 2019 pandemic compared with prepandemic. AIDS. 2022;36(3):355–362. doi: 10.1097/QAD.0000000000003119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boshara AI, Patton ME, Hunt BR, Glick N, Johnson AK. Supporting retention in HIV care: comparing in-person and Telehealth visits in a Chicago-based infectious disease clinic. AIDS Behav. 2022;26:2581–2587. doi: 10.1007/s10461-022-03604-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ennis N, Armas L, Butame S, Joshi H. Factors impacting video telehealth appointment completion during COVID-19 pandemic among people living with HIV in a community-based health system. AIDS Behav. 2022;26(2):407–414. doi: 10.1007/s10461-021-03394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. HIV in the United States and dependent areas. 2019.
- 9.Pick JB, Sarkar A, Johnson J. United States digital divide: state level analysis of spatial clustering and multivariate determinants of ICT utilization. Socioecon Plann Sci. 2015;49:16–32. doi: 10.1016/j.seps.2014.09.001. [DOI] [Google Scholar]
- 10.Schnall R, Musgrove K, Batey DS. Symptom profile and technology use of persons living with HIV who access services at a community-based organization in the deep South. J Assoc Nurses AIDS Care. 2020;31(1):42–50. doi: 10.1097/JNC.0000000000000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ADPH. At A Glance. 2010.
- 12.Mugavero MJ, Westfall AO, Cole SR, et al. Beyond core indicators of retention in HIV care: missed clinic visits are independently associated with all-cause mortality. Clin Infect Dis. 2014;59(10):1471–1479. doi: 10.1093/cid/ciu603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mugavero MJ, Westfall AO, Zinski A, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr (1999) 2012;61(5):574–580. doi: 10.1097/QAI.0b013e318273762f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kay ES, Batey DS, Westfall AO, et al. Compound retention in care and all-cause mortality among persons living with human immunodeficiency virus. Open Forum Infect Dis. 2019;6(4):ofz120. doi: 10.1093/ofid/ofz120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sohail M, Rastegar J, Long D, et al. Data for Care (D4C) Alabama: clinic-wide risk stratification with enhanced personal contacts for retention in HIV Care via the Alabama Quality Management Group. J Acquir Immune Defic Syndr (1999) 1999;2019(82 Suppl 3):S192–s198. doi: 10.1097/QAI.0000000000002205. [DOI] [PubMed] [Google Scholar]
- 16.SAS. SAS Software. Version 9.4. Cary, NC: SAS Institute Inc. 2014.
- 17.Wood BR, Lan KF, Tao Y, et al. Visit trends and factors associated with telemedicine uptake among persons with HIV during the COVID-19 pandemic. Open Forum Infect Dis. 2021;8(11):ofab480. doi: 10.1093/ofid/ofab480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Batey DS, Kay ES, Westfall AO, et al. Are missed- and kept-visit measures capturing different aspects of retention in HIV primary care? AIDS Care. 2020;32(1):98–103. doi: 10.1080/09540121.2019.1659918. [DOI] [PubMed] [Google Scholar]
- 19.Dear N, Duff E, Esber AL, et al. Transient reductions in Human Immunodeficiency Virus (HIV) clinic attendance and food security during the coronavirus disease 2019 (COVID-19) pandemic for people living with HIV in 4 African Countries. Clin Infect Dis. 2021;73:1901–1905. doi: 10.1093/cid/ciab379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baim-Lance A, Angulo M, Chiasson MA, et al. Challenges and opportunities of telehealth digital equity to manage HIV and comorbidities for older persons living with HIV in New York State. BMC Health Serv Res. 2022;22(1):609. doi: 10.1186/s12913-022-08010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting the findings of this study are available from the corresponding author on request.
Code used for this study is available from the corresponding author on request.