Abstract
Purpose of Review
To characterize the barriers and opportunities associated with racial and ethnic disparities in blood pressure (BP) control.
Recent Findings
Blood pressure (BP) control rates in the USA have worsened over the last decade, with significantly lower rates of control among people from racial and ethnic minority groups, with non-Hispanic (NH) Black persons having 10% lower control rates compared to NH White counterparts. Many factors contribute to BP control including key social determinants of health (SDoH) such as health literacy, socioeconomic status, and access to healthcare as well as low awareness rates and dietary habits. Numerous pharmacologic and non-pharmacologic interventions have been developed to reduce racial and ethnic disparities in BP control. Among these, dietary programs designed to help reduce salt intake, faith-based interventions, and community-based programs have found success in achieving better BP control among people from racial and ethnic minority groups.
Summary
Disparities in the prevalence and management of hypertension persist and remain high, particularly among racial and ethnic minority populations. Ongoing efforts are needed to address SDoH along with the unique genetic, social, economic, and cultural diversity within these groups that contribute to ongoing BP management inequalities.
Keywords: Hypertension, Ethnicity, Disparities, Social determinants of health
Introduction: Epidemiology of Hypertension Among Different Racial and Ethnic Groups
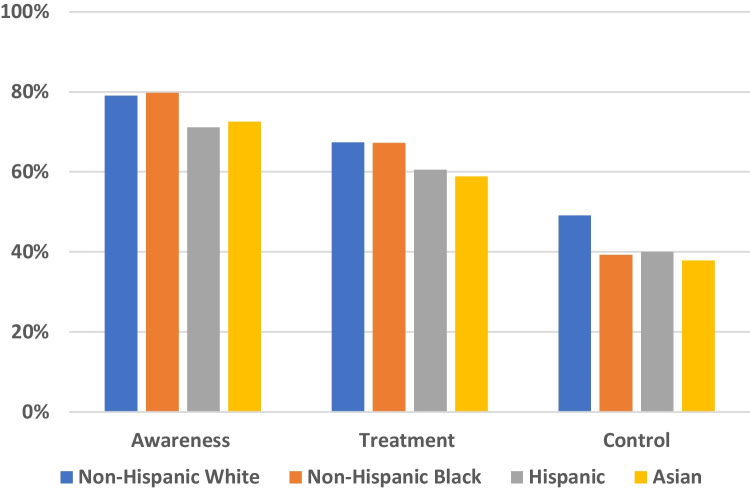
Hypertension is the most prevalent modifiable risk factor for cardiovascular disease (CVD) with nearly half of the US adult population meeting diagnostic criteria [1]. One representative study of over 23,000 participants in the National Health and Nutrition Examination Survey (NHANES) found that half of deaths from coronary heart disease (CHD) and stroke were among individuals with hypertension [2]. The treatment and control of hypertension is an important public health challenge, due to the substantial percentage of patients with uncontrolled BP and its strong association with increased CVD risk, especially stroke and heart failure [3]. Despite efforts to improve treatment and control of BP, management of hypertension has not been equitable for persons from racial and ethnic minority groups [4••]. A recent analysis of hypertension control rates from NHANES found that BP control rates were lower for Hispanic persons (40%), non-Hispanic (NH) Black persons (39%), and Asian American persons (38%) compared to NH White individuals (49%) (Fig. 1) [4••]. Additionally, NH Black persons are diagnosed with hypertension earlier in life and experience greater hypertension-related morbidity and mortality than NH White persons with 30% higher risk of fatal stroke, 50% higher risk of CVD mortality, and more than 4 times higher risk of end-stage renal disease [5]. Overall, NH Black persons experience 4–5 times greater hypertension-related mortality when compared to NH White Americans [6].
Fig. 1.
Awareness, treatment, and control of hypertension stratified by race/ethnicity
Regrettably, hypertension control rates have worsened nationally since 2013–2014 with significantly lower control experienced among persons without health insurance, a usual healthcare facility, or a healthcare visit within the past year [7]. Furthermore, NH Black persons were 12% less likely to have adequately controlled BP even after adjusting for socioeconomic status and access to health care. A similar story exists among the rapidly growing Hispanic/Latinx population [8], with a recent cross-sectional study of 6100 participants from the Hispanic Community Health Study/Study of Latinos showing variable rates of hypertension prevalence and control among Hispanic and Latino subgroups [9]. The highest prevalence was observed among those of Caribbean heritage with a 6-year probability of developing hypertension of 27% for Cuban persons and 28% for Dominican persons compared to the lowest rate of 18% among persons of Mexican American heritage [9]. However, of those men diagnosed with hypertension, achieving adequate control was suboptimal among all subgroups with those of South American heritage showing the lowest control rates at 7.5%, while persons of Dominican heritage had the highest control rates at 36% [9]. Asian American people similarly experience variable BP control rates, especially when analyzed by subgroups. Review of data collected from 600 Asian American persons living in the Baltimore-Washington Metropolitan area found that among Chinese, Korean, and Vietnamese subgroups, hypertension prevalence was 13.4%, 23.2%, and 22.9%, respectively [10]. Of those with hypertension, only about 64% received medical treatment and these rates did not differ among the subgroups (p = 0.36) [10]. Overall, while each of these populations represents a heterogeneous group of individuals with differences in genetic, environmental, and social backgrounds, a systemic pattern of higher hypertension prevalence and lower BP control among these racial and ethnic subgroups still exists.
Barriers to Adequate Diagnosis and Treatment—Social Determinants of Health
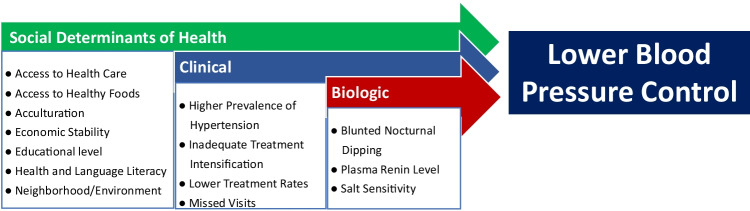
Multiple factors contribute to racial and ethnic disparities in hypertension treatment and control, key among them being SDoH including constrained access to consistent healthcare, low health literacy, lower socioeconomic status, neighborhood/environment stability, and reduced access to healthy food. These factors are compounded by other barriers to hypertension management including inadequate treatment intensification related to clinical inertia and biologic factors such as salt sensitivity (Fig. 2) [11, 12]. Importantly, these factors differ greatly across racial and ethnic populations.
Fig. 2.
Factors contributing to ethnic and racial disparities in hypertension
Lack of access to healthy food options and the presence of food deserts are important components of SDoH that contribute to the racial inequities in BP management and control. In particular, lack of access to affordable, healthy, and nutritious food has been linked to poorer health outcomes, with food insecurity associated with a 14 to 77% increased risk of hypertension [13]. One cross-sectional study of 930 rural participants found that food insecurity was associated with a 77% increased odds for hypertension (p = 0.001) and 51% increased odds for diabetes (p = 0.038) [14]. Recent programs, such as the GOFRESH initiative in Boston, have attempted to mitigate limited access to healthy food caused by “food deserts” that disproportionately impacts minority communities by delivering nutritious groceries to Black residents [15]. This program specifically aims to deliver groceries that meet Dietary Approaches to Stop Hypertension (DASH) criteria, a diet associated with significant reductions in systolic blood pressure (SBP) among NH Black adults (− 7 mm Hg) [16, 17]. The program’s high cost, estimated at approximately $500 per month, limits its expansion [15]. The confluence of the limited availability and high cost of healthy food are major barriers to dietary drivers that can help to reduce disparities in hypertension control.
Limited healthcare access is another major SDoH barrier that impedes an individual’s ability to achieve BP control. Uninsured and underinsured medical coverage status has been implicated in lower BP control among racial and ethnic minorities in the USA. In an analysis of 2013 data from over 120,000 participants in the Behavioral Risk Factor Surveillance System, antihypertensive medication adherence was significantly lower among those who were underinsured (OR 0.83, 95% CI 0.76–0.89) or uninsured (0.39, 0.35–0.43) compared with adequately insured individuals [18]. Similarly, data from 21,664 NHANES (2011–2018) participants showed that absence of a routine healthcare location/facility and/or lack of insurance was associated with a 43 to 82% lower prevalence of controlled BP [19]. Importantly, higher rates of inadequate or non-existent insurance coverage were disproportionately identified among racial and ethnic minorities, with an uninsured prevalence of 26.5% among Hispanic adults, 15% among NH Black adults, and 9% among NH White adults [18]. A recent analysis of 1600 Asian Americans living in Southern California who self-reported lack of insurance also experienced elevated BP [20]. Unfortunately, even when people have physical access to care, their ability to utilize it may be limited by language barriers. Individuals who indicated low English proficiency (defined as completion of a survey in a language other than English or with an interpreter) during an NHANES interview experienced higher rates of uncontrolled BP (OR 1.47, 1.07–2.03) than those with higher English proficiency [21]. Collectively, this demonstrates that lower insurance coverage and lack of healthcare access are important contributors to racial and ethnic disparities in BP control [19].
For foreign-born populations in the USA, acculturation, defined as a process in which individuals integrate, adapt, and retain behaviors, attitudes, and values between two cultures, is another SDoH that is linked to lower BP control [22]. In a study from NHANES comparing NH Black adults born either in the USA or another country, foreign-born NH Black adults experienced much lower rates of hypertension (27%) compared to US-born NH Black adults (42%) [23]. The authors hypothesize that this difference can be partially explained by major differences in lifestyle for NH Black Americans compared to NH Black adults from other parts of the world, especially as it relates to dietary practices, racism, and chronic stress [23]. An analysis of approximately 2600 NH White, 1900 NH Black, 1500 Hispanic, and 800 Chinese participants in the Multi-Ethnic Study of Atherosclerosis (MESA) study also showed that birthplace outside of the USA and a non-English speaking household were both associated with a lower prevalence of hypertension compared to US-born participants [22]. When compared to US-born participants, those with a birthplace outside of the USA had a lower prevalence of hypertension (prevalence ratio 0.82, 95% CI 0.77–0.87) as well as those in a non-English speaking household (prevalence ratio 0.82, 95% CI 0.74–0.85). Conversely, each decade of residence in the USA for foreign-born participants was associated with a 10% increased risk of hypertension [22]. An analysis from the National Health Interview Survey (NHIS) 2010–2014 showed that persons living in the USA for ≥ 10 years had an 18% higher odds ratio for hypertension compared to those living in the USA for < 10 years [24]. Finally, a study examining CVD risk factors in approximately 5000 first and second generation Mexican Americans in the Hispanic Health and Nutrition Examination Study (HHANES) and NHANES database showed that second generation Mexican Americans have 60% higher rates of hypertension than their first generation counterparts [25].
Genetic and Physiologic Differences
Differences in BP physiology among racial and ethnic minority groups have been extensively investigated. Variability in sodium and potassium homeostasis has been observed among NH Black individuals who demonstrate lower plasma renin levels and higher salt sensitivity along with a decreased ability to excrete a sodium load when compared to NH White individuals [6]. Dietary potassium supplementation can significantly reduce the degree of salt sensitivity among NH Blacks and a randomized control trial found that the addition of 80 mmol/day of potassium reduced SBP by approximately 7 mm Hg [26, 27]. Genetic studies have shown higher frequency of specific polymorphisms among NH Black patients with hypertension that predispose them to better responsiveness to thiazide diuretics as well as increased levels of pro-inflammatory cytokines that may increase end-organ damage [6]. Additionally, a blunted nocturnal decrease in BP, termed “nocturnal dipping,” has been observed among NH Black persons [28, 29]. The Ohasama study, performed in rural Japanese individuals, found nocturnal SBP was more strongly associated with CVD mortality than daytime SBP, and for every 10 mm Hg higher nocturnal SBP value, there was a 34% increased risk for CVD mortality (hazard ratio 1.34; CI 1.14–1.59) at 10-year follow-up [30].
For Asian people in particular, the association between increasing BP and risk of CVD disease is robust, although there is great variability in BP profiles among Asian nationalities. A study conducted using ambulatory BP monitoring in patients with hypertension from Japan and Thailand found significant differences in BP patterns among residents of these countries. Japanese patients had higher 24-h average SBP (133.4 mm Hg vs 131.7 mm Hg, p = 0.02) while Thai patients had higher nighttime SBP (128 mm Hg vs 123 mm Hg, p < 0.001) and less nocturnal dipping (p < 0.001). The physiological basis for these findings may be related to increased circulatory volume and salt sensitivity among Asian persons. The authors suggest that these differences in BP patterns may explain the variations in prevalence of coronary artery disease and stroke in these countries [31, 32].
Racial and Ethnic Specific Dietary and Lifestyle Considerations
Dietary and lifestyle patterns are extremely important factors in the development and management of hypertension [16]. Excess sodium intake is strongly associated with higher BP [33]. While the World Health Organization has recommended that adults should not exceed 2 g/day of sodium, the US Food and Drug Administration has recommended that Americans consume no more than 2.3 g/day, although federal agencies also indicate that African Americans and those with chronic medical conditions should aim for a lower target of 1.5 g/day [33, 34]. However, 90% of US adults consume ≥ 2.3 g/day of sodium [1], with a mean daily sodium intake of approximately 4.2 g/day for men and 3.0 g/day for women [1]. Approximately two-thirds of sodium intake is due to the consumption of processed or pre-prepared foods [35]. Accordingly, many countries have begun to implement multimodal strategies to reduce sodium content in prepared foods and update food policies. The DASH trial showed a significant reduction in SBP that was more effective among persons with hypertension (− 11.5 mm Hg) compared to those without hypertension (− 7 mm Hg, p < 0.001). A subgroup analysis showed that the BP-lowering effect was most pronounced in NH Black patients with hypertension (− 12.6 mm Hg) compared to other subgroups with hypertension (− 9.6 mm Hg, p < 0.001), specifically NH White persons and Asian people [16].
Reduction in sodium intake is an important intervention in East Asian countries such as China, Korea, and Japan, which have some of the highest rates of sodium-associated CVD death, especially due to stroke [36]. In a recent analysis of over 20,000 participants in rural China with almost 90% reporting a history of hypertension, the use of a salt substitute in place of sodium chloride resulted in a 14% lower rate of stroke (rate ratio 0.86; CI 0.77–0.96), 13% lower rate of major CVD events (rate ratio 0.87; CI 0.80–0.94), and 12% lower rate of death (rate ratio 0.88; CI 0.82–0.95) [37]. Importantly, the majority of sodium intake in these rural areas is found in foods prepared at home and not in preprocessed foods. In South Korea, where the average daily consumption of sodium exceeds 4 g/day, a national initiative to increase awareness of sodium intake and availability of lower sodium foods was associated with 24% reduction in sodium consumption between 2010 and 2014. It was also associated with a decrease in hypertension prevalence for both men (from 33.5 to 26.0%) and women (from 25.2 to 21.7%) during the same time period [38]. Dietary sodium reduction is especially important for Asian persons who have both higher salt sensitivity and salt intake compared to persons living in Western Europe and North America [39]. Asian Americans also have one of the highest salt-dense diets of all racial groups with rice, breads, and soups comprising almost 30% of their dietary sodium intake [40]. Focusing efforts on reducing intake of these food groups may be an effective strategy to reduce sodium intake in Asian American diets. Data from the Asia Pacific Cohort Study found a stronger link between hypertension and CVD in Asian individuals than persons living in Western countries, which adds support to the importance of these dietary interventions as an opportunity to reduce hypertension-related morbidity and mortality among persons who live in Asia and those of Asian descent [39].
In the USA, there is significant heterogeneity in dietary patterns, which contributes to observed racial and ethnic disparities in BP control. The Southern diet score, which is characterized by a diet high in intake of added fats, eggs, fried foods, processed red meat, refined grains, and soda/sugar sweetened beverages, is associated with an increased risk of hypertension [41]. In an analysis of 6897 participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS), a Southern dietary pattern was observed as the largest mediator for the difference in incident hypertension between NH Black men (52%) and NH Black women (29%) compared to NH White men and women [42••].
Medication and Treatment Considerations
Racial and ethnic disparities in BP control extend to factors beyond the percentage of patients treated with BP-lowering medications. A pooled analysis of 16,531 individuals in NHANES 2013–2018 found that NH Black Americans achieved lower BP control rates than NH White Americans (39% vs 49%), even though both groups demonstrated similar rates of hypertension awareness and treatment [4••]. This observed difference was partially explained by the results of a study of more than 16,000 patients investigating the association of treatment intensification, follow-up interval, and missed visits in which NH Black Americans had higher rates of uncontrolled hypertension (34%) compared to their NH White (28%), Asian (25%), and Hispanic (27%) counterparts. It was observed that 21% of the BP difference among NH Black adults was accounted for by lower treatment intensification and 14% by missed visits [43]. Even though NH Black patients attended more total visits than patients from all other racial groups, they still had the lowest BP control rate at the end of the study compared to the total average (66% vs 71.9%, respectively). Accordingly, a focus on treatment intensification and prevention of missed visits may be an important strategy to improve BP control among NH Black Americans [43].
The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) blood pressure guideline recommends calcium channel blockers and thiazide diuretics as first-line agents for NH Black adults with hypertension who do not have heart failure or renal disease, along with an added emphasis for the use of antihypertensive medications from two or more different classes [44]. Many trials have evaluated the efficacy of various antihypertensive regimens and found conflicting results, particularly with respect to racial and ethnic-based treatment specific studies, especially among NH Black adults. While the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) trial did not show angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers (CCB), or alpha-receptor blockers to be superior to thiazide diuretics at reducing BP, thiazide diuretics did have a higher efficacy for preventing stroke among NH Black persons compared to the other medication groups [45]. However, in an analysis of NH Black Americans with non-diabetic renal disease, the African American Study of Kidney Disease found that ACE inhibitors were superior to beta-blockers and CCB in slowing progression of renal disease, contradicting a similar analysis in ALLHAT that suggested ACE inhibitors were not superior to other antihypertensive classes at preventing kidney disease [45, 46].
The International Society of Hypertension in Blacks (ISHIB) recommends combination therapy with a CCB plus a renin-angiotensin blocking agent (preferably angiotensin receptor blocker [ARB]) as first-line treatment for NH Black patients with hypertension. NH Black persons experience higher rates of angioedema with ACE inhibitors making ARB the preferred option [47, 48]. These recommendations were based on the Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial that found a combination of ACE inhibitor/CCB was superior to ACE inhibitor/thiazide diuretic in reducing cardiovascular event rates (HR, 0.80, 95% CI, 0.72 to 0.90; p < 0.001). However, low dose of hydrochlorothiazide (12.5 mg) was used instead of the more potent and longer-acting chlorthalidone (up to 25 mg) that was used in the ALLHAT trial and may have contributed to the discrepancy of the results [45, 49].
Unfortunately, similar guidelines do not exist for Hispanic and Asian populations. However, some studies have shown that Japanese patients may benefit from diuretic monotherapy as salt-sensitive hypertension is very common, and the Japanese Society of Hypertension currently recommends diuretics as one of its first-line agents [50]. South Asian patients have been shown to be particularly responsive to ACE-inhibitor/ARB therapy [51]. However, this is complicated by the fact that Asian people, particularly East Asian persons (OR 4.3, CI 1.2 to 14.8), have some of the highest rates of ACE inhibitor-related cough which may be a significant barrier to medication adherence [52].
NH Black adults also have higher rates of resistant hypertension, defined as persistently elevated BP despite three adequately dosed antihypertensives or the need for four antihypertensives to achieve BP control, compared to NH White adults [53]. NH Black adults also have lower rates of hypertension control and lower treatment intensification [43, 53]. However, it is important to differentiate true resistant hypertension from inadequate treatment dosing, medication non-adherence, and suboptimal use of first-line antihypertensive medications [53].
Novel Approaches to Blood Pressure Management for Different Racial and Ethnic Groups
As awareness of the racial and ethnic differences in hypertension treatment and control increases, innovative approaches focusing on SDoH have been investigated to specifically target the needs of vulnerable communities (Fig. 3). Community-based outreach programs have seen major growth over the past decade with efforts focused on improving access to health care and health literacy. The Los Angeles Barbershop Blood Pressure Study examined the efficacy of a health promotion and medication management intervention in a cluster-randomized trial design. In this study, NH Black barbers in the intervention group were trained to measure BP and encourage pharmacist follow-up in a collaborative practice agreement with physician hypertension specialists. Through this innovative approach, NH Black men in the intervention group experienced a 22 mm Hg greater reduction in SBP compared to the control group (p < 0.001), with 63% in the intervention group achieving a BP of < 130/80 mm Hg at 6-month follow-up [54, 55••].
Fig. 3.
Interventions to improve racial and ethnic disparities in blood pressure control
In Detroit, MI, the Wayne Health Mobile Unit program was launched in 2020 initially to address coronavirus disease testing inequities and soon grew into a mobile health department aimed at improving access to health care and health literacy by implementing an intervention focused on the extremely high prevalence of hypertension among its NH Black residents [56]. These units provided hypertension screening and arranged for follow-up care at local health clinics [56]. Of the approximately 3000 patients who participated, 63% were diagnosed with hypertension. This community-based effort was a groundbreaking approach to target vulnerable minority communities that have lower levels of hypertension awareness and treatment.
Another effort focused on improving access to health care concentrated on increasing medication adherence among NH Black Americans by enrolling primary care and emergency department hypertensive patients in a text-messaging-based program to send reminders to take scheduled medication doses. This program showed modest, although non-significant improvement in medication adherence (p = 0.26) with a mean − 13 mm Hg change in SBP (p = 0.78) and − 5 mm Hg (p = 0.54) change in diastolic BP. Higher baseline SBP on enrollment was a predictor of greater SBP decrease (β = − 0.63, p < 0.001) [57]. A remote BP monitoring was performed in rural Mississippi using telemonitoring and home BP kits. One hundred and twenty individuals with uncontrolled hypertension were provided home BP monitors, including 65% women, 60% NH Black people, 27.5% who did not complete high school, and 46.7% with reported annual household income < $30 000. Participants transmitted daily BP readings that were evaluated by a pharmacist every 3 weeks with specific algorithms for medication up titration. By the end of the 6-month study, the mean reduction in SBP was 14 mm Hg (CI − 17 to − 11 mm Hg, p < 0.001). Half of participants achieved a BP < 130/80 mm Hg and 80% achieved BP < 140/90 mm Hg demonstrating promise in using remote telemonitoring technology even in low-income and rural communities [58].
A faith-based study in Asian communities in the metropolitan New York area examined interventions to improve health literacy, reduce language barriers, and improve access to healthcare. Approximately 1600 congregants of Asian Indian, Korean, Filipino, and Bangladeshi religious communities underwent regularly scheduled culturally sensitive counseling regarding lifestyle and dietary modifications and were also provided assistance in navigating the healthcare system. Participants with BP readings > 140/90 mm Hg on screening were referred to a clinician for further treatment. After 6 months, the average SBP of participants decreased significantly (− 1.7 mm Hg, p = 0.03) with the most substantial reduction seen in Bangladeshi individuals (− 6.3 mm Hg, p = 0.007) [59].
A similar community-based intervention was applied in a study of approximately 8000 Latino patients in San Antonio, TX, with pre-existing CVD risk factors. These patients were paired with cultural navigators who performed diet and lifestyle counseling and assisted each patient with recording home BP readings. After 90 days, the average SBP decrease was 7.6 mm Hg (p < 0.001) [60]. Overall, initiatives targeting SDoH such as access to healthcare, health literacy, language barriers, and neighborhood/environment stability are effective intervention strategies to reduce racial and ethnic disparities in hypertension treatment and control (Table 1).
Table 1.
Novel interventions to improve blood pressure control
| Trial | Type of intervention | Social determinant of health | Study population | Intervention | Outcomes |
|---|---|---|---|---|---|
| Dietary Approaches to Stop Hypertension (DASH) [16] | Dietary | Nutrition |
•Primarily NH Black and NH White participants •With or without a HTN diagnosis |
Randomized to DASH diet or control diet; with varying sodium intake levels | •7.1 mm Hg SBP decrease (without HTN) and 11.5 mm Hg decrease (with HTN) (p < 0.001) |
| Remote telehealth in Mississippi [56] | Remote monitoring |
Income Access to healthcare Education |
•Participants with BP ≥ 140/90 mm Hg •60% NH Black |
Home BP monitoring reviewed by pharmacists, paired with medication management |
•14 mm Hg reduction in SBP at6 months (p < 0.001) •50% achieved BP < 130/80 mm Hg •81% achieved BP < 140/90 mmHg |
| Los Angeles Barbershop Blood Pressure Study [52] | Community-based | Access to healthcare | •Primarily NH Black participants with SBP ≥ 140 mm Hg | Cluster randomization of barbershops to screening or community-based pharmacist medication management |
•22 mm Hg reduction in SBP (p < 0.001) •64% in the intervention group achieved BP < 130/80 mm Hg |
| Faith-based intervention in New York City [57] | Community-based | Health literacy | •Asian Indians, Koreans, Filipinos, and Bangladeshis attending faith-based organizations | Culturally tailored lifestyle counseling, health coaching, healthcare navigation | •1.7 mm Hg decrease in SBP (p = 0.03) |
| San Antonio-based peer navigation program [58] | Community-based | Access to healthcare | •Latinx with CVD risk factors | BP monitoring, lifestyle and dietary counseling, medical follow-up | •7.6 mm Hg decrease in SBP (p < 0.001) |
| Health literacy | •92% were prescribed antihypertensives | •Improved quality of life |
Abbreviations: SBP, systolic blood pressure; BP, blood pressure; HTN, hypertension; CVD, cardiovascular disease
Future Directions
The Pooled Cohort Equation (PCE), which is based on traditional ASCVD risk factors, is recommended by the ACC/AHA to estimate ASCVD risk among US adults [61]. However, this risk calculator only stratifies for NH White and NH Black individuals and offers no specific assessment for Hispanic people and Asian people. Studies demonstrate that ASCVD risk is often overestimated by the PCE in Asian subgroups. An analysis of 922 patients of Chinese, Indian, and Malaysian descent calculated a median PCE risk score of 10.1%, but the observed ASCVD event rate was only 4.9% [62, 63]. However, these results were pooled individuals of multiple Asian ethnicities, and the lack of disaggregation of Asian subgroups for risk assessment remains a significant clinical issue. There are major differences in ASCVD risk with South Asian people at substantially higher risk while most East Asian people, including Chinese-Americans, Japanese-Americans, and Korean-Americans at much lower risk [64, 65]. Similar to Asian subgroups, those of Hispanic or Latinx origin also experience heterogeneity in ASCVD risk, with people of Puerto Rican or Caribbean descent carrying a higher risk than those of Mexican descent [61]. A recent analysis of patients in California of primarily Hispanic (Puerto Rican, Mexican, other Hispanic) and Asian (Chinese, Asian Indian, Filipino, Korean, Japanese, Vietnamese) subgroups found that the PCE overestimated ASCVD risk for these populations as a whole, but not necessarily for each individual subgroup. The predicted-to-observed ratio of ASCVD events was 1.3 (p < 0.001) for Mexican patients but 1.1 (p = 0.89) for Puerto Rican patients [66].
While all racial and ethnic groups comprise individuals of highly variable genetic and environmental backgrounds, very limited racial and ethnic stratification exists in the CVD risk tools used in US clinical practice, largely due to a lack of high-risk cohorts from which to derive them [64]. Increased representation of these racial and ethnic groups through oversampling for national health surveys such as NHANES and NHIS could provide a foundation to create specific ASCVD risk assessment tools tailored to Asian and Hispanic subgroups.
Conclusions
The prevalence of hypertension in the USA remains high while substantial racial and ethnic differences in disease awareness, treatment, and control persist—many of these disparities disproportionally affect racial and ethnic minority populations. SDoH, including healthcare access, socioeconomic status, reduced access to healthy foods, acculturation, health literacy, and language, are major drivers of these disparities among racial and ethnic minorities. Suboptimal dietary and lifestyle patterns and lower rates of antihypertensive medication intensification further impede optimal BP control. Recognizing that ethnic and minority groups are genetically, socially, and environmentally diverse is crucial in developing a multifaceted approach to hypertension treatment. Dietary interventions such as the DASH diet and dietary salt substitution along with novel treatment strategies such as the Los Angeles Barbershop study and other community-based intervention programs have proven to be effective strategies for racial and ethnic minority groups. Efforts focused on increasing clinician awareness to the importance of SDoH, evaluating racial and ethnic-specific pharmacologic and nonpharmacologic treatment plans, along with consideration of novel intervention strategies will be critical to addressing the widespread issue of racial and ethnic disparities in hypertension control in the USA and reducing CVD morbidity and mortality.
Compliance with Ethical Standards
Conflict of Interest
Dr. Yang reports the following relationships and activities: Measure Labs (medical advisory board, developing technology for blood pressure monitoring) and Microsoft Research (research grant to support study on remote PPG technologies). The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Hypertension
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation. 2011;123(16):1737–1744. doi: 10.1161/CIRCULATIONAHA.110.005645. [DOI] [PubMed] [Google Scholar]
- 3.2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 10.1161/HYP.0000000000000066
- 4.••.Aggarwal R, Chiu N, Wadhera RK, et al. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertens Dallas Tex 1979. 2021;78(6):1719–1726. 10.1161/HYPERTENSIONAHA.121.17570. There are significant differences in blood pressure prevalence, treatment, and control among non-Hispanic Black, Hispanic, and Asian Americans. [DOI] [PMC free article] [PubMed]
- 5.Hardy ST, Chen L, Cherrington AL, et al. Racial and ethnic differences in blood pressure among US adults, 1999–2018. Hypertension. 2021;78(6):1730–1741. doi: 10.1161/HYPERTENSIONAHA.121.18086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferdinand KC, Armani AM. The management of hypertension in African Americans. Crit Pathw Cardiol. 2007;6(2):67–71. doi: 10.1097/HPC.0b013e318053da59. [DOI] [PubMed] [Google Scholar]
- 7.Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324(12):1190–1200. doi: 10.1001/jama.2020.14545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Projections of the size and composition of the U.S. population: 2014 to 2060. Published online 2014:13.
- 9.Elfassy T, Zeki Al Hazzouri A, Cai J, et al. Incidence of hypertension among US Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos, 2008 to 2017. J Am Heart Assoc. 2020;9(12):e015031. 10.1161/JAHA.119.015031 [DOI] [PMC free article] [PubMed]
- 10.Jung MY, Lee S, Thomas SB, Juon HS. Hypertension prevalence, treatment, and related behaviors among Asian Americans: an examination by method of measurement and disaggregated subgroups. J Racial Ethn Health Disparities. 2019;6(3):584–593. doi: 10.1007/s40615-018-00557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu A, Yue Y, Desai RP, Argulian E. Racial and ethnic differences in antihypertensive medication use and blood pressure control among US adults with hypertension: the National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10(1):e003166. doi: 10.1161/CIRCOUTCOMES.116.003166. [DOI] [PubMed] [Google Scholar]
- 12.Min LY, Islam RB, Gandrakota N, Shah MK. The social determinants of health associated with cardiometabolic diseases among Asian American subgroups: a systematic review. BMC Health Serv Res. 2022;22(1):257. doi: 10.1186/s12913-022-07646-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Te Vazquez J, Feng SN, Orr CJ, Berkowitz SA. Food insecurity and cardiometabolic conditions: a review of recent research. Curr Nutr Rep. 2021;10(4):243–254. doi: 10.1007/s13668-021-00364-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Helmick M, Smith TM, Parks CA, Hill JL. Food insecurity increases odds of diabetes and hypertension, not obesity in medically underserved region. J Hunger Environ Nutr. 2020;15(1):128–139. doi: 10.1080/19320248.2018.1538921. [DOI] [Google Scholar]
- 15.GoFresh. GoFresh. Accessed May 16, 2022. https://www.gofreshstudy.org/
- 16.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. 10.1056/NEJM200101043440101 [DOI] [PubMed]
- 17.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 18.Fang J, Zhao G, Wang G, Ayala C, Loustalot F. Insurance status among adults with hypertension—the impact of underinsurance. J Am Heart Assoc. 5(12):e004313. 10.1161/JAHA.116.004313 [DOI] [PMC free article] [PubMed]
- 19.Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens. 2021;34(7):707–717. doi: 10.1093/ajh/hpab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng I, Ho WE, Woo BK, Tsiang JT. Correlations between health insurance status and risk factors for cardiovascular disease in the elderly Asian American population. Cureus. 2018;10(3):e2303. doi: 10.7759/cureus.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim EJ, Kim T, Paasche-Orlow MK, Rose AJ, Hanchate AD. Disparities in hypertension associated with limited English proficiency. J Gen Intern Med. 2017;32(6):632–639. doi: 10.1007/s11606-017-3999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moran A, Diez Roux AV, Jackson SA, et al. Acculturation is associated with hypertension in a multiethnic sample*. Am J Hypertens. 2007;20(4):354–363. 10.1016/j.amjhyper.2006.09.025 [DOI] [PubMed]
- 23.Brown AGM, Houser RF, Mattei J, Mozaffarian D, Lichtenstein AH, Folta SC. Hypertension among US-born and foreign-born non-Hispanic Blacks: National Health and Nutrition Examination Survey 2003–2014 data. J Hypertens. 2017;35(12):2380–2387. doi: 10.1097/HJH.0000000000001489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Commodore‐Mensah Y, Ukonu N, Obisesan O, et al. Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: a contemporary analysis of the National Health Interview Survey. J Am Heart Assoc. 5(11):e004059. 10.1161/JAHA.116.004059 [DOI] [PMC free article] [PubMed]
- 25.Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican-Americans. J Immigr Minor Health. 2011;13(1):61–68. doi: 10.1007/s10903-009-9262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kurtz TW, DiCarlo SE, Pravenec M, Morris RC. No evidence of racial disparities in blood pressure salt sensitivity when potassium intake exceeds levels recommended in the US dietary guidelines. Am J Physiol Heart Circ Physiol. 2021;320(5):H1903–H1918. doi: 10.1152/ajpheart.00980.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brancati FL, Appel LJ, Seidler AJ, Whelton PK. Effect of potassium supplementation on blood pressure in African Americans on a low-potassium diet. A randomized, double-blind, placebo-controlled trial. Arch Intern Med. 1996;156(1):61–67. [PubMed]
- 28.Jones DW, Hall JE. Racial and ethnic differences in blood pressure. Circulation. 2006;114(25):2757–2759. doi: 10.1161/CIRCULATIONAHA.106.668731. [DOI] [PubMed] [Google Scholar]
- 29.Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta-analysis. Hypertens Dallas Tex 1979. 1999;33(5):1099–1104. 10.1161/01.hyp.33.5.1099 [DOI] [PubMed]
- 30.Kikuya M, Ohkubo T, Asayama K, et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality. Hypertension. 2005;45(2):240–245. doi: 10.1161/01.HYP.0000152079.04553.2c. [DOI] [PubMed] [Google Scholar]
- 31.Tomitani N, Wanthong S, Roubsanthisuk W, Buranakitjaroen P, Hoshide S, Kario K. Differences in ambulatory blood pressure profiles between Japanese and Thai patients with hypertension/suspected hypertension. J Clin Hypertens. 2020;23(3):614–620. doi: 10.1111/jch.14107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kario K. The HOPE Asia Network activity for “zero” cardiovascular events in Asia: overview 2020. J Clin Hypertens. 2020;22(3):321–330. doi: 10.1111/jch.13750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nutrition C for FS and A. FDA issues sodium reduction final guidance. FDA. Published online October 13, 2021. Accessed June 11, 2022. https://www.fda.gov/food/cfsan-constituent-updates/fda-issues-sodium-reduction-final-guidance
- 34.Committee on the Consequences of Sodium Reduction in Populations, Food and Nutrition Board, Board on Population Health and Public Health Practice, Institute of Medicine. Sodium intake in populations: assessment of evidence. In: Strom BL, Yaktine AL, Oria M (eds). National Academies Press (US); 2013. Accessed July 14, 2022. http://www.ncbi.nlm.nih.gov/books/NBK201519/ [PubMed]
- 35.Harnack LJ, Cogswell ME, Shikany JM, et al. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775–1783. doi: 10.1161/CIRCULATIONAHA.116.024446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 37.Neal B, Wu Y, Feng X, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med. 2021;385(12):1067–1077. doi: 10.1056/NEJMoa2105675. [DOI] [PubMed] [Google Scholar]
- 38.Park HK, Lee Y, Kang BW, et al. Progress on sodium reduction in South Korea. BMJ Glob Health. 2020;5(5):e002028. doi: 10.1136/bmjgh-2019-002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kario K, Chen CH, Park S, et al. Consensus document on improving hypertension management in Asian patients, taking into account Asian characteristics. Hypertens Dallas Tex 1979. 2018;71(3):375–382. 10.1161/HYPERTENSIONAHA.117.10238 [DOI] [PubMed]
- 40.Firestone MJ, Beasley JM, Kwon SC, Ahn J, Trinh-Shevrin C, Yi SS. Asian American dietary sources of sodium and salt behaviors compared with other racial/ethnic groups, NHANES, 2011–2012. Ethn Dis. 27(3):241–248. doi:10.18865/ed.27.3.241 [DOI] [PMC free article] [PubMed]
- 41.Judd SE, Gutiérrez OM, Newby PK, et al. Dietary patterns are associated with incident stroke and contribute to excess risk of stroke in Black Americans. Stroke. 2013;44(12):3305–3311. doi: 10.1161/STROKEAHA.113.002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.••.Howard G, Cushman M, Moy CS, et al. Association of clinical and social factors with excess hypertension risk in Black compared with White US adults. JAMA. 2018;320(13):1338–1348. 10.1001/jama.2018.13467. A Southern dietary pattern was the largest mediator for incident hypertension among non-Hispanic Black persons compared to non-Hispanic White persons. [DOI] [PMC free article] [PubMed]
- 43.Fontil V, Pacca L, Bellows BK, et al. Association of differences in treatment intensification, missed visits, and scheduled follow-up interval with racial or ethnic disparities in blood pressure control. JAMA Cardiol. 2022;7(2):204–212. doi: 10.1001/jamacardio.2021.4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 45.The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288(23):2981–2997. 10.1001/jama.288.23.2981 [DOI] [PubMed]
- 46.Wright JT, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288(19):2421–2431. doi: 10.1001/jama.288.19.2421. [DOI] [PubMed] [Google Scholar]
- 47.Montinaro V, Cicardi M. ACE inhibitor-mediated angioedema. Int Immunopharmacol. 2020;78:106081. doi: 10.1016/j.intimp.2019.106081. [DOI] [PubMed] [Google Scholar]
- 48.Whelton PK, Einhorn PT, Muntner P, et al. Research needs to improve hypertension treatment and control in African Americans. Hypertens Dallas Tex 1979. 2016;68(5):1066–1072. 10.1161/HYPERTENSIONAHA.116.07905 [DOI] [PMC free article] [PubMed]
- 49.Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417–2428. doi: 10.1056/NEJMoa0806182. [DOI] [PubMed] [Google Scholar]
- 50.Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019) Hypertens Res Off J Jpn Soc Hypertens. 2019;42(9):1235–1481. doi: 10.1038/s41440-019-0284-9. [DOI] [PubMed] [Google Scholar]
- 51.Bennett A, Parto P, Krim SR. Hypertension and ethnicity. Curr Opin Cardiol. 2016;31(4):381–386. doi: 10.1097/HCO.0000000000000293. [DOI] [PubMed] [Google Scholar]
- 52.Morimoto T, Gandhi TK, Fiskio JM, et al. Development and validation of a clinical prediction rule for angiotensin-converting enzyme inhibitor-induced cough. J Gen Intern Med. 2004;19(6):684–691. doi: 10.1111/j.1525-1497.2004.30016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Flack JM, Nasser SA, Levy PD. Therapy of hypertension in African Americans. Am J Cardiovasc Drugs. 2011;11(2):83–92. doi: 10.2165/11586930-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 54.Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in Black barbershops. N Engl J Med. 2018;378(14):1291–1301. doi: 10.1056/NEJMoa1717250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.••.Victor RG, Blyler CA, Li N, et al. Sustainability of blood pressure reduction in Black barbershops. Circulation. 2019;139(1):10–19. 10.1161/CIRCULATIONAHA.118.038165. Among Black male barbershops clients with hypertension, those that underwent blood pressure management driven by an innovative collaboration between pharmacists and barbers had significantly lower blood pressure than those who underwent conventional management by pharmacists alone. [DOI] [PMC free article] [PubMed]
- 56.Brook RD, Dawood K, Foster B, et al. Utilizing mobile health units for mass hypertension screening in socially vulnerable communities across Detroit. Hypertens Dallas Tex 1979. 2022;79(6):e106-e108. 10.1161/HYPERTENSIONAHA.122.19088 [DOI] [PMC free article] [PubMed]
- 57.Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR MHealth UHealth. 2017;5(2):e9. doi: 10.2196/mhealth.6630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clark D, Woods J, Zhang Y, Chandra S, Summers RL, Jones DW. Home blood pressure telemonitoring with remote hypertension management in a rural and low-income population. Hypertension. 2021;78(6):1927–1929. doi: 10.1161/HYPERTENSIONAHA.121.18153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yi SS, Wyatt LC, Patel S, et al. A faith-based intervention to reduce blood pressure in underserved metropolitan New York immigrant communities. Prev Chronic Dis. 2019;16:E106. doi: 10.5888/pcd16.180618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Langabeer JR, Henry TD, Perez Aldana C, DeLuna L, Silva N, Champagne-Langabeer T. Effects of a community population health initiative on blood pressure control in Latinos. J Am Heart Assoc. 2018;7(21):e010282. doi: 10.1161/JAHA.118.010282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Racial disparities in hypertension prevalence and management: a crisis control? American College of Cardiology. Accessed May 11, 2022. https://www.acc.org/latest-in-cardiology/articles/2020/04/06/08/53/http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2farticles%2f2020%2f04%2f06%2f08%2f53%2fracial-disparities-in-hypertension-prevalence-and-management
- 62.Chia YC, Lim HM, Ching SM. Validation of the pooled cohort risk score in an Asian population - a retrospective cohort study. BMC Cardiovasc Disord. 2014;14:163. doi: 10.1186/1471-2261-14-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee CH, Woo YC, Lam JKY, et al. Validation of the pooled cohort equations in a long-term cohort study of Hong Kong Chinese. J Clin Lipidol. 2015;9(5):640–646.e2. doi: 10.1016/j.jacl.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 64.Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018;138(1):e1–e34. doi: 10.1161/CIR.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 65.Shah NS, Xi K, Kapphahn KI, et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes. 2022;15(5):e008651. doi: 10.1161/CIRCOUTCOMES.121.008651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rodriguez F, Chung S, Blum MR, Coulet A, Basu S, Palaniappan LP. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc. 2019;8(14):e011874. doi: 10.1161/JAHA.118.011874. [DOI] [PMC free article] [PubMed] [Google Scholar]