Abstract
Almost one year since the COVID-19 was declared a global pandemic, mental distress remains elevated with high prevalence of post-traumatic stress disorder (PTSD). Yet studies suggest these challenging circumstances might be conducive of post-traumatic growth (PTG). This study aims to investigate the factors associated with growth after the original trauma. A sample of 252 Lebanese adults filled an online survey to determine levels of PTG, PTSD and gratitude using validated self-rating scales. Participants also subjectively evaluated the sources of their distress such as the COVID-19 pandemic, the Beirut port explosion and/or their deteriorating financials. The PTGi-SF evaluated dimensions of growth while the IES-R_22 measured the degree of distress post-trauma. The GQ-6 was used to measure the proneness to experience gratitude daily. Results indicated 41% of participants scored above the cutoff for PTSD symptomatology. Yet, PTSD was positively correlated, alongside gratitude and accumulated subjective distress, with higher levels of PTG. A forward linear regression taking PTG scores as the dependent variable further showed that more gratitude (Beta = 0.57), a higher impact of events (Beta = 0.16), and knowing anyone who died from COVID-19 (Beta = 3.93) were significantly associated with more growth. The study highlights elevated levels of PTSD symptoms in a context of a global pandemic worsened by financial and socio-political instabilities. It mostly identifies personal factors, including high initial symptomatology post-trauma and gratitude, related to the capacity for growth in spite of these accumulating hardships. As such, it advocates the need to investigate and bolster silver linings amidst unprecedented traumas.
Keywords: Post-traumatic growth, Post-traumatic stress disorder, COVID-19, Gratitude, Lebanon
Introduction
The COVID-19 pandemic - a highly contagious and potentially lethal disease caused by SARS-CoV-2 (Mahalmani et al., 2020) - has brought drastic menaces to our lives; with dual medical and psychological threats to physical and mental health extensively documented since its outbreak (Xiong et al., 2020). On top of health concerns related to the fear of COVID-19, people were faced with severe containment measures including home isolation, travel bans and social distancing and had to navigate uncertainty, hopelessness and loss of control (Shanahan et al., 2020). Prolonged and strict quarantines (Moris & Schizas, 2020) as well as unemployment (Petterson et al., 2020), have led to increased mental distress such as anxiety, depression and post-traumatic stress disorder (PTSD) (Ettman et al., 2020) and maladaptive behaviors like domestic violence or substance use (Gautam et al., 2020; Moreno et al., 2020).
Longitudinal studies consistently reported an overall rise in mental health problems compared to pre-pandemic levels (Li et al., 2020), with meta-analyses documenting PTSD as the most prevalent source of mental distress during COVID-19 (Arora et al., 2022), alongside sleeplessness, behavioral changes and numbness (Serafini et al., 2020). Mental health responses to this disaster were worse for younger adults, female, minority groups and the unemployed (Deng et al., 2021). Images of ill people on social media, dead bodies and the idea of not being able to say goodbye to those dying have intensified social distress (Nations, 2020). Those working on the front lines exposed to high workload and trauma are more susceptible to experience depression, burnout as well as PTSD (The Lancet Infectious Diseases, 2020). A study conducted in Lebanon showed that individuals with a high level of fear of COVID-19 had a lower general well-being (Sfeir et al., 2021), and that the perceived stress in one’s life during the pandemic positively correlated with anxiety, depression, PTSD as well as sleep alterations (El Khoury-Malhame et al., 2022).
Early into the pandemic, population surveys systematically indicated elevated incidences of overall mental distress and particularly PTSD (Di Blasio et al., 2021; Bueno-Notivol et al., 2021). Overall, exposure to COVID-19 increased symptoms of PTSD (80.9%), with around 20–30% of people struggling with severe PTSD, compared to around 10% pre-pandemic (Yunitri et al., 2021). In addition, 96.2% of COVID-19-hospitalized patients scored above cut-off for PTSD symptoms (Boyraz & Legros, 2020). It could be that people infected with COVID-19 and those who lost someone close due to viral infection lived traumatic experience or alternatively, that the situation was excessively worrisome and stressful (Blackman, 2020). The risk for the latter to develop PTSD increases nonetheless, as neurological changes instigated by chronic stress could also lead to mental disorders (Sun et al., 2021). In PTSD, symptoms’ severity is known to bias people’s attention towards threat detection (El Khoury-Malhame et al., 2011) and weaken their ability to disengage from fearful cues to allocate mental resources to problem-solving or pleasurable experiences (Eysenck et al., 2007).
One year into COVID-19 viral threat, follow-up results showed more heterogeneity, with some studies documenting depression, anxiety and PTSD remaining high 10-month into the pandemic (Nikolaidis et al., 2022; Feter et al., 2022; El Zouki et al., 2022) while others in the US and the UK reported levelling off to pre-pandemic levels (Robinson & Daly, 2021, Pierce et al., 2020). Although in some studies post-traumatic symptoms were reported to generally decline since start of the pandemic, they nonetheless continued to be highly prevalent (Chi et al., 2021, Lixia et al., 2022). Yet, despite the adverse persistency of the COVID19 pandemic, Hamam et al. (2021) identified clusters of people who managed to thrive and grow after being exposed to trauma (Bonanno, 2004). This so-called post-traumatic growth (PTG) has been mostly studied in cancer patients (Bussell et al., 2010) and has been associated with positive change experienced as a result of a major life crisis or trauma (Calhoun & Tedeschi, 2014). PTG correlates with increased psychological and physical wellbeing (Park & Helgeson, 2006). Perhaps more surprisingly, studies have documented a positive correlation between PTSD and PTG (Zhou et al., 2015).
To date, numerous studies focused on the negative outcomes of the COVID-19 pandemic on mental health (Chew et al., 2020; Czeisler et al., 2020; Krishnamoorthy et al., 2020; Xiong et al., 2020). Few others, however, evaluated positive outcomes from the pandemic such as PTG (Tamiolaki & Kalaitzaki, 2020; Vazquez et al., 2021; Zhai et al., 2021). Although PTG correlates with overall positive psychological outcomes (Bussell & Naus, 2010), research remains scarce regarding its prevalence during the COVID-19 outbreak. The process of PTG includes deliberate rumination (Calhoun & Tedeschi, 2014), which refers to the individual’s reexamination of the traumatic event in order to further understand the cause and meaning of it (Calhoun et al., 2000). This kind of rumination was found to be a predictor of PTG (Taku et al., 2008; Zhou et al., 2015).
Gratitude has also been documented as a predictor of PTG (Jang & Kim, 2017) and was further shown to mediate the effect of PTSD on PTG (Vieselmeyer et al., 2017; Leppma et al., 2018a). Gratitude is a moral positive emotion that allows oneself to recall and focus on previous positive experiences (Watkins et al., 2003) and allow others to feel appreciated (McCullough et al., 2004). This in turn would increase appreciation of everyday events (McCullough et al., 2002), subsequently facilitating more adaptive coping (Fredrickson, 2004). Individuals who are grateful are generally found to experience higher life satisfaction (Lambert et al., 2009). Grateful respondents for instance showed lower levels of anxiety and depression during and after the lockdowns in the COVID-19 pandemic (Bono et al., 2020; Butler & Jaffe, 2021). A meta-analysis of impact of COVID19 on mental health of more than 72,000 participants in fact suggested lockdowns were not uniformly detrimental and most people show psychological resilience (Prati et al., 2021). Moreover, according to Nguyen et al. (2021) gratitude was positively linked with overall well-being throughout the pandemic, and further increased emotional and mental health in adults with PTSD (Jans-Beken and Wong, 2021).
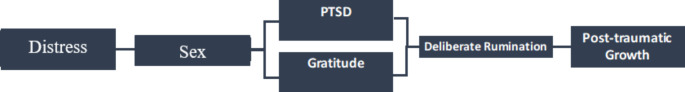
The following conceptual framework (Fig. 1) illustrates the proposed association of PTG with gratitude, PTSD and distress. Initially, elevated incidences of PTSD were reported early on at the onset of the pandemic, and chronicity of the health crisis as well as severity of isolation and quarantine measures in addition to exposure to the deadly COVID-19 virus subsequently increased PTSD symptoms. After experiencing trauma, grateful individuals would invest in gathering or focusing on resources and adapting their self-perceptions to match a more positive approach that would allow them to survive and strive. Attitudes of gratitude in turn reinforce deliberate rumination and positively impacts capacity for PTG. This would protect individuals from the distressing intrusive thoughts and general avoidance that underlie PTSD (Eysenck et al., 2007). In this viewpoint, females are known to engage more in deliberate rumination. According to the founders Tedeschi and Calhoun (2004), PTG sets on a positive psychological framing when faced with challenges. Decades of accumulating research have documented its interplay with a variety of positive psychology concepts (Collier, 2016); leading to a shift in one’s mindset in pursuit of hope and meaning (Schueller & Parks, 2014) and to an increased overall well-being and functioning (Duckworth et al., 2005).
Fig. 1.
Conceptual framework showing the association of PTG with COVID-19 distress, PTSD, gratitude and sex as explained by the theory of positive psychology.
Bueno-Notivol et al., 2021; Collier, 2016; Eysenck et al., 2007 ; Di Blasio et al., 2021; Duckworth et al., 2005; Fredrickson, 2004; Kim & Bae, 2019; Leppma et al., 2018a; Schueller & Parks 2014; Tedeschi & Calhoun, 2004; Tsai et al., 2016; Vishnevsky et al., 2010 and Zhou et al., 2015
People in Lebanon have been faced with many nation-wide adversities on-going at the time of data collection, alongside the COVID-19 pandemic. These include the deteriorating of the socio-political situation, the devaluation of the local currency (World report, 2021), and the catastrophic Beirut port Explosion on August 4, 2020. A recent cross-sectional study in fact showed that an alarming one-third of Lebanese adults had mental distress (Obeid et al., 2020). COVID-19 seemed to worsen stress, anxiety and PTSD levels (El Othman et al., 2021), already elevated in Lebanese pre-pandemic data due the historic political and economic instability in the country (Rayan & Fawaz, 2018; Shaar, 2013). As such, the goal of the current study was to evaluate the factors associated with PTG such as PTSD and gratitude one year into the COVID-19 pandemic in a population faced with accumulating challenges.
Methods
Participants
A total of 252 adults agreed to participate in the study. Demographic data included age, sex, education level, current occupation and employment status, COVID-19 infection status during the pandemic (yes/no), knowing someone who got infected with COVID-19 (yes/no) and knowing anyone close who died because of COVID-19 (yes/no).
Procedure
The study was done in according to the Declaration of Helsinki and approved by the IRB board of LAU (LAU.SAS.MM11.18/May/2020). All participants approved the informed consent before filling questionnaire and demographics on a circulated google link, disseminated via email and other social media platforms on Mar 2021 at the end of 1.5 month of extremely strict lockdown imposed in Lebanon after the dramatic increase in viral incidences after the Christmas Holiday.
Measurements and scales
Three psychological self-filled scales were used in this study to assess the psychological variables and standard cut-off levels for severity were used respectively.
Post-traumatic Growth Inventory (PTGi-SF) was used to measure growth. It is a 10-item self-filled scale to measure favorable outcomes after a traumatic event, including 5 dimensions: relating to others, new possibilities, personal strength, spiritual change and appreciation of life. (Cann et al., 2010). According to Yu et al. (2010) scores at the 60th percentile or higher (≥ 32) indicate probable personal growth (Cronbach’s alpha = 0.90).
Impact of Event Scale (IES-R_22) is one of the most widely-used self-report measures within the trauma literature (Weiss & Marmar, 1997). It is a 22-item scale to evaluate the degree of distress one experiences in response to a given trauma. A cutoff value of > 24 was used as indication of clinical worry and a value of > 33 indicated likely PTSD diagnosis in our study (Cronbach’s alpha = 0.95).
Gratitude Questionnaire (GQ-6) is a 6-item self-report measure designed to quantify individual variances in the proneness to experience gratitude in daily life. Items are rated on a 7-point Likert-type scale (where 1 = strongly disagree and 7 = strongly agree) (McCullough et al., 2002) (Cronbach’s alpha = 0.68).
Subjective distress
Participants were also asked to fill Likert scales ranging from 0 (not at all) to 10 (very much) to indicate subjectively whether their distress resulted from (1) the COVID-19 pandemic, (2) the Beirut Port explosion or (3) the financial devaluation separately. A total distress score was computed by adding the scores derived from the three events.
Statistical analysis
All statistical analyses were conducted using SPSS, version 22. Cronbach’s alpha values were calculated for the scales. The PTG score followed a normal distribution since the skewness (=-0.474) and kurtosis (=-0.561) values varied between − 1 and + 1 (Hair et al., 2021.). Student t test was used to compare means, whereas the Pearson correlations were used to test correlations between PTG scores and the other continuous variables. A linear regression was then conducted to assess associations with PTG, while adjusting for all variables that showed a p < .25 in the bivariate analysis (Bursac et al., 2008). Significance level of p < .05 was set for all tests.
Results
Socio-demographics and personal characteristics
Demographic data for the 252 respondents is represented in Table 1. It is noteworthy to mention that at the time of data collection there was no mention of an efficient vaccine yet. Reports indicate that 42% of participants were infected at some point with COVID-19, as many as 98% of participants knew someone who got infected with the COVID-19 and 63% of them reported losing someone close because of the COVID-19 virus.
Table 1.
Sociodemographic Characteristics of the Participants
| N = 252. | |
|---|---|
| Variable | N (%) |
| Age (in years) | 25.00 ± 8.25 (Mean ± SD) |
| Sex | |
| Male | 71 (28.3%) |
| Female | 180 (71.7%) |
| Education level | |
| Secondary or less | 64 (25.4%) |
| University | 188 (74.6%) |
| Healthcare provider | |
| No | 197 (82.4%) |
| Yes | 42 (17.6%) |
| Employment | |
| No | 157 (62.3%) |
| Yes | 95 (37.7%) |
| COVID-19 infection during the lockdown | |
| No | 146 (57.9%) |
| Yes | 106 (42.1%) |
| Knows anyone who got infected by COVID-19 | |
| No | 5 (2.0%) |
| Yes | 247 (98.0%) |
| Knows anyone close who died from COVID-19 | |
| No | 95 (37.7%) |
| Yes | 157 (62.3%) |
PS: Some values do not add up to the total N because of missing values
PTG, PTSD, gratitude and subjective distress
Mean values of PTSD (IES-R_22), PTG (PTGi-SF) and gratitude (GQ-6) are represented in Table 2. Results show 50% of participants scored above cut-off for PTSD, with 41% having severe symptoms and likely clinical diagnoses (scores above 33 on the scale). Results also show that around 55% of the participants had moderate to high post-traumatic growth.
Table 2.
Values of Different Continuous Variables Used
| Scale | Mean ± SD |
|---|---|
| Impact of events (IES-R_22) | 30.13 ± 19.70 |
| Post-traumatic growth (PTGi-SF) | 30.33 ± 11.65 |
| Gratitude (GQ-6) | 31.88 ± 5.84 |
| Distress from COVID-19 | 6.0 ± 2.7 |
| Distress from the port explosion | 5.6 ± 2.9 |
| Distress from financial deterioration | 7.7 ± 2.6 |
| Total distress from COVID-19, port explosion and financial deterioration | 19.25 ± 6.34 |
Subjective scales further reflect participant’s perception of their source of distress with financial deterioration (mean = 7.7) ranking first, COVID-19-related distress second (mean = 6.0) and distress from the port explosion contributing least (mean = 5.6).
Bivariate correlations
The bivariate correlation matrix highlighting the relationship between studied variables and PTG is illustrated in Table 3. A higher mean PTG was significantly seen in females vs. males (31.53 vs. 27.39; p = .019) and in those who knew anyone who died from COVID-19 (31.97 vs. 27.61; p = .006).
Table 3.
Bivariate Analysis of categorical variables associated with PTG.
| Variable | Post-traumatic growth | |
|---|---|---|
| Mean ± SD | p | |
| Sex | 0.019 | |
| Male | 27.39 ± 12.90 | |
| Female | 31.53 ± 10.95 | |
| Education level | 0.335 | |
| Secondary or less | 29.11 ± 10.79 | |
| University | 30.74 ± 11.93 | |
| Healthcare provider | 0.507 | |
| No | 30.03 ± 12.08 | |
| Yes | 31.36 ± 10.20 | |
| Employment | 0.698 | |
| No | 30.55 ± 11.36 | |
| Yes | 29.96 ± 12.17 | |
| COVID-19 infection during the lockdown | 0.502 | |
| No | 29.90 ± 12.13 | |
| Yes | 30.91 ± 10.99 | |
| Knows anyone who got infected by COVID-19 | 0.835 | |
| No | 31.40 ± 13.83 | |
| Yes | 30.30 ± 11.64 | |
| Knows anyone close who died from COVID-19 | 0.006 | |
| No | 27.61 ± 12.82 | |
| Yes | 31.97 ± 10.60 | |
Numbers in bold indicate significant p-values
Higher impact of events (r = .23), more gratitude (r = .26), and more total distress (r = .19) were significantly associated with more post-traumatic growth.
Multiple regression model
A first linear regression taking the post-traumatic growth score as the dependent variable and each distress score as an independent variable, showed that more gratitude (Beta = 0.52), a higher impact of events (Beta = 0.13), and knowing anyone who died from COVID-19 (Beta = 3.76) were significantly associated with more post-traumatic growth (Table 5, Model 1). When entering the total distress score as an independent variable, the results remained the same (Table 4 and 5, Model 2).
Table 5.
Multivariable analysis: Linear regression (using the ENTER method) with the post-traumatic growth score as the dependent variable
| Beta | β | p | 95% CI | |
|---|---|---|---|---|
| Model 1: Each distress score taken as an independent variable (R2 = 0.181). | ||||
| Impact of events | 0.13 | 0.23 | < 0.001 | 0.06; 0.21 |
| Distress due to COVID-19 | − 0.19 | 0.04 | 0.530 | − 0.39; 0.77 |
| Distress due to the port explosion | 0.38 | 0.10 | 0.153 | − 0.14; 0.91 |
| Distress due to the financial deterioration | − 0.12 | − 0.03 | 0.694 | 0.71; 0.47 |
| Gratitude | 0.52 | 0.26 | < 0.001 | 0.29; 0.76 |
| Sex (females vs. males*) | 2.56 | 0.10 | 0.097 | − 0.47; 5.59 |
| Knows anyone close who died from COVID-19 (yes vs. no*) | 3.76 | 0.16 | 0.008 | 0.99; 6.53 |
| Model 2: Total distress score taken as an independent variable (R2 = 0.181). | ||||
| Impact of events | 0.13 | 0.22 | < 0.001 | 0.06; 0.20 |
| Total distress score | 0.16 | 0.09 | 0.156 | − 0.06; 0.39 |
| Gratitude | 0.54 | 0.27 | < 0.001 | 0.31; 0.78 |
| Sex (females vs. males*) | 2.69 | 0.10 | 0.078 | − 0.30; 5.68 |
| Knows anyone close who died from COVID-19 (yes vs. no*) | 3.78 | 0.16 | 0.008 | 1.02; 6.55 |
*Reference group; Nagelkerke R2 = 16.3%; Beta = unstandardized beta; β = standardized beta; CI = Confidence interval; numbers in bold indicate significant p-values.
Variables entered in the model 1: Impact of events, Individual distress scores, Gratitude, Sex, Knows anyone close who died from COVID-19.
Variables entered in the model 2: Impact of events, Total distress score, Gratitude, Sex, Knows anyone close who died from COVID-19.
Table 4.
Correlations of continuous variables with post-traumatic growth
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Post-traumatic growth | 1 | |||||||
| 2. Age | − 0.03 | 1 | ||||||
| 3. Impact of events (IES) | 0.23*** | − 0.31*** | 1 | |||||
| 4. Gratitude (GQ) | 0.19** | − 0.11 | 0.34*** | 1 | ||||
| 5. Distress due to the COVID-19 pandemic | 0.18** | 0.17** | 0.35*** | 0.73*** | 1 | |||
| 6. Distress due to the port explosion | 0.19** | 0.04 | 0.20** | 0.81*** | 0.37*** | 1 | ||
| 7. Distress due to financial deterioration | 0.07 | 0.06 | 0.25*** | 0.77*** | 0.34*** | 0.45*** | 1 | |
| 8. Total distress (from COVID-19 pandemic, port explosion and financial deterioration) | 0.26*** | 0.05 | − 0.13* | 0.003 | − 0.01 | 0.09 | − 0.09 | 1 |
***p < .001; **p < .01; *p < .05; numbers in the table refer to Pearson correlation coefficients
Discussion
To the best of our knowledge, this is the first study investigating factors and predictors of growth one year into the COVID-19 pandemic, in a context of sociopolitical and economic instability in Lebanon.
First and foremost, our results illustrate a worrisome sustained and intense psychological impact of COVID-19 on the general population in Lebanon with elevated PTSD levels, where 50% of the participants scored above cut-off for PTSD and one third potentially qualifying for a severe PTSD diagnosis. These numbers are quite similar with overall prevalence documented in the first few months of the pandemic in the country (El Khoury-Malhame et al., under review; Obeid et al., 2020). They also resemble increased numbers in a study comparing the effect of the pandemic on Lebanese adults at the second and fourth week of quarantine (Fawaz & Samaha, 2020). In contrast to countries reporting leveling off of COVID-19-induced mental health distress one year into the pandemic, rates in Lebanon might have remained elevated due to the accumulation of socio-political and financial instabilities and the lack of governmental efforts targeting mental health relief (El Khoury et al., 2021). This points to the short and long-term impact of COVID-19 on public health and highlights the need to address potential intricate presentations of PTSD symptomatology as previous research in clinical samples suggest that prolonged exposure to repetitive and cumulative trauma is correlated with more complex forms of PTSD (Cloitre et al., 2011; Karam et al., 2014) and as such points to the necessity to focus on countries with pre-existing national struggles.
Our results mostly show that in spite of those accumulating adversities, growth after trauma is still possible in as many as half of the participants. It seems to be higher when the initial emotional impact is greater, which is in line with previous findings documenting a positive correlation between PTSD and PTG (Jian et al., 2022), and corroborates with reports suggesting heterogeneity of individual responses to major life stressors (Baños et al., 2021). During the COVID-19-pandemic, viral-related fears (Hyun et al., 2021) as well as general worries about the pandemic were surprisingly shown to predict higher scores of PTG (Na et al., 2021). Moreover, higher prevalence of PTG was found among veterans who had PTSD symptoms related to the pandemic (Pietrzak et al., 2021). It seemed that those who have faced resource-gathering obstacles, such as COVID-19 related fear or losing someone to the virus, may have amplified their capacity to overcome hardship (Hyun et al., 2021). In that regard, PTG manifested in those emotionally fueled by adversity but able to mobilize positive resources such as gratitude combined with higher spiritual functionality (such as meaning making after losing someone to COVID-19). Although PTG does not dampen the initial traumatic response underlying the adjustment to the massive unprecedented challenge, it could foster resilience and self-compassion (Jin et al., 2014; Lau et al., 2020; Ikizer et al., 2021).
Our model supports earlier findings that gratitude predicts PTG. We found that participants with higher levels of gratitude show increased capacity for growth during the prolonged COVID-19 pandemic, aligning with previous results reporting that gratitude predicted PTG after one year of an earthquake in China (Zhou et al., 2015). This could be because people who are highly grateful tend to positively find resources in their lives after experiencing trauma and tend to experience positive perceptions of their environments as well as themselves (Fredrickson, 2004). Gratitude was further shown to have a positive impact on PTG, with heightened levels of gratitude reinforcing the influence of deliberate rumination on PTG (Kim & Bae, 2019 Zhou et al., 2015). This specific influence of gratitude-activated deliberate rumination on PTG could play a buffer role in the face of intrusive thoughts of stressors known to be one of the trademarks of PTSD (Leppma et al., 2018a; Tsai et al., 2016). Intrusive rumination which are also included in PTG along with deliberate rumination (Calhoun & Tedeschi, 2014), refers to a cognitive process where individuals focus on the negative perspective of the traumatic event (Nolen-Hoeksema & Davis, 2004). Grateful individuals would engage in cognitive reframing of a traumatic situation or event geared towards meaning making and better understanding and as such, although dwelling on cues related to the trauma might increase symptoms of PTSD, it would provide the cognitive framework needed to facilitate PTG altogether (McCullough et al., 2006; Watkins, 2013).
Lastly, when asked for subjective inputs to rate sources of distress, people first and foremost attributed their mental struggles to the financial deterioration, followed by the COVID-19 pandemic and least to the Beirut port explosion. Hong et al. (2022) had found comparable results with around 50% of their participants being more stressed by the viral pandemic than the explosion (Hong et al., 2022). It has been documented that worsening financials, financial instability and unemployment, contribute to poorer mental health and persistence of PTSD after trauma (Galea et al., 2004) and impairs capacity for growth. From more general perspective, failing to address financial burden and subsequently accumulating adversity might have contributed to the maintenance of mental health symptoms in the Lebanese sample one year into the pandemic, similarly to other countries (Nikolaidis et al., 2022); while addressing perceived financial risks and health concerns might have facilitated the levelling-off of general distress in others (Robinson & Daly, 2021).
Clinical implications
Inasmuch as its traditional focus on signs of psychopathology post-trauma exposure, the scientific community could increase the focus on inherent capacities of some to growth after distress. Clinicians and researchers alike could promote cost-effective cognitive-behavioral tools, such as gratitude, to attempt reducing intrusive rumination and increasing deliberate rumination in order to subsequent boost PTG (Kim & Bae, 2019). In such contexts, cognitive restructuring and mindfulness-based therapies could provide useful resources.
Limitations
These results are to be generalized with caution due to the modest sample size and the selection bias of digitally-literate individuals as the questionnaire were circulated via online platforms. The study did not entail in-person diagnoses due to the quarantine and lockdown restriction. The Cronbach’s alpha value of the gratitude questionnaire was a bit low, though it had shown higher values in previous studies (Watkins et al., 2003). Also, residual confounds might bias some of the findings such as pre-existing psychiatric diagnoses or previous traumatic experiences could also mitigate the overall findings. Yet some studies show that those with prior trauma history might have more realistic appraisals of current difficulties associated with traumas and are less reactive to unsettling PTSD symptoms (Pazderka et al., 2021). Follow-up studies are further needed to monitor levels of PTSD and PTG once the stressors are discontinued including COVID-19 pandemic subsiding and economic inflation stabilizing as people could arguably be currently functioning in survival mode with altered fear circuitry or dysphoric networks (Birkeland & Heir, 2017).
Conclusion
Our findings highlight the capacity of some people to grow after major chronic collective traumas, in unstable socio-political and economic conditions. Women compared to men, those who were faced with the death of a loved one during the COVID-19 pandemic, those who had a higher levels of emotional distress with higher post-traumatic symptoms and also those who had higher levels of gratitude were more likely to exhibit potential for PTG. Future longitudinal studies with national representative samples are needed to better understand the correlation between PTSD, PTG and gratitude and to further factor in additional variables associated with PTG, such as religiosity, coping strategies and resilience.
Authors’ Contributions
MEK and TS contributed to the study conception and design, material preparation and data collection. SH overviewed the statistical analysis and clinical relevance. MEK and MS wrote the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Statements and declarations
No funding was received for conducting this study. The authors have no relevant financial or non-financial interests to disclose. Approval was obtained from the ethics committee of LAU under the reference LAU.SAS.MM11.18/May/2020. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Obtained from all individual participants included in the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Arora, T., Grey, I., Östlundh, L., Lam, K. B. H., Omar, O. M., & Arnone, D. (2022 Mar). The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. Journal Of Health Psychology, 27(4), 805–824. [DOI] [PubMed]
- Baños, R. M., Garcés, J. J., Miragall, M., Herrero, R., Vara, M., & Soria-Olivas, E. (2021). Exploring the heterogeneity and trajectories of positive functioning variables, emotional distress, and post-traumatic growth during strict confinement due to COVID-19.Journal of Happiness Studies,1–26. [DOI] [PMC free article] [PubMed]
- Birkeland MS, Heir T. Making connections: exploring the centrality of posttraumatic stress symptoms and covariates after a terrorist attack. European Journal of Psychotraumatology. 2017;8(sup3):1333387. doi: 10.1080/20008198.2017.1333387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackman JS. A psychoanalytic view of reactions to the coronavirus pandemic in china. The American Journal of Psychoanalysis. 2020;80(2):119–132. doi: 10.1057/s11231-020-09248-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bono, G., Reil, K., & Hescox, J. (2020). Stress and wellbeing in urban college students in the US during the COVID-19 pandemic: Can grit and gratitude help?International Journal of Wellbeing, 10(3)
- Boyraz G, Legros DN. Coronavirus disease (COVID-19) and traumatic stress: probable risk factors and correlates of posttraumatic stress disorder. Journal of Loss and Trauma. 2020;25(6–7):503–522. [Google Scholar]
- Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. International Journal of Clinical and Health Psychology. 2021;21(1):100196. doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):1–8. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussell VA, Naus MJ. A longitudinal investigation of coping and posttraumatic growth in breast cancer survivors. Journal of Psychosocial Oncology. 2010;28(1):61–78. doi: 10.1080/07347330903438958. [DOI] [PubMed] [Google Scholar]
- Butler, J., & Jaffe, S. (2021). Challenges and gratitude: A diary study of software engineers working from home during COVID-19 pandemic. Paper presented at the 2021 IEEE/ACM 43rd International Conference on Software Engineering: Software Engineering in Practice (ICSE-SEIP), 362–363.
- Calhoun LG, Cann A, Tedeschi RG, McMillan J. A correlational test of the relationship between posttraumatic growth, religion, and cognitive processing. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies. 2000;13(3):521–527. doi: 10.1023/A:1007745627077. [DOI] [PubMed] [Google Scholar]
- Calhoun, L. G., & Tedeschi, R. G. (2014). Handbook of posttraumatic growth. Research and practice. Routledge.
- Cann A, Calhoun LG, Tedeschi RG, Taku K, Vishnevsky T, Triplett KN, Danhauer SC. A short form of the posttraumatic growth inventory. Anxiety Stress & Coping. 2010;23(2):127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, Shanmugam GN. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behavior and Immunity. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, X., Huang, L., Hall, D. L., Li, R., Liang, K., Hossain, M. M., & Guo, T. (2021). Posttraumatic stress symptoms among chinese college students during the COVID-19 pandemic: A longitudinal study.Frontiers in Public Health, 9 [DOI] [PMC free article] [PubMed]
- Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress. 2011;24(6):615–627. doi: 10.1002/jts.20697. [DOI] [PubMed] [Google Scholar]
- Collier, L. (2016). Growth after trauma. Why are some people more resilient than others—and can it be taught?. American Psychological Association.
- Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR. Morbidity and mortality weekly report, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed]
- Di Blasi M, Gullo S, Mancinelli E, Freda MF, Esposito G, Gelo OCG, Pazzagli C. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. Journal of Affective Disorders. 2021;284:18–26. doi: 10.1016/j.jad.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., Drakos, A., Zuo, Q. K., & Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res; 301:113863. [DOI] [PMC free article] [PubMed]
- Diseases TLI. The intersection of COVID-19 and mental health. The Lancet Infectious Diseases. 2020;20(11):1217. doi: 10.1016/S1473-3099(20)30797-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duckworth A, Steen TA, Seligman ME. Positive psychology in clinical practice. Annu Rev Clin Psychol. 2005;1:629–651. doi: 10.1146/annurev.clinpsy.1.102803.144154. [DOI] [PubMed] [Google Scholar]
- El-Khoury J, Medawar B. Beirut, Lebanon. Lancet Psychiatry. 2021;8(2):104. doi: 10.1016/S2215-0366(20)30561-7. [DOI] [PubMed] [Google Scholar]
- El Khoury-Malhame M, Reynaud E, Soriano A, Michael K, Salgado-Pineda P, Zendjidjian X, Gellato C, Eric F, Lefebvre MN, Rouby F, Samuelian JC, Anton JL, Blin O, Khalfa S. Amygdala activity correlates with attentional bias in PTSD. Neuropsychologia Jun. 2011;49(7):1969–1973. doi: 10.1016/j.neuropsychologia.2011.03.025. [DOI] [PubMed] [Google Scholar]
- El Khoury-Malhame, M., Boulos, R., Joukayem, E., Rechdane, A., & Sawma, T. (2022). The Psychological Impact of COVID-19 In A Socio-politically Unstable Society: A Cultural Perspective On Sleep And Gratitude In Lebanon. BMC Psychology(Accepted) [DOI] [PMC free article] [PubMed]
- El Othman R, Touma E, El Othman R, Haddad C, Hallit R, Obeid S, Hallit S. COVID-19 pandemic and mental health in lebanon: a cross-sectional study. International Journal of Psychiatry in Clinical Practice. 2021;25(2):152–163. doi: 10.1080/13651501.2021.1879159. [DOI] [PubMed] [Google Scholar]
- El Zouki, C. J., Chahine, A., Mhanna, M., Obeid, S., & Hallit, S. (2022 Aug). Rate and correlates of post-traumatic stress disorder (PTSD) following the Beirut blast and the economic crisis among lebanese University students: a cross-sectional study. Bmc Psychiatry, 5(1), 532. 10.1186/s12888-022-04180-y [DOI] [PMC free article] [PubMed]
- Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. [DOI] [PMC free article] [PubMed]
- Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7(2):336–353. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- Fawaz M, Samaha A. COVID-19 quarantine: post-traumatic stress symptomatology among lebanese citizens. International Journal of Social Psychiatry. 2020;66(7):666–674. doi: 10.1177/0020764020932207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feter N, Caputo EL, Leite JS, Smith EC, Doring IR, Cassuriaga J, Reichert FF. Depression and anxiety symptoms remained elevated after 10 months of the COVID-19 pandemic in southern brazil: findings from the PAMPA cohort. Public Health. 2022;204:14–20. doi: 10.1016/j.puhe.2021.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson, B. L. (2004). Series in affective science. The Psychology of Gratitude.
- Gautam M, Thakrar A, Akinyemi E, Mahr G. Current and future challenges in the delivery of mental healthcare during COVID-19. SN Comprehensive Clinical Medicine. 2020;2(7):865–870. doi: 10.1007/s42399-020-00348-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea, S., Vlahov, D., Tracy, M., Hoover, D. R., Resnick, H., & Kilpatrick, D. (2004). Hispanic ethnicity and post-traumatic stress disorder after a disaster: evidence from a general population survey after September 11, 2001. Annals of epidemiology, 14(8), 520–531. [DOI] [PubMed]
- Hair, J. F. Jr., Hult, G. T. M., Ringle, C. M., & Sarstedt, M. (2021). A primer on partial least squares structural equation modeling (PLS-SEM). Sage publications.
- Hamam AA, Milo S, Mor I, Shaked E, Eliav AS, Lahav Y. Peritraumatic reactions during the COVID-19 pandemic–the contribution of posttraumatic growth attributed to prior trauma. Journal of Psychiatric Research. 2021;132:23–31. doi: 10.1016/j.jpsychires.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong, J., Mreydem, H. W., Abou Ali, B. T., Saleh, N. O., Hammoudi, S. F., Lee, J., Ahn, J., Park, J., Hong, Y., Suh, S., & Chung, S. (2022). Mediation Effect of Self-Efficacy and Resilience on the Psychological Well-Being of Lebanese People During the Crises of the COVID-19 Pandemic and the Beirut Explosion. Frontiers in psychiatry, 12, 733578. 10.3389/fpsyt.2021.733578 [DOI] [PMC free article] [PubMed]
- Hyun S, Wong GTF, Levy-Carrick NC, Charmaraman L, Cozier Y, Yip T, Liu CH. Psychosocial correlates of posttraumatic growth among US young adults during the COVID-19 pandemic. Psychiatry Research. 2021;302:114035. doi: 10.1016/j.psychres.2021.114035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikizer G, Karanci AN, Gul E, Dilekler I. Post-traumatic stress, growth, and depreciation during the COVID-19 pandemic: evidence from turkey. European Journal of Psychotraumatology. 2021;12(1):1872966. doi: 10.1080/20008198.2021.1872966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang H, Kim JS. A meta-analysis on relationship between post-traumatic growth and related variables. Korean Journal of Counseling. 2017;18(5):85–105. [Google Scholar]
- Jans-Beken L, Wong PT. Development and preliminary validation of the existential gratitude scale (EGS) Counselling Psychology Quarterly. 2021;34(1):72–86. [Google Scholar]
- Jian, Y., Hu, T., Zong, Y., & Tang, W. (2022). Relationship between post-traumatic disorder and posttraumatic growth in COVID-19 home-confined adolescents: The moderating role of self-efficacy.Current Psychology,1–10. [DOI] [PMC free article] [PubMed]
- Jin Y, Xu J, Liu D. The relationship between post-traumatic stress disorder and post traumatic growth: gender differences in PTG and PTSD subgroups. Social Psychiatry and Psychiatric Epidemiology. 2014;49(12):1903–1910. doi: 10.1007/s00127-014-0865-5. [DOI] [PubMed] [Google Scholar]
- Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, Bromet EJ. Cumulative traumas and risk thresholds: 12-month PTSD in the world mental health (WMH) surveys. Depression and Anxiety. 2014;31(2):130–142. doi: 10.1002/da.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E., & Bae, S. (2019). Gratitude moderates the mediating effect of deliberate rumination on the relationship between intrusive rumination and post-traumatic growth.Frontiers in Psychology, 2665. [DOI] [PMC free article] [PubMed]
- Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Research. 2020;293:113382. doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert NM, Graham SM, Fincham FD, Stillman TF. A changed perspective: how gratitude can affect sense of coherence through positive reframing. The Journal of Positive Psychology. 2009;4(6):461–470. [Google Scholar]
- Lau, B. H., Chan, C. L., & Ng, S. (2020). Self-compassion buffers the adverse mental health impacts of COVID-19-related threats: Results from a cross-sectional survey at the first peak of hong kong’s outbreak.Frontiers in Psychiatry,1203. [DOI] [PMC free article] [PubMed]
- Leppma M, Mnatsakanova A, Sarkisian K, Scott O, Adjeroh L, Andrew ME, McCanlies EC. Stressful life events and posttraumatic growth among police officers: a cross-sectional study. Stress and Health. 2018;34(1):175–186. doi: 10.1002/smi.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S. W., Wang, Y., Yang, Y. Y., Lei, X. M., & Yang, Y. F. (2020). Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chinese Journal of Child Health, 28(3), 1–9.
- Lixia W, Xiaoming X, Lei S, Su H, Wo W, Xin F, Li K. A cross-sectional study of the psychological status of 33,706 hospital workers at the late stage of the COVID-19 outbreak. Journal of Affective Disorders. 2022;297:156–168. doi: 10.1016/j.jad.2021.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalmani VM, Mahendru D, Semwal A, Kaur S, Kaur H, Sarma P, Medhi B. COVID-19 pandemic: a review based on current evidence. Indian Journal of Pharmacology. 2020;52(2):117. doi: 10.4103/ijp.IJP_310_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough ME, Emmons RA, Tsang J. The grateful disposition: a conceptual and empirical topography. Journal of Personality and Social Psychology. 2002;82(1):112. doi: 10.1037//0022-3514.82.1.112. [DOI] [PubMed] [Google Scholar]
- McCullough ME, Root LM, Cohen AD. Writing about the benefits of an interpersonal transgression facilitates forgiveness. Journal of Consulting and Clinical Psychology. 2006;74(5):887. doi: 10.1037/0022-006X.74.5.887. [DOI] [PubMed] [Google Scholar]
- McCullough ME, Tsang J, Emmons RA. Gratitude in intermediate affective terrain: links of grateful moods to individual differences and daily emotional experience. Journal of Personality and Social Psychology. 2004;86(2):295. doi: 10.1037/0022-3514.86.2.295. [DOI] [PubMed] [Google Scholar]
- Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Carr S. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moris D, Schizas D. Lockdown during COVID-19: the greek success. In Vivo. 2020;34(3 suppl):1695–1699. doi: 10.21873/invivo.11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na PJ, Tsai J, Southwick SM, Pietrzak RH. Factors associated with post-traumatic growth in response to the COVID-19 pandemic: results from a national sample of US military veterans. Social Science & Medicine. 2021;289:114409. doi: 10.1016/j.socscimed.2021.114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nations, U. (2020). Policy brief: COVID-19 and the need for action on mental health.
- Nguyen TM, Le GNH. The influence of COVID-19 stress on psychological well-being among vietnamese adults: the role of self-compassion and gratitude. Traumatology. 2021;27(1):86. [Google Scholar]
- Nikolaidis, A., DeRosa, J., Kass, M., Droney, I., Alexander, L., Di Martino, A., & Paksarian, D. (2022). Heterogeneity in COVID-19 pandemic-induced lifestyle stressors and predicts future mental health in adults and children in the US and UK. Journal of Psychiatric Research. [DOI] [PMC free article] [PubMed]
- Nolen-Hoeksema S, Davis CG. Theoretical and methodological issues in the assessment and interpretation of posttraumatic growth. Psychological Inquiry. 2004;15(1):60–64. [Google Scholar]
- Obeid S, Lahoud N, Haddad C, Sacre H, Akel M, Fares K, Hallit S. Factors associated with depression among the lebanese population: results of a cross-sectional study. Perspectives in Psychiatric Care. 2020;56(4):956–967. doi: 10.1111/ppc.12518. [DOI] [PubMed] [Google Scholar]
- Park, C. L., & Helgeson, V. S. (2006). Introduction to the special section: Growth following highly stressful life events--Current status and future directions. Journal of Consulting and Clinical Psychology, 74(5), 791–796. 10.1037/0022-006X.74.5.791 [DOI] [PubMed]
- Pazderka, H., Brown, M. R., McDonald-Harker, C. B., Greenshaw, A. J., Agyapong, V. I., Noble, S., & Brett-MacLean, P. (2021). Model of post-traumatic growth in newly traumatized vs.retraumatized adolescents. Frontiers in Psychiatry, 1682. [DOI] [PMC free article] [PubMed]
- Petterson, S., Westfall, J. M., & Miller, B. F. (2020). Projected deaths of despair during the coronavirus recession. Well being Trust, 8, 2020.
- Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, McManus S. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak, R. H., Tsai, J., & Southwick, S. M. (2021). Association of symptoms of posttraumatic stress disorder with posttraumatic psychological growth among US veterans during the COVID-19 pandemic.JAMA Network Open, 4(4), e214972. [DOI] [PMC free article] [PubMed]
- Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine. 2021;51(2):201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayan, A., & Fawaz, M. (2018). Cultural misconceptions and public stigma against mental illness among Lebanese university students. Perspectives in psychiatric care, 54(2), 258–265. 10.1111/ppc.12232 [DOI] [PubMed]
- Robinson E, Daly M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the united states: longitudinal evidence from the understanding America study. British Journal of Health Psychology. 2021;26(2):570–587. doi: 10.1111/bjhp.12493. [DOI] [PubMed] [Google Scholar]
- Schueller, S. M., & Parks, A. C. (2014). The science of self-help. European Psychologist,
- Serafini, G., Parmigiani, B., Amerio, A., Aguglia, A., Sher, L., & Amore, M. (2020). The Psychological Impact of COVID-19 on the Mental Health in the General Population, [DOI] [PMC free article] [PubMed]
- Sfeir, M., Akel, M., Hallit, S., & Obeid, S. (2022). Factors associated with general well-being among lebanese adults: The role of emotional intelligence, fear of COVID, healthy lifestyle, coping strategies (avoidance and approach).Current Psychology,1–10. [DOI] [PMC free article] [PubMed]
- Shaar, K. H. (2013). Post-traumatic stress disorder in adolescents in Lebanon as wars gained in ferocity: A systematic review.Journal of Public Health Research, 2(2) [DOI] [PMC free article] [PubMed]
- Shanahan, L., Steinhoff, A., Bechtiger, L., Murray, A. L., Nivette, A., Hepp, U., & Eisner, M. (2020). Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study.Psychological Medicine,1–10. [DOI] [PMC free article] [PubMed]
- Sun L, Sun Z, Wu L, Zhu Z, Zhang F, Shang Z, Wang Y. Prevalence and risk factors for acute posttraumatic stress disorder during the COVID-19 outbreak. Journal of Affective Disorders. 2021;283:123–129. doi: 10.1016/j.jad.2021.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taku K, Calhoun LG, Cann A, Tedeschi RG. The role of rumination in the coexistence of distress and posttraumatic growth among bereaved japanese university students. Death Studies. 2008;32(5):428–444. doi: 10.1080/07481180801974745. [DOI] [PubMed] [Google Scholar]
- Tamiolaki A, Kalaitzaki AE. “That which does not kill us, makes us stronger”: COVID-19 and posttraumatic growth. Psychiatry Research. 2020;289:113044. doi: 10.1016/j.psychres.2020.113044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. ” posttraumatic growth: conceptual foundations and empirical evidence". Psychological Inquiry. 2004;15(1):1–18. [Google Scholar]
- Tsai J, Sippel LM, Mota N, Southwick SM, Pietrzak RH. Longitudinal course of posttraumatic growth among US military veterans: results from the national health and resilience in veterans study. Depression and Anxiety. 2016;33(1):9–18. doi: 10.1002/da.22371. [DOI] [PubMed] [Google Scholar]
- Vazquez C, Valiente C, García FE, Contreras A, Peinado V, Trucharte A, Bentall RP. Post-traumatic growth and stress-related responses during the COVID-19 pandemic in a national representative sample: the role of positive core beliefs about the world and others. Journal of Happiness Studies. 2021;22(7):2915–2935. doi: 10.1007/s10902-020-00352-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieselmeyer J, Holguin J, Mezulis A. The role of resilience and gratitude in posttraumatic stress and growth following a campus shooting. Psychological Trauma: Theory Research Practice and Policy. 2017;9(1):62. doi: 10.1037/tra0000149. [DOI] [PubMed] [Google Scholar]
- Vishnevsky T, Cann A, Calhoun LG, Tedeschi RG, Demakis GJ. Gender differences in self-reported posttraumatic growth: a meta-analysis. Psychology of Women Quarterly. 2010;34(1):110–120. [Google Scholar]
- Watkins, P. C. (2013). Gratitude and the good life: toward a psychology of appreciation. Springer.
- Watkins PC, Woodward K, Stone T, Kolts RL. Gratitude and happiness: development of a measure of gratitude, and relationships with subjective well-being. Social Behavior and Personality: An International Journal. 2003;31(5):431–451. [Google Scholar]
- Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event Scale-Revised. In J. P. Wilson and T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). New York: The Guilford Press.
- World report (2021). World report 2021: Lebanon. human rights watch. Retrieved from https://www.hrw.org/world-report/2021/country‐chapters/lebanon
- Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, Majeed A. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X, Lau JT, Zhang J, Mak WW, Choi KC, Lui WW, Chan EY. Posttraumatic growth and reduced suicidal ideation among adolescents at month 1 after the sichuan earthquake. Journal of Affective Disorders. 2010;123(1–3):327–331. doi: 10.1016/j.jad.2009.09.019. [DOI] [PubMed] [Google Scholar]
- Yunitri N, Chu H, Kang XL, Jen H, Pien L, Tsai H, Chou K. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: a meta-analysis. International Journal of Nursing Studies. 2021;126:104136. doi: 10.1016/j.ijnurstu.2021.104136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai, H., Li, Q., Hu, Y., Cui, Y., Wei, X., & Zhou, X. (2021). Emotional creativity improves posttraumatic growth and mental health during the COVID-19 pandemic. Frontiers in Psychology, 12, 600789. 10.3389/fpsyg.2021.600798 [DOI] [PMC free article] [PubMed]
- Zhou X, Wu X, Chen J. Longitudinal linkages between posttraumatic stress disorder and posttraumatic growth in adolescent survivors following the wenchuan earthquake in china: a three-wave, cross-lagged study. Psychiatry Research. 2015;228(1):107–111. doi: 10.1016/j.psychres.2015.04.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.