Abstract
Telemedicine is becoming increasingly important to address the shortage of gastrointestinal surgeons and disparities in domestic and international treatment outcomes for patients with colorectal cancer. The development of a low-latency communication system using existing communication infrastructure (shared internet access: SIA) is necessary to promote the use of telemedicine. The aim of this study was to develop a low-latency communication system using SIA. We conducted an experiment between Sapporo and Tokyo using an ultralow-latency communication system for remote medical education (TELEPRO®). The latency was measured using 2000 annotations from a monitor in Sapporo, which confirmed a median latency of 27.5 ms. A low-latency communication system based on SIA with latency lower than the maximum allowable latency for telemedicine was developed successfully.
Keywords: Telemedicine, Latency, SDGs
Issues with surgical care have been raised in recent years, domestically and internationally. First, there is a growing shortage of surgeons in Japan, especially in regional areas where the number of surgeons per population is much lower than in urban areas [1]. National and international disparities in cancer treatment outcomes for colon and rectal cancers have become evident, and survival rates are particularly low in countries with inadequate medical services [2, 3]. Furthermore, the number of female surgeons has been increasing worldwide [4] and the work-life balance of surgeons has changed. These international trends and problems must be addressed to achieve efficient and disparate surgical care.
The Sustainable Development Goals (SDGs) are 17 international goals set to achieve a sustainable and better world by 2030. They include overcoming poverty and hunger, protecting the global environment, and eliminating discrimination [5]. Six of these goals (Goal 3: Good Health and Well-Being; Goal 4: Quality Education; Goal 5: Gender Equality; Goal 8: Decent Work and Economic Growth; Goal 10: Reduced Inequality; Goal 17: Partnerships for the Goals) are necessary for the future development of surgical medicine and “telemedicine” has become a focus of attention in the Society 5.0 initiative [5]. As the novel coronavirus disease 2019 (COVID-19) pandemic has restricted mobility, travel times have been eliminated and the CO2 emissions associated with travel have been reduced. The idea of “carbon neutrality,” which is important for Society 5.0 and the aforementioned SDGs, highlights the importance of telemedicine.
The realization of telemedicine has the following advantages:
Correcting the disparity in surgical skills between facilities and promoting standardization of surgery.
Promoting the implementation of minimally invasive surgery (MIS) worldwide, especially in countries with limited medical industries.
Eliminating long travel times.
Supporting the career paths of female surgeons.
Contributing to carbon neutrality to achieve the SDGs.
Currently, the functionality of telemedicine is affected by issues related to shared internet access (SIA), which exhibits a noticeable latency and is not clinically applicable [6]. The development of a low-latency communication system using existing communication infrastructure is mandatory for promoting the use of telemedicine. Thus, the aim of this study was to develop a low-latency communication system using SIA.
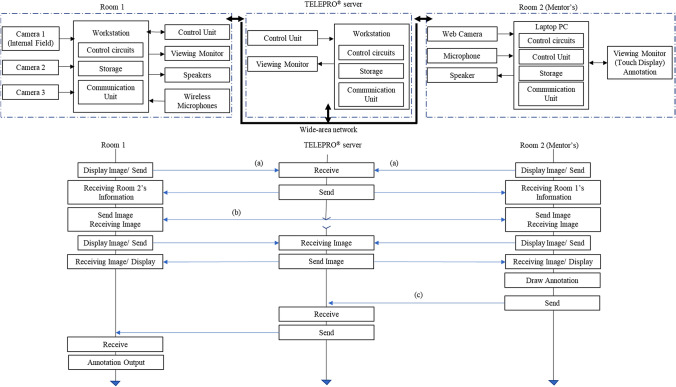
We conducted an experiment involving 2 remote locations using an ultralow-latency communication system for remote medical education (TELEPRO®, Tenmashimon Co. Ltd., Tokyo, Japan; Patent pending in Japan). The entire system is based on room 1 and room 2 (mentor’s room), which are connected to a wide area network through the internet via the TELEPRO® server (Fig. 1). The internet connection was not dedicated internet access (DIA), but SIA with a maximum transmission speed of 100 Mbps. It was not strengthened, to allow it to be widely used in the future, even in facilities where DIA lines cannot be installed for financial, geographical, and infrastructural reasons. From a remote location, the mentor can communicate using a microphone, speaker, and web camera, in addition to annotation lines drawn on a touch panel monitor that shows images with audio (Fig. 1). Camera images from room 1 and room 2 are received and connected to the TELEPRO® server (indicated by (a) in Fig. 1) to achieve interactive communication between 2 locations. Once 2-way communication is established, all further video transmissions are performed without passing through the server (indicated by (b) in Fig. 1) to reduce latency and the load on the servers, unless the mentor begins to draw annotation lines (indicated by (c) in Fig. 1). The server also records the latency between the two remote locations by detecting the touch of the annotation pen on the surface of the touch monitor.
Fig. 1.
TELEPRO® structure and initiation process of interactive communication. The entire system is based on 2 remote locations connected to a wide area network (WAN) through the internet via the TELEPRO® server. Room 1: Precision Tower 5820®. The CPU used in the experiment was Intel® Xeon® W-2245, the GPU was NVIDIA Quadro RTX 4000, and the memory was 64 GB. Room 2: HP ENVY Laptop 15-ep0xxx. The CPU used in the experiment was Intel® Core™ i7-10750H, the GPU was NVIDIA GeForce GTX 1660, and the memory was 16 GB. The refresh rate of the monitor was 60 Hz
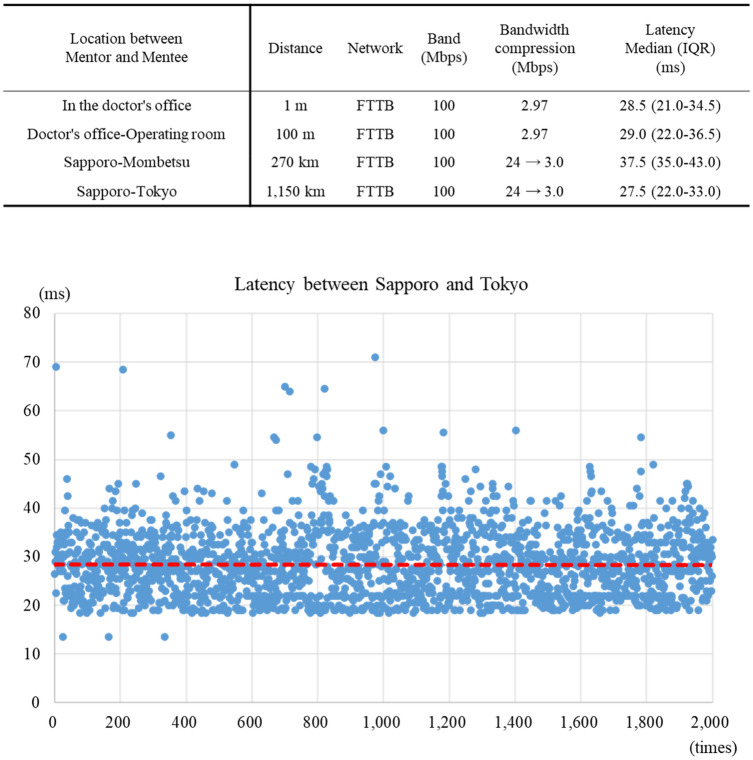
First, we measured the latency by arranging the PCs at 1 m intervals in the medical office and found the median latency to be 28.5 ms. We then gradually increased the distance between the 2 points. The median latency between the doctor’s office and the operating room (100 m) was 29.0 ms, and that between Sapporo Medical University and the Kouiki Mombetsu Hospital (270 km) was 37.5 ms (Fig. 2). A communication experiment was conducted between a doctor’s office at Sapporo Medical University and an office at Tenmashimon Co. Ltd., in Tokyo, Japan. We measured the latency by completing 2000 annotations using a monitor in Sapporo and found the median latency to be 27.5 ms (Fig. 2).
Fig. 2.
Scatter plot of the latency time between Sapporo and Tokyo. The latency was measured using 2000 annotations from a monitor in Sapporo. The median latency was 27.5 ms (red dashed line). Vertical axis: Latency (ms); Horizontal axis: Annotation number (times). FTTB Fiber to the building, IQR Interquartile Range
In telemedicine processes, a latency of up to 200 to 250 ms is generally considered acceptable, whereas a longer latency might be a major obstacle [7–9]. One of the main purposes of telemedicine is to improve medical education and services in remote areas such as small islands, sparsely populated villages, and other locations that cannot be accessed easily. SIA must be utilized in these areas as their communication infrastructure for telemedicine is typically lacking. Therefore, cost-effective communications systems may be achieved using existing network environments. Facilitating low-latency communications over existing SIA circuits will promote the implementation of telemedicine.
In this study, we achieved a median latency of 27.5 ms during communication using an SIA. This represents a communication speed approximately 6–7 times less than the acceptable latency range, which is within 200 to 250 ms. The results of our study suggest that latency may be distance-independent. The mechanism that enables low-latency communications allows all further video transmissions to be performed without passing through the server to reduce latency, whereby the load on the servers after 2-way communication is established. This system is expected to address the “latency” issue of telemedicine.
Telemedicine is classified into categories such as teleproctoring, teleconference, and teleimaging, among which teleproctoring represents the most demanding application of technology to clinical practice. Teleproctoring is expected to become an incentive for young surgeons to work in rural areas, as they can continue to receive surgical education and support from supervisors at core facilities while engaging in community medicine [10]. The system presented in this study denotes the potential practical application of such communications systems in the field of surgery.
This study has several limitations. First, although low-latency communication was achieved, this system is acceptable only for small 1:1 communications and the latency measured also varies. If it is to be applied to future larger-scale communications, it is important to expand the bandwidth and stability of communications to withstand this issue and to develop network infrastructure at the national level. Second, system installation of equipment is necessary in the core hospitals of each medical region. The other limitations relate to personal information protection and responsibility, for which legal advice is needed. With the use of electronic systems, confidentiality becomes an issue and special measures must be taken to prevent the improper communication of medical data [11]. In the event of a serious accident, such as intraoperative complications or patient death, it is necessary to decide whether the responsibility lies with the mentor or mentee, as well as with the robot operator or robot owner [11].
In conclusion, the foundation for a communication system based on SIA with a latency lower than the maximum allowable latency for telemedicine has been established. In this study, we demonstrated the use of the TELEPRO® system, which can be utilized, not only domestically, but also internationally, as evidenced by the experiments we conducted between Sapporo and Tokyo.
Abbreviations
- SDGs
Sustainable Development Goals
- COVID-19
Novel coronavirus disease 2019
- MIS
Minimally invasive surgery
- SIA
Shared internet access
Author contributions
TK, KO, KO, AH, MM, EA, YS, MI, RM, TI, TN, and IT designed this study. TK, KO, KO, AH, MM, and IT wrote the manuscript. All authors have read and approved the final manuscript.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The dataset supporting our conclusions is included within the article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
TK, KO, KO, AH, MM, EA, YS, MI, RM, TI, TN, and IT have no financial disclosures relevant to this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ministry of Health, Labour and Welfare [internet]. Japan: Ministry of Health, Labour and Welfare [updated Mar 2022]. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/index.html.
- 2.Allemani C, Matsuda T, Di Carlo VD, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward ZJ, Scott AM, Hricak H, Abdel-Wahab M, Paez D, Lette MM, et al. Estimating the impact of treatment and imaging modalities on 5-year net survival of 11 cancers in 200 countries: a simulation-based analysis. Lancet Oncol. 2020;21:1077–1088. doi: 10.1016/S1470-2045(20)30317-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.OECD Health Statistics 2022 [internet]. France: OECD org [updated Oct 2022]. Available from: https://www.oecd.org/health/health-data.htm.
- 5.Innovation for SDGs-Road to society 5.0- [internet]. Japan: Keidanren Japan Business Federation [updated Jul 2018]. Available from: https://www.keidanren.or.jp/en/policy/2018/059_casestudy.pdf.
- 6.Mitsuno D, Hirota Y, Akamatsu J, Kino H, Okamoto T, Ueda K. Telementoring demonstration in craniofacial surgery with hololens, skype, and three-layer facial models. J Craniofac Surg. 2019;30:28–32. doi: 10.1097/SCS.0000000000004899. [DOI] [PubMed] [Google Scholar]
- 7.Kim T, Zimmerman PM, Wade MJ, Weiss CA., III The effect of delayed visual feedback on telerobotic surgery. Surg Endosc. 2005;19:683–686. doi: 10.1007/s00464-004-8926-6. [DOI] [PubMed] [Google Scholar]
- 8.Xu S, Perez M, Yang K, Perrenot C, Felblinger J, Hubert J. Determination of the latency effects on surgical performance and the acceptable latency levels in telesurgery using the dV-Trainer® simulator. Surg Endosc. 2014;28:2569–2576. doi: 10.1007/s00464-014-3504-z. [DOI] [PubMed] [Google Scholar]
- 9.Korte C, Nair SS, Nistor V, Low TP, Doarn CR, Schaffner G. Determining the threshold of time-delay for teleoperation accuracy and efficiency in relation to telesurgery. Telemed J E Health. 2014;20:1078–1086. doi: 10.1089/tmj.2013.0367. [DOI] [PubMed] [Google Scholar]
- 10.Hakamada K, Mori M. The changing surgical scene: from the days of billroth to the upcoming future of artificial intelligence and telerobotic surgery. Ann Gastroenterol Surg. 2021;5:268–269. doi: 10.1002/ags3.12466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Săceanu SM, Angelescu C, Valeriu S, Patrașcu A. Telesurgery and robotic surgery: ethical and legal aspect. J Commun Med Health Educ. 2015;5:355. doi: 10.4172/2161-0711.1000355. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting our conclusions is included within the article.