Abstract
Objectives
We set out to determine the accuracy of the interRAI Emergency Department (ED) Screener in predicting the need for detailed geriatric assessment in the ED. Our secondary objective was to determine the discriminative ability of the interRAI ED Screener for predicting the odds of discharge home and extended ED length of stay (>24 hours).
Methods
We conducted a multiprovince prospective cohort study in Canada. The need for detailed geriatric assessment was determined using the interRAI ED Screener and the interRAI ED Contact Assessment as the reference standard. A score of ≥5 was used to classify high‐risk patients. Assessments were conducted by emergency and research nurses. We calculated the sensitivity, positive predictive value, and false discovery rate of the interRAI ED Screener. We employed logistic regression to predict ED outcomes while adjusting for age, sex, academic status, and the province of care.
Results
A total of 5629 older ED patients across 11 ED sites were evaluated using the interRAI ED Screener and 1061 were evaluated with the interRAI ED Contact Assessment. Approximately one‐third of patients were discharged home or experienced an extended ED length of stay. The interRAI ED Screener had a sensitivity of 93%, a positive predictive value of 82%, and a false discovery rate of 18%. The interRAI ED Screener predicted discharge home and extended ED length of stay with fair accuracy.
Conclusion
The interRAI ED Screener is able to accurately and rapidly identify individuals with medical complexity. The interRAI ED Screener predicts patient‐important health outcomes in older ED patients, highlighting its value for vulnerability screening.
Keywords: emergency department, frailty, geriatrics, interRAI, screening, vulnerability
1. INTRODUCTION
1.1. Background
Emergency departments (EDs) act as a primary portal into local hospital systems and are uniquely situated to positively influence the healthcare trajectories of older patients. 1 Older adults contribute a disproportionately high rate of overall and urgent ED visitation, lengthier ED stays, and greater resource use (eg, radiography, laboratory studies) when compared with younger counterparts. 2 Atypical presentations and complex medical and psychosocial histories further complicate emergency management and increase the risk for adverse health events in older ED patients. 3 To identify and support high‐risk older adults, geriatric ED guidelines and recommendations emphasize the need for proactive and targeted screening of at‐risk older ED patients who may benefit from additional geriatric assessment and resources. 1 , 4 , 5 Although the Comprehensive Geriatric Assessment (CGA) is the gold standard for evaluating older adults, it is resource intensive and may be best targeted for high‐risk patients during hospitalization or following ED discharge. 6 High patient volumes, medical acuity, and time‐sensitive quality measures are factors likely to inhibit or delay the completion of an ED‐based CGA.
1.2. Importance
Vulnerability and frailty screeners are increasingly incorporated in ED triage and treatment areas to support clinical decision‐making regarding geriatric complexity and the need for further detailed assessment. 6 , 7 This multistage approach is thought to be ideal when aiming to identify and support the most vulnerable ED patients, whereby screener results can inform the need for additional geriatric evaluation. 6 The interRAI ED Assessment System uses a staged assessment strategy. The interRAI ED Screener score is used to pre‐emptively gauge which individuals are most likely to benefit from additional detailed geriatric assessment interventions, including assessment using the interRAI ED Contact Assessment. 8 Both the interRAI ED Screener and ED Contact Assessment report the Assessment Urgency Algorithm, a prognostic model specifically purposed to identify high‐risk older ED patients who may benefit from a CGA after their ED visit. 8
1.3. Goals of this investigation
We set out to determine the sensitivity, positive predictive value, and false discovery rate of the interRAI ED Screener when aiming to delineate which older ED patients have the greatest need for a CGA after emergency care when compared against the interRAI ED Contact Assessment as a reference standard. Our secondary objective was to determine the discriminative ability of the interRAI ED Screener when predicting the odds of discharge home and an extended ED length of stay, 2 patient‐centered health outcomes.
2. METHODS
2.1. Study design and setting
We conducted a prospective multisite cohort study in 11 ED sites across three provinces in Canada (Ontario, Quebec, and Newfoundland). Among the 11 sites, six were academic‐affiliated centers. We purposely recruited small and mid‐sized community hospitals that were not academic centers to ensure diversity in the participating organizations. We consecutively enrolled patients aged 65 years and older who presented to the ED during predefined study enrollment periods. The Strengthening the Reporting of Observational Studies in Epidemiology statement was used to guide the reporting of this study. 9 Ethics approval was obtained from the research ethics boards of all participating hospital sites and from the University of Waterloo.
The Bottom Line
The interRAI Emergency Department Screener is a tool to predict the need for geriatric assessment. The screener is completed in <2 minutes and can predict patient‐important outcomes, including discharge home and emergency department length of stay.
2.2. Selection of study participants
We identified older ED patients using ED rosters at the start of hospital‐specific day shifts. The vast majority of the older patients recruited for the study were recruited during daytime hours 7am ‐ 7pm, when older adults are more likely to present for emergency care. 10 Triage nurses flagged patients for study exclusion if they were expected to die within 24 hours of ED presentation, were medically unstable, or could not speak English or French. We obtained consent to participate from the patient or their substitute decision‐maker in accordance with standard practices.
2.3. Measurements
We provided standardized training on geriatric assessment to emergency nurses or research assistants in all participating institutions on the interRAI ED Screener and ED Contact Assessment, excluding institutions located in Quebec, which elected to use trained research nurses. Training included a several‐hour coaching session with all assessors and the study site team leads on how to use the interRAI ED Assessment System and any supplementary software. Research staff and clincians external to the study were not trained on how to interpret or use the interRAI instruments. Site K was the only ED outside of Quebec that elected to use research nurses.
Study assessors collected demographic and baseline assessments and undertook the interRAI ED Screener and ED Contact Assessments. Vulnerability screening was completed with the interRAI ED Screener during ED triage or within a few hours of ED presentation. After completion of the interRAI ED Screener, the interRAI ED Contact Assessment was completed in the clinical treatment area of the ED before emergency disposition.
We derived an Assessment Urgency Algorithm score for each patient using the interRAI ED Screener results. Assessors were trained to approach patients who received an interRAI ED Screener score ≥4 for further evaluation with the interRAI ED Contact Assessment when possible. Data from the interRAI ED Screener and ED Contact Assessment were not made available to the clinical staff. Thus, risk scores from the instruments did not influence emergency management pathways or clinical decision‐making.
The interRAI ED Contact Assessment is a brief assessment and a standardized clinical decision support tool to inform emergency care, discharge planning, and referral decision‐making in ED. 8 This instrument has clinical items that assess patient condition, performance, and capacity across various domains, including physical function, cognition, comprehension, mood, falls, nutritional risk, pain, and dyspnea. 8 The items of the interRAI ED Contact Assessment have established content validity in acute care, 11 high interrater reliability, 12 , 13 and high predictive validity across a series of outcomes in the ED setting. 14 , 15 , 16
The Assessment Urgency Algorithm included in the interRAI ED Screener and Contact Assessment includes questions on activities of daily living, cognitive skills for daily decision making, self‐rated mood and health, caregiver distress, labile medical condition, and dyspnea. 8 The scoring algorithm is sequenced and adapted to prior item responses, although most high‐risk persons can be identified with just a few screening questions. 8 The Assessment Urgency Algorithm reports a score from 1 to 6, with higher scores indicating a priority need for a CGA after emergency care. Any functional or cognitive impairment automatically classifies the patient as a score of ≥4, with priority further determined by indicators of caregiver distress, mood, or difficulties with personal hygiene.
Prior work has validated the prognostic utility of the Assessment Urgency Algorithm and its association with mortality, hospital admissions, lengthy hospital stays, and the need for long‐term care services (ie, nursing or retirement home placement) in medically complex older ED and home‐care patients. 17 , 18 , 19 The Assessment Urgency Algorithm is readily available for public and hospital use via the interRAI ED Screener, a free mobile application that can be downloaded on mobile phones and tablets (www.interRAI.org).
2.4. Outcomes
We elected to examine the Assessment Urgency Algorithm score assigned by the interRAI ED Contact Assessment as the primary outcome of interest and reference standard when determining which patients have the greatest need for a CGA after ED care. An Assessment Urgency Algorithm score of 5 or 6 using either instrument indicates a patient in greatest need of a CGA. 8 Therefore, we dichotomized the Assessment Urgency Algorithm values provided by both the interRAI ED Screener and ED Contact Assessment in this manner to facilitate diagnostic measurement.
A total of 2 informative and patient‐important outcomes were used to determine the prognostic value of the interRAI ED Screener,—discharge home and ED length of stay. 20 , 21 , 22 We assigned a “discharge home” status to any patient who was discharged from the ED directly to their baseline place of residence. An extended ED length of stay was defined as an ED length of stay >24 hours. This time metric is commonly used in ED research of older persons and conveniently represents the top quartile of the length‐of‐stay data. 23 , 24 , 25 , 26 ED registration time was used as the point of reference when determining ED length of stay.
2.5. Analysis
We reported descriptive statistics of all baseline characteristics using general measures of frequency and central tendency. Cross‐tabulations were created to facilitate the calculation of sensitivity, positive predictive value, and false discovery rate for the interRAI ED Screener. We then undertook binary logistic regression to determine the adjusted associations between the interRAI ED Screener score and patient outcomes after adjusting for patient age, sex (male or female [reference]), province (Quebec or Ontario [reference]), and academic status of the treating institution (non‐academic center [reference]). Participants from Newfoundland are missing from predictive analytics, as they provided no ED disposition data.
We conducted a post‐hoc subgroup analysis to evaluate and compare diagnostic measures between the 3 provinces. We also conducted a post‐hoc sensitivity analysis to determine if diagnostic measures were robust to the removal of participants from site K for the Ontario analysis, as this was the non‐Quebec site that elected to use research assistants, as opposed to registered nurses for data collection. Concordance (c) statistics and the corresponding confidence intervals (CIs) are reported for all models. Cases with missing data were deleted in each analysis. Data were managed and analyzed using the stats, psych, and pROC packages in R (version 4.0.0).
3. RESULTS
3.1. Study participant and visit characteristics
A total of 5629 older ED patients across 11 ED sites were evaluated using the interRAI ED Screener. The mean age of the sample was 84 years (standard deviation [SD] = 5.8), and the majority of patients were women (57%). The mean length of stay for participants was 19.2 hours (SD = 12.6). The mean time of interRAI ED Screener completion was 1.9 minutes (SD = 1.2). Table 1 displays the patient characteristics for all patients evaluated with the interRAI ED Screener, and characteristics stratified across differing interRAI ED Screener thresholds can be found in Tables S1 and S2. The proportion of missing data for the interRAI ED Screener cohort was approximately 18% and primarily driven by missing age (42%) and length of stay data (67%) rather than assessment data. These data can be found in Table S3.
TABLE 1.
Baseline characteristics for 5629 older ED patients evaluated with interRAI ED Screener
| Variable | n (%) |
|---|---|
| Age, years a | 84 (5.8) |
| Sex, female | 2432 (57) |
| Daytime presentation b | 4733 (85.9) |
| Assessment Urgency Algorithm Score | |
| 1 (least urgent) | 1149 (20.4) |
| 2 | 325 (5.8) |
| 3 | 1175 (20.9) |
| 4 | 455 (8.1) |
| 5 | 315 (5.6) |
| 6 (most urgent) | 2210 (39.2) |
| Length of interRAI ED Screener evaluation, minutes a | 1.9 (1.2) |
| Length of ED stay, hours a | 19.2 (12.6) |
Abbreviation: ED, emergency department.
Data reported as mean (standard deviation).
Day shift was classified as 7am to 7pm
A total of 1061 patients were further evaluated using the interRAI ED Contact Assessment. The proportion of missing data in this cohort, excluding ED disposition data, was <1%. The age and sex distributions between those evaluated with the interRAI ED Screener and ED Contact Assessment were similar, with age slightly higher in the interRAI ED Contact Assessment group. Most patients evaluated with the interRAI ED Contact Assessment received a high‐risk Assessment Urgency Algorithm score of 5 or 6 (88%) from the interRAI ED Screener and a high‐acuity Canadian Triage Acuity Scale score of ≤3 (90%), indicating a need for urgent or emergent care. Figure 1 displays a flow diagram of patients who received the interRAI ED Screener and the ED Contact Assessment. Table 2 describes the presence of geriatric syndromes in those assessed with the interRAI ED Contact Assessment.
FIGURE 1.
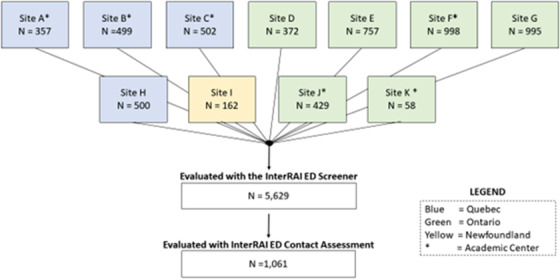
Patient flow diagram. ED, emergency department
TABLE 2.
Baseline characteristics for 1061 older ED patients (65 years and older) evaluated with the interRAI ED Contact Assessment
| Variable | interRAI ED Screener, n (%) | interRAI ED Screener, n (%) | |
|---|---|---|---|
| Score = 4 | Scores = 5–6 | ||
| n (%) | N = 71, 6.7% | N = 938, 88.4% | |
| Age, years a | 85.4 (6.1) | 86.5 (5.8) | 85.3 (6.1) |
| Sex, female | 613 (57.8) | 20 (28.2) | 399 (42.5) |
| Lives alone | 462 (43.5) | 39 (54.9) | 402 (42.9) |
| Caregiver distress b | 501 (47.2) | 9 (12.6) | 484 (51.6) |
| Cognitive impairment c | 442 (41.7) | 22 (31) | 403 (43) |
| Acute change in mental status d | 252 (23.8) | 10 (14.1) | 232 (24.7) |
| ADL impairment | |||
| Bathing | 643 (60.6) | 42 (59.1) | 590 (62.9) |
| Personal hygiene | 329 (31) | 8 (11.2) | 318 (33.9) |
| Dressing lower body | 410 (38.6) | 17 (23.9) | 390 (41.6) |
| Locomotion | 215 (20.3) | 11 (15.4) | 203 (21.6) |
| Independent ADL | |||
| Difficulty with medications e | 579 (54.5) | 24 (33.8) | 540 (57.6) |
| Difficulty with stairs f | 643 (60.6) | 42 (59.2) | 590 (62.8) |
| Impaired comprehension g | 87 (8.2) | 3 (4.2) | 83 (89) |
| Conditions and symptoms | |||
| Poor self‐reported health h | 255 (24) | 19 (26.7) | 227 (24.2) |
| Symptoms of a mood disorder i | 260 (24.5) | 23 (32.4) | 227 (24.2) |
| Hallucinations or delusions | 87 (8.2) | 3 (4.2) | 83 (8.8) |
| Any falls in the past 90 days | 519 (48.9) | 26 (36.7) | 466 (49.7) |
| Traumatic injury | 204 (19.2) | 12 (16.9) | 179 (19.1) |
| Daily or severe pain j | 496 (46.7) | 36 (50.7) | 436 (46.4) |
| Dyspnea k | 392 (36.9) | 29 (40.8) | 350 (37.3) |
| Decrease food intake or weight loss l | 457 (43.1) | 40 (56.3) | 391 (41.7) |
| Urgent Triage Score, CTAS ≤3 | 950 (89.5) | 59 (83.1) | 844 (90) |
| High‐risk AUA score, 5 or 6 | 830 (78.3) | 32 (45.1) | 773 (82.4) |
| Province | |||
| Ontario | 853 (80.4) | 20 (28.1) | 784 (83.5) |
| Québec | 172 (16.2) | 49 (69) | 32 (3.4) |
| Newfoundland | 36 (3.4) | 2 (2.8) | 122 (13) |
Abbreviations: ADL, activities of daily living; AUA, Assessment Urgency Algorithm; CTAS, Canadian Triage Acuity Scale; ED, emergency department.
Data are reported as mean (standard deviation).
Primary informal helper(s) expresses feelings of distress, anger, or depression.
Modified independent or any impairment in making decisions regarding tasks of daily living.
Acute change in mental status from person's usual functioning (eg, restlessness, lethargy, difficult to arouse, altered environmental perception).
Difficulty remembering to take medicines, opening bottles, taking correct drug dosages, giving injections, or applying ointments.
Supervision or the need for any assistance while walking a full flight of stairs (12–14 stairs).
Sometimes, rarely, or never understands direct communication.
When asked, “In general, how would you rate your health?” Person responds “Poor.”
When asked, patient reports feeling sad, depressed, hopeless, anxiousness, or anhedonia.
Pain that is excruciating or daily in past 3 days.
Dyspnea at rest or present when performing normal day‐to‐day activities.
3.2. Main results
Table 3 displays a cross‐tabulation of all patients assessed with both instruments. Most patients received a high‐risk Assessment Urgency Algorithm score of 5 or 6 using both the interRAI ED Screener and ED Contact Assessment (73%). Using this cut‐off, the sensitivity of the interRAI ED Screener was determined to have a sensitivity of 93%, a positive predictive value of 82%, and a false discovery rate of 18%. The raw data and cross‐tabulation of the interRAI ED Screener and ED Contact Assessment in their full forms can be found in Table S4.
TABLE 3.
Comparison of high‐risk assessment between 1061 older ED patients assessed with the interRAI ED Screener and Contact Assessment
| interRAI ED Contact Assessment | |||
|---|---|---|---|
| interRAI ED Screener | High risk, AUA 5–6 | Low to medium risk, AUA 1–4 | Total |
| High risk, AUA 5–6 | 773 (72.9) | 165 (15.6) | 938 |
| Low to medium risk, AUA 1–4 | 57 (5.4) | 66 (6.2) | 123 |
| 830 | 231 | 1061 | |
Abbreviations: AUA, Assessment Urgency Algorithm; ED, emergency department. Data reported as frequencies and proportions.
Table 4 displays the subgroup analysis of diagnostic measures across the provinces. The sensitivity and false discovery rate were highest for participants evaluated in Ontario, whereas the positive predictive value was highest for Newfoundland (91%) followed by Quebec (87%). A sensitivity analysis of diagnostic evaluation in Ontario, excluding site K, found the sensitivity to be 94%, positive predictive value to be 84%, and the false discovery rate to be 16%, similar to the primary inclusive model.
TABLE 4.
Subgroup analysis of diagnostic measures across 3 Canadian provinces
| Province | |||
|---|---|---|---|
| Diagnostic measure |
Ontario (N = 853) |
Quebec (N = 172) |
Newfoundland (N = 36) |
| Sensitivity | 95% | 84% | 83% |
| Positive predictive value | 83% | 87% | 91% |
| False discovery rate | 17% | 13% | 9% |
3.3. Prognostic value of the interRAI ED Screener
More than one‐third (38%) of the patients were discharged home or back to their prior place of residence from the ED. After adjusting for age, sex, province, and the academic status of hospitals, the interRAI ED Screener was able to identify patients discharged home from the ED with fair discriminative accuracy (c = 0.66; 95% CI = 0.63–0.68). In this model, academic centers had 1.58 times the odds of discharging a patient home (odds ratio [OR] = 1.58; 95% CI = 1.25–1.98).
A similar number of patients (34%) experienced an ED length of stay greater than 24 hours. The interRAI ED Screener was able to discriminate patients who experienced an extended length of stay with fair accuracy (c = 0.60; 95% CI = 0.58–0.62) after adjusting for age, gender, sex, province, and academic status. Patients had twice the odds of experiencing an extended ED length of stay if they resided in Quebec compared with Ontario (OR = 2.0; 95% CI = 1.53–2.6). Patients treated at an academic center had lower odds of experiencing an extended ED stay (OR = 0.78; 95% CI = 0.63–0.97). Table 5 displays the adjusted associations between patient and visit characteristics in relation to ED disposition outcomes. All adjusted models had >20 events per variable. The proportion of missing disposition data was 19.2%, with 3 sites from Ontario contributing no outcome data.
TABLE 5.
Adjusted associations between the assessment urgency algorithm, discharge home, and an extended length of stay of 2273 older ED patients
| Covariate | Extended ED | |
|---|---|---|
| Discharge home | Length of stay | |
| N = 862 (38%) | N = 774 (34%) | |
| Intercept | 22.6 (5.73–89) | 0.31 (0.08–1.22) |
| Age, years | 0.96 (0.95–0.98) | 1.0 (0.98–1.02) |
| Sex, male | 1.08 (0.91–1.3) | 0.91 (0.76–2.59) |
| Province | ||
| Quebec | 0.8 (0.64–1.02) | 2.0 (1.53–2.6) |
| Ontario, reference | – | – |
| Academic, yes | 1.58 (1.25–1.98) | 0.78 (0.63–0.97) |
| Assessment Urgency Algorithm | ||
| 6 | 0.36 (0.27–0.45) | 1.43 (1.11–1.85) |
| 5 | 0.39 (0.23–0.66) | 1.37 (0.83–2.25) |
| 4 | 0.45 (0.32–0.62) | 1.63 (1.17–2.26) |
| 3 | 0.67 (0.52–0.82) | 1.03 (0.78–1.34) |
| 2 | 0.82 (0.53–1.26) | 0.9 (0.55–1.45) |
| 1, reference | – | – |
| Concordance statistic | 0.66 (0.63–0.68) | 0.6 (0.58–0.62) |
Note: Data are presented as odds ratio (95% confidence interval). Extended ED length of stay defined as >24 hours spent in the ED.
Abbreviation: ED, emergency department.
4. LIMITATIONS
We demonstrated the value of a rapid screening strategy in a heterogeneous group of patients from a variety of clinical settings and health systems. Our study participants represented a diverse group of older adults, including those who presented with cognitive impairment, a cohort commonly excluded in clinical and emergency research. This study is not without its limitations.
Although all patients were evaluated with the interRAI ED Screener, only a small subgroup (n = 1061) was further evaluated with the interRAI ED Contact Assessment. This limited our evaluation of overall agreement and negative predictive value between these 2 tools, as the interRAI ED Contact Assessment was specified for those with higher interRAI ED Screener scores when staff availability and resources allowed. A small number of patients with interRAI ED Screener scores <4 were screened with the interRAI ED Contact Assessment, although this was not intentional, and the characteristics of these individuals can be found in the supplemental file.
In addition, data were not collected on the proportion or characteristics of those who we were unable to screen; this information would have shed light on any potential selection biases by study recruiters. The proportion of patients who received an interRAI ED Contact Assessment also varied greatly across the study sites. Our goals were pragmatic with limited study costs. Thus, we collected minimal clinical data (eg, diagnoses, interventions) and were unable to examine additional important outcomes and provide a detailed contextual understanding of the findings.
Data on mortality were not collected, although prior work has demonstrated that <1% of older Canadian patients will die in the ED, 16 and ≈5% will die within 1 month of presentation. 26 , 27 We used ED registration as the starting point for length of stay, which may have increased additional health system–based confounders associated with disposition time. Missing data were systematically missing, whereby particular sites provided no data on age, and only Quebec hospitals reported on interRAI ED Screener time or ED disposition.
5. DISCUSSION
Our findings demonstrate that the interRAI ED Screener is designed to detect complex health and social concerns to assist in identifying patients at greatest need for a CGA after emergency care. When compared against the more detailed interRAI ED Contact Assessment done by a registered nurse, the interRAI ED Screener had excellent sensitivity (93%) and positive predictive value (82%), demonstrating its utility for rapidly identifying high‐risk older adults in greatest need of further assessment. In addition, we were able to determine that a 2‐minute screener only falsely classified 5.4% of patients as lower risk when they were classified as high risk by a more complete assessment. We believe this to be an entirely acceptable rate given the work efficiency gains in triaging patients to longer assessment strategies.
The interRAI ED screener was completed in <2 minutes on average in a wide array of patients in a variety of settings with different resource constraints. It therefore not only performs well but also may be easily implemented in dynamic and time‐pressed ED settings. The interRAI ED Screener was also able to predict patient‐important outcomes such as discharge home and extended ED length of stay (>24 hours) with fair accuracy, further highlighting the value of this tool for proactive clinical decision making.
The interRAI ED Screener is also associated with other patient‐important outcomes such as mortality, functional decline, and the need for formal support services in the community, 19 , 28 further highlighting the utility of this rapid screener. In addition, the interRAI ED Screener has shown to be useful in complex interventions geared toward improving geriatric models of care and shared decision making between high‐risk patients and ED clinicians. 29 , 30 The interRAI ED Screener has also been used in the prehospital setting, where it was predictive of the need for hospitalization from the ED, the need for home care services after discharge, and mortality in older ED patients transported by paramedics. 18
The interRAI ED Screener fosters system integration by providing a common measurement approach to identify the need for a comprehensive assessment used in other health sectors. The Assessment Urgency Algorithm is widely used by home care programs in Canada as a basis for intake screening. Therefore, the use of the interRAI ED Screener allows hospitals to use a common strategy for flagging older adults with complex needs. This proactive screening facilitates communication between care clinicians regarding patient needs more effectively, with the aim of supporting the initiation of community services that may attenuate the risk of future repeat visits to the ED. In the ED, the interRAI ED Assessment System is designed to delineate geriatric complexity and would be ideally incorporated in the emergency management pathway, as there are multiple points of contact to support decision making about the need for additional detailed geriatric assessment, with the interRAI ED Screener providing a rapid assessment of risk, and the interRAI ED Contact Assessment further highlights geriatric syndromes of concern and the need for a CGA.
6. CONCLUSION
We demonstrated the value of the interRAI ED Screener to identify individuals experiencing complex health and social concerns who present to the ED. The screener was accurate, feasible to learn and implement, and took <2 minutes to administer. It also predicted meaningful outcomes, including hospitalizations and discharge home. Further research will assist in better understanding how screening can be used to guide more detailed assessments and care plans.
AUTHOR CONTRIBUTIONS
Fabrice I. Mowbray conducted all study analyses and drafted the original manuscript. Paul Hebert, George Heckman, and Andrew P. Costa provided academic support and mentorship. All the authors contributed critical edits to this manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supporting Information
ACKNOWLEDGMENT
This study received funding from the Canadian Frailty Network (no. SIG2014F‐31).
Biography
Fabrice Mowbray, PhD, RN, is an assistant professor and research methodologist in the College of Nursing at Michigan State University. His research focuses on evaluating geriatric models of care, resuscitation, emergency management pathways, and advance care planning.

Mowbray FI, Heckman G, Hirdes JP, et al. Examining the utility and accuracy of the interRAI Emergency Department Screener in identifying high‐risk older emergency department patients: A Canadian multiprovince prospective cohort study. JACEP Open. 2023;4:e12876. 10.1002/emp2.12876
Supervising Editor: Catherine Marco, MD.
This study received funding from the Canadian Frailty Network (no. SIG2014F‐31).
REFERENCES
- 1. American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, Society for Academic Emergency Medicine, Geriatric Emergency Department Guidelines Task Force, American College of Emergency Physicians. Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7‐25. 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 2. Latham LP, Ackroyd‐Stolarz S. Emergency department utilization by older adults: a descriptive study. Can Geriatr J. 2014;17(4):118‐125. 10.5770/cgj.17.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238‐247. 10.1067/mem.2002.121523 [DOI] [PubMed] [Google Scholar]
- 4. Perry A, Macias Tejada J, Melady D. An approach to the older patient in the emergency department. Clin Geriatr Med. 2018;34(3):299‐311. 10.1016/j.cger.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 5. Bullard MJ, Melady D, Emond M, et al. Guidance when applying the Canadian Triage and Acuity Scale (CTAS) to the geriatric patient: executive summary. CJEM. 2017;19(S2):S28‐S37. 10.1017/cem.2017.363 [DOI] [PubMed] [Google Scholar]
- 6. Carpenter CR, Mooijaart SP. Geriatric screeners 2.0: time for a paradigm shift in emergency department vulnerability research. J Am Geriatr Soc. 2020;68(7):1402‐1405. 10.1111/jgs.16502 [DOI] [PubMed] [Google Scholar]
- 7. Elliott A, Taub N, Banerjee J, et al. Does the clinical frailty scale at triage predict outcomes from emergency care for older people? Ann Emerg Med. 2020;77(6):620‐627. 10.1016/j.annemergmed.2020.09.006 [DOI] [PubMed] [Google Scholar]
- 8. Costa AP, Hirdes JP, Arino‐Blasco S. InterRAI Emergency Department (ED) Assessment System Manual: For Use with the InterRAIED Screener (EDS) and ED Contact Assessment (ED‐CA). 9.3 Ed . InterRAI; 2017.
- 9. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500‐1524. 10.1016/j.ijsu.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 10. Downing A, Wilson R. Older people's use of accident and emergency services. Age Ageing. 2005;34(1):24‐30. 10.1093/ageing/afh214 [DOI] [PubMed] [Google Scholar]
- 11. Wellens NIH, Deschodt M, Boonen S, et al. Validity of the interRAI Acute Care based on test content: a multi‐center study. Aging Clin Exp Res. 2011;23(5‐6):476‐486. 10.1007/BF03325244 [DOI] [PubMed] [Google Scholar]
- 12. Hirdes JP, Ljunggren G, Morris JN, et al. Reliability of the interRAI suite of assessment instruments: a 12‐country study of an integrated health information system. BMC Health Serv Res. 2008;8:277. 10.1186/1472-6963-8-277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wellens NIH, Van Lancker A, Flamaing J, et al. Interrater reliability of the interRAI Acute Care (interRAI AC). Arch Gerontol Geriatr. 2012;55(1):165‐172. 10.1016/j.archger.2011.07.005 [DOI] [PubMed] [Google Scholar]
- 14. Costa AP, Hirdes JP, Heckman GA, et al. Geriatric syndromes predict postdischarge outcomes among older emergency department patients: findings from the interRAI multinational emergency department study. Acad Emerg Med. 2014;21(4):422‐433. 10.1111/acem.12353 [DOI] [PubMed] [Google Scholar]
- 15. Mowbray F, Zargoush M, Jones A, et al. Predicting hospital admission for older emergency department patients: insights from machine learning. Int J Med Inf. 2020;140:104163. 10.1016/j.ijmedinf.2020.104163 [DOI] [PubMed] [Google Scholar]
- 16. Brousseau AA, Dent E, Hubbard R, et al. Identification of older adults with frailty in the emergency department using a frailty index: results from a multinational study. Age Ageing. 2018;47(2):242‐248. 10.1093/ageing/afx168 [DOI] [PubMed] [Google Scholar]
- 17. Sinn CLJ, Heckman G, Poss JW, et al. A comparison of 3 frailty measures and adverse outcomes in the intake home care population: a retrospective cohort study. CMAJ Open. 2020;8(4):E796‐E809. 10.9778/cmajo.20200083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Whate A, Elliott J, Carter D, Stolee P. Performance of the interRAI ED Screener for risk‐screening in older adults accessing paramedic services. Can Geriatr J CGJ. 2021;24(1):8‐13. 10.5770/cgj.24.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gretarsdottir E, Jonsdottir AB, Sigurthorsdottir I, et al. Patients in need of comprehensive geriatric assessment: the utility of the InterRAI emergency department screener. Int Emerg Nurs. 2021;54:100943. 10.1016/j.ienj.2020.100943 [DOI] [PubMed] [Google Scholar]
- 20. Akpan A, Roberts C, Bandeen‐Roche K, et al. Standard set of health outcome measures for older persons. BMC Geriatr. 2018;18(1):36. 10.1186/s12877-017-0701-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chang AM, Lin A, Fu R, McConnell KJ, Sun B. Associations of emergency department length of stay with publicly reported quality‐of‐care measures. Acad Emerg Med. 2017;24(2):246‐250. 10.1111/acem.13102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15(9):825‐831. 10.1111/j.1553-2712.2008.00200.x [DOI] [PubMed] [Google Scholar]
- 23. Salehi L, Phalpher P, Valani R, et al. Emergency department boarding: a descriptive analysis and measurement of impact on outcomes. CJEM. 2018;20(6):929‐937. 10.1017/cem.2018.18 [DOI] [PubMed] [Google Scholar]
- 24. Brouns SHA, Stassen PM, Lambooij SLE, et al. Organisational factors induce prolonged emergency department length of stay in elderly patients ‐ a retrospective cohort study. PloS One. 2015;10(8):e0135066. 10.1371/journal.pone.0135066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sweeny A, Keijzers G, O'Dwyer J, et al. Predictors of a long length of stay in the emergency department for older people. Intern Med J. 2020;50(5):572‐581. 10.1111/imj.14441 [DOI] [PubMed] [Google Scholar]
- 26. Mowbray FI, Aryal K, Mercier E, Heckman G, Costa AP. Older emergency department patients: does baseline care status matter? Can Geriatr J. 2020;23(4):289‐296. 10.5770/cgj.23.421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blomaard LC, Speksnijder C, Lucke JA, et al. Geriatric screening, triage urgency, and 30‐day mortality in older emergency department patients. J Am Geriatr Soc. 2020;68(8):1755‐1762. 10.1111/jgs.16427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van Dam CS, Trappenburg MC, Ter Wee MM, et al. The accuracy of four frequently used frailty instruments for the prediction of adverse health outcomes among older adults at two Dutch emergency departments: findings of the AmsterGEM study. Ann Emerg Med. 2021;78(4):538‐548. 10.1016/j.annemergmed.2021.04.027 [DOI] [PubMed] [Google Scholar]
- 29. Ma C, Riehm LE, Bernacki R, et al. Quality of clinicians’ conversations with patients and families before and after implementation of the Serious Illness Care Program in a hospital setting: a retrospective chart review study. CMAJ Open. 2020;8(2):E448‐E454. 10.9778/cmajo.20190193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Heeren P, Devriendt E, Fieuws S, et al. Unplanned readmission prevention by a geriatric emergency network for transitional care (URGENT): a prospective before‐after study. BMC Geriatr. 2019;19(1):215. 10.1186/s12877-019-1233-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


