Abstract
Odontoid fractures are the most common cervical spine fractures in the elderly. Although many classification systems have been developed for them, the ambiguity in various definitions can potentially lead to misunderstandings. This paper aims to review the terminologies and current classification systems of odontoid fractures and propose a new, simplified anatomical classification. Given the descriptive variability of odontoid fractures in current classifications, we systematically reviewed the literature using PRISMA guidelines querying the National Library of Medicine PubMed database. The initial literature search yielded 175 publications. A total of seven reports met the inclusion criteria and were ultimately included for a full review. The classification systems previously used to categorize fractures of the odontoid process often need to be more transparent, imprecise, and incongruous. To simplify them, a new embryologically accurate system is proposed. A new embryological and anatomically-based system, combining the former systems' specific attributes, allows a more straightforward and adaptable classification of odontoid fractures.
Keywords: classification system, fractures, dens, odontoid process, axis, c2
Introduction and background
Odontoid fractures account for 10-15% of all cervical vertebral fractures [1,2]. In patients over 70 years, fractures of the odontoid process are the most common cervical spine fractures [3]. The classification systems have been divided into categories according to fracture location, fracture direction, and odontoid process anatomy [4]. Each current classification system is located within that framework, yet some ambiguities and obscurities can potentially lead to misunderstandings.
The purpose of this paper is to review the current classification systems of odontoid fractures with their complexities, ambiguities, and drawbacks and to propose a new simplified anatomical classification based on the embryology of the C2 vertebra.
Review
Methods
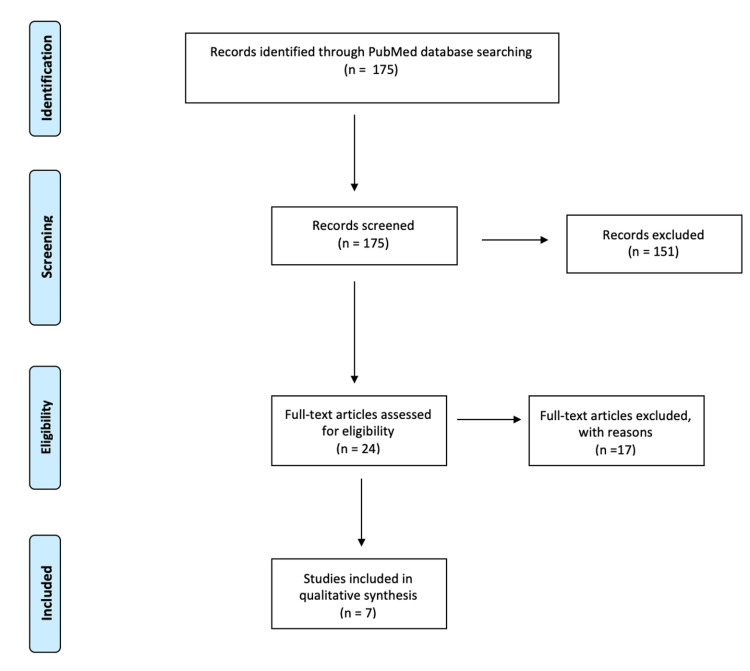
We reviewed the literature systematically without meta-analysis by Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [5] regarding current classifications of odontoid fractures, querying the National Library of Medicine PubMed database using the combination of MeSH terms "Odontoid fracture OR Dens fracture" AND "Classification." Abstracts were then screened using the inclusion criteria of English reports discussing odontoid fracture classification. The search period ranged from 1970 to 2022. We excluded articles that (1) did not mention fractures relating to the odontoid process or dens or (2) focused solely on surgical treatment strategies and outcomes (Figure 1).
Figure 1. PRISMA flow chart of literature review.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Results
The initial literature search yielded 175 publications. Of these, 24 were found to meet the inclusion criteria and were subjected to review for exclusion. From the past 52 years, seven reports were ultimately selected for full review since 17 were found irrelevant owing to one or both points listed in the exclusion criteria. A search flow diagram is provided in Figure 1. All of the included reports discussed unique proposed classification systems for odontoid fractures.
Korres et al. [4] divided the classification systems into three separate categories depending on if their classification was based on: (1) fracture location and position, (2) fracture direction, or (3) odontoid process anatomy. Each of the following systems is located within that framework. The Schatzker [6], Althoff [7], and Anderson-D'Alonzo systems [8] fall under the umbrella of fracture position. Grauer et al. [9] and Hadley et al. [10]independently subclassified the Anderson-D'Alonzo system. The Roy-Camille system classified odontoid fractures based on fracture direction [11].
This report discusses the previous classification systems in detail with their advantages and drawbacks (Table 1). Additionally, we propose a new simplified classification system based on the embryological development of the odontoid process and its anatomy and guide clinical decision-making in their management.
Table 1. Summary of current and previous odontoid fracture classification systems with their drawbacks.
| System | Based on | Classification | Drawback |
| Schatzker’s (1971) et al. [6] | Fracture position and location in relation to the attachment of the accessory ligaments | Low fracture either at the level or below the level of the attachment of the accessory ligaments | 1. Diversity of terminologies surrounding the location of the fracture 2. Some lack of internal fracture morphology and type of fracture 3. Discrepancies regarding fracture stability, comminution and displacement which ultimately affect management recommendation 4. Often no distinct anatomic borders defined between fracture types |
| High fracture on one or both sides, above the attachment of the accessory ligaments | |||
| Anderson and D’Alonzo’s (1974) et al. [8] | Fracture position and location | Type I oblique fracture at the tip of the odontoid process | |
| Type II at the base of the dens and the junction with the body | |||
| Type III at the junction of the dens with the anterior portion of the axial body extending into the body and lateral masses of C2 | |||
| Althoff’s (1979) et al. [7] | Fracture position and location | Type A above the neck | |
| Type B through the neck including superior C2 body | |||
| Type C includes the medial part of one C2 superior articulating process | |||
| Type D includes fractures through the body of C2, including the medial part of both superior articulating processes | |||
| Hadley’s (1988) et al. [10] | Subclassification of Anderson and D’Alonzo’s | Type I and type III the same as Anderson and D’Alonzo’s | |
| Type IIA additional bone fragment at the dens fracture site | |||
| Grauer’s (2005) et al. [9] | Subclassification of Anderson and D’Alonzo’s | Type I and type III same as Anderson and D’Alonzo’s | |
| Type IIA not displaced from their site of origin | |||
| Type IIB displaced and/or extend transversely from anterior superior to posterior inferior | |||
| Type IIC comminuted and/or extend from anterior inferior to posterior superior | |||
| Roy-Camille’s (1979) et al. [11] | The direction of the fracture line and the amount of displacement | Type I obliquely slanted from posterior to anterior displacing the odontoid process anteriorly | 1. Fails to describe fracture location 2. Did not address the relationship of fractures involving the body of C2 |
| Type II oblique angle slants anterior to posterior displacing the odontoid process posteriorly | |||
| Type II horizontal fracture with no angulation displacing the odontoid process anteriorly or posteriorly | |||
| Current system | Embryological development and anatomy of the odontoid process | Type I involving the upper ¼ of the dens (zone I) | 1. Only fractures involving and related to the anatomical odontoid process |
| IA non displaced | |||
| IB displaced and/or angulated odontoid process anteriorly or posteriorly | |||
| Type II involving the lower ¾ of the dens (zone II) | |||
| IIA non displaced | |||
| IIB displaced and/or angulated odontoid process anteriorly or posteriorly |
Discussion
Embryology and Odontoid Development
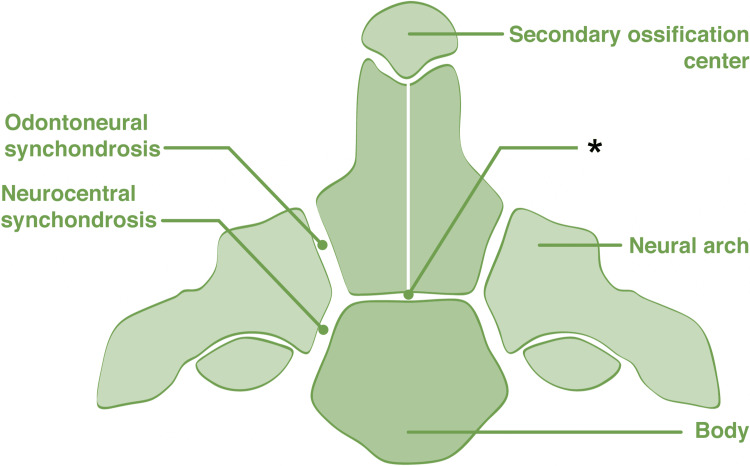
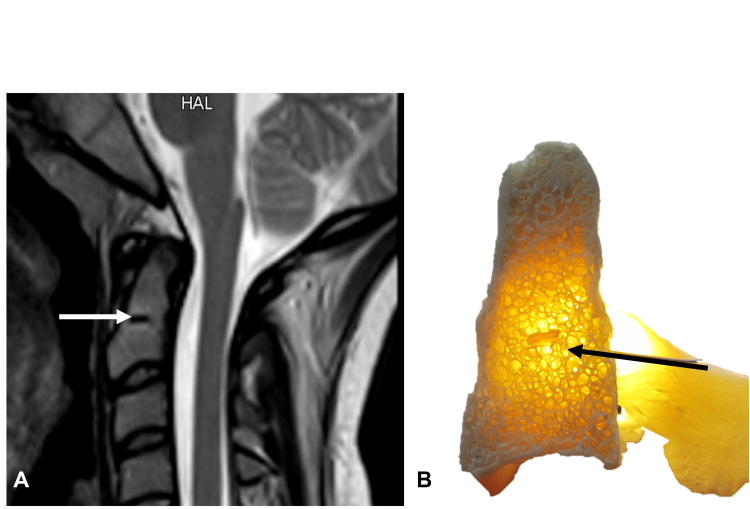
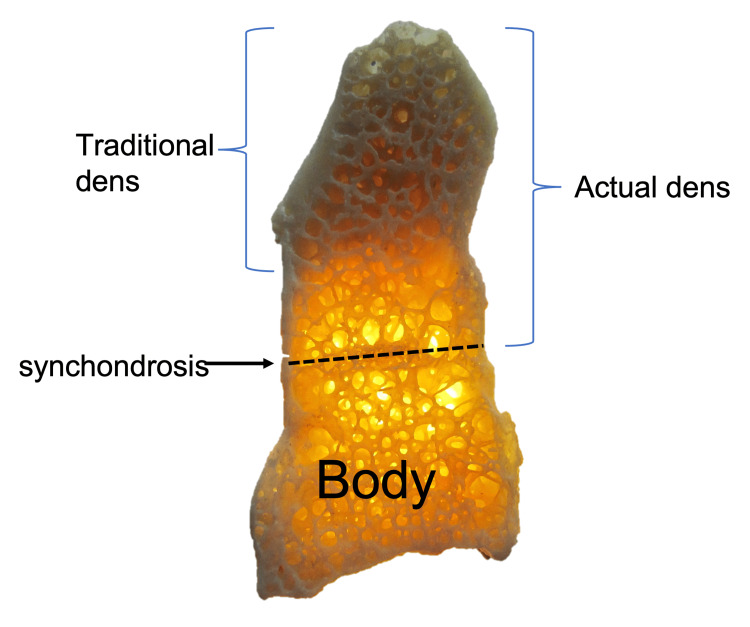
The odontoid process of C2 (dens) has been widely studied because of its anatomical importance. Formerly thought to originate as a displaced body of C1 (atlas), it is now accepted that the dens separate from the anterior arch of C1, moving inferiorly to fuse with the axis during the sixth and seventh weeks of gestation [12]. The dens are derived from two separate ossification centers. The primary ossification centers form laterally at the base of the odontoid, which comprises the union between the two primary ossification centers and fuses in the midline by the eighth month of fetal life. The secondary ossification center (called the cuneiform cartilage) forms the apex/tip of the odontoid process (Figure 2). The subdental synchondrosis develops between the primary ossification centers of the odontoid process and the corpus of C2 (Figure 3), which remains visible on radiographic imaging until the 11th year of life [12,13]. There is significant variability in research concerning the timeline for the persistence of these synchondroses through adulthood, as Jenkins et al. [14] found in as few as 25% of cases. In contrast, Gebauer et al. [13] detected them in almost 90%. The development and morphology of the odontoid process provide a foundation for classifying odontoid fractures and their treatment options.
Figure 2. Coronal view of the C2 vertebra noting its embryological fusion sites.
The subdental synchondrosis is seen at the *
Author's own work.
Figure 3. A: MRI and B: dry bone specimen noting the subdental synchondrosis (arrows).
Author's own work.
Odontoid Process Anatomy and Nomenclature
The odontoid process is a conical projection from the C2 vertebral body and serves as an attachment site for the cranioatlantoaxial ligamentous complex [12,15]. It is often referred to as the dens, odontoid peg, or processus epitrophysis [12,16,17]. The tip of the odontoid process extends from the apex of the dens to the apicodental junction.
The apex gives origin to the apical ligament, which extends rostrally to attach to the basion. The atlas' anterior arch articulates with the odontoid process's anterior surface [15]. The broad posterior groove and the posterolateral surfaces are attachment sites for the transverse and alar ligaments [12,16,17].
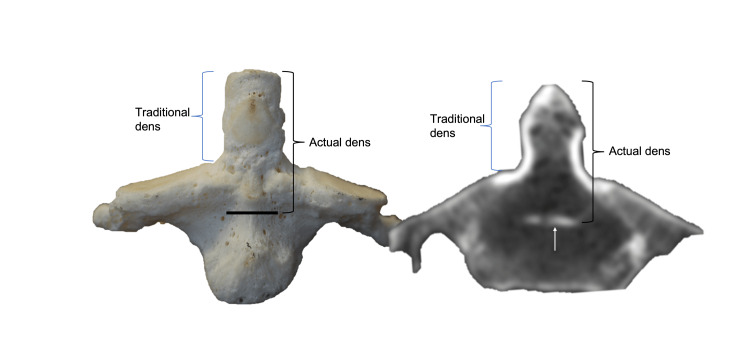
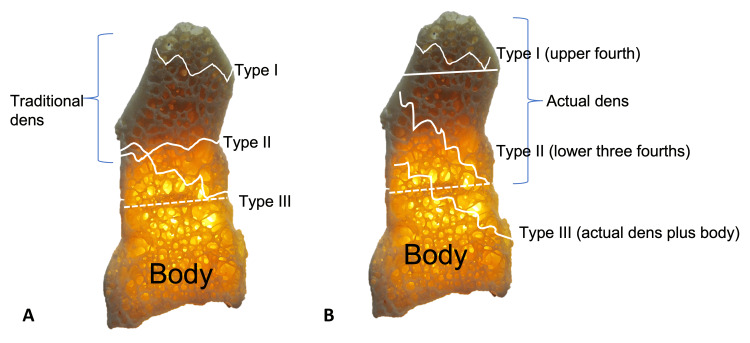
The bone between the apicodental junction and a horizontal line connecting bilateral superior articular processes forming the neck of the dens is known as the chondrum terminale [18,19]. The base or waist of the dens is where it attaches to the C2 vertebral body with the narrowest transverse diameter, just superior to the body of C2 (Figures 4, 5) [8,20-22].
Figure 4. Anterior view of C2 vertebra on skeletal specimen and CT noting the subdental synchondrosis and the traditional and actual extents of the dens.
Author's own work.
Figure 5. Sagittal view of C2 vertebra on skeletal specimen noting the subdental synchondrosis and the traditional and actual extents of the dens.
Author's own work.
However, others have defined the base as the bone between the part of the dens found along a horizontal line connecting bilateral superior articular processes and the subdental synchondrosis, also known as the dentocentral junction or odontocentral synchondrosis (Figures 4, 5) [18]. The terms waist and neck are used interchangeably for the part where the transverse ligament passes posteriorly [23]. The connection between the waist and tip of the dens has also been described as the neck, the stem, or the shaft of the dens, which is connected inferiorly to the C2 vertebra centrum at the subdental synchondrosis [24,25].
Schatzker's Classification System
In 1971, Schatzker's classification divided the dens into two types according to where the accessory ligaments are attached. The fractures could be above or below those ligaments; a low fracture is either at the level of the attachment or below it, while a higher fracture involving either one or both sides is above the attachment [6].
Anderson and D'Alonzo's Classification System
D'Alonzo and Anderson [8] in 1974 proposed that odontoid fractures can be categorized into Types I, II, or III according to their anatomic location (Figure 6A). Type I fractures, which are the least common, occur at the tip of the odontoid process [8]. Type II fractures are the most common, accounting for 65-74% of cases, and occur at the base of the dens causing subluxation of the atlas on C2 [3,8]. The etiology of these fractures is age-related; as younger patients present due to high loading, for instance, in motor vehicle accidents; whereas in patients aged over 60, these fractures tend to result from hyperflexion/extension of the neck during low energy activities such as falling from an upright position [26]. This distinction is bolstered by studies showing a strong link between osteoporosis and odontoid fractures following minor trauma in the elderly [26,27]. Amling et al. [28] revealed that normal physiological degeneration of the dens entailed a loss of cortical thickness, decreased trabecular volume, and weakening of trabecular bone connectivity. Jenkins et al. [14] further developed this concept using microCT imaging to show that the trabecula was most dense between the subdental synchondrosis and the apex, the region of Type II fractures. Finally, type III fractures occur at the junction of the dens with the anterior portion of the axial body, extending into the lateral masses of the axis [8,14]. Generally, types I and III fractures are more stable, causing limited nerve involvement, and are often treated with non-invasive measures such as external mobilization [29,30]. Although this is the most commonly-used system, Barker et al. [31] found only "fair" interrater reliability and rejected their hypothesis that this system was reliable and reproducible.
Figure 6. A: Sagittal view of C2 vertebra noting fractures and using a traditional system to describe these injuries. B. Application of the new simplified system (Tulane classification) of describing odontoid fractures.
The upper horizontal line (right) approximates the apicodental synchondrosis, and the lower dotted lines represent the subdental synchondroses.
Author's own work.
Althoff’s classification system
In 1979, Althoff [7] proposed four types of fractures depending on the anatomic level. Type A is a fracture above the neck, Type B is through the neck, including the most superior aspect of the body of C2, Type C includes the medial part of one superior articular facet, and Type D includes fractures through the body of C2 including the medial part of bilateral superior articular facets. Types A-C have pseudoarthroses of 64%, 55%, and 50%, respectively, whereas Type D has a 97% rate of a union. In his initial study, the bony union was significantly increased with fractures involving the body of the axis and those displaced anteriorly compared to posterior displacement.
Roy-Camille's Classification System
Roy-Camille et al. [11,32] created a system based on the fracture line's direction and the displacement amount. Odontoid instability, and therefore patient prognosis, is related to the comminution and directionality of the fracture line. The authors classify a Type I fracture as obliquely slanted from posterior to anterior, allowing the dens to be displaced anteriorly. Similar to Type I, a Type II fracture's oblique angle slants anterior to posterior with possible posterior displacement of the dens. Type III is a horizontal fracture with no angulation, in which the dens can displace anteriorly or posteriorly. Finally, Type IV is described as a "policeman's hat fracture," a horizontal fracture extending through the C2 body, becoming transarticular. Predictive validity testing showed that this classification correlates with the speed of fracture healing, otherwise known as the rate of union [29].
Hadley's Classification System
Hadley et al. [10] also developed a subclassification of Anderson and D'Alonzo's classification system, specifically within the Type II fracture. This new description encompassed fractures with bone chips at the base of the dens fracture, which hinders proper re-alignment and bony union [10,33]. This subclass, accounting for <10% of odontoid fractures, led to non-union regardless of the initial amount of dens dislocation [10]. Because these often appear like Type II fractures, they were classified as Type IIA [10,33].
Grauer's Classification System
In 2005, Grauer et al. [9] proposed a modified classification system with descriptions very similar to Anderson and D'Alonzo's types I and III but with subclassification of type II fractures. Type IIA fractures were without displaced from their site of origin. Type IIB included fractures with oblique fractures from anterior superior to posterior inferior or with transverse displacement. Type IIC included fractures that extend from anterior inferior to posterior superior or were comminuted, but these do not include the superior articular facets. The advantage of this subclassification of Type II fractures was to guide treatment recommendations where type IIA underwent non-operative external immobilization, type IIB was considered for odontoid screw, and type IIC for posterior C1-2 fusion.
Drawbacks of Previous Classification System
The Anderson and D'Alonzo system can confuse owing to the diversity of terminologies surrounding the location of the fracture. A type I fracture can be depicted as an "apical (tip) fracture of the dens" [29], "an oblique fracture through the upper part of the odontoid" [30], or "located in the upper part of the odontoid process" [27]. This is further confused by Hadley's and Grauer's subclassification of Anderson-D'Alonzo class II; IIA, IIB, IIC. Because of the variety of descriptors, this classification can be confusing. In addition, their fracture types are solely anatomically based without further stratification of the fracture type, internal morphology, or degree of displacement.
The Roy-Camille system denotes the direction of the fracture and the displacement of the odontoid and predicts the rate of a union during treatment but fails to describe the location of the fracture. Also, it needs to precisely address the relationship between type 2 fractures and the body of C2. In this classification, some studies depict type II fractures as being at "the base of the odontoid process" [27]. In contrast, others describe them as "at the junction between the body of the odontoid process and the body of the C2 vertebra" [3]. Further clarity and consistency are needed about what is considered the base. To ensure reliability, the terminology used to depict these types should be unanimously agreed upon across each system.
Treatment options for odontoid fractures, including spinal fusion, depending on whether the fracture is stable or unstable. For instance, a Hadley type IIA fracture is considered unstable owing to the comminution, so treatment requires surgery to ensure union [33]. However, a Grauer type IIA fracture is characterized as non-displaced, so treatment is non-invasive, for example, by external immobilization [9]. The coalescence of nomenclature in classification systems can lead to confusion and could be more accurate, depending on the system under which the patient is placed.
Lastly, there are examples in the literature where none of the previous classifications apply. For instance, Adam et al. [30] described a patient with an odontoid fracture fitting none of those above criteria. The patient was a 91-year-old female who had suffered trauma from a low-energy fall. The fracture extended through the base of the odontoid and into the vertebral body, causing a 4 mm anterior-inferior displacement. The authors concluded that a new classification system should be created.
A New Simplified Classification System
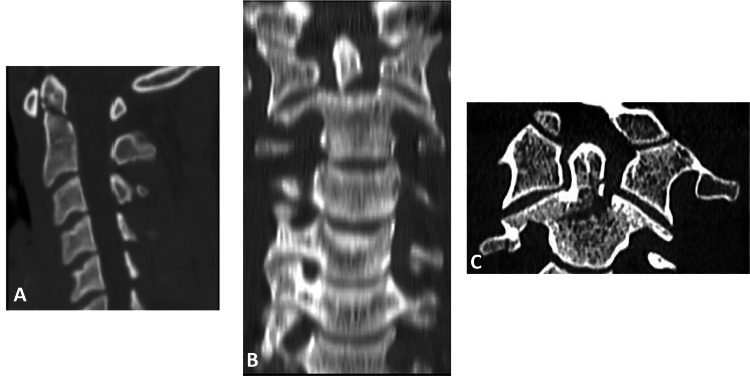
A simplified and easily reproducible classification system originated from nomenclature proposed based on the developmental anatomy of the odontoid, developed by Johal et al. [34]. The apex of the dens develops from a unique secondary ossification center, while the remainder is formed from two laterally located primary ossification centers. The former does not necessarily fuse with the rest of the dens until puberty, and the latter forms the subdental synchondrosis. This classification system defines the dens anatomically from the superior part of the apex to the site of fusion with the body of C2 (at the synchondrosis). It consists of two zones. Zone I extends from the apex of the odontoid to the junction of the primary and secondary ossification centers (e.g., the upper ¼ of the dens or, i.e., the apicodental junction). Zone II extends from that junction to the synchondrosis (e.g., the lower ¾) [34]. This system allows for easy communication about the location of a fracture, on which further descriptors can be superimposed (Figures 6B, 7). For example, a fracture can be described as a "zone two oblique fracture with anterior displacement." Every party would then know that the fracture is located in the inferior ¾ of the dens.
Figure 7. Examples of odontoid fractures.
Using the new simplified system, A: Type I fracture. B: Type II fracture. C: Type III fracture.
Subclassification and Surgical Implications
Furthermore, the proposed classification can be subdivided according to whether the dens are displaced or angulated. If neither, we classify the fracture as type A; if there is any dens displacement and/or angulation either anteriorly or posteriorly, we can classify it as type B (Table 1). As techniques for odontoid fixation have evolved, management with either external or internal fixation depends on multiple factors, including fracture morphology, displacement, angulation, timing and stability of the fracture, integrity of the transverse ligament, patient age, and comorbidities, patient preference.
Therefore, both proposed types and subtypes can be considered unstable fractures, and we advocate surgical management for both. For type IA and type IIA and in the absence of contraindications, an anterior approach with an odontoid screw could be considered. Certain superior-type IA fractures may be managed with rigid external fixation at the surgeon's discretion. Contraindications for odontoid screw placement in type IA or IIA fractures most notably include transverse ligament disruption or type IIA with oblique type fracture. On the other hand, in type IB and type IIB, the surgical approach depends on the degree of angulation and displacement. In mild angulation and displacement cases, the anterior approach with an odontoid screw could be considered if there are no contraindications. These contraindications traditionally include anterior-inferior to the superior-posterior fracture line, transverse ligament injury, chronic fractures, pathologic fractures, comminuted internal morphology, or neck or chest anatomic limitations, including enlarged thoracic cavity diameter. In moderate to severe cases or in the presence of the above contraindications, the posterior approach with atlantoaxial fusion could be considered. The currently proposed system represents an evolution of the previous systems, considering the embryological development of the odontoid process and its anatomy. The proposal is only the first step for better communication and simplified classification. This system's prospective application to the classification and management of odontoid fractures will be required to evaluate and validate its utility.
Limitations
This proposed system has limitations. It would only include fractures related to the anatomical odontoid. Fractures involving the body of C2 would be excluded. This would remove any related confusion. Although the system does not address all the intricacies of related fractures and their underlying etiologies, it provides a reliable guide to the location of the fracture, which can be specified further [35-37]. Lastly, although not explored in the literature with comparative studies, ethnicity and sex could also play a role in the prevalence and type of fractures in this bone.
Conclusions
Many classification systems for odontoid fractures have been developed, yet some ambiguities can potentially lead to misunderstandings. To help alleviate this ambiguity, we propose a simplified classification system (Tulane classification) that uses the embryological lines of development of the C2 vertebra as a foundation that can be built upon to describe odontoid fractures accurately. Prospective application of this system to both the classification and treatment of odontoid fractures will be required to validate its utility.
Acknowledgments
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase humanity's overall knowledge, which can then improve patient care. Therefore, these donors and their families deserve our highest gratitude [38]. The authors state that every effort was made to follow all local and international ethical guidelines and laws pertaining to using human cadaveric donors in anatomical research [39].
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Oblique axis body fracture: an unstable subtype of Anderson type III odontoid fractures apropos of two cases. Takai H, Konstantinidis L, Schmal H, Helwig P, Knöller S, Südkamp N, Hauschild O. Case Rep Orthop. 2016;2016:7561682. doi: 10.1155/2016/7561682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fractures of the cervical spine. Marcon RM, Cristante AF, Teixeira WJ, Narasaki DK, Oliveira RP, de Barros Filho TE. Clinics (Sao Paulo) 2013;68:1455–1461. doi: 10.6061/clinics/2013(11)12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Surgical treatment of Type II odontoid fractures: anterior odontoid screw fixation or posterior cervical instrumented fusion? Joaquim AF, Patel AA. Neurosurg Focus. 2015;38:0. doi: 10.3171/2015.1.FOCUS14781. [DOI] [PubMed] [Google Scholar]
- 4.It is time to reconsider the classification of dens fractures: an anatomical approach. Korres D, Mavrogenis AF, Gratsias P, Lyritis G, Papagelopoulos PJ. Eur J Orthop Surg Traumatol. 2008;18:189–195. [Google Scholar]
- 5.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fractures of the dens (odontoid process). an analysis of thirty-seven cases. Schatzker J, Rorabeck CH, Waddell JP. https://pubmed.ncbi.nlm.nih.gov/5562366/ J Bone Joint Surg Br. 1971;53:392–405. [PubMed] [Google Scholar]
- 7.Fracture of the odontoid process. an experimental and clinical study. Althoff B. Acta Orthop Scand Suppl. 1979;177:1–95. doi: 10.3109/ort.1979.50.suppl-177.01. [DOI] [PubMed] [Google Scholar]
- 8.Fractures of the odontoid process of the axis. Anderson LD, D'Alonzo RT. https://pubmed.ncbi.nlm.nih.gov/4434035/ J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 9.Proposal of a modified, treatment-oriented classification of odontoid fractures. Grauer JN, Shafi B, Hilibrand AS, et al. Spine J. 2005;5:123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 10.New subtype of acute odontoid fractures (type IIA) Hadley MN, Browner CM, Liu SS, Sonntag VK. https://pubmed.ncbi.nlm.nih.gov/3344089/ Neurosurgery. 1988;22:67–71. doi: 10.1227/00006123-198801010-00010. [DOI] [PubMed] [Google Scholar]
- 11.Fracture de l'odontoïde associée à une fracture des pédicules de l'axis. a propos de 11 cas [French] Roy-Camille R, Bleynie JF, Saillant G, Judet T. https://pubmed.ncbi.nlm.nih.gov/161043/ Rev Chir Orthop Reparatrice Appar Mot. 1979;65:387–391. [PubMed] [Google Scholar]
- 12.The odontoid process: a comprehensive review of its anatomy, embryology, and variations. Akobo S, Rizk E, Loukas M, Chapman JR, Oskouian RJ, Tubbs RS. Childs Nerv Syst. 2015;31:2025–2034. doi: 10.1007/s00381-015-2866-4. [DOI] [PubMed] [Google Scholar]
- 13.Subdental synchondrosis and anatomy of the axis in aging: a histomorphometric study on 30 autopsy cases. Gebauer M, Lohse C, Barvencik F, Pogoda P, Rueger JM, Püschel K, Amling M. Eur Spine J. 2006;15:292–298. doi: 10.1007/s00586-005-0990-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Internal morphology of the odontoid process: anatomical and imaging study with application to C2 fractures. Jenkins S, Bordes S, Aly I, et al. World Neurosurg. 2019;127:0–6. doi: 10.1016/j.wneu.2019.04.052. [DOI] [PubMed] [Google Scholar]
- 15.Standring S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. Edinburgh. Edinburgh: Elsevier Churchill Livingston; 2016. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41st Edition. [Google Scholar]
- 16.Morphological and functional studies on the odontoid process of the human axis. Koebke J. Anat Embryol (Berl) 1979;155:197–208. doi: 10.1007/BF00305752. [DOI] [PubMed] [Google Scholar]
- 17.The three-dimensional morphometry of the odontoid peg and its impact on ventral screw osteosynthesis. Puchwein P, Jester B, Freytag B, Tanzer K, Maizen C, Gumpert R, Pichler W. Bone Joint J. 2013;95-B:536–542. doi: 10.1302/0301-620X.95B4.30949. [DOI] [PubMed] [Google Scholar]
- 18.The segments and the inferior boundaries of the odontoid process of C2 based on the magnetic resonance imaging study. Aydin K, Cokluk C. https://pubmed.ncbi.nlm.nih.gov/18382973/ Turk Neurosurg. 2008;18:23–29. [PubMed] [Google Scholar]
- 19.Weinstein SL. The Pediatric Spine: Principles and Practice. 2nd Edition. Philadelphia: Lippincott Williams and Wilkins; 2001. The Pediatric Spine: Principles and Practice. 2nd Edition; pp. 3–54. [Google Scholar]
- 20.The dens: normal development, developmental variants, and anomalies, and traumatic injuries. O'Brien WT Sr, Shen P, Lee P. J Clin Imaging Sci. 2015;5:38. doi: 10.4103/2156-7514.159565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acute axis fractures: a review of 229 cases. Hadley MN, Dickman CA, Browner CM, Sonntag VK. J Neurosurg. 1989;71:642–647. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 22.Vaccaro AR. Boca Raton, FL: CRC Press; 2002. Fractures of the cervical, thoracic, and lumbar spine. [Google Scholar]
- 23.Sherk HH, Parke WW. The Cervical Spine, 2nd Edition. Philadelphia: JB Lippincott Company; 1989. Normal adult anatomy; pp. 8–22. [Google Scholar]
- 24.Jinkins JR. Philadelphia: Lippincott Williams & Wilkins; 2000. Atlas of neuroradiologic embryology, anatomy, and variants. [Google Scholar]
- 25.Korres DS. The axis vertebra. Milan: Springer-Verlag; 2013. The Axis Vertebra; pp. 45–59. [Google Scholar]
- 26.Treatment modality in type II odontoid fractures defines the outcome in elderly patients. Scheyerer MJ, Zimmermann SM, Simmen HP, Wanner GA, Werner CM. BMC Surg. 2013;13:54. doi: 10.1186/1471-2482-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.A case of dens fracture: a pictorial review and discussion. Desai B, Slish J, Allen B. Case Rep Emerg Med. 2012;2012:864160. doi: 10.1155/2012/864160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Structure of the axis--key to the etiology of the dens fracture [German] Amling M, Wening VJ, Pösl M, Grote HJ, Hahn M, Delling G. https://pubmed.ncbi.nlm.nih.gov/7821077/ Chirurg. 1994;65:964–969. [PubMed] [Google Scholar]
- 29.Chapman JR, Dettori JR, Norvell DC. AO Publishing. Dübendorf: AO Publishing; 2009. Spine classifications and severity measures. . [Google Scholar]
- 30.Odontoid fracture that is not listed in the existing classifications: a new subtype of odontoid fracture: case report. Adam D, Cergan R, Iftimie D, Moisescu C. https://journals.lapub.co.uk/index.php/roneurosurgery/article/view/874 Romanian Neurosurgery. 2016;30:57–64. [Google Scholar]
- 31.Reliability and reproducibility of dens fracture classification with use of plain radiography and reformatted computer-aided tomography. Barker L, Anderson J, Chesnut R, Nesbit G, Tjauw T, Hart R. https://pubmed.ncbi.nlm.nih.gov/16391255/ J Bone Joint Surg Am. 2006;88:106–112. doi: 10.2106/JBJS.D.02834. [DOI] [PubMed] [Google Scholar]
- 32.Fractures of the odontoid process. conservative and operative treatment. prognostic factors. van Holsbeeck E, Stoffelen D, Fabry G. https://pubmed.ncbi.nlm.nih.gov/8484317/ Acta Orthop Belg. 1993;59:17–21. [PubMed] [Google Scholar]
- 33.Surgical vs non operative treatment of Hadley type IIA odontoid fractures. Aldrian S, Erhart J, Schuster R, et al. Neurosurgery. 2012;70:676–682. doi: 10.1227/NEU.0b013e318235ade1.. [DOI] [PubMed] [Google Scholar]
- 34.The dens: a review of its diverse nomenclature and a recommended simplified terminology. Johal J, Fisahn C, Burgess B, Loukas M, Chapman J, Oskouian RJ, Tubbs RS. Cureus. 2017;9:0. doi: 10.7759/cureus.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rheumatoid arthritis in review: clinical, anatomical, cellular and molecular points of view. Sharif K, Sharif A, Jumah F, Oskouian R, Tubbs RS. Clin Anat. 2018;31:216–223. doi: 10.1002/ca.22980. [DOI] [PubMed] [Google Scholar]
- 36.Translation of Hecker's 1922 "the occipital-atlanto-axial ligament system": a study in comparative anatomy. Oakes PC, Sardi JP, Iwanaga J, Topale N, Oskouian RJ, Tubbs RS. Clin Anat. 2017;30:322–329. doi: 10.1002/ca.22853. [DOI] [PubMed] [Google Scholar]
- 37.Down syndrome-a narrative review with a focus on anatomical features. Arumugam A, Raja K, Venugopalan M, Chandrasekaran B, Kovanur Sampath K, Muthusamy H, Shanmugam N. Clin Anat. 2016;29:568–577. doi: 10.1002/ca.22672. [DOI] [PubMed] [Google Scholar]
- 38.Acknowledging the use of human cadaveric tissues in research papers: recommendations from anatomical journal editors. Iwanaga J, Singh V, Ohtsuka A, et al. Clin Anat. 2021;34:2–4. doi: 10.1002/ca.23671. [DOI] [PubMed] [Google Scholar]
- 39.Standardized statement for the ethical use of human cadaveric tissues in anatomy research papers: Recommendations from Anatomical Journal Editors-in-Chief. Iwanaga J, Singh V, Takeda S, et al. Clin Anat. 2022;35:526–528. doi: 10.1002/ca.23849. [DOI] [PubMed] [Google Scholar]