Abstract
Background
During the COVID-19 pandemic, infodemic spread even more rapidly than the pandemic itself. The COVID-19 vaccine hesitancy has been prevalent worldwide and hindered pandemic exiting strategies. Misinformation around COVID-19 vaccines is a vital contributor to vaccine hesitancy. However, no evidence systematically summarized COVID-19 vaccine misinformation.
Objective
This review aims to synthesize the global evidence on misinformation related to COVID-19 vaccines, including its prevalence, features, influencing factors, impacts, and solutions for combating misinformation.
Methods
We performed a systematic review by searching 5 peer-reviewed databases (PubMed, Embase, Web of Science, Scopus, and EBSCO). We included original articles that investigated misinformation related to COVID-19 vaccines and were published in English from January 1, 2020, to August 18, 2022. We excluded publications that did not cover or focus on COVID-19 vaccine misinformation. The Appraisal tool for Cross-Sectional Studies, version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2), and Critical Appraisal Skills Programme Checklist were used to assess the study quality. The review was guided by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and registered with PROSPERO (CRD42021288929).
Results
Of the 8864 studies identified, 91 observational studies and 11 interventional studies met the inclusion criteria. Misinformation around COVID-19 vaccines covered conspiracy, concerns on vaccine safety and efficacy, no need for vaccines, morality, liberty, and humor. Conspiracy and safety concerns were the most prevalent misinformation. There was a great variation in misinformation prevalence, noted among 2.5%-55.4% in the general population and 6.0%-96.7% in the antivaccine/vaccine hesitant groups from survey-based studies, and in 0.1%-41.3% on general online data and 0.5%-56% on antivaccine/vaccine hesitant data from internet-based studies. Younger age, lower education and economic status, right-wing and conservative ideology, and having psychological problems enhanced beliefs in misinformation. The content, format, and source of misinformation influenced its spread. A 5-step framework was proposed to address vaccine-related misinformation, including identifying misinformation, regulating producers and distributors, cutting production and distribution, supporting target audiences, and disseminating trustworthy information. The debunking messages/videos were found to be effective in several experimental studies.
Conclusions
Our review provides comprehensive and up-to-date evidence on COVID-19 vaccine misinformation and helps responses to vaccine infodemic in future pandemics.
Trial Registration
PROSPERO CRD42021288929; https://tinyurl.com/2prejtfa
Keywords: COVID-19, COVID-19 vaccine, misinformation, anti-vaccine, review, social media, survey
Introduction
Background
The COVID-19 pandemic has become the most threatening global health issue for almost 3 years [1]. As a cost-effective measure to protect people, governments have implemented various policies to promote the COVID-19 vaccination. However, as of early 2022, the global acceptance rate of the COVID-19 vaccination was only 67.8% [2]. Considering the powerful capability of the omicron variant to escape neutralizing antibodies elicited by current vaccines, the current vaccine acceptance rate is not enough to control the omicron variant [3,4]. It is thus necessary to investigate the negative factors that hinder the COVID-19 vaccination and take actions to increase vaccine coverage.
Vaccine acceptance is determined by contextual influences, individual/social group influences, and vaccine- and vaccination-specific issues [5]. Among all these factors, influences of infodemic and vaccine misinformation deserve more attention for the COVID-19 vaccination. An infodemic is an overabundance of information including misinformation in digital and physical environments, which makes it hard to find trustworthy sources and reliable guidance during a disease outbreak [6]. In the era of social media, the dissemination of information, especially misinformation, has been intensified [7]. During the COVID-19 pandemic, COVID-19 infodemic spread even more rapidly than the pandemic itself. The COVID-19 infodemic had jeopardized public trust in the pandemic response strategies such as vaccination and attracted attention from governments and health agencies across the world [8]. It is difficult but urgent to terminate and resolve the infodemic to promote the vaccination.
Misinformation is referred to false or inaccurate information deliberately intended to deceive [9]. It originates from rumors, websites and social media, works of fiction, governments, politicians, and vested interests [10,11]. Misinformation around COVID-19 vaccines is a noteworthy component of contextual influences on vaccine acceptance or hesitancy [12,13]. It can distort people’s perception of COVID-19 vaccines [14], exaggerate the probability of adverse events following vaccination [15], and lead to extreme political sentiments [16]. COVID-19 vaccine hesitancy, partially driven by misinformation, heavily hindered the pandemic exiting strategies worldwide.
Some reviews have summarized COVID-19–related infodemic and misinformation during the pandemic, but there is a lack of systematic evidence focusing on COVID-19 vaccine misinformation. For instance, Ries [17] synthesized the mechanisms and impacts of COVID-19 infodemic. Gabarron and colleagues [18] summarized the types of COVID-19–related misinformation and its possible consequences. A few studies focused on misinformation about COVID-19 vaccines, but they mainly evaluated its influence on vaccine hesitancy [19,20]. However, no evidence systematically summarized the distribution of COVID-19 vaccine misinformation in the population, what features it has, and how to fight against it.
Objective
We aimed to synthesize global evidence on misinformation related to COVID-19 vaccines, including its prevalence, features, influencing factors, impacts, and solutions for combating misinformation around COVID-19 vaccines. Specifically, the following questions guided our inquiry: How prevalent was COVID-19 vaccine misinformation across regions and populations? What types and features did the misinformation have? Where did the misinformation come from? How was it distributed among the general population? What factors affected misinformation believing and spreading? How did the misinformation influence vaccine hesitancy and behaviors? How to fight against vaccine misinformation in a future pandemic? This systematic review would enrich the evidence regarding vaccine misinformation and inform response strategies when new vaccines are introduced in future pandemics.
Methods
Search Strategy and Selection Criteria
According to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we conducted a systematic review of empirical articles on COVID-19 vaccine misinformation. The PRISMA checklist can be found in Multimedia Appendix 1. The review protocol was registered with PROSPERO (registration number CRD42021288929). This review was developed based on 5 peer-reviewed databases (PubMed, Embase, Web of Science, Scopus, and EBSCO). We used keywords related to COVID-19 vaccines and misinformation to identify empirical articles published in English from January 1, 2020, to August 18, 2022.
To identify the keywords of “misinformation,” we referred to the codebook by Kata [10], a widely recognized study on the classification of vaccine misinformation. We also referred to the fact sheet of COVID-19 vaccine misinformation published by the US Centers for Disease Control and Prevention (CDC) and collected the keywords on their websites to match the emerging misinformation about COVID-19 vaccines [21]. Using the keywords above, we piloted literature search in PubMed and Web of Science, and further refined the keywords according to literature searching results. The search strategy (Multimedia Appendix 2) consisted of 2 major concepts: COVID-19 vaccine and misinformation, which contains the general descriptions of misinformation (such as “misinformation,” “infodemic,” “myth”) and specified descriptions of some certain misinformation (such as “fertility,” “toxic,” “freedom”).
Original observational or interventional articles that investigated misinformation related to COVID-19 vaccines were included. We excluded studies that (1) investigated non-COVID-19 vaccines or the COVID-19 pandemic instead of COVID-19 vaccines, (2) did not investigate misinformation, and (3) did not focus on COVID-19 vaccine misinformation. We also excluded the following article types: conference abstract, editorial, letter, commentary, correspondence, study protocol, and review.
Data Screening and Extraction
We exported identified articles from databases, imported them into EndNote 20 (Clarivate Analytics), and removed the duplicates. Two reviewers (SH and SZ) first screened titles and abstracts independently to include articles meeting the inclusion criteria. The full texts of included studies after initial screening were scrutinized to assess the overall eligibility based on the inclusion and exclusion criteria by 2 independent reviewers (SH and SZ). When discrepancies in article inclusion emerged between the 2 reviewers, they engaged in discussion with a third researcher (XZ) to reach a consensus.
For eligible studies, data were independently extracted by 2 reviewers (SH and SZ), and inconsistencies or disagreements were reconciled in data extraction. Besides the study characteristics (region and period, study design, data sources, target population, sample size, and analysis methods), we extracted 4 outcomes of interest for each included study: (1) the types, sources, and prevalence of COVID-19 vaccine misinformation; (2) factors that affect the believing and spreading of COVID-19 vaccine misinformation; (3) the impact of misinformation on vaccine hesitancy and behaviors; and (4) proposed solutions for combating misinformation.
Classification of Study Types, Populations, and Phases
In this systematic review, we covered 4 types of study design: survey-based study, internet-based study, interview, and experiment. Survey-based study included cross-sectional or follow-up studies conducted among population using questionnaires; and internet-based study referred to studies that acquired publicly available information thought the internet. The prevalence and impact of COVID-19 vaccine misinformation might be different between the vaccine hesitant/refusal group and the general population. Thus, each type of studies was divided into 2 subgroups according to their study population’s prior defined attitudes toward COVID-19 vaccines: the antivaccine/vaccine hesitant group and the general population group.
To investigate the potential change in vaccine misinformation in terms of its types, contents, prevalence, and impact, we used 2 key time points to define 3 phases in this review: prevaccination phase (phase 1), from the outbreak of COVID-19 to the first dose of COVID-19 vaccines being injected at December 8, 2020 [22]; postvaccination and pre-Omicron phase (phase 2), from the end of phase 1 to the date that the new variant Omicron was officially reported (November 26, 2021) [23]; post-Omicron phase (phase 3), after November 26, 2021. If the time frame in data collection covered the time point and the ending/beginning date was not close to the time point (over 1 month), the study phase was considered to have crossed 2 phases.
Framework of Classifying Misinformation Types and Contents
Like the identification process of misinformation-related keywords, we first adapted the codebook by Kata [10] to construct a framework to classify the types and contents of COVID-19 vaccine misinformation. To cover the emerging and evolving COVID-19 vaccine infodemic, we further referred to the CDC fact sheet to revise the framework [21]. Our primary framework consisted of main classifications and contents from Kata’s work as well as contents from the CDC fact sheet. New types or contents of misinformation may have occurred when we extracted data from the included studies, and would be considered to finalize our framework. The original misinformation contents extracted from articles were rechecked using the final framework. Discrepancies in misinformation classification were discussed and reconciled.
Framework of Solutions for Combating Misinformation
For clarity and consistency in data extraction, we sorted solutions for combating misinformation into a 5-step framework, which was adapted from the disinfodemic policy brief by the United Nations Educational, Scientific and Cultural Organization (UNESCO) [24]. In this policy brief, solutions to debunk the misinformation consisted of 4-part responses: identifying misinformation, regulating producers and distributors, cutting production and distribution, and supporting the target audiences of misinformation. As the dissemination of trustworthy information deserved more attention, it was added as the fifth part of the framework.
Quality Assessment
As study designs varied across eligible studies, we used 3 kinds of quality assessment tools to assess their quality. The Appraisal tool for Cross-Sectional Studies (AXIS) was used to evaluate survey-based cross-sectional studies, and its modified version was applied to assess internet-based studies [25]. The version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) tool and the Critical Appraisal Skills Programme Checklist were used to assess methodological quality in experimental studies and interviews, respectively [26,27]. Quality assessment was conducted by 2 reviewers (SH and SZ), and the risk of bias for each eligible study was classified as “low risk,” “some concerns,” or “high risk.” The detailed scoring criteria of quality assessment are shown in Multimedia Appendix 3.
Patient and Public Involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Ethical Approval
Ethical approval was waived as this is a secondary analysis on the published articles.
Results
Basic Characteristics of Included Studies
In total, we identified 23,398 studies from 5 peer-reviewed databases (Figure 1). After removing duplicates, 8864 studies were initially screened based on their titles and abstracts, and after initial screening, 313 studies underwent full-text assessment for eligibility. A total of 102 studies met the inclusion criteria, including 91 observational studies and 11 interventional studies. According to the quality assessment criteria, the majority (90/102) of included studies were in the low risk of bias category. Eight studies were classified as “some concerns” and 4 were classified as “high risk.” The basic characteristics of included studies are presented in Table 1, and further details about each study are listed in Multimedia Appendix 4 (see also [28-71]).
Figure 1.
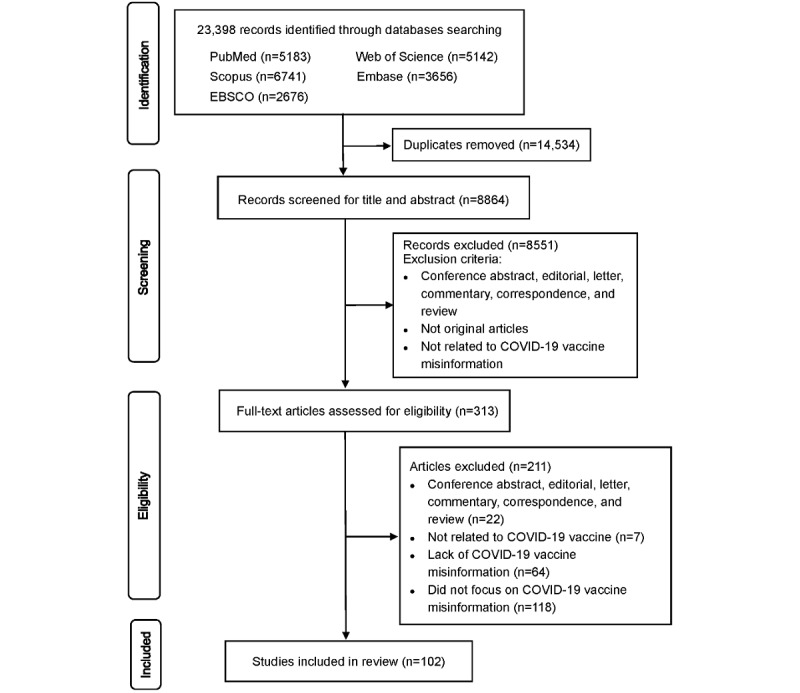
Flow diagram.
Table 1.
Basic characteristics of included articles.
| Study characteristics | Studies, n | ||||||
| Study type |
|
||||||
|
|
Observational study |
|
|
||||
|
|
|
Survey-based study |
|
38 | |||
|
|
|
Internet-based study |
|
42 | |||
|
|
|
Interview |
|
10 | |||
|
|
|
Mixed methods study |
|
1 | |||
|
|
Experimental study |
|
|
||||
|
|
|
Randomized trial |
|
9 | |||
|
|
|
Quasi trial |
|
2 | |||
| Risk of bias |
|
|
|||||
|
|
Low risk |
|
90 | ||||
|
|
Some concern |
|
8 | ||||
|
|
High risk |
|
4 | ||||
| Study phasea |
|
|
|||||
|
|
No report |
|
8 | ||||
|
|
Phase 1 |
|
28 | ||||
|
|
Phase 2 |
|
49 | ||||
|
|
Phase 3 |
|
1 | ||||
| Region |
|
|
|||||
|
|
Worldwideb |
|
26 | ||||
|
|
African |
|
6 | ||||
|
|
American |
|
25 | ||||
|
|
Eastern Mediterranean |
|
11 | ||||
|
|
European |
|
19 | ||||
|
|
South-East Asian |
|
5 | ||||
|
|
Western Pacific |
|
4 | ||||
|
|
More than 1 regionc |
|
6 | ||||
| Prior defined attitudes toward COVID-19 vaccinesd (n=80) |
|
|
|||||
|
|
Survey-based study |
|
|
||||
|
|
|
General population |
|
31 | |||
|
|
|
Antivaccine/vaccine hesitant population |
|
4 | |||
|
|
|
Both groups above |
|
3 | |||
|
|
Internet-based study |
|
|
||||
|
|
|
General online data |
|
22 | |||
|
|
|
Antivaccine/vaccine hesitant data |
|
19 | |||
|
|
|
Both groups above |
|
1 | |||
| Platform for internet-based studies (n=42) |
|
|
|||||
|
|
Social media |
|
|
||||
|
|
|
|
20 | ||||
|
|
|
YouTube |
|
5 | |||
|
|
|
|
4 | ||||
|
|
|
TikTok |
|
1 | |||
|
|
|
Parler |
|
1 | |||
|
|
|
Multiple social media platformse |
|
3 | |||
| Google Trends |
|
1 | |||||
| Google Images |
|
1 | |||||
| Internet news |
|
1 | |||||
| Online article database |
|
1 | |||||
| Multiple platformsf |
|
1 | |||||
aStudy phase was defined as follows: phase 1, from November 2019 to December 8, 2020; phase 2, from December 8, 2020, to November 26, 2021; phase 3 from November 26, 2021, to the latest ending date of data collection in included studies.
bStudies covering worldwide, including internet-based study with no limit in data collection (n=24), and survey-based study in multiple countries (n=2).
cStudies covering more than 1 region: 3 studies on American, European, and Western Pacific regions; and another 3 on American and European regions.
dStudy populations differ by their prior defined attitudes toward COVID-19 vaccines: studies reporting misinformation among the vaccine hesitancy or refusal group (“antivaccine/vaccine hesitant group” and “antivaccine/vaccine hesitant data” in the table), and studies which did not prior define the vaccine hesitancy or refusal group (“general population” and “general online data” in the table).
eMultiple social media platforms in 3 studies [28,72,73] were Facebook, Instagram, and Twitter; Instagram and Facebook; and YouTube, Twitter, Facebook, and Instagram.
fMultiple platforms included Google, Google Fact Check, Facebook, YouTube, Twitter, fact-checking agency websites, and websites of television and newspaper.
Among the 91 observational studies, 38 conducted surveys, 42 analyzed data from the internet, 10 used interviews, and the remaining 1 performed mixed methods of cross-sectional survey and interview. In terms of study region, the American region was the most studied (n=25), followed by the European (n=19) and Eastern Mediterranean (n=11) regions. By contrast, the African (n=6), South-East Asian (n=5), and Western Pacific (n=4) regions were the less investigated.
According to the prior defined attitudes toward COVID-19 vaccines in study populations, survey- and internet-based studies can be divided into the following: survey-based study on general population (n=31), survey-based study on antivaccine/vaccine hesitant population (n=4), internet-based study on general online data (n=22), and internet-based study on antivaccine/vaccine hesitant data (n=19). A total of 3 survey-based studies and 1 internet-based study reported results from both general population/data and antivaccine/vaccine hesitant population/data.
Most internet-based studies used social media platforms as data source, of which the most frequently discussed was Twitter (n=20), followed by YouTube (n=5), Facebook (n=4), TikTok (n=1), and Parler (n=1). Besides social media, 4 studies used general internet information, such as Google and online news database, as data source. A total of 4 studies used data from multiple platforms or multiple social media. Most internet-based studies did not limit the region of data source (n=24). Among those internet-based studies reporting study regions, the Americas (n=8) and Europe (n=6) were more commonly addressed, whereas the Western Pacific (n=2), Eastern Mediterranean (n=1), Africa (n=1) were less studied, leaving no internet-based study in South-East Asia. Most internet-based studies analyzed information written in English (n=33), whereas non-English information were less studied: 3 for Spanish, 2 for Arabic, 1 for both English and Spanish together, and 1 each for Chinese, Italian, and Turkish.
Types, Sources, and Prevalence of Misinformation
About 90% (91/102, 89.2%) of studies mentioned the types of COVID-19 vaccine–related misinformation. Using the coding framework mentioned in the “Methods” section, we divided vaccine-related misinformation into 7 types: conspiracy, concerns on vaccine safety and efficacy, no need for vaccines, morality, liberty, humor, and overstatement. We further divided these types into 54 different contents (Table 2). Conspiracy, being discussed in 77 studies, was the most commonly studied misinformation, and it could be further specified as vaccine existence conspiracy, political conspiracy, vaccine development and promotion conspiracy, and conspiracy related to a certain group. Concerns on vaccine safety and efficacy, emphasizing the unsubstantiated concerns on safety and efficacy, were the secondary most studied misinformation (n=63). Misinformation about the necessity of vaccines (no need for vaccines) was found in 23 studies, and its subtypes included simple claims such as vaccines are unnecessary, preference of natural immunity and protective behavior, claims about mild COVID-19, COVID-19 denial, underestimation of personal need, and overstatement of vaccine refusal. Misinformation on morality and liberty was found in 15 and 13 studies, respectively; 2 studies investigated humor and another 2 found the overstatement on the effect of COVID-19 vaccines.
Table 2.
Types and contents of COVID-19 vaccine–related misinformation.
| Type of misinformation and subtype | Explanation | Contents | |
| Conspiracy |
|
|
|
|
|
Vaccine existence conspiracy | Conspiracy about the existence of COVID-19 vaccines |
|
|
|
Political conspiracy | Conspiracy about political purpose related to the vaccines |
|
|
|
Vaccine development and promotion conspiracy | Conspiracy about COVID-19 in vaccine development and vaccination promotion |
|
|
|
Conspiracy related to a certain group | The conspiracy that vaccines will be harmful, used to control, or be tested in a specific group |
|
| Concerns on vaccine safety and efficacy | |||
|
|
Effectiveness | Beliefs that vaccines are ineffective |
|
|
|
Safety | Unsubstantiated safety concern |
|
| No need for vaccines |
|
|
|
|
|
Unnecessary | A simple claim that COVID-19 vaccines are unnecessary without explanation |
|
|
|
Natural immunity and protective behavior | Beliefs that it is better to get natural immunity or get immunity through naturally protective ways, etc. |
|
|
|
Mild COVID-19 | Believe COVID is a mild disease and no need for vaccines |
|
|
|
COVID-19 denial | Denial of COVID-19 pandemic leading to COVID-19 vaccines |
|
|
|
Personal need | Beliefs that it is unnecessary for the vaccines because of their health status |
|
|
|
Overstatement of vaccine refusal | Exaggeration about vaccine refusal rate in other places |
|
| Morality |
|
|
|
|
|
Religion | Vaccines go against religious belief, or are viewed as a sign of demon |
|
|
|
Human experiment | Vaccine campaign is a human experiment |
|
|
|
Fetal tissue | Fetal remains in vaccines |
|
| Liberty |
|
|
|
|
|
Against mandatory vaccines/control | False claims about mandatory vaccination, and refusal to obey “control” |
|
|
|
Support for freedom | Claims that vaccine infringes individual freedom |
|
|
|
Ignore consent | Concerns that children will be forced to get vaccinated without parents’ consent |
|
| Humor |
|
|
|
|
|
N/Aa | A humorous but exaggerated way to express unsubstantiated vaccine rumor |
|
| Overstatement |
|
|
|
|
|
Overstatement of the protection/progress of vaccines | Exaggeration about the effect and the scientific progress in COVID-19 vaccines |
|
aN/A: not applicable.
Vaccine-related misinformation changed in its contents over time. We compared the misinformation among 3 phases, and found that some conspiracy theories and concerns on vaccine safety circulated in all 3 phases: depopulation, control people, microchip for monitor/control, and financial incentives behind vaccine development in terms of conspiracy; vaccines would alter DNA, and cause fertility, death, or other diseases; the worry of no one would be responsible for potential side effects; beliefs in alternatives such as natural immunity and protection behaviors; referring to vaccines as immoral human experiments and comprising fetal tissue; and individual freedom. Meanwhile, there were emerging and disappearing topics on misinformation. The claims that vaccines were a hoax/fraud only appeared in phase 1. With the progress of COVID-19 vaccination, especially after the massive immunization (phase 2), misinformation about registration (false claims that some vaccines were rejected), against government control (such as fake news that some government will make COVID-19 vaccination mandatory), and conspiracy about vaccine promotion (claims that physicians or people will get financial benefit through promoting vaccination, and that the news about celebrities getting vaccinated are fake: they did not really get vaccinated; rather, they were injected with saline) emerged.
Eight studies surveyed the sources of misinformation. Three studies reported social media as main source [74-76]. Two studies found that family and friends also played a role [74,77]. One study measured proportions of different sources: social media (57.6%), followed by family or friends (13.1%), and television (5.7%) [74]. On social media, misinformation was generated majorly by antivaccine groups or well-known antivaccine individuals [78-80]. Two studies found that online celebrity tended to contribute more misinformation [80,81]. One Twitter-based study showed that the highly polarized antivaccine information was mainly from political and nonmedical users, while health care workers were less engaged in COVID-19 vaccine conversation on online platforms [78].
A total of 57 studies reported the prevalence of misinformation (Table 3), including 27 survey-based studies and 30 internet-based studies; further details on the prevalence reported in each study are presented in Multimedia Appendix 5 (see also [29,30,34,36,37,41-43,46-50,52-57,60,62,67,68,70,71]). Among 27 surveys, some investigated both general population and antivaccine groups. The 24 surveys on general population reported a prevalence of general misinformation ranging from 2.5% to 55.4%; concerning the prevalence of specific types of misinformation, conspiracy beliefs varied from 2.5% to 48.4%, concerns about vaccine safety and efficacy from 2.78% to 55.4%, “no need for vaccine” from 3.8% to 28.1%, morality from 1.4% to 20.6%, and liberty from 6% to 36.3%. A total of 6 surveys [29-32,76,82] on antivaccine/vaccine hesitant groups reported a higher prevalence of misinformation: conspiracy, 6.0%-22%; concerns on vaccine safety and efficacy, 12.2%-96.7%; and no need for vaccines, 6.3%-70.4%. The 96.7% prevalence rate was simply driven by 1 study [30] that reported the prevalence on concerns and no need for vaccines; after excluding this outlier, the prevalence of misinformation varied between 6.0% and 20.1%.
Table 3.
Prevalence of COVID-19 vaccine–related misinformation.
| Study design and subtype of misinformation | Study, n | Prevalence, % | |
| Surveys on general population | 24 | 2.5-55.4 | |
|
|
Conspiracy | 22 | 2.5-48.4 |
|
|
Concerns on vaccine safety and efficacy | 12 | 2.78-55.4 |
|
|
No need for vaccines | 6 | 3.8-28.1 |
|
|
Morality | 2 | 1.4-20.6 |
|
|
Liberty | 2 | 6-36.3 |
| Surveys on the antivaccine/vaccine hesitant group | 6 | 6.0-96.7 | |
|
|
Conspiracy | 4 | 6.0-22 |
|
|
Concerns on vaccine safety and efficacy | 4 | 12.2-96.7 |
|
|
No need for vaccines | 5 | 6.3-70.4 |
| Internet-based studies on general online data | 16 | 0.1-41.3 | |
|
|
Conspiracy | 8 | 5.3-21.7 |
|
|
Concerns on vaccine safety and efficacy | 3 | 0.4-11.1 |
|
|
No need for vaccines | 1 | 10.1 |
|
|
Morality | 2 | 3.9-20.6 |
|
|
Liberty | 1 | 41.1 |
|
|
Humor | 1 | 26 |
| Internet-based studies on antivaccine/vaccine hesitant data | 15 | 0.5-56 | |
|
|
Conspiracy | 10 | 3.9-55.4 |
|
|
Concerns on vaccine safety and efficacy | 8 | 1.3-44.8 |
|
|
No need for vaccines | 3 | 0.5-3.7 |
|
|
Morality | 2 | 2-10.4 |
|
|
Liberty | 5 | 5-46 |
Among 30 internet-based studies, 16 investigated general online data and reported the prevalence of general misinformation ranging from 0.1% to 41.3%; for the prevalence of specific types of misinformation, conspiracy ranged from 5.3% to 21.7%, concerns on vaccine safety and efficacy from 0.4% to 11.1%, humor at 26%, no need for vaccines at 10.1%, and vaccine morality from 3.9% to 20.6% (Table 3). Regarding social media platforms, YouTube showed the lowest prevalence of misinformation, ranging from 1.7% to 10.7%, and the prevalence on Twitter varied from 0.4% to 56%; the prevalence of conspiracy is 3% on TikTok and 12.44%-40% on Reddit. Humor accounted for up 26% of all COVID-19 vaccine–related videos in TikTok. In addition, antivaccine/hesitant online posts from the remaining 16 internet-based studies reported a 0.5%-56% prevalence of misinformation; specifically, conspiracy ranged from 3.9% to 55.4%, concerns on vaccine safety and efficacy from 1.3% to 44.8%, no need for vaccines from 0.5% to 3.7%, morality from 2% to 10.4%, and liberty from 5% to 46%.
Some studies reported that the prevalence of misinformation fluctuated over time, and both increasing and decreasing trends were noted [83,84]. One study showed that the change in misinformation was in close association with news or events related to vaccine developments [81].
Factors That Affect Misinformation Believing and Spreading
In total, 37 articles reported factors that affected the believing and spreading of misinformation. Textbox 1 summarizes individual characteristics and information-seeking behaviors that affect (enhance or reduce) beliefs in misinformation (n=25) as well as misinformation features that promote its spread (n=14).
Factors that affect misinformation believing and spreading.
Individual characteristics that “enhance” beliefs in misinformation
Geographic areas:
United States
Living in a village instead of a city
Age:
Younger adults
Sex:
Mixed influence
Ethnicity:
Mixed influence in the United States
Religion:
Christians
Higher level of religiosity
Socioeconomic status:
Lower education level
Lower income
Lower social economic status
Occupation:
Employed people
Political orientation:
Republicans
Conservatives
Far-right
Not being affected or vaccinated
Disease experience:
Having basic diseases
Migration experience:
Having migration experience
Psychology status and beliefs:
Depression
National narcissism
Perceived ethnic discrimination
General conspiracy-mindedness
Information-related behaviors that “enhance” beliefs in misinformation
Source of information:
Social media
Conservative media
Family and friends
Awareness of information:
Feeling less informed about science
Perceive higher incidence of fake news
Online posting:
Posting more online
Individual characteristics and information-related behaviors that “reduce” beliefs in misinformation
Occupation:
Medical workers
Channels to accessing information:
Taking lectures about COVID-19 vaccines
Trust celebrities for information
Features of misinformation that “promote” its spread
Type of misinformation:
Safety concern
Conspiracy
Efficacy concern
Content of misinformation:
Positive valence (positive emotion)
Concreteness
Format of misinformation:
Number of hashtags
Language or format that mimics news/scientific reports
Source of misinformation:
Antivaccine group
Social media influencer
Health care workers
Unregulated bot
Platform:
Different platforms present different misinformation
Newer social media
In terms of geographical areas, 2 studies found a relatively higher prevalence of misinformation in the United States [85,86]. Another study found that Wyoming had the highest level of misinformation in the United States [87]. Living in a village instead of a city was also found to relate to misinformation [88]. Concerning demographic factors, a younger age was found to enhance beliefs in misinformation in 5 studies [89]. The role of sex remained controversial: 5 studies found that females were more likely to accept conspiracy theories than males, while 2 studies found that males were more fragile [90-92]. In the United States, 2 studies found ethnic minorities were related to beliefs in misinformation [93,94], whereas 1 study found that Whites were more susceptible to misinformation than racial/ethnic minorities [91]. Christians or those with a higher level of religiosity were more likely to be influenced by misinformation [91].
Social economic status and occupation also affected beliefs in misinformation. Most studies documented that lower education and economic status were linked to accepting misinformation [89,90,92-100], although 1 study in African and Middle East countries indicated that individuals with higher education levels believed rumors such as changes in human genome due to vaccines [101]. Medical workers were less susceptible to misinformation than the general population in the UK and Jordan, and among medical workers, juniors were more susceptible to misinformation [94,102]. In addition, the unemployed were less likely to trust misinformation than the employed in the UK [91].
For political orientation, right-wing and conservative ideology would increase the conspiracy belief [90,97], and in the United States, Republicans were more likely to accept vaccine conspiracy than Independents [82,103,104]. For disease and migration experience, having basic diseases, no experience of COVID-19 infection or vaccination, and migration could enhance beliefs in misinformation [97,101]. For psychological status and beliefs, depression, perceived ethnic discrimination, national narcissism, and general conspiracy-mindedness were more likely to accept misinformation [93,97,105,106].
The following information-seeking behaviors also enhanced beliefs in misinformation: usage of social media and conservative media [1,92,107,108], posting more online [109], feeling less informed about science [97], and trusting friends or family for COVID-19 information [91]. People who take lectures about COVID-19 vaccines or trust celebrities for COVID-19 information tended to refuse misinformation [91].
In addition, some features of misinformation promoted its spread. Safety concerns, conspiracy, and efficacy concerns were reported as the most popular misinformation types [85,110]. Misinformation posts that had a higher level of positive valence and concreteness would spread [111]. The hashtags and the language or format mimicking news/scientific reports helped misinformation spread [72,110,111]. Misinformation from antivaccine groups, social media influencers, health care workers such as Sherri Tenpenny, and unregulated bots can speed its spread [79,81,112-114]. Each social media has its prevailing misinformation topics [115], and a newer social media platform was more likely to bolster vaccine conspiracy [110].
Impact of Misinformation on Vaccine Hesitancy and Behaviors
A total of 29 studies indicated that misinformation is related to vaccine hesitancy or negative vaccine perception, and 3 experimental studies also supported this finding [75,91,116]. Misinformation would ignite concerns and fears about the safety profile of vaccines and lead to vaccine hesitancy and refusal [94]. Four studies found a negative relationship between misinformation and vaccine uptake rate [84,87,89,99]. One experimental study in the UK and United States verified that the misinformation exposure significantly reduced both intentions of self-vaccination and vaccination to protect others by around 6% [91]. Skepticism also attenuated the effect of public service messages on promoting vaccination willingness [116]. Besides vaccination behaviors, misinformation reduced the uptake of self-protection behaviors such as mask wearing, distancing, and compliance with health guidance [1,90,107].
The impacts of misinformation may change across different study phases. Impacts of misinformation on protective behaviors were mainly studied in phase 1 (n=4). One study in phase 3 showed a negative relationship between some religious beliefs on COVID-19 vaccines and protective behaviors such as masks and distancing remained [99]. After mass vaccination (phase 2), the negative impact of misinformation on vaccine uptake rate was uncovered and lasted up to phase 3. The negative association of misinformation with attitudes and intention of taking vaccines was consistent among all 3 phases.
Interventions to Address Misinformation
Overview
A total of 65 studies proposed solutions to address COVID-19 vaccine misinformation, and 9 studies assessed the effects of various interventions to combat misinformation. Table 4 summarizes the proposed solutions according to our 5-step framework and specific solutions in each study are detailed in Multimedia Appendix 6 (see also [28, 31, 32, 37-41, 43-45, 48, 50, 52, 54, 56-58, 60, 63-66]).
Table 4.
Proposed solutions to address COVID-19 vaccine-related misinformation.
| Framework and meaning | Detailed solutions | No. of articles | Main actors | Targets | |
| Identifying misinformation | |||||
| Identifying misinformation through diverse channels |
|
5 | Government and health officers | Misinformation | |
| Regulating producers and distributors | |||||
| Regulating the source of misinformation |
|
3 | Political power | Sources of misinformation | |
| Cutting production and distribution | |||||
| Cutting the circulation of misinformation |
|
5 | News media, social media | Misinformation | |
|
1 | News media, social media | Misinformation | ||
|
4 | News media, social media | The public | ||
| Supporting the target audiences of misinformation | |||||
| Improving target population’s health literacy and helping the public identify misinformation |
|
13 | Multiple | Different misinformed groups | |
|
3 | Multiple | The public | ||
| Disseminating trustworthy information | |||||
| Implementing multitiered strategies to convey the message by multiple media | N/Aa | 23 | Multiple: public health agencies, medical professionals, religious leaders, etc. | The public | |
aN/A: not applicable.
Identifying Misinformation
This step contained the routine fact-check and monitoring and investigation of misinformation. A total of 7 articles emphasized that government and health officers should develop a public health surveillance system to track the emergence of misinformation and the outlets of antivaccine groups through data mining applications [97].
Regulating Producers and Distributors
Producers and distributors of misinformation need to be regulated by political power. A total of 6 articles mentioned that policy and legal actions should be implemented by the government.
Cutting Production and Distribution
This step underlined the reaction to communication platforms, including news media and social media. A total of 11 articles in our review specified this part, which consisted of technical, economic, and curatorial responses. Technical response required social media companies to build and execute more effective moderation policies, such as checking information, altering keyword searches, redirecting individuals to correct sources, banning overt conspiracy groups, and flagging or rapidly removing misinformation [104]. The economic response could be either the boycott of harmful content by advertisers or the monetization limit of the channels producing misinformation [24,108]. The curatorial response emphasized that messages should be directly debunking misinformation. The “backfire effect” (ie, factual counterargument entrenches false beliefs) was found when using debunking messages to address misinformation [117,118]. Therefore, pre-debunking message (inoculation message) before public message communication should be piloted [73,119].
Supporting the Target Audiences of Misinformation
A total of 20 studies outlined the importance of supporting the target audiences. Tailored interventions targeting different misinformed groups were considered an important approach to counter the misinformation. Empowerment of the public was recommended to improve health literacy and awareness. Public awareness campaigns were also mentioned in 2 studies [74,102].
Disseminating Trustworthy Information
This step seems similar to the curatorial response, yet it focused not only on messages that directly debunk misinformation, but also aimed to pass correct and scientific information. Most studies (n=39) mentioned or exemplified how to disseminate evidence-based information, and they recommended to mobilize trusted medical professionals and scientists to engage in social media conversation. Health care workers and public health agencies should engage in social media and learn how to produce short scientific videos [78,102,120]. Further, collaboration with social media influencers allowed a wider reach to the public [121,122]. Both social media and mass media should be utilized to spread information [123], which can express vaccine support, emphasize scientific procedure, appeal to altruism, picture the meaning and importance of vaccination, create a sense of companionship in the battle of infodemic, or encourage participation through peer pressure. Evidence-based messages should be delivered in ways understandable to individuals from a variety of socioeconomic and educational background. Therefore, youth, religious leaders, community stakeholders, faith-based organizations, and schools could be engaged to co-design culturally compelling and context-appropriate messages [85].
Although many studies proposed solutions, only 9 assessed effects of some interventions to combat misinformation. One observational study detected a limited active impact of the policies developed by Twitter [113]. Among 8 experimental studies, 4 assessed the effect of debunking message/video, 3 assessed the effect of inoculation messages, and 1 assessed the effect of warning tag/cover. All 4 experiments found that debunking message/video could reduce the belief in misinformation [118,124-126]. Yet, 1 experiment found that this effect worked well for people without strong beliefs in misinformation; when it comes to people who strongly believe in misinformation, the result became counterproductive because it may evoke small backfiring effects of vaccination intention [118]. One experiment further showed that partisans exposed to ingroup media (media held the same political preference as participants) perceived debunking messages as more credible and held higher engagement [125]. For inoculation messages, 2 experiments found that simple inoculation message/video could protect people from misinformation [119,127], while the remaining 1 found it had no significant effect, but was useful when combined with viewing or writing comments on the inoculation message [128]. In terms of warning tag/cover, interstitial warnings or cover warnings, which require individuals to click through to continue, were found to be more effective to help participants identify misinformation while warning tags showed no effect [104].
Discussion
Principal Findings
This review revealed the features, influencing factors, impacts, and solutions for COVID-19 vaccine misinformation and provided evidence to combat vaccine-related misinformation. The included articles were predominantly from American and European regions, and there was less evidence from African, South-East Asian, and Western Pacific regions. Social media was considered as the main source of COVID-19 vaccine misinformation. Conspiracy, concerns on vaccine safety and efficacy, and no need for vaccines were the most prevalent types of misinformation.
Our review documented the high but wide prevalence of COVID-19 vaccine misinformation. The great variation may be due to the ambiguity in misinformation classification and the difference across social media platforms, regions, and study participants. On social media, antivaccine or misinformation tweets accounted for 0.1%-41.3% of all vaccine-related tweets. Its prevalence varied from 2.5% to 55.4% among the general population, which was consistent with a previous review on general COVID-19 misinformation [18]. Another systematic review also illustrated that the prevalence of misinformation on general vaccines ranged from 1% to 65% on social media between 2012 and 2018 [129]. The prevalence of misinformation posed challenges to the COVID-19 vaccination. As the most prevalent type of COVID-19 vaccine misinformation, conspiracies were usually presented as half-truths, which made it hard to recognize them as misinformation. Therefore, dealing with conspiracy or skepticism should be the priority to combat the prevalent vaccine misinformation.
Social media is considered a “double-edged sword” to inform the public [7]. The endorsement of COVID-19 misinformation was strongly associated with the information sources. People who rely on print media and mainstream print were less apt to endorse COVID-19 misinformation, while the use of social media was positively associated with misperceptions regarding COVID-19 facts. In our review, as the main source of COVID-19 vaccine misinformation, social media usage was related to misinformation believing. Because of its wide usage, social media should be used to debunk misinformation and disseminate trustworthy information [121]. Public health authorities and health professionals should change their low engagement status and be more actively engaged in COVID-19 vaccine conversation on online platforms [78,120]. Social media platforms should also make rules and policies to combat misinformation [113].
The global acceptance of COVID-19 vaccine remains at a low level [2]. Misinformation is negatively associated with vaccine acceptance and self-protection behaviors. In our review, geographic areas, demographic characteristics, education, occupation, political orientation, disease and migration experience, psychological status and beliefs, and information-seeking behaviors were found to influence the believing and spreading of vaccine misinformation. However, there is less clarity on the induced pathway between these factors and misinformation. For example, the higher prevalence of COVID-19 vaccine misinformation in African and West Mediterranean regions was associated with feeling less informed, and the less informed were further linked to poor socioeconomic status, low education level, and lack of information [130]. Future research should thus focus on how these factors influence the believing and spreading of misinformation, and verify targeted populations and intervention strategies to combat vaccine misinformation.
It is urgent to implement effective intervention strategies to combat COVID-19 vaccine misinformation. Through the solutions proposed by 65 included studies, we constructed a 5-step framework to address vaccine-related misinformation. The dissemination of trustworthy information was the most frequently mentioned, followed by supporting target audiences of misinformation and cutting its production and distribution, whereas identifying misinformation and regulating its producers and distributors were less mentioned. However, most proposed solutions were not verified regarding their effects on misinformation. With the limited experimental studies, the debunking message/video was considered as effective interventions against misinformation during the COVID-19 pandemic [118,124-126].
Combating misinformation is a persistent and complex work. More scientific evidence is needed to support misinformation surveillance, punishment of misinformation producers, and dissemination of trustworthy information [24]. As many countries reported the first case of mpox, another epidemic in the shadow of the COVID-19 pandemic is looming [131]. In this context, it is particularly important to synthesize potential intervention strategies to combat vaccine misinformation for future anti-infodemic campaign.
Limitations
Our review has several limitations. First, most included studies were observational, leading to low quality of evidence. More interventional studies are needed to evaluate the effect of misinformation interventions and identify effective interventions. Second, we only included publications in English, and social media platforms in non-English languages were not included in our review. The feature, prevalence, and impact of COVID-19 vaccine misinformation may differ by languages. Third, nearly one-half of the included articles were based on the internet; however, the internet penetration rates are low in low-income countries. Our review may thus not provide enough data and evidence of COVID-19 vaccine misinformation in low-income countries. Fourth, the included studies were published from January 2020 to August 2022, therefore this period may be insufficient to observe and explore the long-term impact of COVID-19 vaccine misinformation.
Conclusion
Our review provides comprehensive and up-to-date evidence on COVID-19 vaccine misinformation and helps responses to vaccine infodemic in future pandemics. Its prevalence was high but widely varied worldwide. The most frequent misinformation types were conspiracy and concerns about vaccine safety and efficacy. Information features, information-seeking behaviors, and demographic factors influenced the spreading and believing of misinformation. More evidence is needed to verify potential intervention strategies to combat vaccine misinformation.
Acknowledgments
This work was supported by the Soft Science Research Project of Shanghai (22692107600).
Abbreviations
- AXIS
Appraisal tool for Cross-Sectional Studies
- CDC
Centers for Disease Control and Prevention
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RoB 2
version 2 of the Cochrane risk-of-bias tool for randomized trials
- UNESCO
United Nations Educational, Scientific and Cultural Organization
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Search strategy for 5 peer-reviewed databases.
Quality assessment criteria.
Characteristics of included studies.
Prevalence of COVID-19 vaccine–related misinformation by study design.
Proposed solutions to address misinformation in each study.
Footnotes
Authors' Contributions: ZH conceived the review. ZH, SZ, and XZ refined the search strategy. SZ and XZ searched for articles. SZ, SH, XZ, QW, HZ, YZ screened and extracted the articles. SZ and SH assessed the quality of the articles and analyzed data. SZ and SH wrote the first draft of the manuscript. SS revised the manuscript. ZH supervised the review process and prepared the final draft for submission. All authors read and approved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.Romer D, Jamieson KH. Patterns of Media Use, Strength of Belief in COVID-19 Conspiracy Theories, and the Prevention of COVID-19 From March to July 2020 in the United States: Survey Study. J Med Internet Res. 2021 Apr 27;23(4):e25215. doi: 10.2196/25215. https://www.jmir.org/2021/4/e25215/ v23i4e25215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Q, Hu S, Du F, Zang S, Xing Y, Qu Z, Zhang X, Lin L, Hou Z. Mapping global acceptance and uptake of COVID-19 vaccination: A systematic review and meta-analysis. Commun Med (Lond) 2022 Sep 12;2(1):113. doi: 10.1038/s43856-022-00177-6. https://europepmc.org/abstract/MED/36101704 .177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin C, Tu P, Beitsch LM. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines (Basel) 2020 Dec 30;9(1):16. doi: 10.3390/vaccines9010016. https://www.mdpi.com/resolver?pii=vaccines9010016 .vaccines9010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu L, Mok Bobo Wing Yee, Chen Lin Lei, Chan JM-C, Tsang OT-Y, Lam Bosco Hoi Shiu, Chuang Vivien Wai Man, Chu Allen Wing Ho, Chan Wan Mui, Ip Jonathan Daniel, Chan Brian Pui Chun, Zhang Ruiqi, Yip Cyril Chik Yan, Cheng Vincent Chi Chung, Chan Kwok Hung, Jin Dong Yan, Hung Ivan Fan Ngai, Yuen Kwok Yung, Chen Honglin, To Kelvin Kai Wang. Neutralization of Severe Acute Respiratory Syndrome Coronavirus 2 Omicron Variant by Sera From BNT162b2 or CoronaVac Vaccine Recipients. Clin Infect Dis. 2022 Aug 24;75(1):e822–e826. doi: 10.1093/cid/ciab1041.6463504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arede M, Bravo-Araya M, Bouchard É, Singh Gill G, Plajer V, Shehraj A, Adam Shuaib Y. Combating Vaccine Hesitancy: Teaching the Next Generation to Navigate Through the Post Truth Era. Front Public Health. 2018;6:381. doi: 10.3389/fpubh.2018.00381. https://europepmc.org/abstract/MED/30693276 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization Infodemic. 2020. [2022-11-11]. https://www.who.int/health-topics/infodemic .
- 7.Cuan-Baltazar JY, Muñoz-Perez Maria José, Robledo-Vega C, Pérez-Zepeda Maria Fernanda, Soto-Vega E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill. 2020 Apr 09;6(2):e18444. doi: 10.2196/18444. https://publichealth.jmir.org/2020/2/e18444/ v6i2e18444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang S, Pian W, Ma F, Ni Z, Liu Y. Characterizing the COVID-19 Infodemic on Chinese Social Media: Exploratory Study. JMIR Public Health Surveill. 2021 Feb 05;7(2):e26090. doi: 10.2196/26090. https://publichealth.jmir.org/2021/2/e26090/ v7i2e26090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan American Health Organization The potential of frequently used information technologies during the pandemic. 2020. [2022-11-11]. https://iris.paho.org/handle/10665.2/52021 .
- 10.Kata A. A postmodern Pandora's box: anti-vaccination misinformation on the Internet. Vaccine. 2010 Feb 17;28(7):1709–16. doi: 10.1016/j.vaccine.2009.12.022.S0264-410X(09)01926-4 [DOI] [PubMed] [Google Scholar]
- 11.Lewandowsky S, Ecker UKH, Seifert CM, Schwarz N, Cook J. Misinformation and Its Correction: Continued Influence and Successful Debiasing. Psychol Sci Public Interest. 2012 Dec;13(3):106–31. doi: 10.1177/1529100612451018.13/3/106 [DOI] [PubMed] [Google Scholar]
- 12.Sabahelzain MM, Moukhyer M, Dubé Eve, Hardan A, van den Borne B, Bosma H. Towards a further understanding of measles vaccine hesitancy in Khartoum state, Sudan: A qualitative study. PLoS One. 2019;14(6):e0213882. doi: 10.1371/journal.pone.0213882. https://dx.plos.org/10.1371/journal.pone.0213882 .PONE-D-19-05929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chou WS, Budenz A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. 2020 Dec;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 14.Blane Janice T, Bellutta Daniele, Carley Kathleen M. Social-Cyber Maneuvers During the COVID-19 Vaccine Initial Rollout: Content Analysis of Tweets. J Med Internet Res. 2022 Mar 07;24(3):e34040. doi: 10.2196/34040. https://www.jmir.org/2022/3/e34040/ v24i3e34040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herrera-Peco I, Jiménez-Gómez Beatriz, Romero Magdalena CS, Deudero JJ, García-Puente María, Benítez De Gracia Elvira, Ruiz Núñez Carlos. Antivaccine Movement and COVID-19 Negationism: A Content Analysis of Spanish-Written Messages on Twitter. Vaccines (Basel) 2021 Jun 15;9(6):656. doi: 10.3390/vaccines9060656. https://www.mdpi.com/resolver?pii=vaccines9060656 .vaccines9060656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Timothy G, Axel B, Guangnan Z. Like a virus: the coordinated spread of coronavirus disinformation. 2020. [2022-11-11]. https://doi.org/APO-305864 .
- 17.Gruber Amit, Ghiringhelli Matteo, Edri Oded, Abboud Yousef, Shiti Assad, Shaheen Naim, Ballan Nimer, Neuberger Ami, Caspi Oren. Literature Review and Knowledge Distribution During an Outbreak: A Methodology for Managing Infodemics. Acad Med. 2021 Jul 01;96(7):1005–1009. doi: 10.1097/ACM.0000000000004073.00001888-202107000-00046 [DOI] [PubMed] [Google Scholar]
- 18.Gabarron E, Oyeyemi SO, Wynn R. COVID-19-related misinformation on social media: a systematic review. Bull World Health Organ. 2021 Jun 01;99(6):455–463A. doi: 10.2471/BLT.20.276782. https://europepmc.org/abstract/MED/34108756 .BLT.20.276782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E. Misinformation About COVID-19 Vaccines on Social Media: Rapid Review. J Med Internet Res. 2022 Aug 04;24(8):e37367. doi: 10.2196/37367. https://www.jmir.org/2022/8/e37367/ v24i8e37367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lieneck C, Heinemann K, Patel J, Huynh H, Leafblad A, Moreno E, Wingfield C. Facilitators and Barriers of COVID-19 Vaccine Promotion on Social Media in the United States: A Systematic Review. Healthcare (Basel) 2022 Feb 08;10(2):321. doi: 10.3390/healthcare10020321. https://www.mdpi.com/resolver?pii=healthcare10020321 .healthcare10020321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease ControlPrevention. Myths and Facts about COVID-19 Vaccines. 2022. [2022-11-11]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/facts.html .
- 22.Taylor D. A Timeline of the Coronavirus Pandemic. 2021. [2022-11-11]. https://www.nytimes.com/article/coronavirus-timeline.html .
- 23.World Health Organization Classification of Omicron (B1.1.529): SARS-CoV-2 Variant of Concern. 2021. [2022-11-11]. https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern .
- 24.Bontcheva K, Posetti J. Disinfodemic: dissecting responses to COVID-19 disinformation. [2022-11-11]. https://unesdoc.unesco.org/ark:/48223/pf0000374417 .
- 25.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016 Dec 08;6(12):e011458. doi: 10.1136/bmjopen-2016-011458. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=27932337 .bmjopen-2016-011458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Critical Appraisal Skills Programme CASP Qualitative Checklist. [2022-11-11]. https://casp-uk.net/casp-tools-checklists/
- 27.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H, Corbett MS, Eldridge SM, Emberson JR, Hernán Miguel A, Hopewell S, Hróbjartsson Asbjørn, Junqueira DR, Jüni Peter, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;366:l4898. doi: 10.1136/bmj.l4898. https://eprints.whiterose.ac.uk/150579/ [DOI] [PubMed] [Google Scholar]
- 28.Wong Li Ping, Lin Yulan, Alias Haridah, Bakar Sazaly Abu, Zhao Qinjian, Hu Zhijian. COVID-19 Anti-Vaccine Sentiments: Analyses of Comments from Social Media. Healthcare (Basel) 2021 Dec 09;9(11):1530. doi: 10.3390/healthcare9111530. https://www.mdpi.com/resolver?pii=healthcare9111530 .healthcare9111530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Magadmi Rania M, Kamel Fatemah O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021 Jul 21;21(1):1438. doi: 10.1186/s12889-021-11501-5.10.1186/s12889-021-11501-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yousuf Hamza, van der Linden Sander, van Essen Ted, Gommers Diederik, Scherder Erik, Narula Jagat, Hofstra Leonard. Dutch Perspectives Toward Governmental Trust, Vaccination, Myths, and Knowledge About Vaccines and COVID-19. JAMA Netw Open. 2021 Dec 01;4(12):e2140529. doi: 10.1001/jamanetworkopen.2021.40529. https://europepmc.org/abstract/MED/34967887 .2787606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kricorian Katherine, Civen Rachel, Equils Ozlem. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother. 2022 Dec 31;18(1):1950504. doi: 10.1080/21645515.2021.1950504. https://europepmc.org/abstract/MED/34325612 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bíró-Nagy András, Szászi Áron József. The roots of COVID-19 vaccine hesitancy: evidence from Hungary. J Behav Med. 2022 May 14;:1–16. doi: 10.1007/s10865-022-00314-5. https://europepmc.org/abstract/MED/35567729 .10.1007/s10865-022-00314-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alliheibi FM, Omar A, Al-Horais N. Opinion Mining of Saudi Responses to COVID-19 Vaccines on Twitter: A Computational Linguistic Approach. International Journal of Advanced Computer Science and Applications. 2021;12(6):72–78. doi: 10.14569/IJACSA.2021.0120610. [DOI] [Google Scholar]
- 34.Basch Corey H, Meleo-Erwin Zoe, Fera Joseph, Jaime Christie, Basch Charles E. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Hum Vaccin Immunother. 2021 Aug 03;17(8):2373–2377. doi: 10.1080/21645515.2021.1894896. https://europepmc.org/abstract/MED/33764283 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bishnoi HR, Avasthi RD, Sharma SK. A Qualitative Study To Myths And Reality About Covid-19 Vaccination Among People In Western Rajasthan. Journal of Cardiovascular Disease Research. 2022 Apr;12(1):476–482. https://www.researchgate.net/publication/360237028_A_Qualitative_Study_To_Myths_And_Reality_About_Covid-19_Vaccination_Among_People_In_Western_Rajasthan . [Google Scholar]
- 36.Charquero-Ballester M, Walter Jg, Nissen Ia, Bechmann A. Different types of COVID-19 misinformation have different emotional valence on Twitter. Big Data & Society. 2021 Sep 22;8(2):205395172110412. doi: 10.1177/20539517211041279. [DOI] [Google Scholar]
- 37.Dereje Nebiyu, Tesfaye Abigel, Tamene Beamlak, Alemeshet Dina, Abe Haymanot, Tesfa Nathnael, Gedion Saron, Biruk Tigist, Lakew Yabets. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-method study. BMJ Open. 2022 May 30;12(5):e052432. doi: 10.1136/bmjopen-2021-052432. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=35636790 .bmjopen-2021-052432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ebrahimi Omid V, Johnson Miriam S, Ebling Sara, Amundsen Ole Myklebust, Halsøy Øyvind, Hoffart Asle, Skjerdingstad Nora, Johnson Sverre Urnes. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front Public Health. 2021;9:700213. doi: 10.3389/fpubh.2021.700213. https://europepmc.org/abstract/MED/34277557 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garcia Jonathan, Vargas Nancy, de la Torre Cynthia, Magana Alvarez Mario, Clark Jesse Lawton. Engaging Latino Families About COVID-19 Vaccines: A Qualitative Study Conducted in Oregon, USA. Health Educ Behav. 2021 Dec;48(6):747–757. doi: 10.1177/10901981211045937. https://journals.sagepub.com/doi/abs/10.1177/10901981211045937?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gesualdo Francesco, Parisi Lorenza, Croci Ileana, Comunello Francesca, Parente Andrea, Russo Luisa, Campagna Ilaria, Lanfranchi Barbara, Rota Maria Cristina, Filia Antonietta, Tozzi Alberto Eugenio, Rizzo Caterina. How the Italian Twitter Conversation on Vaccines Changed During the First Phase of the Pandemic: A Mixed-Method Analysis. Front Public Health. 2022;10:824465. doi: 10.3389/fpubh.2022.824465. https://europepmc.org/abstract/MED/35664110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffith Janessa, Marani Husayn, Monkman Helen. COVID-19 Vaccine Hesitancy in Canada: Content Analysis of Tweets Using the Theoretical Domains Framework. J Med Internet Res. 2021 Apr 13;23(4):e26874. doi: 10.2196/26874. https://www.jmir.org/2021/4/e26874/ v23i4e26874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bou Hamdan M, Singh S, Polavarapu M, Jordan Tr, Melhem Nm. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol. Infect. 2021 Nov 02;149:e242. doi: 10.1017/s0950268821002314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hernández-García Ignacio, Gascón-Giménez Irene, Gascón-Giménez Alba, Giménez-Júlvez Teresa. Information in Spanish on YouTube about Covid-19 vaccines. Hum Vaccin Immunother. 2021 Nov 02;17(11):3916–3921. doi: 10.1080/21645515.2021.1957416. https://europepmc.org/abstract/MED/34375570 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hossain Mohammad Bellal, Alam Md Zakiul, Islam Md Syful, Sultan Shafayat, Faysal Md Mahir, Rima Sharmin, Hossain Md Anwer, Mamun Abdullah Al. COVID-19 vaccine hesitancy among the adult population in Bangladesh: A nationwide cross-sectional survey. PLoS One. 2021;16(12):e0260821. doi: 10.1371/journal.pone.0260821.PONE-D-21-14374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kant R, Varea RR, Titifanue J. COVID-19 vaccine online misinformation in Fiji: Preliminary findings. Pacific Journalism Review. 2022;27(1-2):47–62. doi: 10.24135/pjr.v27i1&2.1189. https://www.researchgate.net/publication/354948870_COVID-19_vaccine_online_misinformation_in_Fiji_Preliminary_findings . [DOI] [Google Scholar]
- 46.Küçükali Hüseyin, Ataç Ömer, Palteki Ayşe Seval, Tokaç Ayşe Zülal, Hayran Osman. Vaccine Hesitancy and Anti-Vaccination Attitudes during the Start of COVID-19 Vaccination Program: A Content Analysis on Twitter Data. Vaccines (Basel) 2022 Jan 21;10(2):161. doi: 10.3390/vaccines10020161. https://www.mdpi.com/resolver?pii=vaccines10020161 .vaccines10020161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kulkarni M, Khurana K. Acceptance and myths regarding covid vaccination among general population. Medical Science. 2022;26(124):ms255e2245. doi: 10.54905/disssi/v26i124/ms255e2245. https://www.discoveryjournals.org/medicalscience/current_issue/v26/n124/ms255e2245.htm . [DOI] [Google Scholar]
- 48.Kumar Navin, Corpus Isabel, Hans Meher, Harle Nikhil, Yang Nan, McDonald Curtis, Sakai Shinpei Nakamura, Janmohamed Kamila, Chen Keyu, Altice Frederick L, Tang Weiming, Schwartz Jason L, Jones-Jang S Mo, Saha Koustuv, Memon Shahan Ali, Bauch Chris T, Choudhury Munmun De, Papakyriakopoulos Orestis, Tucker Joseph D, Goyal Abhay, Tyagi Aman, Khoshnood Kaveh, Omer Saad. COVID-19 vaccine perceptions in the initial phases of US vaccine roll-out: an observational study on reddit. BMC Public Health. 2022 Mar 07;22(1):446. doi: 10.1186/s12889-022-12824-7. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-12824-7 .10.1186/s12889-022-12824-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laforet Priscila E, Basch Corey H, Tang Hao. Understanding the content of COVID-19 vaccination and pregnancy videos on YouTube: An analysis of videos published at the start of the vaccine rollout. Hum Vaccin Immunother. 2022 Nov 30;18(5):2066935. doi: 10.1080/21645515.2022.2066935. https://europepmc.org/abstract/MED/35507867 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lamptey Emmanuel, Senkyire Ephraim Kumi, Dorcas Serwaa, Benita Dooshima Aki, Boakye Evans Osei, Ikome Theckla, Asamoah Alex. Exploring the myths surrounding the COVID-19 vaccines in Africa: the study to investigate their impacts on acceptance using online survey and social media. Clin Exp Vaccine Res. 2022 May;11(2):193–208. doi: 10.7774/cevr.2022.11.2.193. https://europepmc.org/abstract/MED/35799880 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee Sun Kyong, Sun Juhyung, Jang Seulki, Connelly Shane. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022 Aug 11;12(1):13681. doi: 10.1038/s41598-022-17430-6. doi: 10.1038/s41598-022-17430-6.10.1038/s41598-022-17430-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li Heidi Oi-Yee, Pastukhova Elena, Brandts-Longtin Olivier, Tan Marcus G, Kirchhof Mark G. YouTube as a source of misinformation on COVID-19 vaccination: a systematic analysis. BMJ Glob Health. 2022 Mar;7(3):e008334. doi: 10.1136/bmjgh-2021-008334. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=35264318 .bmjgh-2021-008334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liao TF. Understanding Anti-COVID-19 Vaccination Protest Slogans in the US. Front. Commun. 2022 Jun 30;7:941872. doi: 10.3389/fcomm.2022.941872. https://www.frontiersin.org/articles/10.3389/fcomm.2022.941872/full . [DOI] [Google Scholar]
- 54.Lurie Peter, Adams Jordan, Lynas Mark, Stockert Karen, Carlyle Robyn Correll, Pisani Amy, Evanega Sarah Davidson. COVID-19 vaccine misinformation in English-language news media: retrospective cohort study. BMJ Open. 2022 Jun 01;12(6):e058956. doi: 10.1136/bmjopen-2021-058956. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=35649595 .bmjopen-2021-058956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Muric Goran, Wu Yusong, Ferrara Emilio. COVID-19 Vaccine Hesitancy on Social Media: Building a Public Twitter Data Set of Antivaccine Content, Vaccine Misinformation, and Conspiracies. JMIR Public Health Surveill. 2021 Nov 17;7(11):e30642. doi: 10.2196/30642. https://publichealth.jmir.org/2021/11/e30642/ v7i11e30642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Neely Stephen R, Eldredge Christina, Ersing Robin, Remington Christa. Vaccine Hesitancy and Exposure to Misinformation: a Survey Analysis. J Gen Intern Med. 2022 Jan;37(1):179–187. doi: 10.1007/s11606-021-07171-z. https://europepmc.org/abstract/MED/34671900 .10.1007/s11606-021-07171-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Obreja Dragoş M. Narrative communication regarding the Covid-19 vaccine: a thematic analysis of comments on Romanian official Facebook page "RO Vaccinare". SN Soc Sci. 2022;2(8):119. doi: 10.1007/s43545-022-00427-3. https://europepmc.org/abstract/MED/35875608 .427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Okoro Olihe, Kennedy Janet, Simmons Glenn, Vosen Elyse Carter, Allen Kay, Singer Desiré, Scott Desmond, Roberts Renee. Exploring the Scope and Dimensions of Vaccine Hesitancy and Resistance to Enhance COVID-19 Vaccination in Black Communities. J Racial Ethn Health Disparities. 2022 Dec;9(6):2117–2130. doi: 10.1007/s40615-021-01150-0. https://europepmc.org/abstract/MED/34553340 .10.1007/s40615-021-01150-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Oleksy Tomasz, Wnuk Anna, Gambin Małgorzata, Łyś Agnieszka, Bargiel-Matusiewicz Kamilla, Pisula Ewa. Barriers and facilitators of willingness to vaccinate against COVID-19: Role of prosociality, authoritarianism and conspiracy mentality. A four-wave longitudinal study. Pers Individ Dif. 2022 May;190:111524. doi: 10.1016/j.paid.2022.111524. https://europepmc.org/abstract/MED/35068638 .S0191-8869(22)00027-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sallam Malik, Dababseh Deema, Eid Huda, Hasan Hanan, Taim Duaa, Al-Mahzoum Kholoud, Al-Haidar Ayat, Yaseen Alaa, Ababneh Nidaa A, Assaf Areej, Bakri Faris G, Matar Suzan, Mahafzah Azmi. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int J Environ Res Public Health. 2021 Mar 01;18(5):2407. doi: 10.3390/ijerph18052407. https://www.mdpi.com/resolver?pii=ijerph18052407 .ijerph18052407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Savolainen R. Assessing the credibility of COVID-19 vaccine mis/disinformation in online discussion. Journal of Information Science. 2021 Aug 19;:016555152110406. doi: 10.1177/01655515211040653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thelwall M, Kousha K, Thelwall S. Covid-19 vaccine hesitancy on English-language Twitter. El Profesional de la Información. 2021;30(2):1–13. doi: 10.3145/epi.2021.mar.12. [DOI] [Google Scholar]
- 63.Wang Chia-Wen, de Jong Erik Pieter, Faure Josemyrne Ashley, Ellington Jaylynn Leigh, Chen Chi-Hsin Sally, Chan Chang-Chuan. A matter of trust: a qualitative comparison of the determinants of COVID-19 vaccine hesitancy in Taiwan, the United States, the Netherlands, and Haiti. Hum Vaccin Immunother. 2022 Nov 30;18(5):2050121. doi: 10.1080/21645515.2022.2050121. https://europepmc.org/abstract/MED/35349382 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Watermeyer Jennifer, Scott Megan, Kapueja Lethu, Ware Lisa Jayne. To trust or not to trust: an exploratory qualitative study of personal and community perceptions of vaccines amongst a group of young community healthcare workers in Soweto, South Africa. Health Policy Plan. 2022 Oct 12;37(9):1167–1176. doi: 10.1093/heapol/czac060. https://europepmc.org/abstract/MED/35880606 .6649996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wawrzuta Dominik, Jaworski Mariusz, Gotlib Joanna, Panczyk Mariusz. What Arguments against COVID-19 Vaccines Run on Facebook in Poland: Content Analysis of Comments. Vaccines (Basel) 2021 May 10;9(5):481. doi: 10.3390/vaccines9050481. https://www.mdpi.com/resolver?pii=vaccines9050481 .vaccines9050481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wonodi Chizoba, Obi-Jeff Chisom, Adewumi Funmilayo, Keluo-Udeke Somto Chloe, Gur-Arie Rachel, Krubiner Carleigh, Jaffe Elana Felice, Bamiduro Tobi, Karron Ruth, Faden Ruth. Conspiracy theories and misinformation about COVID-19 in Nigeria: Implications for vaccine demand generation communications. Vaccine. 2022 Mar 18;40(13):2114–2121. doi: 10.1016/j.vaccine.2022.02.005. https://linkinghub.elsevier.com/retrieve/pii/S0264-410X(22)00126-8 .S0264-410X(22)00126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wu Wei, Lyu Hanjia, Luo Jiebo. Characterizing Discourse about COVID-19 Vaccines: A Reddit Version of the Pandemic Story. Health Data Sci. 2021;2021:9837856. doi: 10.34133/2021/9837856. https://europepmc.org/abstract/MED/36405359 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yang Zheng, Luo Xi, Jia Hepeng. Is It All a Conspiracy? Conspiracy Theories and People's Attitude to COVID-19 Vaccination. Vaccines (Basel) 2021 Sep 22;9(10):1051. doi: 10.3390/vaccines9101051. https://www.mdpi.com/resolver?pii=vaccines9101051 .vaccines9101051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yaseen Muhammad Osama, Saif Arifa, Khan Tahir Mehmood, Yaseen Misha, Saif Alia, Bukhsh Allah, Shahid Muhammad Nabeel, Alsenani Faisal, Tahir Humera, Ming Long Chiau, Amin Muhammad Usman, Suleiman Amal K, Al-Worafi Yaser Mohammed, Baig Mirza Rafi, Saeed Imran Muhammad, Jaber Ammar A. A qualitative insight into the perceptions and COVID-19 vaccine hesitancy among Pakistani pharmacists. Hum Vaccin Immunother. 2022 Dec 31;18(1):2031455. doi: 10.1080/21645515.2022.2031455. https://europepmc.org/abstract/MED/35192781 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abbas SW, Zareen SF, Nisar S, Farooq A, Rasheed A, Saleem MU. COVID-19 Vaccines: Community Myths Vs Facts. Pakistan Armed Forces Medical Journal. 2022;72(2):497–500. doi: 10.51253/pafmj.v72i2.6970. https://www.pafmj.org/index.php/PAFMJ/article/view/6970/3999 . [DOI] [Google Scholar]
- 71.Al-Rawi Ahmed, Fakida Abdelrahman, Grounds Kelly. Investigation of COVID-19 Misinformation in Arabic on Twitter: Content Analysis. JMIR Infodemiology. 2022;2(2):e37007–500. doi: 10.2196/37007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9327499/pdf/infodemiology_v2i2e37007.pdf .v2i2e37007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ngai CSB, Singh RG, Yao L. Impact of COVID-19 Vaccine Misinformation on Social Media Virality: Content Analysis of Message Themes and Writing Strategies. J Med Internet Res. 2022 Jul 06;24(7):e37806. doi: 10.2196/37806.v24i7e37806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hughes B, Miller-Idriss C, Piltch-Loeb R, Goldberg B, White K, Criezis M, Savoia E. Development of a Codebook of Online Anti-Vaccination Rhetoric to Manage COVID-19 Vaccine Misinformation. Int J Environ Res Public Health. 2021 Jul 15;18(14):7556. doi: 10.3390/ijerph18147556. https://www.mdpi.com/resolver?pii=ijerph18147556 .ijerph18147556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Arshad MS, Hussain I, Mahmood T, Hayat K, Majeed A, Imran I, Saeed H, Iqbal MO, Uzair M, Rehman AU, Ashraf W, Usman A, Syed SK, Akbar M, Chaudhry MO, Ramzan B, Islam M, Saleem MU, Shakeel W, Iqbal I, Hashmi F, Rasool MF. A National Survey to Assess the COVID-19 Vaccine-Related Conspiracy Beliefs, Acceptability, Preference, and Willingness to Pay among the General Population of Pakistan. Vaccines (Basel) 2021 Jul 01;9(7):720. doi: 10.3390/vaccines9070720. https://www.mdpi.com/resolver?pii=vaccines9070720 .vaccines9070720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thaker J, Subramanian A. Exposure to COVID-19 Vaccine Hesitancy Is as Impactful as Vaccine Misinformation in Inducing a Decline in Vaccination Intentions in New Zealand: Results from Pre-Post Between-Groups Randomized Block Experiment. Front. Commun. 2021 Aug 19;6:721982. doi: 10.3389/fcomm.2021.721982. [DOI] [Google Scholar]
- 76.Solís Arce Julio S, Warren Shana S, Meriggi Niccolò F, Scacco Alexandra, McMurry Nina, Voors Maarten, Syunyaev Georgiy, Malik Amyn Abdul, Aboutajdine Samya, Adeojo Opeyemi, Anigo Deborah, Armand Alex, Asad Saher, Atyera Martin, Augsburg Britta, Awasthi Manisha, Ayesiga Gloria Eden, Bancalari Antonella, Björkman Nyqvist Martina, Borisova Ekaterina, Bosancianu Constantin Manuel, Cabra García Magarita Rosa, Cheema Ali, Collins Elliott, Cuccaro Filippo, Farooqi Ahsan Zia, Fatima Tatheer, Fracchia Mattia, Galindo Soria Mery Len, Guariso Andrea, Hasanain Ali, Jaramillo Sofía, Kallon Sellu, Kamwesigye Anthony, Kharel Arjun, Kreps Sarah, Levine Madison, Littman Rebecca, Malik Mohammad, Manirabaruta Gisele, Mfura Jean Léodomir Habarimana, Momoh Fatoma, Mucauque Alberto, Mussa Imamo, Nsabimana Jean Aime, Obara Isaac, Otálora María Juliana, Ouédraogo Béchir Wendemi, Pare Touba Bakary, Platas Melina R, Polanco Laura, Qureshi Javaeria Ashraf, Raheem Mariam, Ramakrishna Vasudha, Rendrá Ismail, Shah Taimur, Shaked Sarene Eyla, Shapiro Jacob N, Svensson Jakob, Tariq Ahsan, Tchibozo Achille Mignondo, Tiwana Hamid Ali, Trivedi Bhartendu, Vernot Corey, Vicente Pedro C, Weissinger Laurin B, Zafar Basit, Zhang Baobao, Karlan Dean, Callen Michael, Teachout Matthieu, Humphreys Macartan, Mobarak Ahmed Mushfiq, Omer Saad B. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021 Aug;27(8):1385–1394. doi: 10.1038/s41591-021-01454-y. https://europepmc.org/abstract/MED/34272499 .10.1038/s41591-021-01454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Magee L, Knights F, Mckechnie DGJ, Al-Bedaery Roaa, Razai MS. Facilitators and barriers to COVID-19 vaccination uptake among ethnic minorities: A qualitative study in primary care. PLoS One. 2022;17(7):e0270504. doi: 10.1371/journal.pone.0270504. https://dx.plos.org/10.1371/journal.pone.0270504 .PONE-D-22-03174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hernandez RG, Hagen L, Walker K, O'Leary Heather, Lengacher C. The COVID-19 vaccine social media : healthcare providers' missed dose in addressing misinformation and vaccine hesitancy. Hum Vaccin Immunother. 2021 Sep 02;17(9):2962–2964. doi: 10.1080/21645515.2021.1912551. https://europepmc.org/abstract/MED/33890838 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jemielniak D, Krempovych Y. An analysis of AstraZeneca COVID-19 vaccine misinformation and fear mongering on Twitter. Public Health. 2021 Nov;200:4–6. doi: 10.1016/j.puhe.2021.08.019. https://europepmc.org/abstract/MED/34628307 .S0033-3506(21)00346-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Calac AJ, Haupt MR, Li Z, Mackey T. Spread of COVID-19 Vaccine Misinformation in the Ninth Inning: Retrospective Observational Infodemic Study. JMIR Infodemiology. 2022;2(1):e33587. doi: 10.2196/33587. https://europepmc.org/abstract/MED/35320982 .v2i1e33587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jiang LC, Chu TH, Sun M. Characterization of Vaccine Tweets During the Early Stage of the COVID-19 Outbreak in the United States: Topic Modeling Analysis. JMIR Infodemiology. 2021;1(1):e25636. doi: 10.2196/25636. https://europepmc.org/abstract/MED/34604707 .v1i1e25636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021 Feb 12;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. http://europepmc.org/abstract/MED/33461833 .S0264-410X(21)00014-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.An L, Russell DM, Mihalcea R, Bacon E, Huffman S, Resnicow K. Online Search Behavior Related to COVID-19 Vaccines: Infodemiology Study. JMIR Infodemiology. 2021;1(1):e32127. doi: 10.2196/32127. https://europepmc.org/abstract/MED/34841200 .v1i1e32127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen Y, Chen Y, Yang K, Lai F, Huang C, Chen Y, Tu Y. The Prevalence and Impact of Fake News on COVID-19 Vaccination in Taiwan: Retrospective Study of Digital Media. J Med Internet Res. 2022 Apr 26;24(4):e36830. doi: 10.2196/36830. https://www.jmir.org/2022/4/e36830/ v24i4e36830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Islam MS, Kamal AM, Kabir A, Southern DL, Khan SH, Hasan SMM, Sarkar T, Sharmin S, Das S, Roy T, Harun MGD, Chughtai AA, Homaira N, Seale H. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021;16(5):e0251605. doi: 10.1371/journal.pone.0251605. https://dx.plos.org/10.1371/journal.pone.0251605 .PONE-D-21-06301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Savoia E, Harriman NW, Piltch-Loeb R, Bonetti M, Toffolutti V, Testa MA. Exploring the Association between Misinformation Endorsement, Opinions on the Government Response, Risk Perception, and COVID-19 Vaccine Hesitancy in the US, Canada, and Italy. Vaccines (Basel) 2022 Apr 23;10(5):671. doi: 10.3390/vaccines10050671. https://www.mdpi.com/resolver?pii=vaccines10050671 .vaccines10050671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pierri F, Perry BL, DeVerna MR, Yang K, Flammini A, Menczer F, Bryden J. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci Rep. 2022 Apr 26;12(1):5966. doi: 10.1038/s41598-022-10070-w. doi: 10.1038/s41598-022-10070-w.10.1038/s41598-022-10070-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hammad AM, Al-Qerem W, Abu Zaid A, Khdair SI, Hall FS. Misconceptions Related to COVID 19 Vaccines Among the Jordanian Population: Myth and Public Health. Disaster Med Public Health Prep. 2022 Jun 08;:1–8. doi: 10.1017/dmp.2022.143. https://europepmc.org/abstract/MED/35673791 .S1935789322001434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Eshel Y, Kimhi S, Marciano H, Adini B. Conspiracy claims and secret intentions as predictors of psychological coping and vaccine uptake during the COVID-19 pandemic. J Psychiatr Res. 2022 Jul;151:311–318. doi: 10.1016/j.jpsychires.2022.04.042. https://europepmc.org/abstract/MED/35526447 .S0022-3956(22)00245-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hornsey MJ, Chapman CM, Alvarez B, Bentley S, Salvador Casara BG, Crimston CR, Ionescu O, Krug H, Preya Selvanathan H, Steffens NK, Jetten J. To what extent are conspiracy theorists concerned for self versus others? A COVID-19 test case. Eur J Soc Psychol. 2021 Mar;51(2):285–293. doi: 10.1002/ejsp.2737. https://europepmc.org/abstract/MED/33821057 .EJSP2737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021 Mar;5(3):337–348. doi: 10.1038/s41562-021-01056-1.10.1038/s41562-021-01056-1 [DOI] [PubMed] [Google Scholar]
- 92.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines (Basel) 2021 Jan 12;9(1):42. doi: 10.3390/vaccines9010042. https://www.mdpi.com/resolver?pii=vaccines9010042 .vaccines9010042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Andrade G. Covid-19 vaccine hesitancy, conspiracist beliefs, paranoid ideation and perceived ethnic discrimination in a sample of University students in Venezuela. Vaccine. 2021 Nov 16;39(47):6837–6842. doi: 10.1016/j.vaccine.2021.10.037. https://europepmc.org/abstract/MED/34711439 .S0264-410X(21)01371-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Manby L, Dowrick A, Karia A, Maio L, Buck C, Singleton G, Lewis-Jackson S, Uddin I, Vanderslott S, Martin S, Vindrola-Padros C. Healthcare workers’ perceptions and attitudes towards the UK’s COVID-19 vaccination programme: a rapid qualitative appraisal. BMJ Open. 2022 Feb 15;12(2):e051775. doi: 10.1136/bmjopen-2021-051775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mahmud MR, Bin Reza R, Ahmed SZ. The effects of misinformation on COVID-19 vaccine hesitancy in Bangladesh. GKMC. 2021 Oct 24;:ahead-of-print. doi: 10.1108/gkmc-05-2021-0080. [DOI] [Google Scholar]
- 96.Buturoiu R, Udrea G, Oprea D, Corbu N. Who Believes in Conspiracy Theories about the COVID-19 Pandemic in Romania? An Analysis of Conspiracy Theories Believers’ Profiles. Societies. 2021 Nov 13;11(4):138. doi: 10.3390/soc11040138. [DOI] [Google Scholar]
- 97.Jensen EA, Pfleger A, Herbig L, Wagoner B, Lorenz L, Watzlawik M. What Drives Belief in Vaccination Conspiracy Theories in Germany? Front. Commun. 2021 May 25;6:105. doi: 10.3389/fcomm.2021.678335. [DOI] [Google Scholar]
- 98.Caycho-Rodríguez T, Ventura-León J, Valencia PD, Vilca LW, Carbajal-León C, Reyes-Bossio M, White M, Rojas-Jara C, Polanco-Carrasco R, Gallegos M, Cervigni M, Martino P, Palacios DA, Moreta-Herrera R, Samaniego-Pinho A, Lobos Rivera ME, Buschiazzo Figares A, Puerta-Cortés DX, Corrales-Reyes IE, Calderón R, Pinto Tapia B, Arias Gallegos WL, Petzold O. What Is the Support for Conspiracy Beliefs About COVID-19 Vaccines in Latin America? A Prospective Exploratory Study in 13 Countries. Front. Psychol. 2022 May 6;13:105. doi: 10.3389/fpsyg.2022.855713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Exline JJ, Pait KC, Wilt JA, Schutt WA. Demonic and Divine Attributions around COVID-19 Vaccines: Links with Vaccine Attitudes and Behaviors, QAnon and Conspiracy Beliefs, Anger, Spiritual Struggles, Religious and Political Variables, and Supernatural and Apocalyptic Beliefs. Religions. 2022 Jun 06;13(6):519. doi: 10.3390/rel13060519. [DOI] [Google Scholar]
- 100.Lin F, Chen X, Cheng EW. Contextualized impacts of an infodemic on vaccine hesitancy: The moderating role of socioeconomic and cultural factors. Information Processing & Management. 2022 Sep;59(5):103013. doi: 10.1016/j.ipm.2022.103013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Asadi Faezi N, Gholizadeh P, Sanogo M, Oumarou A, Mohamed MN, Cissoko Y, Saliou Sow M, Keita BS, Baye YAM, Pagliano P, Akouda P, Soufiane S, Iknane AA, Safiatou Diallo MO, Gansane Z, Ali Khan B, Köse Şükran, Allahverdipour H, Ganvarov K, Soumaré Mariam, Asgharzadeh M, Dao S, Samadi Kafil H. Peoples' attitude toward COVID-19 vaccine, acceptance, and social trust among African and Middle East countries. Health Promot Perspect. 2021;11(2):171–178. doi: 10.34172/hpp.2021.21. https://europepmc.org/abstract/MED/34195040 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Aloweidi A, Bsisu I, Suleiman A, Abu-Halaweh S, Almustafa M, Aqel M, Amro A, Radwan N, Assaf D, Abdullah MZ, Albataineh M, Mahasneh A, Badaineh A, Obeidat H. Hesitancy towards COVID-19 Vaccines: An Analytical Cross-Sectional Study. Int J Environ Res Public Health. 2021 May 12;18(10):5111. doi: 10.3390/ijerph18105111. https://www.mdpi.com/resolver?pii=ijerph18105111 .ijerph18105111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pierri F, Perry B, DeVerna M, Yang K, Flammini A, Menczer F, Bryden John. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci Rep. 2022 Apr 26;12(1):5966. doi: 10.1038/s41598-022-10070-w. doi: 10.1038/s41598-022-10070-w.10.1038/s41598-022-10070-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sharevski F, Alsaadi R, Jachim P, Pieroni E. Misinformation warnings: Twitter's soft moderation effects on COVID-19 vaccine belief echoes. Comput Secur. 2022 Mar;114:102577. doi: 10.1016/j.cose.2021.102577. https://europepmc.org/abstract/MED/34934255 .S0167-4048(21)00401-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Marchlewska M, Hamer K, Baran M, Górska Paulina, Kaniasty K. COVID-19: Why Do People Refuse Vaccination? The Role of Social Identities and Conspiracy Beliefs: Evidence from Nationwide Samples of Polish Adults. Vaccines (Basel) 2022 Feb 10;10(2):268. doi: 10.3390/vaccines10020268. https://www.mdpi.com/resolver?pii=vaccines10020268 .vaccines10020268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Perlis RH, Ognyanova K, Santillana M, Lin J, Druckman J, Lazer D, Green J, Simonson M, Baum MA, Della Volpe J. Association of Major Depressive Symptoms With Endorsement of COVID-19 Vaccine Misinformation Among US Adults. JAMA Netw Open. 2022 Jan 04;5(1):e2145697. doi: 10.1001/jamanetworkopen.2021.45697. https://europepmc.org/abstract/MED/35061036 .2788284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020 Oct;263:113356. doi: 10.1016/j.socscimed.2020.113356. https://linkinghub.elsevier.com/retrieve/pii/S0277-9536(20)30575-X .S0277-9536(20)30575-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jennings W, Stoker G, Bunting H, Valgarðsson Viktor Orri, Gaskell J, Devine D, McKay L, Mills MC. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines (Basel) 2021 Jun 03;9(6):593. doi: 10.3390/vaccines9060593. https://www.mdpi.com/resolver?pii=vaccines9060593 .vaccines9060593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kumar M, Madhumathi J, Gayathri K, A Rozario Amanda G, Vijayaprabha R, Balusamy M, Sonekar H, Panda S. Community voices around COVID-19 vaccine in Chennai, India: A qualitative exploration during early phase of vaccine rollout. Indian J Med Res. 2022;155(5&6):451–460. doi: 10.4103/ijmr.ijmr_668_22.353889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baines A, Ittefaq M, Abwao M. #Scamdemic, #Plandemic, or #Scaredemic: What Parler Social Media Platform Tells Us about COVID-19 Vaccine. Vaccines (Basel) 2021 Apr 22;9(5):421. doi: 10.3390/vaccines9050421. https://www.mdpi.com/resolver?pii=vaccines9050421 .vaccines9050421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Saini V, Liang L, Yang Y, Le HM, Wu C. The Association Between Dissemination and Characteristics of Pro-/Anti-COVID-19 Vaccine Messages on Twitter: Application of the Elaboration Likelihood Model. JMIR Infodemiology. 2022;2(1):e37077. doi: 10.2196/37077. https://europepmc.org/abstract/MED/35783451 .v2i1e37077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lanyi K, Green R, Craig D, Marshall C. COVID-19 Vaccine Hesitancy: Analysing Twitter to Identify Barriers to Vaccination in a Low Uptake Region of the UK. Front Digit Health. 2021;3:804855. doi: 10.3389/fdgth.2021.804855. http://europepmc.org/abstract/MED/35141699 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Larrondo-Ureta A, Fernández S, Morales-i-Gras J. Desinformación, vacunas y Covid-19. Análisis de la infodemia y la conversación digital en Twitter. RLCS. 2021 Jun 07;(79):1–18. doi: 10.4185/rlcs-2021-1504. [DOI] [Google Scholar]
- 114.Kalichman S, Eaton L, Earnshaw V, Brousseau N. Faster than warp speed: early attention to COVD-19 by anti-vaccine groups on Facebook. J Public Health (Oxf) 2022 Mar 07;44(1):e96–e105. doi: 10.1093/pubmed/fdab093. https://europepmc.org/abstract/MED/33837428 .6218921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wawrzuta D, Klejdysz J, Jaworski M, Gotlib J, Panczyk M. Attitudes toward COVID-19 Vaccination on Social Media: A Cross-Platform Analysis. Vaccines (Basel) 2022 Jul 27;10(8):1190. doi: 10.3390/vaccines10081190. https://www.mdpi.com/resolver?pii=vaccines10081190 .vaccines10081190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jin Q, Raza SH, Yousaf M, Zaman U, Siang JMLD. Can Communication Strategies Combat COVID-19 Vaccine Hesitancy with Trade-Off between Public Service Messages and Public Skepticism? Experimental Evidence from Pakistan. Vaccines (Basel) 2021 Jul 07;9(7):757. doi: 10.3390/vaccines9070757. https://www.mdpi.com/resolver?pii=vaccines9070757 .vaccines9070757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, van der Linden S. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020 Oct;7(10):201199. doi: 10.1098/rsos.201199. https://royalsocietypublishing.org/doi/10.1098/rsos.201199?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .rsos201199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Helfers A, Ebersbach M. The differential effects of a governmental debunking campaign concerning COVID-19 vaccination misinformation. Journal of Communication in Healthcare. 2022 Mar 17;:1–9. doi: 10.1080/17538068.2022.2047497. [DOI] [PubMed] [Google Scholar]
- 119.Vivion M, Anassour Laouan Sidi E, Betsch C, Dionne M, Dubé E, Driedger SM, Gagnon D, Graham J, Greyson D, Hamel D, Lewandowsky S, MacDonald N, Malo B, Meyer SB, Schmid P, Steenbeek A, van der Linden S, Verger P, Witteman HO, Yesilada M. Prebunking messaging to inoculate against COVID-19 vaccine misinformation: an effective strategy for public health. Journal of Communication in Healthcare. 2022 Mar 04;15(3):232–242. doi: 10.1080/17538068.2022.2044606. [DOI] [Google Scholar]
- 120.Basch CH, Hillyer GC, Zagnit EA, Basch CE. YouTube coverage of COVID-19 vaccine development: implications for awareness and uptake. Hum Vaccin Immunother. 2020 Nov 01;16(11):2582–2585. doi: 10.1080/21645515.2020.1790280. http://europepmc.org/abstract/MED/32701403 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chan C, Sounderajah V, Daniels E, Acharya A, Clarke J, Yalamanchili S, Normahani P, Markar S, Ashrafian H, Darzi A. The Reliability and Quality of YouTube Videos as a Source of Public Health Information Regarding COVID-19 Vaccination: Cross-sectional Study. JMIR Public Health Surveill. 2021 Jul 08;7(7):e29942. doi: 10.2196/29942. https://publichealth.jmir.org/2021/7/e29942/ v7i7e29942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Criss S, Nguyen TT, Norton S, Virani I, Titherington E, Tillmanns EL, Kinnane C, Maiolo G, Kirby AB, Gee GC. Advocacy, Hesitancy, and Equity: Exploring U.S. Race-Related Discussions of the COVID-19 Vaccine on Twitter. Int J Environ Res Public Health. 2021 May 26;18(11):5693. doi: 10.3390/ijerph18115693. https://www.mdpi.com/resolver?pii=ijerph18115693 .ijerph18115693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ginossar T, Cruickshank IJ, Zheleva E, Sulskis J, Berger-Wolf T. Cross-platform spread: vaccine-related content, sources, and conspiracy theories in YouTube videos shared in early Twitter COVID-19 conversations. Hum Vaccin Immunother. 2022 Dec 31;18(1):1–13. doi: 10.1080/21645515.2021.2003647. https://europepmc.org/abstract/MED/35061560 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yousuf H, van der Linden S, Bredius L, Ted van Essen G A, Sweep G, Preminger Z, van Gorp E, Scherder E, Narula J, Hofstra L. A media intervention applying debunking versus non-debunking content to combat vaccine misinformation in elderly in the Netherlands: A digital randomised trial. EClinicalMedicine. 2021 May;35:100881. doi: 10.1016/j.eclinm.2021.100881. https://linkinghub.elsevier.com/retrieve/pii/S2589-5370(21)00161-9 .S2589-5370(21)00161-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lu S, Zhong L. From Believing to Sharingxamining the Effects of Partisan Media's Correction of COVID-19 Vaccine Misinformation. INTERNATIONAL JOURNAL OF COMMUNICATION. 2022 2022. 2022 Jun 15;:16. [Google Scholar]
- 126.Talabi F, Ugbor I, Talabi M, Ugwuoke J, Oloyede D, Aiyesimoju A, Ikechukwu-Ilomuanya Amaka B. Effect of a social media-based counselling intervention in countering fake news on COVID-19 vaccine in Nigeria. Health Promot Int. 2022 Apr 29;37(2):daab140. doi: 10.1093/heapro/daab140.6369161 [DOI] [PubMed] [Google Scholar]
- 127.Piltch-Loeb R, Su M, Hughes B, Testa M, Goldberg B, Braddock K, Miller-Idriss C, Maturo V, Savoia E. Testing the Efficacy of Attitudinal Inoculation Videos to Enhance COVID-19 Vaccine Acceptance: Quasi-Experimental Intervention Trial. JMIR Public Health Surveill. 2022 Jun 20;8(6):e34615. doi: 10.2196/34615. https://publichealth.jmir.org/2022/6/e34615/ v8i6e34615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dai Y(, Jia W, Fu L, Sun M, Jiang LC. The effects of self-generated and other-generated eWOM in inoculating against misinformation. Telematics and Informatics. 2022 Jul;71:101835. doi: 10.1016/j.tele.2022.101835. [DOI] [Google Scholar]
- 129.Suarez-Lledo V, Alvarez-Galvez J. Prevalence of Health Misinformation on Social Media: Systematic Review. J Med Internet Res. 2021 Jan 20;23(1):e17187. doi: 10.2196/17187. https://www.jmir.org/2021/1/e17187/ v23i1e17187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Abdulai A, Tiffere A, Adam F, Kabanunye MM. COVID-19 information-related digital literacy among online health consumers in a low-income country. Int J Med Inform. 2021 Jan;145:104322. doi: 10.1016/j.ijmedinf.2020.104322.S1386-5056(20)31071-6 [DOI] [PubMed] [Google Scholar]
- 131.Hasan Shamimul, Saeed Shazina. Monkeypox Disease: An Emerging Public Health Concern in the Shadow of COVID-19 Pandemic: An Update. Trop Med Infect Dis. 2022 Oct 03;7(10):283. doi: 10.3390/tropicalmed7100283. https://www.mdpi.com/resolver?pii=tropicalmed7100283 .tropicalmed7100283 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Search strategy for 5 peer-reviewed databases.
Quality assessment criteria.
Characteristics of included studies.
Prevalence of COVID-19 vaccine–related misinformation by study design.
Proposed solutions to address misinformation in each study.


