To the Editor,
Bleeding and thrombotic complications are major risks of extracorporeal membrane oxygenation (ECMO). Thrombosis due to blood contact with the extracorporeal circuit exacerbates inflammation, potentially leading to thromboembolism and/or end organ dysfunction,1 whereas anticoagulation increases the risk of fatal and nonfatal bleeding. Therefore, a meticulous balance between bleeding and clotting must be carefully maintained for ECMO patients.
Although unfractionated heparin (UFH) is the most commonly used strategy because of its rapid onset and easy neutralization, a paucity of published data exists regarding anticoagulation in ECMO patients.2, 3 In the current study, we sought to describe our single-centre experience with various anticoagulation strategies used for ECMO.
We conducted a retrospective chart review of patients receiving venovenous (VV) or venoarterial (VA) ECMO from 1 September 1996 to 31 March 2019. Anticoagulation strategies were categorized into UFH, therapeutic low-molecular weight heparin (LMWH), direct thrombin inhibitors (DTI), or venous thromboembolism prophylaxis-dose anticoagulation. The choice of anticoagulation was at the discretion of the physician. Heparin-coated circuit tubing was used for all ECMO cannulations.
The primary outcome was a composite of thrombotic events including device-related complications (need for circuit change), and patient-related complications (arterial or venous thrombus). Secondary outcomes included survival to discharge, surgical exploration for bleeding, and any actionable bleed defined by a Bleeding Academic Research Consortium (BARC) score of 2 or greater.4
We identified a total of 185 patients; 68% were male and the median age was 56 years. Unfractionated heparin was the most common anticoagulation strategy (73%), followed by prophylaxis-only dosing of heparin/LMWH (22%). Therapeutic LMWH and DTI were used in a minority of patients. Baseline characteristics differed between UFH and prophylaxis-only anticoagulation groups, including history of atrial fibrillation/flutter (8.1% vs 28.6%, P = 0.001); dyslipidemia (31.1% vs 52.4%, P = 0.02); warfarin as a home medication (10.4% vs 23.8%, P = 0.04); and precannulation serum potassium (mmol·L−1) (4.10 vs 4.40, P = 0.03).
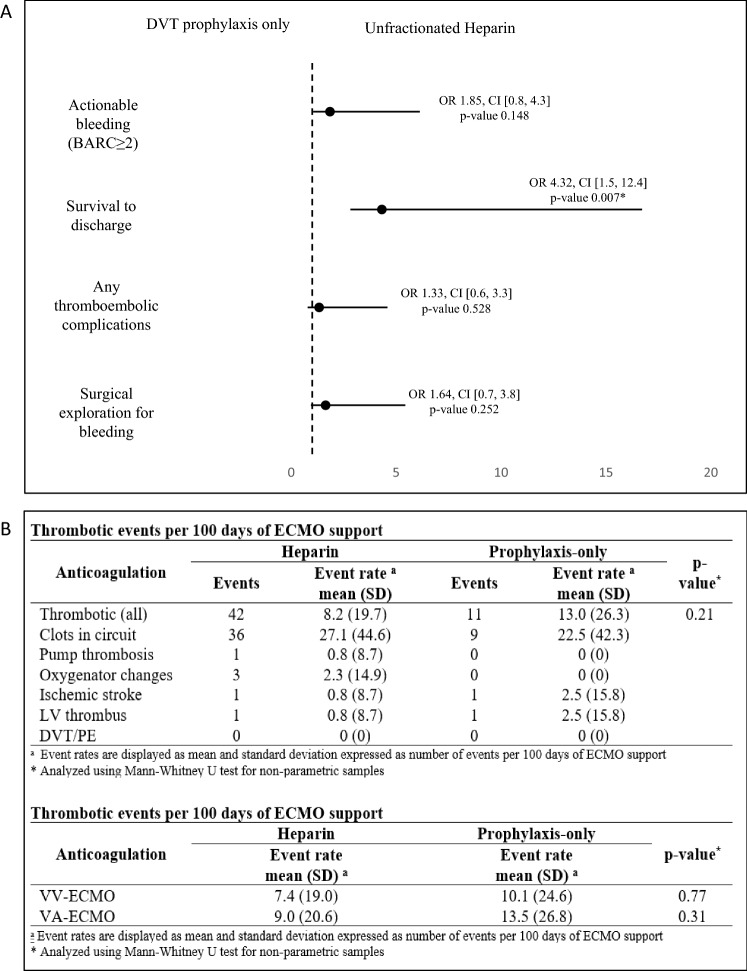
There was no difference in primary or secondary outcomes between anticoagulation strategies. Survival to discharge was significantly higher with UFH than with prophylaxis-only (39.3% vs 11.9%, P = 0.001). Multivariable analysis showed no significant difference in thromboembolic complications, actionable bleeds, or exploration for bleeding between UFH and prophylaxis-only (Figure). Survival to discharge remained significant after adjustment, favoring UFH (OR, 4.32; 95% confidence interval, 1.5 to 12.4; P = 0.007).
Figure.
Multivariable analysis for primary and secondary clinical outcomes based on anticoagulation strategy and thrombotic event rates. (A) Odds ratios for primary and secondary clinical outcomes stratified by anticoagulation strategy; DVT prophylaxis-only or unfractionated heparin. (B) Thrombotic complications * = P value < 0.05. BARC = Bleeding Academic Research Consortium; CI = confidence interval; DVT = deep-vein thrombosis; ECMO = extracorporeal membrane oxygenation; LV = left ventricle; OR = odds ratio; PE = pulmonary embolus; SD = standard deviation; VA = venoarterial; VV = venovenous
Our results showed no significant differences in thromboembolic or bleeding complications between patients receiving UFH or prophylaxis-only anticoagulation. Nevertheless, the prophylaxis-only group were less likely to survive than the UFH group. This could potentially be explained by sicker and more coagulopathic patients being more likely to receive prophylaxis-dose anticoagulation only.
The 2021 Extracorporeal Life Support Organization guidelines are in keeping with our findings, endorsing a primary strategy of UFH, with DTIs like bivalirudin and argatroban reserved as alternatives. Still, optimal anticoagulation strategies for adult ECMO continues to be contentious, recognized in the guidelines by acknowledging evidence that may suggest lower or no anticoagulation as a viable strategy, especially in VV-ECMO.5
Our results are limited by the heterogeneity of ECMO patients. We attempted to control for baseline differences with multivariable regression adjustment, but recognize that available data fields may not capture some nuances effecting clinical decisions. Small group sizes in the LMWH and DTI groups add additional limitations to our conclusions.
In our study, UFH was the predominant strategy of choice. Prophylaxis-dose only anticoagulation may offer a lower risk alternative that seems not to increase thrombotic events in our experience, and may be considered for those with elevated bleeding risk. Further data are needed to elucidate optimal anticoagulation strategies in ECMO patients, with the addition of therapeutic monitoring data of anticoagulants, as this remains an important standard of practice.5
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
Disclosures
None.
Funding statement
We received no specific funding for this work.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oliver WC. Anticoagulation and coagulation management for ECMO. Semin Cardiothorac Vasc Anesth. 2009;13:154–175. doi: 10.1177/1089253209347384. [DOI] [PubMed] [Google Scholar]
- 2.Extracorporeal Life Support Organization (ELSO). General guidelines for all ECLS cases, 2017. Available from URL: https://www.elso.org/Portals/0/ELSO%20Guidelines%20General%20All%20ECLS%20Version%201_4.pdf (accessed October 2022).
- 3.Protti A, Iapichino GE, Di Nardo M, Panigada M, Gattinoni L. Anticoagulation management and antithrombin supplementation practice during veno-venous extracorporeal membrane oxygenation: a worldwide survey. Anesthesiology. 2020;132:562–570. doi: 10.1097/aln.0000000000003044. [DOI] [PubMed] [Google Scholar]
- 4.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123:2736–2747. doi: 10.1161/circulationaha.110.009449. [DOI] [PubMed] [Google Scholar]
- 5.McMichael AB, Ryerson LM, Ratano D, Fan E, Faraoni D, Annich GM. 2021 ELSO adult and pediatric anticoagulation guidelines. ASAIO J. 2021;68:303–310. doi: 10.1097/mat.0000000000001652. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.