Abstract
Objectives:
The adverse effect of living alone on health has been well-documented in community-dwelling older adults. A less understood topic in this research area is whether some neighborhood characteristics may mitigate the negative impact of living alone on health outcomes and mortality. This study aimed to extend the existing work on living arrangements and health by examining the potential interactive effect of living alone and perceived neighborhood cohesion on all-cause mortality among older Chinese Americans.
Methods:
Data were drawn from 3,154 (58.0% female) participants from a prospective cohort study of community-dwelling US older Chinese adults aged 60 and older in the greater Chicago area. Living arrangements and perceived neighborhood cohesion were assessed at baseline from 2011–2013. Mortality status was tracked through December 2021. Covariates, including sociodemographic characteristics, health and behavioral covariates, loneliness, depression, and social engagement, were assessed at baseline. Cox proportional hazards regression model was used to test our hypotheses.
Results:
Living alone was significantly associated with an increased risk of all-cause mortality among participants reporting low levels of perceived neighborhood cohesion but not among those reporting high levels of perceived neighborhood cohesion. This protective effect of perceived neighborhood cohesion was robust to the inclusion of covariates.
Conclusions:
Our results suggest that strong perceived neighborhood cohesion may protect against the increased risk of premature mortality associated with living alone in community-dwelling older Chinese Americans.
Keywords: Social isolation, living alone, mortality, perceived neighborhood cohesion, older Chinese Americans
1. Introduction
Living alone has been linked to various poor health outcomes, including depression (Hu et al., 2012), cardiovascular disease (Gan et al., 2021), dementia (Desai et al., 2020), poor biological health (Zilioli & Jiang, 2021), and premature mortality (Holt-Lunstad et al., 2015). Living alone, however, is not uncommon. For example, in the U.S., about 27% of people ages 60 and older live alone (Ausubel, 2020), though older adults have been indicated to be particularly vulnerable to the adverse health impacts associated with living alone (Shaw et al., 2018; Yeh & Lo, 2004). Although the association between living alone and poor health has been largely documented, few studies have examined the potential protective factors that can buffer against the adverse effect of living alone on health outcomes and premature mortality (Stahl et al., 2017). Identifying such protective factors is critical, as older adults wish to age in place (Wiles et al., 2012). Findings from this research direction can inform the development of interventions to improve health in older adults living alone. This study, therefore, aimed to examine the potential protective effect of perceived neighborhood cohesion on all-cause mortality associated with living alone in community-dwelling older Chinese Americans.
Living alone is a key risk factor contributing to premature mortality in older adults (Gopinath et al., 2013; Jensen et al., 2019; Ng et al., 2015). A meta-analysis of 70 studies estimated that living alone was associated with a 32% increased risk of mortality (Holt-Lunstad et al., 2015). Many prior studies on the health impact of living alone have been conducted among Caucasian populations in Western countries (Holt-Lunstad et al., 2015). The emerging studies in other populations suggest that the adverse health impact of living alone seems to be similar across cultures. For example, a few studies conducted in Asian regions, including China, reported a higher mortality risk among Asian older adults living alone than those living with others (Feng et al., 2017; Ng et al., 2015; Yu et al., 2020), though there are exceptions documenting no significant associations between living alone and mortality (Iwasa et al., 2008).
Living alone has been suggested to lead to poor health and premature mortality in multiple ways. First, living alone is associated with an increased risk of low social ties (Finlay & Kobayashi, 2018), which, in turn, may reduce the opportunities to fulfill psychological and social needs associated with health (Holt-Lunstad & Steptoe, 2022; Kemp et al., 2017). Older adults living alone have been found to report a shrinkage of social networks (Barrenetxea et al., 2022; Chou & Chi, 2000). Social relationships, according to Weiss’s (1974) theory of the function of social relationships, serve to meet several needs, such as attachment, social integration, and guidance, that are essential for maintaining good health. Indeed, diverse social networks have been linked to better health outcomes (Li & Zhang, 2015). It is important to note that although living alone is a risk factor for reduced social networks, living alone does not necessarily imply limited social networks in older adults (Smith & Victor, 2019). Second, although living alone and loneliness, a subjective indicator of social isolation, are two distinctive constructs, loneliness has been proposed as a key mechanism through which living alone affects health (Park et al., 2017; Yang et al., 2020). Older adults living alone tend to feel lonely (Yeh & Lo, 2004; Theeke, 2009). Loneliness, in turn, is consistently associated with poor health and premature mortality (Erzen & Çikrikci, 2018; Rico-Uribe et al., 2018). The adverse health effect of living alone, however, may be only partially explained by loneliness. Some studies have found a unique effect of living alone on mortality, over and above the effect of loneliness (Teguo et al., 2016; Yu et al., 2020).
An important question that has not been fully examined in this research area is whether some neighborhood characteristics, including perceived neighborhood cohesion, could ameliorate the adverse effect of living alone on mortality. Perceived neighborhood cohesion, defined as the perception of trust, connectedness, and solidarity between members of a group (Cagney et al., 2009; Manca, 2014), has been linked to various health outcomes, including premature mortality (Clark et al., 2011; Inoue et al., 2013; Robinette et al., 2018). For example, strong perceived neighborhood cohesion was associated with a 22% decreased risk of 10-year all-cause mortality in a cohort study of older adults in Japan (Inoue et al., 2013). Previous studies have indicated that the health benefits of perceived neighborhood cohesion may be driven by the enhancement of social integration (Tang et al., 2020). Therefore, perceived neighborhood cohesion may be particularly important for older adults living alone, as strong perceived neighborhood cohesion can reduce the risk of social isolation and loneliness (Johnson et al., 2018; Kowitt et al., 2020). As a result, perceived neighborhood cohesion may serve as a protective factor to reduce the effect of living alone on poor health.
Importantly, the potential effect of perceived neighborhood cohesion on health may be especially salient in older adults from collectivist cultures. Individuals from a collectivist culture (e.g., Chinese culture) generally place higher values on mutual support and belonging within a group than their counterparts from an individualistic culture (Gambrel & Cianci, 2003), suggesting the importance of perceived neighborhood cohesion in collectivist cultures. A recent study, using data from the United Kingdom household longitudinal study, found a stronger relationship between perceived neighborhood cohesion and mental health in participants from some Asian countries, such as Bangladesh, than their white counterparts (Chum et al., 2021).
Evidence from a small body of research has shown the potential buffering effect of perceived neighborhood cohesion on health in older adults living alone (Gyasi et al., 2019; Stahl et al., 2017). In a cross-sectional study of older adults in Ghana, perceived neighborhood cohesion was found to buffer the negative impact of living alone on psychological distress (Gyasi et al., 2019). Similarly, Stahl and colleagues (2017) found a stronger relationship between living alone and depression among participants reporting lower levels of perceived neighborhood cohesion in a cross-sectional study of U.S. older adults. These converging findings provide initial support that perceived neighborhood cohesion might buffer the detrimental effects of living alone on various health outcomes but have not examined effects on premature mortality.
A few studies have indicated sex differences in mortality risk associated with living alone (Kandler et al., 2007; Schmaltz et al., 2007), though the findings are somewhat inconsistent (Abell & Steptoe, 2021). For example, Kandler et al. (2007) found that living alone was associated with a twofold risk of all-cause mortality in men but not in women in a population-based cohort study in Germany. Yet, in a more recent study, no sex differences were found in the association between living alone and mortality risk in the English Longitudinal Study of Ageing (Abell & Steptoe, 2021). Given possible sex differences in the association between living alone and mortality risk, this study also explored sex differences in the health effects of living alone.
The primary purpose of the current study is to examine the moderating effect of perceived neighborhood cohesion on the association between living alone and all-cause mortality in a sample of community-dwelling older Chinese Americans. Given the reported moderating effect of perceived neighborhood cohesion on mental health among older adults living alone (Gyasi et al., 2019; Stahl et al., 2017), we hypothesized that perceived neighborhood cohesion would moderate the association between living alone and all-cause mortality. That is, there would be a stronger relationship between living alone and all-cause mortality among participants reporting lower levels of perceived neighborhood cohesion. A secondary purpose of the current study was to explore potential sex differences in the relationship between living alone and all-cause mortality and the buffering effect of perceived neighborhood cohesion on this relationship. Given that previous findings on this topic are limited and mixed, we did not have specific hypotheses regarding sex differences.
2. Methods
2.1. Participants
Data were drawn from the Population Study of Chinese Elderly in Chicago (PINE), a population-based epidemiological study of community-dwelling older Chinese Americans aged 60 and older living in the greater Chicago area (Dong, 2014). The baseline cohort of the PINE study consisted of 3,157 participants who self-identified as Chinese. All participants completed a face-to-face home interview at baseline from 2011–2013. The interviews were conducted by trained multicultural and multilingual interviewers. Of the 3,157 participants, 3 had missing data on the date of death, resulting in a final sample of 3,154 participants (mean age = 72.81 years, SD = 8.30; 58.0% female) in the current study. The study was approved by the Institutional Review Board at Rush University Medical Center in Chicago, Illinois. Written informed consent was obtained from all participants.
2.2. Measures
2.2.1. Mortality
Mortality was tracked through December 2021. The vital status of participants was obtained from informants and family members through regular contacts made by our research team. Our study team also regularly searched local newspapers and websites for obituaries. In the current study, 640 (20.3%) participants were deceased.
2.2.2. Living arrangements
Living arrangements were assessed at baseline (i.e., 2011–2013) by asking participants the number of family members living in the same household, which were coded as 1 = living alone (i.e., participant was the only person living in the household) and 0 = living with others.
2.2.3. Perceived neighborhood cohesion
Perceived neighborhood cohesion was assessed at baseline using a 6-item questionnaire adopted from the Chicago Neighborhood and Disability Study (Cagney et al., 2009). The items were used to assess the subjective perception of integration (e.g., “how often in your neighborhood do you see neighbors talking outside in the yard or in the street?”; responses ranging from 0 = never to 3 = often) and the overall social cohesiveness (e.g., “how many neighbors do you know by name?”; responses ranging from 0–21 or more). Responses on each item were z-scored due to different response options across items and then averaged to create a composite score of neighbor cohesion. Cronbach’s α was 0.77 in the present study.
2.2.4. Covariates
Several key covariates assessed at baseline were included in this analysis, given their associations with mortality in previous studies (Imami et al., 2022; Li & Dong, 2020). These covariates included sociodemographic, health, behavioral, and psychosocial variables. The sociodemographic covariates included age, sex (0 = male, 1 = female), highest grade or years of school completed (0–26 years), annual income (responses ranging from 1 = 0-$4,999 to 10 = $75,000 or more), access to health insurance (0 = no, 1 = yes), number of children, and years living in the community.
Health covariates included the total number of self-reported health conditions out of 10 conditions (e.g., heart disease, stroke, cancer) and activities of daily living limitations. Activities of daily living limitations were assessed using eight items adapted from the Activities of Daily Living (ADL; Katz & Akpom, 1976). Participants were asked whether they needed help with eating, dressing, bathing, walking, transferring, grooming, incontinence, and toileting on a 4-point scale from 0 = none to 3 = most of the time. Responses on the eight items were summed to create a composite of ADL limitations. Behavioral covariates included smoking (0 = never smoked, 1 = ever or current smoking) and regular alcohol use (0 = no [2–4 times a month or less], 1 = yes [2–3 times a week or more]). Smoking was initially coded into three groups (0 = never smoked, 1 = ever smoked, 2 = current smoking). Given that there were no differences in mortality rate between participants who ever smoked and those who were currently smoking (28.1% vs. 27.1%, p > .05), smoking was recoded into two groups (0 = never smoked, 1 = ever or current smoking).
Psychosocial covariates included loneliness, social engagement, and depression. Loneliness was assessed using the 3-item UCLA Loneliness Scale (Hughes et al., 2004). Participants were asked to report their subjective perception of lacking companionship, feeling left out of life, and feeling isolated from others on a 3-point scale from 0 = hardly ever and 2 = often. Responses on each item were summed up to create a composite of loneliness (Cronbach’s α = 0.76). Social engagement was assessed using 10 items from the Social Engagement Scale (Dong et al., 2014). Of the 10 items, six items were used to ask participants the frequency they engaged in social activities (i.e., having friends or relatives for dinner or a party; going out to a movie, restaurant, or sporting event; visiting relatives, friends, or neighborhoods; playing mahjong; playing games; going to day trips or overnight trips) on a 5-point scale from 0 = once a year or less to 4 = every day or almost every day. The other four items were used to ask participants the frequency they visited a museum, a library, and community centers and attended a concert, play, or musical in the past five years on a 5-point scale from 0 = never to 4 = 20 or more times. A composite score of social engagement was created by averaging the responses on the 10 items, with a higher score reflecting a higher level of social engagement. Depression was assessed using the Patient Health Questionnaire-9 (Spitzer et al., 1999) on a 4-point scale from 1 = not at all to 4 = most of the time. Responses on the nine items were summed to create a composite depression score (Cronbach’s α = 0.81).
2.3. Statistical Analyses
The t-test for continuous variables and chi-square test for categorical variables were used to test differences in participants’ characteristics by living arrangements, mortality status, and sex. Cox proportional-hazards regression was carried out to test the main effect of living alone on all-cause mortality and the interactive effect of living alone and perceived neighborhood cohesion (i.e., perceived neighborhood cohesion × living alone) on all-cause mortality. To test the validity of the proportional hazards assumption, we tested the correlations between the Schoenfeld residuals (Schoenfeld, 1982) and survival time. The correlations were statistically nonsignificant for all variables and the interaction term (ps > .05), except for depression (p = .013), supporting the proportionality assumption. Significant moderating effects of perceived neighborhood cohesion were further interpreted by plotting survival curves by living alone at different levels of neighborhood cohesion categorized into tertiles: low (0–33%), moderate (34–66%), and high (67–100%). Cox proportional-hazards regression was also used to test the two-way interaction between sex and living alone on all-cause mortality and the three-way interaction among sex, living alone, and perceived neighborhood cohesion on all-cause mortality. Following a similar hierarchical estimation approach outlined in previous research on social isolation (Kobayashi & Steptoe, 2018), the models were first run by adjusting for age and sex (Model 1), next adjusting for additional sociodemographic covariates (Model 2), then further adjusting for health and behavioral covariates (Model 3), and finally additionally adjusting for loneliness, social engagement, and depression (Model 4). Such a hierarchical estimation approach allows the examination of how results change when multiple covariates are controlled for, particularly in the situation in which some covariates may serve as possible mediators (e.g., smoking, loneliness) linking living alone to all-cause mortality. Continuous variables were standardized so that the hazard ratio (HR) reflected the changes in the ratio of the hazard rate for one standard deviation change in continuous variables. The incidence of missing data was 0.5%. The expectation-maximization algorithm was used to impute missing data on continuous variables, and mode imputation was used for categorical variables. Previous studies suggest that the expectation-maximization algorithm yields less biased estimates than ad hoc methods (e.g., listwise deletion; Schafer & Graham, 2002). All analyses were conducted in SPSS 27.0 (IBM Corp., Armonk, New York).
3. Results
3.1. Descriptive Results
Table 1 displays the demographic characteristics of participants by living arrangements. Compared to participants living with others, those living alone were older, more likely to die and be female, had a lower level of education but a high level of income, and reported more chronic health conditions (ps < .01). Participants living alone reported a higher level of neighborhood cohesion, loneliness, and depression than their counterparts living with others (ps < .05). There were no differences in social engagement or daily living limitations between participants living alone and those living with others (ps > .10). In addition, Supplementary Tables 1 and 2 display the demographic characteristics of participants by vital status and sex, respectively.
Table 1.
Demographic characteristics of the sample by living arrangements.
| Living arrangementsa | ||||
|---|---|---|---|---|
| Variables (Means, SDs) | Overall (N = 3,154) | Living with others (N = 2,475) | Living alone (N = 678) | p |
| Mortality (deceased; N, %) | 640(20.3) | 447(18.1) | 193(28.5) | < .001 |
| Perceived neighborhood cohesion | 0.00(0.77) | −0.05(0.76) | 0.18(0.78) | < .001 |
| Female (N, %) | 1,829(58.0) | 1,308 (52.8) | 521(76.8) | < .001 |
| Age (years) | 72.81(8.30) | 71.50(7.94) | 77.61(7.84) | < .001 |
| Education (years) | 8.72(5.05) | 9.08(4.95) | 7.42(5.20) | < .001 |
| Income | 1.95(1.14) | 1.92(1.18) | 2.04(0.94) | .006 |
| Health insurance (yes; N, %) | 2,382(76.0) | 1,747(71.0) | 635(94.1) | < .001 |
| Number of children | 2.88(1.51) | 2.79(1.44) | 3.18(1.69) | < .001 |
| Years living in the community | 12.14(11.03) | 11.45(10.61) | 14.66(12.14) | < .001 |
| Chronic health conditions | 2.06(1.46) | 1.97(1.44) | 2.41(1.49) | < .001 |
| Activities of daily living | 0.39(2.12) | 0.38(2.17) | 0.42(1.91) | .65 |
| Smoking (ever/current smoking; N, %) | 927(29.4) | 816(33.0) | 111(16.4) | < .001 |
| Alcohol use (yes; N, %) | 458(14.5) | 384(15.5) | 74(10.9) | .003 |
| Loneliness | 0.56(1.21) | 0.48(1.09) | 0.99(1.54) | < .001 |
| Social engagement | 0.97(0.53) | 0.96(0.52) | 1.00(0.56) | .12 |
| Depression | 2.64(4.12) | 2.54(4.01) | 3.02(4.46) | .012 |
Note. p values obtained from the t-test for continuous variables and the chi-square test for categorical variables.
Numbers did not sum to the total sample size due to missing data from one participant.
3.2. Main and interactive effects
Results from the models testing the main effect of living alone showed that living alone was not significantly associated with all-cause mortality (ps > .05, see Table 2). Yet, the moderation analyses showed a significant interactive effect of living alone and perceived neighborhood cohesion on all-cause mortality in all four models (ps < .05, see Table 3). To interpret this interactive effect of living alone and perceived neighborhood cohesion on all-cause mortality, Figure 1 displays the survival curves by living alone at low, moderate, and high levels of perceived neighborhood cohesion. Notably, perceived neighborhood cohesion was treated as a continuous variable in the above moderation analyses and as a categorical variable for survival curve plotting only. Survival curves showed that among participants reporting low levels of perceived neighborhood cohesion, older Chinese Americans living alone had a 48.5% increased risk of all-cause mortality than their counterparts living with others (HR = 1.485, 95%CI [1.101, 2.004], p = .010). Among participants reporting high levels of perceived neighborhood cohesion, participants living alone and those living with others had no statistically significant differences in all-cause mortality (HR = 1.076, 95%CI [0.772, 1.501], p = .67).
Table 2.
Main effects of living alone on all-cause mortality.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Variables | HR (95%CI) | HR (95%CI) | HR (95%CI) | HR (95%CI) |
| Living alone | 1.091(0.909, 1.308) | 1.049(0.874, 1.261) | 1.139(0.946, 1.370) | 1.142(0.945, 1.381) |
| Female | 0.499(0.424, 0.589)*** | 0.451(0.380, 0.534)*** | 0.508(0.400, 0.645)*** | 0.500(0.393, 0.636)*** |
| Age | 2.808(2.580, 3.055)*** | 2.588(2.356, 2.843)*** | 2.415(2.192, 2.660)*** | 2.334(2.116, 2.575)*** |
| Education | 0.831(0.763, 0.905)*** | 0.866(0.793, 0.945)** | 0.899(0.821, 0.984)* | |
| Income | 0.944(0.841, 1.059) | 0.928(0.826, 1.043) | 0.936(0.833, 1.051) | |
| Health insurance | 1.204(0.884, 1.641) | 1.156(0.845, 1.580) | 1.188(0.868, 1.627) | |
| Number of children | 1.024(0.949, 1.104) | 1.041(0.965, 1.122) | 1.047(0.971, 1.129) | |
| Years living in the community | 1.076(0.998, 1.159) | 1.082(1.006, 1.165)* | 1.070(0.994, 1.152) | |
| Chronic health conditions | 1.112(1.027, 1.205)** | 1.112(1.027, 1.204)** | ||
| Activities of daily living | 1.165(1.119, 1.212)*** | 1.148(1.101, 1.197)*** | ||
| Smoking | 1.448(1.148, 1.825)** | 1.432(1.134, 1.809)** | ||
| Alcohol use | 0.725(0.563, 0.934)* | 0.750(0.581, 0.968)* | ||
| Loneliness | 1.098(1.013, 1.191)* | |||
| Social engagement | 0.838(0.761, 0.922)*** | |||
| Depression | 0.943(0.864, 1.029) |
Note. HR = Hazard ratio; CI = confidence interval.
p < .05;
p < .01;
p < .001.
Table 3.
Interactive effects of living alone and perceived neighborhood cohesion on all-cause mortality.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Variables | HR (95%CI) | HR (95%CI) | HR (95%CI) | HR (95%CI) |
| Living alone | 1.137(0.946, 1.366) | 1.086(0.902, 1.307) | 1.158(0.961, 1.395) | 1.142(0.944, 1.383) |
| Perceived neighborhood cohesion (PNC) | 0.861(0.781, 0.950)** | 0.875(0.791, 0.968)* | 0.919(0.831, 1.016) | 0.950(0.857, 1.053) |
| Living alone × PNC | 0.793(0.648, 0.971)* | 0.811(0.663, 0.994)* | 0.797(0.653, 0.972)* | 0.815(0.667, 0.997)* |
| Female | 0.499(0.423, 0.588)*** | 0.460(0.388, 0.544)*** | 0.522(0.411, 0.664)*** | 0.511(0.401, 0.651)*** |
| Age | 2.742(2.523, 2.980)*** | 2.533(2.308, 2.782)*** | 2.383(2.164, 2.624)*** | 2.327(2.110, 2.565)*** |
| Education | 0.858(0.787, 0.936)** | 0.886(0.810, 0.968)** | 0.906(0.826, 0.992)* | |
| Income | 0.950(0.847, 1.065) | 0.935(0.833, 1.050) | 0.939(0.836, 1.055) | |
| Health insurance | 1.278(0.937, 1.745) | 1.205(0.880, 1.649) | 1.220(0.891, 1.672) | |
| Number of children | 1.031(0.956, 1.112) | 1.046(0.970, 1.128) | 1.050(0.974, 1.132) | |
| Years living in the community | 1.067(0.991, 1.149) | 1.074(0.999, 1.156) | 1.065(0.989, 1.146) | |
| Chronic health conditions | 1.119(1.033, 1.213)** | 1.118(1.032, 1.211)** | ||
| Activities of daily living | 1.150(1.104, 1.198)*** | 1.142(1.095, 1.191)*** | ||
| Smoking | 1.461(1.158, 1.844)** | 1.443(1.142, 1.824)** | ||
| Alcohol use | 0.735(0.570, 0.947)* | 0.748(0.579, 0.966)* | ||
| Loneliness | 1.094(1.008, 1.186)* | |||
| Social engagement | 0.868(0.786, 0.958)** | |||
| Depression | 0.943(0.865, 1.029) |
Note. HR = Hazard ratio; CI = confidence interval.
p < .05;
p < .01;
p < .001.
Fig. 1.
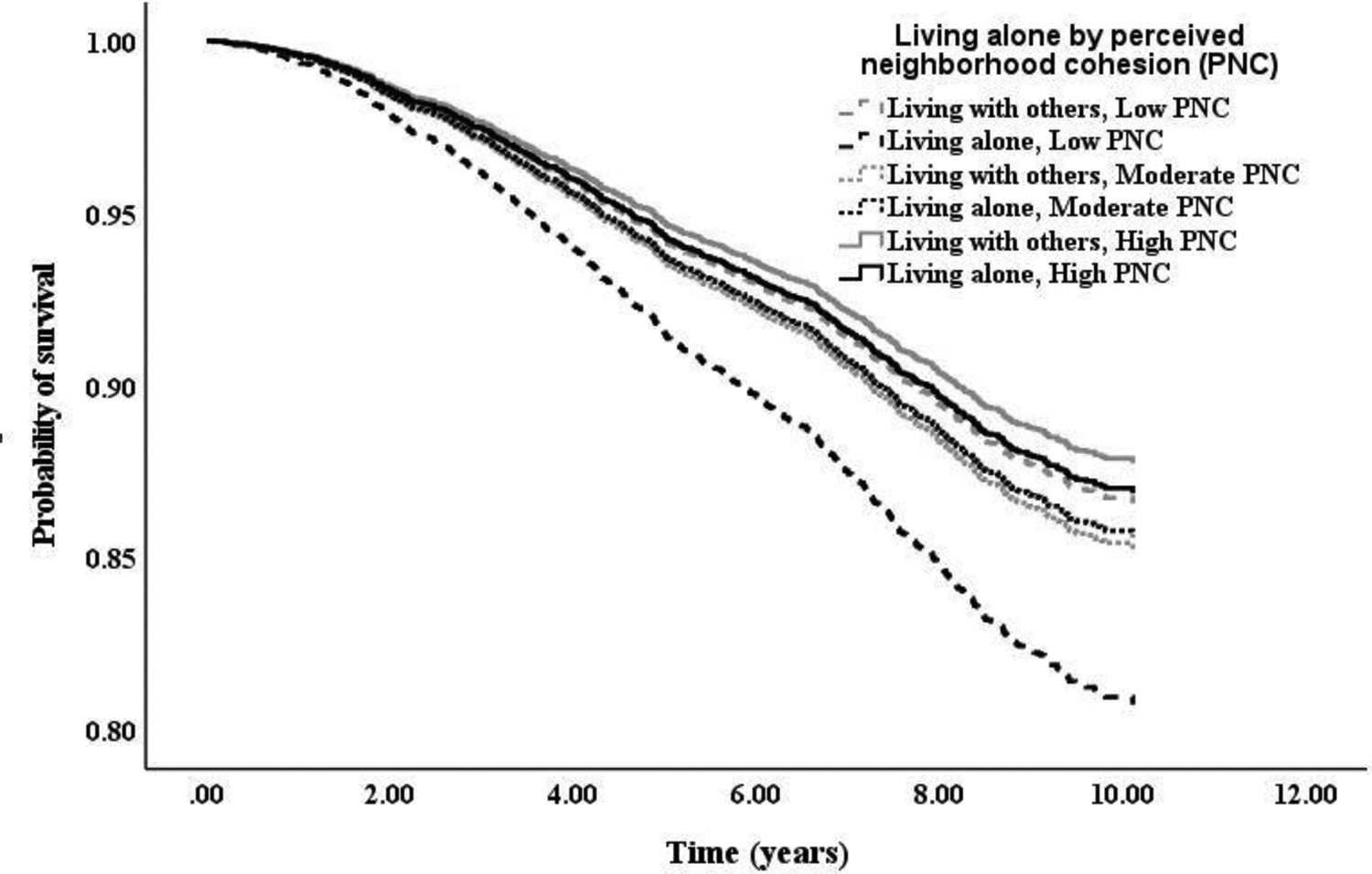
Survival curves by living alone at low (0–33%), moderate (34–66%), and high (67–100%) levels of perceived neighborhood cohesion.
A sensitivity analysis was performed to account for the potential impact of COVID-19-related mortality. Model 4 testing the interactive effect between living alone and perceived neighborhood cohesion was rerun in which mortality was recorded before March 2020 (N = 525 deceased). The results showed a similar and significant interactive effect between living alone and perceived neighborhood cohesion on all-cause mortality (p = .021).
3.3. Sex differences
A two-way interaction term (sex × living alone) was included in the main-effect model to examine sex differences in the association between living alone and all-cause mortality. There were no statistically significant interactive effects between sex and living alone on all-cause mortality in all four models (ps > .05). The three-way interaction among sex, living alone, and neighborhood cohesion was also not statistically significant (ps > .05).
4. Discussion
The adverse health effect of living alone has been well documented (Gopinath et al., 2013; Jensen et al., 2019; Ng et al., 2015). Few studies, however, have examined the potential protective factors that can ameliorate the adverse health effects associated with living alone. The current study aimed to fill this gap by examining the protective effect of perceived neighborhood cohesion on the association between living alone and all-cause mortality among community-dwelling older Chinese Americans. Several findings emerged from the current study. Our results showed that living alone was not statistically associated with all-cause mortality. Instead, we found that living alone interacted with perceived neighborhood cohesion to predict all-cause mortality. That is, living alone was significantly associated with increased mortality risk at low but not high levels of perceived neighborhood cohesion. Notably, this interactive effect was robust to the inclusion of sociodemographic, health, behavioral, and psychosocial covariates. No significant sex differences were found in the association between living alone and mortality or in the moderating effect of perceived neighborhood cohesion.
Supporting our hypothesis, we found a significant protective effect of neighborhood cohesion on the association between living alone and all-cause mortality in community-dwelling older Chinese Americans. This result extends previous cross-sectional studies documenting the buffering effect of perceived neighborhood cohesion on psychological distress in older adults living alone (Gyasi et al., 2019; Stahl et al., 2017), indicating the protective effect of strong perceived neighborhood cohesion on physical health, including premature mortality. One explanation for this protective effect is that perceived neighborhood cohesion may reduce the risk of experiencing loneliness in older adults living alone (Kowitt et al., 2020). Nonetheless, the interactive effect of living alone and perceived neighborhood cohesion on mortality was robust to the inclusion of loneliness, suggesting that other potential mechanisms may explain the protective effect of perceived neighborhood cohesion. In this respect, another alternative explanation is that neighborhoods with strong cohesion may reflect more access to health information and social support from neighbors (Miao et al., 2019; Mulvaney-Day et al., 2007), which can reduce the adverse health effect associated with living alone. That is, strong neighborhood cohesion may facilitate the rapid diffusion of health-related information in communities and the exchange of instrumental support between community members to promote health. The health benefits of strong neighborhood cohesion may be particularly salient for older Chinese Americans, as many of them face the risk of losing social connections with their home country due to immigration (Gao et al., 2021) and experience barriers to health care access due to language barriers and limited health literacy (Kim & Keefe, 2010). Altogether, our result adds to the existing literature on neighborhood and health by showing the protective effect of social neighborhood environment (e.g., perceived neighborhood cohesion) on mortality among older adults who live alone.
Somewhat surprisingly, our results did not support a main effect of living alone on all-cause mortality. This finding is inconsistent with many prior studies documenting the increased mortality risk associated with living alone (Holt-Lunstad et al., 2015), though null results have been reported in some studies (Iwasa et al., 2008). A possible explanation for this null finding is that older adults who live alone may not uniformly feel socially isolated and/or lonely (Koivunen et al., 2020). Although participants living alone in this study reported higher levels of loneliness than those living with others, there were no statistically significant differences in social engagement between these two groups. It is likely that participants living alone in our study were a mixed group of socially isolated and socially integrated individuals, some of whom may have diverse social networks and do not feel lonely (Smith & Victor, 2019), and in turn, may not experience an elevated mortality risk (Steptoe et al., 2013). Nevertheless, our result suggests that living alone may not necessarily be associated with poor health outcomes among older Chinese Americans. Variations in some social characteristics (e.g., neighborhood cohesion) of the neighborhoods in which older Chinese Americans live may attenuate the association between living alone and mortality. Germane to this point, we found that living alone was associated with increased mortality risk among those reporting low levels of perceived neighborhood cohesion but not high levels of perceived neighborhood cohesion, highlighting the importance of assessing neighborhood characteristics when studying health outcomes in older Chinese Americans living alone.
Interestingly, we did not find sex differences in the association between living alone and all-cause mortality or in the moderating effect of perceived neighborhood cohesion. Previous studies have shown a higher risk of all-cause mortality among male than female adults who live alone (Kandler et al., 2007; Schmaltz et al., 2007). Still, our results did not seem to support this hypothesis. One possible explanation for this null finding may be due to a small percentage of male participants living alone (5% of the sample) in this study, which may lack adequate statistical power to detect meaningful differences. Nonetheless, our results are not surprising, given mixed findings reported in previous studies (Abell & Steptoe, 2021; Shaw et al., 2020). More studies on this research topic are warranted. Nevertheless, our results suggest that the effect of living alone on mortality and the protective effect of perceived neighborhood cohesion on this association may be consistent across male and female older adults, at least in our sample.
The moderating effect of perceived neighborhood cohesion reported in this study has important implications for social policy and public health interventions in older adults, particularly those living alone. Our results suggest that the absence of neighborhood cohesion may pose challenges in achieving healthy aging for older adults living alone. Healthcare and social services may need to pay particular attention to older adults who live alone in neighborhoods without strong cohesion, as they may experience a higher mortality risk. Meanwhile, our findings highlight that strengthening neighborhood cohesion through social policy and public health initiatives may be a promising direction to improve health in older adults living alone. Existing health promotion practices for older adults have primarily focused on individual and family factors (Huey & Tilley, 2018; Wolff & Boyd, 2015). Our results suggest that community-level interventions that facilitate neighborhood cohesion have the potential to promote health and reduce early mortality risk among older Chinese Americans who live alone. For example, a prior study among older Chinese adults found that a brief community intervention comprised of community activities (e.g., day camps, thematic activities) significantly improved neighborhood cohesion (Shen et al., 2017). Still, it is important to note that facilitating social cohesiveness can be a great challenge, particularly for ethnic minority older populations (e.g., Asian Americans), due to some social and cultural factors, such as anti-Asian racism (Santos et al., 2021).
4.1. Limitations
A few limitations need to be acknowledged when interpreting our results. First, although this study accounted for a comprehensive set of covariates, some other unmeasured factors (e.g., physical activity; Blair & Haskell, 2006) may partially explain the results reported in this study. For example, older adults who live alone tend to be less likely to engage in physical activity than those who live with others (Jeong & Cho, 2017), while physical activity has been found to be associated with a decreased mortality risk (Lee & Skerrett, 2001). Also, our results should be cautiously interpreted due to a lack of information about housing structures (e.g., single-family homes; apartments). Living alone in a single-family home may have a different experience than living alone in a large apartment, particularly regarding the opportunities for social activities (Glaeser & Sacerdote, 2000), which in turn may confound the protective effect of perceived neighborhood cohesion reported in this study. Germane to this point, our results, however, did not find that inclusion of social engagement altered the moderating effect of perceived neighborhood cohesion. Second, future longitudinal studies are needed to formally examine the potential intermediate roles of some covariates (e.g., loneliness) included in this study in linking living alone to all-cause mortality. Third, this study only examined the potential protective effect of perceived social neighborhood characteristics (i.e., neighborhood cohesion) on the association between living alone and all-cause mortality. Some other aspects of neighborhood characteristics, such as physical neighborhood characteristics, may modify the mortality risk associated with living alone. In this regard, higher levels of green space in the neighborhood were found to be associated with a reduced risk of all-cause mortality in a sample of community-dwelling older Chinese living in Hong Kong (Wang et al., 2017). In addition, the use of self-report measure of perceived neighborhood cohesion may be subject to reporting bias, as older adults who experience high levels of psychological distress (e.g., depression) and poor health tend to report low levels of perceived neighborhood cohesion (Miao et al., 2019; Robinette et al., 2013). It is of note, in contrast, that the moderating effect of perceived neighborhood cohesion was robust to the inclusion of baseline health outcomes (e.g., chronic health conditions) and psychological covariates (e.g., depression) in this study, suggesting that the moderating effect of perceived neighborhood cohesion may not likely be attributed to reporting bias. Last, this study included a representative sample of older Chinese Americans living in the greater Chicago area. Our findings may not be generalizable to older Chinese living in other regions or other ethnic populations.
5. Conclusions
This study is one of the first studies to examine the moderating effect of perceived neighborhood cohesion on the association between living alone and all-cause mortality in older adults. Our results indicated a significant interactive effect of living alone and perceived neighborhood cohesion on all-cause mortality, showing a stronger relationship between living alone and increased mortality risk among participants reporting lower levels of perceived neighborhood cohesion. These results highlight the salient challenges in achieving healthy aging among older Chinese Americans who live alone in less cohesive neighborhoods. Meanwhile, our findings provide important implications suggesting that the development of interventions strengthening neighborhood cohesion could be a fruitful direction to promote health and well-being for this group.
Supplementary Material
Highlights.
Perceived neighborhood cohesion interacted with living alone to predict mortality.
Living alone predicted mortality at low levels of perceived neighborhood cohesion.
No sex differences were found in the above moderating effect.
Acknowledgement:
Data collection of the PINE study was supported by the National Institute of Health (R01AG042318). The preparation of the manuscript was partly supported by the Rutgers-NYU Center for Asian Health Promotion and Equity under NIH/NIMHD Grant 1P50MD017356-01. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Credit author statement
Yanping Jiang: Conceptualization, Data analysis and interpretation, Writing-original draft.
Mengting Li: Writing- original draft and reviewing.
Tammy Chung: Writing-editing and reviewing.
Declaration of interest: none.
References
- Abell JG, & Steptoe A (2021). Why is living alone in older age related to increased mortality risk? A longitudinal cohort study. Age and Ageing, 50, 2019–2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ausubel J (2020). Older people are more likely to live alone in the US than elsewhere in the world. Pew Research Center. [Google Scholar]
- Barrenetxea J, Yang Y, Pan A, Feng Q, & Koh W-P (2022). Social disconnection and living arrangements among older adults: the Singapore Chinese Health Study. Gerontology, 68, 330–338. [DOI] [PubMed] [Google Scholar]
- Blair SN, & Haskell WL (2006). Objectively measured physical activity and mortality in older adults. Jama, 296, 216–218. [DOI] [PubMed] [Google Scholar]
- Cagney KA, Glass TA, Skarupski KA, Barnes LL, Schwartz BS, & Mendes de Leon CF (2009). Neighborhood-level cohesion and disorder: measurement and validation in two older adult urban populations. Journals of Gerontology: Series B, 64, 415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou K-L, & Chi I (2000). Comparison between elderly Chinese living alone and those living with others. Journal of Gerontological Social Work, 33, 51–66. [Google Scholar]
- Chum A, Teo C, & Azra KK (2021). Does the longitudinal association between neighbourhood cohesion and mental health differ by ethnicity? Results from the UK Household Longitudinal Survey. Social psychiatry and psychiatric epidemiology, 1–14. [DOI] [PubMed] [Google Scholar]
- Clark CJ, Guo H, Lunos S, Aggarwal NT, Beck T, Evans DA, et al. (2011). Neighborhood cohesion is associated with reduced risk of stroke mortality. Stroke, 42, 1212–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai R, John A, Stott J, & Charlesworth G (2020). Living alone and risk of dementia: A systematic review and meta-analysis. Ageing Research Reviews, 62, 101122. [DOI] [PubMed] [Google Scholar]
- Dong X (2014). The Population Study of Chinese Elderly in Chicago. Journal of aging and health, 26, 1079–1084. [DOI] [PubMed] [Google Scholar]
- Dong X, Li Y, & Simon MA (2014). Social engagement among US Chinese older adults—Findings from the PINE Study. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 69, S82–S89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzen E, & Çikrikci Ö (2018). The effect of loneliness on depression: A meta-analysis. International Journal of Social Psychiatry, 64, 427–435. [DOI] [PubMed] [Google Scholar]
- Feng Z, Falkingham J, Liu X, & Vlachantoni A (2017). Changes in living arrangements and mortality among older people in China. SSM-population health, 3, 9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay JM, & Kobayashi LC (2018). Social isolation and loneliness in later life: A parallel convergent mixed-methods case study of older adults and their residential contexts in the Minneapolis metropolitan area, USA. Social science & medicine, 208, 25–33. [DOI] [PubMed] [Google Scholar]
- Gambrel PA, & Cianci R (2003). Maslow’s hierarchy of needs: Does it apply in a collectivist culture. Journal of Applied Management and Entrepreneurship, 8, 143. [Google Scholar]
- Gan T, Yang J, Jiang L, & Gao Y (2021). Living alone and cardiovascular outcomes: a meta-analysis of 11 cohort studies. Psychology, Health & Medicine, 1–13. [DOI] [PubMed] [Google Scholar]
- Gao S, Dupre K, & Bosman C (2021). Understanding the neighbourhood environment and the health and wellbeing of older Chinese immigrants: a systematic literature review. Ageing & Society, 41, 815–835. [Google Scholar]
- Glaeser EL, & Sacerdote B (2000). The social consequences of housing. Journal of housing economics, 9, 1–23. [Google Scholar]
- Gopinath B, Rochtchina E, Anstey KJ, & Mitchell P (2013). Living alone and risk of mortality in older, community-dwelling adults. JAMA internal medicine, 173, 320–321. [DOI] [PubMed] [Google Scholar]
- Gyasi RM, Yeboah AA, Mensah CM, Ouedraogo R, & Addae EA (2019). Neighborhood, social isolation and mental health outcome among older people in Ghana. Journal of Affective Disorders, 259, 154–163. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on psychological science, 10, 227–237. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, & Steptoe A (2022). Social isolation: An underappreciated determinant of physical health. Current opinion in psychology, 43, 232–237. [DOI] [PubMed] [Google Scholar]
- Hu X-Y, Cheng Q, Peng X-D, Zhang X-M, & Huang C-Q (2012). Living arrangements and risk for late life depression: a meta-analysis of published literature. The International Journal of Psychiatry in Medicine, 43, 19–34. [DOI] [PubMed] [Google Scholar]
- Huey SJ Jr, & Tilley JL (2018). Effects of mental health interventions with Asian Americans: A review and meta-analysis. Journal of consulting and clinical psychology, 86, 915. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Research on aging, 26, 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imami L, Jiang Y, Murdock KW, & Zilioli S (2022). Links Between Socioeconomic Status, Daily Depressive Affect, Diurnal Cortisol Patterns, and All-Cause Mortality. Psychosomatic Medicine, 84, 29–39. [DOI] [PubMed] [Google Scholar]
- Inoue S, Yorifuji T, Takao S, Doi H, & Kawachi I (2013). Social cohesion and mortality: a survival analysis of older adults in Japan. American journal of public health, 103, e60–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwasa H, Masui Y, Gondo Y, Inagaki H, Kawaai C, & Suzuki T (2008). Personality and all-cause mortality among older adults dwelling in a Japanese community: A five-year population-based prospective cohort study. The American Journal of Geriatric Psychiatry, 16, 399–405. [DOI] [PubMed] [Google Scholar]
- Jensen MT, Marott JL, Holtermann A, & Gyntelberg F (2019). Living alone is associated with all-cause and cardiovascular mortality: 32 years of follow-up in the Copenhagen Male Study. European Heart Journal-Quality of Care and Clinical Outcomes, 5, 208–217. [DOI] [PubMed] [Google Scholar]
- Jeong S, & Cho S.i. (2017). Effects of living alone versus with others and of housemate type on smoking, drinking, dietary habits, and physical activity among elderly people. Epidemiology and health, 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KJ, Latham-Mintus K, & Poey JL (2018). Productive aging via volunteering: Does social cohesion influence level of engagement? Journal of Gerontological Social Work, 61, 817–833. [DOI] [PubMed] [Google Scholar]
- Kandler U, Meisinger C, Baumert J, & Löwel H (2007). Living alone is a risk factor for mortality in men but not women from the general population: a prospective cohort study. BMC Public Health, 7, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S, & Akpom CA (1976). A measure of primary sociobiological functions. International journal of health services, 6, 493–508. [DOI] [PubMed] [Google Scholar]
- Kemp AH, Arias JA, & Fisher Z (2017). Social ties, health and wellbeing: a literature review and model. Neuroscience and social science, 397–427. [Google Scholar]
- Kim W, & Keefe RH (2010). Barriers to healthcare among Asian Americans. Social Work in Public Health, 25, 286–295. [DOI] [PubMed] [Google Scholar]
- Kobayashi LC, & Steptoe A (2018). Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Annals of Behavioral Medicine, 52, 582–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koivunen K, Sillanpää E, von Bonsdorff M, Sakari R, Pynnönen K, & Rantanen T (2020). Living alone vs. living with someone as a predictor of mortality after a bone fracture in older age. Aging clinical and experimental research, 32, 1697–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowitt SD, Aiello AE, Callahan LF, Fisher EB, Gottfredson NC, Jordan JM, et al. (2020). Associations among neighborhood poverty, perceived neighborhood environment, and depressed mood are mediated by physical activity, perceived individual control, and loneliness. Health & place, 62, 102278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee I-M, & Skerrett PJ (2001). Physical activity and all-cause mortality: what is the doseresponse relation? Medicine and science in sports and exercise, 33, S459–S471. [DOI] [PubMed] [Google Scholar]
- Li M, & Dong X (2020). Filial discrepancy and mortality among community-dwelling older adults: a prospective cohort study. Aging & mental health, 24, 1365–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, & Zhang Y (2015). Social network types and the health of older adults: Exploring reciprocal associations. Social science & medicine, 130, 59–68. [DOI] [PubMed] [Google Scholar]
- Manca AR (2014). Social Cohesion. In Michalos AC (Ed.), Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer. [Google Scholar]
- Miao J, Wu X, & Sun X (2019). Neighborhood, social cohesion, and the Elderly’s depression in Shanghai. Social science & medicine, 229, 134–143. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day NE, Alegria M, & Sribney W (2007). Social cohesion, social support, and health among Latinos in the United States. Social science & medicine, 64, 477–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng TP, Jin A, Feng L, Nyunt MSZ, Chow KY, Feng L, et al. (2015). Mortality of older persons living alone: Singapore Longitudinal Ageing Studies. BMC geriatrics, 15, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park NS, Jang Y, Lee BS, & Chiriboga DA (2017). The relation between living alone and depressive symptoms in older Korean Americans: do feelings of loneliness mediate? Aging & mental health, 21, 304–312. [DOI] [PubMed] [Google Scholar]
- Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, & Miret M (2018). Association of loneliness with all-cause mortality: A meta-analysis. PloS one, 13, e0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinette JW, Charles ST, & Gruenewald TL (2018). Neighborhood cohesion, neighborhood disorder, and cardiometabolic risk. Social science & medicine, 198, 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinette JW, Charles ST, Mogle JA, & Almeida DM (2013). Neighborhood cohesion and daily well-being: Results from a diary study. Social science & medicine, 96, 174–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos PMG, Dee EC, & Deville C (2021). Confronting anti-Asian racism and health disparities in the era of COVID-19. JAMA Health Forum pp. e212579-e212579): American Medical Association. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: our view of the state of the art. Psychological methods, 7, 147. [PubMed] [Google Scholar]
- Schmaltz HN, Southern D, Ghali WA, Jelinski SE, Parsons GA, King KM, et al. (2007). Living alone, patient sex and mortality after acute myocardial infarction. Journal of general internal medicine, 22, 572–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenfeld D (1982). Partial residuals for the proportional hazards regression model. Biometrika, 69, 239–241. [Google Scholar]
- Shaw BA, Dahlberg L, Nilsen C, & Agahi N (2020). Trends in the mortality risk of living alone during old age in Sweden, 1992–2011. Journal of Aging and Health, 32, 1399–1408. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Fors S, Fritzell J, Lennartsoon C, & Agahi N (2018). Who lives alone during old age? Trends in the social and functional disadvantages of Sweden’s solitary living older adults. Research on Aging, 40, 815–838. [DOI] [PubMed] [Google Scholar]
- Shen C, Wan A, Kwok LT, Pang S, Wang X, Stewart SM, et al. (2017). A community based intervention program to enhance neighborhood cohesion: The Learning Families Project in Hong Kong. PloS one, 12, e0182722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KJ, & Victor C (2019). Typologies of loneliness, living alone and social isolation, and their associations with physical and mental health. Ageing & Society, 39, 1709–1730. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & and the Patient Health Questionnaire Primary Care Study, G. (1999). Validation and Utility of a Self-report Version of PRIME-MD: The PHQ Primary Care Study. JAMA : the journal of the American Medical Association, 282, 1737–1744. [DOI] [PubMed] [Google Scholar]
- Stahl ST, Beach SR, Musa D, & Schulz R (2017). Living alone and depression: the modifying role of the perceived neighborhood environment. Aging & mental health, 21, 1065–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Shankar A, Demakakos P, & Wardle J (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences, 110, 5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang F, Zhang W, Chi I, Li M, & Dong XQ (2020). Importance of activity engagement and neighborhood to cognitive function among older Chinese Americans. Research on Aging, 42, 226–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teguo MT, Simo-Tabue N, Stoykova R, Meillon C, Cogne M, Amiéva H, et al. (2016). Feelings of loneliness and living alone as predictors of mortality in the elderly: the PAQUID study. Psychosomatic medicine, 78, 904–909. [DOI] [PubMed] [Google Scholar]
- Theeke LA (2009). Predictors of loneliness in US adults over age sixty-five. Archives of psychiatric nursing, 23, 387–396. [DOI] [PubMed] [Google Scholar]
- Wang D, Lau KK-L, Yu R, Wong SY, Kwok TT, & Woo J (2017). Neighbouring green space and mortality in community-dwelling elderly Hong Kong Chinese: a cohort study. BMJ open, 7, e015794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss R (1974). The provisions of social relationships. In Zick R (Ed.), Doing unto others pp. 17–26). Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Wiles JL, Leibing A, Guberman N, Reeve J, & Allen RE (2012). The meaning of “aging in place” to older people. The gerontologist, 52, 357–366. [DOI] [PubMed] [Google Scholar]
- Wolff JL, & Boyd CM (2015). A look at person-centered and family-centered care among older adults: results from a national survey. Journal of general internal medicine, 30, 1497–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R, Wang H, Edelman LS, Tracy EL, Demiris G, Sward KA, et al. (2020). Loneliness as a mediator of the impact of social isolation on cognitive functioning of Chinese older adults. Age and Ageing, 49, 599–604. [DOI] [PubMed] [Google Scholar]
- Yeh SCJ, & Lo SK (2004). Living alone, social support, and feeling lonely among the elderly. Social Behavior and Personality: an international journal, 32, 129–138. [Google Scholar]
- Yu B, Steptoe A, Chen L-J, Chen Y-H, Lin C-H, & Ku P-W (2020). Social isolation, loneliness, and all-cause mortality in patients with cardiovascular disease: a 10-year follow-up study. Psychosomatic medicine, 82, 208–214. [DOI] [PubMed] [Google Scholar]
- Zilioli S, & Jiang Y (2021). Endocrine and immunomodulatory effects of social isolation and loneliness across adulthood. Psychoneuroendocrinology, 128, 105194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


