Abstract
Objective:
To describe the up-to-date trend of total, diagnosed and undiagnosed diabetes and prediabetes, assess their associated disparities among population subgroups, and examine their relationship with sociodemographic factors among adults in the United States (US).
Study design:
This was a cross-sectional study from a nationally representative sample of US adults (⩾20 years old) who participated in the National Health and Nutrition Examination Survey (NHANES).
Methods
Diagnosed diabetes was defined as a self-reported previous diagnosis of diabetes by a physician or any other health professionals (other than during pregnancy). Undiagnosed diabetes was defined as elevated levels of fasting plasma glucose (FPG⩾126 mg/dL) or HbA1c (⩾6.5%). Total diabetes included those who had either diagnosed or undiagnosed diabetes. Prediabetes was defined as a HbA1c level of 5.7% - 6.4% or an FPG level of 100 mg/dL-125 mg/dL. All estimates were age-standardized to the 2010 US census population for age groups 20–44, 45–64, and 65+ years. All analyses accounted for the complex survey design. Logistic regressions were used to conduct the analyses.
Results:
A total of 21,600 (mean, 47.2 years [SD, 14.7]) individuals were analyzed. From 1999 to 2018, the age-standardized prevalence increased significantly from 9.17% to 14.7% (difference, 5.52%; 95% CI, 2.69%–8.35%; P-trend<.001) for total diabetes, increased from 6.15% to 11.0% (difference, 4.79%; 95% CI, 2.27%–7.32%; P-trend<.001) for diagnosed diabetes and remained stable from 3.01% to 3.73% (difference, 0.72%; 95% CI, −0.47% to 1.91%; P-trend=0.19) for undiagnosed diabetes. The age-standardized prevalence of prediabetes increased significantly from 29.5% to 48.3% (difference, 18.8%; 95% CI, 13.3%–24.4%; P-trend<0.001). Disparities persisted with higher prevalence among adults with obesity and populations that have been marginalized including racial and ethnic minorities, low income, less educated Americans, and those living in food-insecure household.
Conclusions:
The prevalence of diabetes and prediabetes increased significantly from 1999 to 2018 among US adults. There are substantial and persistent disparities among racial and ethnic minorities, populations experienceing socioeconomic disadvantages, and adults with obesity.
Keywords: Diabetes, Prediabetes, Health disparities, Chronic Disease, NHANES
Introduction
Diabetes mellitus is a leading cause of death in the United States (US) and globally.1 As a complex chronic metabolic disease, diabetes affects multiple organ systems and is associated with an increased risk of heart disease, stroke, and other serious complications such as kidney failure, blindness, amputation, and severe COVID-19.2,3 Among adults, more than 1 in 10 Americans have diabetes and 1 in 3 have prediabetes.2 Furthermore, more than 25% of adults with diabetes and 80% of those with prediabetes are not aware of their conditions.4 The economic burden of diabetes is high with the estimated direct and indirect cost of $327 billion in 2017.5 Timely and accurate assessment of national trends in diabetes and prediabetes is important to reflect dynamic changes corresponding to policy, systems, and environmental factors and to advance in diabetes awareness, diagnosis, treatment, control, and prevention.
Several previous studies have evaluated the prevalence of diabetes or prediabetes at the population level from 1988–1994 and 1999–2010,6 from 1988–2012,7 from 1999–2010,8 from 1999–2014,9 from 1999–2016,10 and from 2011–2016.11 Their findings suggested a significant increasing pattern in prevalence of diabetes and prediabetes, particularly among racial and ethnic minorities and adults with obesity. However, these studies have important limitations; their data are at this time outdated, their outcomes were restricted to either diabetes or prediabetes, and the scope is narrow in assessment of disparities. Thus, a more recent and comprehensive understanding of the trends in total (diagnosed and undiagnosed) diabetes and prediabetes, and disparities, particularly among diverse race and ethnic groups, individuals with different household incomes, different educational attainments, food security status and health insurance status, is urgently needed. This type of trend assessment could help aid in reducing diabetes-related disparities and promote health equity through the identification of challenges and opportunities for diabetes prevention and management as well as populations at greatest-risk for diabetes and prediabetes.
To fill those research gaps, we used data from the National Health and Nutrition Examination Survey (NHANES) to estimate national trends in prevalence of total diabetes (diagnosed and undiagnosed) and prediabetes over the past 20 years. In addition, we assessed potential disparities in trends by age, gender, race/ethnicity, levels of body mass index (BMI), education, household income, food security status, and insurance status. We also modeled the association of diabetes and prediabetes with those sociodemographic factors.
Methods
Study Design, Population and Data Collection
NHANES is a series of cross-sectional surveys using a complex, multistage probability design to sample the civilian, non-institutionalized population residing in the 50 states and District of Columbia. The NHANES protocol was approved by the Centers for Disease Control and Prevention/National Center for Health Statistics (NCHS) Ethics Review Board, and all participants provided written informed consent. Because the data are publicly available and deidentified, institutional review board approval was not required for this analysis. Details on the study design, protocol, and data collection methods have been documented.12
This investigation used data across 10 cycles of NHANES (1999–2000 through 2017–2018). Of the 101,316 participants, we included adults aged 20 years and older who completed the interview and examination and excluded women who were pregnant because pregnancy could affect glucose measurements (eFigure 1 in the Supplement).
Data were collected through questionnaires (demographics and medical history), a physical examination, and blood collection. Sociodemographic variables included gender, age, race/ethnicity, education level, household income level, household food security status, and insurance status. Age was self-reported during the interview and was grouped into three groups (20–44, 45–64 and 65+). Race/ethnicity data were self-reported in the interview and were categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Asian (hereafter, White, Black, Hispanic, and Asian American). Individuals reporting multiple races were categorized as Other and were included in the analyses of the entire population but not shown separately. Education levels were categorized as less than a high school degree, high school graduate or GED, some college and greater than college graduate. The family income to poverty ratio (IPR) is a measure of family income relative to poverty guidelines specific to the survey year. We classified family income levels into three categories (low-income, IPR <=1.0; middle-income IPR >1 and <4; and high-income, IPR ⩾4.0). Those cutoffs were selected based on the thresholds used in the Patient Protection and Affordable Care Act, in which adults with a PIR between 1 and 4 are eligible for insurance subsidies.13 Information on food security status was collected through the US Household Food Security Survey Module developed by the US Department of Agriculture.14 The module consists of 18 items for households with children under the age of 18 years and 10 items for households without children. Based on the number of affirmative responses, the NCHS created four response levels (full food security, marginal food security, low food security and very low food security). During the examination component in the mobile examination center (MEC), standardized measures of weight and height were obtained, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Blood samples were obtained by trained phlebotomists according to a standardized protocol in the MEC and data were recorded directly into a computerized database.
Definitions of Diabetes and Prediabetes
Diagnosed diabetes was defined as a self-reported previous diagnosis of diabetes by a physician or any other health professional (other than during pregnancy) during the interview. In persons without a previous diagnosis of diabetes, undiagnosed diabetes was defined as having either elevated levels of fasting plasma glucose (FPG⩾126 mg/dL [⩾7.0 mmol/L]) or HbA1c (⩾6.5% [⩾48 mmol/mol]). Total diabetes was defined as any participant who had either diagnosed diabetes or undiagnosed diabetes defined by FPG or HbA1c. Prediabetes was defined as any participant who did not have diabetes but who had a HbA1c level of 5.7% to 6.4% or an FPG level of 100 mg/dL to 125 mg/dL.
Statistical Analysis
Survey analysis procedures were used to account for sampling weights, stratification, and clustering in the NHANES complex sampling design to derive nationally representative estimates. The crude weighted prevalence and 95% confidence intervals (CIs) of total, diagnosed, undiagnosed diabetes and prediabetes were estimated by NHANES cycles from 1999–2000 through 2017–2018. The overall and all stratified estimates by gender, race/ethnicity, family income, education, food security status, insurance status and BMI were age-standardized to the 2010 US census population using standardizing proportions for the age groups 20–44 years, 45–64 years, and 65 years or older, allowing comparisons independent of age.
To evaluate trends over time, survey-weighted logistic regression was used to calculate a P-value for crude and age-standardized trends across cycles overall and by subgroups. To access statistical heterogeneity of trends by subgroups, a survey-weighted Wald test was used to test for an interaction term between cycle and sociodemographic factors (i.e., age, gender, race/ethnicity, household income, education, food security status, insurance status and BMI). Survey-weighted Poisson regression models with robust standard errors were used to examine the associations of those sociodemographic factors with the prevalence of total, diagnosed, undiagnosed diabetes and prediabetes using NHANES cycles of 2015–2016 and 2017–2018. Adjusted prevalence ratios (aPR) and corresponding 95% CIs are presented.
Interview weights were used to estimate diagnosed diabetes whereas examination weights were used for undiagnosed diabetes and prediabetes identified by HbA1c and FPG. The use of different sample weights, which account for differential probabilities of selection, nonresponse, and noncoverage, for different set of analyses maximizes the use of survey information and sample sizes.
To assess whether observed trends were driven by sociodemographic factor shifts, we performed a sensitivity analysis that adjusted for those factors in the study. All statistical analyses were performed using Stata version 14.0 (Stata Corp, College Station). A two-sided P values <0.05 was considered statistically significant. P-values were not adjusted for multiple testing and should be interpreted as exploratory.
Results
Characteristics of Study Population
Over these 10 NHANES cycles from 1999–2000 through 2017–2018, a total of 21,600 adults aged 20 years or older (mean age 47.2 years, [SD, 14.7 years]; 51.2% female) were analyzed and their characteristics were presented in Table 1. The study population became older and more diverse over the study period. The adults with obesity increased from 29.1% to 40.3% whereas the adults with normal weight decreased from 36.8% to 26.5%. In addition, the proportion of participants with less than high school education dropped from 24.1% to 11.8% while those with a college degree or above increased from 22.3% to 29.4%. Adults living in full food-secure households dropped from 85.1% to 70.5% while those living in food insecure households increased.
Table 1.
Participant Sociodemographic by NHANES Cycle, 1999–2000 to 2017–2018
| Characteristics | N (Survey-Weighted %)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 (n=1,737) |
2001–2002 (n=2,078) |
2003–2004 (n=1,874) |
2005–2006 (n=1,824) |
2007–2008 (n=2,329) |
2009–2010 (n=2,585) |
2011–2012 (n=2,287) |
2013–2014 (n=2,368) |
2015–2016 (n=2,244) |
2017–2018 (n=2,274) |
|
| Age group | ||||||||||
| 20–44 | 711 (51.8) | 870 (48.8) | 747 (49.3) | 762 (45.9) | 895 (45.8) | 1062(46.3) | 1009(45.7) | 985 (45.9) | 884 (43.7) | 827 (42.3) |
| 45–64 | 566 (31.8) | 680 (35.6) | 575 (34.6) | 596 (36.6) | 821 (37.2) | 898 (35.4) | 779 (36.6) | 844 (35.3) | 793 (35.9) | 863 (37.2) |
| ≥65 | 460 (16.3) | 528 (15.6) | 552 (16.1) | 466 (17.5) | 613 (17.0) | 625 (18.3) | 499 (17.7) | 539 (18.8) | 567 (20.4) | 584 (20.5) |
| Sex | ||||||||||
| Male | 865 (49.1) | 1050(49.1) | 946 (48.9) | 956 (48.8) | 1144(48.9) | 1220(49.0) | 1145(48.3) | 1139(48.6) | 1093(48.6) | 1093(48.7) |
| Female | 872 (50.9) | 1028(50.9) | 928 (51.1) | 868 (51.2) | 1185(51.1) | 1365(51.1) | 1142(51.7) | 1229(51.4) | 1151(51.4) | 1181(51.3) |
| Race/ethnicity | ||||||||||
| Non-Hispanic White | 787 (70.5) | 1123(73.5) | 1022(72.1) | 932 (72.3) | 1130(70.3) | 1224(68.3) | 884 (66.7) | 1058(66.5) | 765 (63.8) | 757 (61.9) |
| Non-Hispanic Black | 314 (10.8) | 365 (10.0) | 349 (11.2) | 415 (11.0) | 436 (10.9) | 426 (11.0) | 527 (11.4) | 435 (11.4) | 454 (11.4) | 515 (11.3) |
| Non-Hispanic Asian | 332 (5.29) | 287 (5.25) | 260 (5.82) | 326 (5.65) | ||||||
| Hispanic | 593 (15.2) | 526 (11.9) | 423 (10.9) | 401 (11.2) | 676 (13.0) | 794 (13.7) | 483 (14.1) | 532 (14.8) | 688 (15.0) | 548 (16.3) |
| Others | ||||||||||
| Weight Categories | ||||||||||
| Underweight | 29 (2.50) | 29 (1.58) | 24 (1.50) | 33 (1.98) | 34 (1.60) | 36 (1.79) | 47 (1.67) | 42 (1.58) | 43 (2.35) | 30 (1.27) |
| Normal weight | 561 (36.8) | 624 (32.6) | 541 (31.7) | 516 (30.9) | 626 (31.2) | 677 (29.3) | 659 (29.3) | 681 (28.1) | 557 (24.8) | 561 (26.5) |
| Overweight | 592 (31.5) | 764 (37.2) | 660 (34.2) | 587 (32.0) | 808 (34.6) | 871 (32.5) | 722 (32.8) | 754 (33.0) | 725 (32.0) | 716 (31.9) |
| Obese | 545 (29.1) | 578 (28.6) | 621 (32.6) | 654 (35.1) | 821 (32.6) | 978 (36.4) | 833 (36.2) | 869 (37.3) | 902 (40.8) | 930 (40.3) |
| Education | ||||||||||
| <High school | 666 (24.1) | 616 (19.3) | 542 (18.3) | 483 (17.1) | 693 (19.4) | 746 (18.7) | 534 (17.5) | 521 (16.2) | 525 (15.1) | 474 (11.8) |
| High school graduate or GED | 380 (26.7) | 476 (25.4) | 462 (26.3) | 452 (26.2) | 581 (24.8) | 573 (22.3) | 481 (19.8) | 511 (20.9) | 489 (21.7) | 539 (28.0) |
| Some college | 404 (26.9) | 586 (31.9) | 511 (31.5) | 542 (32.2) | 581 (28.1) | 727 (30.2) | 665 (31.5) | 718 (32.4) | 654 (31.7) | 726 (30.8) |
| ≥College | 283 (22.3) | 395 (23.4) | 356 (24.0) | 344 (24.5) | 472 (27.7) | 533 (28.8) | 606 (31.2) | 616 (30.5) | 576 (31.5) | 533 (29.4) |
| Income levels | ||||||||||
| Low | 280 (13.2) | 332 (14.1) | 301 (12.1) | 283 (9.98) | 413 (13.6) | 519 (14.6) | 506 (16.3) | 508 (17.4) | 472 (15.1) | 365 (12.9) |
| Middle | 806 (49.9) | 1020 49.2) | 1000 52.4) | 986 (54.2) | 1176 48.6) | 1243(51.3) | 1080(50.2) | 1127(48.4) | 1071(49.2) | 1100(50.3) |
| High | 426 (36.9) | 587 (36.7) | 467 (35.5) | 473 (35.9) | 548 (37.8) | 576 (34.1) | 515 (33.5) | 575 (34.1) | 483 (35.7) | 512 (36.8) |
| Food Security Status | ||||||||||
| Very low | 63 (3.13) | 73 (3.59) | 92 (4.64) | 86 (3.60) | 116 (3.50) | 180 (4.74) | 164 (6.16) | 156 (5.67) | 191 (6.62) | - |
| Low | 167 (6.52) | 168 (5.44) | 149 (6.36) | 172 (6.31) | 252 (8.04) | 334 (9.76) | 303 (10.5) | 254 (9.17) | 357 (11.8) | - |
| Marginal | 115 (5.22) | 132 (5.16) | 123 (4.80) | 182 (8.23) | 226 (7.42) | 276 (7.77) | 274 (9.79) | 262 (9.93) | 296 (11.1) | - |
| Full | 1368(85.1) | 1591(85.8) | 1432(84.2) | 1370(81.9) | 1723(81.0) | 1764(77.7) | 1536(73.5) | 1680(75.2) | 1340(70.5) | - |
| Insurance status | ||||||||||
| Yes | 1369(83.1) | 1668(83.6) | 1479(80.4) | 1427(80.8) | 1780(82.1) | 1901(78.4) | 1751(80.0) | 1868(82.0) | 1835(85.7) | 1921(85.9) |
| No | 348(16.9) | 387(16.4) | 382(19.6) | 395(19.2) | 545(17.9) | 682(21.6) | 535 (20.0) | 497 (18.0) | 402 (14.3) | 349 (14.2) |
Abbreviation: GED, general equivalency diploma; NHANES, National Health and Nutrition Examination Survey.
Data were weighted to be nationally representative.
Trends and Disparities in Prevalence of Total, Diagnosed and Undiagnosed Diabetes
From 1999 to 2018, the age-standardized prevalence of total diabetes increased significantly from 9.17% to 14.7% (difference, 5.52%; 95% CI, 2.69%–8.35%; P-trend<.001). The age-standardized prevalence of diagnosed diabetes increased from 6.15% to 11.0% (difference, 4.79%; 95% CI, 2.27%–7.32%; P-trend<.001) whereas that of undiagnosed diabetes remained stable from 3.01% to 3.73% (difference, 0.72%; 95% CI, −0.47% to 1.91%; P-trend=0.19) (Table 2). The findings in prevalence of total, diagnosed and undiagnosed diabetes for sensitivity analysis were not materially altered after adjusting for sociodemographic factors (eTable 1 in the Supplement).
Table 2.
Trends in Age-Standardized Prevalence of Total, Diagnosed and Undiagnosed Diabetes and Prediabetes Among US Adults Aged 20 Years or Older by NHANES Survey Cycle, 1999–2018
| Prevalence | Survey-Weighted % (95% CI)a | P-trend | Difference, 2017–2018 vs 1999–2000 (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 (n=1,737) |
2001–2002 (n=2,078) |
2003–2004 (n=1,874) |
2005–2006 (n=1,824) |
2007–2008 (n=2,329) |
2009–2010 (n=2,585) |
2011–2012 (n=2,287) |
2013–2014 (n=2,368) |
2015–2016 (n=2,244) |
2017–2018 (n=2,274) |
|||
| Total diabetes | 9.17 (7.39–11.3) | 11.0 (9.25–13.0) | 10.9 (9.17–12.8) | 11.3 (9.62–13.2) | 12.7 (11.3–14.4) | 12.8 (11.0–14.9) | 13.2 (10.9–15.8) | 13.6 (12.1–15.2) | 14.6 (13.0–16.3) | 14.7 (12.8–16.8) | <.001 | 5.52 (2.69–8.35) |
| Diagnosed | 6.15 (4.65–8.10) | 7.09 (5.73–8.74) | 7.59 (6.21–9.24) | 7.89 (6.62–9.39) | 8.63 (7.39–10.1) | 8.47 (6.99–10.2) | 9.19 (7.33–11.5) | 9.90 (8.52–11.5) | 10.6 (9.13–12.3) | 11.0 (9.23–13.0) | <.001 | 4.79 (2.27–7.32) |
| Undiagnosed | 3.01 (2.26–4.0) | 3.88 (3.13–4.79) | 3.28 (2.46–4.37) | 3.38 (2.54–4.49) | 4.10 (3.41–4.92) | 4.33 (3.53–5.29) | 3.96 (2.97–5.28) | 3.66 (3.02–4.43) | 3.93 (3.17–4.87) | 3.73 (2.99–4.65) | 0.19 | 0.72 (−0.47, 1.91) |
| Prediabetes | 29.5 (25.4–33.9) | 35.0 (31.8–38.3) | 32.5 (28.5–36.7) | 37.8 (33.9–41.8) | 49.0 (46.3–51.8) | 45.5 (43.0–47.9) | 45.2 (41.8–48.7) | 40.7 (37.1–44.4) | 44.3 (40.8–47.8) | 48.3 (44.8–51.9) | <.001 | 18.8 (13.3–24.4) |
Abbreviation: NHANES, National Health and Nutrition Examination Survey.
Data were weighted to be nationally representative. Overall age-adjusted and by other stratums were age adjusted to 2010 US census population using age groups 20–44 years, 45–64 years, and ≥65 years.
Trends in age-standardized prevalence of total diabetes increased among most of subgroups except young adults aged 20–44 years, individuals with normal weight, and those with very low and marginal food security status showing no significant change (eTable 2 in the Supplement). Differences in prevalence of total diabetes persisted by age group, gender, race/ethnicity, BMI level, educational level, household income level and food security status. For example, by race/ethnicity, the age-adjusted prevalence of total diabetes increased from 8.77% (95% CI, 7.33%–10.5%) to 12.5% (95% CI, 11.0%–14.3%) (P-trend<.001) among White participants; from 14.3% (95% CI, 12.2%–16.8%) to 19.0% (95% CI, 17.2%–21.0%) (P-trend=.02) among Black participants; and from 13.7% (95% CI, 10.8%–17.1%) to 21.3% (95% CI, 19.6%–23.0%) (P-trend<.001) among Hispanic participants; and from 17.6% (95% CI, 14.7%–20.9%) to 17.6% (95% CI, 15.1%–20.5%) among Asian American participants (from 2011 to 2018; P-trend=0.28) (Figure 1). By household income, the age-standardized prevalence of total diabetes increased from 15.5% (95% CI, 12.7%–18.9%) to 19.5% (95% CI, 17.0%–22.2%) (P-trend=.004) for low-income participants and increased from 6.85% (95% CI, 5.28%–8.84%) to 11.5% (95% CI, 9.34%–14.1%) (P-trend=.001) for high-income participants (Figure 1). Similar findings were found for the prevalence of diagnosed diabetes (eTable 3 in the Supplement). Trends in prevalence of undiagnosed diabetes remained stable among most of subgroups except an increasing trend in young adults aged 20–44 years (P-trend=.04) and Hispanic adults from 2.77% (95% CI, 1.88%–4.06%) to 5.50% (95% CI, 4.27%–7.05%) (P-trend=.01) (eTable 4 in the Supplement). Trends in percentages of undiagnosed diabetes out of total diabetes slightly decreased overall but remained stable among most of the subgroups except decreasing trends observed among older adults (eTable 5 in the Supplement).
Figure 1.
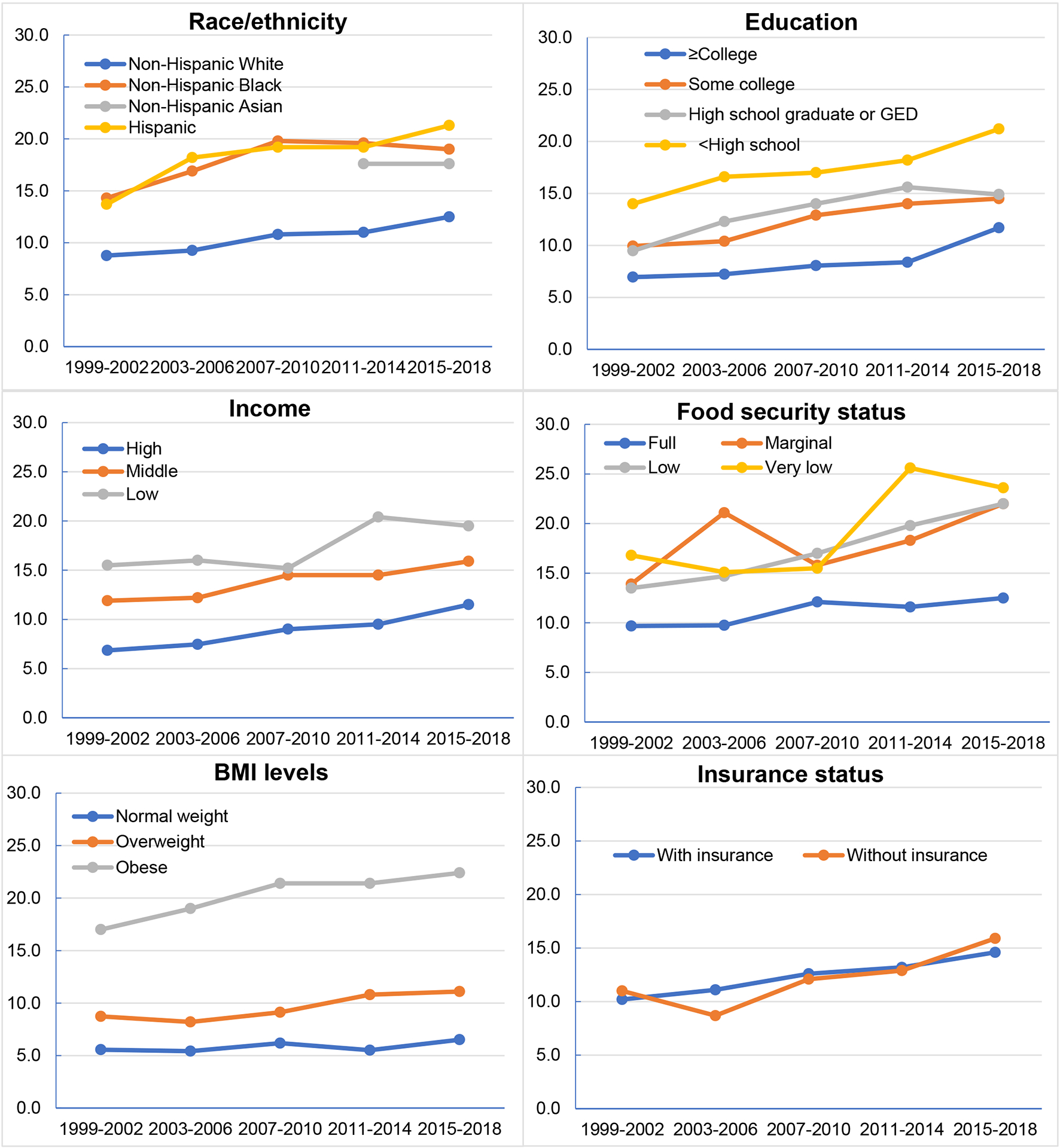
Trends in age-adjusted prevalence of total diabetes among US adults (20+), NHANES 1999–2018 by race/ethnicity, education, income, food security status, body mass index levels and insurance status (Details see in Supplemental Table 2).
Trends and Disparities in Prevalence of Prediabetes
Over the study period, the trend in age-standardized prevalence of prediabetes increased significantly from 29.5% to 48.3% (difference, 18.8%; 95% CI, 13.3%–24.4%; P-trend<0.001) (Figure 2, Table 2) overall and by population subgroups (eTable 6 in the Supplement). The findings in prevalence of prediabetes for sensitivity analysis were also not materially altered after adjusting for sociodemographic factors (eTable 1 in the Supplement). The rate of increase in prediabetes prevalence was higher for young adults compared to older adults (P-interaction<.001) and was lower among participants with obesity as compared to individuals with normal weight (P-interaction=.01). The differences in prevalence of prediabetes persisted and was more pronounced among older adults, male, and participants with obesity. For example, the age-standardized prevalence of prediabetes increased from 20.8% (95% CI, 17.7%–24.4%) to 35.8% (95% CI, 32.2%–39.6%) among participants with normal weight and from 41.8% (95% CI, 38.0%–45.6%) to 51.2% (95% CI, 47.8%–54.6%) among individuals with obesity.
Figure 2.
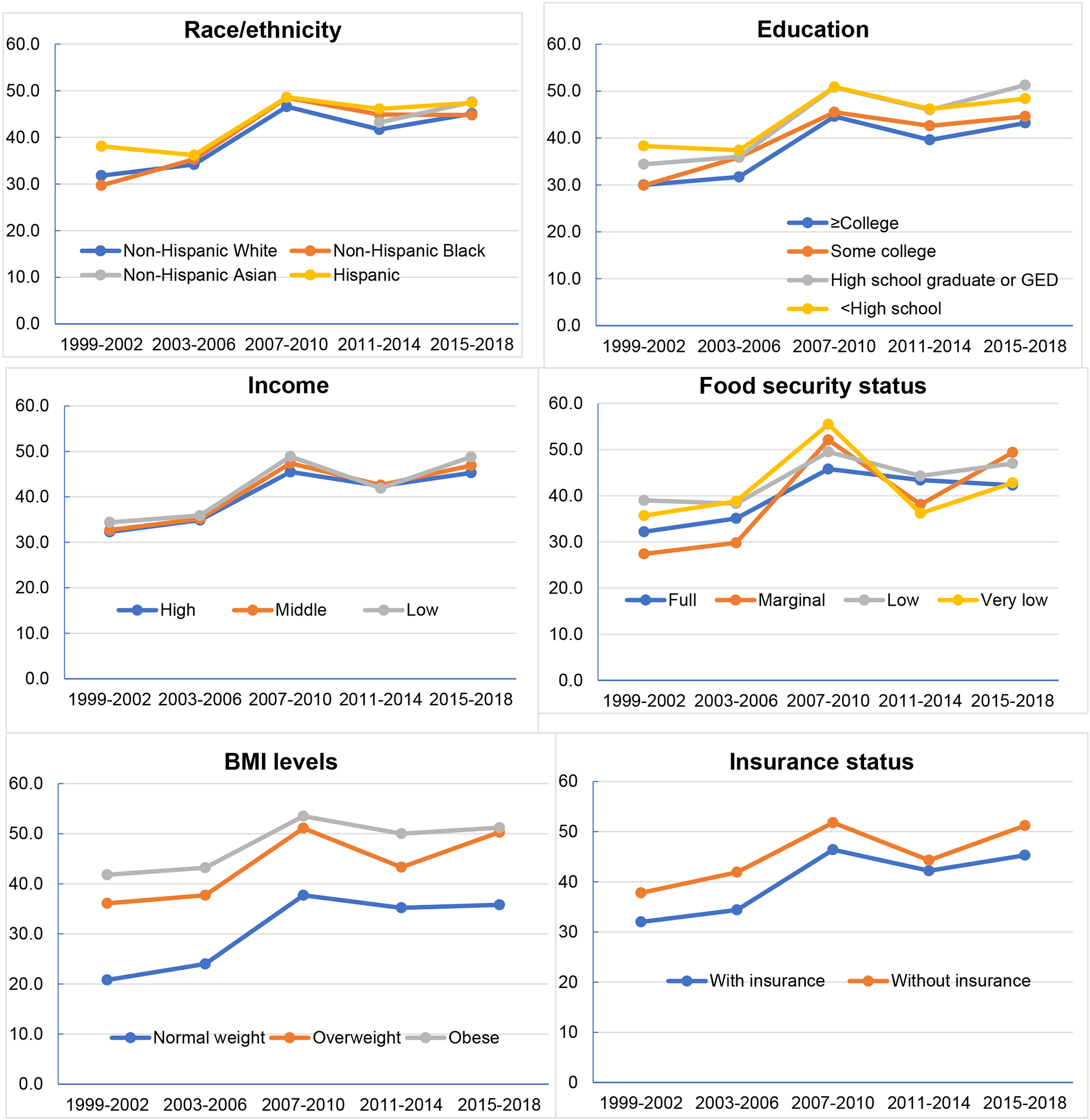
Trends in age-adjusted prevalence of prediabetes among US adults (20+), NHANES 1999–2018 by race/ethnicity, education, income, food security status, body mass index levels and insurance status (Details see in Supplemental Table 6).
Association of Diabetes and Prediabetes with Sociodemographic Factors
In multivariable Poisson regression models, we found that age, gender, race/ethnicity, and BMI were significantly associated with total diabetes, diagnosed and undiagnosed diabetes, and prediabetes (Table 3). For example, compared with White adults, significant higher risk of having total diabetes were found among Black adults (aPR, 1.40; 95% CI, 1.23–1.61); among Hispanic adults (aPR, 1.38; 95% CI, 1.21–1.57); and among Asian American adults (aPR, 2.18; 95% CI, 1.74–2.70). Compared with adults with normal weight, adults with obesity had an aPR of 3.86 (95% CI, 3.19–4.67) for total diabetes, 3.77 (2.93–4.84) for diagnosed diabetes, 4.12 (2.74–6.21) for undiagnosed diabetes, and 1.42 (1.29–1.58) for prediabetes. In addition, income levels, education levels, food security status and insurance status were significantly associated with total diabetes; education, food security status and insurance status were associated with diagnosed diabetes; and only income was associated with undiagnosed diabetes.
Table 3:
Weighted Poisson Regression Models for Total, Diagnosed, and Undiagnosed Diabetes and Prediabetes Among US Adults 20 Years or Older, NHANES 2015–2018
| Characteristics | Total diabetes | Diagnosed diabetes | Undiagnosed diabetes | Prediabetes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Adjusted prevalence ratio (95% CI) | P value | Cases | Adjusted prevalence ratio (95% CI) | P value | Cases | Adjusted prevalence ratio (95% CI) | P value | Cases | Adjusted prevalence ratio (95% CI) | P value | |
| Age group | ||||||||||||
| 20–44 | 223 | 1.00 (reference) | 132 | 1.00 (reference) | 91 | 1.00 (reference) | 1356 | 1.00 (reference) | ||||
| 45–64 | 817 | 4.06 (3.32–4.98) | <0.001 | 589 | 4.85 (3.66–6.43) | <0.001 | 228 | 2.95 (2.02–4.30) | <0.001 | 1704 | 1.39 (1.28–1.50) | <0.001 |
| ≥65 | 767 | 6.37 (5.24–7.74) | <0.001 | 602 | 8.52 (6.61–11.0) | <0.001 | 165 | 3.23 (2.13–4.88) | <0.001 | 1148 | 1.59 (1.46–1.72) | <0.001 |
| Sex | ||||||||||||
| Male | 958 | 1.00 (reference) | 696 | 1.00 (reference) | 262 | 1.00 (reference) | 2247 | 1.00 (reference) | ||||
| Female | 849 | 0.76 (0.69–0.85) | <0.001 | 627 | 0.78 (0.67–0.91) | 0.02 | 222 | 0.72 (0.53–0.97) | 0.03 | 1961 | 0.81 (0.75–0.87) | <0.001 |
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | 571 | 1.00 (reference) | 425 | 1.00 (reference) | 146 | 1.00 (reference) | 1565 | 1.00 (reference) | ||||
| Non-Hispanic Black | 443 | 1.40 (1.23–1.61) | <0.001 | 333 | 1.42 (1.22–1.65) | <.001 | 110 | 1.36 (0.98–1.88) | 0.06 | 897 | 1.03 (0.95–1.12) | 0.42 |
| All Hispanic | 522 | 1.38 (1.21–1.57) | <0.001 | 380 | 1.36 (1.15–1.61) | <.001 | 142 | 1.41 (1.09–1.84) | 0.01 | 1053 | 1.05 (0.96–1.14) | 0.29 |
| Non-Hispanic Asian | 211 | 2.18 (1.74–2.70) | <0.001 | 135 | 1.97 (1.55–2.49) | <.001 | 76 | 2.71 (1.82–4.03) | <0.001 | 557 | 1.21 (1.11–1.33) | <0.001 |
| Others | 60 | 1.15 (0.75–1.75) | 0.47 | 50 | 1.31 (0.85–2.04) | 0.22 | 10 | 0.71 (0.34–1.48) | 0.35 | 136 | 1.14 (0.94–1.38) | 0.18 |
| Weight Categories | ||||||||||||
| Underweight | 8 | 0.74 (0.95–1.45) | 0.60 | 8 | 1.04 (0.52–2.10) | 0.90 | 0 | - | - | 42 | 0.82 (0.63–1.08) | 0.16 |
| Normal weight | 240 | 1.00 (reference) | 171 | 1.00 (reference) | 69 | 1.00 (reference) | 961 | 1.00 (reference) | ||||
| Overweight | 517 | 1.86 (1.49–2.31) | <0.001 | 393 | 1.90 (1.45–2.48) | <0.001 | 124 | 1.75 (1.09–2.82) | 0.02 | 1427 | 1.30 (1.17–1.44) | <0.001 |
| Obese | 1013 | 3.86 (3.19–4.67) | <0.001 | 729 | 3.77 (2.93–4.84) | <0.001 | 284 | 4.12 (2.74–6.21) | <0.001 | 1744 | 1.42 (1.29–1.58) | <0.001 |
| Income levels | ||||||||||||
| Low | 411 | 1.00 (reference) | 300 | 1.00 (reference) | 111 | 1.00 (reference) | 1.00 (reference) | |||||
| Middle | 889 | 0.91 (0.79–1.04) | 0.03 | 651 | 0.98 (0.80–1.19) | 0.83 | 238 | 0.76 (0.54–1.08) | 0.12 | 835 | 0.98 (0.89–1.09) | 0.75 |
| High | 327 | 0.78 (0.62–0.99) | 0.04 | 240 | 0.93 (0.69–1.23) | 0.58 | 87 | 0.52 (0.34–0.80) | 0.004 | 1997 | 1.0 (0.87–1.15) | 0.98 |
| Education | 962 | |||||||||||
| <High school | 562 | 1.00 (reference) | 419 | 1.00 (reference) | 143 | 1.00 (reference) | 985 | 1.00 (reference) | ||||
| High school graduate or GED | 412 | 0.88 (0.73–1.07) | 0.20 | 290 | 0.89 (0.70–1.14) | 0.35 | 122 | 0.86 (0.62–1.20) | 0.38 | 1003 | 1.07 (0.97–1.17) | 0.20 |
| Some college | 493 | 0.83 (0.70–0.97) | 0.02 | 369 | 0.81 (0.65–1.01) | 0.06 | 124 | 0.86 (0.62–1.21) | 038 | 1223 | 0.96 (0.88–1.06) | 0.44 |
| ≥College | 338 | 0.71 (0.58–0.88) | 0.002 | 243 | 0.65 (0.49–0.87) | 0.005 | 95 | 0.90 (0.58–1.37) | 0.61 | 995 | 0.94 (0.83–1.06) | 0.28 |
| Food Security Status | ||||||||||||
| Very low | 130 | 1.24 (0.97–1.59) | 0.09 | 96 | 1.38 (1.01–1.89) | 0.049 | 34 | 0.96 (0.54–1.70) | 0.89 | 215 | 0.94 (0.85–1.04) | 0.22 |
| Low | 195 | 1.25 (1.02–1.54) | 0.03 | 146 | 1.42 (1.09–1.83) | 0.01 | 49 | 0.91 (0.65–1.27) | 0.57 | 414 | 0.98 (0.87–1.10) | 0.68 |
| Marginal | 165 | 1.24 (0.97–1.59) | 0.09 | 122 | 1.25 (1.01–1.56) | 0.045 | 43 | 1.02 (0.65–1.58) | 0.94 | 359 | 1.04 (0.94–1.15) | 0.43 |
| Full | 793 | 1.00 (reference) | 558 | 1.00 (reference) | 235 | 1.00 (reference) | 2087 | 1.00 (reference) | ||||
| Insurance status | ||||||||||||
| Yes | 1556 | 1.15 (0.97–1.36) | 0.11 | 1164 | 1.28 (1.02–1.59) | 0.03 | 392 | 0.93 (0.69–1.26) | 0.65 | 3372 | 0.94 (0.85–1.04) | 0.25 |
| No | 247 | 1.00 (reference) | 157 | 1.00 (reference) | 90 | 1.00 (reference) | 825 | 1.00 (reference) | ||||
Abbreviation: GED, general equivalency diploma; NHANES, National Health and Nutrition Examination Survey.
Data were weighted to be nationally representative.
Discussion
In this nationally representative sample of US adults, we reported trends in age-standardized prevalence of total diabetes, diagnosed and undiagnosed diabetes, and prediabetes, and their disparities by population subgroups from 1999–2000 to 2017–2018. We found that the age-standardized prevalence of total diabetes, diagnosed diabetes and prediabetes significantly increased over the study period overall and among most of population subgroups with few exceptions such as normal-weight individuals for total diabetes. The prevalence of undiagnosed diabetes remained stable, accounting for one third of total diabetes. Disparities in prevalence of diabetes and prediabetes persisted among subgroups; prevalence estimates were significantly higher among older adults, male, racial minorities, lower educational attainment, lower household income, food insecure, and higher BMI levels.
We additionally reported the multivariable-adjusted association of total diabetes, diagnosed and undiagnosed diabetes, and prediabetes with sociodemographic factors. Higher odds of diabetes or prediabetes were found among older vs younger adults, male vs female, Asian Americans, Black and Hispanic Americans vs white participants, higher vs lower BMI levels, higher vs lower educational attainment, higher vs lower household income, food insecure vs food secure, and insured vs uninsured adults.
Our study is consistent with prior work demonstrating that diabetes is one of the fastest growing diseases.2,7,11,15,16 Our findings update previous trend analyses with recent nationally representative data and suggest that diabetes continues to be a major health concern in the US. Not only does diabetes increase risk of premature death and serious health complications,2 but diabetes also exacerbates the clinical severity of the COVID-19. A recent modeling study conducted in US estimated that one in five COVID-19 hospitalizations were attributable to diabetes.3
The rise in diabetes prevalence may be due to several factors, including the increase in obesity prevalence, shifting age demographics, and improvements in diagnosis and management of diabetes. Previous studies have suggested that the most significant driver of the rising trend for diabetes and prediabetes is an increasing trend of obesity.17 Obesity is the leading risk factor for high blood glucose, causing changes in the body’s ability to regulate insulin and contributing to the pathophysiology of type 1 and type 2 diabetes.18,19 From 1999–2000 and 2017–2018, the age-standardized prevalence of obesity significantly increased from 27.5% to 43.0%.20 Demographic shifts in the aging population may also contribute to increasing diabetes prevalence. Improvements in diabetes care and management has reduced morbidity and improved survival.21,22 Furthermore, prior research showed that expanding healthcare coverage facilitates the diagnosis of diabetes.23 Our study found that insured adults had significantly higher odds of total and diagnosed diabetes but not prediabetes compared to uninsured individuals.
Substantial disparities exist in prevalence of diabetes and prediabetes. Persistent higher prevalence of diabetes and prediabetes were observed among populations experiencing structural racism and racial/ethnic and socioeconomic marginalization, including Black, Hispanic, Asian American, low-income, less-educated and food insecure adults. These findings are consistent with previous studies assessing diabetes,11,24 suggesting that structural and social determinants of health are key drivers of health disparities and need to be addressed to promote health equity.25 Another related foci contributable to those disparities is inequitable access to healthy diets. For example, using data from NHANES researchers have shown that Black and Hispanic participants had higher proportions of poor diet quality compared to their White counterparts.26 The COVID-19 pandemic further exposed the impact of structural racism and systemic inequity on health. The proportion of COVID-19 hospitalizations attributable to diabetes was highest among Hispanics, followed by Asian Americans, Blacks and Whites.3 The integration of social determinants of health into healthcare has become recognized as an important strategy to reduce health disparities. Future research is needed to explore the effectiveness of interventions addressing and eliminating the root causes of diabetes disparities to promote health equity.27
Strengths of this study included assessment of the most up-to-date available data from NHANES to evaluate trends over the past 20 years, objective measurements on diabetes-related biomarkers, examination of potential disparities by diverse sociodemographic subgroups, and investigation of the multiple-adjusted associations of total, diagnosed and undiagnosed diabetes and prediabetes with sociodemographic factors. This study has several limitations. First, institutionalized individuals (eg, nursing home residents) were not sampled in the NHANES, which may underestimate the prevalence of prediabetes and diabetes. Second, information on subtype of diabetes is not collected, type 1 and type 2 diabetes were hence indistinguishable, and we could not report them separately. Third, even though Asian Americans was separately reported, this measure is still a composite measure that could not reflect their heterogeneity in prevalence of diabetes and prediabetes built-in Asian origin. Fourth, due to lack of information on 2-hour PG in NHANES from 1999 to 2004 and 2017–2018, our analysis did not incorporate this information, which may underestimate undiagnosed diabetes. However, 2-hour PG is not frequently used in clinic settings due to high cost and burdensome for the patients.
Conclusion
From 1999–2000 to 2017–2018, the age-standardized prevalence of total diabetes, diagnosed and undiagnosed diabetes, and prediabetes significantly increased among US adults. Disparities persisted and higher prevalence over time was observed among populations experiencing marginalization including racial minorities, adults with low income and educational attainment, and adults living in food-insecure households.
Supplementary Material
Acknowledgements
This study was supported by the National Heart, Lung, and Blood Institute of the NIH under award number R01HL141427. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Control CfD, Prevention. National diabetes statistics report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services. 2020:12–15. [Google Scholar]
- 3.O’Hearn M, Liu J, Cudhea F, Micha R, Mozaffarian D. Coronavirus Disease 2019 Hospitalizations Attributable to Cardiometabolic Conditions in the United States: A Comparative Risk Assessment Analysis. J Am Heart Assoc. 2021;10(5):e019259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020. [Google Scholar]
- 5.American Diabetes A. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med. 2014;160(8):517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–1029. [DOI] [PubMed] [Google Scholar]
- 8.Zhang N, Yang X, Zhu X, Zhao B, Huang T, Ji Q. Type 2 diabetes mellitus unawareness, prevalence, trends and risk factors: National Health and Nutrition Examination Survey (NHANES) 1999–2010. J Int Med Res. 2017;45(2):594–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caspard H, Jabbour S, Hammar N, Fenici P, Sheehan JJ, Kosiborod M. Recent trends in the prevalence of type 2 diabetes and the association with abdominal obesity lead to growing health disparities in the USA: An analysis of the NHANES surveys from 1999 to 2014. Diabetes Obes Metab. 2018;20(3):667–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang M Trends in the Prevalence of Diabetes Among U.S. Adults: 1999–2016. Am J Prev Med. 2018;55(4):497–505. [DOI] [PubMed] [Google Scholar]
- 11.Cheng YJ, Kanaya AM, Araneta MRG, et al. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011–2016. JAMA. 2019;322(24):2389–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. NHANES Questionnaires, Datasets, and Related Documentation. Available at, https://wwwn.cdc.gov/nchs/nhanes/default.aspx. Accessed on Mary 31, 2021.
- 13.Odutayo A, Gill P, Shepherd S, et al. Income Disparities in Absolute Cardiovascular Risk and Cardiovascular Risk Factors in the United States, 1999–2014. JAMA Cardiol. 2017;2(7):782–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security Revised 2000. U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. March, 2000. Available from: https://www.fns.usda.gov/guide-measuring-household-food-security-revised-2000 [Google Scholar]
- 15.Chan JCN, Lim LL, Wareham NJ, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396(10267):2019–2082. [DOI] [PubMed] [Google Scholar]
- 16.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312(12):1218–1226. [DOI] [PubMed] [Google Scholar]
- 17.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 18.Barnes AS. The epidemic of obesity and diabetes: trends and treatments. Tex Heart Inst J. 2011;38(2):142–144. [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 2014;7:587–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogden CL, Fryar CD, Martin CB, et al. Trends in Obesity Prevalence by Race and Hispanic Origin- 1999–2000 to 2017–2018. JAMA. 2020;324(12):1208–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raghavan S, Vassy JL, Ho YL, et al. Diabetes Mellitus-Related All-Cause and Cardiovascular Mortality in a National Cohort of Adults. J Am Heart Assoc. 2019;8(4):e011295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–1523. [DOI] [PubMed] [Google Scholar]
- 23.Marino M, Angier H, Springer R, et al. The Affordable Care Act: Effects of Insurance on Diabetes Biomarkers. Diabetes Care. 2020;43(9):2074–2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social Determinants of Health and Diabetes: A Scientific Review. Diabetes Care. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999–2012. JAMA. 2016;315(23):2542–2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daniel H, Bornstein SS, Kane GC, Health, Public Policy Committee of the American College of P. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577–578. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


